Sun, Feb 22, 2026
Volume 7, Issue 4 (Autumn 2021)
Iran J Neurosurg 2021, 7(4): 171-178 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Saadat S, Vaghari M, Hoodinshad S, Isanazar A, Hosseininezhad M. Depression and Anxiety in Patients With Multiple Sclerosis: A Systematic Review. Iran J Neurosurg 2021; 7 (4) :171-178
URL: http://irjns.org/article-1-283-en.html
URL: http://irjns.org/article-1-283-en.html
Sajjad Saadat1 

 , Maryam Vaghari2
, Maryam Vaghari2 

 , Shahrzad Hoodinshad3
, Shahrzad Hoodinshad3 

 , Adele Isanazar4
, Adele Isanazar4 

 , Mozaffar Hosseininezhad *5
, Mozaffar Hosseininezhad *5 




 , Maryam Vaghari2
, Maryam Vaghari2 

 , Shahrzad Hoodinshad3
, Shahrzad Hoodinshad3 

 , Adele Isanazar4
, Adele Isanazar4 

 , Mozaffar Hosseininezhad *5
, Mozaffar Hosseininezhad *5 


1- Neuroscience Research Center, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
2- Department of Psychology, Faculty of Humanities, Rasht Branch, Islamic Azad University, Rasht, Iran
3- Department of Psychology, Faculty of Humanities, Tehran North Branch, Islamic Azad University, Tehran, Iran
4- Department of Psychiatry, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
5- Department of Neurology, Neuroscience Research Center, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran ,hosseininezhadm@gmail.com
2- Department of Psychology, Faculty of Humanities, Rasht Branch, Islamic Azad University, Rasht, Iran
3- Department of Psychology, Faculty of Humanities, Tehran North Branch, Islamic Azad University, Tehran, Iran
4- Department of Psychiatry, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
5- Department of Neurology, Neuroscience Research Center, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran ,
Full Text [PDF 701 kb]
(2095 Downloads)
| Abstract (HTML) (4135 Views)
Full Text: (3602 Views)
1. Introduction
Multiple Sclerosis (MS) is among the most prevalent neurological diseases. Moreover, this chronic disease involves multiple areas of the central nervous system as one of its main features. The disease is prevalent in 20- to 40-year-old individuals. It also continues for years by developing incapacitating symptoms; eventually, MS causes serious psychosocial health issues [1]. Patients with MS experience an all-inclusive range of movement limitations, pain, chronic fatigue, memory impairment, and concentration problems daily [2]. Consequently, MS influences all fields of a subject's life, including employment, relationships, leisure, and daily activities [3]. Accordingly, these limitations and disabilities might highly influence the experience of unpleasant emotions and the development of mood and anxiety disorders in them [4].
There is no remedy for MS and it is usually diagnosed early in life; thus, these patients live with these challenging symptoms for multiple years [5]. Patients with MS encounter higher levels of mental disorders, such as depression, stress, and anxiety, compared with the healthy population and those with other chronic conditions. These symptoms may directly result from the inflammation and demyelination of the nervous system [6]. The most valid study in a large sample using Magnetic Resonance Imaging (MRI) indicated that individuals with MS had "more hyperintense lesions in the left inferior medial frontal regions and greater atrophy of the left anterior temporal regions". These two areas of the brain predict 42% of the variance in depression in individuals with MS [7]. The relationship between depressive symptoms and disease-modifying therapies, especially interferon-β, remains contradictory [8]. However, a meta-analysis reported no significant relationship between depression and interferon-β treatment in MS; a history of depression is an important risk factor for depressive syndrome in interferon-β treatment [9]. Consequently, Major Depressive Disorder (MDD) has been reported in up to 50% of MS patients while it has been estimated to range from 10% to 15% in the general population [1, 10]. Studies have also revealed that patients with MS experience high levels of anxiety (about 36%-54%) and approximately 30% of patients with MS develop generalized anxiety disorder [11].
There is a complicated relationship between mental disorders and MS; its frequency can be a reaction to several factors. Moreover, physical symptoms such as fatigue, disability, the experience of family problems, work, and social life result in the recurrence of psychological symptoms; consequently, it leads to an increase in the pressure of chronic disease [12]. The relationship between depressed mood and the prevalent symptoms of MS was supported by several studies. Studies almost revealed a mutual relationship between depression and MS symptoms worldwide [13]. Some researchers have assigned the prevalence of depressive disorders in MS patients to the symptoms of chronic fatigue, cognitive disorders, and pain experience; it is assumed that perceived fatigue and disability, as well as pain, can expedite depression [14]. It was determined that nearly half of MS patients experience cognitive disorders. The speed to process the information, attention and concentration, memory, and executive function is considered as the most significant cognitive disorders experienced by MS patients. The symptoms of cognitive disorders can cause extensive difficulties in individual and social functioning that might cause depression [15]. Furthermore, depression and anxiety in patients with MS cause different psychosocial risk factors including inadequate coping or poor social support or MS-related biological processes such as changes in brain structure or immunological and inflammatory pathways [16]. The most concerning issue in this field indicates a high risk of suicide in patients with MS and comorbid depressive symptoms. Evidence implies that the risk of suicide in depressed patients with MS is between 1.6 and 2.3 times higher than that in the general population. Additionally, approximately a quarter of patients with MS permanently contemplate suicide [17].
MDD is highly significant in patients with MS; however, anxiety has been less considered in this disease. Several studies have been conducted in this field and suggested that approximately 25%-41% of patients with MS are anxious. The clinical interview structure was applied only in two studies to evaluate the diagnosis of anxiety; consequently, both investigations reached the rate of 36% in patients. Generally, an anxiety score of up to 18.6% is normal in MS patients. Those patients who develop anxiety are frequently women with depression who contemplate suicide [18].
Examining the conducted studies revealed that the quality of life in depressed patients with MS is extremely lower than that in patients who are not depressed; even if nervous disabilities and fatigue are controlled. Depression unpleasantly affects MS patients. Depressed patients with MS experience the bewilderment of social and family support. Besides, there is even evidence that depression stops self-management behaviors in these patients [19]. Furthermore, depression and anxiety in patients with MS are associated with poor quality of life, cognitive dysfunction, increased risk of suicide, and occupational problems [18]. Depression and anxiety in MS appear to become more serious over time. It can be frequently treated at the beginning, i.e., significant to diagnose the disease early. Moreover, precisely examining and identifying psychological disorders, such as anxiety and depression in patients with MS play an effective role in developing treatment programs to reduce these disorders. Accordingly, this review study examined depression and anxiety in patients with MS.
2. Methods and Materials/Patients
This was a systematic review. We searched 4 online databases (PsycNET, PubMed, Scopus, and Magiran). Searches were performed applying the following keywords: “multiple sclerosis, MS, psychiatric issues, psychological disorders, psychological problems, anxiety, mental health, quality of life, and depression”. The search was performed in each database after conducting specific filters (publication date, title/abstract, and article type). For example, the search was conducted based on the Medical Subject Heading (MeSH) in the PubMed database. We first searched the keyword “multiple sclerosis” by applying restrictions (all time from 2010 to 2020 and title/abstract). There was no limitation in the research design of the studies and quantitative and qualitative studies were analyzed. We removed duplicates after identifying the studies and examined the results based on titles and abstracts. Full texts were examined for the qualified studies of retrieval and additional inclusion and exclusion criteria.
If these studies reported experiences or psychological consequences (anxiety & depression) observed in patients with MS, they could be the inclusion criteria. The exclusion criteria were as follows: studies which had evaluated psychological consequences in patients with other disorders (Not MS), non-original studies (systematic review, etc.), studies based on clinical intervention, studies written in languages other than English or Persian, studies which aimed at developing and validating scales, studies which had examined acute stress, studies which only had examined the linear relationships between the variables and studies which did not report the frequency of disorders. The two arbitrators evaluated the papers according to the inclusion criteria. The second arbitrator examined and approved the papers and the disputes were resolved through discussion. Figure 1 shows the search process. The critical appraisal was performed by two psychologists based on 3 indicators; evaluating the validity of selected articles, interpreting the results, and applying the results to clinical situations.
3. Results
Table 1 explains the results of analyzing 14 studies.
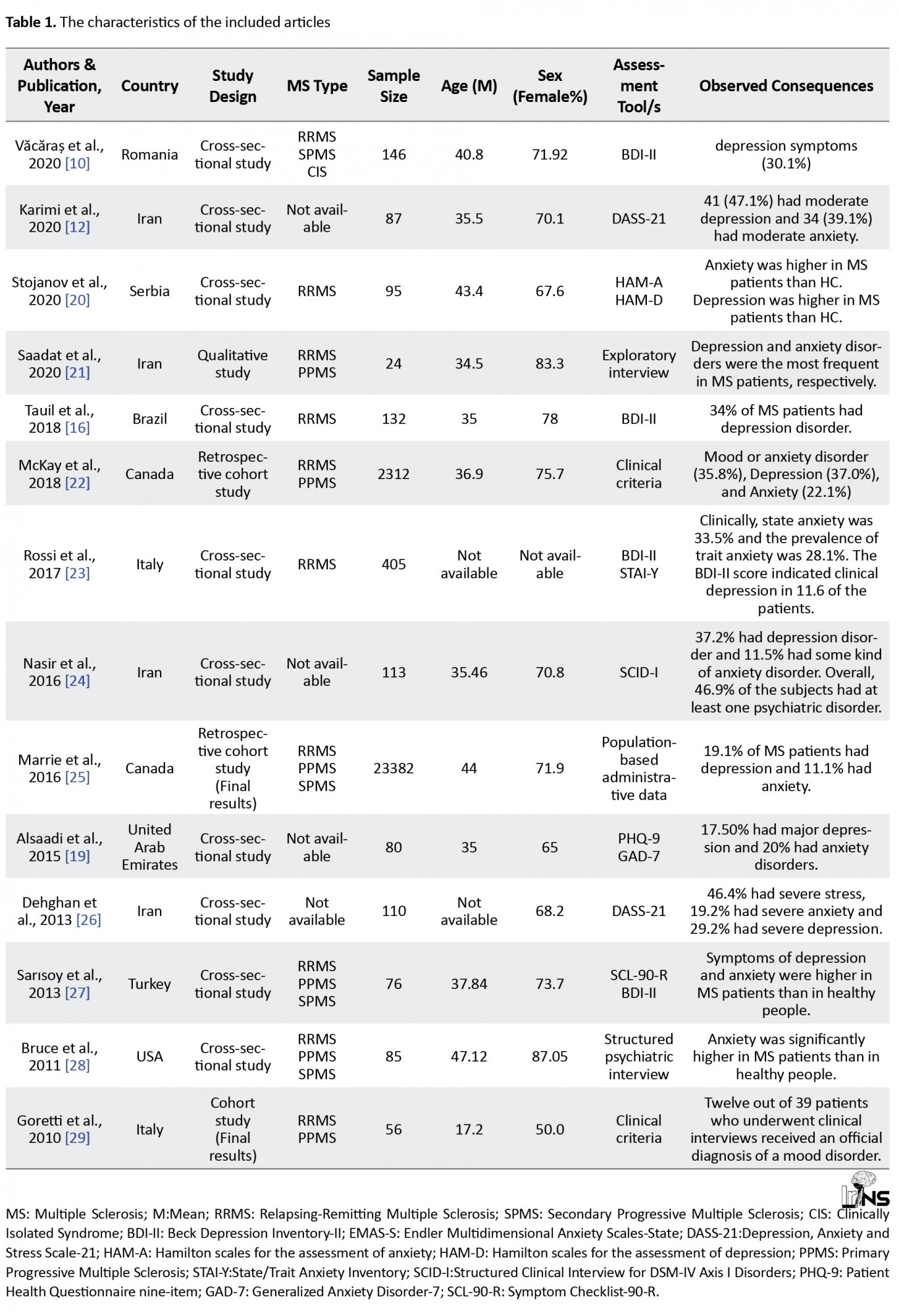
A total of 27106 patients with MS participated in these studies. Văcăraș et al. [10] reported that depressive syndrome’ prevalence equals 30.1%. Karimi et al. [12] measured the prevalence of moderate depression and anxiety as 47.1% and 39.1%, respectively. Stojanov et al. [20] explained that patients with MS achieved higher scores on anxiety and depression scales, compared with healthy individuals. Saadat et al. [21], in a qualitative study using exploratory interviews, suggested that anxiety and depression are highly prevalent in patients with MS. Tauil et al. [16] argued that 34% of patients with MS presented MDD symptoms. McKay et al. [22] reported a prevalence of mood disorders or depression as 35.8%, depression 37%, and anxiety as 22.1%. According to Rossi et al. [23], 33.5% of patients had state anxiety, 28.1% had trait anxiety, and 11.6% of patients encountered a severe depressive disorder. Nasir et al. [24] found that ≥46.9% of patients with MS reported at least one psychiatric disorder.
Based on Marrie et al. [25], 19.1% of patients with MS had depression, 11.1% had anxiety, and 3.15% had bipolar disorder. Alsaadi et al. [19] explained that 17.50% of patients with MS had MDD and 20% had anxiety disorders. Dehghan et al. [26] found that 19.2% of patients had severe anxiety and 29.2% had severe depression. Sarısoy et al. [27] reported that depressive and anxiety disorders were significantly more prevalent in patients with MS, compared with healthy individuals. Bruce et al. [28] revealed that anxiety was significantly higher in patients with MS, compared with healthy individuals. Goretti et al. [29] stated that mood disorders are more prevalent in adolescents suffering from MS compared with the general population.
4. Discussion
The data of the current review revealed that anxiety and depression are more prevalent in patients with MS, compared with healthy subjects. Perhaps, the comorbid depression and anxiety in these patients is a natural reaction to the unpredictable course of an incapacitating and chronic disease. Depression and anxiety can also negatively affect health status, treatment adherence, or provide direct pathophysiological effects on immunity by increasing the severity of symptoms [30].
Moreover, the risk of depression in MS varies from 11% to 35% [16, 17, 18, 19, 20, 21, 22, 23, 24, 25]. These differences can be caused by multiple methodological issues such as differences in used definitions, measurement instruments, diagnostic criteria, sample size, and nature of the studied population [31]. Most studies measured and reported depression and anxiety using self-report questionnaires; consequently, using different tools can be among the reasons for heterogeneity in various statistics that have different cutting points [32]. Furthermore, it is impossible to apply these scales to formally diagnose psychiatric disorders; they tend to overestimate the prevalence, compared with diagnostic interviews [31]. The symptoms of depression and anxiety in MS have been frequently assessed in small samples of MS in the related treatment centers, which fail to represent all MS patients [17, 18, 19]. Increasing the risk of developing anxiety in MS varies from 11% to 33% [16, 17, 18, 19, 20, 21, 22, 23, 24, 25]. Numerous studies revealed a significant relationship between high levels of anxiety and depression in patients with MS. One study explained that depression was identified as the most significant factor related to anxiety [33]. A prospective study conducted in two years revealed that depression is the most significant predictor of anxiety in these patients [34]. Women included the majority of participants in many studies. Gender imbalance plays a significant role in the frequency and prevalence of anxiety; in general, women are more anxious compared with men [35].
Comorbid anxiety and depression can present unpleasant consequences on disease claims and quality of life among MS patients [33]. Treatment interventions to simultaneously decrease depression and anxiety in the research background were ignored for MS patients; however, transcendental interventions which apply fundamental principles concerning mental disorders were beneficial for individuals with comorbid anxiety and depression [36]. These interventions apply the fundamental principles and techniques regarding cognitive behavioral therapy, like exposure and cognitive restructuring. They target the common processes of anxiety and depression. Besides, a systematic review on these interventions for depression and anxiety disorders in adults indicated a considerable reduction in anxiety and depression and enhanced average quality of life [37]. Selective Serotonin Reuptake Inhibitors (SSRIs) are also regarded as the initial treatment line for depression and anxiety disorders [38]. Moreover, combining benzodiazepines with SSRI can result in faster control of anxiety and enhance the control of episodic or situational anxiety [39]. Tricyclic Antidepressants (TCAs) such as amitriptyline were also highly effective on relieving depressive symptoms [40], though there is no credible evidence of clinical trials in MS patients. Urinary incontinence is one of the most common problems in these patients; thus, using TCAs for improving urinary incontinence and mood syndrome was suggested [41]. There exists little evidence considering the drug treatment of depression and anxiety specifically for MS patients. In general, clinical trials are required for drug treatment in MS to make strong evidence of their efficacy for depression and anxiety.
One of the causes for the heterogeneity of statistics about the frequency of anxiety and depression in MS patients addresses various definitions of anxiety and depression. Accordingly, in some research, anxiety, and depression were assessed as a disorder based on accurate clinical criteria and in others as a trait of the patients. Thus, it is required to assess anxiety as a disorder applying clinical interviews in future studies. In surveying the frequency of depression and anxiety, the clinical and demographic status of these patients must be regarded. Therefore, some research indicated that anxiety is higher in patients with recurrent MS. There is also a relationship between early age and depression and anxiety. Therefore, age can be a confounding variable in reporting the frequency of depression and anxiety. Furthermore, employment status influenced the severity of anxiety and depression in these patients [42].
A research discovered that depression, regardless of other factors, is associated with fatigue and aging [43]. Generally, the prevalence of anxiety and depression in MS patients is very high; the relationship between economic and clinical status and psychological symptoms of depression and anxiety is significant [12]. Based on findings of another study, the prevalence of depression was high during relapse and gradually decreased after relapse [44]. Based on these data, in reporting the frequency of psychological disorders in MS patients, the role of demographic and clinical factors of these patients must be considered. These factors can be among the reasons for heterogeneous statistics on the frequency of psychological disorders in these patients.
5. Conclusion
Generally, anxiety and depression, whether as traits and symptoms or disorders, are more prevalent in MS patients, compared with the general population. Further research is required on the prevalence of depression and anxiety in MS patients to provide more accurate information considering the mentioned limitations. For the sake of practical use, it is proposed that MS patients be constantly assessed by psychiatric specialists via the course of the disease to inhibit the recurrence of symptoms with early diagnosis. The effects of disease-modifying therapies, like interferon-β on depression in MS patients remains unclear. However, medication should be used more carefully in MS patients with depressive symptoms. It is recommended that pharmacological and psychotherapeutic interventions be applied to improve the psychological conditions of MS patients based on their clinical symptoms.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally in performing the project and preparing the manuscript.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgements
The authors would like to thank all the previous researchers whose studies were used in this review.
References
Multiple Sclerosis (MS) is among the most prevalent neurological diseases. Moreover, this chronic disease involves multiple areas of the central nervous system as one of its main features. The disease is prevalent in 20- to 40-year-old individuals. It also continues for years by developing incapacitating symptoms; eventually, MS causes serious psychosocial health issues [1]. Patients with MS experience an all-inclusive range of movement limitations, pain, chronic fatigue, memory impairment, and concentration problems daily [2]. Consequently, MS influences all fields of a subject's life, including employment, relationships, leisure, and daily activities [3]. Accordingly, these limitations and disabilities might highly influence the experience of unpleasant emotions and the development of mood and anxiety disorders in them [4].
There is no remedy for MS and it is usually diagnosed early in life; thus, these patients live with these challenging symptoms for multiple years [5]. Patients with MS encounter higher levels of mental disorders, such as depression, stress, and anxiety, compared with the healthy population and those with other chronic conditions. These symptoms may directly result from the inflammation and demyelination of the nervous system [6]. The most valid study in a large sample using Magnetic Resonance Imaging (MRI) indicated that individuals with MS had "more hyperintense lesions in the left inferior medial frontal regions and greater atrophy of the left anterior temporal regions". These two areas of the brain predict 42% of the variance in depression in individuals with MS [7]. The relationship between depressive symptoms and disease-modifying therapies, especially interferon-β, remains contradictory [8]. However, a meta-analysis reported no significant relationship between depression and interferon-β treatment in MS; a history of depression is an important risk factor for depressive syndrome in interferon-β treatment [9]. Consequently, Major Depressive Disorder (MDD) has been reported in up to 50% of MS patients while it has been estimated to range from 10% to 15% in the general population [1, 10]. Studies have also revealed that patients with MS experience high levels of anxiety (about 36%-54%) and approximately 30% of patients with MS develop generalized anxiety disorder [11].
There is a complicated relationship between mental disorders and MS; its frequency can be a reaction to several factors. Moreover, physical symptoms such as fatigue, disability, the experience of family problems, work, and social life result in the recurrence of psychological symptoms; consequently, it leads to an increase in the pressure of chronic disease [12]. The relationship between depressed mood and the prevalent symptoms of MS was supported by several studies. Studies almost revealed a mutual relationship between depression and MS symptoms worldwide [13]. Some researchers have assigned the prevalence of depressive disorders in MS patients to the symptoms of chronic fatigue, cognitive disorders, and pain experience; it is assumed that perceived fatigue and disability, as well as pain, can expedite depression [14]. It was determined that nearly half of MS patients experience cognitive disorders. The speed to process the information, attention and concentration, memory, and executive function is considered as the most significant cognitive disorders experienced by MS patients. The symptoms of cognitive disorders can cause extensive difficulties in individual and social functioning that might cause depression [15]. Furthermore, depression and anxiety in patients with MS cause different psychosocial risk factors including inadequate coping or poor social support or MS-related biological processes such as changes in brain structure or immunological and inflammatory pathways [16]. The most concerning issue in this field indicates a high risk of suicide in patients with MS and comorbid depressive symptoms. Evidence implies that the risk of suicide in depressed patients with MS is between 1.6 and 2.3 times higher than that in the general population. Additionally, approximately a quarter of patients with MS permanently contemplate suicide [17].
MDD is highly significant in patients with MS; however, anxiety has been less considered in this disease. Several studies have been conducted in this field and suggested that approximately 25%-41% of patients with MS are anxious. The clinical interview structure was applied only in two studies to evaluate the diagnosis of anxiety; consequently, both investigations reached the rate of 36% in patients. Generally, an anxiety score of up to 18.6% is normal in MS patients. Those patients who develop anxiety are frequently women with depression who contemplate suicide [18].
Examining the conducted studies revealed that the quality of life in depressed patients with MS is extremely lower than that in patients who are not depressed; even if nervous disabilities and fatigue are controlled. Depression unpleasantly affects MS patients. Depressed patients with MS experience the bewilderment of social and family support. Besides, there is even evidence that depression stops self-management behaviors in these patients [19]. Furthermore, depression and anxiety in patients with MS are associated with poor quality of life, cognitive dysfunction, increased risk of suicide, and occupational problems [18]. Depression and anxiety in MS appear to become more serious over time. It can be frequently treated at the beginning, i.e., significant to diagnose the disease early. Moreover, precisely examining and identifying psychological disorders, such as anxiety and depression in patients with MS play an effective role in developing treatment programs to reduce these disorders. Accordingly, this review study examined depression and anxiety in patients with MS.
2. Methods and Materials/Patients
This was a systematic review. We searched 4 online databases (PsycNET, PubMed, Scopus, and Magiran). Searches were performed applying the following keywords: “multiple sclerosis, MS, psychiatric issues, psychological disorders, psychological problems, anxiety, mental health, quality of life, and depression”. The search was performed in each database after conducting specific filters (publication date, title/abstract, and article type). For example, the search was conducted based on the Medical Subject Heading (MeSH) in the PubMed database. We first searched the keyword “multiple sclerosis” by applying restrictions (all time from 2010 to 2020 and title/abstract). There was no limitation in the research design of the studies and quantitative and qualitative studies were analyzed. We removed duplicates after identifying the studies and examined the results based on titles and abstracts. Full texts were examined for the qualified studies of retrieval and additional inclusion and exclusion criteria.
If these studies reported experiences or psychological consequences (anxiety & depression) observed in patients with MS, they could be the inclusion criteria. The exclusion criteria were as follows: studies which had evaluated psychological consequences in patients with other disorders (Not MS), non-original studies (systematic review, etc.), studies based on clinical intervention, studies written in languages other than English or Persian, studies which aimed at developing and validating scales, studies which had examined acute stress, studies which only had examined the linear relationships between the variables and studies which did not report the frequency of disorders. The two arbitrators evaluated the papers according to the inclusion criteria. The second arbitrator examined and approved the papers and the disputes were resolved through discussion. Figure 1 shows the search process. The critical appraisal was performed by two psychologists based on 3 indicators; evaluating the validity of selected articles, interpreting the results, and applying the results to clinical situations.
3. Results
Table 1 explains the results of analyzing 14 studies.
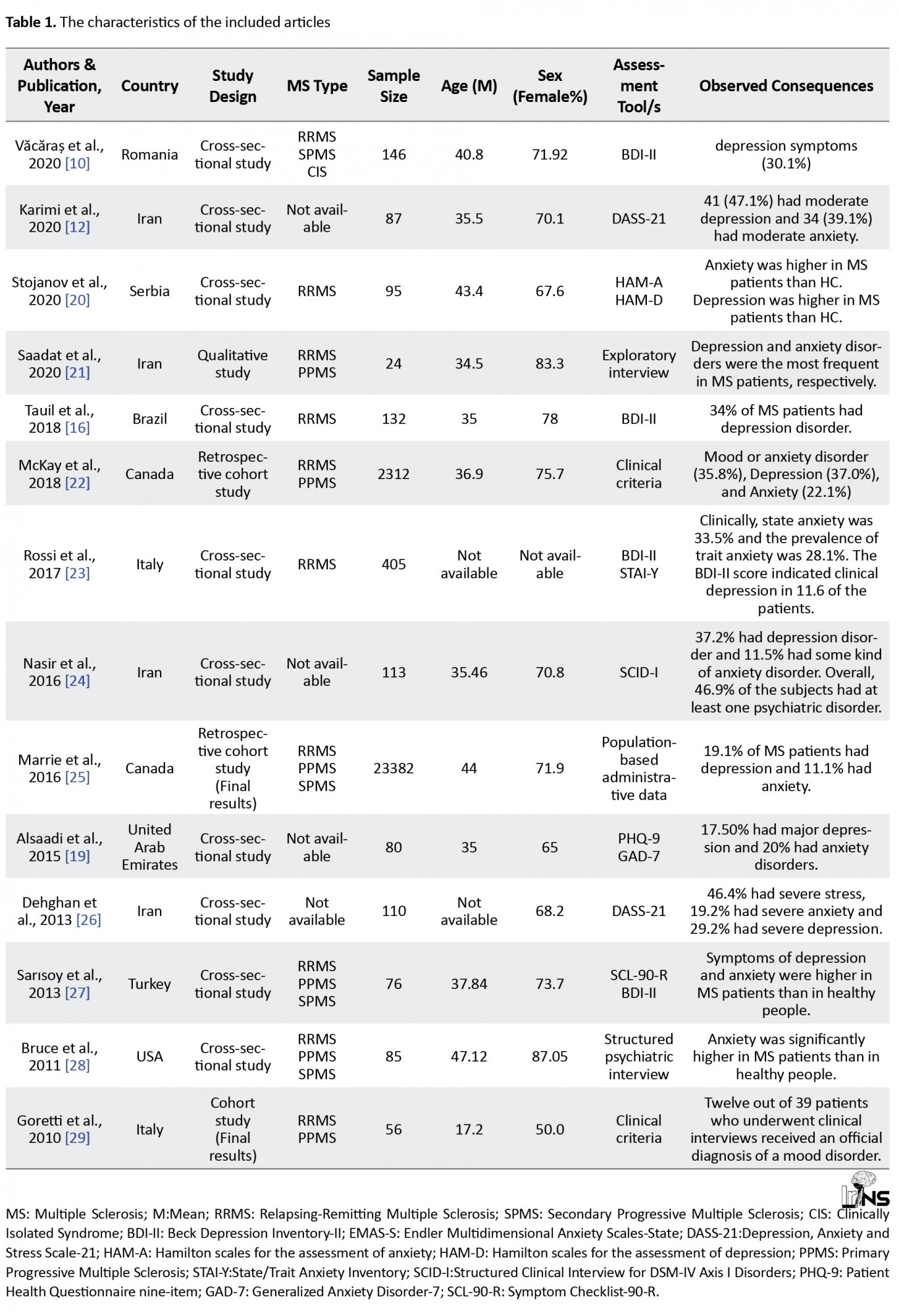
A total of 27106 patients with MS participated in these studies. Văcăraș et al. [10] reported that depressive syndrome’ prevalence equals 30.1%. Karimi et al. [12] measured the prevalence of moderate depression and anxiety as 47.1% and 39.1%, respectively. Stojanov et al. [20] explained that patients with MS achieved higher scores on anxiety and depression scales, compared with healthy individuals. Saadat et al. [21], in a qualitative study using exploratory interviews, suggested that anxiety and depression are highly prevalent in patients with MS. Tauil et al. [16] argued that 34% of patients with MS presented MDD symptoms. McKay et al. [22] reported a prevalence of mood disorders or depression as 35.8%, depression 37%, and anxiety as 22.1%. According to Rossi et al. [23], 33.5% of patients had state anxiety, 28.1% had trait anxiety, and 11.6% of patients encountered a severe depressive disorder. Nasir et al. [24] found that ≥46.9% of patients with MS reported at least one psychiatric disorder.
Based on Marrie et al. [25], 19.1% of patients with MS had depression, 11.1% had anxiety, and 3.15% had bipolar disorder. Alsaadi et al. [19] explained that 17.50% of patients with MS had MDD and 20% had anxiety disorders. Dehghan et al. [26] found that 19.2% of patients had severe anxiety and 29.2% had severe depression. Sarısoy et al. [27] reported that depressive and anxiety disorders were significantly more prevalent in patients with MS, compared with healthy individuals. Bruce et al. [28] revealed that anxiety was significantly higher in patients with MS, compared with healthy individuals. Goretti et al. [29] stated that mood disorders are more prevalent in adolescents suffering from MS compared with the general population.
4. Discussion
The data of the current review revealed that anxiety and depression are more prevalent in patients with MS, compared with healthy subjects. Perhaps, the comorbid depression and anxiety in these patients is a natural reaction to the unpredictable course of an incapacitating and chronic disease. Depression and anxiety can also negatively affect health status, treatment adherence, or provide direct pathophysiological effects on immunity by increasing the severity of symptoms [30].
Moreover, the risk of depression in MS varies from 11% to 35% [16, 17, 18, 19, 20, 21, 22, 23, 24, 25]. These differences can be caused by multiple methodological issues such as differences in used definitions, measurement instruments, diagnostic criteria, sample size, and nature of the studied population [31]. Most studies measured and reported depression and anxiety using self-report questionnaires; consequently, using different tools can be among the reasons for heterogeneity in various statistics that have different cutting points [32]. Furthermore, it is impossible to apply these scales to formally diagnose psychiatric disorders; they tend to overestimate the prevalence, compared with diagnostic interviews [31]. The symptoms of depression and anxiety in MS have been frequently assessed in small samples of MS in the related treatment centers, which fail to represent all MS patients [17, 18, 19]. Increasing the risk of developing anxiety in MS varies from 11% to 33% [16, 17, 18, 19, 20, 21, 22, 23, 24, 25]. Numerous studies revealed a significant relationship between high levels of anxiety and depression in patients with MS. One study explained that depression was identified as the most significant factor related to anxiety [33]. A prospective study conducted in two years revealed that depression is the most significant predictor of anxiety in these patients [34]. Women included the majority of participants in many studies. Gender imbalance plays a significant role in the frequency and prevalence of anxiety; in general, women are more anxious compared with men [35].
Comorbid anxiety and depression can present unpleasant consequences on disease claims and quality of life among MS patients [33]. Treatment interventions to simultaneously decrease depression and anxiety in the research background were ignored for MS patients; however, transcendental interventions which apply fundamental principles concerning mental disorders were beneficial for individuals with comorbid anxiety and depression [36]. These interventions apply the fundamental principles and techniques regarding cognitive behavioral therapy, like exposure and cognitive restructuring. They target the common processes of anxiety and depression. Besides, a systematic review on these interventions for depression and anxiety disorders in adults indicated a considerable reduction in anxiety and depression and enhanced average quality of life [37]. Selective Serotonin Reuptake Inhibitors (SSRIs) are also regarded as the initial treatment line for depression and anxiety disorders [38]. Moreover, combining benzodiazepines with SSRI can result in faster control of anxiety and enhance the control of episodic or situational anxiety [39]. Tricyclic Antidepressants (TCAs) such as amitriptyline were also highly effective on relieving depressive symptoms [40], though there is no credible evidence of clinical trials in MS patients. Urinary incontinence is one of the most common problems in these patients; thus, using TCAs for improving urinary incontinence and mood syndrome was suggested [41]. There exists little evidence considering the drug treatment of depression and anxiety specifically for MS patients. In general, clinical trials are required for drug treatment in MS to make strong evidence of their efficacy for depression and anxiety.
One of the causes for the heterogeneity of statistics about the frequency of anxiety and depression in MS patients addresses various definitions of anxiety and depression. Accordingly, in some research, anxiety, and depression were assessed as a disorder based on accurate clinical criteria and in others as a trait of the patients. Thus, it is required to assess anxiety as a disorder applying clinical interviews in future studies. In surveying the frequency of depression and anxiety, the clinical and demographic status of these patients must be regarded. Therefore, some research indicated that anxiety is higher in patients with recurrent MS. There is also a relationship between early age and depression and anxiety. Therefore, age can be a confounding variable in reporting the frequency of depression and anxiety. Furthermore, employment status influenced the severity of anxiety and depression in these patients [42].
A research discovered that depression, regardless of other factors, is associated with fatigue and aging [43]. Generally, the prevalence of anxiety and depression in MS patients is very high; the relationship between economic and clinical status and psychological symptoms of depression and anxiety is significant [12]. Based on findings of another study, the prevalence of depression was high during relapse and gradually decreased after relapse [44]. Based on these data, in reporting the frequency of psychological disorders in MS patients, the role of demographic and clinical factors of these patients must be considered. These factors can be among the reasons for heterogeneous statistics on the frequency of psychological disorders in these patients.
5. Conclusion
Generally, anxiety and depression, whether as traits and symptoms or disorders, are more prevalent in MS patients, compared with the general population. Further research is required on the prevalence of depression and anxiety in MS patients to provide more accurate information considering the mentioned limitations. For the sake of practical use, it is proposed that MS patients be constantly assessed by psychiatric specialists via the course of the disease to inhibit the recurrence of symptoms with early diagnosis. The effects of disease-modifying therapies, like interferon-β on depression in MS patients remains unclear. However, medication should be used more carefully in MS patients with depressive symptoms. It is recommended that pharmacological and psychotherapeutic interventions be applied to improve the psychological conditions of MS patients based on their clinical symptoms.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally in performing the project and preparing the manuscript.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgements
The authors would like to thank all the previous researchers whose studies were used in this review.
References
- Siegert RJ, Abernethy DA. Depression in multiple sclerosis: A review. Journal of Neurology, Neurosurgery, and Psychiatry. 2005; 76(4):469-75. [PMID] [PMCID]
- Mitchell AJ, Benito-León J, González JM, Rivera-Navarro J. Quality of life and its assessment in multiple sclerosis: Integrating physical and psychological components of wellbeing. The Lancet. Neurology. 2005; 4(9):556-66. [PMID]
- Simmons RD. Life issues in multiple sclerosis. Nature Reviews. Neurology. 2010; 6(11):603-10. [PMID]
- Ferreira AM, Leal B, Ferreira I, Brás S, Moreira I, Samões R, et al. Depression and anxiety in multiple sclerosis patients: The role of genetic variability of interleukin 1β. Multiple Sclerosis and Related Disorders. 2021; 52:102982. [PMID]
- Qaderi K, Merghati Khoei E. Sexual problems and quality of life in women with multiple sclerosis. Sexuality and Disability. 2013; 32:35-43. [DOI:10.1007/s11195-013-9318-4]
- Henry A, Tourbah A, Camus G, Deschamps R, Mailhan L, Castex C, et al. Anxiety and depression in patients with multiple sclerosis: The mediating effects of perceived social support. Multiple Sclerosis and Related Disorders. 2019; 27:46-51. [PMID]
- Feinstein A, Roy P, Lobaugh N, Feinstein K, O’Connor P, Black S. Structural brain abnormalities in multiple sclerosis patients with major depression. Neurology. 2004; 62(4):586-90. [PMID]
- Schippling S, O’Connor P, Knappertz V, Pohl C, Bogumil T, Suarez G, et al. Incidence and course of depression in multiple sclerosis in the multinational BEYOND trial. Journal of Neurology. 2016; 263(7):1418-26. [PMID] [PMCID]
- Alba Palé L, León Caballero J, Samsó Buxareu B, Salgado Serrano P, Pérez Solà V. Systematic review of depression in patients with multiple sclerosis and its relationship to interferonβ treatment. Multiple Sclerosis and Related Disorders. 2017; 17:138-43. [PMID]
- Vǎcǎra V, Vǎcǎra V, Nistor C, Vǎcǎra D, Opre AN, Blaga P, et al. The influence of depression and anxiety on neurological disability in multiple sclerosis patients. Behavioural Neurology. 2020; 2020:1-8. [DOI: 10.1155/2020/6738645]
- Kidd T, Carey N, Mold F, Westwood S, Miklaucich M, Konstantara E, et al. A systematic review of the effectiveness of self-management interventions in people with multiple sclerosis at improving depression, anxiety and quality of life. PLoS One. 2017; 12(10):e0185931. [PMID] [PMCID]
- Karimi S, Andayeshgar B, Khatony A. Prevalence of anxiety, depression, and stress in patients with multiple sclerosis in Kermanshah-Iran: A cross-sectional study. BMC Psychiatry. 2020; 20(1):166. [PMID] [PMCID]
- Patten SB, Marrie RA, Carta MG. Depression in multiple sclerosis. International Review of Psychiatry. 2017; 29(5):463-72. [PMID]
- Greeke EE, Chua AS, Healy BC, Rintell DJ, Chitnis T, Glanz BI. Depression and fatigue in patients with multiple sclerosis. Journal of the Neurological Sciences. 2017; 380:236-41. [PMID]
- Turner AP, Alschuler KN, Hughes AJ, Beier M, Haselkorn JK, Sloan AP, et al. Mental health comorbidity in MS: Depression, anxiety, and bipolar disorder. Current Neurology and Neuroscience Reports. 2016; 16(12):106. [PMID]
- Tauil CB, Grippe TC, Dias RM, Dias-Carneiro RPC, Carneiro NM, Aguilar ACR, et al. Suicidal ideation, anxiety, and depression in patients with multiple sclerosis. Arquivos de Neuro-Psiquiatria. 2018; 76(5):296-301. [PMID]
- Viner R, Patten SB, Berzins S, Bulloch AG, Fiest KM. Prevalence and risk factors for suicidal ideation in a multiple sclerosis population. Journal of Psychosomatic Research. 2014; 76(4):312-6. [PMID]
- Chwastiak LA, Ehde DM. Psychiatric issues in multiple sclerosis. The Psychiatric Clinics of North America. 2007; 30(4):803-17. [PMID] [PMCID]
- Alsaadi T, El Hammasi K, Shahrour TM, Shakra M, Turkawi L, Mudhafar A, et al. Prevalence of depression and anxiety among patients with multiple sclerosis attending the MS Clinic at Sheikh Khalifa Medical City, UAE: Cross-Sectional Study. Multiple Sclerosis International. 2015; 2015:487159. [PMID] [PMCID]
- Stojanov A, Malobabic M, Milosevic V, Stojanov J, Vojinovic S, Stanojevic G, et al. Psychological status of patients with relapsing-remitting multiple sclerosis during coronavirus disease-2019 outbreak. Multiple Sclerosis and Related Disorders. 2020; 45:102407. [PMID] [PMCID]
- Saadat S, Kalantari M, Kajbaf MB, Hosseininezhad M. [Psychological status of multiple sclerosis patients: A qualitative study (Persian)]. Journal of Health System Research. 2020; 15(4):296-303. http://hsr.mui.ac.ir/article-1-1099-fa.html
- McKay KA, Tremlett H, Fisk JD, Zhang T, Patten SB, Kastrukoff L, et al. Psychiatric comorbidity is associated with disability progression in multiple sclerosis. Neurology. 2018; 90(15):e1316-23. [PMID] [PMCID]
- Rossi S, Studer V, Motta C, Polidoro S, Perugini J, Macchiarulo G, et al. Neuroinflammation drives anxiety and depression in relapsing-remitting multiple sclerosis. Neurology. 2017; 89(13):1338-47. [PMID]
- Nasiri M, Hosseini H, Sakhaei Y, Tabrizi N, Yazdani Cherati J, Abedini M. [Prevalence of psychiatric disorders in patients with multiple sclerosis in Mazandaran, Iran (Persian)]. Journal of Mazandaran University of Medical Sciences. 2016; 26(140):60-70. http://jmums.mazums.ac.ir/article-1-8549-en.html
- Marrie RA, Patten SB, Tremlett H, Wolfson C, Warren S, Svenson LW, et al. Sex differences in comorbidity at diagnosis of multiple sclerosis: A population-based study. Neurology. 2016; 86(14):1279-86. [PMID] [PMCID]
- Dehghan A, Mohammadkhani Kermanshahi S, Memarian R. [Abundance of stress, anxiety and depression in multiple sclerosis patients (Persian)]. Alborz University Medical Journal. 2013; 2(2):82-8. http://aums.abzums.ac.ir/article-1-95-en.html
- Sarısoy G, Terzi M, Gümüş K, Pazvantoğlu O. Psychiatric symptoms in patients with multiple sclerosis. General Hospital Psychiatry. 2013; 35(2):134-40. [PMID]
- Bruce JM, Lynch SG. Personality traits in multiple sclerosis: Association with mood and anxiety disorders. Journal of Psychosomatic Research. 2011; 70(5):479-85. [PMID]
- Goretti B, Ghezzi A, Portaccio E, Lori S, Zipoli V, Razzolini L, et al. Psychosocial issue in children and adolescents with multiple sclerosis. Neurological Sciences. 2010; 31(4):467-70. [PMID]
- Katon W, Lin EH, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. General Hospital Psychiatry. 2007; 29(2):147-55. [PMID]
- Patten SB, Metz LM. Depression in multiple sclerosis. Psychotherapy and Psychosomatics. 1997; 66(6):286-92. [PMID]
- Minden SL, Feinstein A, Kalb RC, Miller D, Mohr DC, Patten SB, et al. Evidence-based guideline: Assessment and management of psychiatric disorders in individuals with MS: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2014; 82(2):174-81. [PMID] [PMCID]
- Garfield AC, Lincoln NB. Factors affecting anxiety in multiple sclerosis. Disability and Rehabilitation. 2012; 34(24):2047-52. [PMID]
- Brown RF, Valpiani EM, Tennant CC, Dunn SM, Sharrock M, Hodgkinson, et al. Longitudinal assessment of anxiety, depression, and fatigue in people with multiple sclerosis. Psychology and Psychotherapy. 2009; 82(Pt 1):41-56. [PMID]
- Orton SM, Herrera BM, Yee IM, Valdar W, Ramagopalan SV, Sadovnick AD, et al. Sex ratio of multiple sclerosis in Canada: A longitudinal study. The Lancet. Neurology. 2006; 5(11):932-6. [PMID]
- McEvoy PM, Nathan P, Norton PJ. Efficacy of transdiagnostic treatments: A review of published outcome studies and future research directions. Journal of Cognitive Psychotherapy: An International Quarterl. 2009; 23(1):20-33. http://ruby.fgcu.edu/courses/twimberley/10199/psy/transrx.pdf
- Newby JM, McKinnon A, Kuyken W, Gilbody S, Dalgleish T. Systematic review and meta-analysis of transdiagnostic psychological treatments for anxiety and depressive disorders in adulthood. Clinical Psychology Review. 2015; 40:91-110. [PMID]
- Coplan JD, Aaronson CJ, Panthangi V, Kim Y. Treating comorbid anxiety and depression: Psychosocial and pharmacological approaches. World Journal of Psychiatry. 2015; 5(4):366-78. [PMID] [PMCID]
- Dunlop BW, Davis PG. Combination treatment with benzodiazepines and SSRIs for comorbid anxiety and depression: A review. Primary Care Companion to The Journal of Clinical Psychiatry. 2008; 10(3):222-8. [PMID] [PMCID]
- Anderson IM. SSRIS versus tricyclic antidepressants in depressed inpatients: A meta- analysis of efficacy and tolerability. Depression and Anxiety. 1998; 7 (Suppl 1):11-7. [PMID]
- Zecca C, Riccitelli GC, Disanto G, Singh A, Digesu GA, Panicari L, et al. Urinary incontinence in multiple sclerosis: Prevalence, severity and impact on patients’ quality of life. European Journal of Neurology. 2016; 23(7):1228-34. [PMID]
- Jones KH, Ford DV, Jones PA, John A, Middleton RM, Lockhart-Jones H, et al. A large-scale study of anxiety and depression in people with Multiple Sclerosis: A survey via the web portal of the UK MS Register. PLoS One. 2012; 7(7):e41910. [PMID] [PMCID]
- Seyed Saadat SM, Hosseininezhad M, Bakhshayesh B, Seyed Saadat SN, Nabizadeh SP. Prevalence and predictors of depression in Iranian patients with multiple sclerosis: A population-based study. Neurological Sciences. 2014; 35(5):735-40. [PMID]
- Moore P, Hirst C, Harding KE, Clarkson H, Pickersgill TP, Robertson NP. Multiple sclerosis relapses and depression. Journal of Psychosomatic Research. 2012; 73(4):272-6. [PMID]
Type of Study: Review |
Subject:
Neuroscience
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |



.jpg)
