Fri, Apr 19, 2024
Volume 2, Issue 2 (9-2016)
Iran J Neurosurg 2016, 2(2): 20-23 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Capozza M, Pansini G, Buccoliero A M, Barbagli G, Ashraf-Noubari B, Mariotti F et al . Foreign Body Reaction Mimicking Intracranial Abscess following the Use of Oxidized Regenerated Cellulose (SurgicelTM): Case Report and Literature Review. Iran J Neurosurg 2016; 2 (2) :20-23
URL: http://irjns.org/article-1-40-en.html
URL: http://irjns.org/article-1-40-en.html
Matteo Capozza * 
 1, Gastone Pansini2
1, Gastone Pansini2 
 , Anna Maria Buccoliero3
, Anna Maria Buccoliero3 
 , Giovanni Barbagli1
, Giovanni Barbagli1 
 , Bahman Ashraf-Noubari1
, Bahman Ashraf-Noubari1 
 , Furio Mariotti2
, Furio Mariotti2 
 , Franco Ammannati2
, Franco Ammannati2 


 1, Gastone Pansini2
1, Gastone Pansini2 
 , Anna Maria Buccoliero3
, Anna Maria Buccoliero3 
 , Giovanni Barbagli1
, Giovanni Barbagli1 
 , Bahman Ashraf-Noubari1
, Bahman Ashraf-Noubari1 
 , Furio Mariotti2
, Furio Mariotti2 
 , Franco Ammannati2
, Franco Ammannati2 

1- MD, Department of Neurosurgery, University of Florence, Italy
2- MD, Neurosurgical Unit, Careggi General Hospital, Florence, Italy
3- MD, Unit of Pathology, Meyer Hospital, Florence, Italy
2- MD, Neurosurgical Unit, Careggi General Hospital, Florence, Italy
3- MD, Unit of Pathology, Meyer Hospital, Florence, Italy
Keywords: Foreign Body Reaction, Surgicel™, Oxidized Regenerated Cellulose, Topical Haemostatic Agents, Intracranial Abscess, Brain Surgery
Full Text [PDF 719 kb]
(2890 Downloads)
| Abstract (HTML) (6701 Views)
Full Text: (1822 Views)
Background & Importance
Uncontrolled bleeding has to be absolutely avoided in brain surgery. For this purpose, neurosurgeons use topical haemostatic agents in their practice (3). Because of the delicate nature of intracranial tissues, commonly bioabsorbable materials such as oxidized regenerated cellulose (SurgicelTM; Ethicon, Inc., Somerville, NJ) have been used and left in the surgical field in order to prevent re-bleeding after closure (10). This practice may induce a rare granulomatous inflammatory reaction close to and onto the surgical site (6). This may lead to symptoms and/or neuroradiological findings such as mass lesions virtually indistinguishable from recurrent tumor or postoperative intracranial abscesses at CT-MRI scans (7).
The occurrence of granulomatous inflammatory foreign body reaction due to the use of oxidized regenerated cellulose (SurgicelTM; Ethicon, Inc., Somerville, NJ) is extremely rare: only few cases were published (2,5-9). We report a case of 54 year-old man previously operated for intracranial meningioma who underwent surgery again for a granulomatous foreign body reaction mimicking postoperative brain abscess.
Case Presentation
History
A 54-year-old man underwent surgery at our institution for sudden onset of weakness of the left arm and gait difficulties. MRI scans showed right frontoparietal mass tumor. The histopathological diagnosis was atypical meningioma (grade II, WHO 2007; MIB-1=10%). During the operation, as usual, the surgeon took the SurgicelTM in order to prevent the bleeding from the surgical field. Clinical conditions of the patient improved and he was discharged a few days later. After one month, the patient came back to our department for the recurrence of left side rapidly worsening arm weakness.
Physical Examination
Patient was conscious, alert and cooperative (GCS=15). Pupils were normal and no cranial nerve palsies were noted. We observed left hemiparesis with marked weakness of the arm with positivity to the Mingazzini’s test. Deep tendon reflexes were very weak on the left side so walking became more difficult and unstable. Immunology and haematological profile reported normal range values and temperature was average.
Preoperative Neuroimaging
We performed enhancing CT and MRI scans with the evidence of a large hypodense area with inhomogeneous enhancement and cystic areas with surrounding edema such as cystic-necrotic lesion into previous surgical field (Figures 1&2). The patient also underwent total body scintigraphy (WBC PAO 99mTc): this study reported data suggestive for septic inflammation. Based on these results and the short time run after previous surgery, the suspected diagnosis was postoperative brain abscess. Then, the patient experienced surgery again.
Surgery
The patient was placed in supine position with the head tilted about 30 degrees on the left side. Then, curve shape skin incision on the old wound was performed, cranial operculum was removed and the dura layer opened observing a large extracerebral mass with irregular borders and malignant appearance. With the aid of intraoperative microscope, the lesion was identified. On
Uncontrolled bleeding has to be absolutely avoided in brain surgery. For this purpose, neurosurgeons use topical haemostatic agents in their practice (3). Because of the delicate nature of intracranial tissues, commonly bioabsorbable materials such as oxidized regenerated cellulose (SurgicelTM; Ethicon, Inc., Somerville, NJ) have been used and left in the surgical field in order to prevent re-bleeding after closure (10). This practice may induce a rare granulomatous inflammatory reaction close to and onto the surgical site (6). This may lead to symptoms and/or neuroradiological findings such as mass lesions virtually indistinguishable from recurrent tumor or postoperative intracranial abscesses at CT-MRI scans (7).
The occurrence of granulomatous inflammatory foreign body reaction due to the use of oxidized regenerated cellulose (SurgicelTM; Ethicon, Inc., Somerville, NJ) is extremely rare: only few cases were published (2,5-9). We report a case of 54 year-old man previously operated for intracranial meningioma who underwent surgery again for a granulomatous foreign body reaction mimicking postoperative brain abscess.
Case Presentation
History
A 54-year-old man underwent surgery at our institution for sudden onset of weakness of the left arm and gait difficulties. MRI scans showed right frontoparietal mass tumor. The histopathological diagnosis was atypical meningioma (grade II, WHO 2007; MIB-1=10%). During the operation, as usual, the surgeon took the SurgicelTM in order to prevent the bleeding from the surgical field. Clinical conditions of the patient improved and he was discharged a few days later. After one month, the patient came back to our department for the recurrence of left side rapidly worsening arm weakness.
Physical Examination
Patient was conscious, alert and cooperative (GCS=15). Pupils were normal and no cranial nerve palsies were noted. We observed left hemiparesis with marked weakness of the arm with positivity to the Mingazzini’s test. Deep tendon reflexes were very weak on the left side so walking became more difficult and unstable. Immunology and haematological profile reported normal range values and temperature was average.
Preoperative Neuroimaging
We performed enhancing CT and MRI scans with the evidence of a large hypodense area with inhomogeneous enhancement and cystic areas with surrounding edema such as cystic-necrotic lesion into previous surgical field (Figures 1&2). The patient also underwent total body scintigraphy (WBC PAO 99mTc): this study reported data suggestive for septic inflammation. Based on these results and the short time run after previous surgery, the suspected diagnosis was postoperative brain abscess. Then, the patient experienced surgery again.
Surgery
The patient was placed in supine position with the head tilted about 30 degrees on the left side. Then, curve shape skin incision on the old wound was performed, cranial operculum was removed and the dura layer opened observing a large extracerebral mass with irregular borders and malignant appearance. With the aid of intraoperative microscope, the lesion was identified. On
intraoperative ultrasonographic guide, cystic areas were repeatedly punctured with Cushing’s needle: we did not notice any leakage of liquid material. Then, the lesion was carefully isolated from surrounding brain tissue and removed with en-bloc technique, preserving nervous structures. Specimen appeared stiff, hard and parenchymatous. Hemostasis was appropriate and obtained without using SurgicelTM in order to prevent postoperative hemorrhage.
Post-operative Course
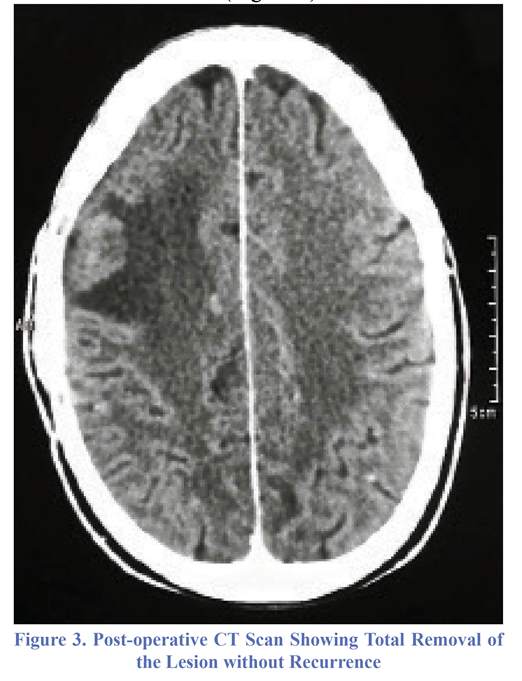
Following surgery, the patient experienced fast relief and his neurologic status started improving gradually. At the 2 months follow-up, he was completely asymptomatic. Serial postoperative CT scans showed total removal of the lesion without recurrence (Figure 3).
Post-operative Course
Following surgery, the patient experienced fast relief and his neurologic status started improving gradually. At the 2 months follow-up, he was completely asymptomatic. Serial postoperative CT scans showed total removal of the lesion without recurrence (Figure 3).
Pathologic Findings
Histopathological findings revealed foreign body granulomas but did not show any evidence of recurrent meningioma. In detail, the microscopic examination showed a rich inflammatory infiltrate represented by multinucleated giant cells associated with residues of surgicel, foam cells, lymphocytes and polymorphonucleate. Moreover, micro-hemorrhagic phenomena, occasional hemosiderin deposits and calcifications were also present (Figure 4).
Discussion
Literature Review and Analysis of Patients
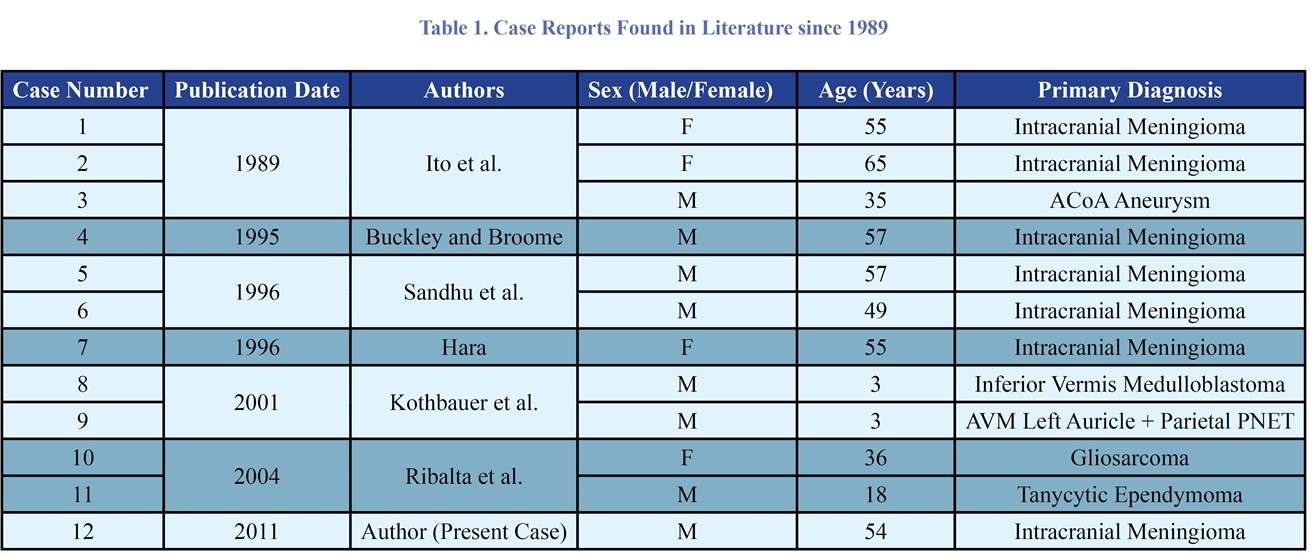
From a comprehensive review of the literature, we found only 11 cases of foreign body reaction related to Surgicel™ as haemostatic agent following neurosurgical procedures (Table 1). On the table mentioned above, are summed a worldwide literature review of intracranial foreign body reaction mimicking recurrent tumor or post-operative abscess due to previous use of oxidized regenerated cellulose (Surgicel™). We reviewed literature since 1989 and excluded all cases of foreign body reaction after surgery where other local haemostatic agents were used. Thus, our inclusion criteria encompassed only patients where local haemostasis of the surgical field had been obtained by use of oxidized regenerated cellulose left in situ. Case reports where surgical hemostasis were obtained by use of local agents such as Gelfoam, cotton, acrylate monomer, rayon, Avitene and other materials were excluded from our literature review. We could observe that the occurrence of a granulomatous reaction after using oxidized regenerated cellulose usually required to achieve adequate hemostasis in brain surgery is very rare. The first three cases of foreign body reaction after using oxidized regenerated cellulose were published back in 1989 (6). Since then, only 12 cases (including patient reported in this work) were found. The review considered 8 males (66.66%) and 4 females (33.33%) with an age range from 3 to 65 years old, and mean age of 40.58. Among all, we considered 2 three-year-old children (16.66%). Patients included in this review underwent surgery first time for intracranial meningioma removal in 7 cases (58.33%) (2,5,6,9), intracranial aneurysm clipping in 1 case (8.33%) (6), inferior vermis medulloblastoma in 1 case (8.33%) (7), AVM+parietal PNET in 1 case (8.33%) (7), gliosarcoma in 1 case (8.33%) and tanycityc ependymoma in the other 1 case (8.33%) (8).
Histopathological findings revealed foreign body granulomas but did not show any evidence of recurrent meningioma. In detail, the microscopic examination showed a rich inflammatory infiltrate represented by multinucleated giant cells associated with residues of surgicel, foam cells, lymphocytes and polymorphonucleate. Moreover, micro-hemorrhagic phenomena, occasional hemosiderin deposits and calcifications were also present (Figure 4).
Discussion
Literature Review and Analysis of Patients
From a comprehensive review of the literature, we found only 11 cases of foreign body reaction related to Surgicel™ as haemostatic agent following neurosurgical procedures (Table 1). On the table mentioned above, are summed a worldwide literature review of intracranial foreign body reaction mimicking recurrent tumor or post-operative abscess due to previous use of oxidized regenerated cellulose (Surgicel™). We reviewed literature since 1989 and excluded all cases of foreign body reaction after surgery where other local haemostatic agents were used. Thus, our inclusion criteria encompassed only patients where local haemostasis of the surgical field had been obtained by use of oxidized regenerated cellulose left in situ. Case reports where surgical hemostasis were obtained by use of local agents such as Gelfoam, cotton, acrylate monomer, rayon, Avitene and other materials were excluded from our literature review. We could observe that the occurrence of a granulomatous reaction after using oxidized regenerated cellulose usually required to achieve adequate hemostasis in brain surgery is very rare. The first three cases of foreign body reaction after using oxidized regenerated cellulose were published back in 1989 (6). Since then, only 12 cases (including patient reported in this work) were found. The review considered 8 males (66.66%) and 4 females (33.33%) with an age range from 3 to 65 years old, and mean age of 40.58. Among all, we considered 2 three-year-old children (16.66%). Patients included in this review underwent surgery first time for intracranial meningioma removal in 7 cases (58.33%) (2,5,6,9), intracranial aneurysm clipping in 1 case (8.33%) (6), inferior vermis medulloblastoma in 1 case (8.33%) (7), AVM+parietal PNET in 1 case (8.33%) (7), gliosarcoma in 1 case (8.33%) and tanycityc ependymoma in the other 1 case (8.33%) (8).
Surgical Considerations
Adequate hemostasis is an important and indispensable element of cranial surgery. For this purpose, Surgicel™ and other similar materials are currently available on the market. Bjorenson et al. and Spiller et al. focused on the effect of absorbable topical haemostatic agents on the relaxation of time blood on in vitro study (1,10), emphasizing that even if Surgicel™ is the most widely used in neurosurgery, it can develop local inflammation presumably due to its acidity (1,2,4). Furthermore, oxidized regenerated cellulose, affecting the 1/T1 of blood, is likely to alter post-operative MR images, causing misinterpretations. This aspect, in fact, was evaluated by Young et al. showing how oxidized regenerated cellulose could mimic on postoperative CT scans of an abscess (11). Ereth et al. evaluated the comparative safety and efficacy of Arista, Surgicel, Floseal and Avitene with positive and negative controls in a rat neurosurgical model (3). This study found that different hemostatic materials were similar in their effects in order to consider safety and efficacy, but pointed out differences comparing the inflammation observed histologically. In fact, while Avitene and Floseal showed a propensity to form granulomas, no evidence of granuloma formation or foreign body reaction associated with Arista and Surgicel exists. Nowadays, as a bioabsorbable material, Surgicel™ is the most widely used hemostatic agent in neurosurgery. Indeed, proper availment of this material should be provided only in case of bleeding, whereas its removal can cause re-bleeding anyway. For this reason, Surgicel™ in daily practice is commonly left in place, especially after the removal of bulky lesions such as intracranial meningiomas, which can cause hemorrhagic infarction of surrounding tissues. Nevertheless, oxidized regenerated cellulose is used in all craniotomies at our institution and intentionally left in place in most cases to prevent the potentially disastrous consequences of postoperative intracranial hemorrhage. This is first and unique case we have reported on such an inflammatory reaction so far.
Conclusion
The use of oxidized regenerated cellulose (Surgicel™) as bioabsorbable topical hemostatic agent in intracranial surgery should still continue to be considered absolutely safe and effectiveness. The potential risk of postoperative intracranial hemorrhages especially after large tumor masses removal such as meningiomas leads the surgeon to left in place this hemostatic material with its progressive resorption and regular postoperative course. Although rare, foreign body granuloma should be included in the differential diagnosis with abscess or tumor recurrence,
Adequate hemostasis is an important and indispensable element of cranial surgery. For this purpose, Surgicel™ and other similar materials are currently available on the market. Bjorenson et al. and Spiller et al. focused on the effect of absorbable topical haemostatic agents on the relaxation of time blood on in vitro study (1,10), emphasizing that even if Surgicel™ is the most widely used in neurosurgery, it can develop local inflammation presumably due to its acidity (1,2,4). Furthermore, oxidized regenerated cellulose, affecting the 1/T1 of blood, is likely to alter post-operative MR images, causing misinterpretations. This aspect, in fact, was evaluated by Young et al. showing how oxidized regenerated cellulose could mimic on postoperative CT scans of an abscess (11). Ereth et al. evaluated the comparative safety and efficacy of Arista, Surgicel, Floseal and Avitene with positive and negative controls in a rat neurosurgical model (3). This study found that different hemostatic materials were similar in their effects in order to consider safety and efficacy, but pointed out differences comparing the inflammation observed histologically. In fact, while Avitene and Floseal showed a propensity to form granulomas, no evidence of granuloma formation or foreign body reaction associated with Arista and Surgicel exists. Nowadays, as a bioabsorbable material, Surgicel™ is the most widely used hemostatic agent in neurosurgery. Indeed, proper availment of this material should be provided only in case of bleeding, whereas its removal can cause re-bleeding anyway. For this reason, Surgicel™ in daily practice is commonly left in place, especially after the removal of bulky lesions such as intracranial meningiomas, which can cause hemorrhagic infarction of surrounding tissues. Nevertheless, oxidized regenerated cellulose is used in all craniotomies at our institution and intentionally left in place in most cases to prevent the potentially disastrous consequences of postoperative intracranial hemorrhage. This is first and unique case we have reported on such an inflammatory reaction so far.
Conclusion
The use of oxidized regenerated cellulose (Surgicel™) as bioabsorbable topical hemostatic agent in intracranial surgery should still continue to be considered absolutely safe and effectiveness. The potential risk of postoperative intracranial hemorrhages especially after large tumor masses removal such as meningiomas leads the surgeon to left in place this hemostatic material with its progressive resorption and regular postoperative course. Although rare, foreign body granuloma should be included in the differential diagnosis with abscess or tumor recurrence,
especially when it had been discovered at short-term follow up. Even if the pathophysiological mechanism of this occurrence is not yet fully understood, surgeons should be aware to avoid misinterpretations in case of suspected postoperative abscess or tumor recurrence.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflicts of Interest
None.
Authors' Contribution
All authors of this study equally helped for realization and revision of it.
References
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflicts of Interest
None.
Authors' Contribution
All authors of this study equally helped for realization and revision of it.
References
- Bjorenson JE, Grove HF, List MG Sr, et al. Effects of hemostatic agents on the pH of body fluids. Journal of Endodontists. 1986;12(7):289-92.
- Buckley SC, Broome JC. A foreign body reaction to Surgicel (R) mimicking an abscess or tumor recurrence. British Journal of Neurosurgery. 1995;9(4):561-3.
- Chater-Cure G, Fonnegra-Caballero A, Baldión-Elorza AM, Jimenez-Hakim E. Gossypiboma in neurosurgery. Case report and literature review. Neurocirugia (Asturias, Spain). 2009;20(1):44-8.
- Ereth MH, Schaff M, Ericson EF, et al. Comparative safety and efficacy of topical hemostatic agents in a rat neurosurgical model. Neurosurgery. 2008;63(4 Suppl 2):369-72.
- Feldman RP, Marcovici A, Suarez M, Goodrich JT. Foreign body granuloma mimicking intracranial meningioma: case report and review of the literature. Neurosurgery. 1999;44(4):855-8.
- Hara N. Intracranial foreign-body granuloma caused by oxidized cellulose. Acta Neurochir (Wien) 1996;138(12):1468-9.
- Ito H, Onishi H, Shoin K, et al. Granuloma caused by oxidized cellulose following craniotomy. Acta Neurochir (Wien). 1989;100(1-2):70-3.
- Kothbauer KF, Jallo GI, Siffert J, et al. Foreign body reaction to hemostatic materials mimicking recurrent brain tumor. Report of three cases. Journal of Neurosurgery. 2001;95(3):503-6.
- Ribalta T, McCutcheon IE, Neto AG, et al. Textiloma (gossypiboma) mimicking recurrent intracranial tumor. Archive of Pathology Laboratory Medicine. 2004;128(7):749-58.
- Sandhu GS, Elexpuru-Camiruaga JA, Buckley S. Oxidized cellulose (Surgicel) granulomata mimicking tumor recurrence. British Journal of Neurosurgery. 1996;10(6):617-9.
- Spiller M, Tenner MS, Couldwell WT. Effect of absorbable topical hemostatic agents on the relaxation time of blood: an in vitro study with implications for postoperative magnetic resonance imaging. Journal of Neurosurgery. 2001;95(4):687-93.
- Young ST, Paulson EK, McCann RL, Baker ME. Appearance of oxidized cellulose (Surgicel) on postoperative CT scans: similarity to postoperative abscess. AJR. American Journal of Roentgenology. 1993;160(2):275-7.
Type of Study: Case report |
Subject:
Gamma Knife Radiosurgery
References
1. Bjorenson JE, Grove HF, List MG Sr, et al. Effects of hemostatic agents on the pH of body fluids. Journal of Endodontists. 1986;12(7):289-92. [DOI:10.1016/S0099-2399(86)80110-8]
2. Buckley SC, Broome JC. A foreign body reaction to Surgicel (R) mimicking an abscess or tumor recurrence. British Journal of Neurosurgery. 1995;9(4):561-3. [DOI:10.1080/02688699550041241]
3. Chater-Cure G, Fonnegra-Caballero A, Baldión-Elorza AM, Jimenez-Hakim E. Gossypiboma in neurosurgery. Case report and literature review. Neurocirugia (Asturias, Spain). 2009;20(1):44-8.
https://doi.org/10.4321/S1130-14732009000100006 [DOI:10.1016/S1130-1473(09)70193-9]
4. Ereth MH, Schaff M, Ericson EF, et al. Comparative safety and efficacy of topical hemostatic agents in a rat neurosurgical model. Neurosurgery. 2008;63(4 Suppl 2):369-72. [PMID]
5. Feldman RP, Marcovici A, Suarez M, Goodrich JT. Foreign body granuloma mimicking intracranial meningioma: case report and review of the literature. Neurosurgery. 1999;44(4):855-8. [DOI:10.1097/00006123-199904000-00091] [PMID]
6. Hara N. Intracranial foreign-body granuloma caused by oxidized cellulose. Acta Neurochir (Wien) 1996;138(12):1468-9. [DOI:10.1007/BF01411128]
7. Ito H, Onishi H, Shoin K, et al. Granuloma caused by oxidized cellulose following craniotomy. Acta Neurochir (Wien). 1989;100(1-2):70-3. [DOI:10.1007/BF01405278]
8. Kothbauer KF, Jallo GI, Siffert J, et al. Foreign body reaction to hemostatic materials mimicking recurrent brain tumor. Report of three cases. Journal of Neurosurgery. 2001;95(3):503-6. [DOI:10.3171/jns.2001.95.3.0503] [PMID]
9. Ribalta T, McCutcheon IE, Neto AG, et al. Textiloma (gossypiboma) mimicking recurrent intracranial tumor. Archive of Pathology Laboratory Medicine. 2004;128(7):749-58. [PMID]
10. Sandhu GS, Elexpuru-Camiruaga JA, Buckley S. Oxidized cellulose (Surgicel) granulomata mimicking tumor recurrence. British Journal of Neurosurgery. 1996;10(6):617-9. [DOI:10.1080/02688699646989] [PMID]
11. Spiller M, Tenner MS, Couldwell WT. Effect of absorbable topical hemostatic agents on the relaxation time of blood: an in vitro study with implications for postoperative magnetic resonance imaging. Journal of Neurosurgery. 2001;95(4):687-93. [DOI:10.3171/jns.2001.95.4.0687] [PMID]
12. Young ST, Paulson EK, McCann RL, Baker ME. Appearance of oxidized cellulose (Surgicel) on postoperative CT scans: similarity to postoperative abscess. AJR. American Journal of Roentgenology. 1993;160(2):275-7. [DOI:10.2214/ajr.160.2.8424333] [PMID]
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |