Fri, Apr 19, 2024
Volume 1, Issue 1 (6-2015)
Iran J Neurosurg 2015, 1(1): 10-22 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Salehpoor F, Meshkini A, Shokouhi G, Aghazade J, Lotfinia I, Shakeri M, et al . Prognostic Serum Factors in Traumatic Brian Injury: A Systematic Review. Iran J Neurosurg 2015; 1 (1) :10-22
URL: http://irjns.org/article-1-1-en.html
URL: http://irjns.org/article-1-1-en.html
Firooz Salehpoor 

 , Ali Meshkini
, Ali Meshkini 
 , Ghaffar Shokouhi
, Ghaffar Shokouhi 
 , Javad Aghazade
, Javad Aghazade 
 , Iraj Lotfinia
, Iraj Lotfinia 
 , Moslem Shakeri
, Moslem Shakeri 
 , Mohammad Shimia
, Mohammad Shimia 
 , Alireza Razzaghi
, Alireza Razzaghi 
 , Farhad Mirzaee
, Farhad Mirzaee 
 , Atta Mahdkhah *
, Atta Mahdkhah * 
 1
1


 , Ali Meshkini
, Ali Meshkini 
 , Ghaffar Shokouhi
, Ghaffar Shokouhi 
 , Javad Aghazade
, Javad Aghazade 
 , Iraj Lotfinia
, Iraj Lotfinia 
 , Moslem Shakeri
, Moslem Shakeri 
 , Mohammad Shimia
, Mohammad Shimia 
 , Alireza Razzaghi
, Alireza Razzaghi 
 , Farhad Mirzaee
, Farhad Mirzaee 
 , Atta Mahdkhah *
, Atta Mahdkhah * 
 1
1
1- , mahdkhah@yahoo.com
Full Text [PDF 647 kb]
(3520 Downloads)
| Abstract (HTML) (8185 Views)
References
1. Goyal A, Carter M, Niyonkuru C, Fabio A, Amin K, Berger RP, Wagner AK M D. S100b as a Prognostic Biomarker in Outcome Prediction for Patients with Severe TBI. J Neurotrauma. 2013;30(11):946-57.
2. Mowery NT. Stress Insulin Resistance is a Marker for Mortality in Traumatic Brain Injury. J Trauma. 2009:66(1):145-51; 151-3.
3. CampelloYurgel V, Ikuta N, Brondani da Rocha A, Lunge VR, Fett Schneider R, Kazantzi Fonseca AS, et al. Role of Plasma DNA as a Predictive Marker of Fatal Outcome following Severe Head Injury in Males. J Neurotrauma. 2007;24(7):1172–81. Available from: http://dx.doi.org/10.1089/neu.2006.0160
4. Ali E. Seif El-Deen, Said Hammad. Preoperative Serum S100 B Protein as a Prognostic Marker for Traumatic Brain Injury Patients. E.J.N.S. 2009;24 (1)135-152.
5. DeFazio MV, Rammo RA, Robles JR, Bramlett HM, Dietrich WD, Bullock MR. The Potential Utility of Blood-Derived Biochemical Markers as Indicators of Early Clinical Trends Following Severe Traumatic Brain Injury. World Neurosurgery. 2014;81(1):151–8. Available from: http://dx.doi.org/10.1016/j.wneu.2013.01.015
6. Beers SR, Berger RP, Adelson PD. Neurocognitive outcome and serum biomarkers in inflicted versus non-inflicted traumatic brain injury in young children. J Neurotrauma. 2007;24(1):97-105.
7. A.Salim. Persistent Hyperglycemia in Severe Traumatic Brain Injury: An Independent Predictor of Outcome. Am Surg. 2009;75(1):25-9.
8. Gopcevic A. Plasma interleukin-8 as a potential predictor of mortality in adult patients with severe traumatic brain injury. Tohoku J Exp Med. 2007;211(4):387-93.
9.Liu L, Wei H, Chen F, Wang J, Dong JF, Zhang J. Endothelial progenitor cells correlate with clinical outcome of traumatic brain injury. Crit Care Med. 2011;39(7):1760-5.
10. Bayir A, Kalkan E, Kocak S, Ak A, Cander B, Bodur S. Fibrinolytic markers and neurologic outcome in traumatic brain injury. Neurol India.2006;54:363-5.
11.Copin H.Matrix metalloproteinase 9 and cellular fibronectin plasma concentrations are predictors of the composite endpoint of length of stay and death in the intensive care unit after severe traumatic brain injury. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine.2012;43(6): 23-27.
12.Meshkini A,Salehpour F. Relationships of hyperglycemia and neurological outcome in patients with head injury.Anesthesia.2007;43(2): 2-6.
13. Douglas D. Fraser. Severe traumatic brain injury in children elevates glial fibrillary acidic protein in cerebrospinal fluid and serum. Pediatr Crit Care Med.2011;32(6):33-36.
14. Choon Hong Kan, MohdSaffari, TeikHooiKhoo. Prognostic Factors of Severe Traumatic Brain Injury Outcome in Children Aged 2-16 Years at A Major Neurosurgical Referral Centre. Malaysian Journal of Medical Sciences.2009;16(4):25-33.
15. SalehpoorF, Meshkini A. Prognostic value of serum LDH in head trauma. The International Medical Journal. 2005;4(2)31-37.
16. Meier R. Differential temporal profile of lowered blood glucose levels (3.5 to 6.5 mmol/l versus 5 to 8 mmol/l) in patients with severe traumatic brain injury. Crit Care.2008;12(4):98-102.
17. Hohl E. Plasma levels of oxidative stress biomarkers and hospital mortality in severe head injury: A multivariate analysis. Journal of Critical Care 27, 523.e11–523.e19;2012.
18.Liliang PC. Tau Proteins in Serum Predict Outcome After Severe Traumatic Brain Injury.Journal of Surgical Research. 2010;160(5):302–307.
19. Hossam M, Jehan H. Sabry, Deena A. El-Shabrawy. The Predictability of at Admission Serum GFAP and S100 protein Levels for the Outcome of Traumatic Brain Injury Patients. Egy. J. Neur. Surg. 2011;26(1):50-56.
20. Gullo J da S, Bertotti MM, Silva CCP, Schwarzbold M, Diaz AP, Soares FMS, et al. Hospital Mortality of Patients with Severe Traumatic Brain Injury is Associated with Serum PTX3 Levels. Neurocrit Care. 2010; 23;14(2):194–9. Available from: http://dx.doi.org/10.1007/s12028-010-9462-y.
21.Greuters. Acute and delayed mild coagulopathy are related to outcome in patients with isolated traumatic.brain injury.Crit Care.2011;15(1):2.
22.StefaniaM. Neuronal and glial markers are differently associated with computed tomography findings and outcome in patients with severe traumatic brain injury: a case control study. Critical Care.2012;15(1):156-159.
24. Guzel A.Serum neuron-specific enolase as a predictor of short-term outcome and its correlation with Glasgow Coma Scale in traumatic brain injury.Neurosurg Rev.2008; 31:439–445.
25. Zitnay GA, Zitnay KM, Povlishock JT, Hall ED, Marion DW, Trudel T, et al. Traumatic Brain Injury Research Priorities: The Conemaugh International Brain Injury Symposium. Journal of Neurotrauma 2008;25(10):1135–52. Available from: http://dx.doi.org/10.1089/neu.2008.0599
26. Hada M. Role of early cell-free DNA levels decrease as a predictive marker of fatal outcome after severe traumatic brain injury. ClinicaChimica Acta.2012; 414: 12–17.
27.Lanier WL, StanglandKJ ,Scheithaure BW. The effects of dextrose infusion and head position on neurologic outcome after complete cerebral ischemia in primates: examination of a model. Anesthesiology.1987;66:39-48.
28.Chabok SY, Moghadam AD, Saneei Z, Amlashi FG, Leili EK, Amiri ZM. Neuron-specific enolase and S100BB as outcome predictors in severe diffuse axonal injury. Journal of Trauma and Acute Care Surgery. 2012;72(6):1654–7. Available from: http://dx.doi.org/10.1097/ta.0b013e318246887e
29.Pelinka LE, Kroepfl A, Leixnering M, Buchinger W, Raabe A, Redl H. GFAP Versus S100B in Serum after Traumatic Brain Injury: Relationship to Brain Damage and Outcome. J Neurotrauma. 2004; 21(11):1553–61. Available from: http://dx.doi.org/10.1089/0897715042441846
30. Smith A.Relationship between hyperglycemia and outcome in children with severe traumatic brain injury.PediatrCrit Care Med.2012;13(1):85-91.
31. Lin C, Huang SJ, Wang N, Shen ZP. Relationship between plasma leptin levels and clinical outcomes.
32.Turgeon AF, Lauzier F, Burns KEA, Meade MO, Scales DC, Zarychanski R. Determination of neurological prognosis in adult patients with severe traumatic brain injury: a survey of Canadian intensivists, neurosurgeons and neurologists. Crit Care Med ,epub ahead of print; 2013 .
33. HergenroederG.W. Serum IL-6: a candidate biomarker for intracranial pressure elevation following isolated traumatic brain injury. Journal of Neuroinflammation.2010;3:7-19.
34. Jeremitsky E. The Impact of Hyperglycemia on Patients with Severe Brain Injury. J Trauma. Jan.2005;58(1):31-36.
35. Liu D.Clinical Impact of Early Hyperglycemia during Acute Phase of Traumatic Brain Injury.Neurocrit Care.2009;11:151–157.
36. Donald E. G. Griesdale, Marie-He´le`ne Tremblay, Jonathan McEwen, Dean R. Chittock. Glucose Control and Mortality in Patients with Severe Traumatic Brain Injury. Neurocrit Care.2009;11:311–316.
37. Llompart-Pou JA. Relationship between plasma adrenocorticotropin hormone and intensive care unit survival in early traumatic brain injury. J Trauma.2007;62(6):1457-61.
38.Tude M. Mortality in Children with Severe Head Trauma: Predictive Factors and Proposal for a New Predictive Scale. Neurosurgery.2010;67(6):1542-7.
39.Hossam M, Jehan H. Sabry, Deena A. El-Shabrawy. The Predictability of at Admission Serum GFAP and S100 protein Levels for the Outcome of Traumatic Brain Injury Patients. Egy. J. Neur. Surg.2011;26(1);11-19.
40.Matsushima K, Peng M, Velasco C, Schaefer E, Diaz-Arrastia R, Frankel H. Glucose variability negatively impacts long-term functional outcome in patients with traumatic brain injury. J Crit Care.2012;27(2):125-31.
41. Žurek J, Bartlová L, Fedora M. Hyperphosphorylatedneurofilament NF-H as a predictor of mortality after brain injury in children. Brain InjInforma Healthcare; 2011;25(2):221–6. Available from: http://dx.doi.org/10.3109/02699052.2010.541895
42.Amy K., Wagner. Acute Serum Hormone Levels: Characterization and Prognosis after Severe Traumatic Brain Injury. J Neurotrauma.2011;28(6): 871–888.
43.Olivecrona M, Rodling-Wahlstrom M, Naredi S, Koskinen L-OD. S-100B and neuron specific enolase are poor outcome predictors in severe traumatic brain injury treated by an intracranial pressure targeted therapy. Journal of Neurology, Neurosurgery & Psychiatry. BMJ;2009;80(11):1241–8. Available from: http://dx.doi.org/10.1136/jnnp.2008.158196
44. SaadatS. Association of persistent hyperglycemia with outcome of severe traumatic brain injury in pediatric population. Childs Nerv Syst.2012; 28:1773–1777.
45. Naeimi ZS, Weinhofer A, Sarahrudi K, Heinz T, Vécsei V. Predictive value of S-100B protein and neuron specific-enolase as markers of traumatic brain damage in clinical use. Brain Inj. Informa UK Limited; 2006;20(5):463–8. Available from: http://dx.doi.org/10.1080/02699050600664418
46.CzeiterR. Brain Injury Biomarkers May Improve the Predictive Power of the IMPACT Outcome Calculator. Journal of Neurotrauma.2012; 29:1770–1778 .
47. Nazik A, Fatih T, Muhammet Ş. Admission hyperglycemia is a reliable outcome predictor in children with severe traumatic brain injury. J Pediatr (Rio J).2011;87(4):325-8.
48. Salim A. Significance of Troponin Elevation after Severe Traumatic Brain Injury. J Trauma.2008; 64(1):46-52.
49. Nelson DW, Rudehill A, MacCallum RM, Holst A, Wanecek M, Weitzberg E, et al. Multivariate Outcome Prediction in Traumatic Brain Injury with Focus on Laboratory Values. Journal of Neurotrauma. 2012;29(17):2613–24. Available from: http://dx.doi.org/10.1089/neu.2012.2468
50.Perel P, Wasserberg J, Ravi RR, Shakur H, Edwards P, Roberts I. Prognosis following head injury: a survey of doctors from developing and developed countries. J EvalClin Pract2007;13:464-0005.
51.Melo JR. Acute hyperglycemia is a reliable outcome predictor in children with severe traumatic brain injury. ActaNeurochir (Wien).2010; 152(9):1559-65.
52. Rachel P. Berger, Ronald L. Hayes, Rudolph Richichi, Sue R. Beers. Serum Concentrations of Ubiquitin C-Terminal Hydrolase-L1 and αII-Spectrin Breakdown Product 145kDa Correlate with Outcome after Pediatric TBI. J Neurotrauma.2012; 29(1): 162–167.
53. Samit M. Biochemical Serum Markers in Head Injury, Clinical Neurosurgery.2012;57:134-140.
54. Tude M. Defenestration in children younger than 6 years old: mortality predictors in severe head trauma. Childs Nerv Syst.2009; 25:1077–1083.
55.Mondello E. Clinical Utility of Serum Levels of Ubiquitin C-Terminal Hydrolase as a Biomarker for Severe Traumatic Brain Injury. Neurosurgery.2012;70(3):666-75.
56. Nyle K. Increased serum-GFAP in patients with severe traumatic brain injury is related to outcome. Journal of the Neurological Sciences.2006; 240: 85 – 91.
57.Mc Gonzalez-Mao. Model Predicting Survival / ExitusAfter Traumatic Brain Injury: Biomarker S100B 24H. Clin. Lab.2011; 57:587-597.
58. Soares L. Interleukin-10 Is an Independent Biomarker of Severe Traumatic Brain Injury Prognosis. Neuroimmunomodulation. 2012;19:377–385.
59.Salehpour F, Bazzazi AM, Porhomayon J, NaderND. Correlation between coagulopathy and outcome in severe head trauma in neurointensive care and trauma units. J Crit Care.2011;26(4):352-6.
60.Stein DM. Relationship of Serum and Cerebrospinal Fluid Biomarkers With Intracranial Hypertension and Cerebral Hypoperfusion After Severe Traumatic Brain Injury. J Trauma.2011;70(5):1096-103.
61. Nelson DW. Hierarchical log linear analysis of admission blood parameters and clinical outcome following traumatic brain injury. J Neurotrauma.2012;29(17):2613-24.
62. NyleN. Serum levels of S100B, S100A1B and S100BB are all related to outcome after severe traumatic brain injury. ActaNeurochir (Wien).2008;150(3):221-7.
63. Raineya T, Leskob M. Predicting outcome after severe traumatic brain injury using the serum S100B biomarker: Results using a single (24 h) time-point. Resuscitation.2009; 341–345.
64.ŽurekJ ,Fedora M. The usefulness of S100B, NSE, GFAP, NF-H, secretagogin and Hsp70 as a predictive biomarker of outcome in children with traumatic brain injury. Acta Neurochir.2012; 154:93–103.
66. Els C.H. Prognosis of six-month function after traumatic brain injury.Rehabil Med.2010; 42: 425–436.
67.V. Jain, S. Tiwari, S. Misra, Tiwari, Nagendra. Predictive Value of Serum Lactate Dehydrogenase in Head Injury. The Internet Journal of Surgery. 2010; 22(2):101-110.
68.Barlow P, Teasdale G. Prediction of outcome and the management of severe head injuries: the attitudes of neurosurgeons. Neurosurg.1986; 19:989-991.
69. Gong D, Hao M, Liu L, Liu C, Dong J, Cui Z, et al. Prognostic relevance of circulating endothelial progenitor cells for severe traumatic brain injury. Brain Inj. Informa Healthcare. 2012;26(3):291–7. Available from: http://dx.doi.org/10.3109/02699052.2011.648710
70. Oliviera D. Plasma von Willebrand Factor Levels Correlate with Clinical Outcome of Severe Traumatic Brain Injury. Journal of neurotrauma.2007; 24:1331–1338.
71. Papa L. Serum levels of ubiquitin C-terminal hydrolase distinguish mild traumatic brain injury from trauma controls and are elevated in mild and moderate traumatic brain injury patients with intracranial lesions and neurosurgical intervention. J Trauma Acute Care Surg.2012; 72(5):1335-44.
72. WhaSookSeo, HyunSoo Oh. Comparisons of Acute Physiological Parameters Influencing Outcome in Patients with Traumatic Brain Injury and Hemorrhagic Stroke. Worldviews Evid Based Nurs.6(1):36-43;2009.
73.Prisco L, Iscra F, Ganau M, Berlot G.Early predictive factors on mortality in head injured patients: a retrospective analysis of 112 traumatic brain injured patients. J Neurosurg Sci. 2012 Jun;56(2):131-6.
Full Text: (2084 Views)
Introduction
Traumatic brain injury still remains a serious concern and one of the leading causes of death and disability, particularly among young adults (1,2). Based on studies of prevention of diseases in United States, the most common causes of traumatic brain injury include factors like traffic accidents (20%), hit a barrier (19%) and assault (11%) (1). Traumatic brain injury can be classified into two types, primary and secondary. The primary injury occurs at the time of the accident causing direct damage to nerve tissue. Secondary damage is not seen at an early stage. Such harm is the natural and physiological response to the initial injury. Tissue hypoxia, which occurs within hours to months after the initial injury is this group (1). Early determination of prognosis after traumatic brain injury is a priority for relatives and physicians involved in the care of these patients (2,3). New prognostic information beyond the clinical examination, patient demographics and radiological imaging from admission is needed to allow early prediction of short, mid, and long term outcome of patients with moderate and severe traumatic brain injury (1,2,3). One of the factors involved in secondary damage that may occur following head trauma is the changes in blood parameters and biomarkers. Assessment of brain damage using biochemical tests and cerebrospinal fluid (CSF) and serum enzymes during the past decade has been done (4). Biomarkers of structural damage such as S-100, tau, enolase Neuron Specific (NSE) and myelin basic protein (MBP) may be used as potential diagnostic tools, prognostic and therapeutic supplements (1). The purpose of this study was to systematically review articles that studied the changes in hematological parameters in patients with traumatic brain injury and its correlation with the final outcome of treatment.of brain damage using biochemical tests, and cerebrospinal fluid (CSF) and serum enzymes during the past decade has been done (4). Biomarkers of structural damage, such as S-100, tau, enolase Neuron Specific (NSE) and myelin basic protein (MBP), may be used as potential diagnostic tools, prognostic and therapeutic supplements (1). The purpose of this study was to systematically review articles that studied the changes in hematological parameters in patients with traumatic brain injury and its correlation with the final outcome of treatment.
Methods and Materials/Patients
Search strategy
Sampling based on the search of information resources PUBMED, COCHRANE, Embase, Google scholar. Databases were searched for relevant publications between 2005 and 2014. The following keywords were used: prognosis, prognostic model, predict, head trauma, brain trauma, head injury, brain injury, biochemistric tests, biomarkers, blood markers, blood glucose, and serum markers.
Study selection
Two reviewers (FS and AM or AR) independently reviewed all publications and selected eligible studies. A third author (GS) was consulted in case of disagreement. We included cohort studies and determined serum factors concentrations in patients with moderate and/or severe traumatic brain injury as defined by a Glasgow coma score<13.
Inclusion criteria were:
1. (Due to the dramatic change in measuring biomarker concentrations and the treatment of traumatic injuries in recent years), studies which were published from 2005 until 2014.
2. Studies in which, factors affecting the outcome after TBI were evaluated.
3. Studies that defined TBI as “acute changes in brain function resulting in a strong external force to the head.
4. Studies in which the result was measured by Glasgow Outcome Score or a comparable measure describing the activity limitation and neurological state.
5. Studies in which correlation between the measured factors in the first month after injury and the prognosis was addressed.
6. The studies population were patients with moderate and/or severe (GCS <13) TBI with or without patients with mild injury or a subgroup consisting of patients with moderate or severe TBI were analyzed separately.
7. The article was written in English or English form of it was available.
Quality Assessment
Each paper was qualitatively evaluated according to criteria intended to establish study strength. These included:
1. Twenty-five or more patients in the series with complete follow-up.
2. Outcomes measured -Glasgow Outcome Scale or Mortality- at six months or more.
3.Data gathered prospectively, although retrospective examination from a database creating an ongoing cohort of patients could be used.
4.Glasgow Coma Scale score measured within 24 hours.
5.Appropriate statistics (e.g. multivariate analysis) was used to include adjustment for prognostic variables.
Data Extraction
Two reviewers (FS and AM or AR) independently collected data using a standardised data abstraction form. We abstracted information related to study design, patient characteristics, treatments (operative and pharmacological), laboratory aspects of the testing factor (type of assay used, time period of sampling, and sampling type) and clinical outcomes (outcome type and timing of assessment). In instances of duplicate reporting, we used data from the study that included the largest number of patients or, when available, individual patient data from each study. We contacted authors for clarification on study sample or for missing data. If multiple measurements were carried out, we used the first measurement after the injury for analysis. If outcomes were assessed at multiple time points, we used the measurement furthest from injury for analysis. Data of studies, inclusion and exclusion criteria, number of participants, time after injury, failure to continue follow-up, measurements of outcome, prognostic factors and results of their relationships with outcome were extracted using a standardized form.
Analysis
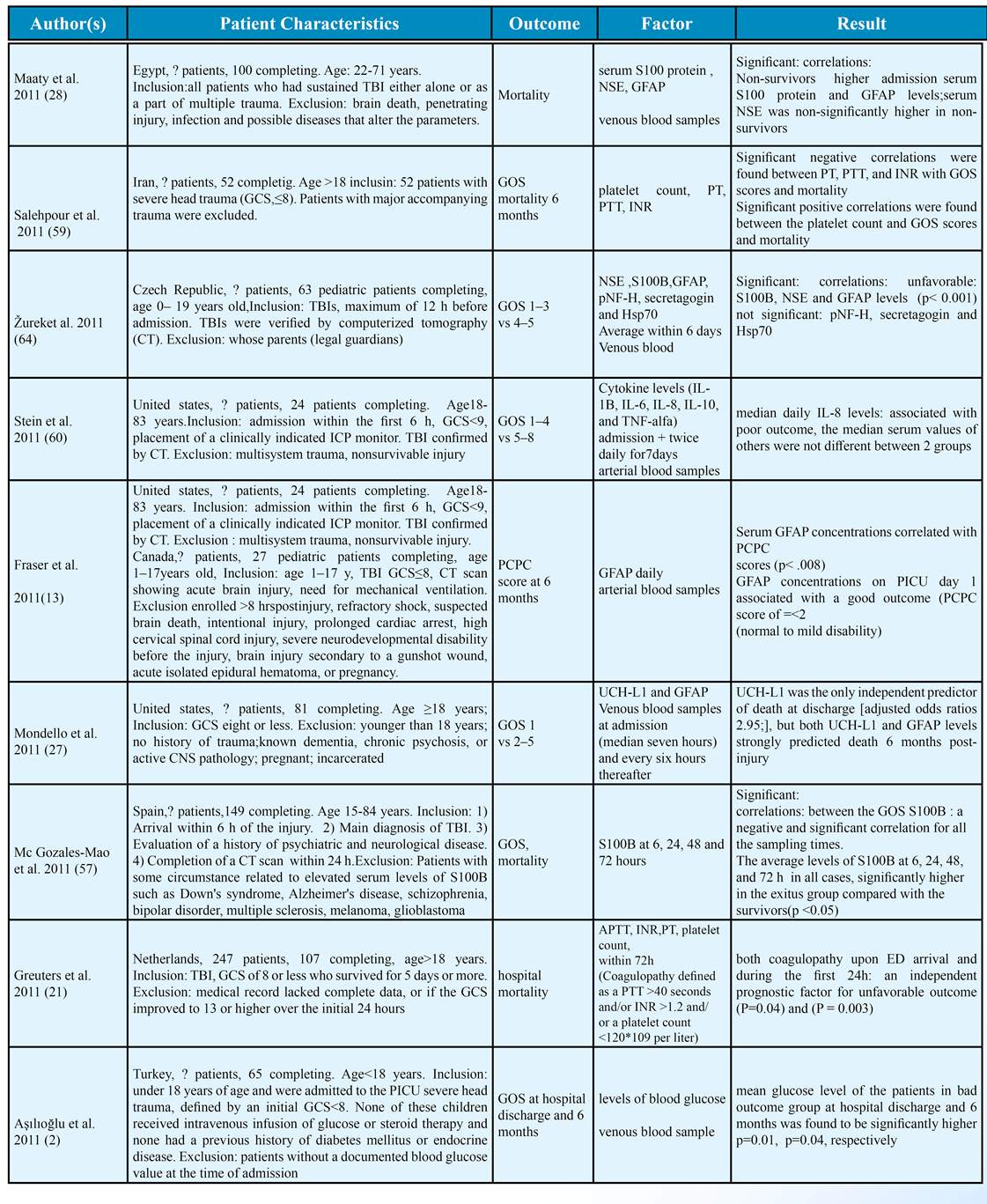
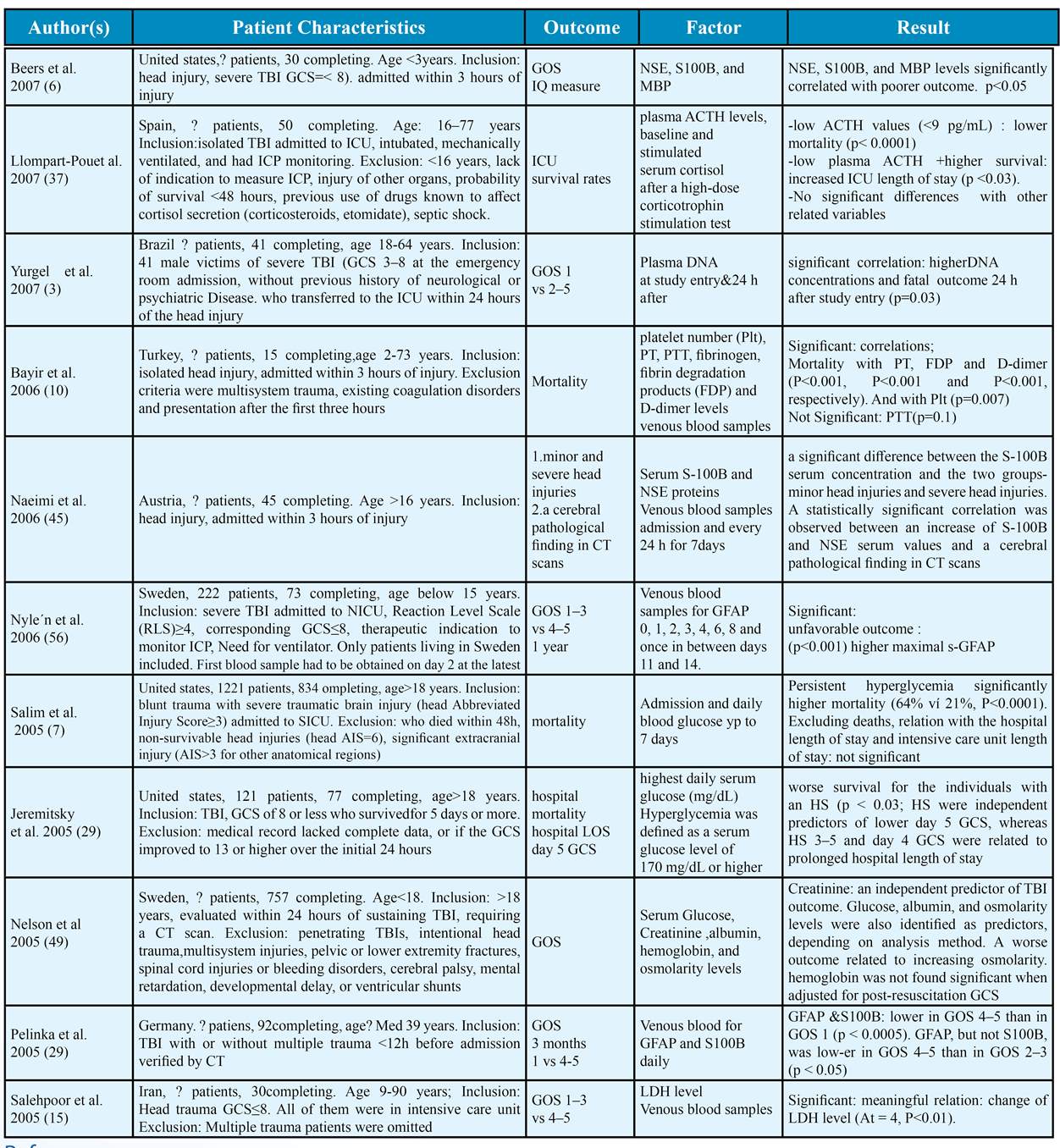
Significant relative risk ratios (RR), odds ratios (OR) or significant correlations (P<0.05) which were introduced by studies, was used to determine levels of evidence. If multivariate analysis was performed in the study, the results of it were used to establish the level of evidence. Otherwise, the results of the univariate analysis were used (table 1).
Results
Study selection
In total, 1021 citations were identified and after elimination of duplicates and screening and after using the inclusion and exclusion criteria, agreement was initially reached in 82 of articles and consensus was sought and finally, 63 articles were selected.
Study characteristics
The study characteristics are presented in Table 2. All articles were written in English. The number of patients studied was from 20 to 834 individuals with moderate to severe and sometimes mild traumatic brain injury. Penetrating trauma was not mentioned.
The main measure used for prognosis was GOS (30 studies). Other measures include mortality, GCS, ASI, PCPC, GOSE, EDSS, and DRS (Table 2). Most of the investigated factors were: blood glucose, serum protein S100 and NSE, as follows:16 study assessed the serum S100 protein (13 studied: S100B, 2 study: S100BB, 1 study: S100A1B), 22 study assessed the blood glucose levels and in 14 study, NSE levels were examined. 45 studies exclusively evaluated adults and 16 studies exclusively evaluated children. In other studies, age was not an entry criterion. Of all studies, in 20 studies, venous blood samples were taken. In 11 studies, arterial blood and in one study capillary blood (finger) was sampled. Other studies did not specify the sampling site.
Neuronal markers:
1. Protein S100:
According to the studies, serum concentration of S100 protein is a strong prognostic factor in adults and in children and there was strong evidence of relationship between serum levels of protein S100 and outcome. 19 studies were reviewed which assessed S100 protein in the blood as a prognostic factor in TBI. In all but two studies (6,7), high levels associated with poor prognosis. All of these studies assessed serum levels of S100B but a study conducted in 2012 by Yousefzadeh et al. (28) evaluated the S100BB levels and Nyle’n et al. (62) studied serum levels of 3 types of this protein (S100B, S100A1B and S100BB). In studies on children with TBI (6,9,10,11,12,13) in many of them significant correlation with the prognosis of patients was achieved except a study performed by Beers et al. (2007) (6) in which a statistical correlation between serum protein and GOS at 3-4 and 6-8 months after trauma was not found. Of the studies on the adults with traumatic brain injury (7,8,15, 16,17,18,19,20) all except one study (7) showed significant correlation between prognosis and S100 levels in serum.
2. Neuron specific enolase:
The evidence for the predictive value of concentration of neuron specific enolase in adults and in children with TBI was strong. 12 studies which had evaluated NSE as a prognostic factor were reviewed; all but three studies (6,13) achieved significant associated between high levels of NSE and poor prognosis.
Six studies were performed on children with traumatic brain injury (6,11,12) and seven studies on adults (13,15,16,17,20,22)
3. Hyperphosphorylated neurofilament:
According to the studies, serum concentration of NF-H is a strong prognostic factor in children. Two studies (10,24) evaluated serum NF-H levels as a prognostic factor in TBI; Both studies performed on children in both studies, high levels associated with poor prognosis.
4. Ubiquitin C-Terminal Hydrolase:
5 articles that studied (Table 2) serum levels of UCHL1 as a prognostic factor in TBI were reviewed. All of them studied the correlation between UCHL1 values and GOS except for a study conducted in 2012 by L.Papa et al. (25) in which outcome measures included the following:
(1) GCS scores obtained at presentation to the ED,
(2) the presence of intracranial lesions on initial CT scan; and
(3) the need for neurosurgical intervention (NSI).
In this study, there was a significant relationship between all these three outcome measures, and levels of UCHL1 in adult patients with TBI. All of the other studies also found a significant correlation between high serum UCHL1 values and low GOS (unfavorable outcome).
5. TAU Protein
The evidence for the prognostic value of serum levels of TAU protein was Limited. Only one study (26) assessed serum levels of TAU protein as a prognostic factor in TBI. This study was conducted in 2008 by L. Nyle’n et al. (62) and reported high level of TAU protein levels as an independent risk factor for a poor outcome (GOS 1-3) (P=0.043). ROC evaluating the ability of serum t protein level to predict a poor outcome showed an area under the curve of 0.939 with 88% sensitivity and 94% specificity at a serum TAU protein level of 114.5 pg/mL.
6. Myelin basic protein
2 studies (6,11) evaluated the levels of myelin basic protein (MBP) in serum, as a TBI prognostic factor. In the study which was performed on children under 15 years of age with traumatic brain injury, a significant relation was found between levels of this protein and the GOS, 3-4 and 6-8 months after trauma (6). In another study on children under 3 years who suffered a traumatic brain injury of varying intensities, high serum levels of MBP correlated with bad 6-month outcome which was measured by (Glasgow Outcome Scale using (GOS), Vineland Adaptive Behavior Scale (VABS) and the Intelligence Coefficient (IQ)
7. Glial Fibrillary Acidic Protein
The evidence for the prognostic value of serum levels of GFAP was strong. Seven studies (7,10,27,28,29,30,31) investigated serum GFAP levels as a prognostic factor and all of them reported the high values of GFAP correlates with poor prognosis. Four studies evaluated prognosis of TBI in children and reminding were performed on adults. In a study performed by S. Mondello and coworkers (27) in 2011, multivariate logistic regression analysis showed that of all the variables assessed, only UCH-L1 was an independent predictor of mortality at discharge and also strongly predicted deaths in 6 months after the damage predicted. Highly significant correlation between UCH-L1 and GFAP were found. GFAP did not have an additional contribution when UCH-L1 was already entered in the model. Similar predictive value for GFAP and UCH-L1 (c=0.93) was determined.
- Biochemical test
1. Blood sugar:
In 22 studies, blood glucose levels were investigated as a prognostic factor. All but three studies (32,33,34) reported that high levels of BS is associated with poor prognosis. All of the studies performed on children with traumatic brain injury (35,36,37,38) achieved significant correlation between BS levels and patient prognosis. All of the studies on adults with traumatic brain injury (32,33,34,40,41,42,43,44,45,46,47,48,49,50) and studies without a age limit (51,52) reported a significant relationship between blood glucose levels and prognosis achieved except two studies (32,34). The evidence for the prognostic value of BS levels was strong both in adults and in children with traumatic brain injury.
2. Lactate Dehydrogenase:
One study (53) evaluated Lactate Dehydrogenase levels as a prognostic factor of TBI. In both studies high levels were associated with poor prognosis. The evidence for the prognostic value of serum levels of LDH was strong. In V. Jain et al. study (68) in 2010, a significant relationship between serum LDH outcome after traumatic brain injury was found in patients with isolated brain trauma. In this study, the average increase in serum LDH was found in patients with a poor outcome and LDH levels increased continuously during the study period in both disabled and dead groups.
3.Plasma Osmolarity:
Two studies (34,46) investigated plasma osmolarity as a prognostic factor. In a study by WhaSook Seo and HyunSoo Oh in 2009 (72) on patients with traumatic brain injury (and hemorrhagic stroke), 6 months after the trauma one of the physiologically significant predictors of cognitive abilities in patients with TBI was admission serum osmolarity (p= 0.01), but there was no significant association between plasma osmolarity mortality and functional disability. In Nelson DW et al. study (49), poorer outcomes were observed with increasing osmolarity. According to these two studies, the evidence for the prognostic value plasma osmolarity was inconclusive.
4.Total cholesterol:
In WhaSook Seo and HyunSoo Oh study (72), 6 months after trauma, relationship between total cholesterol and mortality, cognitive abilities and functional disability in patients with TBI were not significant. In another study by Adel Helmy et al. (50), Total cholesterol only had a statistical relationship with traumatic brain injury outcome, via at least one other variable and was designated as ‘level 2’ of the hierarchy. According to these studies, serum total cholesterol probably is not a prognostic factor in patients with traumatic brain injury with a moderate level of evidence.
5.Albumin:
3 studies (34,46,50) investigated albumin level as a prognostic factor in TBI. In WhaSook Seo and HyunSoo Oh study (72) and in Adel Helmy et al. study (50), correlation of albumin levels with outcome was like total cholesterol level. In Nelson DW et al. study (49), low albumin relationship with poor outcome in patients with TBI was statistically significant. According to these studies, the evidence for the prognostic value of low albumin was also inconclusive.
6.Other biochemical tests:
Nelson DW study in 2005 (61) reported blood creatinine as an independent predictor of outcome after TBI. In study by Helmy et al. (50), low magnesium only had a statistical relationship with outcome via at least two other variables and was designated as ‘level 3’ of the hierarchy. Hohl and colleagues in a study in 2012 (12) found that sodium in the blood of those who died after TBI was significantly higher. According to the above studies, the levels blood sodium was a strong prognostic factor of poor outcome in patients with traumatic brain injury, but the evidence for the prognostic value of the other variables was limited and uncertain.
Complete Blood Count (CBC):
1. Hemoglobin
Five studies (34,43,46,48,50) were reviewed which assessed Hb levels as a prognostic factor in TBI. In 3 of them (43,48,50), low levels associated with poor prognosis. In two studies (34,46) there was no significant correlations between Hb levels and prognosis. According to the studies, there was inconclusive evidence of relationship between Hb level and outcome in traumatic brain injury.
2. The leukocyte count
Three studies (38,50,55) were reviewed which assessed WBC count as a prognostic factor in TBI. None of them showed significant correlations between WBC levels and TBI prognosis. According to the studies, there was strong evidence of no relationship between WBC level and outcome in traumatic brain injury.
- Blood Gases and ABG Results:
3 studies (34,39,43) were reviewed which assessed ABG results as a prognostic factor in TBI. In study by WhaSook Seo & HyunSoo Oh (72), 6 months after trauma physiological predictors of mortality in patients with traumatic brain injury was arterial oxygen pressure (F=11.83, p=0.00) and arterial carbon dioxide pressure (F=4.40, p=0.02). In another study performed by Tude Melo et al. in 2010 (38), low blood oxygen saturation found to be a prognostic factor for mortality (OR)=1.67. According to the studies, there was a limited evidence of relationship between PaCO2, PaO2, aPH, O2sat and outcome of traumatic brain injury.
Coagulation Factors and Products:
8 studies (31,38,39,43,58,71) were reviewed which assessed coagulation factors and products as a prognostic factor in TBI:
5 studies (38,39,43,58) assessed prothrombin time (PT) as a prognostic factor in TBI and all of them found a significant correlation between increased PT and poor outcome and mortality. So the evidence about prognosis prediction of PT is strong.
3 studies (38,58) assessed partial thromboplastin time (PTT) as a prognostic factor in TBI and two studies (38,58) found a significant correlation between increased a PTT and poor outcome. So the evidence about prognosis prediction of PTT is strong.
3 studies (38,58) assessed platelet count as a prognostic factor in TBI and two studies (58) found a significant correlation between decreased platelet count and poor outcome. So the evidence about prognosis prediction of platelet count is strong.
2 studies (14) assessed D.dimer levels in serum as a prognostic factor in TBI and none of them found a significant correlation between its levels and outcome. Therefore, the evidence about that there is no relation between prognosis and levels of D.dimer is strong.
Only one study assessed each serum FDP levels and serum VWF factor levels (31) found a significant correlation between them and outcome. Thus, the evidence about prognosis prediction of both of these is limited.
-Acute Phase Reactants:
1.Heat Shock Protein 70 (HSP 70):
2 studies (58,59) assessed HSP 70 levels in serum as a prognostic factor in TBI and both of them found a significant correlation between its levels and outcome. So the evidence about prognosis prediction of HSP70 is strong.
2. Pentraxin-PTX3
Only one study (54) investigated Pentraxin-PTX3 serum protein as a prognostic factor. In this study which was conducted in 2011 by Jackson da Silva Gullo et al., (20) increased PTX3 levels correlated with mortality (P<0.04). Thus, the evidence about prognosis prediction of PTX3 levels is limited.
-Inflammatory Factors:
3 studies (60,61,62) assessed some of the cytokines and inflammatory factors as prognostic factor in TBI. In Gopcevic et al. study (8), plasma level of IL-8 was significantly lower in survivors (71.00 +/- 14.17 pg/ml) than in non-survivors (111.26 +/- 16.9 pg/ml). In Stein et al. study (60), median daily IL-8 levels associated with poor outcome, the median serum values of other Cytokine levels (IL-1B, IL-6, IL-8, IL-10, and TNF-alfa) were not different between 2 groups (GOSE 1–4 vs 5–8). In Soares et al. study (58), significant correlations of elevated serum levels of IL-10, but not TNF-α, with hospital mortality in patients with severe TBI were reported (p=0.01). Considering all these studies suggest that increased serum levels of IL-8 may be a strong prognostic factor but uncertain and limited predictive power of other inflammatory factors was seen.
- Hormones
1. ACTH
2. Cortisol
3. Estradiol
4. Testosterone
5. Progesterone
6.LH & FSH
2 studies (63,64) were reviewed which assessed Cortisol (63,64), ACTH (63) and sex hormones (64) as prognostic factors in TBI.
In K. Wagner et al. study (42), high estradiol and testosterone associated with mortality (p=0.026 and p=0.033, respectively). Significant effect of LH, FSH, progesterone on mortality through their association with estradiol (p=0.049). High estradiol was associated with worse outcomes. Stradiol mediated progesterone associations with GOS (p=0.045). Serum cortisol was not associated with mortality or GOS. In Llompart-Poue et al. study (37), patients with low ACTH values (<9 pg/mL): statistically significant lower mortality (7% vs. 55%, p<0.0001) and low plasma ACTH in patient who survived, correlated with increased ICU length of stay (p<0.03). But no significant differences with baseline and stimulated serum cortisol after a high-dose corticotrophin stimulation test were seen. According to these studies, the serum cortisol strongly has no relation with outcome of patients with brain injury. And the evidence of the prognostic value of serum levels other hormones mentioned, was inclusive.
Matrix metalloproteinase 9:
In the study conducted by M. DeFazio et al. (17) a significant difference in the mean concentration of MMP-9 at admission (P=0.115) or in 24 h (P=0.535) was not found between the short term outcome groups. The study conducted by J. Copin et al. (11) a significant relationship between serum MMP-9 levels and three-month GOSE in patients with severe TBI was not seen. According to these studies, the serum MMP9 levels have no relation with outcome of patients with brain injury with moderate evidence.
α II-Spectrin Breakdown Product 145kDa:
Only one study (6) investigated serum SBDP145 level as a prognostic factor in TBI.
In one study (6), unfavorable outcome was correlated with higher concentrations of SBDP145.
According to this study, the evidence for the prognostic value of low SBDP145 was limited.
Circulating endothelial progenitor cells:
2 studies (66,67) were reviewed which assessed circulating endothelial progenitor cells as prognostic factor in TBI.
In Li Liu et al. study (9), number of circulating EPCs was significantly lower in who died p<0.01 .
In Gong D et al. study (69), number of circulating EPCs was significantly correlated with GOS scores 6 months after TBI. Thus, the evidence for the predictive value of circulating endothelial progenitor cells was strong.
- Miscellaneous:
The studies of other factors, including serum oxidative stress parameters: thiobarbituric acid reactive species (TBARS) and carbonyl group (48), serum leptin (68) serum fibronectin CFn and troponin cTnI were also reviewed which due to the low number of these studies for each factor, they can be a potential prognostic factors with limited evidence for TBI.
Conclusion
This systematic review summarized the results of 63 articles about the predictive value of various factors on prognosis after brain damage. Providing new information or explaining the findings in terms of pathophysiology is not the primary goal of a systematic review. Therefore, although relevant for clinicians, we were cautious not to speculate about underlying mechanisms or explanations for which no evidence was given in the included studies. Our study established strong evidence that serum concentration of S100 protein, neuron specific enolase, MBP, NF-H, GFAP, UCH-L1, blood glucose levels, serum levels of LDH, sodium level, prothrombin time, partial thromboplastin time, platelet count, D.dimer, HSP 70, serum levels of IL-8, number of circulating EPCs, and DNA levels in serum were predictors of post-TBI outcome. This study found strong evidence that WBC count and serum cortisol levels do not predict outcome. Moreover, moderate evidence was found that serum total cholesterol count do not predict outcome. Moderate evidence showed that high serum MMP9 levels predict poor outcome. For all other determinants the evidence was limited or inconclusive. Although these profiles are best evidence for prognosis after TBI, they seem to be of limited value; hence still we are not able to correct or prevent or treat some of these factors. Overall, it can be concluded that much information is needed on long term outcome moderate and severe traumatic brain injury.
Limitations of the review
It was very difficult to reach a consensus on all epidemiological findings across the 63 published studies because of critical differences in methods employed across the reports. Firstly, we searched studies published between the 2005 and 2014. It is possible that relevant publications before or after that time were not included in this review. However, we think that it would be inappropriate to include older studies in a review on prognostic factors, because there have been dramatic changes in measuring biomarkers concentrations and the treatment of traumatic injuries over the last years.
Some of the included studies excluded penetrating head injury, other studies did not. Little information was given in the studies about how many patients had closed or open head injuries. It is not clear whether this has influenced our results. There was considerable heterogeneity for all outcomes of interest and in the time period over which outcome was evaluated. In the literature, different definitions for traumatic brain injury and the diagnostic methods are used. We decided to define brain injuries as the changes in brain function because of severe damage by an external force. We choose this fairly extensive definition is brain damage, so we would be able to enter many of the relevant studies. Furthermore, the populations studied were varied extensively in each literature from the other, in terms of gender, age, region and country in which they lived and were treated. Finally, we did not include studies published in languages other than English.
Recommendations:
Prediction of outcome after brain injury is not always straightforward, and there is always some uncertainty. Multiple factors may affect the outcome. Much of the literature available is written from an isolated neurological, neurosurgical or rehabilitation perspective. To improve outcome prediction, multidisciplinary research should take place, and knowledge should be integrated.
Although several biomarkers of brain injury have been identified, continued research is required. A single biomarker may not have desired sensitivity and specificity for predicting outcome. Biomarkers, in combination with other clinical data, such as GCS and head CT scan, would maximize the accuracy. Future studies will be required to not only identify these biomarkers prognostic ability together with other factors.
Acknowledgment
The authors would like to thank the staff of the Neurosurgery Ward of Imam-Hossein Hospital, Tehran, Iran.
Funding
None declared.
Conflicts of Interest
The authors declare that they have no competing interests.
Traumatic brain injury still remains a serious concern and one of the leading causes of death and disability, particularly among young adults (1,2). Based on studies of prevention of diseases in United States, the most common causes of traumatic brain injury include factors like traffic accidents (20%), hit a barrier (19%) and assault (11%) (1). Traumatic brain injury can be classified into two types, primary and secondary. The primary injury occurs at the time of the accident causing direct damage to nerve tissue. Secondary damage is not seen at an early stage. Such harm is the natural and physiological response to the initial injury. Tissue hypoxia, which occurs within hours to months after the initial injury is this group (1). Early determination of prognosis after traumatic brain injury is a priority for relatives and physicians involved in the care of these patients (2,3). New prognostic information beyond the clinical examination, patient demographics and radiological imaging from admission is needed to allow early prediction of short, mid, and long term outcome of patients with moderate and severe traumatic brain injury (1,2,3). One of the factors involved in secondary damage that may occur following head trauma is the changes in blood parameters and biomarkers. Assessment of brain damage using biochemical tests and cerebrospinal fluid (CSF) and serum enzymes during the past decade has been done (4). Biomarkers of structural damage such as S-100, tau, enolase Neuron Specific (NSE) and myelin basic protein (MBP) may be used as potential diagnostic tools, prognostic and therapeutic supplements (1). The purpose of this study was to systematically review articles that studied the changes in hematological parameters in patients with traumatic brain injury and its correlation with the final outcome of treatment.of brain damage using biochemical tests, and cerebrospinal fluid (CSF) and serum enzymes during the past decade has been done (4). Biomarkers of structural damage, such as S-100, tau, enolase Neuron Specific (NSE) and myelin basic protein (MBP), may be used as potential diagnostic tools, prognostic and therapeutic supplements (1). The purpose of this study was to systematically review articles that studied the changes in hematological parameters in patients with traumatic brain injury and its correlation with the final outcome of treatment.
Methods and Materials/Patients
Search strategy
Sampling based on the search of information resources PUBMED, COCHRANE, Embase, Google scholar. Databases were searched for relevant publications between 2005 and 2014. The following keywords were used: prognosis, prognostic model, predict, head trauma, brain trauma, head injury, brain injury, biochemistric tests, biomarkers, blood markers, blood glucose, and serum markers.
Study selection
Two reviewers (FS and AM or AR) independently reviewed all publications and selected eligible studies. A third author (GS) was consulted in case of disagreement. We included cohort studies and determined serum factors concentrations in patients with moderate and/or severe traumatic brain injury as defined by a Glasgow coma score<13.
Inclusion criteria were:
1. (Due to the dramatic change in measuring biomarker concentrations and the treatment of traumatic injuries in recent years), studies which were published from 2005 until 2014.
2. Studies in which, factors affecting the outcome after TBI were evaluated.
3. Studies that defined TBI as “acute changes in brain function resulting in a strong external force to the head.
4. Studies in which the result was measured by Glasgow Outcome Score or a comparable measure describing the activity limitation and neurological state.
5. Studies in which correlation between the measured factors in the first month after injury and the prognosis was addressed.
6. The studies population were patients with moderate and/or severe (GCS <13) TBI with or without patients with mild injury or a subgroup consisting of patients with moderate or severe TBI were analyzed separately.
7. The article was written in English or English form of it was available.
Quality Assessment
Each paper was qualitatively evaluated according to criteria intended to establish study strength. These included:
1. Twenty-five or more patients in the series with complete follow-up.
2. Outcomes measured -Glasgow Outcome Scale or Mortality- at six months or more.
3.Data gathered prospectively, although retrospective examination from a database creating an ongoing cohort of patients could be used.
4.Glasgow Coma Scale score measured within 24 hours.
5.Appropriate statistics (e.g. multivariate analysis) was used to include adjustment for prognostic variables.
Data Extraction
Two reviewers (FS and AM or AR) independently collected data using a standardised data abstraction form. We abstracted information related to study design, patient characteristics, treatments (operative and pharmacological), laboratory aspects of the testing factor (type of assay used, time period of sampling, and sampling type) and clinical outcomes (outcome type and timing of assessment). In instances of duplicate reporting, we used data from the study that included the largest number of patients or, when available, individual patient data from each study. We contacted authors for clarification on study sample or for missing data. If multiple measurements were carried out, we used the first measurement after the injury for analysis. If outcomes were assessed at multiple time points, we used the measurement furthest from injury for analysis. Data of studies, inclusion and exclusion criteria, number of participants, time after injury, failure to continue follow-up, measurements of outcome, prognostic factors and results of their relationships with outcome were extracted using a standardized form.
Analysis
Significant relative risk ratios (RR), odds ratios (OR) or significant correlations (P<0.05) which were introduced by studies, was used to determine levels of evidence. If multivariate analysis was performed in the study, the results of it were used to establish the level of evidence. Otherwise, the results of the univariate analysis were used (table 1).
Results
Study selection
In total, 1021 citations were identified and after elimination of duplicates and screening and after using the inclusion and exclusion criteria, agreement was initially reached in 82 of articles and consensus was sought and finally, 63 articles were selected.
Study characteristics
The study characteristics are presented in Table 2. All articles were written in English. The number of patients studied was from 20 to 834 individuals with moderate to severe and sometimes mild traumatic brain injury. Penetrating trauma was not mentioned.
The main measure used for prognosis was GOS (30 studies). Other measures include mortality, GCS, ASI, PCPC, GOSE, EDSS, and DRS (Table 2). Most of the investigated factors were: blood glucose, serum protein S100 and NSE, as follows:16 study assessed the serum S100 protein (13 studied: S100B, 2 study: S100BB, 1 study: S100A1B), 22 study assessed the blood glucose levels and in 14 study, NSE levels were examined. 45 studies exclusively evaluated adults and 16 studies exclusively evaluated children. In other studies, age was not an entry criterion. Of all studies, in 20 studies, venous blood samples were taken. In 11 studies, arterial blood and in one study capillary blood (finger) was sampled. Other studies did not specify the sampling site.
Neuronal markers:
1. Protein S100:
According to the studies, serum concentration of S100 protein is a strong prognostic factor in adults and in children and there was strong evidence of relationship between serum levels of protein S100 and outcome. 19 studies were reviewed which assessed S100 protein in the blood as a prognostic factor in TBI. In all but two studies (6,7), high levels associated with poor prognosis. All of these studies assessed serum levels of S100B but a study conducted in 2012 by Yousefzadeh et al. (28) evaluated the S100BB levels and Nyle’n et al. (62) studied serum levels of 3 types of this protein (S100B, S100A1B and S100BB). In studies on children with TBI (6,9,10,11,12,13) in many of them significant correlation with the prognosis of patients was achieved except a study performed by Beers et al. (2007) (6) in which a statistical correlation between serum protein and GOS at 3-4 and 6-8 months after trauma was not found. Of the studies on the adults with traumatic brain injury (7,8,15, 16,17,18,19,20) all except one study (7) showed significant correlation between prognosis and S100 levels in serum.
2. Neuron specific enolase:
The evidence for the predictive value of concentration of neuron specific enolase in adults and in children with TBI was strong. 12 studies which had evaluated NSE as a prognostic factor were reviewed; all but three studies (6,13) achieved significant associated between high levels of NSE and poor prognosis.
Six studies were performed on children with traumatic brain injury (6,11,12) and seven studies on adults (13,15,16,17,20,22)
3. Hyperphosphorylated neurofilament:
According to the studies, serum concentration of NF-H is a strong prognostic factor in children. Two studies (10,24) evaluated serum NF-H levels as a prognostic factor in TBI; Both studies performed on children in both studies, high levels associated with poor prognosis.
4. Ubiquitin C-Terminal Hydrolase:
5 articles that studied (Table 2) serum levels of UCHL1 as a prognostic factor in TBI were reviewed. All of them studied the correlation between UCHL1 values and GOS except for a study conducted in 2012 by L.Papa et al. (25) in which outcome measures included the following:
(1) GCS scores obtained at presentation to the ED,
(2) the presence of intracranial lesions on initial CT scan; and
(3) the need for neurosurgical intervention (NSI).
In this study, there was a significant relationship between all these three outcome measures, and levels of UCHL1 in adult patients with TBI. All of the other studies also found a significant correlation between high serum UCHL1 values and low GOS (unfavorable outcome).
5. TAU Protein
The evidence for the prognostic value of serum levels of TAU protein was Limited. Only one study (26) assessed serum levels of TAU protein as a prognostic factor in TBI. This study was conducted in 2008 by L. Nyle’n et al. (62) and reported high level of TAU protein levels as an independent risk factor for a poor outcome (GOS 1-3) (P=0.043). ROC evaluating the ability of serum t protein level to predict a poor outcome showed an area under the curve of 0.939 with 88% sensitivity and 94% specificity at a serum TAU protein level of 114.5 pg/mL.
6. Myelin basic protein
2 studies (6,11) evaluated the levels of myelin basic protein (MBP) in serum, as a TBI prognostic factor. In the study which was performed on children under 15 years of age with traumatic brain injury, a significant relation was found between levels of this protein and the GOS, 3-4 and 6-8 months after trauma (6). In another study on children under 3 years who suffered a traumatic brain injury of varying intensities, high serum levels of MBP correlated with bad 6-month outcome which was measured by (Glasgow Outcome Scale using (GOS), Vineland Adaptive Behavior Scale (VABS) and the Intelligence Coefficient (IQ)
7. Glial Fibrillary Acidic Protein
The evidence for the prognostic value of serum levels of GFAP was strong. Seven studies (7,10,27,28,29,30,31) investigated serum GFAP levels as a prognostic factor and all of them reported the high values of GFAP correlates with poor prognosis. Four studies evaluated prognosis of TBI in children and reminding were performed on adults. In a study performed by S. Mondello and coworkers (27) in 2011, multivariate logistic regression analysis showed that of all the variables assessed, only UCH-L1 was an independent predictor of mortality at discharge and also strongly predicted deaths in 6 months after the damage predicted. Highly significant correlation between UCH-L1 and GFAP were found. GFAP did not have an additional contribution when UCH-L1 was already entered in the model. Similar predictive value for GFAP and UCH-L1 (c=0.93) was determined.
- Biochemical test
1. Blood sugar:
In 22 studies, blood glucose levels were investigated as a prognostic factor. All but three studies (32,33,34) reported that high levels of BS is associated with poor prognosis. All of the studies performed on children with traumatic brain injury (35,36,37,38) achieved significant correlation between BS levels and patient prognosis. All of the studies on adults with traumatic brain injury (32,33,34,40,41,42,43,44,45,46,47,48,49,50) and studies without a age limit (51,52) reported a significant relationship between blood glucose levels and prognosis achieved except two studies (32,34). The evidence for the prognostic value of BS levels was strong both in adults and in children with traumatic brain injury.
2. Lactate Dehydrogenase:
One study (53) evaluated Lactate Dehydrogenase levels as a prognostic factor of TBI. In both studies high levels were associated with poor prognosis. The evidence for the prognostic value of serum levels of LDH was strong. In V. Jain et al. study (68) in 2010, a significant relationship between serum LDH outcome after traumatic brain injury was found in patients with isolated brain trauma. In this study, the average increase in serum LDH was found in patients with a poor outcome and LDH levels increased continuously during the study period in both disabled and dead groups.
3.Plasma Osmolarity:
Two studies (34,46) investigated plasma osmolarity as a prognostic factor. In a study by WhaSook Seo and HyunSoo Oh in 2009 (72) on patients with traumatic brain injury (and hemorrhagic stroke), 6 months after the trauma one of the physiologically significant predictors of cognitive abilities in patients with TBI was admission serum osmolarity (p= 0.01), but there was no significant association between plasma osmolarity mortality and functional disability. In Nelson DW et al. study (49), poorer outcomes were observed with increasing osmolarity. According to these two studies, the evidence for the prognostic value plasma osmolarity was inconclusive.
4.Total cholesterol:
In WhaSook Seo and HyunSoo Oh study (72), 6 months after trauma, relationship between total cholesterol and mortality, cognitive abilities and functional disability in patients with TBI were not significant. In another study by Adel Helmy et al. (50), Total cholesterol only had a statistical relationship with traumatic brain injury outcome, via at least one other variable and was designated as ‘level 2’ of the hierarchy. According to these studies, serum total cholesterol probably is not a prognostic factor in patients with traumatic brain injury with a moderate level of evidence.
5.Albumin:
3 studies (34,46,50) investigated albumin level as a prognostic factor in TBI. In WhaSook Seo and HyunSoo Oh study (72) and in Adel Helmy et al. study (50), correlation of albumin levels with outcome was like total cholesterol level. In Nelson DW et al. study (49), low albumin relationship with poor outcome in patients with TBI was statistically significant. According to these studies, the evidence for the prognostic value of low albumin was also inconclusive.
6.Other biochemical tests:
Nelson DW study in 2005 (61) reported blood creatinine as an independent predictor of outcome after TBI. In study by Helmy et al. (50), low magnesium only had a statistical relationship with outcome via at least two other variables and was designated as ‘level 3’ of the hierarchy. Hohl and colleagues in a study in 2012 (12) found that sodium in the blood of those who died after TBI was significantly higher. According to the above studies, the levels blood sodium was a strong prognostic factor of poor outcome in patients with traumatic brain injury, but the evidence for the prognostic value of the other variables was limited and uncertain.
Complete Blood Count (CBC):
1. Hemoglobin
Five studies (34,43,46,48,50) were reviewed which assessed Hb levels as a prognostic factor in TBI. In 3 of them (43,48,50), low levels associated with poor prognosis. In two studies (34,46) there was no significant correlations between Hb levels and prognosis. According to the studies, there was inconclusive evidence of relationship between Hb level and outcome in traumatic brain injury.
2. The leukocyte count
Three studies (38,50,55) were reviewed which assessed WBC count as a prognostic factor in TBI. None of them showed significant correlations between WBC levels and TBI prognosis. According to the studies, there was strong evidence of no relationship between WBC level and outcome in traumatic brain injury.
- Blood Gases and ABG Results:
3 studies (34,39,43) were reviewed which assessed ABG results as a prognostic factor in TBI. In study by WhaSook Seo & HyunSoo Oh (72), 6 months after trauma physiological predictors of mortality in patients with traumatic brain injury was arterial oxygen pressure (F=11.83, p=0.00) and arterial carbon dioxide pressure (F=4.40, p=0.02). In another study performed by Tude Melo et al. in 2010 (38), low blood oxygen saturation found to be a prognostic factor for mortality (OR)=1.67. According to the studies, there was a limited evidence of relationship between PaCO2, PaO2, aPH, O2sat and outcome of traumatic brain injury.
Coagulation Factors and Products:
8 studies (31,38,39,43,58,71) were reviewed which assessed coagulation factors and products as a prognostic factor in TBI:
5 studies (38,39,43,58) assessed prothrombin time (PT) as a prognostic factor in TBI and all of them found a significant correlation between increased PT and poor outcome and mortality. So the evidence about prognosis prediction of PT is strong.
3 studies (38,58) assessed partial thromboplastin time (PTT) as a prognostic factor in TBI and two studies (38,58) found a significant correlation between increased a PTT and poor outcome. So the evidence about prognosis prediction of PTT is strong.
3 studies (38,58) assessed platelet count as a prognostic factor in TBI and two studies (58) found a significant correlation between decreased platelet count and poor outcome. So the evidence about prognosis prediction of platelet count is strong.
2 studies (14) assessed D.dimer levels in serum as a prognostic factor in TBI and none of them found a significant correlation between its levels and outcome. Therefore, the evidence about that there is no relation between prognosis and levels of D.dimer is strong.
Only one study assessed each serum FDP levels and serum VWF factor levels (31) found a significant correlation between them and outcome. Thus, the evidence about prognosis prediction of both of these is limited.
-Acute Phase Reactants:
1.Heat Shock Protein 70 (HSP 70):
2 studies (58,59) assessed HSP 70 levels in serum as a prognostic factor in TBI and both of them found a significant correlation between its levels and outcome. So the evidence about prognosis prediction of HSP70 is strong.
2. Pentraxin-PTX3
Only one study (54) investigated Pentraxin-PTX3 serum protein as a prognostic factor. In this study which was conducted in 2011 by Jackson da Silva Gullo et al., (20) increased PTX3 levels correlated with mortality (P<0.04). Thus, the evidence about prognosis prediction of PTX3 levels is limited.
-Inflammatory Factors:
3 studies (60,61,62) assessed some of the cytokines and inflammatory factors as prognostic factor in TBI. In Gopcevic et al. study (8), plasma level of IL-8 was significantly lower in survivors (71.00 +/- 14.17 pg/ml) than in non-survivors (111.26 +/- 16.9 pg/ml). In Stein et al. study (60), median daily IL-8 levels associated with poor outcome, the median serum values of other Cytokine levels (IL-1B, IL-6, IL-8, IL-10, and TNF-alfa) were not different between 2 groups (GOSE 1–4 vs 5–8). In Soares et al. study (58), significant correlations of elevated serum levels of IL-10, but not TNF-α, with hospital mortality in patients with severe TBI were reported (p=0.01). Considering all these studies suggest that increased serum levels of IL-8 may be a strong prognostic factor but uncertain and limited predictive power of other inflammatory factors was seen.
- Hormones
1. ACTH
2. Cortisol
3. Estradiol
4. Testosterone
5. Progesterone
6.LH & FSH
2 studies (63,64) were reviewed which assessed Cortisol (63,64), ACTH (63) and sex hormones (64) as prognostic factors in TBI.
In K. Wagner et al. study (42), high estradiol and testosterone associated with mortality (p=0.026 and p=0.033, respectively). Significant effect of LH, FSH, progesterone on mortality through their association with estradiol (p=0.049). High estradiol was associated with worse outcomes. Stradiol mediated progesterone associations with GOS (p=0.045). Serum cortisol was not associated with mortality or GOS. In Llompart-Poue et al. study (37), patients with low ACTH values (<9 pg/mL): statistically significant lower mortality (7% vs. 55%, p<0.0001) and low plasma ACTH in patient who survived, correlated with increased ICU length of stay (p<0.03). But no significant differences with baseline and stimulated serum cortisol after a high-dose corticotrophin stimulation test were seen. According to these studies, the serum cortisol strongly has no relation with outcome of patients with brain injury. And the evidence of the prognostic value of serum levels other hormones mentioned, was inclusive.
Matrix metalloproteinase 9:
In the study conducted by M. DeFazio et al. (17) a significant difference in the mean concentration of MMP-9 at admission (P=0.115) or in 24 h (P=0.535) was not found between the short term outcome groups. The study conducted by J. Copin et al. (11) a significant relationship between serum MMP-9 levels and three-month GOSE in patients with severe TBI was not seen. According to these studies, the serum MMP9 levels have no relation with outcome of patients with brain injury with moderate evidence.
α II-Spectrin Breakdown Product 145kDa:
Only one study (6) investigated serum SBDP145 level as a prognostic factor in TBI.
In one study (6), unfavorable outcome was correlated with higher concentrations of SBDP145.
According to this study, the evidence for the prognostic value of low SBDP145 was limited.
Circulating endothelial progenitor cells:
2 studies (66,67) were reviewed which assessed circulating endothelial progenitor cells as prognostic factor in TBI.
In Li Liu et al. study (9), number of circulating EPCs was significantly lower in who died p<0.01 .
In Gong D et al. study (69), number of circulating EPCs was significantly correlated with GOS scores 6 months after TBI. Thus, the evidence for the predictive value of circulating endothelial progenitor cells was strong.
- Miscellaneous:
The studies of other factors, including serum oxidative stress parameters: thiobarbituric acid reactive species (TBARS) and carbonyl group (48), serum leptin (68) serum fibronectin CFn and troponin cTnI were also reviewed which due to the low number of these studies for each factor, they can be a potential prognostic factors with limited evidence for TBI.
Conclusion
This systematic review summarized the results of 63 articles about the predictive value of various factors on prognosis after brain damage. Providing new information or explaining the findings in terms of pathophysiology is not the primary goal of a systematic review. Therefore, although relevant for clinicians, we were cautious not to speculate about underlying mechanisms or explanations for which no evidence was given in the included studies. Our study established strong evidence that serum concentration of S100 protein, neuron specific enolase, MBP, NF-H, GFAP, UCH-L1, blood glucose levels, serum levels of LDH, sodium level, prothrombin time, partial thromboplastin time, platelet count, D.dimer, HSP 70, serum levels of IL-8, number of circulating EPCs, and DNA levels in serum were predictors of post-TBI outcome. This study found strong evidence that WBC count and serum cortisol levels do not predict outcome. Moreover, moderate evidence was found that serum total cholesterol count do not predict outcome. Moderate evidence showed that high serum MMP9 levels predict poor outcome. For all other determinants the evidence was limited or inconclusive. Although these profiles are best evidence for prognosis after TBI, they seem to be of limited value; hence still we are not able to correct or prevent or treat some of these factors. Overall, it can be concluded that much information is needed on long term outcome moderate and severe traumatic brain injury.
Limitations of the review
It was very difficult to reach a consensus on all epidemiological findings across the 63 published studies because of critical differences in methods employed across the reports. Firstly, we searched studies published between the 2005 and 2014. It is possible that relevant publications before or after that time were not included in this review. However, we think that it would be inappropriate to include older studies in a review on prognostic factors, because there have been dramatic changes in measuring biomarkers concentrations and the treatment of traumatic injuries over the last years.
Some of the included studies excluded penetrating head injury, other studies did not. Little information was given in the studies about how many patients had closed or open head injuries. It is not clear whether this has influenced our results. There was considerable heterogeneity for all outcomes of interest and in the time period over which outcome was evaluated. In the literature, different definitions for traumatic brain injury and the diagnostic methods are used. We decided to define brain injuries as the changes in brain function because of severe damage by an external force. We choose this fairly extensive definition is brain damage, so we would be able to enter many of the relevant studies. Furthermore, the populations studied were varied extensively in each literature from the other, in terms of gender, age, region and country in which they lived and were treated. Finally, we did not include studies published in languages other than English.
Recommendations:
Prediction of outcome after brain injury is not always straightforward, and there is always some uncertainty. Multiple factors may affect the outcome. Much of the literature available is written from an isolated neurological, neurosurgical or rehabilitation perspective. To improve outcome prediction, multidisciplinary research should take place, and knowledge should be integrated.
Although several biomarkers of brain injury have been identified, continued research is required. A single biomarker may not have desired sensitivity and specificity for predicting outcome. Biomarkers, in combination with other clinical data, such as GCS and head CT scan, would maximize the accuracy. Future studies will be required to not only identify these biomarkers prognostic ability together with other factors.
Acknowledgment
The authors would like to thank the staff of the Neurosurgery Ward of Imam-Hossein Hospital, Tehran, Iran.
Funding
None declared.
Conflicts of Interest
The authors declare that they have no competing interests.
References
1. Goyal A, Carter M, Niyonkuru C, Fabio A, Amin K, Berger RP, Wagner AK M D. S100b as a Prognostic Biomarker in Outcome Prediction for Patients with Severe TBI. J Neurotrauma. 2013;30(11):946-57.
2. Mowery NT. Stress Insulin Resistance is a Marker for Mortality in Traumatic Brain Injury. J Trauma. 2009:66(1):145-51; 151-3.
3. CampelloYurgel V, Ikuta N, Brondani da Rocha A, Lunge VR, Fett Schneider R, Kazantzi Fonseca AS, et al. Role of Plasma DNA as a Predictive Marker of Fatal Outcome following Severe Head Injury in Males. J Neurotrauma. 2007;24(7):1172–81. Available from: http://dx.doi.org/10.1089/neu.2006.0160
4. Ali E. Seif El-Deen, Said Hammad. Preoperative Serum S100 B Protein as a Prognostic Marker for Traumatic Brain Injury Patients. E.J.N.S. 2009;24 (1)135-152.
5. DeFazio MV, Rammo RA, Robles JR, Bramlett HM, Dietrich WD, Bullock MR. The Potential Utility of Blood-Derived Biochemical Markers as Indicators of Early Clinical Trends Following Severe Traumatic Brain Injury. World Neurosurgery. 2014;81(1):151–8. Available from: http://dx.doi.org/10.1016/j.wneu.2013.01.015
6. Beers SR, Berger RP, Adelson PD. Neurocognitive outcome and serum biomarkers in inflicted versus non-inflicted traumatic brain injury in young children. J Neurotrauma. 2007;24(1):97-105.
7. A.Salim. Persistent Hyperglycemia in Severe Traumatic Brain Injury: An Independent Predictor of Outcome. Am Surg. 2009;75(1):25-9.
8. Gopcevic A. Plasma interleukin-8 as a potential predictor of mortality in adult patients with severe traumatic brain injury. Tohoku J Exp Med. 2007;211(4):387-93.
9.Liu L, Wei H, Chen F, Wang J, Dong JF, Zhang J. Endothelial progenitor cells correlate with clinical outcome of traumatic brain injury. Crit Care Med. 2011;39(7):1760-5.
10. Bayir A, Kalkan E, Kocak S, Ak A, Cander B, Bodur S. Fibrinolytic markers and neurologic outcome in traumatic brain injury. Neurol India.2006;54:363-5.
11.Copin H.Matrix metalloproteinase 9 and cellular fibronectin plasma concentrations are predictors of the composite endpoint of length of stay and death in the intensive care unit after severe traumatic brain injury. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine.2012;43(6): 23-27.
12.Meshkini A,Salehpour F. Relationships of hyperglycemia and neurological outcome in patients with head injury.Anesthesia.2007;43(2): 2-6.
13. Douglas D. Fraser. Severe traumatic brain injury in children elevates glial fibrillary acidic protein in cerebrospinal fluid and serum. Pediatr Crit Care Med.2011;32(6):33-36.
14. Choon Hong Kan, MohdSaffari, TeikHooiKhoo. Prognostic Factors of Severe Traumatic Brain Injury Outcome in Children Aged 2-16 Years at A Major Neurosurgical Referral Centre. Malaysian Journal of Medical Sciences.2009;16(4):25-33.
15. SalehpoorF, Meshkini A. Prognostic value of serum LDH in head trauma. The International Medical Journal. 2005;4(2)31-37.
16. Meier R. Differential temporal profile of lowered blood glucose levels (3.5 to 6.5 mmol/l versus 5 to 8 mmol/l) in patients with severe traumatic brain injury. Crit Care.2008;12(4):98-102.
17. Hohl E. Plasma levels of oxidative stress biomarkers and hospital mortality in severe head injury: A multivariate analysis. Journal of Critical Care 27, 523.e11–523.e19;2012.
18.Liliang PC. Tau Proteins in Serum Predict Outcome After Severe Traumatic Brain Injury.Journal of Surgical Research. 2010;160(5):302–307.
19. Hossam M, Jehan H. Sabry, Deena A. El-Shabrawy. The Predictability of at Admission Serum GFAP and S100 protein Levels for the Outcome of Traumatic Brain Injury Patients. Egy. J. Neur. Surg. 2011;26(1):50-56.
20. Gullo J da S, Bertotti MM, Silva CCP, Schwarzbold M, Diaz AP, Soares FMS, et al. Hospital Mortality of Patients with Severe Traumatic Brain Injury is Associated with Serum PTX3 Levels. Neurocrit Care. 2010; 23;14(2):194–9. Available from: http://dx.doi.org/10.1007/s12028-010-9462-y.
21.Greuters. Acute and delayed mild coagulopathy are related to outcome in patients with isolated traumatic.brain injury.Crit Care.2011;15(1):2.
22.StefaniaM. Neuronal and glial markers are differently associated with computed tomography findings and outcome in patients with severe traumatic brain injury: a case control study. Critical Care.2012;15(1):156-159.
24. Guzel A.Serum neuron-specific enolase as a predictor of short-term outcome and its correlation with Glasgow Coma Scale in traumatic brain injury.Neurosurg Rev.2008; 31:439–445.
25. Zitnay GA, Zitnay KM, Povlishock JT, Hall ED, Marion DW, Trudel T, et al. Traumatic Brain Injury Research Priorities: The Conemaugh International Brain Injury Symposium. Journal of Neurotrauma 2008;25(10):1135–52. Available from: http://dx.doi.org/10.1089/neu.2008.0599
26. Hada M. Role of early cell-free DNA levels decrease as a predictive marker of fatal outcome after severe traumatic brain injury. ClinicaChimica Acta.2012; 414: 12–17.
27.Lanier WL, StanglandKJ ,Scheithaure BW. The effects of dextrose infusion and head position on neurologic outcome after complete cerebral ischemia in primates: examination of a model. Anesthesiology.1987;66:39-48.
28.Chabok SY, Moghadam AD, Saneei Z, Amlashi FG, Leili EK, Amiri ZM. Neuron-specific enolase and S100BB as outcome predictors in severe diffuse axonal injury. Journal of Trauma and Acute Care Surgery. 2012;72(6):1654–7. Available from: http://dx.doi.org/10.1097/ta.0b013e318246887e
29.Pelinka LE, Kroepfl A, Leixnering M, Buchinger W, Raabe A, Redl H. GFAP Versus S100B in Serum after Traumatic Brain Injury: Relationship to Brain Damage and Outcome. J Neurotrauma. 2004; 21(11):1553–61. Available from: http://dx.doi.org/10.1089/0897715042441846
30. Smith A.Relationship between hyperglycemia and outcome in children with severe traumatic brain injury.PediatrCrit Care Med.2012;13(1):85-91.
31. Lin C, Huang SJ, Wang N, Shen ZP. Relationship between plasma leptin levels and clinical outcomes.
32.Turgeon AF, Lauzier F, Burns KEA, Meade MO, Scales DC, Zarychanski R. Determination of neurological prognosis in adult patients with severe traumatic brain injury: a survey of Canadian intensivists, neurosurgeons and neurologists. Crit Care Med ,epub ahead of print; 2013 .
33. HergenroederG.W. Serum IL-6: a candidate biomarker for intracranial pressure elevation following isolated traumatic brain injury. Journal of Neuroinflammation.2010;3:7-19.
34. Jeremitsky E. The Impact of Hyperglycemia on Patients with Severe Brain Injury. J Trauma. Jan.2005;58(1):31-36.
35. Liu D.Clinical Impact of Early Hyperglycemia during Acute Phase of Traumatic Brain Injury.Neurocrit Care.2009;11:151–157.
36. Donald E. G. Griesdale, Marie-He´le`ne Tremblay, Jonathan McEwen, Dean R. Chittock. Glucose Control and Mortality in Patients with Severe Traumatic Brain Injury. Neurocrit Care.2009;11:311–316.
37. Llompart-Pou JA. Relationship between plasma adrenocorticotropin hormone and intensive care unit survival in early traumatic brain injury. J Trauma.2007;62(6):1457-61.
38.Tude M. Mortality in Children with Severe Head Trauma: Predictive Factors and Proposal for a New Predictive Scale. Neurosurgery.2010;67(6):1542-7.
39.Hossam M, Jehan H. Sabry, Deena A. El-Shabrawy. The Predictability of at Admission Serum GFAP and S100 protein Levels for the Outcome of Traumatic Brain Injury Patients. Egy. J. Neur. Surg.2011;26(1);11-19.
40.Matsushima K, Peng M, Velasco C, Schaefer E, Diaz-Arrastia R, Frankel H. Glucose variability negatively impacts long-term functional outcome in patients with traumatic brain injury. J Crit Care.2012;27(2):125-31.
41. Žurek J, Bartlová L, Fedora M. Hyperphosphorylatedneurofilament NF-H as a predictor of mortality after brain injury in children. Brain InjInforma Healthcare; 2011;25(2):221–6. Available from: http://dx.doi.org/10.3109/02699052.2010.541895
42.Amy K., Wagner. Acute Serum Hormone Levels: Characterization and Prognosis after Severe Traumatic Brain Injury. J Neurotrauma.2011;28(6): 871–888.
43.Olivecrona M, Rodling-Wahlstrom M, Naredi S, Koskinen L-OD. S-100B and neuron specific enolase are poor outcome predictors in severe traumatic brain injury treated by an intracranial pressure targeted therapy. Journal of Neurology, Neurosurgery & Psychiatry. BMJ;2009;80(11):1241–8. Available from: http://dx.doi.org/10.1136/jnnp.2008.158196
44. SaadatS. Association of persistent hyperglycemia with outcome of severe traumatic brain injury in pediatric population. Childs Nerv Syst.2012; 28:1773–1777.
45. Naeimi ZS, Weinhofer A, Sarahrudi K, Heinz T, Vécsei V. Predictive value of S-100B protein and neuron specific-enolase as markers of traumatic brain damage in clinical use. Brain Inj. Informa UK Limited; 2006;20(5):463–8. Available from: http://dx.doi.org/10.1080/02699050600664418
46.CzeiterR. Brain Injury Biomarkers May Improve the Predictive Power of the IMPACT Outcome Calculator. Journal of Neurotrauma.2012; 29:1770–1778 .
47. Nazik A, Fatih T, Muhammet Ş. Admission hyperglycemia is a reliable outcome predictor in children with severe traumatic brain injury. J Pediatr (Rio J).2011;87(4):325-8.
48. Salim A. Significance of Troponin Elevation after Severe Traumatic Brain Injury. J Trauma.2008; 64(1):46-52.
49. Nelson DW, Rudehill A, MacCallum RM, Holst A, Wanecek M, Weitzberg E, et al. Multivariate Outcome Prediction in Traumatic Brain Injury with Focus on Laboratory Values. Journal of Neurotrauma. 2012;29(17):2613–24. Available from: http://dx.doi.org/10.1089/neu.2012.2468
50.Perel P, Wasserberg J, Ravi RR, Shakur H, Edwards P, Roberts I. Prognosis following head injury: a survey of doctors from developing and developed countries. J EvalClin Pract2007;13:464-0005.
51.Melo JR. Acute hyperglycemia is a reliable outcome predictor in children with severe traumatic brain injury. ActaNeurochir (Wien).2010; 152(9):1559-65.
52. Rachel P. Berger, Ronald L. Hayes, Rudolph Richichi, Sue R. Beers. Serum Concentrations of Ubiquitin C-Terminal Hydrolase-L1 and αII-Spectrin Breakdown Product 145kDa Correlate with Outcome after Pediatric TBI. J Neurotrauma.2012; 29(1): 162–167.
53. Samit M. Biochemical Serum Markers in Head Injury, Clinical Neurosurgery.2012;57:134-140.
54. Tude M. Defenestration in children younger than 6 years old: mortality predictors in severe head trauma. Childs Nerv Syst.2009; 25:1077–1083.
55.Mondello E. Clinical Utility of Serum Levels of Ubiquitin C-Terminal Hydrolase as a Biomarker for Severe Traumatic Brain Injury. Neurosurgery.2012;70(3):666-75.
56. Nyle K. Increased serum-GFAP in patients with severe traumatic brain injury is related to outcome. Journal of the Neurological Sciences.2006; 240: 85 – 91.
57.Mc Gonzalez-Mao. Model Predicting Survival / ExitusAfter Traumatic Brain Injury: Biomarker S100B 24H. Clin. Lab.2011; 57:587-597.
58. Soares L. Interleukin-10 Is an Independent Biomarker of Severe Traumatic Brain Injury Prognosis. Neuroimmunomodulation. 2012;19:377–385.
59.Salehpour F, Bazzazi AM, Porhomayon J, NaderND. Correlation between coagulopathy and outcome in severe head trauma in neurointensive care and trauma units. J Crit Care.2011;26(4):352-6.
60.Stein DM. Relationship of Serum and Cerebrospinal Fluid Biomarkers With Intracranial Hypertension and Cerebral Hypoperfusion After Severe Traumatic Brain Injury. J Trauma.2011;70(5):1096-103.
61. Nelson DW. Hierarchical log linear analysis of admission blood parameters and clinical outcome following traumatic brain injury. J Neurotrauma.2012;29(17):2613-24.
62. NyleN. Serum levels of S100B, S100A1B and S100BB are all related to outcome after severe traumatic brain injury. ActaNeurochir (Wien).2008;150(3):221-7.
63. Raineya T, Leskob M. Predicting outcome after severe traumatic brain injury using the serum S100B biomarker: Results using a single (24 h) time-point. Resuscitation.2009; 341–345.
64.ŽurekJ ,Fedora M. The usefulness of S100B, NSE, GFAP, NF-H, secretagogin and Hsp70 as a predictive biomarker of outcome in children with traumatic brain injury. Acta Neurochir.2012; 154:93–103.
66. Els C.H. Prognosis of six-month function after traumatic brain injury.Rehabil Med.2010; 42: 425–436.
67.V. Jain, S. Tiwari, S. Misra, Tiwari, Nagendra. Predictive Value of Serum Lactate Dehydrogenase in Head Injury. The Internet Journal of Surgery. 2010; 22(2):101-110.
68.Barlow P, Teasdale G. Prediction of outcome and the management of severe head injuries: the attitudes of neurosurgeons. Neurosurg.1986; 19:989-991.
69. Gong D, Hao M, Liu L, Liu C, Dong J, Cui Z, et al. Prognostic relevance of circulating endothelial progenitor cells for severe traumatic brain injury. Brain Inj. Informa Healthcare. 2012;26(3):291–7. Available from: http://dx.doi.org/10.3109/02699052.2011.648710
70. Oliviera D. Plasma von Willebrand Factor Levels Correlate with Clinical Outcome of Severe Traumatic Brain Injury. Journal of neurotrauma.2007; 24:1331–1338.
71. Papa L. Serum levels of ubiquitin C-terminal hydrolase distinguish mild traumatic brain injury from trauma controls and are elevated in mild and moderate traumatic brain injury patients with intracranial lesions and neurosurgical intervention. J Trauma Acute Care Surg.2012; 72(5):1335-44.
72. WhaSookSeo, HyunSoo Oh. Comparisons of Acute Physiological Parameters Influencing Outcome in Patients with Traumatic Brain Injury and Hemorrhagic Stroke. Worldviews Evid Based Nurs.6(1):36-43;2009.
73.Prisco L, Iscra F, Ganau M, Berlot G.Early predictive factors on mortality in head injured patients: a retrospective analysis of 112 traumatic brain injured patients. J Neurosurg Sci. 2012 Jun;56(2):131-6.
Type of Study: Review |
Subject:
Gamma Knife Radiosurgery
References
1. Goyal A, Carter M, Niyonkuru C, Fabio A, Amin K, Berger RP, Wagner AK M D. S100b as a Prognostic Biomarker in Outcome Prediction for Patients with Severe TBI. J Neurotrauma. 2013;30(11):946-57. [DOI:10.1089/neu.2012.2579] [PMID] [PMCID]
2. Mowery NT. Stress Insulin Resistance is a Marker for Mortality in Traumatic Brain Injury. J Trauma. 2009:66(1):145-51; 151-3.
3. CampelloYurgel V, Ikuta N, Brondani da Rocha A, Lunge VR, Fett Schneider R, Kazantzi Fonseca AS, et al. Role of Plasma DNA as a Predictive Marker of Fatal Outcome following Severe Head Injury in Males. J Neurotrauma. 2007;24(7):1172–81. Available from: http://dx.doi.org/10.1089/neu.2006.0160 [DOI:10.1089/neu.2006.0160]
4. Ali E. Seif El-Deen, Said Hammad. Preoperative Serum S100 B Protein as a Prognostic Marker for Traumatic Brain Injury Patients. E.J.N.S. 2009;24 (1)135-152.
5. DeFazio MV, Rammo RA, Robles JR, Bramlett HM, Dietrich WD, Bullock MR. The Potential Utility of Blood-Derived Biochemical Markers as Indicators of Early Clinical Trends Following Severe Traumatic Brain Injury. World Neurosurgery. 2014;81(1):151–8. Available from: http://dx.doi.org/10.1016/j.wneu.2013.01.015 [DOI:10.1016/j.wneu.2013.01.015]
6. Beers SR, Berger RP, Adelson PD. Neurocognitive outcome and serum biomarkers in inflicted versus non-inflicted traumatic brain injury in young children. J Neurotrauma. 2007;24(1):97-105. [DOI:10.1089/neu.2006.0055] [PMID]
7. A.Salim. Persistent Hyperglycemia in Severe Traumatic Brain Injury: An Independent Predictor of Outcome. Am Surg. 2009;75(1):25-9. [PMID]
8. Gopcevic A. Plasma interleukin-8 as a potential predictor of mortality in adult patients with severe traumatic brain injury. Tohoku J Exp Med. 2007;211(4):387-93. [DOI:10.1620/tjem.211.387] [PMID]
9. Liu L, Wei H, Chen F, Wang J, Dong JF, Zhang J. Endothelial progenitor cells correlate with clinical outcome of traumatic brain injury. Crit Care Med. 2011;39(7):1760-5. [DOI:10.1097/CCM.0b013e3182186cee] [PMID] [PMCID]
10. Bayir A, Kalkan E, Kocak S, Ak A, Cander B, Bodur S. Fibrinolytic markers and neurologic outcome in traumatic brain injury. Neurol India.2006;54:363-5. [DOI:10.4103/0028-3886.28106] [PMID]
11. Copin H.Matrix metalloproteinase 9 and cellular fibronectin plasma concentrations are predictors of the composite endpoint of length of stay and death in the intensive care unit after severe traumatic brain injury. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine.2012;43(6): 23-27. [DOI:10.1186/1757-7241-20-83]
12. Meshkini A,Salehpour F. Relationships of hyperglycemia and neurological outcome in patients with head injury.Anesthesia.2007;43(2): 2-6.
13. Douglas D. Fraser. Severe traumatic brain injury in children elevates glial fibrillary acidic protein in cerebrospinal fluid and serum. Pediatr Crit Care Med.2011;32(6):33-36. [DOI:10.1097/PCC.0b013e3181e8b32d]
14. Choon Hong Kan, MohdSaffari, TeikHooiKhoo. Prognostic Factors of Severe Traumatic Brain Injury Outcome in Children Aged 2-16 Years at A Major Neurosurgical Referral Centre. Malaysian Journal of Medical Sciences.2009;16(4):25-33.
15. SalehpoorF, Meshkini A. Prognostic value of serum LDH in head trauma. The International Medical Journal. 2005;4(2)31-37.
16. Meier R. Differential temporal profile of lowered blood glucose levels (3.5 to 6.5 mmol/l versus 5 to 8 mmol/l) in patients with severe traumatic brain injury. Crit Care.2008;12(4):98-102. [DOI:10.1186/cc6974] [PMID] [PMCID]
17. Hohl E. Plasma levels of oxidative stress biomarkers and hospital mortality in severe head injury: A multivariate analysis. Journal of Critical Care 27, 523.e11–523.e19;2012. [DOI:10.1016/j.jcrc.2011.06.007] [PMID]
18. Liliang PC. Tau Proteins in Serum Predict Outcome After Severe Traumatic Brain Injury.Journal of Surgical Research. 2010;160(5):302–307. [DOI:10.1016/j.jss.2008.12.022] [PMID]
19. Hossam M, Jehan H. Sabry, Deena A. El-Shabrawy. The Predictability of at Admission Serum GFAP and S100 protein Levels for the Outcome of Traumatic Brain Injury Patients. Egy. J. Neur. Surg. 2011;26(1):50-56.
20. Gullo J da S, Bertotti MM, Silva CCP, Schwarzbold M, Diaz AP, Soares FMS, et al. Hospital Mortality of Patients with Severe Traumatic Brain Injury is Associated with Serum PTX3 Levels. Neurocrit Care. 2010; 23;14(2):194–9. Available from: http://dx.doi.org/10.1007/s12028-010-9462-y. [DOI:10.1007/s12028-010-9462-y]
21. Greuters. Acute and delayed mild coagulopathy are related to outcome in patients with isolated traumatic.brain injury.Crit Care.2011;15(1):2. [DOI:10.1186/cc9399] [PMID] [PMCID]
22. StefaniaM. Neuronal and glial markers are differently associated with computed tomography findings and outcome in patients with severe traumatic brain injury: a case control study. Critical Care.2012;15(1):156-159.
23. Guzel A.Serum neuron-specific enolase as a predictor of short-term outcome and its correlation with Glasgow Coma Scale in traumatic brain injury.Neurosurg Rev.2008; 31:439–445. [DOI:10.1007/s10143-008-0148-2] [PMID]
24. Zitnay GA, Zitnay KM, Povlishock JT, Hall ED, Marion DW, Trudel T, et al. Traumatic Brain Injury Research Priorities: The Conemaugh International Brain Injury Symposium. Journal of Neurotrauma 2008;25(10):1135–52. Available from: http://dx.doi.org/10.1089/neu.2008.0599 [DOI:10.1089/neu.2008.0599]
25. Hada M. Role of early cell-free DNA levels decrease as a predictive marker of fatal outcome after severe traumatic brain injury. ClinicaChimica Acta.2012; 414: 12–17. [DOI:10.1016/j.cca.2012.08.001] [PMID]
26. Lanier WL, StanglandKJ ,Scheithaure BW. The effects of dextrose infusion and head position on neurologic outcome after complete cerebral ischemia in primates: examination of a model. Anesthesiology.1987;66:39-48. [DOI:10.1097/00000542-198701000-00008] [PMID]
27. Chabok SY, Moghadam AD, Saneei Z, Amlashi FG, Leili EK, Amiri ZM. Neuron-specific enolase and S100BB as outcome predictors in severe diffuse axonal injury. Journal of Trauma and Acute Care Surgery. 2012;72(6):1654–7. Available from: http://dx.doi.org/10.1097/ta.0b013e318246887e [DOI:10.1097/TA.0b013e318246887e]
28. Pelinka LE, Kroepfl A, Leixnering M, Buchinger W, Raabe A, Redl H. GFAP Versus S100B in Serum after Traumatic Brain Injury: Relationship to Brain Damage and Outcome. J Neurotrauma. 2004; 21(11):1553–61. Available from: http://dx.doi.org/10.1089/0897715042441846 [DOI:10.1089/0897715042441846]
29. Smith A.Relationship between hyperglycemia and outcome in children with severe traumatic brain injury.PediatrCrit Care Med.2012;13(1):85-91. [DOI:10.1097/PCC.0b013e3182192c30] [PMID] [PMCID]
30. Lin C, Huang SJ, Wang N, Shen ZP. Relationship between plasma leptin levels and clinical outcomes.
31. Turgeon AF, Lauzier F, Burns KEA, Meade MO, Scales DC, Zarychanski R. Determination of neurological prognosis in adult patients with severe traumatic brain injury: a survey of Canadian intensivists, neurosurgeons and neurologists. Crit Care Med, epub ahead of print; 2013 . [DOI:10.1097/CCM.0b013e318275d046]
32. HergenroederG.W. Serum IL-6: a candidate biomarker for intracranial pressure elevation following isolated traumatic brain injury. Journal of Neuroinflammation.2010;3:7-19. [DOI:10.1186/1742-2094-7-19]
33. Jeremitsky E. The Impact of Hyperglycemia on Patients with Severe Brain Injury. J Trauma. Jan.2005;58(1):31-36.
34. Liu D.Clinical Impact of Early Hyperglycemia during Acute Phase of Traumatic Brain Injury.Neurocrit Care.2009;11:151–157. [DOI:10.1007/s12028-009-9228-6] [PMID]
35. Donald E. G. Griesdale, Marie-He´le`ne Tremblay, Jonathan McEwen, Dean R. Chittock. Glucose Control and Mortality in Patients with Severe Traumatic Brain Injury. Neurocrit Care.2009;11:311–316. [DOI:10.1007/s12028-009-9249-1] [PMID]
36. Llompart-Pou JA. Relationship between plasma adrenocorticotropin hormone and intensive care unit survival in early traumatic brain injury. J Trauma.2007;62(6):1457-61. [DOI:10.1097/01.ta.0000219143.69483.71] [PMID]
37. Tude M. Mortality in Children with Severe Head Trauma: Predictive Factors and Proposal for a New Predictive Scale. Neurosurgery.2010;67(6):1542-7. [DOI:10.1227/NEU.0b013e3181fa7049]
38. Hossam M, Jehan H. Sabry, Deena A. El-Shabrawy. The Predictability of at Admission Serum GFAP and S100 protein Levels for the Outcome of Traumatic Brain Injury Patients. Egy. J. Neur. Surg.2011;26(1);11-19.
39. Matsushima K, Peng M, Velasco C, Schaefer E, Diaz-Arrastia R, Frankel H. Glucose variability negatively impacts long-term functional outcome in patients with traumatic brain injury. J Crit Care.2012;27(2):125-31. [DOI:10.1016/j.jcrc.2011.08.012] [PMID]
40. Žurek J, Bartlová L, Fedora M. Hyperphosphorylatedneurofilament NF-H as a predictor of mortality after brain injury in children. Brain InjInforma Healthcare; 2011;25(2):221–6. Available from: http://dx.doi.org/10.3109/02699052.2010.541895 [DOI:10.3109/02699052.2010.541895]
41. Amy K., Wagner. Acute Serum Hormone Levels: Characterization and Prognosis after Severe Traumatic Brain Injury. J Neurotrauma.2011;28(6): 871–888. [DOI:10.1089/neu.2010.1586] [PMID] [PMCID]
42. Olivecrona M, Rodling-Wahlstrom M, Naredi S, Koskinen L-OD. S-100B and neuron specific enolase are poor outcome predictors in severe traumatic brain injury treated by an intracranial pressure targeted therapy. Journal of Neurology, Neurosurgery & Psychiatry. BMJ;2009;80(11):1241–8. Available from: http://dx.doi.org/10.1136/jnnp.2008.158196 [DOI:10.1136/jnnp.2008.158196]
43. SaadatS. Association of persistent hyperglycemia with outcome of severe traumatic brain injury in pediatric population. Childs Nerv Syst.2012; 28:1773–1777. [DOI:10.1007/s00381-012-1753-5] [PMID]
44. Naeimi ZS, Weinhofer A, Sarahrudi K, Heinz T, Vécsei V. Predictive value of S-100B protein and neuron specific-enolase as markers of traumatic brain damage in clinical use. Brain Inj. Informa UK Limited; 2006;20(5):463–8. Available from: http://dx.doi.org/10.1080/02699050600664418 [DOI:10.1080/02699050600664418]
45. CzeiterR. Brain Injury Biomarkers May Improve the Predictive Power of the IMPACT Outcome Calculator. Journal of Neurotrauma.2012; 29:1770–1778 . [DOI:10.1089/neu.2011.2127] [PMID] [PMCID]
46. Nazik A, Fatih T, Muhammet Ş. Admission hyperglycemia is a reliable outcome predictor in children with severe traumatic brain injury. J Pediatr (Rio J).2011;87(4):325-8.
47. Salim A. Significance of Troponin Elevation after Severe Traumatic Brain Injury. J Trauma.2008; 64(1):46-52. [DOI:10.1097/TA.0b013e31815eb15a] [PMID]
48. Nelson DW, Rudehill A, MacCallum RM, Holst A, Wanecek M, Weitzberg E, et al. Multivariate Outcome Prediction in Traumatic Brain Injury with Focus on Laboratory Values. Journal of Neurotrauma. 2012;29(17):2613–24. Available from: http://dx.doi.org/10.1089/neu.2012.2468 [DOI:10.1089/neu.2012.2468]
49. Perel P, Wasserberg J, Ravi RR, Shakur H, Edwards P, Roberts I. Prognosis following head injury: a survey of doctors from developing and developed countries. J EvalClin Pract2007;13:464-0005. [DOI:10.1111/j.1365-2753.2006.00713.x] [PMID]
50. Melo JR. Acute hyperglycemia is a reliable outcome predictor in children with severe traumatic brain injury. ActaNeurochir (Wien).2010; 152(9):1559-65. [DOI:10.1007/s00701-010-0680-z] [PMID]
51. Rachel P. Berger, Ronald L. Hayes, Rudolph Richichi, Sue R. Beers. Serum Concentrations of Ubiquitin C-Terminal Hydrolase-L1 and αII-Spectrin Breakdown Product 145kDa Correlate with Outcome after Pediatric TBI. J Neurotrauma.2012; 29(1): 162–167. [DOI:10.1089/neu.2011.1989] [PMID] [PMCID]
52. Samit M. Biochemical Serum Markers in Head Injury, Clinical Neurosurgery.2012;57:134-140.
53. Tude M. Defenestration in children younger than 6 years old: mortality predictors in severe head trauma. Childs Nerv Syst.2009; 25:1077–1083. [DOI:10.1007/s00381-009-0924-5] [PMID]
54. Mondello E. Clinical Utility of Serum Levels of Ubiquitin C-Terminal Hydrolase as a Biomarker for Severe Traumatic Brain Injury. Neurosurgery.2012;70(3):666-75. [PMID] [PMCID]
55. Nyle K. Increased serum-GFAP in patients with severe traumatic brain injury is related to outcome. Journal of the Neurological Sciences.2006; 240: 85 – 91. [DOI:10.1016/j.jns.2005.09.007] [PMID]
56. Mc Gonzalez-Mao. Model Predicting Survival / ExitusAfter Traumatic Brain Injury: Biomarker S100B 24H. Clin. Lab.2011; 57:587-597. [PMID]
57. Soares L. Interleukin-10 Is an Independent Biomarker of Severe Traumatic Brain Injury Prognosis. Neuroimmunomodulation. 2012;19:377–385. [DOI:10.1159/000342141] [PMID]
58. Salehpour F, Bazzazi AM, Porhomayon J, NaderND. Correlation between coagulopathy and outcome in severe head trauma in neurointensive care and trauma units. J Crit Care.2011;26(4):352-6. [DOI:10.1016/j.jcrc.2010.12.005] [PMID]
59. Stein DM. Relationship of Serum and Cerebrospinal Fluid Biomarkers With Intracranial Hypertension and Cerebral Hypoperfusion After Severe Traumatic Brain Injury. J Trauma.2011;70(5):1096-103. [DOI:10.1097/TA.0b013e318216930d] [PMID]
60. Nelson DW. Hierarchical log linear analysis of admission blood parameters and clinical outcome following traumatic brain injury. J Neurotrauma.2012;29(17):2613-24. [DOI:10.1089/neu.2012.2468] [PMID]
61. NyleN. Serum levels of S100B, S100A1B and S100BB are all related to outcome after severe traumatic brain injury. ActaNeurochir (Wien).2008;150(3):221-7. [DOI:10.1007/s00701-007-1489-2] [PMID]
62. Raineya T, Leskob M. Predicting outcome after severe traumatic brain injury using the serum S100B biomarker: Results using a single (24 h) time-point. Resuscitation.2009; 341–345. [DOI:10.1016/j.resuscitation.2008.11.021] [PMID]
63. ŽurekJ ,Fedora M. The usefulness of S100B, NSE, GFAP, NF-H, secretagogin and Hsp70 as a predictive biomarker of outcome in children with traumatic brain injury. Acta Neurochir.2012; 154:93–103. [DOI:10.1007/s00701-011-1175-2] [PMID]
64. Els C.H. Prognosis of six-month function after traumatic brain injury.Rehabil Med.2010; 42: 425–436. [DOI:10.2340/16501977-0566] [PMID]
65. V. Jain, S. Tiwari, S. Misra, Tiwari, Nagendra. Predictive Value of Serum Lactate Dehydrogenase in Head Injury. The Internet Journal of Surgery. 2010; 22(2):101-110.
66. Barlow P, Teasdale G. Prediction of outcome and the management of severe head injuries: the attitudes of neurosurgeons. Neurosurg.1986; 19:989-991.
https://doi.org/10.1097/00006123-198612000-00014 [DOI:10.1227/00006123-198612000-00014]
67. Gong D, Hao M, Liu L, Liu C, Dong J, Cui Z, et al. Prognostic relevance of circulating endothelial progenitor cells for severe traumatic brain injury. Brain Inj. Informa Healthcare. 2012;26(3):291–7. Available from: http://dx.doi.org/10.3109/02699052.2011.648710 [DOI:10.3109/02699052.2011.648710]
68. Oliviera D. Plasma von Willebrand Factor Levels Correlate with Clinical Outcome of Severe Traumatic Brain Injury. Journal of neurotrauma.2007; 24:1331–1338. [DOI:10.1089/neu.2006.0159] [PMID]
69. Papa L. Serum levels of ubiquitin C-terminal hydrolase distinguish mild traumatic brain injury from trauma controls and are elevated in mild and moderate traumatic brain injury patients with intracranial lesions and neurosurgical intervention. J Trauma Acute Care Surg.2012; 72(5):1335-44. [DOI:10.1097/TA.0b013e3182491e3d] [PMID] [PMCID]
70. WhaSookSeo, HyunSoo Oh. Comparisons of Acute Physiological Parameters Influencing Outcome in Patients with Traumatic Brain Injury and Hemorrhagic Stroke. Worldviews Evid Based Nurs.6(1):36-43;2009. [DOI:10.1111/j.1741-6787.2008.00139.x] [PMID]
71. Prisco L, Iscra F, Ganau M, Berlot G.Early predictive factors on mortality in head injured patients: a retrospective analysis of 112 traumatic brain injured patients. J Neurosurg Sci. 2012 Jun;56(2):131-6. [PMID]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |