Sun, Feb 22, 2026
Volume 1, Issue 2 (12-2015)
Iran J Neurosurg 2015, 1(2): 22-26 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Alijani B, Emamhadi M, Behzadnia H, Azar M, Kazemnejad-Leili E, Yousefzadeh-Chabok S, et al . Curb the Pain of Spondylolisthesis; Comparing Posterolateral Fusion with Posterior Lumbar Interbody Fusion. Iran J Neurosurg 2015; 1 (2) :22-26
URL: http://irjns.org/article-1-11-en.html
URL: http://irjns.org/article-1-11-en.html
Babak Alijani1 
 , Mohammadreza Emamhadi2
, Mohammadreza Emamhadi2 
 , Hamid Behzadnia1
, Hamid Behzadnia1 
 , Maziar Azar2
, Maziar Azar2 
 , Ehsan Kazemnejad-Leili3
, Ehsan Kazemnejad-Leili3 
 , Shahrokh Yousefzadeh-Chabok4
, Shahrokh Yousefzadeh-Chabok4 
 , Alireza Razzaghi5
, Alireza Razzaghi5 
 , Ali Aramnia *6
, Ali Aramnia *6 


 , Mohammadreza Emamhadi2
, Mohammadreza Emamhadi2 
 , Hamid Behzadnia1
, Hamid Behzadnia1 
 , Maziar Azar2
, Maziar Azar2 
 , Ehsan Kazemnejad-Leili3
, Ehsan Kazemnejad-Leili3 
 , Shahrokh Yousefzadeh-Chabok4
, Shahrokh Yousefzadeh-Chabok4 
 , Alireza Razzaghi5
, Alireza Razzaghi5 
 , Ali Aramnia *6
, Ali Aramnia *6 

1- MD, Assistant Professor of Neurosurgery, Neurosurgery Department, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Guilan, Iran
2- MD, Associate Professor of Neurosurgery, Neurosurgery Department, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Guilan, Iran
3- Ph.D, Associate Professor of Biostatistics, Guilan University of Medical Sciences, Rasht, Guilan, Iran
4- M.D, Professor of Neurosurgery, Guilan Road Trauma Research Center, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Guilan, Iran
5- MSc in Epidemiology, Guilan Road Trauma Research Center, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Guilan, Iran
6- MD, Chief Resident of Neurosurgery, Neurosurgery Department, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Guilan, Iran
2- MD, Associate Professor of Neurosurgery, Neurosurgery Department, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Guilan, Iran
3- Ph.D, Associate Professor of Biostatistics, Guilan University of Medical Sciences, Rasht, Guilan, Iran
4- M.D, Professor of Neurosurgery, Guilan Road Trauma Research Center, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Guilan, Iran
5- MSc in Epidemiology, Guilan Road Trauma Research Center, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Guilan, Iran
6- MD, Chief Resident of Neurosurgery, Neurosurgery Department, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Guilan, Iran
Full Text [PDF 504 kb]
(2131 Downloads)
| Abstract (HTML) (8802 Views)
Full Text: (2275 Views)
Introduction
Spondylolisthesis is defined as forward displacement of a vertebra over another vertebra (1). Nowadays, spondylolisthesis is the indication of lumbar fusion surgeries in 30% of cases. It can be categorized into 5 types. The degenerative type mostly affects L4-L5 level and is a more common problem in women, whereas the isthmic type more frequently involves the level of L5-S1 and is more prevalent in men. In the majority of symptomatic patients with spondylolisthesis, a mechanical low back pain that increases with activity is the primary complaint (2). 25% of patients with low grade spondylolisthesis do not respond to any type of non-surgical treatment (3). Patients in whom symptoms become unbearable and disrupt their daily function, patients undergoing a progressive course and patients with a neurological deficit are candidates of surgery (4,5). The commonly used accepted technique to reconstruct the affected segment is pedicle screw instrumentation but there is a considerable controversy about the surgical procedure of choice (4-11). PLF and PLIF are widely accepted fusion techniques (12). PLIF was firstly introduced by Cloward in 1940 (13-15). Some of the studies have represented the PLIF as the superior technique but comparable results of both techniques have been shown by other trials (12, 16-20). The aim of this study was to compare the two common techniques of fusion in terms of pain curb in patients with low grade degenerative and isthmic spondylolisthesis.
Methods and Materials/Patients
This prospective observational study involved 102 patients with isthmic and degenerative spondylolisthesis of low grade who were admitted to Neurosurgical Department of Poursina Hospital, Guilan, Iran between 2012 and 2014. Patients were studied in two groups. Group A included 51 patients in whom the used fusion technique was PLF and group B composed of 51 patients who were operated on with PLIF. Pedicle screw fixation was the applied technique for reconstruction of the affected segment in both groups. Surgeries were carried out by a single team consisted of an associate professor of neurosurgery, an assistant professor of neurosurgery and a neurosurgical resident affiliated with Guilan University of Medical Science (GUMS). Inclusion criteria were as follows: patients with degenerative and isthmic type spondylolisthesis of grade 1 and 2 who failed to respond to conservative therapy and aged between 18 and 75. Patients who reported any prior spinal surgery for spondylolisthesis or had a history of alcohol abuse and patients with an inadequate disk space for performing PLIF were excluded. This study was approved by Ethical Committee of GUMS and all patients signed a written consent form. A questionnaire containing VAS scores was used to measure the pain in patients before exposing the patients to surgical treatment (PLF and PLIF). Moreover, thorough physical examination was done and all of the related signs and symptoms were recorded under supervision of a resident of neurosurgery. In the operation room, all patients were positioned prone. After a midline incision and complete bony exposure, subperiosteal dissection continued till transverse processes were exposed. Decompressive procedure was done thorough laminectomy, medial facetectomy and extensive foraminotomy. Then after three level pedicle screw fixation (one level above and one level below), in PLF group (A), posterolateral fusion was done by autografting with bone chips and in PLIF group (B), after a complete discectomy, lumbar interbody fusion was done by PEEK cages. A brace was prescribed for 3 months and then was tapered off if fusion was achieved. All the patients were informed of a scheduled follow up program explained by residents and they were asked to complete the same questionnaire using VAS scores in the day after surgery, after 6 months and after 1 year. Statistical analysis was done using Repeated Measure ANOVA with post hoc tests (Bonferoni method) of SPSS (Version 21). All of the tests were two tailed and a p-value<0.05 was considered to be statistically significant.
Spondylolisthesis is defined as forward displacement of a vertebra over another vertebra (1). Nowadays, spondylolisthesis is the indication of lumbar fusion surgeries in 30% of cases. It can be categorized into 5 types. The degenerative type mostly affects L4-L5 level and is a more common problem in women, whereas the isthmic type more frequently involves the level of L5-S1 and is more prevalent in men. In the majority of symptomatic patients with spondylolisthesis, a mechanical low back pain that increases with activity is the primary complaint (2). 25% of patients with low grade spondylolisthesis do not respond to any type of non-surgical treatment (3). Patients in whom symptoms become unbearable and disrupt their daily function, patients undergoing a progressive course and patients with a neurological deficit are candidates of surgery (4,5). The commonly used accepted technique to reconstruct the affected segment is pedicle screw instrumentation but there is a considerable controversy about the surgical procedure of choice (4-11). PLF and PLIF are widely accepted fusion techniques (12). PLIF was firstly introduced by Cloward in 1940 (13-15). Some of the studies have represented the PLIF as the superior technique but comparable results of both techniques have been shown by other trials (12, 16-20). The aim of this study was to compare the two common techniques of fusion in terms of pain curb in patients with low grade degenerative and isthmic spondylolisthesis.
Methods and Materials/Patients
This prospective observational study involved 102 patients with isthmic and degenerative spondylolisthesis of low grade who were admitted to Neurosurgical Department of Poursina Hospital, Guilan, Iran between 2012 and 2014. Patients were studied in two groups. Group A included 51 patients in whom the used fusion technique was PLF and group B composed of 51 patients who were operated on with PLIF. Pedicle screw fixation was the applied technique for reconstruction of the affected segment in both groups. Surgeries were carried out by a single team consisted of an associate professor of neurosurgery, an assistant professor of neurosurgery and a neurosurgical resident affiliated with Guilan University of Medical Science (GUMS). Inclusion criteria were as follows: patients with degenerative and isthmic type spondylolisthesis of grade 1 and 2 who failed to respond to conservative therapy and aged between 18 and 75. Patients who reported any prior spinal surgery for spondylolisthesis or had a history of alcohol abuse and patients with an inadequate disk space for performing PLIF were excluded. This study was approved by Ethical Committee of GUMS and all patients signed a written consent form. A questionnaire containing VAS scores was used to measure the pain in patients before exposing the patients to surgical treatment (PLF and PLIF). Moreover, thorough physical examination was done and all of the related signs and symptoms were recorded under supervision of a resident of neurosurgery. In the operation room, all patients were positioned prone. After a midline incision and complete bony exposure, subperiosteal dissection continued till transverse processes were exposed. Decompressive procedure was done thorough laminectomy, medial facetectomy and extensive foraminotomy. Then after three level pedicle screw fixation (one level above and one level below), in PLF group (A), posterolateral fusion was done by autografting with bone chips and in PLIF group (B), after a complete discectomy, lumbar interbody fusion was done by PEEK cages. A brace was prescribed for 3 months and then was tapered off if fusion was achieved. All the patients were informed of a scheduled follow up program explained by residents and they were asked to complete the same questionnaire using VAS scores in the day after surgery, after 6 months and after 1 year. Statistical analysis was done using Repeated Measure ANOVA with post hoc tests (Bonferoni method) of SPSS (Version 21). All of the tests were two tailed and a p-value<0.05 was considered to be statistically significant.
Results
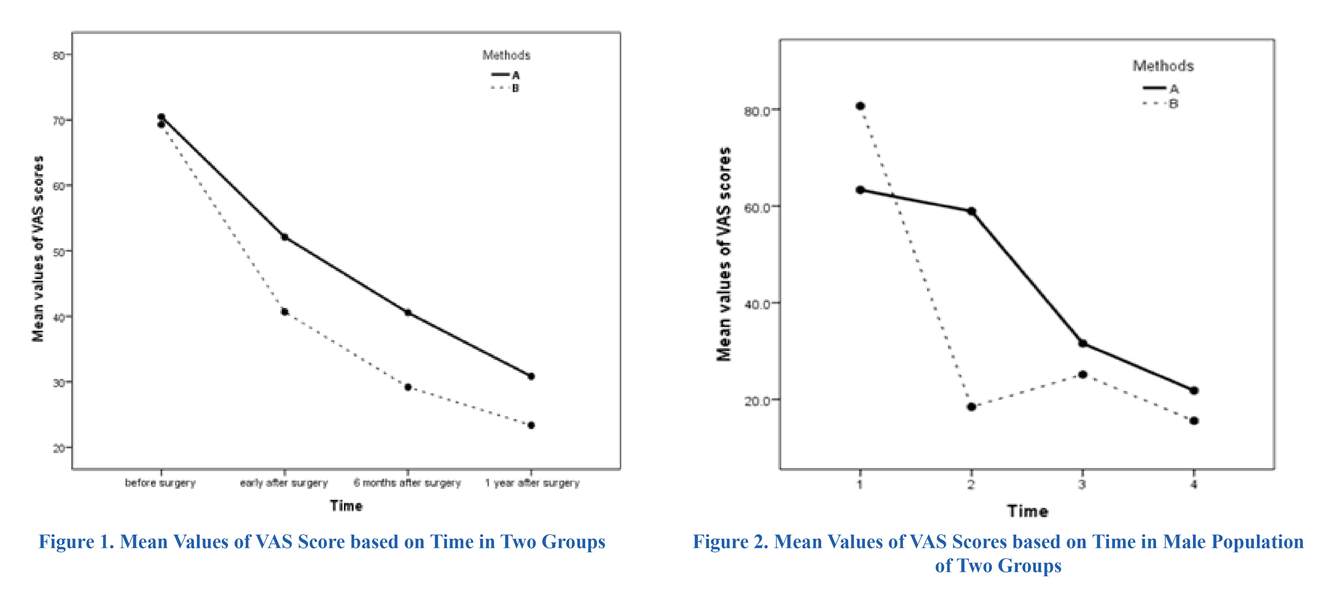
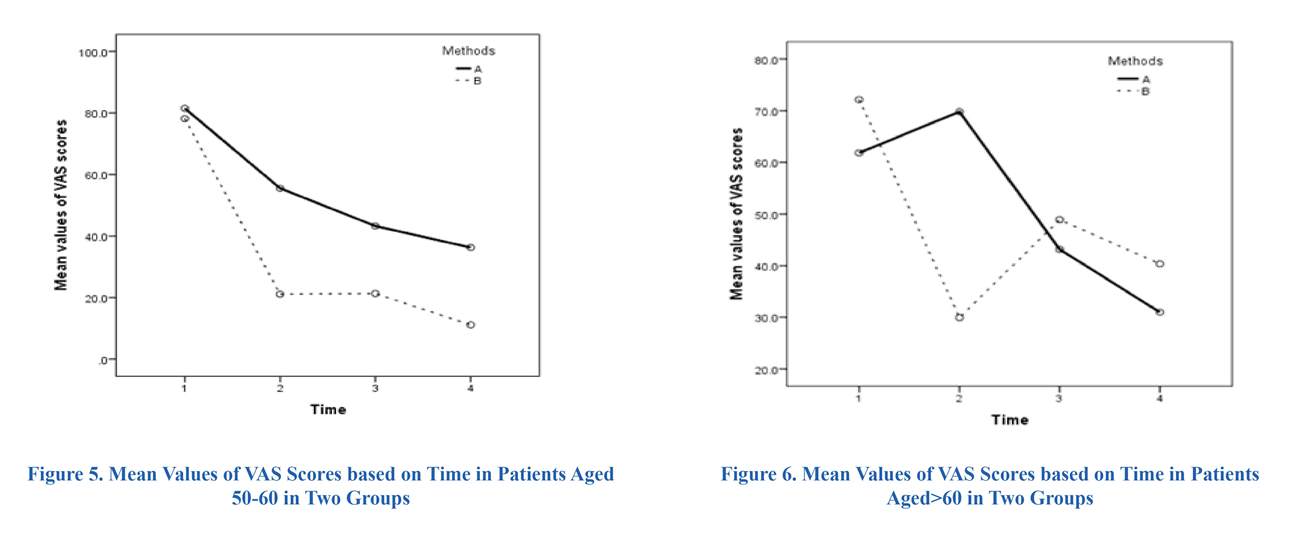
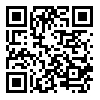
At beginning of study, a total of 102 patients with low grade spondylolisthesis of isthmic and degenerative type were entered into our study including 51 patients in group A (PLF) and 51 patients in group B (PLIF). Of 102 patients, 15 patients dropped out due to incomplete follow-up and one patient died due to cardiovascular disease. Finally, 86 patients, 45 patients in group A (PLF) and 41 patients in group B (PLIF), were studied. The mean age in patients of group A and B was 55.1±9.0 and 52.1±8.0, respectively. This observed difference between the two groups was not statistically significant (p>0.05). Based on distribution of types of spondylolistesis, the proportion of degenerative I and II and Isthmic I in patients group A (PLF) was more than patients group B (PLIF). These observed differences in proportion between two groups were statistically significant (Table 1). The most common clinical presentation was a combination of low back pain, radiculopathy, paresthesia and positive Straight leg raising test (SLR) with a prevalence of 22.2% (10 patients) in group A and 19.5% (8 patients) in groups B. The mean values of VAS scores before surgery, the day after surgery and one year later showed no significant difference between the groups but the difference in mean values after 6 months of surgery turned to be statistically significant (Table 2). Analyzing the course of VAS scores over the study period using repeated measure ANOVA, both groups followed a descending pattern that was statistically significant for both of them (p<0.0001) (Table 2) (Figure 1). Comparison of the overall mean of VAS scores in two groups over the whole period of study showed that the mean of VAS score in group A (48.49±4.39) was higher than group B (41.02±3.41). This observed mean difference was statistically significant (p<0.05). For each group, mean values of VAS scores before surgery represented a significant difference compared to the value of the day after surgery, 6 months later and one year after surgery. Comparisons of mean values of VAS scores at different points in times have been illustrated in Table 3. The interaction of sex and age with the courses of mean values of VAS scores during the study period has been displayed in Figures 2 to 6. Analyzing the interactions using two ways ANOVA revealed a significant effect of sex and insignificant effect of age on the course of VAS scores related to two methods of surgery (p<0.05 and p>0.05, respectively).
Discussion
In our study, both methods of fusion resulted in a remarkable decrease of VAS scores after one year of follow-up. Compared with PLF group, PLIF group reported a less degree of pain which was of statistical significance. Measuring and comparing the pain between two groups at four points in time showed a confusing result. After six months of surgery, PLIF turned to be the superior method in curbing the pain. Although the mean value of VAS related to PLIF group was lower than the PLF group during the whole period of study, this difference was not significant early after surgery and one year later. The very similar mean scores of VAS between groups before the surgery could serve as a rationalization to justify the non-significant difference of VAS values between groups the day after surgery. The effect of fusion techniques on VAS scores in age groups was similar but considering the gender, the effect of surgical methods on VAS score in men differed from women. In Ekman P et al. ´s study (2007) on a population including 163 patients with isthmic spondylolisthesis, pain index was measured before surgery, at 1 year, and 2 years of follow-up. Similar to our study, the pain index had a significant decline from pre-operative
At beginning of study, a total of 102 patients with low grade spondylolisthesis of isthmic and degenerative type were entered into our study including 51 patients in group A (PLF) and 51 patients in group B (PLIF). Of 102 patients, 15 patients dropped out due to incomplete follow-up and one patient died due to cardiovascular disease. Finally, 86 patients, 45 patients in group A (PLF) and 41 patients in group B (PLIF), were studied. The mean age in patients of group A and B was 55.1±9.0 and 52.1±8.0, respectively. This observed difference between the two groups was not statistically significant (p>0.05). Based on distribution of types of spondylolistesis, the proportion of degenerative I and II and Isthmic I in patients group A (PLF) was more than patients group B (PLIF). These observed differences in proportion between two groups were statistically significant (Table 1). The most common clinical presentation was a combination of low back pain, radiculopathy, paresthesia and positive Straight leg raising test (SLR) with a prevalence of 22.2% (10 patients) in group A and 19.5% (8 patients) in groups B. The mean values of VAS scores before surgery, the day after surgery and one year later showed no significant difference between the groups but the difference in mean values after 6 months of surgery turned to be statistically significant (Table 2). Analyzing the course of VAS scores over the study period using repeated measure ANOVA, both groups followed a descending pattern that was statistically significant for both of them (p<0.0001) (Table 2) (Figure 1). Comparison of the overall mean of VAS scores in two groups over the whole period of study showed that the mean of VAS score in group A (48.49±4.39) was higher than group B (41.02±3.41). This observed mean difference was statistically significant (p<0.05). For each group, mean values of VAS scores before surgery represented a significant difference compared to the value of the day after surgery, 6 months later and one year after surgery. Comparisons of mean values of VAS scores at different points in times have been illustrated in Table 3. The interaction of sex and age with the courses of mean values of VAS scores during the study period has been displayed in Figures 2 to 6. Analyzing the interactions using two ways ANOVA revealed a significant effect of sex and insignificant effect of age on the course of VAS scores related to two methods of surgery (p<0.05 and p>0.05, respectively).
Discussion
In our study, both methods of fusion resulted in a remarkable decrease of VAS scores after one year of follow-up. Compared with PLF group, PLIF group reported a less degree of pain which was of statistical significance. Measuring and comparing the pain between two groups at four points in time showed a confusing result. After six months of surgery, PLIF turned to be the superior method in curbing the pain. Although the mean value of VAS related to PLIF group was lower than the PLF group during the whole period of study, this difference was not significant early after surgery and one year later. The very similar mean scores of VAS between groups before the surgery could serve as a rationalization to justify the non-significant difference of VAS values between groups the day after surgery. The effect of fusion techniques on VAS scores in age groups was similar but considering the gender, the effect of surgical methods on VAS score in men differed from women. In Ekman P et al. ´s study (2007) on a population including 163 patients with isthmic spondylolisthesis, pain index was measured before surgery, at 1 year, and 2 years of follow-up. Similar to our study, the pain index had a significant decline from pre-operative
period till 2 years after surgery but unlike our study, no statistical difference was observed in pain at any time interval between the PLIF and PLF groups. Pain was reported not to be significantly different between sexes in this study (17). Cheng et al. conducted a prospective study on 138 patients with spondylolisthesis in 2009. They concluded that VAS score after 4th year was less than the pre-operative period in both PLIF and PLF groups, however, unlike what we concluded, no statistical difference between two groups was seen (4). In 2010, Bròdano et al. in their study on 71 patients with low grade isthmic spondylolisthesis showed that both PLIF and PLF techniques had an acceptable clinical outcome but without statistically significant differences. They assessed
clinical outcome and to define it, what they used was ODI, RMDQ (Roland Morris Disability questionnaire), VAS (leg score and back score), persistent low back pain and persistent sciatica (20, 21). Unlike our study, they did not assess pain separately. Three years later in a meta-analysis by Ye et al. they revealed that three of five studies used VAS to evaluate low back pain, radicular pain or leg pain reduction in PLF and PLIF treated groups (0.5-6 years follow-up). Pain relief over time significantly improved in PLF and PLIF groups (3). In a recent study on 50 patients with lumbar ishmicspondylolisthesis, Habib (2014) also used visual analogue scale to study pain. He demonstrated a significant better long-term VAS score for back pain in PLIF group. A follow-up program of 18 months was scheduled for patients (12). His findings were in consistent with the results of our study. Because the surgery of choice for spondylolisthesis is the field of conflict and pain control in these patients is an important target of management, our findings may hold a clue to the better fusion technique. The limitation of our study was that the two groups were not matched in terms of the level of spondylolisthesis which can act as a confounder.
Conclusion
As well as the substantial reduction of pain resulted by both of techniques, marked post-operative pain relief in PLIF group was noteworthy.
Acknowledgment
The authors offer their special thanks to the Clinical Research Development Unit of Poursina Hospital, Guilan University of Medical Sciences, Rasht, Guilan, Iran.
Funding
None.
Conflicts of Interest
The authors report no conflict of interest.
References
Conclusion
As well as the substantial reduction of pain resulted by both of techniques, marked post-operative pain relief in PLIF group was noteworthy.
Acknowledgment
The authors offer their special thanks to the Clinical Research Development Unit of Poursina Hospital, Guilan University of Medical Sciences, Rasht, Guilan, Iran.
Funding
None.
Conflicts of Interest
The authors report no conflict of interest.
References
- Inamdar D, Alagappan M, Shyam L, Devadoss S, Devadoss A. Posterior lumbar interbody fusion versus intertransverse fusion in the treatment of lumbar spondylolisthesis. Journal of Orthopaedic Surgery. 2006;14(1).
- Winn H. Textbook of Neurological Surgery. Philadelphia: Elsevier Saunders; 2011.
- Ye Y-P, Xu H, Chen D. Comparison between posterior lumbar interbody fusion and posterolateral fusion with transpedicular screw fixation for isthmic spondylolithesis: a meta-analysis. Archives of orthopaedic and trauma surgery. 2013;133(12):1649-55.
- Cheng L, Nie L, Zhang L. Posterior lumbar interbody fusion versus posterolateral fusion in spondylolisthesis: a prospective controlled study in the Han nationality. International orthopaedics. 2009;33(4):1043-7.
- Dai L, Jia L, Yuan W, Ni B, Zhu H. Direct repair of defect in lumbar spondylolysis and mild isthmic spondylolisthesis by bone grafting, with or without facet joint fusion. European Spine Journal. 2001;10(1):78-83.
- Boos N, Webb J. Pedicle screw fixation in spinal disorders: a European view. European Spine Journal. 1997;6(1):2-18.
- Boos N, Marchesi D, Zuber K, Aebi M. Treatment of Severe Spondylolisthesis by Reduction and Pedicular Fixation: A 4-6-Year Follow-Up Study. Spine. 1993;18(12):1655-61.
- Dickman CA, Fessler RG, MacMillan M, Haid RW. Transpedicular screw-rod fixation of the lumbar spine: operative technique and outcome in 104 cases. Journal of neurosurgery. 1992;77(6):860-70.
- La Rosa G, Conti A, Cacciola F, Cardali S, La Torre D, Gambadauro NM, et al. Pedicle screw fixation for isthmic spondylolisthesis: does posterior lumbar interbody fusion improve outcome over posterolateral fusion? Journal of Neurosurgery: Spine. 2003;99(2):143-50.
- Thalgott JS, Aebi M. Manual of internal fixation of the spine: Lippincott Williams & Wilkins; 1996.
- Yuan HA, Garfin SR, Dickman CA, Mardjetko SM. A Historical Cohort Study of Pedicle Screw Fixation in Thoracic, Lumbar, and Sacral Spinal Fusion. Spine. 1994;19(20):2279S-96S.
- Habib H. Posterolateral fusion versus posterior interbody fusion in adult lumbar isthmic spondylolisthesis. Menoufia Medical Journal. 2014;27(1):191.
- Audat Z, Moutasem O, Yousef K, Mohammad B. Comparison of clinical and radiological results of posterolateral fusion, posterior lumbar interbody fusion and transforaminal lumbar interbody fusion techniques in the treatment of degenerative lumbar spine. Singapore medical journal. 2012;53(3):183-7.
- Cloward RB. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion: I. Indications, operative technique, after care. Journal of neurosurgery. 1953;10(2):154-68.
- Lin PM. A technical modification of Cloward's posterior lumbar interbody fusion. Neurosurgery. 1977;1(2):118-24.
- Aoki Y, Yamagata M, Ikeda Y, Nakajima F, Ohtori S, Nakagawa K, et al. A prospective randomized controlled study comparing transforaminal lumbar interbody fusion techniques for degenerative spondylolisthesis: unilateral pedicle screw and 1 cage versus bilateral pedicle screws and 2 cages: clinical article. Journal of Neurosurgery: Spine. 2012;17(2):153-9.
- Ekman P, Möller H, Tullberg T, Neumann P, Hedlund R. Posterior lumbar interbody fusion versus posterolateral fusion in adult isthmic spondylolisthesis. Spine. 2007;32(20):2178-83.
- Xiuxin H, Yue Z, Cui C, Yajun W. A meta-analysis of circumferential fusion versus instrumented posterolateral fusion in the lumbar spine. Spine. 2009;34(17):E618-E25.
- Kim K-T, Lee S-H, Lee Y-H, Bae S-C, Suk K-S. Clinical outcomes of 3 fusion methods through the posterior approach in the lumbar spine. Spine. 2006;31(12):1351-7.
- Zhou Z-J, Zhao F-D, Fang X-Q, Zhao X, Fan S-W. Meta-analysis of instrumented posterior interbody fusion versus instrumented posterolateral fusion in the lumbar spine: A review. Journal of Neurosurgery: Spine. 2011;15(3):295-310.
- Bròdano GB, Lolli F, Martikos K, Gasbarrini A, Bandiera S, Greggi T, et al. Fueling the debate: Are outcomes better after posterior lumbar interbody fusion (PLIF) or after posterolateral fusion (PLF) in adult patients with low-grade adult isthmic spondylolisthesis? Evidence-based spine-care journal. 2010;1(1):29
Type of Study: Research |
Subject:
Gamma Knife Radiosurgery
References
1. Inamdar D, Alagappan M, Shyam L, Devadoss S, Devadoss A. Posterior lumbar interbody fusion versus intertransverse fusion in the treatment of lumbar spondylolisthesis. Journal of Orthopaedic Surgery. 2006;14(1).
2. Winn H. Textbook of Neurological Surgery. Philadelphia: Elsevier Saunders; 2011.
3. Ye Y-P, Xu H, Chen D. Comparison between posterior lumbar interbody fusion and posterolateral fusion with transpedicular screw fixation for isthmic spondylolithesis: a meta-analysis. Archives of orthopaedic and trauma surgery. 2013;133(12):1649-55. [DOI:10.1007/s00402-013-1868-5] [PMID] [PMCID]
4. Cheng L, Nie L, Zhang L. Posterior lumbar interbody fusion versus posterolateral fusion in spondylolisthesis: a prospective controlled study in the Han nationality. International orthopaedics. 2009;33(4):1043-7. [DOI:10.1007/s00264-008-0588-x] [PMID] [PMCID]
5. Dai L, Jia L, Yuan W, Ni B, Zhu H. Direct repair of defect in lumbar spondylolysis and mild isthmic spondylolisthesis by bone grafting, with or without facet joint fusion. European Spine Journal. 2001;10(1):78-83. [DOI:10.1007/s005860000205] [PMID] [PMCID]
6. Boos N, Webb J. Pedicle screw fixation in spinal disorders: a European view. European Spine Journal. 1997;6(1):2-18.
https://doi.org/10.1007/BF00307823 [DOI:10.1007/BF01676569] [PMID] [PMCID]
7. Boos N, Marchesi D, Zuber K, Aebi M. Treatment of Severe Spondylolisthesis by Reduction and Pedicular Fixation: A 4-6-Year Follow-Up Study. Spine. 1993;18(12):1655-61. [DOI:10.1097/00007632-199309000-00014] [PMID]
8. Dickman CA, Fessler RG, MacMillan M, Haid RW. Transpedicular screw-rod fixation of the lumbar spine: operative technique and outcome in 104 cases. Journal of neurosurgery. 1992;77(6):860-70. [DOI:10.3171/jns.1992.77.6.0860] [PMID]
9. La Rosa G, Conti A, Cacciola F, Cardali S, La Torre D, Gambadauro NM, et al. Pedicle screw fixation for isthmic spondylolisthesis: does posterior lumbar interbody fusion improve outcome over posterolateral fusion? Journal of Neurosurgery: Spine. 2003;99(2):143-50. [DOI:10.3171/spi.2003.99.2.0143]
10. Thalgott JS, Aebi M. Manual of internal fixation of the spine: Lippincott Williams & Wilkins; 1996.
11. Yuan HA, Garfin SR, Dickman CA, Mardjetko SM. A Historical Cohort Study of Pedicle Screw Fixation in Thoracic, Lumbar, and Sacral Spinal Fusion. Spine. 1994;19(20):2279S-96S. [DOI:10.1097/00007632-199410151-00005] [PMID]
12. Habib H. Posterolateral fusion versus posterior interbody fusion in adult lumbar isthmic spondylolisthesis. Menoufia Medical Journal. 2014;27(1):191. [DOI:10.4103/1110-2098.132800]
13. Audat Z, Moutasem O, Yousef K, Mohammad B. Comparison of clinical and radiological results of posterolateral fusion, posterior lumbar interbody fusion and transforaminal lumbar interbody fusion techniques in the treatment of degenerative lumbar spine. Singapore medical journal. 2012;53(3):183-7. [PMID]
14. Cloward RB. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion: I. Indications, operative technique, after care. Journal of neurosurgery. 1953;10(2):154-68. [DOI:10.3171/jns.1953.10.2.0154] [PMID]
15. Lin PM. A technical modification of Cloward's posterior lumbar interbody fusion. Neurosurgery. 1977;1(2):118-24.
https://doi.org/10.1227/00006123-197709000-00006 [DOI:10.1097/00006123-197709000-00006] [PMID]
16. Aoki Y, Yamagata M, Ikeda Y, Nakajima F, Ohtori S, Nakagawa K, et al. A prospective randomized controlled study comparing transforaminal lumbar interbody fusion techniques for degenerative spondylolisthesis: unilateral pedicle screw and 1 cage versus bilateral pedicle screws and 2 cages: clinical article. Journal of Neurosurgery: Spine. 2012;17(2):153-9. [DOI:10.3171/2012.5.SPINE111044] [PMID]
17. Ekman P, Möller H, Tullberg T, Neumann P, Hedlund R. Posterior lumbar interbody fusion versus posterolateral fusion in adult isthmic spondylolisthesis. Spine. 2007;32(20):2178-83. [DOI:10.1097/BRS.0b013e31814b1bd8] [PMID]
18. Xiuxin H, Yue Z, Cui C, Yajun W. A meta-analysis of circumferential fusion versus instrumented posterolateral fusion in the lumbar spine. Spine. 2009;34(17):E618-E25. [DOI:10.1097/BRS.0b013e3181a9beab] [PMID]
19. Kim K-T, Lee S-H, Lee Y-H, Bae S-C, Suk K-S. Clinical outcomes of 3 fusion methods through the posterior approach in the lumbar spine. Spine. 2006;31(12):1351-7. [DOI:10.1097/01.brs.0000218635.14571.55] [PMID]
20. Zhou Z-J, Zhao F-D, Fang X-Q, Zhao X, Fan S-W. Meta-analysis of instrumented posterior interbody fusion versus instrumented posterolateral fusion in the lumbar spine: A review. Journal of Neurosurgery: Spine. 2011;15(3):295-310. [DOI:10.3171/2011.4.SPINE10330] [PMID]
21. Bròdano GB, Lolli F, Martikos K, Gasbarrini A, Bandiera S, Greggi T, et al. Fueling the debate: Are outcomes better after posterior lumbar interbody fusion (PLIF) or after posterolateral fusion (PLF) in adult patients with low-grade adult isthmic spondylolisthesis? Evidence-based spine-care journal. 2010;1(1):29 [DOI:10.1055/s-0028-1100890] [PMID] [PMCID]
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |


.jpg)