Thu, Apr 25, 2024
Volume 3, Issue 3 (12-2017)
Iran J Neurosurg 2017, 3(3): 95-102 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Gharib-Salehi M, Alimohammadi E, Bagheri S, Saeidi-Brojeni H, Abdi A, Akbary M, et al . Cerebral Angiographic Findings in Non-Traumatic Intracranial Hemorrhage: A Single Center Experience in the West of Iran. Iran J Neurosurg 2017; 3 (3) :95-102
URL: http://irjns.org/article-1-88-en.html
URL: http://irjns.org/article-1-88-en.html
Mohammad Gharib-Salehi1 
 , Ehsan Alimohammadi *
, Ehsan Alimohammadi * 
 2, Seyed-Reza Bagheri3
2, Seyed-Reza Bagheri3 
 , Hamidreza Saeidi-Brojeni3
, Hamidreza Saeidi-Brojeni3 
 , Alireza Abdi4
, Alireza Abdi4 
 , Meisam Akbary5
, Meisam Akbary5 
 , Mozhgan Nargesi4
, Mozhgan Nargesi4 
 , Zahra Abbasi4
, Zahra Abbasi4 
 , Ameneh Khani4
, Ameneh Khani4 
 , Akram Amiri4
, Akram Amiri4 


 , Ehsan Alimohammadi *
, Ehsan Alimohammadi * 
 2, Seyed-Reza Bagheri3
2, Seyed-Reza Bagheri3 
 , Hamidreza Saeidi-Brojeni3
, Hamidreza Saeidi-Brojeni3 
 , Alireza Abdi4
, Alireza Abdi4 
 , Meisam Akbary5
, Meisam Akbary5 
 , Mozhgan Nargesi4
, Mozhgan Nargesi4 
 , Zahra Abbasi4
, Zahra Abbasi4 
 , Ameneh Khani4
, Ameneh Khani4 
 , Akram Amiri4
, Akram Amiri4 

1- Department of Radiology, Faculty of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran
2- Department of Neurosurgery, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran , hafez125@gmail.com
3- Department of Neurosurgery, Faculty of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran
4- Department of Nursing, Faculty of Nursing and Midwifery, Kermanshah University of Medical Sciences, Kermanshah, Iran
5- Faculty of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran
2- Department of Neurosurgery, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran , hafez125@gmail.com
3- Department of Neurosurgery, Faculty of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran
4- Department of Nursing, Faculty of Nursing and Midwifery, Kermanshah University of Medical Sciences, Kermanshah, Iran
5- Faculty of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran
Full Text [PDF 852 kb]
(1429 Downloads)
| Abstract (HTML) (5797 Views)
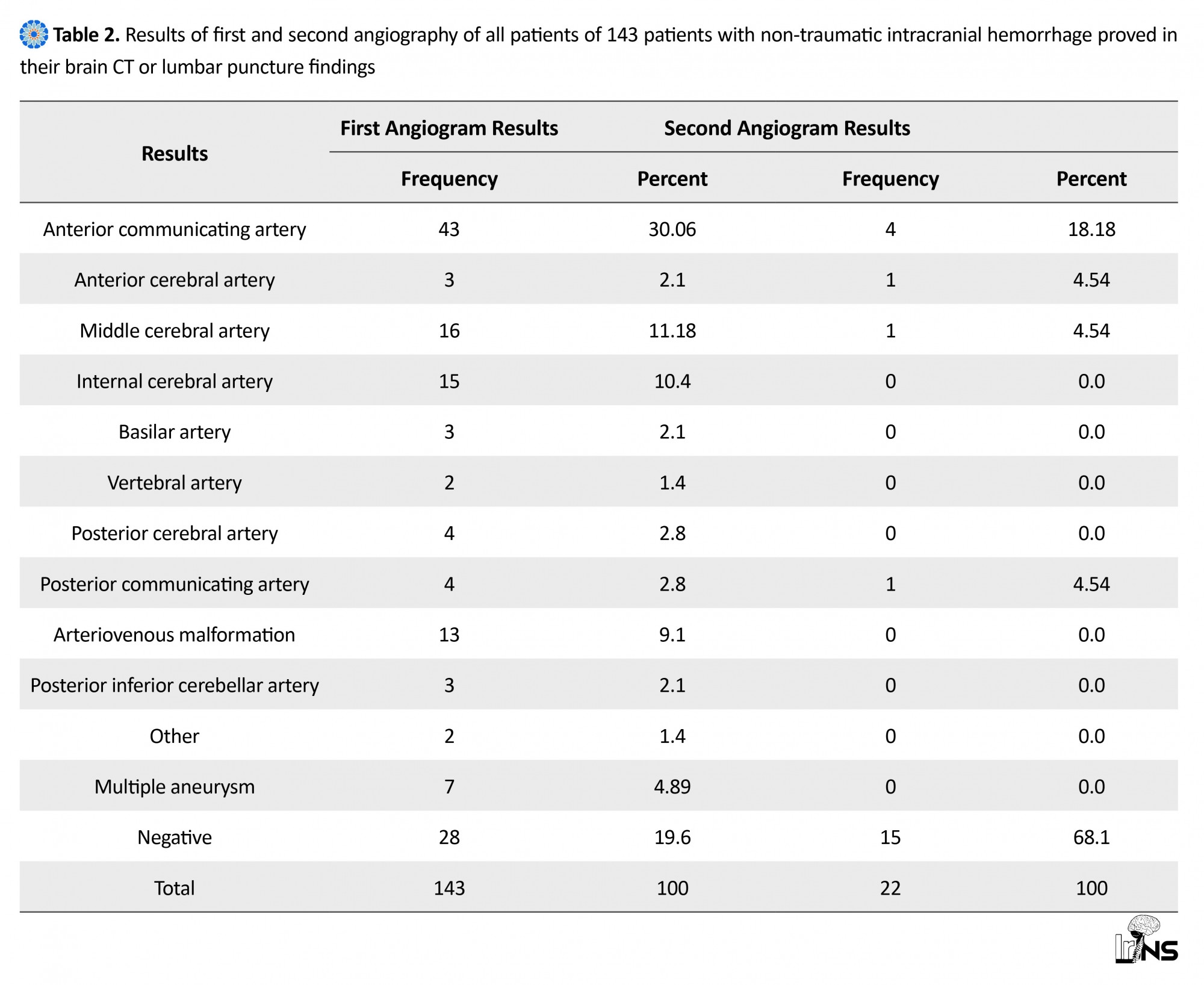
In patients with intracranial aneurysms, eighty-two (82%) aneurysms were in anterior circulation and 18(18%) of them were in posterior circulation. The most common aneurysms were anterior communicating artery (Acom) (43%), middle cerebral artery (MCA) (16%) and internal carotid artery (ICA) (15%), respectively. Moreover, 27(27%) aneurysms had a size less than 5 mm, 67(67%) ones between 5 to 25 mm and 6(6%) ones were giant (size more than 25 mm) (Table 3). We concluded that 13 patients had arteriovenous malformation, 8(61.5%) of them located in parieto-occipital region, 2(15.4%) in temporal, 1(7.7%) in frontal region and 2(15.4%) had deep AVM. Two patients with AVM had aneurysms synchronously, one had intranidal aneurysm and one had proximal aneurysms at the ipsilateral side of AVM. Two (1.4%) patients with SAH had dural arteriovenous fistula in their angiogram. Twenty-eight (19.6%) patients had negative angiogram. Besides, 22 cases underwent second angiography after one to two weeks. The most common positive finding in the second angiogram was Acom aneurysms (18.18%) (Table 2).
4. Discussion
In this study, we evaluated 143 cases suffering non-traumatic intracranial hemorrhage which was confirmed through CT analysis or lumbar puncture. Angiographic detectable causes for non-traumatic intracranial hemorrhage was obtained in 81.4% and 85.31% of cases after the first and second angiography, respectively. Similar to most of the studies, in our study the most common diagnosis with negative angiography was missed aneurysms [16, 17]. The Acom aneurysms had most false negativity in angiography in agreement with other studies [18, 19]. Causes suggested for inducing false negative angiography may include technical errors such as incomplete angiographic views, presence of vasospasm (especially on the 3rd to 14th day of hemorrhage), presence of hematoma mass-effect, existence of thrombosis in the neck of aneurysms and injection of hyperosmolar contrast [20-27]. According to most reports by other researchers, the maximum number of cases with non-traumatic intracranial hemorrhage were detected in age range of 50-59 years old [11, 14, 15, 19, 28]. Increased age has been recognized as a risk factor of hemorrhage; however, extreme old age is protective, decreasing the risk of hemorrhage [12, 16, 19, 22, 29]. In the present work, women at their sixth decade of life consisted most of the patients as in some other studies [9, 11, 25, 30]. The majority of studies have reported a female-to-male ratio of about 1.09-1.42 [23, 31, 32]. Some experts proposed the role of female hormones in female preference for non-traumatic intracranial hemorrhage but there is a controversy about this [33, 34]. The results of this study were compatible with most other studies.
The common causes of non-traumatic intracranial hemorrhage are aneurysms and Arteriovenous Malformations (AVM) [3-5, 35, 36]. Intracranial hemorrhage secondary to AVM occurs in the younger patients relative to aneurysms (before 30 years of age versus after 50 years of age) [37, 38]. In our study, the mean age of patients with AVM were lesser than the mean age of patients with aneurysm.
The risk of bleeding of an aneurysm elevates with increased size of it but aneurysms can present with bleeding at any size [39, 40]. According to the literature, aneurysms with size less than 5 mm are less prone to bleeding while larger aneurysms are more susceptible to bleeding [40, 41]. Age less than 50 years old, aneurysm diameter greater than 4.0 mm, hypertension, and aneurysm multiplicity were found to be predictors of rupture of small aneurysms [39-42].
The possibility of missed smaller aneurysm in angiography is higher than larger ones [35, 37, 43]. In our study, most of the aneurysms had a size between 5 to 15 mm and most of the missed aneurysms in first angiography had a size lesser than 5 mm.
We found 82(82%) aneurysms in anterior circulation and 18(18%) of them in posterior circulation. The most common aneurysms were Acom (43%), MCA (16%) and ICA (15%), respectively. This is compatible with most of other studies [7, 12, 15, 17, 25, 30, 36]. The rate of multiple aneurysms have been reported 10-15% in prior literature but the amount of less than 5% to more than 30% have been reported, too [20, 31, 43]. The rate of multiple aneurysms in this study was 4.89% that is less than other reported ones. According to most studies, multiple aneurysms have a higher risk of hemorrhage, but there is no consistency in the existing data [20, 31, 35, 37].
In our study, AVM was found in 13 (9.1%) of the patients. Eight (61.5%) patients had AVM in parieto-occipital region, 2(15.4%) in temporal, 1(7.7%) in frontal region and 2(15.4%) had deep AVM. The most common presentation of AVM are bleeding, seizure and focal neurological deficits [9, 15]. Intraparenchymal hemorrhage, intraventricular hemorrhage and subarachnoid hemorrhage are the most common types of bleeding in patients with AVM [15, 32, 40]. Subarachnoid hemorrhage is more common when an AVM is located cortically [32, 40]. Interestingly, in our study the most common type of bleeding in these patients was SAH. It may be due to the overall higher number of patients with SAH than ICH and cortical location in most of our AVMs. As a limitation, we can mention the retrospective data collection and the high chance of missing ones.
5. Conclusion
Aneurysms and arteriovenous malformation are the most common causes of non-traumatic intracranial hemorrhage. The most common place of intracranial aneurysms is the circle of Willis. A second angiogram after 1 to 2 weeks is necessary in most patients with negative outcomes in first angiography after non-traumatic intracranial hemorrhage.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that they have no conflicts of interest. Authors' Contribution is as follows: Conception and design: Mohammad Gharib-Salehi, Ehsan Alimohammadi; Data Collection: Meisam Akbari, Mozhgan Nargesi, Zahra Abbasi, Ameneh Khani, Akram Amiri; Drafting the article: Ehsan Alimohammadi, Seyed-Reza Bagheri, Meisam Akbari, Mozhgan Nargesi, Zahra Abbasi, Ameneh Khani, Akram Amiri; Critically revising the article: Hamidreza Saeidi-Brojeni, Alireza Abdi; Reviewing submitted version of manuscript: Alireza Abdi; and Approving the final version of the manuscript: All authors.
References
Full Text: (1819 Views)
1. Introduction
Spontaneous intracranial hemorrhages occur in the absence of trauma [1, 2]. Aneurysm, arteriovenous malformation and cavernous malformation are the most common causes of non-traumatic intracranial hemorrhages [3-5]. Conventional catheter angiography is the gold standard for diagnosis of vascular abnormality; however; other imaging modalities such as CTA and MRA can help to find out about vascular abnormalities [6-8]. Intracranial aneurysms are the most common causes of non-traumatic intracranial hemorrhage, occurring in 60%-85% of cases [9, 10]. The most common place of intracranial aneurysms is the circle of Willis and its immediate branches [11-13]. The location and the size of the aneurysms are the important factors influencing management and prognosis of patients [14, 15]. The main aim of our study was to evaluate the demographic characteristics of 143 patients with non-traumatic intracranial hemorrhage, their angiographic results and correlation of CT scan findings and angiography of patients, investigating the etiologies and their angiographic presentations and discerning the anatomical distribution of cerebral aneurysms and areriovenous malformations in the Kermanshah.
2. Methods & Materials/Patients
Patients
This is a retrospective study in which the records of 143 patients with non-traumatic intracranial hemorrhage based on their brain Computed Tomography (CT) scan images or lumbar puncture findings were reviewed. The study population included the patients with non-traumatic intracranial hemorrhage (which was proven through CT scan or lumbar puncture), referring to Imam Reza Hospital, Kermanshah University of Medical Sciences in Kermanshah city (western Iran). The sample was selected via census method during five years from April 2011 to April 2017. For data collection, a permission was obtained from Kermanshah University of Medical Sciences and the researcher was referred to Imam Reza Hospital.
Inclusion criteria
Documented non-traumatic intracranial hemorrhage finding and age between 10 to 70 years old were the inclusion criteria of this study.
Exclusion criteria
We excluded the patients with severe coagulopathy that accounted for the hemorrhage and those with hemorrhage into the tumor which was diagnosed by brain CT scan or MRI.
Procedure
We used a checklist for data gathering that included demographic features of patients such as age and sex, patients’ brain CT scan findings and results of the first and second angiography. For all patients, four vessel catheter angiography via the femoral approach was performed in the Medical Imaging Center of Kermanshah University of Medical Sciences. Image acquisition was done by Digital Subtraction Angiography (DSA). A positive angiography was defined by the identification of a vascular abnormality accounting for the hemorrhage. The angiogram was repeated after 1 to 2 weeks of primary negative angiogram except in patients with SAH in perimesencephalic cisterns. SPSS (version 20) was used for the data analysis. The statistical error type I and confidence interval were 5% and 95%, respectively.
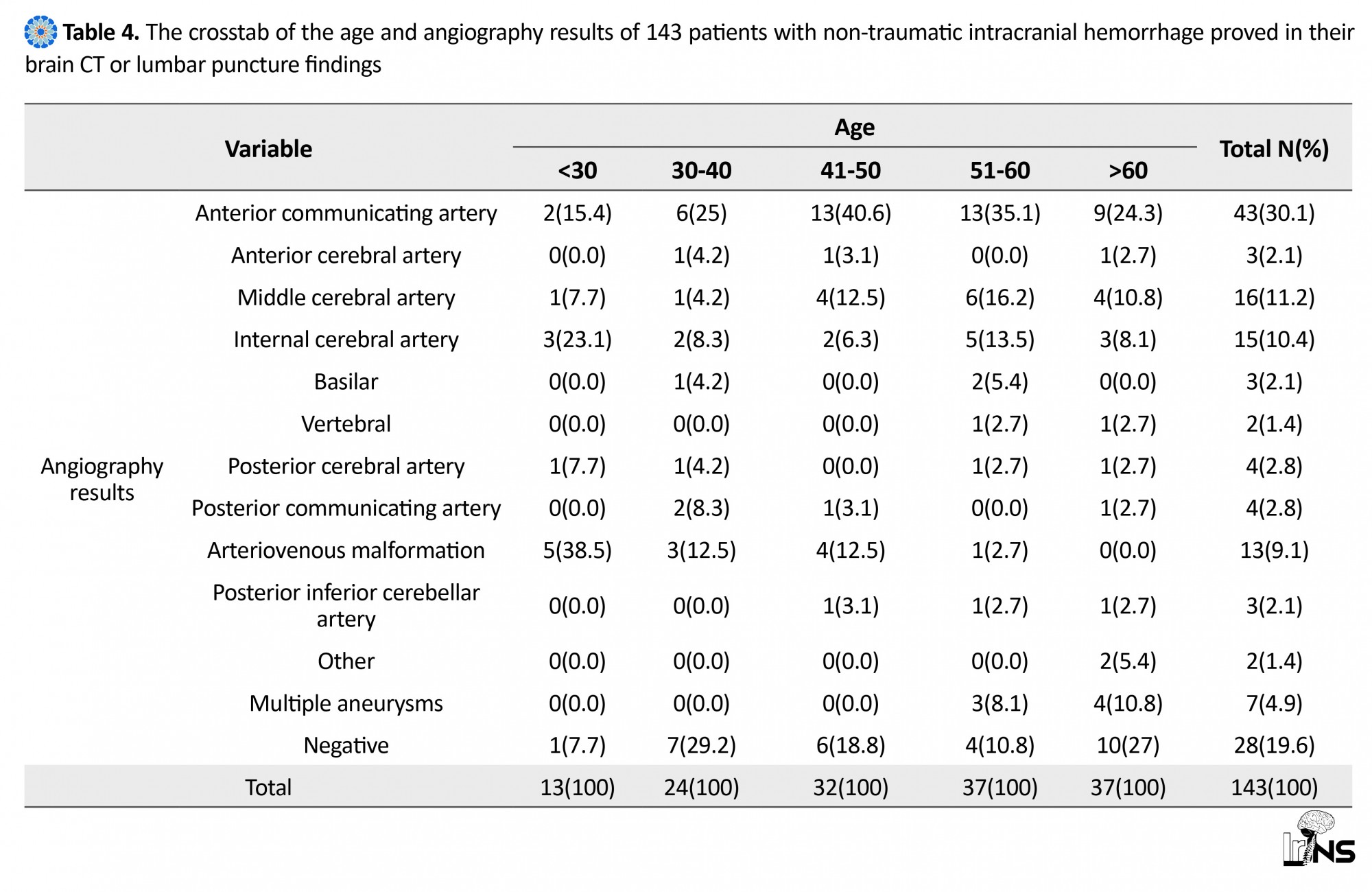
3. Results
In this study, 143 cases of non-traumatic intracranial hemorrhage proven by CT (n=121, 91.61%) or lumbar puncture (n=12, 8.39%) were evaluated. Of 143 patients studied, 64(44.8%) were men and 79(55.2%) women. The mean±SD of patients’ age was 53.7±12.1 years old (Tables 1 and 4). Brain CT findings revealed that 104(72.7%) patients had subarachnoid hemorrhage, 19(13.3%) ones had ICH, 8(5.6%) ones had IVH and 12(8.4%) patients had normal brain CT scan (Tables 1 and 5). Furthermore, the results of the first angiogram showed that 100 cases had aneurysm (69.93%), 13 cases had AVM (9.09%). The angiogram of 28 cases were negative (19.58%), 2 cases had other pathologies (1.4%) and 7(4.89%) cases had multiple aneurysms (all of them had two aneurysms) (Table 2).
Spontaneous intracranial hemorrhages occur in the absence of trauma [1, 2]. Aneurysm, arteriovenous malformation and cavernous malformation are the most common causes of non-traumatic intracranial hemorrhages [3-5]. Conventional catheter angiography is the gold standard for diagnosis of vascular abnormality; however; other imaging modalities such as CTA and MRA can help to find out about vascular abnormalities [6-8]. Intracranial aneurysms are the most common causes of non-traumatic intracranial hemorrhage, occurring in 60%-85% of cases [9, 10]. The most common place of intracranial aneurysms is the circle of Willis and its immediate branches [11-13]. The location and the size of the aneurysms are the important factors influencing management and prognosis of patients [14, 15]. The main aim of our study was to evaluate the demographic characteristics of 143 patients with non-traumatic intracranial hemorrhage, their angiographic results and correlation of CT scan findings and angiography of patients, investigating the etiologies and their angiographic presentations and discerning the anatomical distribution of cerebral aneurysms and areriovenous malformations in the Kermanshah.
2. Methods & Materials/Patients
Patients
This is a retrospective study in which the records of 143 patients with non-traumatic intracranial hemorrhage based on their brain Computed Tomography (CT) scan images or lumbar puncture findings were reviewed. The study population included the patients with non-traumatic intracranial hemorrhage (which was proven through CT scan or lumbar puncture), referring to Imam Reza Hospital, Kermanshah University of Medical Sciences in Kermanshah city (western Iran). The sample was selected via census method during five years from April 2011 to April 2017. For data collection, a permission was obtained from Kermanshah University of Medical Sciences and the researcher was referred to Imam Reza Hospital.
Inclusion criteria
Documented non-traumatic intracranial hemorrhage finding and age between 10 to 70 years old were the inclusion criteria of this study.
Exclusion criteria
We excluded the patients with severe coagulopathy that accounted for the hemorrhage and those with hemorrhage into the tumor which was diagnosed by brain CT scan or MRI.
Procedure
We used a checklist for data gathering that included demographic features of patients such as age and sex, patients’ brain CT scan findings and results of the first and second angiography. For all patients, four vessel catheter angiography via the femoral approach was performed in the Medical Imaging Center of Kermanshah University of Medical Sciences. Image acquisition was done by Digital Subtraction Angiography (DSA). A positive angiography was defined by the identification of a vascular abnormality accounting for the hemorrhage. The angiogram was repeated after 1 to 2 weeks of primary negative angiogram except in patients with SAH in perimesencephalic cisterns. SPSS (version 20) was used for the data analysis. The statistical error type I and confidence interval were 5% and 95%, respectively.
3. Results
In this study, 143 cases of non-traumatic intracranial hemorrhage proven by CT (n=121, 91.61%) or lumbar puncture (n=12, 8.39%) were evaluated. Of 143 patients studied, 64(44.8%) were men and 79(55.2%) women. The mean±SD of patients’ age was 53.7±12.1 years old (Tables 1 and 4). Brain CT findings revealed that 104(72.7%) patients had subarachnoid hemorrhage, 19(13.3%) ones had ICH, 8(5.6%) ones had IVH and 12(8.4%) patients had normal brain CT scan (Tables 1 and 5). Furthermore, the results of the first angiogram showed that 100 cases had aneurysm (69.93%), 13 cases had AVM (9.09%). The angiogram of 28 cases were negative (19.58%), 2 cases had other pathologies (1.4%) and 7(4.89%) cases had multiple aneurysms (all of them had two aneurysms) (Table 2).
In patients with intracranial aneurysms, eighty-two (82%) aneurysms were in anterior circulation and 18(18%) of them were in posterior circulation. The most common aneurysms were anterior communicating artery (Acom) (43%), middle cerebral artery (MCA) (16%) and internal carotid artery (ICA) (15%), respectively. Moreover, 27(27%) aneurysms had a size less than 5 mm, 67(67%) ones between 5 to 25 mm and 6(6%) ones were giant (size more than 25 mm) (Table 3). We concluded that 13 patients had arteriovenous malformation, 8(61.5%) of them located in parieto-occipital region, 2(15.4%) in temporal, 1(7.7%) in frontal region and 2(15.4%) had deep AVM. Two patients with AVM had aneurysms synchronously, one had intranidal aneurysm and one had proximal aneurysms at the ipsilateral side of AVM. Two (1.4%) patients with SAH had dural arteriovenous fistula in their angiogram. Twenty-eight (19.6%) patients had negative angiogram. Besides, 22 cases underwent second angiography after one to two weeks. The most common positive finding in the second angiogram was Acom aneurysms (18.18%) (Table 2).
4. Discussion
In this study, we evaluated 143 cases suffering non-traumatic intracranial hemorrhage which was confirmed through CT analysis or lumbar puncture. Angiographic detectable causes for non-traumatic intracranial hemorrhage was obtained in 81.4% and 85.31% of cases after the first and second angiography, respectively. Similar to most of the studies, in our study the most common diagnosis with negative angiography was missed aneurysms [16, 17]. The Acom aneurysms had most false negativity in angiography in agreement with other studies [18, 19]. Causes suggested for inducing false negative angiography may include technical errors such as incomplete angiographic views, presence of vasospasm (especially on the 3rd to 14th day of hemorrhage), presence of hematoma mass-effect, existence of thrombosis in the neck of aneurysms and injection of hyperosmolar contrast [20-27]. According to most reports by other researchers, the maximum number of cases with non-traumatic intracranial hemorrhage were detected in age range of 50-59 years old [11, 14, 15, 19, 28]. Increased age has been recognized as a risk factor of hemorrhage; however, extreme old age is protective, decreasing the risk of hemorrhage [12, 16, 19, 22, 29]. In the present work, women at their sixth decade of life consisted most of the patients as in some other studies [9, 11, 25, 30]. The majority of studies have reported a female-to-male ratio of about 1.09-1.42 [23, 31, 32]. Some experts proposed the role of female hormones in female preference for non-traumatic intracranial hemorrhage but there is a controversy about this [33, 34]. The results of this study were compatible with most other studies.
The common causes of non-traumatic intracranial hemorrhage are aneurysms and Arteriovenous Malformations (AVM) [3-5, 35, 36]. Intracranial hemorrhage secondary to AVM occurs in the younger patients relative to aneurysms (before 30 years of age versus after 50 years of age) [37, 38]. In our study, the mean age of patients with AVM were lesser than the mean age of patients with aneurysm.
The risk of bleeding of an aneurysm elevates with increased size of it but aneurysms can present with bleeding at any size [39, 40]. According to the literature, aneurysms with size less than 5 mm are less prone to bleeding while larger aneurysms are more susceptible to bleeding [40, 41]. Age less than 50 years old, aneurysm diameter greater than 4.0 mm, hypertension, and aneurysm multiplicity were found to be predictors of rupture of small aneurysms [39-42].
The possibility of missed smaller aneurysm in angiography is higher than larger ones [35, 37, 43]. In our study, most of the aneurysms had a size between 5 to 15 mm and most of the missed aneurysms in first angiography had a size lesser than 5 mm.
We found 82(82%) aneurysms in anterior circulation and 18(18%) of them in posterior circulation. The most common aneurysms were Acom (43%), MCA (16%) and ICA (15%), respectively. This is compatible with most of other studies [7, 12, 15, 17, 25, 30, 36]. The rate of multiple aneurysms have been reported 10-15% in prior literature but the amount of less than 5% to more than 30% have been reported, too [20, 31, 43]. The rate of multiple aneurysms in this study was 4.89% that is less than other reported ones. According to most studies, multiple aneurysms have a higher risk of hemorrhage, but there is no consistency in the existing data [20, 31, 35, 37].
In our study, AVM was found in 13 (9.1%) of the patients. Eight (61.5%) patients had AVM in parieto-occipital region, 2(15.4%) in temporal, 1(7.7%) in frontal region and 2(15.4%) had deep AVM. The most common presentation of AVM are bleeding, seizure and focal neurological deficits [9, 15]. Intraparenchymal hemorrhage, intraventricular hemorrhage and subarachnoid hemorrhage are the most common types of bleeding in patients with AVM [15, 32, 40]. Subarachnoid hemorrhage is more common when an AVM is located cortically [32, 40]. Interestingly, in our study the most common type of bleeding in these patients was SAH. It may be due to the overall higher number of patients with SAH than ICH and cortical location in most of our AVMs. As a limitation, we can mention the retrospective data collection and the high chance of missing ones.
5. Conclusion
Aneurysms and arteriovenous malformation are the most common causes of non-traumatic intracranial hemorrhage. The most common place of intracranial aneurysms is the circle of Willis. A second angiogram after 1 to 2 weeks is necessary in most patients with negative outcomes in first angiography after non-traumatic intracranial hemorrhage.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that they have no conflicts of interest. Authors' Contribution is as follows: Conception and design: Mohammad Gharib-Salehi, Ehsan Alimohammadi; Data Collection: Meisam Akbari, Mozhgan Nargesi, Zahra Abbasi, Ameneh Khani, Akram Amiri; Drafting the article: Ehsan Alimohammadi, Seyed-Reza Bagheri, Meisam Akbari, Mozhgan Nargesi, Zahra Abbasi, Ameneh Khani, Akram Amiri; Critically revising the article: Hamidreza Saeidi-Brojeni, Alireza Abdi; Reviewing submitted version of manuscript: Alireza Abdi; and Approving the final version of the manuscript: All authors.
References
- Ahn SY, Lim DJ, Kim SH, Kim SD, Hong KS, Ha SK. Clinical analysis of patients with spontaneous subarachnoid hemorrhage of initial negative angiography. Korean Journal of Cerebrovascular Surgery. 2011; 13(3):230-4.
- Alén JF, Lagares A, Campollo J, Ballenilla F, Kaen A, Núñez ÁP, et al. Idiopathic subarachnoid hemorrhage and venous drainage: Are they related? Neurosurgery. 2008; 63(6):1106-12. doi: 10.1227/01.neu.0000335777.14055.71
- Almandoz JED, Jagadeesan BD, Refai D, Moran CJ, Cross III DT, Chicoine MR, et al. Diagnostic yield of repeat catheter angiography in patients with catheter and computed tomography angiography negative subarachnoid hemorrhage. Neurosurgery. 2012; 70(5):1135-42. doi: 10.1227/neu.0b013e318242575e
- Boswell S, Thorell W, Gogela S, Lyden E, Surdell D. Angiogram-negative subarachnoid hemorrhage: outcomes data and review of the literature. Journal of Stroke and Cerebrovascular Diseases. 2013; 22(6):750-7. doi: 10.1016/j.jstrokecerebrovasdis.2012.02.001
- Canneti B, Mosqueira AJ, Nombela F, Gilo F, Vivancos J. Spontaneous subarachnoid hemorrhage with negative angiography managed in a stroke unit: Clinical and prognostic characteristics. Journal of Stroke and Cerebrovascular Diseases. 2015; 24(11):2484-90. doi: 10.1016/j.jstrokecerebrovasdis.2015.06.011
- Cánovas D, Gil A, Jato M, de Miquel M, Rubio F. Clinical outcome of spontaneous non‐aneurysmal subarachnoid hemorrhage in 108 patients. European Journal of Neurology. 2012; 19(3):457-61. doi: 10.1111/j.1468-1331.2011.03542.x
- Connors JL, Wojak J. Intracranial aneurysms; general considerations. In: Connors JL, Wojak JC, editors. Interventional Neuroradiology. Philadelphia: WB Saunders. 1998.
- De Oliveira Manoel AL, Turkel-Parrella D, Germans M, Kouzmina E, da Silva Almendra P, Marotta T, et al. Safety of early pharmacological thromboprophylaxis after subarachnoid hemorrhage. The Canadian Journal of Neurological Sciences. 2014; 41(05):554-61. doi: 10.1017/cjn.2014.16
- Dupont SA, Lanzino G, Wijdicks EF, Rabinstein AA. The use of clinical and routine imaging data to differentiate between aneurysmal and nonaneurysmal subarachnoid hemorrhage prior to angiography: Clinical article. Journal of Neurosurgery. 2010; 113(4):790-4. doi: 10.3171/2010.4.jns091932
- El Khaldi M, Pernter P, Ferro F, Alfieri A, Decaminada N, Naibo L, et al. Detection of cerebral aneurysms in nontraumatic subarachnoid haemorrhage: Role of multislice CT angiography in 130 consecutive patients. La radiologia medica. 2007; 112(1):123-37. doi: 10.1007/s11547-007-0126-8
- Elhadi AM, Zabramski JM, Almefty KK, Mendes GA, Nakaji P, McDougall CG, et al. Spontaneous subarachnoid hemorrhage of unknown origin: hospital course and long-term clinical and angiographic follow-up. Journal of Neurosurgery. 2015; 122(3):663-70. doi: 10.3171/2014.10.jns14175
- Flaherty ML, Haverbusch M, Kissela B, Kleindorfer D, Schneider A, Sekar P, et al. Perimesencephalic subarachnoid hemorrhage: incidence, risk factors, and outcome. Journal of Stroke and Cerebrovascular Diseases. 2005; 14(6):267-71. doi: 10.1016/j.jstrokecerebrovasdis.2005.07.004
- Zhao J, Lin H, Summers R, Yang M, Cousins BG, Tsui J. Current treatment strategies for intracranial aneurysms: An overview. Angiology. 2017; 69(1):17-30. doi: 10.1177/0003319717700503
- Fontanella M, Rainero I, Panciani PP, Schatlo B, Benevello C, Garbossa D, et al. Subarachnoid hemorrhage and negative angiography: Clinical course and long-term follow-up. Neurosurgical Review. 2011; 34(4):477-84. doi: 10.1007/s10143-011-0323-8
- Halpin S, Britton J, Byrne J, Clifton A, Hart G, Moore A. Prospective evaluation of cerebral angiography and computed tomography in cerebral haematoma. Journal of Neurology, Neurosurgery & Psychiatry. 1994; 57(10):1180-6. doi: 10.1136/jnnp.57.10.1180
- Huttner H, Hartmann M, Köhrmann M, Neher M, Stippich C, Hähnel S, et al. Repeated digital substraction angiography after perimesencephalic subarachnoid hemorrhage? Journal of Neuroradiology. 2006; 33(2):87-9. doi: 10.1016/s0150-9861(06)77236-4
- Ildan F, Tuna M, Erman T, Göçer AI, Çetinalp E, Burgut R. Prognosis and prognostic factors for unexplained subarachnoid hemorrhage: review of 84 cases. Neurosurgery. 2002; 50(5):1015-25. doi: 10.1227/00006123-200205000-00015
- Inamasu J, Nakamura Y, Saito R, Horiguchi T, Kuroshima Y, Mayanagi K, et al. “Occult” ruptured cerebral aneurysms revealed by repeat angiography: result from a large retrospective study. Clinical Neurology and Neurosurgery. 2003; 106(1):33-7. doi: 10.1016/j.clineuro.2003.09.002
- Ishihara H, Kato S, Akimura T, Suehiro E, Oku T, Suzuki M. Angiogram-negative subarachnoid hemorrhage in the era of three dimensional rotational angiography. Journal of Clinical Neuroscience. 2007; 14(3):252-5. doi: 10.1016/j.jocn.2006.01.011
- Jung JY, Kim YB, Lee JW, Huh SK, Lee KC. Spontaneous subarachnoid haemorrhage with negative initial angiography: A review of 143 cases. Journal of Clinical Neuroscience. 2006; 13(10):1011-7. doi: 10.1016/j.jocn.2005.09.007
- Kaim A, Proske M, Kirsch E, Weymarn Av, Radü EW, Steinbrich W. Value of repeat‐angiography in cases of unexplained Subarachnoid Hemorrhage (SAH). Acta Neurologica Scandinavica. 1996; 93(5):366-73. doi: 10.1111/j.1600-0404.1996.tb00011.x
- Karttunen A, Jartti P, Ukkola V, Sajanti J, Haapea M. Value of the quantity and distribution of subarachnoid haemorrhage on CT in the localization of a ruptured cerebral aneurysm. Acta Neurochirurgica. 2003; 145(8):655-61. doi: 10.1007/s00701-003-0080-8
- Kaufmann TJ, Huston III J, Mandrekar JN, Schleck CD, Thielen KR, Kallmes DF. Complications of diagnostic cerebral angiography: Evaluation of 19 826 consecutive patients 1. Radiology. 2007; 243(3):812-9. doi: 10.1148/radiol.2433060536
- Khan A, Smith JS, Kirkman M, Robertson F, Wong K, Dott C, et al. Angiogram negative subarachnoid haemorrhage: outcomes and the role of repeat angiography. Clinical Neurology and Neurosurgery. 2013; 115(8):1470-5. doi: /10.1016/j.clineuro.2013.02.002
- Kitkhuandee A, Thammaroj J, Munkong W, Duangthongpon P, Thanapaisal C. Cerebral angiographic findings in patients with non-traumatic subarachnoid hemorrhage. Journal of the Medical Association of Thailand. 2012; 95(11):S121-S9. PMID: 23961631
- Konczalla J, Schmitz J, Kashefiolasl S, Senft C, Seifert V, Platz J. Non‐aneurysmal subarachnoid hemorrhage in 173 patients: a prospective study of long‐term outcome. European Journal of Neurology. 2015; 22(10):1329-36. doi: 10.1111/ene.12762
- Bhogal P, AlMatter M, Hellstern V, et al. Difference in aneurysm characteristics between ruptured and unruptured aneurysms in patients with multiple intracranial aneurysms. Surgical Neurology International. 2018;9:(1)1. doi: 10.4103/sni.sni_339_17
- Korja M, Silventoinen K, Laatikainen T, Jousilahti P, Salomaa V, Hernesniemi J, et al. Risk factors and their combined effects on the incidence rate of subarachnoid hemorrhage–a population-based cohort study. PLoS One. 2013;8(9):e73760. doi: 10.1371/journal.pone.0073760
- Little AS, Garrett M, Germain R, Farhataziz N, Albuquerque FC, McDougall CG, et al. Evaluation of patients with spontaneous subarachnoid hemorrhage and negative angiography. Neurosurgery. 2007; 61(6):1139-51. doi: 10.1227/01.neu.0000306091.30517.e7
- Moran CJ. Aneurysmal subarachnoid hemorrhage: DSA versus CT angiography—is the answer available? Radiology. 2011; 258(1):15-7. doi: 10.1148/radiol.101911
- Prestigiacomo CJ, Sabit A, He W, Jethwa P, Gandhi C, Russin J. Three dimensional CT angiography versus digital subtraction angiography in the detection of intracranial aneurysms in subarachnoid hemorrhage. Journal of NeuroInterventional Surgery. 2010; 2(4):385-9. doi: 10.1136/jnis.2010.002246
- Sarabia R, Lagares A, Fernández-Alén J, Arikan F, Vilalta J, Ibáñez J, et al. Idiopathic subarachnoid hemorrhage: a multicentre series of 220 patients. Neurocirugía. 2010; 21(6):441-51. doi: 10.1016/s1130-1473(10)70094-4
- Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. New England Journal of Medicine. 2006; 354(4):387-96. doi: 10.1056/nejmra052732
- Topcuoglu MA, Ogilvy CS, Carter BS, Buonanno FS, Koroshetz WJ, Singhal AB. Subarachnoid hemorrhage without evident cause on initial angiography studies: diagnostic yield of subsequent angiography and other neuroimaging tests. Journal of Neurosurgery. 2003; 98(6):1235-40. doi: 10.3171/jns.2003.98.6.1235
- Vaitkevicius G, Gvazdaitis A, Lukosevicius S. [Spontaneous subarachnoid hemorrhage: Patients’ examination after aneurysm-negative initial angiograms (Lithuanian)]. Medicina (Kaunas, Lithuania). 2001; 38(10):976-81. doi: PMID: 12532705
- Hammer A, Steiner A, Kerry G, et al. Treatment of ruptured intracranial aneurysms yesterday and now. PLoS ONE. 2017;12(3):e0172837. doi: 10.1371/journal.pone.0172837
- Van Gijn J, Rinkel G. Subarachnoid haemorrhage: Diagnosis, causes and management. Brain. 2001; 124(2):249-78. doi: 10.1093/brain/124.2.249
- Vega C, Kwoon JV, Lavine SD. Intracranial aneurysms: current evidence and clinical practice. American Family Physician. 2002; 66(4):601-8. PMID: 12201551
- Vivancos J, Gilo F, Frutos R, Maestre J, García-Pastor A, Quintana F, et al. Clinical management guidelines for subarachnoid haemorrhage. Diagnosis and treatment. Neurología (English Edition). 2014; 29(6):353-70. doi: 10.1016/j.nrl.2012.07.009.
- Willinsky RA, Taylor SM, TerBrugge K, Farb RI, Tomlinson G, Montanera W. Neurologic complications of cerebral angiography: prospective analysis of 2,899 procedures and review of the literature 1. Radiology. 2003; 227(2):522-8. doi: 10.1148/radiol.2272012071
- Yu DW, Jung YJ, Choi BY, Chang CH. Subarachnoid hemorrhage with negative baseline digital subtraction angiography: is repeat digital subtraction angiography necessary? Journal of Cerebrovascular and Endovascular Neurosurgery. 2012; 14(3):210-5. doi: 10.7461/jcen.2012.14.3.210
- Zhu X, Chan M, Poon W. Spontaneous intracranial hemorrhage: which patients need diagnostic cerebral angiography? Stroke. 1997; 28(7):1406-9. doi: 10.1161/01.str.28.7.1406
- Firouznia K, Ghaanati H, Shabani Sm, Shakiba M. Subarachnoid hemorrhage; An an-giographic evaluation in Iran. Iranian Journal of Radiology. 2004; 2(1-2):28-33.
Type of Study: Research |
References
1. Ahn SY, Lim DJ, Kim SH, Kim SD, Hong KS, Ha SK. Clinical analysis of patients with spontaneous subarachnoid hemorrhage of initial negative angiography. Korean Journal of Cerebrovascular Surgery. 2011; 13(3):230-4.
2. Alén JF, Lagares A, Campollo J, Ballenilla F, Kaen A, Nú-ez ÁP, et al. Idiopathic subarachnoid hemorrhage and venous drainage: Are they related? Neurosurgery. 2008; 63(6):1106-12. doi: 10.1227/01.neu.0000335777.14055.71 [DOI:10.1227/01.NEU.0000335777.14055.71]
3. Almandoz JED, Jagadeesan BD, Refai D, Moran CJ, Cross III DT, Chicoine MR, et al. Diagnostic yield of repeat catheter angiography in patients with catheter and computed tomography angiography negative subarachnoid hemorrhage. Neurosurgery. 2012; 70(5):1135-42. doi: 10.1227/neu.0b013e318242575e [DOI:10.1227/NEU.0b013e318242575e]
4. Boswell S, Thorell W, Gogela S, Lyden E, Surdell D. Angiogram-negative subarachnoid hemorrhage: outcomes data and review of the literature. Journal of Stroke and Cerebrovascular Diseases. 2013; 22(6):750-7. doi: 10.1016/j.jstrokecerebrovasdis.2012.02.001 [DOI:10.1016/j.jstrokecerebrovasdis.2012.02.001]
5. Canneti B, Mosqueira AJ, Nombela F, Gilo F, Vivancos J. Spontaneous subarachnoid hemorrhage with negative angiography managed in a stroke unit: Clinical and prognostic characteristics. Journal of Stroke and Cerebrovascular Diseases. 2015; 24(11):2484-90. doi: 10.1016/j.jstrokecerebrovasdis.2015.06.011 [DOI:10.1016/j.jstrokecerebrovasdis.2015.06.011]
6. Cánovas D, Gil A, Jato M, de Miquel M, Rubio F. Clinical outcome of spontaneous non‐aneurysmal subarachnoid hemorrhage in 108 patients. European Journal of Neurology. 2012; 19(3):457-61. doi: 10.1111/j.1468-1331.2011.03542.x [DOI:10.1111/j.1468-1331.2011.03542.x]
7. Connors JL, Wojak J. Intracranial aneurysms; general considerations. In: Connors JL, Wojak JC, editors. Interventional Neuroradiology. Philadelphia: WB Saunders. 1998.
8. De Oliveira Manoel AL, Turkel-Parrella D, Germans M, Kouzmina E, da Silva Almendra P, Marotta T, et al. Safety of early pharmacological thromboprophylaxis after subarachnoid hemorrhage. The Canadian Journal of Neurological Sciences. 2014; 41(05):554-61. doi: 10.1017/cjn.2014.16 [DOI:10.1017/cjn.2014.16]
9. Dupont SA, Lanzino G, Wijdicks EF, Rabinstein AA. The use of clinical and routine imaging data to differentiate between aneurysmal and nonaneurysmal subarachnoid hemorrhage prior to angiography: Clinical article. Journal of Neurosurgery. 2010; 113(4):790-4. doi: 10.3171/2010.4.jns091932 [DOI:10.3171/2010.4.JNS091932]
10. El Khaldi M, Pernter P, Ferro F, Alfieri A, Decaminada N, Naibo L, et al. Detection of cerebral aneurysms in nontraumatic subarachnoid haemorrhage: Role of multislice CT angiography in 130 consecutive patients. La radiologia medica. 2007; 112(1):123-37. doi: 10.1007/s11547-007-0126-8 [DOI:10.1007/s11547-007-0126-8]
11. Elhadi AM, Zabramski JM, Almefty KK, Mendes GA, Nakaji P, McDougall CG, et al. Spontaneous subarachnoid hemorrhage of unknown origin: hospital course and long-term clinical and angiographic follow-up. Journal of Neurosurgery. 2015; 122(3):663-70. doi: 10.3171/2014.10.jns14175 [DOI:10.3171/2014.10.JNS14175]
12. Flaherty ML, Haverbusch M, Kissela B, Kleindorfer D, Schneider A, Sekar P, et al. Perimesencephalic subarachnoid hemorrhage: incidence, risk factors, and outcome. Journal of Stroke and Cerebrovascular Diseases. 2005; 14(6):267-71. doi: 10.1016/j.jstrokecerebrovasdis.2005.07.004 [DOI:10.1016/j.jstrokecerebrovasdis.2005.07.004]
13. Zhao J, Lin H, Summers R, Yang M, Cousins BG, Tsui J. Current treatment strategies for intracranial aneurysms: An overview. Angiology. 2017; 69(1):17-30. doi: 10.1177/0003319717700503 [DOI:10.1177/0003319717700503]
14. Fontanella M, Rainero I, Panciani PP, Schatlo B, Benevello C, Garbossa D, et al. Subarachnoid hemorrhage and negative angiography: Clinical course and long-term follow-up. Neurosurgical Review. 2011; 34(4):477-84. doi: 10.1007/s10143-011-0323-8 [DOI:10.1007/s10143-011-0323-8]
15. Halpin S, Britton J, Byrne J, Clifton A, Hart G, Moore A. Prospective evaluation of cerebral angiography and computed tomography in cerebral haematoma. Journal of Neurology, Neurosurgery & Psychiatry. 1994; 57(10):1180-6. doi: 10.1136/jnnp.57.10.1180 [DOI:10.1136/jnnp.57.10.1180]
16. Huttner H, Hartmann M, Köhrmann M, Neher M, Stippich C, Hähnel S, et al. Repeated digital substraction angiography after perimesencephalic subarachnoid hemorrhage? Journal of Neuroradiology. 2006; 33(2):87-9. doi: 10.1016/s0150-9861(06)77236-4 [DOI:10.1016/S0150-9861(06)77236-4]
17. Ildan F, Tuna M, Erman T, Göçer AI, Çetinalp E, Burgut R. Prognosis and prognostic factors for unexplained subarachnoid hemorrhage: review of 84 cases. Neurosurgery. 2002; 50(5):1015-25. doi: 10.1227/00006123-200205000-00015 [DOI:10.1227/00006123-200205000-00015]
18. Inamasu J, Nakamura Y, Saito R, Horiguchi T, Kuroshima Y, Mayanagi K, et al. "Occult" ruptured cerebral aneurysms revealed by repeat angiography: result from a large retrospective study. Clinical Neurology and Neurosurgery. 2003; 106(1):33-7. doi: 10.1016/j.clineuro.2003.09.002 [DOI:10.1016/j.clineuro.2003.09.002]
19. Ishihara H, Kato S, Akimura T, Suehiro E, Oku T, Suzuki M. Angiogram-negative subarachnoid hemorrhage in the era of three dimensional rotational angiography. Journal of Clinical Neuroscience. 2007; 14(3):252-5. doi: 10.1016/j.jocn.2006.01.011 [DOI:10.1016/j.jocn.2006.01.011]
20. Jung JY, Kim YB, Lee JW, Huh SK, Lee KC. Spontaneous subarachnoid haemorrhage with negative initial angiography: A review of 143 cases. Journal of Clinical Neuroscience. 2006; 13(10):1011-7. doi: 10.1016/j.jocn.2005.09.007 [DOI:10.1016/j.jocn.2005.09.007]
21. Kaim A, Proske M, Kirsch E, Weymarn Av, Radü EW, Steinbrich W. Value of repeat‐angiography in cases of unexplained Subarachnoid Hemorrhage (SAH). Acta Neurologica Scandinavica. 1996; 93(5):366-73. doi: 10.1111/j.1600-0404.1996.tb00011.x [DOI:10.1111/j.1600-0404.1996.tb00011.x]
22. Karttunen A, Jartti P, Ukkola V, Sajanti J, Haapea M. Value of the quantity and distribution of subarachnoid haemorrhage on CT in the localization of a ruptured cerebral aneurysm. Acta Neurochirurgica. 2003; 145(8):655-61. doi: 10.1007/s00701-003-0080-8 [DOI:10.1007/s00701-003-0080-8]
23. Kaufmann TJ, Huston III J, Mandrekar JN, Schleck CD, Thielen KR, Kallmes DF. Complications of diagnostic cerebral angiography: Evaluation of 19 826 consecutive patients 1. Radiology. 2007; 243(3):812-9. doi: 10.1148/radiol.2433060536 [DOI:10.1148/radiol.2433060536]
24. Khan A, Smith JS, Kirkman M, Robertson F, Wong K, Dott C, et al. Angiogram negative subarachnoid haemorrhage: outcomes and the role of repeat angiography. Clinical Neurology and Neurosurgery. 2013; 115(8):1470-5. doi: /10.1016/j.clineuro.2013.02.002
25. Kitkhuandee A, Thammaroj J, Munkong W, Duangthongpon P, Thanapaisal C. Cerebral angiographic findings in patients with non-traumatic subarachnoid hemorrhage. Journal of the Medical Association of Thailand. 2012; 95(11):S121-S9. PMID: 23961631 [PMID]
26. Konczalla J, Schmitz J, Kashefiolasl S, Senft C, Seifert V, Platz J. Non‐aneurysmal subarachnoid hemorrhage in 173 patients: a prospective study of long‐term outcome. European Journal of Neurology. 2015; 22(10):1329-36. doi: 10.1111/ene.12762 [DOI:10.1111/ene.12762]
27. Bhogal P, AlMatter M, Hellstern V, et al. Difference in aneurysm characteristics between ruptured and unruptured aneurysms in patients with multiple intracranial aneurysms. Surgical Neurology International. 2018;9:(1)1. doi: 10.4103/sni.sni_339_17 [DOI:10.4103/sni.sni_339_17]
28. Korja M, Silventoinen K, Laatikainen T, Jousilahti P, Salomaa V, Hernesniemi J, et al. Risk factors and their combined effects on the incidence rate of subarachnoid hemorrhage–a population-based cohort study. PLoS One. 2013;8(9):e73760. doi: 10.1371/journal.pone.0073760 [DOI:10.1371/journal.pone.0073760]
29. Little AS, Garrett M, Germain R, Farhataziz N, Albuquerque FC, McDougall CG, et al. Evaluation of patients with spontaneous subarachnoid hemorrhage and negative angiography. Neurosurgery. 2007; 61(6):1139-51. doi: 10.1227/01.neu.0000306091.30517.e7 [DOI:10.1227/01.neu.0000306091.30517.e7]
30. Moran CJ. Aneurysmal subarachnoid hemorrhage: DSA versus CT angiography—is the answer available? Radiology. 2011; 258(1):15-7. doi: 10.1148/radiol.101911 [DOI:10.1148/radiol.101911]
31. Prestigiacomo CJ, Sabit A, He W, Jethwa P, Gandhi C, Russin J. Three dimensional CT angiography versus digital subtraction angiography in the detection of intracranial aneurysms in subarachnoid hemorrhage. Journal of NeuroInterventional Surgery. 2010; 2(4):385-9. doi: 10.1136/jnis.2010.002246 [DOI:10.1136/jnis.2010.002246]
32. Sarabia R, Lagares A, Fernández-Alén J, Arikan F, Vilalta J, Ibá-ez J, et al. Idiopathic subarachnoid hemorrhage: a multicentre series of 220 patients. Neurocirugía. 2010; 21(6):441-51. doi: 10.1016/s1130-1473(10)70094-4 [DOI:10.1016/S1130-1473(10)70094-4]
33. Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. New England Journal of Medicine. 2006; 354(4):387-96. doi: 10.1056/nejmra052732 [DOI:10.1056/NEJMra052732]
34. Topcuoglu MA, Ogilvy CS, Carter BS, Buonanno FS, Koroshetz WJ, Singhal AB. Subarachnoid hemorrhage without evident cause on initial angiography studies: diagnostic yield of subsequent angiography and other neuroimaging tests. Journal of Neurosurgery. 2003; 98(6):1235-40. doi: 10.3171/jns.2003.98.6.1235 [DOI:10.3171/jns.2003.98.6.1235]
35. Vaitkevicius G, Gvazdaitis A, Lukosevicius S. [Spontaneous subarachnoid hemorrhage: Patients' examination after aneurysm-negative initial angiograms (Lithuanian)]. Medicina (Kaunas, Lithuania). 2001; 38(10):976-81. doi: PMID: 12532705
36. Hammer A, Steiner A, Kerry G, et al. Treatment of ruptured intracranial aneurysms yesterday and now. PLoS ONE. 2017;12(3):e0172837. doi: 10.1371/journal.pone.0172837 [DOI:10.1371/journal.pone.0172837]
37. Van Gijn J, Rinkel G. Subarachnoid haemorrhage: Diagnosis, causes and management. Brain. 2001; 124(2):249-78. doi: 10.1093/brain/124.2.249 [DOI:10.1093/brain/124.2.249]
38. Vega C, Kwoon JV, Lavine SD. Intracranial aneurysms: current evidence and clinical practice. American Family Physician. 2002; 66(4):601-8. PMID: 12201551 [PMID]
39. Vivancos J, Gilo F, Frutos R, Maestre J, García-Pastor A, Quintana F, et al. Clinical management guidelines for subarachnoid haemorrhage. Diagnosis and treatment. Neurología (English Edition). 2014; 29(6):353-70. doi: 10.1016/j.nrl.2012.07.009. [DOI:10.1016/j.nrl.2012.07.009]
40. Willinsky RA, Taylor SM, TerBrugge K, Farb RI, Tomlinson G, Montanera W. Neurologic complications of cerebral angiography: prospective analysis of 2,899 procedures and review of the literature 1. Radiology. 2003; 227(2):522-8. doi: 10.1148/radiol.2272012071 [DOI:10.1148/radiol.2272012071]
41. Yu DW, Jung YJ, Choi BY, Chang CH. Subarachnoid hemorrhage with negative baseline digital subtraction angiography: is repeat digital subtraction angiography necessary? Journal of Cerebrovascular and Endovascular Neurosurgery. 2012; 14(3):210-5. doi: 10.7461/jcen.2012.14.3.210 [DOI:10.7461/jcen.2012.14.3.210]
42. Zhu X, Chan M, Poon W. Spontaneous intracranial hemorrhage: which patients need diagnostic cerebral angiography? Stroke. 1997; 28(7):1406-9. doi: 10.1161/01.str.28.7.1406 [DOI:10.1161/01.STR.28.7.1406]
43. Firouznia K, Ghaanati H, Shabani Sm, Shakiba M. Subarachnoid hemorrhage; An an-giographic evaluation in Iran. Iranian Journal of Radiology. 2004; 2(1-2):28-33.
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |