Tue, Feb 3, 2026
Volume 9 - Continuous Publishing
Iran J Neurosurg 2023, 9 - Continuous Publishing: 38-43 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pandey S, Chore N, Kumar P, Saxena A. Intradural Extramedullary Capillary Hemangioma of Spinal Cord: A Case Report and an Updated Review. Iran J Neurosurg 2023; 9 : 6
URL: http://irjns.org/article-1-317-en.html
URL: http://irjns.org/article-1-317-en.html
1- Department of Neurosurgery, Atal Bihari Vajpayee Institute of Medical Sciences, Dr. Ram Manohar Lohia Hospital, New Delhi, India , drsharad23@yahoo.com
2- Department of Neurosurgery, Atal Bihari Vajpayee Institute of Medical Sciences, Dr. Ram Manohar Lohia Hospital, New Delhi, India
2- Department of Neurosurgery, Atal Bihari Vajpayee Institute of Medical Sciences, Dr. Ram Manohar Lohia Hospital, New Delhi, India
Full Text [PDF 808 kb]
(954 Downloads)
| Abstract (HTML) (3377 Views)
Full Text: (1585 Views)
1. Background and Importance
Primary spinal cord tumors are less common compared with primary tumors of the brain. They constitute only 2% to 4% of all primary central nervous system (CNS) tumors [1, 2]. Common spinal intradural tumors are benign nerve sheath tumors, meningioma, and ependymoma. Capillary hemangiomas in the spinal location are rare, with only about 21 cases reported worldwide. Capillary hemangiomas are believed to be hamartomatous proliferations of vascular endothelial cells. The surgical implication of this is the risk of excessive bleeding during surgery, which can lead to adverse outcomes. Only a few cases have been reported as intradural capillary hemangioma [3, 4]. We are reporting a case of a 38-year-old womanwith capillary hemangioma in the cauda equine region. This study aims to present a detailed and documented analysis of this particular case, including symptoms, diagnosis, treatment, and outcome. Capillary hemangiomas should be kept as rare but plausible differentials in the spinal intradural extramedullarywith the potential for intra-operative excessive bleeding.
2. Case Presentation
A 38-year-old woman came with majorcomplaints of low backache for 4 months. The pain was lancinating in nature. It was radiating to the right thigh and leg along with numbness and weakness in the right foot. The pain was increasing during the night and was not relieved by medicine. The intensity of the pain gradually increased with time. In physical findings, the straight leg raising test was positive on the right side. She also presented with left ankle weakness and sensory deficits in the left L3-L4 dermatome. No local spinal tenderness was observed.
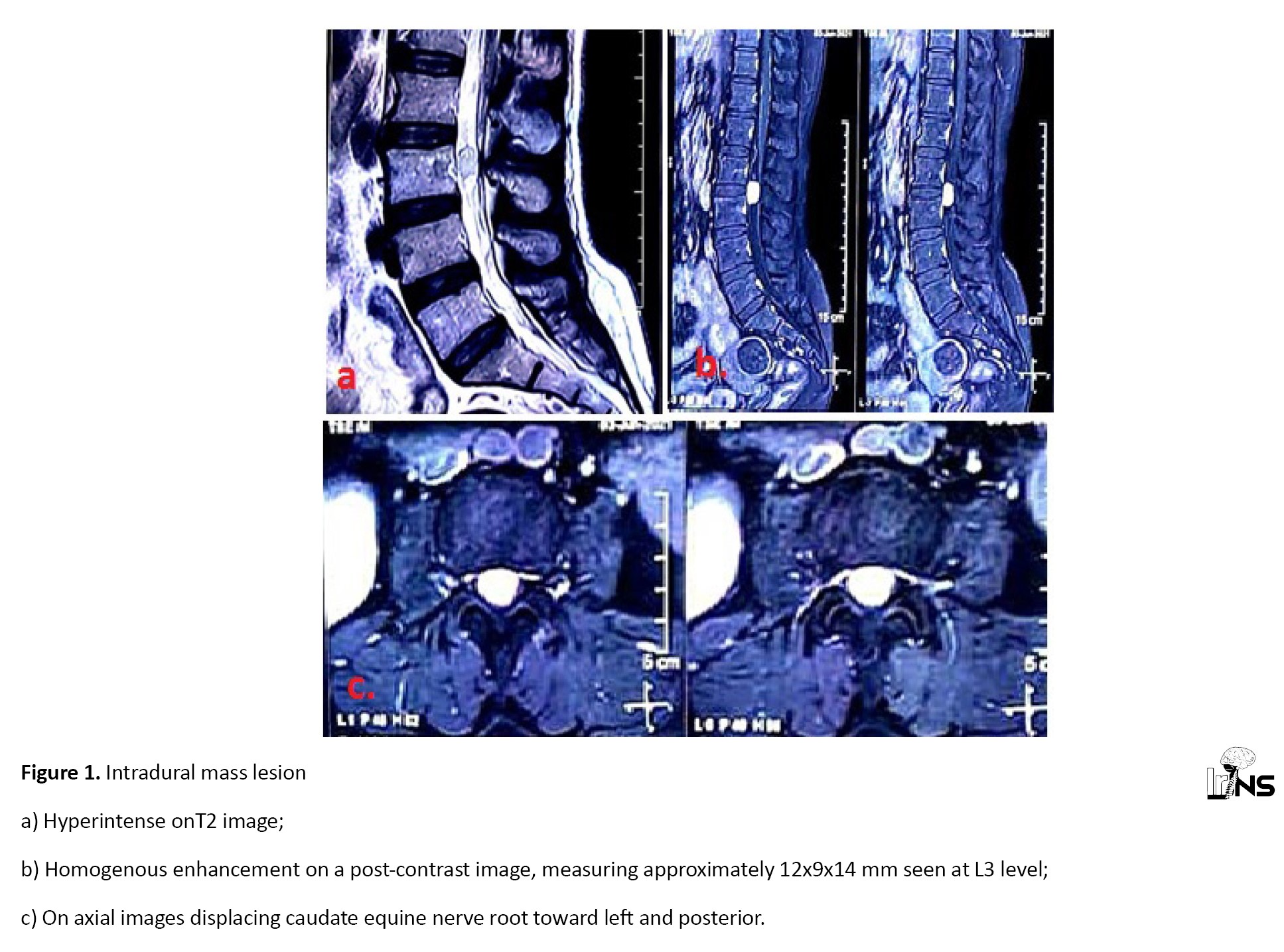
Contrast-enhanced magnetic resonance imaging (MRI)of the lumbosacral spine showed a well-defined lobulated lesion in the spinal canal regional L2-L3 level, in thecal sac, in an intradural compartment with dimensions as 18x14x11 mm, which was isointense on T1 weighted image and slight hyperintensity on T2 weighted image (Figure 1). There was a displacement of nerve roots with gadolinium contrast homogenous enhancement. A provisional diagnosis of benign nerve sheath tumor was put forward. The whole-brain MRI screening was done to rule out intracranial lesions. The rest of the routine investigations were within normal limits except for blood sugar and HbA1c-7.9%. The patient was newly diagnosed with diabetes mellitus type 2 and started on appropriate oral hypoglycemic drugs by the endocrinology team.
The patient underwent L2-L3 laminectomy with tumor excision under general anesthesia in a prone position. A reddish-brown tumor was visualized intraoperatively on midline durotomy at the corresponding level. The tumor was seen compressing underlying nerve roots. With fine dissection, the tumor was resected out and was found to be originating from a single nerve root which had to be sacrificed for complete tumor excision. After achieving complete hemostasis, primary dural closure was done with prolene 4-0.
Histopathological examination of the specimen revealed a well-circumscribed tumor composed of capillaries arranged in the lobular configuration without atypia or mitotic activity suggestive of capillary hemangioma (Figure 2). The patient was followed up in an outpatient setup with serial MRI studies and clinical examinationand showed improvement in symptoms and no recurrences todate.
3. Discussion
Histological features of lobular capillary hemangioma are the presence of normal-sized (size of the capillary) channels tightly aggregated into nodules, each supplied by a feeding vessel [5].
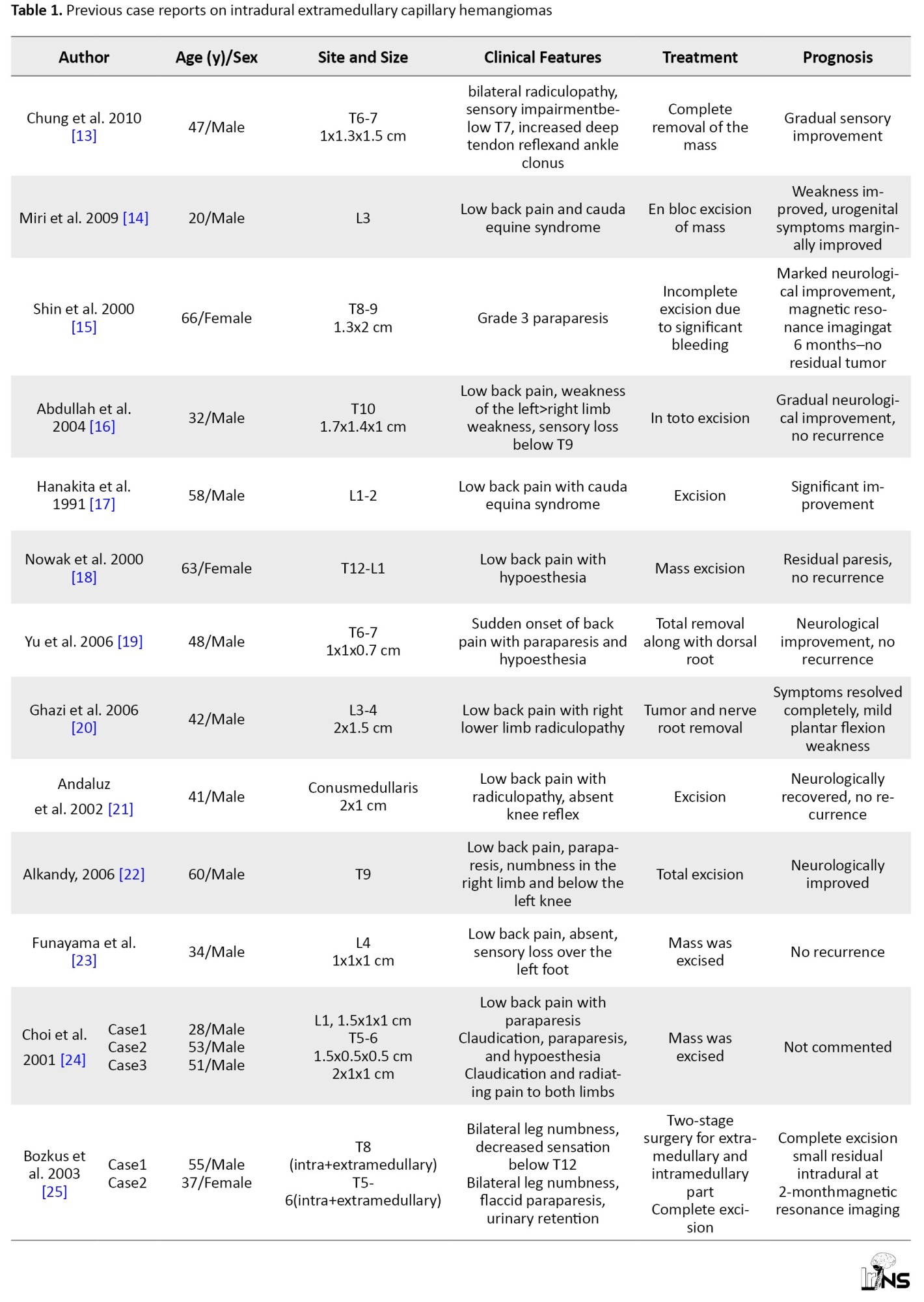
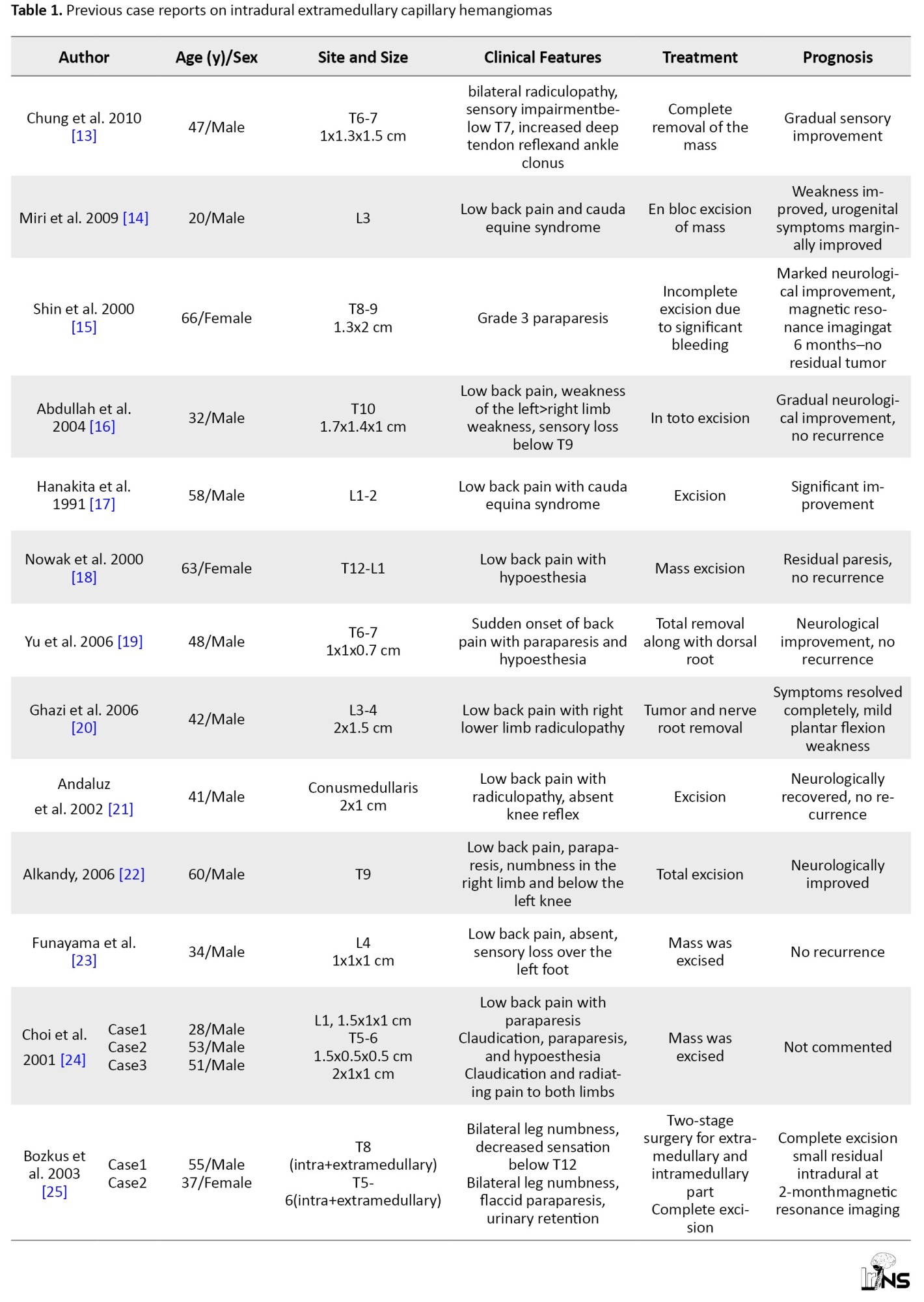
Other than the usual locations of capillary hemangiomas, i.e. cutaneous and subcutaneous, they are rarely seen in neuroaxis [6, 7]. Frequently reported capillary hemangiomas are dural [8], peripheral nerves, muscles [5], skin [9], and mucous membrane [10]. So far, only 21 cases reported as per an advancedsearch on PubMed regarding intradural spinal capillary hemangiomas of the cauda equine region [11]. Hemangiomas may arise from blood vessels of a nerve root in the cauda equine, an inner surface of the dura, or the pial surface of the spinal cord, and the adherence of other roots reflects its associated arachnoiditis [12]. Capillary hemangioma presents as a space-occupying mass leading to chronic progressive myelopathy or radiculopathy and sensory-motor deficits with pain. Sudden neurological deterioration can occur due to the risk of bleeding. We achieved a gross total resection of the tumor in our patient with no recurrences todate. This is at par with the current literature evidence briefly discussed in Table 1.
4. Conclusion
Capillary hemangiomas are rare in intradural extramedullary space with clinical and radiological similarities with common spinal lesions.Therefore,they should be considered a differential diagnosis before surgical intervention.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from the patient.
Funding
The research did not receive any grant from funding agencies in the public, commercial, or non-profitsectors.
Authors' contributions
All authors contribute to the design, running, and writing of all parts of the research.
Conflict of interest
The authors declared no conflict of interest.
References
Primary spinal cord tumors are less common compared with primary tumors of the brain. They constitute only 2% to 4% of all primary central nervous system (CNS) tumors [1, 2]. Common spinal intradural tumors are benign nerve sheath tumors, meningioma, and ependymoma. Capillary hemangiomas in the spinal location are rare, with only about 21 cases reported worldwide. Capillary hemangiomas are believed to be hamartomatous proliferations of vascular endothelial cells. The surgical implication of this is the risk of excessive bleeding during surgery, which can lead to adverse outcomes. Only a few cases have been reported as intradural capillary hemangioma [3, 4]. We are reporting a case of a 38-year-old womanwith capillary hemangioma in the cauda equine region. This study aims to present a detailed and documented analysis of this particular case, including symptoms, diagnosis, treatment, and outcome. Capillary hemangiomas should be kept as rare but plausible differentials in the spinal intradural extramedullarywith the potential for intra-operative excessive bleeding.
2. Case Presentation
A 38-year-old woman came with majorcomplaints of low backache for 4 months. The pain was lancinating in nature. It was radiating to the right thigh and leg along with numbness and weakness in the right foot. The pain was increasing during the night and was not relieved by medicine. The intensity of the pain gradually increased with time. In physical findings, the straight leg raising test was positive on the right side. She also presented with left ankle weakness and sensory deficits in the left L3-L4 dermatome. No local spinal tenderness was observed.
Contrast-enhanced magnetic resonance imaging (MRI)of the lumbosacral spine showed a well-defined lobulated lesion in the spinal canal regional L2-L3 level, in thecal sac, in an intradural compartment with dimensions as 18x14x11 mm, which was isointense on T1 weighted image and slight hyperintensity on T2 weighted image (Figure 1). There was a displacement of nerve roots with gadolinium contrast homogenous enhancement. A provisional diagnosis of benign nerve sheath tumor was put forward. The whole-brain MRI screening was done to rule out intracranial lesions. The rest of the routine investigations were within normal limits except for blood sugar and HbA1c-7.9%. The patient was newly diagnosed with diabetes mellitus type 2 and started on appropriate oral hypoglycemic drugs by the endocrinology team.
The patient underwent L2-L3 laminectomy with tumor excision under general anesthesia in a prone position. A reddish-brown tumor was visualized intraoperatively on midline durotomy at the corresponding level. The tumor was seen compressing underlying nerve roots. With fine dissection, the tumor was resected out and was found to be originating from a single nerve root which had to be sacrificed for complete tumor excision. After achieving complete hemostasis, primary dural closure was done with prolene 4-0.
Histopathological examination of the specimen revealed a well-circumscribed tumor composed of capillaries arranged in the lobular configuration without atypia or mitotic activity suggestive of capillary hemangioma (Figure 2). The patient was followed up in an outpatient setup with serial MRI studies and clinical examinationand showed improvement in symptoms and no recurrences todate.
3. Discussion
Histological features of lobular capillary hemangioma are the presence of normal-sized (size of the capillary) channels tightly aggregated into nodules, each supplied by a feeding vessel [5].
Other than the usual locations of capillary hemangiomas, i.e. cutaneous and subcutaneous, they are rarely seen in neuroaxis [6, 7]. Frequently reported capillary hemangiomas are dural [8], peripheral nerves, muscles [5], skin [9], and mucous membrane [10]. So far, only 21 cases reported as per an advancedsearch on PubMed regarding intradural spinal capillary hemangiomas of the cauda equine region [11]. Hemangiomas may arise from blood vessels of a nerve root in the cauda equine, an inner surface of the dura, or the pial surface of the spinal cord, and the adherence of other roots reflects its associated arachnoiditis [12]. Capillary hemangioma presents as a space-occupying mass leading to chronic progressive myelopathy or radiculopathy and sensory-motor deficits with pain. Sudden neurological deterioration can occur due to the risk of bleeding. We achieved a gross total resection of the tumor in our patient with no recurrences todate. This is at par with the current literature evidence briefly discussed in Table 1.
4. Conclusion
Capillary hemangiomas are rare in intradural extramedullary space with clinical and radiological similarities with common spinal lesions.Therefore,they should be considered a differential diagnosis before surgical intervention.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from the patient.
Funding
The research did not receive any grant from funding agencies in the public, commercial, or non-profitsectors.
Authors' contributions
All authors contribute to the design, running, and writing of all parts of the research.
Conflict of interest
The authors declared no conflict of interest.
References
- Allen IM. Tumours Involving the cauda equina: A review of their clinical features and differential diagnosis. The Journal of Neurology and Psychopathology. 1930; 11(42):111-43. [DOI:10.1136/jnnp.s1-11.42.111] [PMID] [PMCID]
- Rasmussen TB, Kernohan JW, Adson AW. Pathologic classification, with surgical consideration, of intraspinal tumors. Annals of Surgery. 1940; 111(4):513-30. [DOI:10.1097/00000658-194004000-00001] [PMID] [PMCID]
- Sonawane DV, Jagtap SA, Mathesul AA. Intraduralextramedullary capillary hemangioma of lower thoracic spinal cord. Indian Journal of Orthopaedics. 2012; 46(4):475-8. [DOI:10.4103/0019-5413.97262] [PMID] [PMCID]
- Takata Y, Sakai T, Higashino K, Goda Y, Tezuka F, Sairyo K. Intradural extramedullary capillary hemangioma in the upper thoracic spine: A review of the literature. Case Reports in Orthopedics. 2014; 2014:604131. [DOI:10.1155/2014/604131] [PMID] [PMCID]
- Enzinger FM. Benign tumors and tumorlike lesions of blood vessels. In: Enzinger FM, Weiss SW, editors. Soft tissue tumors. Louis: Mosby; l988. [Link]
- Pearl GS, Takei Y. Hemangioendothelioma of the neuraxis: An ultrastructural study. Neurosurgery. l982; 11(4):486-90. [DOI:10.1227/00006123-198210000-00004] [PMID]
- Pearl GS, Takei Y, Tindall GT, O'Brien MS, Payne NS, Hoffman JC. Benign hemangioendothelioma involving the central nervous system: Strawberry nevus of the neuraxis. Neurosurgery. l980; 7(3):249-56. [DOI:10.1227/00006123-198009000-00008] [PMID]
- Burger PC, Scheithauer BW. Tumors of the central nervous system. Washington DC: Armed Forces Institute of Pathology; l994. [Link]
- Pesce C, Valente S, Gandolfo AM, Lenti E. Intravascular lobular capillary haemangioma of the lip. Histopathology. l996; 29(4):382-4. [DOI:10.1111/j.1365-2559.1996.tb01425.x] [PMID]
- El-Sayed Y, Al-Serhani A. Lobular capillary hemangioma (pyogenic granuloma) of the nose.The Journal of Laryngology & Otology. l997; 111(10):941-5. [DOI:10.1017/S0022215100139027] [PMID]
- Hughes LP, Largoza G, Montenegro TS, Matias CM, Stefanelli A, Curtis MT, et al. Intraduralextramedullary capillary hemangioma of the cauda equina: Case report of a rare spinal tumor. Spinal Cord Series and Cases. 2021; 7(1):21. [DOI:10.1038/s41394-021-00383-9] [PMID] [PMCID]
- Zander DR, Lander P, Just N, Albrecht S, Mohr G. Magnetic resonance imaging features of a nerve root capillary hemangioma of the spinal cord: Case report. Canadian Association of Radiologists Journal. 1998; 49(6):398-400. [Link]
- Chung SK, Nam TK, Park SW, Hwang SN. Capillary hemangioma of the thoracic spinal cord. Journal of Korean Neurosurgical Society. 2010; 48(3):272-5. [DOI:10.3340/jkns.2010.48.3.272] [PMID] [PMCID]
- Miri SM, Habibi Z, Hashemi M, Meybodi AT, Tabatabai SA. Capillary hemangioma of cauda equina: A case report. Cases Journal. 2009; 2(1):80. [DOI:10.1186/1757-1626-2-80] [PMID] [PMCID]
- Shin JH, Lee HK, Jeon SR, Park SH. Spinal intradural capillary hemangioma: MR findings. American Journal of Neuroradiology. 2000; 21(5):954-6. [Link]
- Abdullah DC, Raghuram K, Phillips CD, Jane JA, Miller B. Thoracic intradural extramedullary capillary hemangioma. American Journal of Neuroradiology. 2004; 25(7):1294-6. [Link]
- Hanakita J, Suwa H, Nagayasu S, Suzuki H. Capillary hemangioma in the cauda equina: Neuroradiological findings. Neuroradiology. 1991; 33:458-61. [Link]
- Nowak DA, Gumprecht H, Stölzle A, Lumenta CB. Intraneural growth of a capillary haemangioma of the cauda equina. Acta Neurochirurgica. 2000; 142:463-8. [Link]
- Yu H, Lee LY, Hwang SN, Yoo SM, Lee HY, Song IS, et al. Intradural extramedullary capillary hemangioma with long segment of transient cord edema: A case report. Journal of the Korean Radiological Society. 2006; 54(5):343-7. [DOI:10.3348/jkrs.2006.54.5.343]
- Ghazi NG, Jane JA, Lopes MB, Newman SA. Capillary hemangioma of the cauda equina presenting with radiculopathy and papilledema.Journal of Neuro-Ophthalmology. 2006; 26(2):98-102. [DOI:10.1097/01.wno.0000222973.55486.d2] [PMID]
- Andaluz N, Balko MG, Stanek J, Morgan C, Schwetschenau PR. Lobular capillary hemangioma of the spinal cord: Case report and review of the literature. Journal of Neuro-Oncology. 2002; 56:261-4. [Link]
- Alkandy LM, Hercules S, Balamurali G, Reid H, Herwadkar A, Holland JP. Thoracic intradural extramedullary capillary hemangioma. British Journal of Neurosurgery. 2006; 20:235-8. [DOI:10.1080/02688690600852506] [PMID]
- Funayama T, Sakane M, Murai S, Ochiai N. Multiple capillary hemangiomas of the cauda equina at a level of a single vertebra. Journal of Orthopaedic Science. 2010; 15(4):598-602. [Link]
- Choi BY, Chang KH, Choe G, Han MH, Park SW, Yu IK, et al. Spinal intradural extramedullary capillary hemangioma: MR imaging findings. American Journal of Neuroradiology. 2001; 22(4):799-802. [Link]
- Bozkus H, Tanriverdi T, Kizilkilic O, Türeci E, Oz B, Hanci M. Capillary hemangiomas of the spinal cord: Report of two cases. Minim Invasive Neurosurg. 2003; 46(1):41-6. [DOI:10.1055/s-2003-37958] [PMID]
Type of Study: Case report |
Subject:
Spine
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |