Fri, Apr 19, 2024
Volume 5, Issue 1 (Winter 2019)
Iran J Neurosurg 2019, 5(1): 37-42 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Faghih-Jouybari M, Le Huec J, Kazemi F, Sajadi K, Padeganeh T, Abdollahzade S. Hangman’s Fracture with Concomitant Atlantoaxial Dislocation. Iran J Neurosurg 2019; 5 (1) :37-42
URL: http://irjns.org/article-1-157-en.html
URL: http://irjns.org/article-1-157-en.html
Morteza Faghih-Jouybari 1 

 , Jean-Charles Le Huec2
, Jean-Charles Le Huec2 

 , Foad Kazemi 3
, Foad Kazemi 3 

 , Kiavash Sajadi 1
, Kiavash Sajadi 1 

 , Tahereh Padeganeh4
, Tahereh Padeganeh4 

 , Sina Abdollahzade *
, Sina Abdollahzade * 

 5
5


 , Jean-Charles Le Huec2
, Jean-Charles Le Huec2 

 , Foad Kazemi 3
, Foad Kazemi 3 

 , Kiavash Sajadi 1
, Kiavash Sajadi 1 

 , Tahereh Padeganeh4
, Tahereh Padeganeh4 

 , Sina Abdollahzade *
, Sina Abdollahzade * 

 5
5
1- Department of Neurosurgery, Shariati Hospital, School of medicine, Tehran University of Medical Sciences, Tehran, Iran
2- Orthopedic and Spine Surgery Unit tow, Bordeaux University Hospital, Bordeaux, France
3- Department of Neurosurgery, Rasoul-Akram Hospital, Iran University of Medical Sciences, Tehran, Iran
4- Department of Maxillofacial Surgery, Shariati Hospital, Tehran University of Medical Sciences, Tehran, Iran.
5- Department of Neurosurgery, Shahid Rajaee Teaching Center, Qazvin University of Medical Sciences, Qazvin, Iran , sina21@gmail.com
2- Orthopedic and Spine Surgery Unit tow, Bordeaux University Hospital, Bordeaux, France
3- Department of Neurosurgery, Rasoul-Akram Hospital, Iran University of Medical Sciences, Tehran, Iran
4- Department of Maxillofacial Surgery, Shariati Hospital, Tehran University of Medical Sciences, Tehran, Iran.
5- Department of Neurosurgery, Shahid Rajaee Teaching Center, Qazvin University of Medical Sciences, Qazvin, Iran , sina21@gmail.com
Full Text [PDF 526 kb]
(1776 Downloads)
| Abstract (HTML) (3726 Views)
In two similar cases previous to ours, one was reported to be reduced after 3 weeks of bidirectional cervical traction and another was managed by open reduction and stabilization [15, 16]. We considered this kind of injury too unstable to be treated conservatively because of the rupture in C2, C3 disc, posterior longitudinal ligament, and C1, C2 facet capsules. Skull traction could not reduce dislocation completely because the anterior part of C2 was like a loose fragment. During the anterior approach, discectomy and fixation of the plate turned back the C2 vertebral body both in axial and sagittal planes. The posterior approach and lateral mass screw fixation reduced C1, C2 dislocation and augmented stabilization. Follow-up radiography showed adequate reduction and satisfactory spinal alignment.
4. Conclusion
The combination of atlantoaxial dislocation and Hangman’s fracture is extremely rare. The mechanism of injury is probably hyperextension and rotation. Severe neurological deficit is uncommon, considering C2 spondylolisthesis and the widening of the spinal canal. Reduction of dislocation must be achieved as soon as possible. In our patient, open reduction and anteroposterior fixation resulted in a satisfactory long-term outcome, both clinically and radiologically.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from the patient. All identifying data were removed from the images.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization, draft: Morteza Faghih Jouybari and Sina Abdollahzade; Investigation: Foad Kazemi and Kiavash Sajadi; Writing-original: Morteza Faghih-Jouybari, Tahereh Padeganeh and Sina Abdollahzade; Writing-review & editing, Methodology, resources: All Authors; Supervision, Jean-Charles Le Huec.
Conflict of interest
The authors declared no conflict of interest.
References
Torretti JA, Sengupta DK. Cervical spine trauma. Indian Journal of Orthopaedics. 2007; 41(4):255-67. [DOI:10.4103/0019-5413.36985] [PMID] [PMCID]
Samaha C, Lazennec JY, Laporte C, Saillant G. Hangman’s fracture: The relationship between asymmetry and instability. The Journal of Bone and Joint Surgery British volume. 2000; 82(7):1046-52. [DOI:10.1302/0301-620X.82B7.0821046] [PMID]
Moon MS, Moon JL, Moon YW, Sun DH, Choi WT. Traumatic spondylolisthesis of the axis: 42 cases. Bulletin Hospital for Joint Diseases. 2001; 60(2):61-6. [PMID]
Wang L, Liu C, Zhao QH, Tian JW. Classification and surgical management for the axis fracture complicated with adjacent segment instability. International Journal of Clinical and Experimental Medicine. 2014; 7(3):657-64. [PMID] [PMCID]
Kayser R, Weber U, Heyde CE. [Injuries to the craniocervical junction (German)]. Der Orthopäde. 2006; 35(3):244-69. [DOI:10.1007/s00132-005-0920-8] [PMID]
Cao G, Meng C, Zhang W, Kong X. Operative strategy and clinical outcomes of ROI-C(TM) fusion device in the treatment of Hangman’s fracture. International Journal of Clinical and Experimental Medicine. 2015; 8(10):18665-72. [PMID] [PMCID]
Schneider RC, Livingston KE, Cave AJE, Hamilton G. “Hangman’s Fracture” of the cervical spine. Journal of Neurosurgery. 1965; 22(2):141-54. [DOI:10.3171/jns.1965.22.2.0141] [PMID]
Levine A, Edwards C. The management of traumatic spondylolisthesis of the axis. The Journal of Bone & Joint Surgery. 1985; 67(2):217-26. [DOI:10.2106/00004623-198567020-00007] [PMID]
Yang SY, Boniello AJ, Poorman CE, Chang AL, Wang Sh, Passias PG. A review of the diagnosis and treatment of atlantoaxial dislocations. Global Spine Journal. 2014; 4(3):197-210. [DOI:10.1055/s-0034-1376371] [PMID] [PMCID]
Haralson R, Boyd H. Posterior dislocation of the atlas on the axis without fracture: Report of a case. The Journal of Bone & Joint Surgery. 1969; 51(3):561-6. [DOI:10.2106/00004623-196951030-00016] [PMID]
Wong D, Mack R, Craigmile T. Traumatic atlantoaxial dislocation without fracture of the odontoid. Spine. 1991; 16(5):587-9. [DOI:10.1097/00007632-199105000-00021] [PMID]
Patzakis M, Knopf A, Elfering M, Hoffer M, Harvey J. Posterior dislocation of the atlas on the axis: A case report. The Journal of Bone & Joint Surgery. 1974; 56(6):1260-2. [DOI:10.2106/00004623-197456060-00020] [PMID]
Robertson PA, Swan HAP. Traumatic bilateral rotatory facet dislocation of the atlas on the axis. Spine. 1992; 17(10):1252-4. [DOI:10.1097/00007632-199210000-00022] [PMID]
Wise J, Cheney R, Fischgrund J. Traumatic bilateral rotatory dislocation of the atlanto-axial joints: A case report and review of the literature. Journal of Spinal Disorders. 1997; 10(5):451-3. [DOI:10.1097/00002517-199710000-00017] [PMID]
Han K, Cui SB, Wang L, Wei FX, Liu SY. Traumatic bilateral atlantoaxial rotatory subluxation with hangman fracture in an adult. Neurology India. 2016; 64(4):811-4. [DOI:10.4103/0028-3886.185412] [PMID]
Chaudhary SB, Martinez M, Shah NP, Vives MJ. Traumatic atlantoaxial dislocation with Hangman fracture. The Spine Journal. 2015; 15(4):e15-8. [DOI:10.1016/j.spinee.2014.12.150] [PMID]
Full Text: (1136 Views)
1. Background and Importance
Hangman’s fracture is described as a bilateral fracture traversing the pars interarticularis of C2 [1, 2]. It accounts for 23% of axis fractures and is commonly seen with motor vehicle accidents [3, 4]. The relatively capacious area of the spinal cord at the level of fracture explains the scarcity of neurologic injury in affected individuals. The fracture pattern is usually seen following hyperextension and axial loading as well as in flexion injury cases. Traumatic atlantoaxial rotatory dislocation (AARD) also occurs high in the cervical area but with a different mechanism. It results from extreme rotation and distraction trauma of the cervical spine. It is common in children but represents a rare entity in adults. However, we report a rare case of Hangman’s fracture associated with atlantoaxial rotatory dislocation managed successfully by surgical treatment in adult patient.
2. Case presentation
A 32-year-old woman became a victim of a motor vehicle accident as her car collided with another car. The patient was brought to the trauma center of Shariati Hospital by family members. There were no reported significant past medical or surgical illnesses. She had a blood pressure of 115/80 mmHg and a pulse rate of 105 beats/min. Her Glasgow coma scale (GCS) was 15/15. She had equal and reactive pupils bilaterally. She had severe pain radiating from the occipital region of the head to the posterior neck. There was tenderness at the upper part of her neck in the posterior midline and mild torticollis (left lateral flexion) but no neurological deficit was detected.
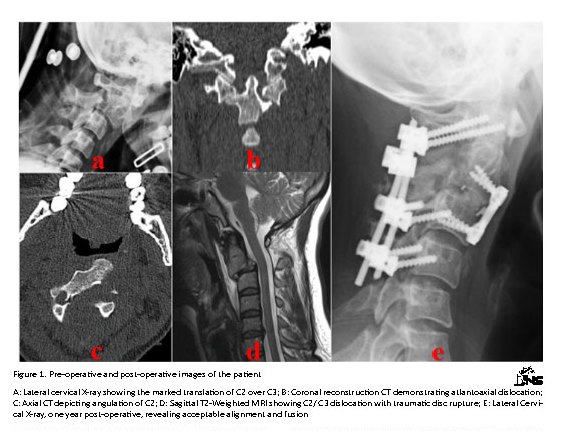
She was placed in a cervical collar and basic spine investigations were done in the form of X-rays and computed tomography (CT) scan. Her cervical spine radiograph (Figure 1a) showed spondylolisthesis of the axis with significant translation and angulation. The CT scan (Figure 1b and 1c) revealed a bilateral atlantoaxial dislocation and a type II Hangman’s fracture involving the vertebral foramina. It seemed that the C2 vertebral body was disconnected from posterior elements and rotated around the axis of the odontoid process. Magnetic resonance imaging (MRI) (Figure 1d) revealed disruption in the C2, C3 disc and anterior and posterior longitudinal ligaments but the transverse ligament remained intact and there was no cord compression.
Immediately after imaging, skeletal traction was gently applied. The traction weight was initially 5 pounds and was gradually increased to 15 pounds under fluoroscopy over one hour. Closed reduction of traumatic C2, C3 spondylolisthesis was partially achieved. Because the fracture was highly unstable and adequate reduction could not be achieved, the decision was made to proceed to surgical intervention.
Under general anesthesia, the patient was positioned supine. A paramedian right cervical oblique incision was made, and the soft tissue was separated deep within the space between the carotid sheath and trachea. The C2, C3 disk was removed and thorough decompression was accomplished. Then a polyether ether ketone (PEEK) cage was inserted into the intervertebral space. An anterior cervical plate was applied to secure the cage and turn back the C2 vertebral body in relation to C1 and C3 (both Hangman’s fracture and AARD were reduced). Then the patient was carefully turned to the prone position with the skull fixed to a head-holder device. Posterior fixation was achieved using C1, C3 and C4 lateral mass screw. We included C4 in posterior arthrodesis since the C3 lateral mass is small and probably not the most efficient as the lower end of instrumentation. At the one-year follow-up, neck pain was almost completely alleviated and a cervical X-ray showed a well-reduced state of C1, C2, C3 (Figure 1E).
3. Discussion
Traumatic spondylolisthesis of the axis is due to fractures of the lamina, articular facets, pedicles, or pars interarticularis and was first described by Bouvier in 1843 [5]. It is the second most frequent fracture of C2 in adults, after odontoid fracture [6]. In 1965, Schneider used the term “Hangman’s fracture” to describe this injury because of the similarities seen in the fractures associated with judicial hangings [7]. Hangman’s fracture rarely leads to spinal cord injury, because the canal widens more than it narrows.
The Levine-Edwards classification system is the most used classification system, and it classifies fractures based on the mechanism of injury [8]. According to this classification, type I injuries are considered stable, whereas type II, IIA, and III injuries are unstable as they usually involve ruptures of the C2, C3 disk and anterior and posterior longitudinal ligament involvement. In our patient, there was type II C2, C3 spondylolisthesis, and the fracture line was through the pedicles and foramen transversarium. The C2, C3 disc and anterior and posterior longitudinal ligament were disrupted, so the anterior part of the C2 vertebra became released and rotated around the axis.
Traumatic atlantoaxial rotatory dislocation is a rare injury in adults and usually occurs in young individuals with ligamentous laxity secondary to Down’s syndrome, Marfan’s syndrome, inflammatory rheumatoid arthritis or Grisel’s syndrome [9-12]. The combination of traumatic spondylolisthesis of the axis and atlantoaxial rotatory dislocation is extremely rare and our case is the third one to have ever been reported in literature. The presence of neurological deficits in patients with atlantoaxial dislocation varies and generally depends on the integrity of the dens and transverse ligaments, and the degree of spinal canal compromise [13, 14]. In our patient, the intact transverse ligament and widening of the spinal canal secondary to spondylolisthesis prevented any neurological deficits.
Hangman’s fracture is described as a bilateral fracture traversing the pars interarticularis of C2 [1, 2]. It accounts for 23% of axis fractures and is commonly seen with motor vehicle accidents [3, 4]. The relatively capacious area of the spinal cord at the level of fracture explains the scarcity of neurologic injury in affected individuals. The fracture pattern is usually seen following hyperextension and axial loading as well as in flexion injury cases. Traumatic atlantoaxial rotatory dislocation (AARD) also occurs high in the cervical area but with a different mechanism. It results from extreme rotation and distraction trauma of the cervical spine. It is common in children but represents a rare entity in adults. However, we report a rare case of Hangman’s fracture associated with atlantoaxial rotatory dislocation managed successfully by surgical treatment in adult patient.
2. Case presentation
A 32-year-old woman became a victim of a motor vehicle accident as her car collided with another car. The patient was brought to the trauma center of Shariati Hospital by family members. There were no reported significant past medical or surgical illnesses. She had a blood pressure of 115/80 mmHg and a pulse rate of 105 beats/min. Her Glasgow coma scale (GCS) was 15/15. She had equal and reactive pupils bilaterally. She had severe pain radiating from the occipital region of the head to the posterior neck. There was tenderness at the upper part of her neck in the posterior midline and mild torticollis (left lateral flexion) but no neurological deficit was detected.
She was placed in a cervical collar and basic spine investigations were done in the form of X-rays and computed tomography (CT) scan. Her cervical spine radiograph (Figure 1a) showed spondylolisthesis of the axis with significant translation and angulation. The CT scan (Figure 1b and 1c) revealed a bilateral atlantoaxial dislocation and a type II Hangman’s fracture involving the vertebral foramina. It seemed that the C2 vertebral body was disconnected from posterior elements and rotated around the axis of the odontoid process. Magnetic resonance imaging (MRI) (Figure 1d) revealed disruption in the C2, C3 disc and anterior and posterior longitudinal ligaments but the transverse ligament remained intact and there was no cord compression.
Immediately after imaging, skeletal traction was gently applied. The traction weight was initially 5 pounds and was gradually increased to 15 pounds under fluoroscopy over one hour. Closed reduction of traumatic C2, C3 spondylolisthesis was partially achieved. Because the fracture was highly unstable and adequate reduction could not be achieved, the decision was made to proceed to surgical intervention.
Under general anesthesia, the patient was positioned supine. A paramedian right cervical oblique incision was made, and the soft tissue was separated deep within the space between the carotid sheath and trachea. The C2, C3 disk was removed and thorough decompression was accomplished. Then a polyether ether ketone (PEEK) cage was inserted into the intervertebral space. An anterior cervical plate was applied to secure the cage and turn back the C2 vertebral body in relation to C1 and C3 (both Hangman’s fracture and AARD were reduced). Then the patient was carefully turned to the prone position with the skull fixed to a head-holder device. Posterior fixation was achieved using C1, C3 and C4 lateral mass screw. We included C4 in posterior arthrodesis since the C3 lateral mass is small and probably not the most efficient as the lower end of instrumentation. At the one-year follow-up, neck pain was almost completely alleviated and a cervical X-ray showed a well-reduced state of C1, C2, C3 (Figure 1E).
3. Discussion
Traumatic spondylolisthesis of the axis is due to fractures of the lamina, articular facets, pedicles, or pars interarticularis and was first described by Bouvier in 1843 [5]. It is the second most frequent fracture of C2 in adults, after odontoid fracture [6]. In 1965, Schneider used the term “Hangman’s fracture” to describe this injury because of the similarities seen in the fractures associated with judicial hangings [7]. Hangman’s fracture rarely leads to spinal cord injury, because the canal widens more than it narrows.
The Levine-Edwards classification system is the most used classification system, and it classifies fractures based on the mechanism of injury [8]. According to this classification, type I injuries are considered stable, whereas type II, IIA, and III injuries are unstable as they usually involve ruptures of the C2, C3 disk and anterior and posterior longitudinal ligament involvement. In our patient, there was type II C2, C3 spondylolisthesis, and the fracture line was through the pedicles and foramen transversarium. The C2, C3 disc and anterior and posterior longitudinal ligament were disrupted, so the anterior part of the C2 vertebra became released and rotated around the axis.
Traumatic atlantoaxial rotatory dislocation is a rare injury in adults and usually occurs in young individuals with ligamentous laxity secondary to Down’s syndrome, Marfan’s syndrome, inflammatory rheumatoid arthritis or Grisel’s syndrome [9-12]. The combination of traumatic spondylolisthesis of the axis and atlantoaxial rotatory dislocation is extremely rare and our case is the third one to have ever been reported in literature. The presence of neurological deficits in patients with atlantoaxial dislocation varies and generally depends on the integrity of the dens and transverse ligaments, and the degree of spinal canal compromise [13, 14]. In our patient, the intact transverse ligament and widening of the spinal canal secondary to spondylolisthesis prevented any neurological deficits.
In two similar cases previous to ours, one was reported to be reduced after 3 weeks of bidirectional cervical traction and another was managed by open reduction and stabilization [15, 16]. We considered this kind of injury too unstable to be treated conservatively because of the rupture in C2, C3 disc, posterior longitudinal ligament, and C1, C2 facet capsules. Skull traction could not reduce dislocation completely because the anterior part of C2 was like a loose fragment. During the anterior approach, discectomy and fixation of the plate turned back the C2 vertebral body both in axial and sagittal planes. The posterior approach and lateral mass screw fixation reduced C1, C2 dislocation and augmented stabilization. Follow-up radiography showed adequate reduction and satisfactory spinal alignment.
4. Conclusion
The combination of atlantoaxial dislocation and Hangman’s fracture is extremely rare. The mechanism of injury is probably hyperextension and rotation. Severe neurological deficit is uncommon, considering C2 spondylolisthesis and the widening of the spinal canal. Reduction of dislocation must be achieved as soon as possible. In our patient, open reduction and anteroposterior fixation resulted in a satisfactory long-term outcome, both clinically and radiologically.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from the patient. All identifying data were removed from the images.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization, draft: Morteza Faghih Jouybari and Sina Abdollahzade; Investigation: Foad Kazemi and Kiavash Sajadi; Writing-original: Morteza Faghih-Jouybari, Tahereh Padeganeh and Sina Abdollahzade; Writing-review & editing, Methodology, resources: All Authors; Supervision, Jean-Charles Le Huec.
Conflict of interest
The authors declared no conflict of interest.
References
Torretti JA, Sengupta DK. Cervical spine trauma. Indian Journal of Orthopaedics. 2007; 41(4):255-67. [DOI:10.4103/0019-5413.36985] [PMID] [PMCID]
Samaha C, Lazennec JY, Laporte C, Saillant G. Hangman’s fracture: The relationship between asymmetry and instability. The Journal of Bone and Joint Surgery British volume. 2000; 82(7):1046-52. [DOI:10.1302/0301-620X.82B7.0821046] [PMID]
Moon MS, Moon JL, Moon YW, Sun DH, Choi WT. Traumatic spondylolisthesis of the axis: 42 cases. Bulletin Hospital for Joint Diseases. 2001; 60(2):61-6. [PMID]
Wang L, Liu C, Zhao QH, Tian JW. Classification and surgical management for the axis fracture complicated with adjacent segment instability. International Journal of Clinical and Experimental Medicine. 2014; 7(3):657-64. [PMID] [PMCID]
Kayser R, Weber U, Heyde CE. [Injuries to the craniocervical junction (German)]. Der Orthopäde. 2006; 35(3):244-69. [DOI:10.1007/s00132-005-0920-8] [PMID]
Cao G, Meng C, Zhang W, Kong X. Operative strategy and clinical outcomes of ROI-C(TM) fusion device in the treatment of Hangman’s fracture. International Journal of Clinical and Experimental Medicine. 2015; 8(10):18665-72. [PMID] [PMCID]
Schneider RC, Livingston KE, Cave AJE, Hamilton G. “Hangman’s Fracture” of the cervical spine. Journal of Neurosurgery. 1965; 22(2):141-54. [DOI:10.3171/jns.1965.22.2.0141] [PMID]
Levine A, Edwards C. The management of traumatic spondylolisthesis of the axis. The Journal of Bone & Joint Surgery. 1985; 67(2):217-26. [DOI:10.2106/00004623-198567020-00007] [PMID]
Yang SY, Boniello AJ, Poorman CE, Chang AL, Wang Sh, Passias PG. A review of the diagnosis and treatment of atlantoaxial dislocations. Global Spine Journal. 2014; 4(3):197-210. [DOI:10.1055/s-0034-1376371] [PMID] [PMCID]
Haralson R, Boyd H. Posterior dislocation of the atlas on the axis without fracture: Report of a case. The Journal of Bone & Joint Surgery. 1969; 51(3):561-6. [DOI:10.2106/00004623-196951030-00016] [PMID]
Wong D, Mack R, Craigmile T. Traumatic atlantoaxial dislocation without fracture of the odontoid. Spine. 1991; 16(5):587-9. [DOI:10.1097/00007632-199105000-00021] [PMID]
Patzakis M, Knopf A, Elfering M, Hoffer M, Harvey J. Posterior dislocation of the atlas on the axis: A case report. The Journal of Bone & Joint Surgery. 1974; 56(6):1260-2. [DOI:10.2106/00004623-197456060-00020] [PMID]
Robertson PA, Swan HAP. Traumatic bilateral rotatory facet dislocation of the atlas on the axis. Spine. 1992; 17(10):1252-4. [DOI:10.1097/00007632-199210000-00022] [PMID]
Wise J, Cheney R, Fischgrund J. Traumatic bilateral rotatory dislocation of the atlanto-axial joints: A case report and review of the literature. Journal of Spinal Disorders. 1997; 10(5):451-3. [DOI:10.1097/00002517-199710000-00017] [PMID]
Han K, Cui SB, Wang L, Wei FX, Liu SY. Traumatic bilateral atlantoaxial rotatory subluxation with hangman fracture in an adult. Neurology India. 2016; 64(4):811-4. [DOI:10.4103/0028-3886.185412] [PMID]
Chaudhary SB, Martinez M, Shah NP, Vives MJ. Traumatic atlantoaxial dislocation with Hangman fracture. The Spine Journal. 2015; 15(4):e15-8. [DOI:10.1016/j.spinee.2014.12.150] [PMID]
Type of Study: Case report |
Subject:
Spine
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |