Sat, Apr 20, 2024
Volume 2, Issue 4 ( 2017)
Iran J Neurosurg 2017, 2(4): 18-21 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Thiam A B, Thioub M, Agbo-Panzo M G E, Sy C E H N, Faye M, Badiane S B. Intradural Lumbar Disc Herniation: Report of Two Cases and Review of the Literature. Iran J Neurosurg 2017; 2 (4) :18-21
URL: http://irjns.org/article-1-79-en.html
URL: http://irjns.org/article-1-79-en.html
Alioune B. Thiam1 
 , Mbaye Thioub1
, Mbaye Thioub1 
 , Martial G. E. Agbo-Panzo *
, Martial G. E. Agbo-Panzo * 
 2, Cheikh E. H. N. Sy1
2, Cheikh E. H. N. Sy1 
 , Mohameth Faye1
, Mohameth Faye1 
 , Seydou B. Badiane1
, Seydou B. Badiane1 


 , Mbaye Thioub1
, Mbaye Thioub1 
 , Martial G. E. Agbo-Panzo *
, Martial G. E. Agbo-Panzo * 
 2, Cheikh E. H. N. Sy1
2, Cheikh E. H. N. Sy1 
 , Mohameth Faye1
, Mohameth Faye1 
 , Seydou B. Badiane1
, Seydou B. Badiane1 

1- Neurosurgery Department, National Teaching Hospital of Fann, BP 5035, Dakar, Senegal
2- Neurosurgery Department, National Teaching Hospital of Fann, BP 5035, Dakar, Senegal , panzojeff@yahoo.fr
2- Neurosurgery Department, National Teaching Hospital of Fann, BP 5035, Dakar, Senegal , panzojeff@yahoo.fr
Full Text [PDF 704 kb]
(2440 Downloads)
| Abstract (HTML) (6982 Views)
Alioune B. Thiam 1, Mbaye Thioub 1, Martial G. E. Agbo-Panzo 1*, Cheikh E. H. N. Sy 1, Mohameth Faye 1, Seydou B. Badiane 1
1 Neurosurgery Department, National Teaching Hospital of Fann, BP 5035, Dakar, Senegal
*Corresponding Author Address: BP 5035 Dakar, TelFax: +221774685008. Email: panzojeff@yahoo.fr
Article Type: Case Series Received: December 11, 2016, Last Revised: January 26, 2017, Accepted: February 3, 2017, Published: March 31, 2017
Abstract
Keywords: Intradural Disc Herniation; Cauda Equina Syndrom; Discectomy; Durotomy
Full Text: (2737 Views)
Intradural Lumbar Disc Herniation: Report of Two Cases and Review of the Literature
Alioune B. Thiam 1, Mbaye Thioub 1, Martial G. E. Agbo-Panzo 1*, Cheikh E. H. N. Sy 1, Mohameth Faye 1, Seydou B. Badiane 1
1 Neurosurgery Department, National Teaching Hospital of Fann, BP 5035, Dakar, Senegal
*Corresponding Author Address: BP 5035 Dakar, TelFax: +221774685008. Email: panzojeff@yahoo.fr
Article Type: Case Series Received: December 11, 2016, Last Revised: January 26, 2017, Accepted: February 3, 2017, Published: March 31, 2017
Abstract
Background and Importance: Intradural lumbar disc herniation is a rare and uncommon presentation of lumbar disc herniation. It signifies a challenge for diagnostic and therapeutic scheme, and is associated with a greater incidence of cauda equina syndrome at presentation.
Case Presentation: We describe two cases of intradural disc herniation who underwent surgery in Senegal review literature, and discuss difficulties in the preoperative diagnosis, surgical technique and functional outcome of our patients.
Conclusion: We conclude that diagnosis of this affection in developing countries is done during surgery, and the functional outcome of patients can be excellent.Keywords: Intradural Disc Herniation; Cauda Equina Syndrom; Discectomy; Durotomy
Please cite this paper as: Thiam AB, Thioub M, Agbo-Panzo MGE, Sy CEHN, Faye M, Badiane SB. Intradural Lumbar Disc Herniation: Report of Two Cases and Review of the Literature. IrJNS. 2017;2(4):18-21
Background & Importance
The intradural disc herniation (IDH) is defined as a nucleus pulposus fragment of the intervertebral disc intruding through the dural sheath [1]. The first case of this pathology was described in 1942 by Dandy [2]. It is a relatively rare complication of the disc herniation, with a rate of about 0.27% to 0.33% of all cases. About 151 cases of IDH have been reported since 1942 with 92% being at the lumbar level, 5% at the dorsal level, and 3% at the cervical level [3]. The preoperative diagnosis remains difficult in spite of great improvement of neuroradiological evaluations with the help of CT scan (CTs) and Magnetic Resonance Imaging (MRI) [4] with final diagnosis usually made during surgery in most cases. In this paper, we report two cases of lumbar IDH who have been operated in Dakar, that were diagnosed intra-operatively. We discuss probable etiology and pathogenesis, diagnostic aspects, and functional outcome of our two patients and review the patient literature, accordingly.
Case Presentation
Both patients included in this study showed their informed consent for publishing their CT-scans, MRIs, intra-operative images, and history.
Case 1
A 25-year-old fisherman presented with a history of low back pain for two years. The beginning of the illness was marked by bilateral S1 hyperalgesia resistant to the common pain killers. Two months before his admission to our center, the pain was complicated by sense of weakness and tingling in bilateral S1 distribution with walking distance limited to 100 meters due to claudication. On admission, the patient was not able to walk but could stand up. The neurological examination showed a lumbar kyphosis, and a finger-to-toe distance of 30 cm. There was paravertebral muscles spasm from L2 to S1 level, and the tapping of the spinous apophysis of vertebra was painful; Lasègue’s sign was positive at 30° bilaterally with a motor force of 2/5 in S1 distribution. The patient had bowel and urinary retention and saddle's hypoesthesia. The lumbar axial CTs and sagittal reconstruction showed a voluminous L4-L5 disc herniation occupying about 70% of the vertebral canal and the patient was selected for surgery. After a complete L4 and partial L5 laminectomy, we noticed a reddish, thinned, very tense and indurated dura mater which was impossible to be mobilized in the vertebral canal. After a midline posterior durotomy, intradural exploration was performed under surgical microscope. A voluminous intradural disc herniation was noticed covered by fibrosis which had compressed rootlets posteriorly and medially. The disc material was removed and the dura mater tightly closed. Just after surgery, we noticed a clinic improvement with disappearance of sciatalgia, sphincter disturbances, and motor strength improvement to 4/5 in bilateral S1 distributions. However, pre-operative saddle’s hypoesthesia did not change. The patient was discharged on day 9 after surgery, and started a motor and urology rehabilitation. One month after surgery, the patient returned with recurrence of the same signs and symptoms but exacerbated with a urinary incontinence. The lumbar spine MRI with contrast enhancement suggested a remnant of L4-L5 disc herniation anterior to the dural sac occupying more than 50% of the vertebral canal with peripheral enhancement (Figure 1). In second surgery, disc herniation was found and removed lateral to the dural sheath with complete decompression of the vertebral canal. The patient was discharged on day 6 of the second surgery. Bilateral sciatalgia motor, and sensory deficits completely recovered. The patient was able to walk without aid by a month. Although the urinary incontinence disappeared after four months, the saddle hypoesthesia has persisted 6 months after surgery.
Background & Importance
The intradural disc herniation (IDH) is defined as a nucleus pulposus fragment of the intervertebral disc intruding through the dural sheath [1]. The first case of this pathology was described in 1942 by Dandy [2]. It is a relatively rare complication of the disc herniation, with a rate of about 0.27% to 0.33% of all cases. About 151 cases of IDH have been reported since 1942 with 92% being at the lumbar level, 5% at the dorsal level, and 3% at the cervical level [3]. The preoperative diagnosis remains difficult in spite of great improvement of neuroradiological evaluations with the help of CT scan (CTs) and Magnetic Resonance Imaging (MRI) [4] with final diagnosis usually made during surgery in most cases. In this paper, we report two cases of lumbar IDH who have been operated in Dakar, that were diagnosed intra-operatively. We discuss probable etiology and pathogenesis, diagnostic aspects, and functional outcome of our two patients and review the patient literature, accordingly.
Case Presentation
Both patients included in this study showed their informed consent for publishing their CT-scans, MRIs, intra-operative images, and history.
Case 1
A 25-year-old fisherman presented with a history of low back pain for two years. The beginning of the illness was marked by bilateral S1 hyperalgesia resistant to the common pain killers. Two months before his admission to our center, the pain was complicated by sense of weakness and tingling in bilateral S1 distribution with walking distance limited to 100 meters due to claudication. On admission, the patient was not able to walk but could stand up. The neurological examination showed a lumbar kyphosis, and a finger-to-toe distance of 30 cm. There was paravertebral muscles spasm from L2 to S1 level, and the tapping of the spinous apophysis of vertebra was painful; Lasègue’s sign was positive at 30° bilaterally with a motor force of 2/5 in S1 distribution. The patient had bowel and urinary retention and saddle's hypoesthesia. The lumbar axial CTs and sagittal reconstruction showed a voluminous L4-L5 disc herniation occupying about 70% of the vertebral canal and the patient was selected for surgery. After a complete L4 and partial L5 laminectomy, we noticed a reddish, thinned, very tense and indurated dura mater which was impossible to be mobilized in the vertebral canal. After a midline posterior durotomy, intradural exploration was performed under surgical microscope. A voluminous intradural disc herniation was noticed covered by fibrosis which had compressed rootlets posteriorly and medially. The disc material was removed and the dura mater tightly closed. Just after surgery, we noticed a clinic improvement with disappearance of sciatalgia, sphincter disturbances, and motor strength improvement to 4/5 in bilateral S1 distributions. However, pre-operative saddle’s hypoesthesia did not change. The patient was discharged on day 9 after surgery, and started a motor and urology rehabilitation. One month after surgery, the patient returned with recurrence of the same signs and symptoms but exacerbated with a urinary incontinence. The lumbar spine MRI with contrast enhancement suggested a remnant of L4-L5 disc herniation anterior to the dural sac occupying more than 50% of the vertebral canal with peripheral enhancement (Figure 1). In second surgery, disc herniation was found and removed lateral to the dural sheath with complete decompression of the vertebral canal. The patient was discharged on day 6 of the second surgery. Bilateral sciatalgia motor, and sensory deficits completely recovered. The patient was able to walk without aid by a month. Although the urinary incontinence disappeared after four months, the saddle hypoesthesia has persisted 6 months after surgery.
