Sun, Feb 22, 2026
Volume 7, Issue 4 (Autumn 2021)
Iran J Neurosurg 2021, 7(4): 197-204 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghasemi A A. The Effects of Body Mass Index on Lumbar Microdiscectomy Outcomes. Iran J Neurosurg 2021; 7 (4) :197-204
URL: http://irjns.org/article-1-285-en.html
URL: http://irjns.org/article-1-285-en.html
Department of Neurosurgery, School of Medicine, Urmia University of Medical Sciences, Urmia, Iran , dr.amirghasemi@ymail.com
Full Text [PDF 592 kb]
(1817 Downloads)
| Abstract (HTML) (3479 Views)
Full Text: (1907 Views)
1. Introduction
The incidence of obesity has steadily risen to epidemic proportions in numerous world regions [1, 2]. In the United States and other developed countries, morbid obesity has been particularly rapid in its increase. Among its numerous consequences, it has been associated with an increased incidence of spinal degenerative disc diseases [3]. Obesity may be related to disc degeneration of the lumbar spine [4]. In parallel with the increasing prevalence of obesity, patients’ referral to spine surgeons is more likely to increase; thus, we need to know the answers regarding treatment cost and complication risk in this population [5]. Specific data related to these patients will be necessary to clarify both risks of surgical complications and overall hospital costs. Beyond healthcare costs, however, obesity seems to be related to higher surgical complications [6]. Two separate studies have shown that patients with elevated BMI have higher difficulties after spinal fusions [7, 8].
The results of previous studies on the link between obesity and spinal surgery outcomes are still debated. Our aim in this study was to evaluate the effect of BMI on the surgical outcomes of patients undergoing lumbar microdiscectomy.
2. Methods and Materials/Patients
A retrospective case-series study was conducted on patients who underwent single-level lumbar microdiscectomy at our institution between January 2014 and April 2018. Indications for surgery included severe or progressive neurological deficit and significant pain (Visual Analogue Scale equal to or greater than 4) [9] that is refractory to conservative management. Patients with: (1) recurrent herniation (2) comorbid disorders (diabetes mellitus, increased blood pressure, coronary artery disease) (3) malignant tumor (4) lumbar spine trauma (5) inherited anomalies (6) vertebral osteomyelitis (7) instability of the lumbar spine, were excluded from the study.
The senior spine surgeon performed all the surgical procedures using the standard surgical methods accepted by the neurosurgical community in general. We obtained ethical approval for our research from the Ethics Committee of Urmia University of medical sciences. Informed consent was obtained from all patients.
The steps of the procedure were conducted as follows: All patients were placed in the prone position (a) A 3-cm longitudinal skin incision was made, and tendinous insertions of paravertebral muscles were incised using subperiosteal dissection for access of the lamina; (b) The Caspar lumbar microdiscectomy retractor System was used to separate the edges of the incision; (c) radiographs obtained using C- arms to confirm the level of surgery (d) then, the operative microscope was used to visualize all tissues clearly; (e) small laminotomies were also performed and the ligamentum flavum was then removed (f) ipsilateral foraminotomy and medial facetectomy was performed for adequate decompression of exiting nerve root, the disc sequestrum or any loose disc fragments were removed; (h) epidural particulate steroids were not administered; (i) hemovac drains were placed in all cases; (j) wound closure was performed in a standard sequential manner.
BMI was measured as body weight (kg) divided by the square of the patient’s height (m). The patients were considered underweight if BMI <18.50 kg/m2 (group 1), normal weight (BMI 18.5-24.9 kg/m2) (group 2), pre-obesity (25-29.9 kg/m2) (group 3), obese (≥ 30 kg/m2) (group 4) [10].
The primary study parameters were Visual Analogue Scale (VAS) and Oswestry Disability Index (ODI) before and two years after surgery. The 10 CM visual analog scale was used for our study [11].
ODI scale was used for assessing the severity of back pain and functional impairment of patients [12]. It comprises 10 questions with 6 probable answers. Variables include pain, self-care, lifting, walking, sitting, standing, sleeping, sexual activity, social interaction, and traveling. Values range from 0 to 5. The total score is measured and introduced on a scale from 0 to 100 as follows: 0 to 20 indicates minimal impairment; 21 to 40 equals moderate impairment; 41 to 60 refers to severe impairment; 61 to 80 indicates debilitating back pain; 81 to 100 indicates that the patient is bedridden [13]. The patients were asked to complete ODI and VAS forms before surgery and on the final visit.
The patients’ medical records were carefully reviewed to extract data relevant to our study, including operative time, average blood loss during surgery, hematoma formation, wound infection, CSF leak, deep vein thrombosis, and length of stay after surgery neurologic deficit.
The Analysis of Variance (ANOVA) was used to assess meaningful differences between non-continuous variables; however, the regression analysis evaluated differences in continuous variables. Moreover, P<0.05 was considered significant. SPSS performed data analysis.
3. Results
We evaluated 500 patients who were eligible to enter the study; 275 were women, and 225 were men with a mean±SD age of 40.3±5.2 years (range: 19-70 y). Demographic and descriptive characteristics of patients are presented in Table 1.
.jpg)
Surgical outcome measures (VAS, ODI) significantly improved postoperatively in all patients (Table 2).
.jpg)
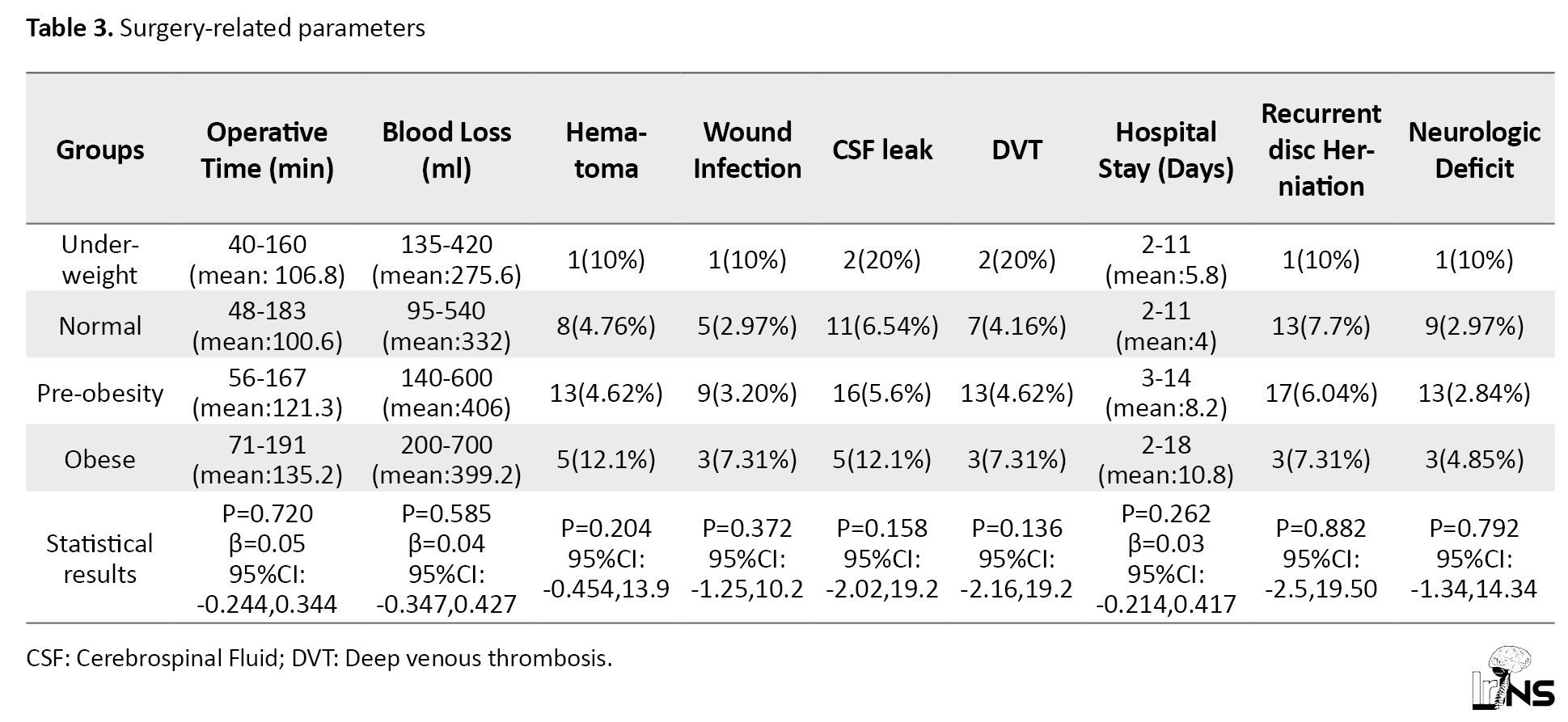
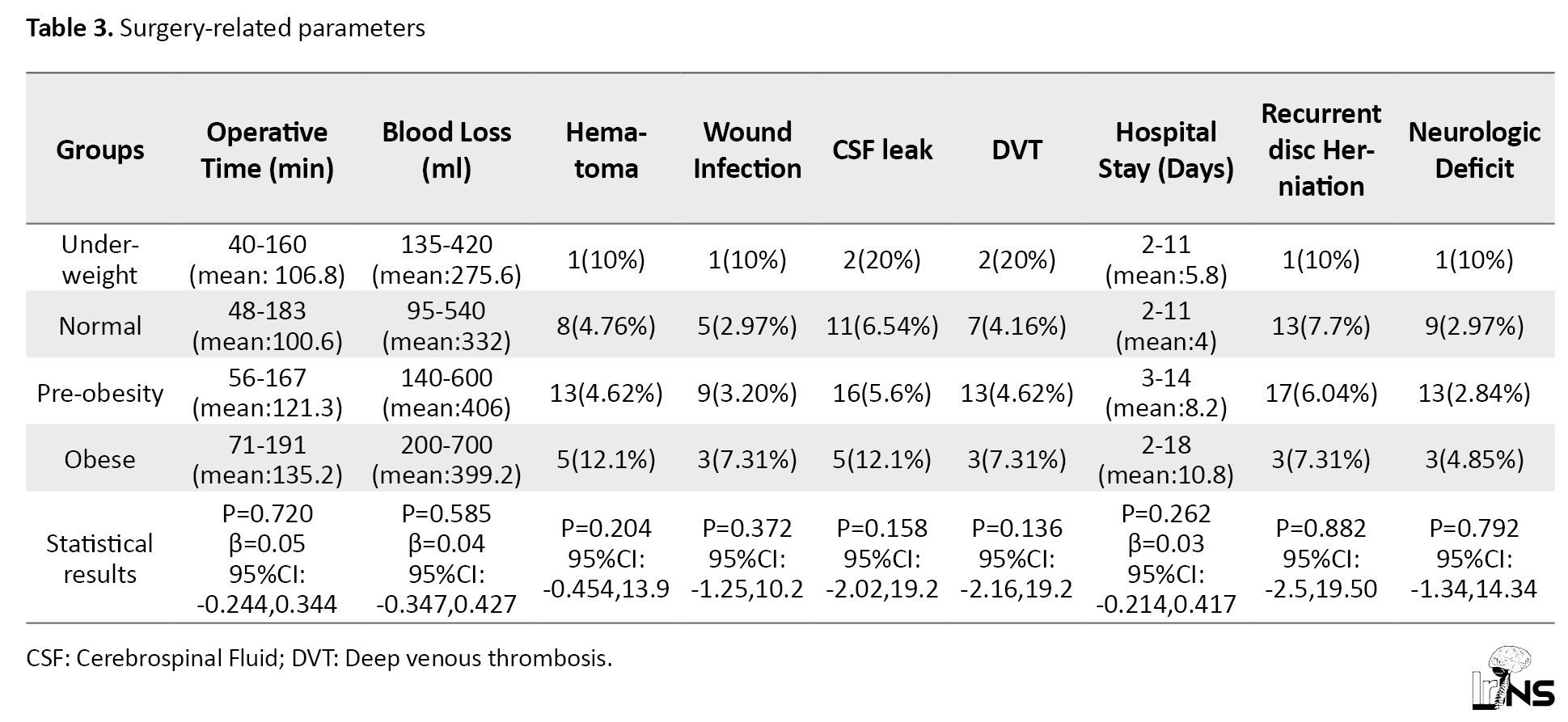
Concerning surgery-related parameters, no significant difference was found between study groups (Table 3).
4. Discussion
Obesity is more prevalent in the United States, compared with other countries [14]. Several studies have demonstrated a higher complication rate and wound problems in obese patients than non-obese patients who underwent spine surgery [15]. Various types of local changes, such as tissue ischemia and decreased resistance to infection, are considered responsible for these complications [16]. Fat tissue vascular insufficiency and more enormous wound wall may be linked to these complications. Longer operative time increases the chance of wound problems in obese patients [17].
Carragee et al. suggested an association between increased BMI and recurrent disc herniation [18]. It is also revealed by Djurasovic et al. that Obesity also increases the risk of surgical site infection, blood loss, and position-associated nerve palsies [19]. Operative time and hospital stay were significantly longer in obese patients [20].
Other studies have found different findings. Quah et al. concluded that obesity was not a risk factor for recurrent disc herniation following lumbar microdiscectomy [21]. Andreshak et al. [22], obese and non-obese patients were not significantly different regarding surgical complications and outcome. In a study performed by Yadla and colleagues [23], BMI did not affect surgical complications.
As we could expect, minimally invasive spine surgeries have lower complication rates than the conventional type, and it could be an alternative for obese patients [24]. Endoscopic lumbar discectomy does not have more significant complications and recurrent disc herniations in obese than non-obese patients [25]. In a study performed by Barber et al. [26], tubular microdiscectomy and open microdiscectomy for lumbar disc herniations had similar outcomes. Ruan et al. [27] conducted a study to compare the outcome of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy. Percutaneous endoscopic lumbar discectomy did not offer an advantage over open lumbar microdiscectomy regarding the clinical outcome.
We designed a retrospective case series study to determine in a real-world setting whether patients with different BMI had any difference in clinical outcome and surgery-related parameters following lumbar microscopic discectomy.
This study and former analytical research indicated dramatic improvement in pain, disability, and health quality in obese and non-obese patients. In another study over the elderly (older than 65 years), Gepstein et al. [25], lumbar decompression was equally effective in pain relief and disability in obese and nonobese patients.
In analytical research, Rihn et al. [28] concluded no correlation between obesity and outcome measures after lumbar spinal canal stenosis surgery. The meta-analysis findings performed by Jin Jiang et al. [29] revealed that increased BMI is associated with higher surgical complications. McGuire et al. [30] performed a subgroup analysis study found that infection rate and operative time were more significant in morbidly obese patients.
In the current study, no association was found between obesity and other surgical and health-related complications, including the operative time, mean blood loss during surgery, hematoma formation, wound infection, CSF leak, deep vein thrombosis, length of stay after surgery, recurrent disc herniation and neurologic deficit. A prospective study designed by Rosen et al. [31]showed that BMI did not influence the outcome measures, operative time, and hospital stay. Contrarily, Telfeian et al. [32] mentioned that outcome measures were dramatically related to BMI.
Comorbid disorders such as ischemic heart disease and diabetes mellitus are more prevalent in Obese patients undergoing spine surgery, i.e., independent predictors of surgical complications [33]. To investigate the effect of just BMI on the outcome, we excluded patients with comorbid disorders. Our reason to exclude those with comorbidities is that complications from underlying comorbidities may be incorrectly attributed to the BMI.Our results do not support the hypothesis that obesity is associated with worse outcomes after lumbar microdiscectomy [34, 35]. At the 24-month follow-up evaluation, the obese and nonobese patient population showed significant mean improvements in all outcome measures.
5. Conclusion
Even with the limitations mentioned above, we can conclude that the findings from this study showed that BMI does not adversely impact the outcome of patients undergoing lumbar microdiscectomy. This study has some limitations which have to be pointed out. The small patient population (especially in the underweight group) and the retrospective nature of the survey with its limitations including Inferior level of evidence in contrast to prospective studies, subject to confounding (other risk factors may be present, i.e., not measured), cannot assess causality, just correlation.
Ethical Considerations
Compliance with ethical guidelines
We obtained approval from the ethics committee of Urmia University of Medical Sciences, West Azarbaijan, Iran (Code: IR.UMSU.REC.1399.307). Written informed consent was obtained from all patients.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All steps of the study were performed by Dr. Amir Abbas Ghasemi.
Conflict of interest
The author declared no conflict of interest.
References
The incidence of obesity has steadily risen to epidemic proportions in numerous world regions [1, 2]. In the United States and other developed countries, morbid obesity has been particularly rapid in its increase. Among its numerous consequences, it has been associated with an increased incidence of spinal degenerative disc diseases [3]. Obesity may be related to disc degeneration of the lumbar spine [4]. In parallel with the increasing prevalence of obesity, patients’ referral to spine surgeons is more likely to increase; thus, we need to know the answers regarding treatment cost and complication risk in this population [5]. Specific data related to these patients will be necessary to clarify both risks of surgical complications and overall hospital costs. Beyond healthcare costs, however, obesity seems to be related to higher surgical complications [6]. Two separate studies have shown that patients with elevated BMI have higher difficulties after spinal fusions [7, 8].
The results of previous studies on the link between obesity and spinal surgery outcomes are still debated. Our aim in this study was to evaluate the effect of BMI on the surgical outcomes of patients undergoing lumbar microdiscectomy.
2. Methods and Materials/Patients
A retrospective case-series study was conducted on patients who underwent single-level lumbar microdiscectomy at our institution between January 2014 and April 2018. Indications for surgery included severe or progressive neurological deficit and significant pain (Visual Analogue Scale equal to or greater than 4) [9] that is refractory to conservative management. Patients with: (1) recurrent herniation (2) comorbid disorders (diabetes mellitus, increased blood pressure, coronary artery disease) (3) malignant tumor (4) lumbar spine trauma (5) inherited anomalies (6) vertebral osteomyelitis (7) instability of the lumbar spine, were excluded from the study.
The senior spine surgeon performed all the surgical procedures using the standard surgical methods accepted by the neurosurgical community in general. We obtained ethical approval for our research from the Ethics Committee of Urmia University of medical sciences. Informed consent was obtained from all patients.
The steps of the procedure were conducted as follows: All patients were placed in the prone position (a) A 3-cm longitudinal skin incision was made, and tendinous insertions of paravertebral muscles were incised using subperiosteal dissection for access of the lamina; (b) The Caspar lumbar microdiscectomy retractor System was used to separate the edges of the incision; (c) radiographs obtained using C- arms to confirm the level of surgery (d) then, the operative microscope was used to visualize all tissues clearly; (e) small laminotomies were also performed and the ligamentum flavum was then removed (f) ipsilateral foraminotomy and medial facetectomy was performed for adequate decompression of exiting nerve root, the disc sequestrum or any loose disc fragments were removed; (h) epidural particulate steroids were not administered; (i) hemovac drains were placed in all cases; (j) wound closure was performed in a standard sequential manner.
BMI was measured as body weight (kg) divided by the square of the patient’s height (m). The patients were considered underweight if BMI <18.50 kg/m2 (group 1), normal weight (BMI 18.5-24.9 kg/m2) (group 2), pre-obesity (25-29.9 kg/m2) (group 3), obese (≥ 30 kg/m2) (group 4) [10].
The primary study parameters were Visual Analogue Scale (VAS) and Oswestry Disability Index (ODI) before and two years after surgery. The 10 CM visual analog scale was used for our study [11].
ODI scale was used for assessing the severity of back pain and functional impairment of patients [12]. It comprises 10 questions with 6 probable answers. Variables include pain, self-care, lifting, walking, sitting, standing, sleeping, sexual activity, social interaction, and traveling. Values range from 0 to 5. The total score is measured and introduced on a scale from 0 to 100 as follows: 0 to 20 indicates minimal impairment; 21 to 40 equals moderate impairment; 41 to 60 refers to severe impairment; 61 to 80 indicates debilitating back pain; 81 to 100 indicates that the patient is bedridden [13]. The patients were asked to complete ODI and VAS forms before surgery and on the final visit.
The patients’ medical records were carefully reviewed to extract data relevant to our study, including operative time, average blood loss during surgery, hematoma formation, wound infection, CSF leak, deep vein thrombosis, and length of stay after surgery neurologic deficit.
The Analysis of Variance (ANOVA) was used to assess meaningful differences between non-continuous variables; however, the regression analysis evaluated differences in continuous variables. Moreover, P<0.05 was considered significant. SPSS performed data analysis.
3. Results
We evaluated 500 patients who were eligible to enter the study; 275 were women, and 225 were men with a mean±SD age of 40.3±5.2 years (range: 19-70 y). Demographic and descriptive characteristics of patients are presented in Table 1.
.jpg)
Surgical outcome measures (VAS, ODI) significantly improved postoperatively in all patients (Table 2).
.jpg)
Concerning surgery-related parameters, no significant difference was found between study groups (Table 3).
4. Discussion
Obesity is more prevalent in the United States, compared with other countries [14]. Several studies have demonstrated a higher complication rate and wound problems in obese patients than non-obese patients who underwent spine surgery [15]. Various types of local changes, such as tissue ischemia and decreased resistance to infection, are considered responsible for these complications [16]. Fat tissue vascular insufficiency and more enormous wound wall may be linked to these complications. Longer operative time increases the chance of wound problems in obese patients [17].
Carragee et al. suggested an association between increased BMI and recurrent disc herniation [18]. It is also revealed by Djurasovic et al. that Obesity also increases the risk of surgical site infection, blood loss, and position-associated nerve palsies [19]. Operative time and hospital stay were significantly longer in obese patients [20].
Other studies have found different findings. Quah et al. concluded that obesity was not a risk factor for recurrent disc herniation following lumbar microdiscectomy [21]. Andreshak et al. [22], obese and non-obese patients were not significantly different regarding surgical complications and outcome. In a study performed by Yadla and colleagues [23], BMI did not affect surgical complications.
As we could expect, minimally invasive spine surgeries have lower complication rates than the conventional type, and it could be an alternative for obese patients [24]. Endoscopic lumbar discectomy does not have more significant complications and recurrent disc herniations in obese than non-obese patients [25]. In a study performed by Barber et al. [26], tubular microdiscectomy and open microdiscectomy for lumbar disc herniations had similar outcomes. Ruan et al. [27] conducted a study to compare the outcome of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy. Percutaneous endoscopic lumbar discectomy did not offer an advantage over open lumbar microdiscectomy regarding the clinical outcome.
We designed a retrospective case series study to determine in a real-world setting whether patients with different BMI had any difference in clinical outcome and surgery-related parameters following lumbar microscopic discectomy.
This study and former analytical research indicated dramatic improvement in pain, disability, and health quality in obese and non-obese patients. In another study over the elderly (older than 65 years), Gepstein et al. [25], lumbar decompression was equally effective in pain relief and disability in obese and nonobese patients.
In analytical research, Rihn et al. [28] concluded no correlation between obesity and outcome measures after lumbar spinal canal stenosis surgery. The meta-analysis findings performed by Jin Jiang et al. [29] revealed that increased BMI is associated with higher surgical complications. McGuire et al. [30] performed a subgroup analysis study found that infection rate and operative time were more significant in morbidly obese patients.
In the current study, no association was found between obesity and other surgical and health-related complications, including the operative time, mean blood loss during surgery, hematoma formation, wound infection, CSF leak, deep vein thrombosis, length of stay after surgery, recurrent disc herniation and neurologic deficit. A prospective study designed by Rosen et al. [31]showed that BMI did not influence the outcome measures, operative time, and hospital stay. Contrarily, Telfeian et al. [32] mentioned that outcome measures were dramatically related to BMI.
Comorbid disorders such as ischemic heart disease and diabetes mellitus are more prevalent in Obese patients undergoing spine surgery, i.e., independent predictors of surgical complications [33]. To investigate the effect of just BMI on the outcome, we excluded patients with comorbid disorders. Our reason to exclude those with comorbidities is that complications from underlying comorbidities may be incorrectly attributed to the BMI.Our results do not support the hypothesis that obesity is associated with worse outcomes after lumbar microdiscectomy [34, 35]. At the 24-month follow-up evaluation, the obese and nonobese patient population showed significant mean improvements in all outcome measures.
5. Conclusion
Even with the limitations mentioned above, we can conclude that the findings from this study showed that BMI does not adversely impact the outcome of patients undergoing lumbar microdiscectomy. This study has some limitations which have to be pointed out. The small patient population (especially in the underweight group) and the retrospective nature of the survey with its limitations including Inferior level of evidence in contrast to prospective studies, subject to confounding (other risk factors may be present, i.e., not measured), cannot assess causality, just correlation.
Ethical Considerations
Compliance with ethical guidelines
We obtained approval from the ethics committee of Urmia University of Medical Sciences, West Azarbaijan, Iran (Code: IR.UMSU.REC.1399.307). Written informed consent was obtained from all patients.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All steps of the study were performed by Dr. Amir Abbas Ghasemi.
Conflict of interest
The author declared no conflict of interest.
References
- Hruby A, Hu FB. The epidemiology of obesity: A big picture. PharmacoEconomics. 2015; 33(7):673-89 [DOI:10.1007/s40273-014-0243-x] [PMID] [PMCID]
- Reilly JJ, El_Hamdouchi A, Diouf A, Monyeki A, Somda SA. Determining the worldwide prevalence of obesity. The Lancet. 2018; 391(10132):1773-4. [DOI:10.1016/S0140-6736(18)30794-3]
- Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity. 2008; 16(10):2323-30. [DOI:10.1038/oby.2008.351] [PMID]
- Olsen MA, Nepple JJ, Riew KD, Lenke LG, Bridwell KH, Mayfield J, et al. Risk factors for surgical site infection following orthopedic spinal operations. The Journal of Bone and Joint Surgery. 2008; 90(1):62-9. [DOI:10.2106/JBJS.F.01515] [PMID]
- Jackson KL, Devine JG. The effects of obesity on spine surgery: A systematic review of the literature. Global Spine Journal. 2016; 6(4):394-400. [DOI:10.1055/s-0035-1570750] [PMID] [PMCID]
- Kalanithi PA, Arrigo R, Boakye M. Morbid obesity increases cost and complication rates in spinal arthrodesis. Spine. 2012; 37(11):982-8 [DOI:10.1097/BRS.0b013e31823bbeef] [PMID]
- Owens RK 2nd, Djurasovic M, Onyekwelu I, Bratcher KR, McGraw KE, Carreon LY. Outcomes and revision rates in normal, overweight, and obese patients 5 years after lumbar fusion. The Spine Journal. 2016; 16(10):1178-83. [PMID]
- Buerba RA, Fu MC, Gruskay JA, Long WD 3rd, Grauer JN. Obese Class III patients at significantly greater risk of multiple complications after lumbar surgery: An analysis of 10,387 patients in the ACS NSQIP database. The Spine Journal. 2014; 14(9):2008-18. [DOI:10.1016/j.spinee.2013.11.047] [PMID]
- Carr EC, Meredith P, Chumbley G, Killen R, Prytherch DR, Smith GB. Pain: A quality of care issue during patients’ admission to hospital. Journal of Advanced Nursing. 2014; 70(6):1391-403 [DOI:10.1111/jan.12301] [PMID]
- Nuttall FQ. Body mass index: Obesity, BMI, and health: A critical review. Nutrition Today. 2015; 50(3):117-28. [DOI:10.1097/NT.0000000000000092] [PMID] [PMCID]
- Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine. 2005; 30(11):1331-4.[DOI:10.1097/01.brs.0000164099.92112.29] [PMID]
- Mehra A, Baker D, Disney S, Pynsent PB. Oswestry Disability Index scoring made easy. Annals of The Royal College of Surgeons of England. 2008; 90(6):497-9. [DOI:10.1308/003588408X300984] [PMID] [PMCID]
- Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine. 2000; 25(24):3115-24. [DOI:10.1097/00007632-200012150-00006] [PMID]
- WHO Consultation on Obesity, World Health Organization. Obesity: Preventing and managing the global epidemic: Report of a WHO consultation. Geneva: World Health Organization; 2000. https://apps.who.int/iris/handle/10665/42330?locale-attribute=en&
- Thelwall S, Harrington P, Sheridan E, Lamagni T. Impact of obesity on the risk of wound infection following surgery: Results from a nationwide prospective multicenter cohort study in England. Clinical Microbiology and Infection. 2015; 21(11):1008.e1-8. [DOI:10.1016/j.cmi.2015.07.003] [PMID]
- Eming SA, Martin P, Tomic-Canic M. Wound repair and regeneration: Mechanisms, signaling, and translation. Science Translational Medicine. 2014; 6(265):265sr6. [DOI:10.1126/scitranslmed.3009337] [PMID] [PMCID]
- Atiyeh BS, Ioannovich J, Al-Amm CA, El-Musa KA. Management of acute and chronic open wounds: The importance of moist environment in optimal wound healing. Current Pharmaceutical Biotechnology. 2002; 3(3):179-95. [DOI:10.2174/1389201023378283] [PMID]
- Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: The effects of fragment type and annular competence. The Journal of Bone and Joint Surgery. 2003; 85(1):102-8. [DOI:10.2106/00004623-200301000-00016]
- Djurasovic M, Bratcher KR, Glassman SD, Dimar JR, Carreon LY. The effect of obesity on clinical outcomes after lumbar fusion. Spine. 2008; 33(16):1789-92. [DOI:10.1097/BRS.0b013e31817b8f6f] [PMID]
- Fanuele JC, Abdu WA, Hanscom B, Weinstein JN. Association between obesity and functional status in patients with spine disease. Spine. 2002; 27(3):306-12. [DOI:10.1097/00007632-200202010-00021] [PMID]
- Quah C, Syme G, Swamy GN, Nanjayan S, Fowler A, Calthorpe D. Obesity and recurrent intervertebral disc prolapse after lumbar microdiscectomy. Annals of The Royal College of Surgeons of England. 2014; 96(2):140-3. [DOI:10.1308/003588414X13814021676873] [PMID] [PMCID]
- Andreshak TG, An Howard S, Hall J, Stein B. Lumbar spine surgery in the obese patient. Journal of Spinal Disorders. 1997; 10(5):376-9. [DOI:10.1097/00002517-199710000-00003]
- Yadla S, Malone J, Campbell PG, Maltenfort MG, Harrop JS, Sharan AD, et al. Obesity and spine surgery: Reassessment based on a prospective evaluation of perioperative com-plications in elective degenerative thoracolumbar procedures. The Spine Journal. 2010; 10(7):581-7. [DOI:10.1016/j.spinee.2010.03.001] [PMID]
- Othman YA, Alhammoud A, Aldahamsheh O, Vaishnav AS, Gang CH, Qureshi SA. Minimally invasive spine lumbar surgery in obese patients: A systematic review and meta-analysis. HSS Journal : The Musculoskeletal Journal of Hospital for Special Surgery. 2020; 16(2):168-76 [DOI:10.1007/s11420-019-09735-6] [PMID] [PMCID]
- Gepstein R, Shabat S, Arinzon ZH, Berner Y, Catz A, Folman Y. Does obesity affect the results of lumbar decompressive spinal surgery in the elderly? Clinical Orthopaedics and Related Research. 2004; (426):138-44. [DOI:10.1097/01.blo.0000141901.23322.98] [PMID]
- Barber SM, Nakhla J, Konakondla S, Fridley JS, Oyelese AA, Gokaslan ZL, et al. Outcomes of endoscopic discectomy compared with open microdiscectomy and tubular microdiscectomy for lumbar disc herniations: A meta-analysis. Journal of Neurosurgery. Spine. 2019; 6:1-14. [PMID]
- Ruan W, Feng F, Liu Z, Xie J, Cai L, Ping A. Comparison of percutaneous endoscopic lumbar discectomy versus open lumbar microdiscectomy for lumbar disc herniation: A meta-analysis. International Journal of Surgery. 2016; 31:86-92. [DOI:10.1016/j.ijsu.2016.05.061] [PMID]
- Rihn JA, Radcliff K, Hilibrand AS, Anderson DT, Zhao W, Lurie J, et al. Does obesity affect outcomes of treatment for lumbar stenosis and degenerative spondylolisthesis? Analysis of the Spine Patient Outcomes Research Trial (SPORT). Spine. 2012; 37(23):1933-46. [DOI:10.1097/BRS.0b013e31825e21b2] [PMID] [PMCID]
- Jiang J, Teng Y, Fan Z, Khan S, Xia Y. Does obesity affect the surgical outcome and complication rates of spinal surgery? A meta-analysis. Clinical Orthopaedics and Related Research. 2014; 472(3):968-75. [DOI:10.1007/s11999-013-3346-3] [PMID] [PMCID]
- McGuire KJ, Khaleel MA, Rihn JA, Lurie JD, Zhao W, Weinstein JN. The effect of high obesity on outcomes of treatment for lumbar spinal conditions: Subgroup analysis of the spine patient outcomes research trial. Spine. 2014; 39(23):1975-80. [DOI:10.1097/BRS.0000000000000577] [PMID] [PMCID]
- Rosen DS, Ferguson SD, Ogden AT, Huo D, Fessler RG. Obesity and self reported outcome after minimally invasive lumbar spinal fusion surgery. Neurosurgery. 2008; 63(5):956-60; discussion 960. [DOI:10.1227/01.NEU.0000313626.23194.3F] [PMID]
- Telfeian AE, Reiter GT, Durham SR, Marcotte P. Spine surgery in morbidly obese patients. Journal of Neurosurgery. 2002; 97(1 Suppl):20-4. [DOI:10.3171/spi.2002.97.1.0020] [PMID]
- Patel N, Bagan B, Vadera S, Maltenfort MG, Deutsch H, Vaccaro AR, et al. Obesity and spine surgery: Relation to perioperative complications. Journal of Neurosurgery. Spine. 2007; 6(4):291-7. [DOI:10.3171/spi.2007.6.4.1] [PMID]
- Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity: An evaluation of potential bias. Vital & Health Statistics. Series 3,. 2018; (42):1-21. [PMID]
- Valentijn TM, Galal W, Tjeertes EK, Hoeks SE, Verhagen HJ, Stolker RJ. The obesity paradox in the surgical population. The surgeon : Journal of the Royal Colleges of Surgeons of Edinburgh and Ireland. 2013; 11(3):169-76. [DOI:10.1016/j.surge.2013.02.003] [PMID]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