Case 2
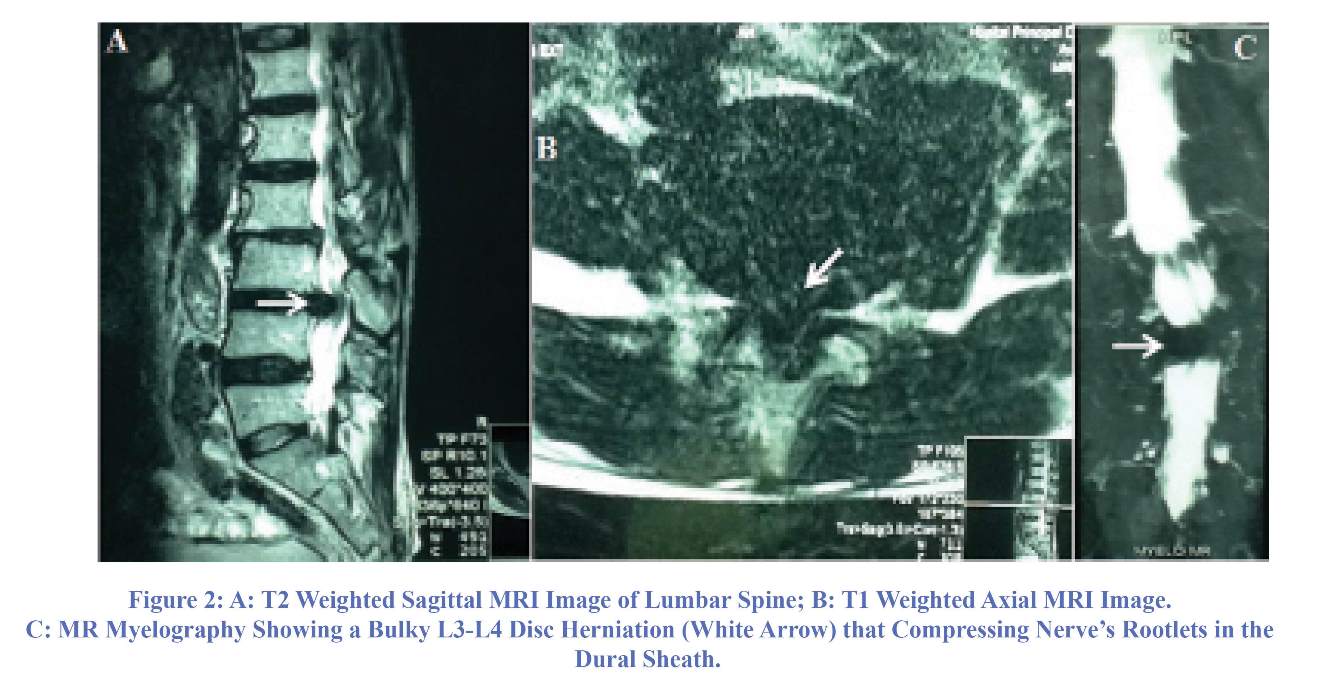
A 63 year-old-male farmer with chronic low back pain for the last 20 years presented with worsening condition during the previous 7 weeks as a new bilateral L5 sciatic pain (more severe on the left) was added to his previous back pain.
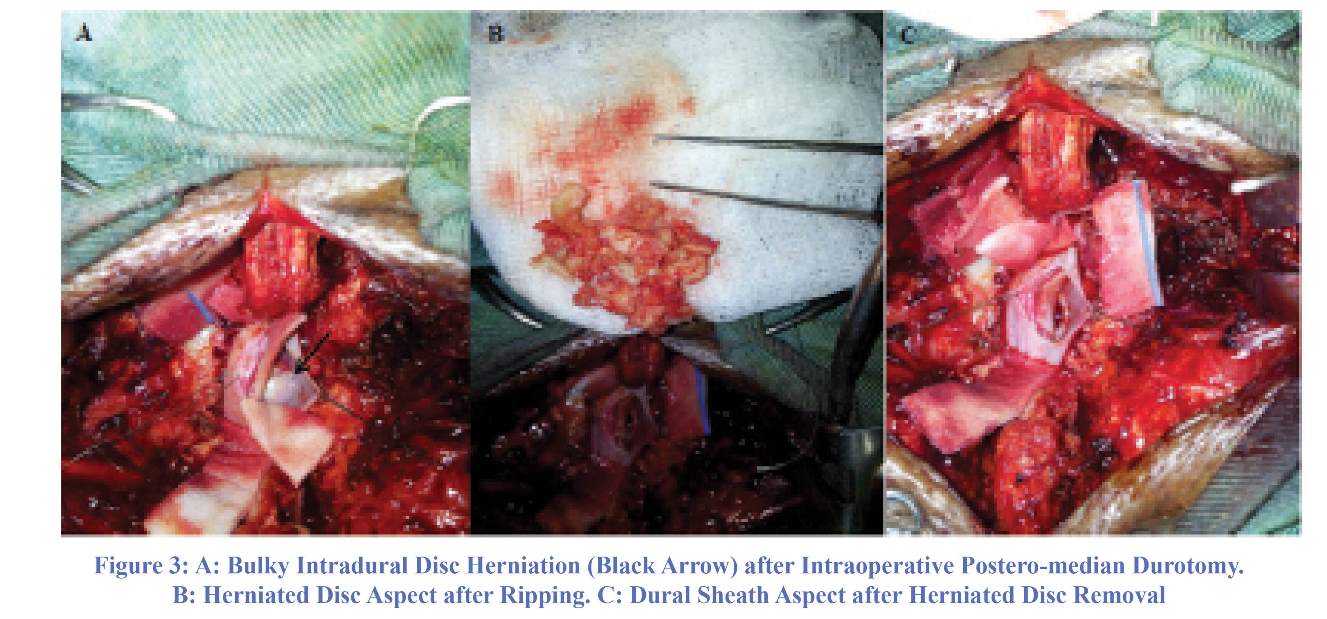
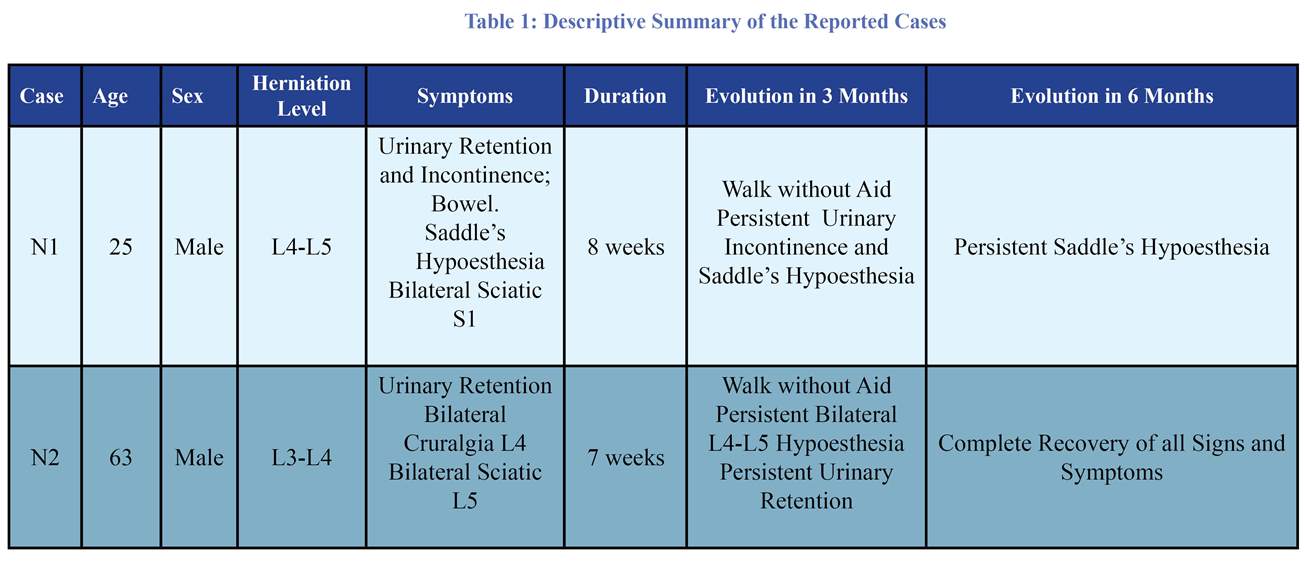
He had developed urinary retention and was using a cane while walking due to tha pain. On the neurologic examination, he showed bilateral L5 and L5 hyposthesia and L4 motor weakness. He showed positive doorbell sign, but not Lasègue. The lumbar spine MRI revealed a voluminous median L3-L4 disc herniation occupying a great portion of the vertebral canal, compressing nerve rootlets in the dural sheath (Figure 2). MR-myelography showed a complete block at L3-L4 level. An emergency surgery was performed to explore the disc herniation. After bilateral complete L4 and partial L3 laminectomy, the dural sheath was noticed to be bulging, tense, indurated, and sticked firmly to the posterior longitudinal ligament. We did a posterior durotomy and the nerve rootlets and cerebrospinal fluid (CSF) sprayed out in the vertebral canal. The nerve rootlets had been compressed by a voluminous herniated disc continuing to the L3-L4 disc space (Figure 3). The intradural disc material was removed under microscopic visualization relieving the compression on nerve rootlets. L3-L4 disc space was curetted, and then, sub-cutaneous fat was laid anterior to the dural sac. The posterior wall was sutured in a water tight fashion. Post-operative period was uneventful and the patient was discharged on day 6. After 3 months of physical rehabilitation, he gained full recovery. of motor deficits. Sensory disturbances and urinary retention completely disappeared after 4 months from surgery (Table 1).
Discussion
Intra-dural herniation is a rare complication of disc herniations [3,5]. Its pathophysiology is not well understood [1,6]. Several predisposing anatomic factors have been mentioned in the literature. These factors predispose dural sheath to tears through which intrusion of discal material happens [7-10].
IDH is usually considered a degenerative disease of old persons [1,7,10]. In our cases, the occurring of IDH in a young patient of 25 years is probably due to his job involving daily pressure on his lumbar spine while carrying, rolling, or throwing fishing nets.
L4-L5 and L3-L4 levels are considered to be the most common sites for lumbar disc herniation [7,11]. The bilateral features of radicular symptoms combined with cauda equine syndrome superimposed on a low back pain in our 2 patients are highly presumptive of IDH as many authors have described [1,6,12,13]. However presence or absence of the cauda-equine syndrom is not directly linked to the bulk of the intradural disc fragment. Only 30% of the patients with IDH suffer from cauda equine syndrome [1].
In our both cases, the diagnosis was during the surgery and pre-operative radiological studies failed to show or confirm such diagnosis. In the lumbar spine MRI on T2 weighted sagittal image, the “Y sign” described by Sasaji et al. as being an interposition of a discal material between the dura and arachnoid, leaving then a space in “Y” between its two layers is not specific [14]. Shoi et al. described “Hawk beak sign” on T2 weighted axial image of lumbar spine MRI [4] which is again, not specific. Hida et al. also reported this “Hawk beak sign” and heavy enhancement of intradural material on the lumbar spine enhanced MRI [15]. According to them, contrast enhanced MRI is useful to narrow differential diagnoses among schwannomas, meningiomas, ependymomas, dermoïd and epidermoïd cysts [16]. However, most authors conclude that this kind of diagnosis is usually done during the surgery. Only eight cases have been diagnosed before surgery, of which two were diagnosed on CT myelography, and the remaining on MRI [16,19-22].
As well described in the literature and also experienced by us, a midline posterior durotomy is advised to reach to these intra-dural pathologies [13]. At the conclusion of surgery, the dural sheath is completely closed and fat tissue laid over to reduce chance of CSF leakage. Both our patients showed significant functional recovery on 6 month follow up after surgery. This functional outcome is directly correlated to the symptoms duration before surgery, the features of the symptoms (i.e. radiculopathy vs. cauda equine syndrome), and the history of previous spine surgery [1]. If cauda equina syndrome exists, emergent surgery should be done within 48 hours from the beginning of the symptoms [23,24]. Although our patients were
A 63 year-old-male farmer with chronic low back pain for the last 20 years presented with worsening condition during the previous 7 weeks as a new bilateral L5 sciatic pain (more severe on the left) was added to his previous back pain.
He had developed urinary retention and was using a cane while walking due to tha pain. On the neurologic examination, he showed bilateral L5 and L5 hyposthesia and L4 motor weakness. He showed positive doorbell sign, but not Lasègue. The lumbar spine MRI revealed a voluminous median L3-L4 disc herniation occupying a great portion of the vertebral canal, compressing nerve rootlets in the dural sheath (Figure 2). MR-myelography showed a complete block at L3-L4 level. An emergency surgery was performed to explore the disc herniation. After bilateral complete L4 and partial L3 laminectomy, the dural sheath was noticed to be bulging, tense, indurated, and sticked firmly to the posterior longitudinal ligament. We did a posterior durotomy and the nerve rootlets and cerebrospinal fluid (CSF) sprayed out in the vertebral canal. The nerve rootlets had been compressed by a voluminous herniated disc continuing to the L3-L4 disc space (Figure 3). The intradural disc material was removed under microscopic visualization relieving the compression on nerve rootlets. L3-L4 disc space was curetted, and then, sub-cutaneous fat was laid anterior to the dural sac. The posterior wall was sutured in a water tight fashion. Post-operative period was uneventful and the patient was discharged on day 6. After 3 months of physical rehabilitation, he gained full recovery. of motor deficits. Sensory disturbances and urinary retention completely disappeared after 4 months from surgery (Table 1).
Discussion
Intra-dural herniation is a rare complication of disc herniations [3,5]. Its pathophysiology is not well understood [1,6]. Several predisposing anatomic factors have been mentioned in the literature. These factors predispose dural sheath to tears through which intrusion of discal material happens [7-10].
IDH is usually considered a degenerative disease of old persons [1,7,10]. In our cases, the occurring of IDH in a young patient of 25 years is probably due to his job involving daily pressure on his lumbar spine while carrying, rolling, or throwing fishing nets.
L4-L5 and L3-L4 levels are considered to be the most common sites for lumbar disc herniation [7,11]. The bilateral features of radicular symptoms combined with cauda equine syndrome superimposed on a low back pain in our 2 patients are highly presumptive of IDH as many authors have described [1,6,12,13]. However presence or absence of the cauda-equine syndrom is not directly linked to the bulk of the intradural disc fragment. Only 30% of the patients with IDH suffer from cauda equine syndrome [1].
In our both cases, the diagnosis was during the surgery and pre-operative radiological studies failed to show or confirm such diagnosis. In the lumbar spine MRI on T2 weighted sagittal image, the “Y sign” described by Sasaji et al. as being an interposition of a discal material between the dura and arachnoid, leaving then a space in “Y” between its two layers is not specific [14]. Shoi et al. described “Hawk beak sign” on T2 weighted axial image of lumbar spine MRI [4] which is again, not specific. Hida et al. also reported this “Hawk beak sign” and heavy enhancement of intradural material on the lumbar spine enhanced MRI [15]. According to them, contrast enhanced MRI is useful to narrow differential diagnoses among schwannomas, meningiomas, ependymomas, dermoïd and epidermoïd cysts [16]. However, most authors conclude that this kind of diagnosis is usually done during the surgery. Only eight cases have been diagnosed before surgery, of which two were diagnosed on CT myelography, and the remaining on MRI [16,19-22].
As well described in the literature and also experienced by us, a midline posterior durotomy is advised to reach to these intra-dural pathologies [13]. At the conclusion of surgery, the dural sheath is completely closed and fat tissue laid over to reduce chance of CSF leakage. Both our patients showed significant functional recovery on 6 month follow up after surgery. This functional outcome is directly correlated to the symptoms duration before surgery, the features of the symptoms (i.e. radiculopathy vs. cauda equine syndrome), and the history of previous spine surgery [1]. If cauda equina syndrome exists, emergent surgery should be done within 48 hours from the beginning of the symptoms [23,24]. Although our patients were
admitted several weeks after symptoms, good recovery of both motor and sensory symptoms were observed. This signifies the importance of urgent operations when dealing with incomplete deficits to facilitate preservation or even recovery of the symptoms.
Conclusion
Quick worsening of a chronic sciatic pain associated with cauda equine syndrome should raise the suspicion of a lumbar IDH. In case of neurological deficit, emergent surgeries are usually warranted to increase the chance of recovery.
Lumbar IDH is a rare disease usually undiagnosed by pre-operative evaluations. Its effective diagnosis before surgery will allow a better surgical planning.
Funding
No fund was received for this publication from any organization.
Conflicts of Interest
The authors declare no conflict of interest.
Conclusion
Quick worsening of a chronic sciatic pain associated with cauda equine syndrome should raise the suspicion of a lumbar IDH. In case of neurological deficit, emergent surgeries are usually warranted to increase the chance of recovery.
Lumbar IDH is a rare disease usually undiagnosed by pre-operative evaluations. Its effective diagnosis before surgery will allow a better surgical planning.
Funding
No fund was received for this publication from any organization.
Conflicts of Interest
The authors declare no conflict of interest.
Authors' Contribution
All authors took part in all parts of writing the manuscript.
References
1. D’Andrea G, Trillo G, Roperto R, Celli P, Orlando ER, Ferrante L. Intradural lumbar disc herniations : the role of MRI in preoperative diagnosis and review of the literature. Neurosurg Rev 2004;27:75-80.
2. Dandy WE. Serious complications of ruptured intervertebral disks. JAMA 1942;119:474-477.
3. Epstein NE, Syrquin MS, Epstein JA, Decker RE. Intradural disc herniation in the cervical, thoracic and lumbar spine: report of three cases and review of the literature. J Spinal Disord 1990;3:396-403.
4. Choi JY, Lee WS, Sung KH. Intradural lumbar disc herniation – Is it predictable preoperatively? A report of two cases. The Spine Journal 2007;7:111-117.
5. Aydin MV, Ozel S, Sem O, Erdogan B, Yildirim T. Intradural disc mimicking: a spinal tumor lesion. Spinal Cord 2004;42:52-54.
6. Yildizhan A, Pasaoglu A, Okten T, Ekinci N, Aycan K, Aral O. Intradural disc herniations: pathogenesis, clinical picture, diagnosis and treatment. Actaneurochir (Wien) 1991;110(3-4):160-165.
7. Kataoka O, Nishibayashi Y, Sho T. Intradural lumbar disc herniation: report of three cases with a review of the literature. Spine 1989;14:529-533.
8. Ozer AF, Ozek MM, Pamir MN, Zirh TA, Erzen C. Intradural rupture of cervical vertebral disc. Spine 1994;19:843-845.
9. Paini KC, Muduli H, Chauder K, Kav VK. Intrathecal disc prolapse associated with lumbar canal stenosis. Neurology (Bombay) 1972;20:64-66.
All authors took part in all parts of writing the manuscript.
References
1. D’Andrea G, Trillo G, Roperto R, Celli P, Orlando ER, Ferrante L. Intradural lumbar disc herniations : the role of MRI in preoperative diagnosis and review of the literature. Neurosurg Rev 2004;27:75-80.
2. Dandy WE. Serious complications of ruptured intervertebral disks. JAMA 1942;119:474-477.
3. Epstein NE, Syrquin MS, Epstein JA, Decker RE. Intradural disc herniation in the cervical, thoracic and lumbar spine: report of three cases and review of the literature. J Spinal Disord 1990;3:396-403.
4. Choi JY, Lee WS, Sung KH. Intradural lumbar disc herniation – Is it predictable preoperatively? A report of two cases. The Spine Journal 2007;7:111-117.
5. Aydin MV, Ozel S, Sem O, Erdogan B, Yildirim T. Intradural disc mimicking: a spinal tumor lesion. Spinal Cord 2004;42:52-54.
6. Yildizhan A, Pasaoglu A, Okten T, Ekinci N, Aycan K, Aral O. Intradural disc herniations: pathogenesis, clinical picture, diagnosis and treatment. Actaneurochir (Wien) 1991;110(3-4):160-165.
7. Kataoka O, Nishibayashi Y, Sho T. Intradural lumbar disc herniation: report of three cases with a review of the literature. Spine 1989;14:529-533.
8. Ozer AF, Ozek MM, Pamir MN, Zirh TA, Erzen C. Intradural rupture of cervical vertebral disc. Spine 1994;19:843-845.
9. Paini KC, Muduli H, Chauder K, Kav VK. Intrathecal disc prolapse associated with lumbar canal stenosis. Neurology (Bombay) 1972;20:64-66.
10. Mercier P, Hayer G, Ben Ali H, Fournier D, Menei P, Mansour BH, Guy G. Hernies discales lombaires intradurales. A propos de six cas et revue de la littérature. Neurochirurgie 1997;43:142-147.
11. Connolly PJ, Rosenbaum AE, Sacks T, Kopacz KJ. Incomplete intradural
lumbar disk herniation. Orthopediscs 1997;20:977-979.
12. Pradeep KS, Sandeep S, Rajesh D, Pankaj B, Sharad G. Dorsal Herniation of Cauda Equina due to sequestrated intradural disc. Asian Spine J. 2012;6(2):145-147.
13. Ducati LG, Silva MV, Brandao MM, Romero FR, Zianini MA. Intradural lumbar disc herniation: report of five cases with literature review. Eur Spine J. 2013;22(Suppl3):S404-S408.
14. Sasaji T, Horaguchi K, Yamada N, Iwai Kazuo. The specific sagittal Magnetic Resonance Imaging on intradural extraarachnoïd lumbar disc herniation. Hindawi Publishing Corporation, case reports in medicine. 2012;Article ID 383451, 3 pages doi:10.1155/2012/383451.
15. Hida K, Jawasaki Y, Abe H, Shimazaki M, Matsuzaki T. Magnetic Resonance Imaging of intradural lumbar disc herniation. J Clin Neurosci 1999;6:345-347.
16. Wasserstrom R, Mamourian AC, Black JF, Lehman RAW. Intradural lumbar disk fragment with ring enhancement on MR. AJNR Am J Neuroradiol 1993;14:401-404.
17. Fang CM, Huang TJ, Chen WJ, Lee ST, Hsu RW. Intradural lumbar disc herniation. A case report. Chang Keng I Hsueh 1994;17:297-300.
18. Kaiser MC, Sandt G, Roilgen A, Capesius P, Poos D, Ohanna F. Intradural disk herniation with CT appearance of gas collection. AJNR Am J Neuroradiol 1985;6:117-118.
19. Isla AI, Roda JM, Bencosme J, Alvarez MP, Blazquez MG. Intradural herniated dorsal disc. Case report and review of the literature. Neurosurgery 1988;22:737-739.
20. Lidov M, Stollman A, Casden A, Som P, Bederson J. MRI of lumbar intradural disc herniation. Clin Imaging 1994;18:173-178.
21. Snow RD, Williams JP, Weber ED, Richardson PH. Enhancing transdural lumbar disk herniation. Clin Imaging 1995;19:12-16.
22. Whittaker CK, Bernhardt M. Magnetic resonance imaging shows gadolinium enhancement of intradural herniated disc. Spine 1994;19:1505-1507.
23. Arrigo RT, Kalanithi P, Boakye M. Is cauda equine syndrome being treated within the recommended time frame? Neurosurgery 2011;68(6):1520-1526.
24. Kardaun JW, White LR, Shaffer WO. Acute complications in patients with surgical treatment of lumbar herniated disc. J Spinal Disord 1990;3(1):30-38.
11. Connolly PJ, Rosenbaum AE, Sacks T, Kopacz KJ. Incomplete intradural
lumbar disk herniation. Orthopediscs 1997;20:977-979.
12. Pradeep KS, Sandeep S, Rajesh D, Pankaj B, Sharad G. Dorsal Herniation of Cauda Equina due to sequestrated intradural disc. Asian Spine J. 2012;6(2):145-147.
13. Ducati LG, Silva MV, Brandao MM, Romero FR, Zianini MA. Intradural lumbar disc herniation: report of five cases with literature review. Eur Spine J. 2013;22(Suppl3):S404-S408.
14. Sasaji T, Horaguchi K, Yamada N, Iwai Kazuo. The specific sagittal Magnetic Resonance Imaging on intradural extraarachnoïd lumbar disc herniation. Hindawi Publishing Corporation, case reports in medicine. 2012;Article ID 383451, 3 pages doi:10.1155/2012/383451.
15. Hida K, Jawasaki Y, Abe H, Shimazaki M, Matsuzaki T. Magnetic Resonance Imaging of intradural lumbar disc herniation. J Clin Neurosci 1999;6:345-347.
16. Wasserstrom R, Mamourian AC, Black JF, Lehman RAW. Intradural lumbar disk fragment with ring enhancement on MR. AJNR Am J Neuroradiol 1993;14:401-404.
17. Fang CM, Huang TJ, Chen WJ, Lee ST, Hsu RW. Intradural lumbar disc herniation. A case report. Chang Keng I Hsueh 1994;17:297-300.
18. Kaiser MC, Sandt G, Roilgen A, Capesius P, Poos D, Ohanna F. Intradural disk herniation with CT appearance of gas collection. AJNR Am J Neuroradiol 1985;6:117-118.
19. Isla AI, Roda JM, Bencosme J, Alvarez MP, Blazquez MG. Intradural herniated dorsal disc. Case report and review of the literature. Neurosurgery 1988;22:737-739.
20. Lidov M, Stollman A, Casden A, Som P, Bederson J. MRI of lumbar intradural disc herniation. Clin Imaging 1994;18:173-178.
21. Snow RD, Williams JP, Weber ED, Richardson PH. Enhancing transdural lumbar disk herniation. Clin Imaging 1995;19:12-16.
22. Whittaker CK, Bernhardt M. Magnetic resonance imaging shows gadolinium enhancement of intradural herniated disc. Spine 1994;19:1505-1507.
23. Arrigo RT, Kalanithi P, Boakye M. Is cauda equine syndrome being treated within the recommended time frame? Neurosurgery 2011;68(6):1520-1526.
24. Kardaun JW, White LR, Shaffer WO. Acute complications in patients with surgical treatment of lumbar herniated disc. J Spinal Disord 1990;3(1):30-38.
Type of Study: Case report |
Subject:
Gamma Knife Radiosurgery
References
1. D'Andrea G, Trillo G, Roperto R, Celli P, Orlando ER, Ferrante L. Intradural lumbar disc herniations : the role of MRI in preoperative diagnosis and review of the literature. Neurosurg Rev 2004;27:75-80. [DOI:10.1007/s10143-003-0296-3] [PMID]
2. Dandy WE. Serious complications of ruptured intervertebral disks. JAMA 1942;119:474-477. [DOI:10.1001/jama.1942.02830230008002]
3. Epstein NE, Syrquin MS, Epstein JA, Decker RE. Intradural disc herniation in the cervical, thoracic and lumbar spine: report of three cases and review of the literature. J Spinal Disord 1990;3:396-403. [PMID]
4. Choi JY, Lee WS, Sung KH. Intradural lumbar disc herniation – Is it predictable preoperatively? A report of two cases. The Spine Journal 2007;7:111-117. [DOI:10.1016/j.spinee.2006.02.025] [PMID]
5. Aydin MV, Ozel S, Sem O, Erdogan B, Yildirim T. Intradural disc mimicking: a spinal tumor lesion. Spinal Cord 2004;42:52-54. [DOI:10.1038/sj.sc.3101476] [PMID]
6. Yildizhan A, Pasaoglu A, Okten T, Ekinci N, Aycan K, Aral O. Intradural disc herniations: pathogenesis, clinical picture, diagnosis and treatment. Actaneurochir (Wien) 1991;110(3-4):160-165. [DOI:10.1007/BF01400685]
7. Kataoka O, Nishibayashi Y, Sho T. Intradural lumbar disc herniation: report of three cases with a review of the literature. Spine 1989;14:529-533. [DOI:10.1097/00007632-198905000-00011] [PMID]
8. Ozer AF, Ozek MM, Pamir MN, Zirh TA, Erzen C. Intradural rupture of cervical vertebral disc. Spine 1994;19:843-845. [DOI:10.1097/00007632-199404000-00021] [PMID]
9. Paini KC, Muduli H, Chauder K, Kav VK. Intrathecal disc prolapse associated with lumbar canal stenosis. Neurology (Bombay) 1972;20:64-66.
10. Mercier P, Hayer G, Ben Ali H, Fournier D, Menei P, Mansour BH, Guy G. Hernies discales lombaires intradurales. A propos de six cas et revue de la littérature. Neurochirurgie 1997;43:142-147. [PMID]
11. Connolly PJ, Rosenbaum AE, Sacks T, Kopacz KJ. Incomplete intradural lumbar disk herniation. Orthopediscs 1997;20:977-979.
12. Pradeep KS, Sandeep S, Rajesh D, Pankaj B, Sharad G. Dorsal Herniation of Cauda Equina due to sequestrated intradural disc. Asian Spine J. 2012;6(2):145-147. [DOI:10.4184/asj.2012.6.2.145] [PMID] [PMCID]
13. Ducati LG, Silva MV, Brandao MM, Romero FR, Zianini MA. Intradural lumbar disc herniation: report of five cases with literature review. Eur Spine J. 2013;22(Suppl3):S404-S408. [DOI:10.1007/s00586-012-2516-4] [PMID] [PMCID]
14. Sasaji T, Horaguchi K, Yamada N, Iwai Kazuo. The specific sagittal Magnetic Resonance Imaging on intradural extraarachnoïd lumbar disc herniation. Hindawi Publishing Corporation, case reports in medicine. 2012;Article ID 383451, 3 pages doi:10.1155/2012/383451. [DOI:10.1155/2012/383451]
15. Hida K, Jawasaki Y, Abe H, Shimazaki M, Matsuzaki T. Magnetic Resonance Imaging of intradural lumbar disc herniation. J Clin Neurosci 1999;6:345-347. [DOI:10.1016/S0967-5868(99)90062-0]
16. Wasserstrom R, Mamourian AC, Black JF, Lehman RAW. Intradural lumbar disk fragment with ring enhancement on MR. AJNR Am J Neuroradiol 1993;14:401-404. [PMID]
17. Fang CM, Huang TJ, Chen WJ, Lee ST, Hsu RW. Intradural lumbar disc herniation. A case report. Chang Keng I Hsueh 1994;17:297-300. [PMID]
18. Kaiser MC, Sandt G, Roilgen A, Capesius P, Poos D, Ohanna F. Intradural disk herniation with CT appearance of gas collection. AJNR Am J Neuroradiol 1985;6:117-118. [PMID]
19. Isla AI, Roda JM, Bencosme J, Alvarez MP, Blazquez MG. Intradural herniated dorsal disc. Case report and review of the literature. Neurosurgery 1988;22:737-739. [DOI:10.1227/00006123-198804000-00020] [PMID]
20. Lidov M, Stollman A, Casden A, Som P, Bederson J. MRI of lumbar intradural disc herniation. Clin Imaging 1994;18:173-178. [DOI:10.1016/0899-7071(94)90077-9]
21. Snow RD, Williams JP, Weber ED, Richardson PH. Enhancing transdural lumbar disk herniation. Clin Imaging 1995;19:12-16. [DOI:10.1016/0899-7071(93)00014-P]
22. Whittaker CK, Bernhardt M. Magnetic resonance imaging shows gadolinium enhancement of intradural herniated disc. Spine 1994;19:1505-1507. [DOI:10.1097/00007632-199407000-00016]
23. Arrigo RT, Kalanithi P, Boakye M. Is cauda equine syndrome being treated within the recommended time frame? Neurosurgery 2011;68(6):1520-1526. [DOI:10.1227/NEU.0b013e31820cd426] [PMID]
24. Kardaun JW, White LR, Shaffer WO. Acute complications in patients with surgical treatment of lumbar herniated disc. J Spinal Disord 1990;3(1):30-38. [DOI:10.1097/00002517-199003000-00006] [PMID]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |