Tue, Feb 3, 2026
Volume 9 - Continuous Publishing
Iran J Neurosurg 2023, 9 - Continuous Publishing: 127-132 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rahimizadeh A, Ahmadi S, Soufiani H, L. Williamson W, Amirzadeh M, Rahimizadeh S. Ossification of the Ligamentum Flavum of the Cervical Spine in an Iranian Woman: Report of a Case With Myelopathy and Review of the Literature. Iran J Neurosurg 2023; 9 : 17
URL: http://irjns.org/article-1-330-en.html
URL: http://irjns.org/article-1-330-en.html
Abolfazl Rahimizadeh *1 

 , Seyed-Ali Ahmadi2
, Seyed-Ali Ahmadi2 

 , Housain Soufiani2
, Housain Soufiani2 

 , Walter L. Williamson2
, Walter L. Williamson2 

 , Mahan Amirzadeh2
, Mahan Amirzadeh2 

 , Shaghayegh Rahimizadeh2
, Shaghayegh Rahimizadeh2 




 , Seyed-Ali Ahmadi2
, Seyed-Ali Ahmadi2 

 , Housain Soufiani2
, Housain Soufiani2 

 , Walter L. Williamson2
, Walter L. Williamson2 

 , Mahan Amirzadeh2
, Mahan Amirzadeh2 

 , Shaghayegh Rahimizadeh2
, Shaghayegh Rahimizadeh2 


1- Pars Advanced and Minimally Invasive Medical Manners Research Center, Pars Hospital, University of Medical Sciences, Tehran, Iran , a_rahimizadeh@hotmail.com
2- Pars Advanced and Minimally Invasive Medical Manners Research Center, Pars Hospital, University of Medical Sciences, Tehran, Iran
2- Pars Advanced and Minimally Invasive Medical Manners Research Center, Pars Hospital, University of Medical Sciences, Tehran, Iran
Keywords: Cervical myelopathy, Spine, Calcification of ligamentum flavum, Ossification of ligamentum flavum, Ossification of the posterior longitudinal ligament
Full Text [PDF 1304 kb]
(1590 Downloads)
| Abstract (HTML) (3625 Views)
Full Text: (2386 Views)
1. Introduction
The first example of cervical OLF was described in 1962 by Koizumi who reported this pathology in an autopsy of a 55-year-old man who had progressive quadriparesis for the last two years of his life [1]. The second instance was described by Kirita in 1973 in a woman with cervical myelopathy [2]. Since then, with the inclusion of the current presentation, 75 additional cases have been published so far [3-8]. Herein, we present an elderly Iranian woman with symptomatic cervical OLF who was managed by our team’s practice.
2. Case Presentation
A 68-year-old old woman was admitted due to an unsteady gait and weakness within all four limbs. Her neurological examination revealed alertness with spastic quadriparesis more prominent within the lower extremities. The tendon reflexes were hyperactive with positive Hoffmann and Babinski signs bilaterally. Her modified Japanese Orthopedic Association (mJOA) score at the time of admission was noted to be 10. MRI revealed a set of 2-level, bilaterally and posteriorly located masses compressing the dural sac at the C4-C5, and C5-C6 levels. Both were hypointense on T1- and T2-weighted images, compatible with the ossification of the ligamentum flavum (Figure 1a). A myelopathic patch was also demonstrated at the C4-C5 spinal level (Figure 1b). Axial computed tomography (CT scan) demonstrated elliptical, immense, and ossified masses, at both levels (Figure 2). With the diagnosis of a 2-level bilateral OLF, the patient underwent a C4 to C6 laminectomy. After making a longitudinal groove on the side of the lateral masses, laminectomy with a high-speed air drill was undertaken. It was at this time that a level of dural sac compression was noted to be produced by overtly large ossified masses. Subsequently, the masses displayed a mild adhesion to the dura and could be mobilized and then removed. After resection of the mass, the dural sac showed the expected re-expansion and adequate pulsation.
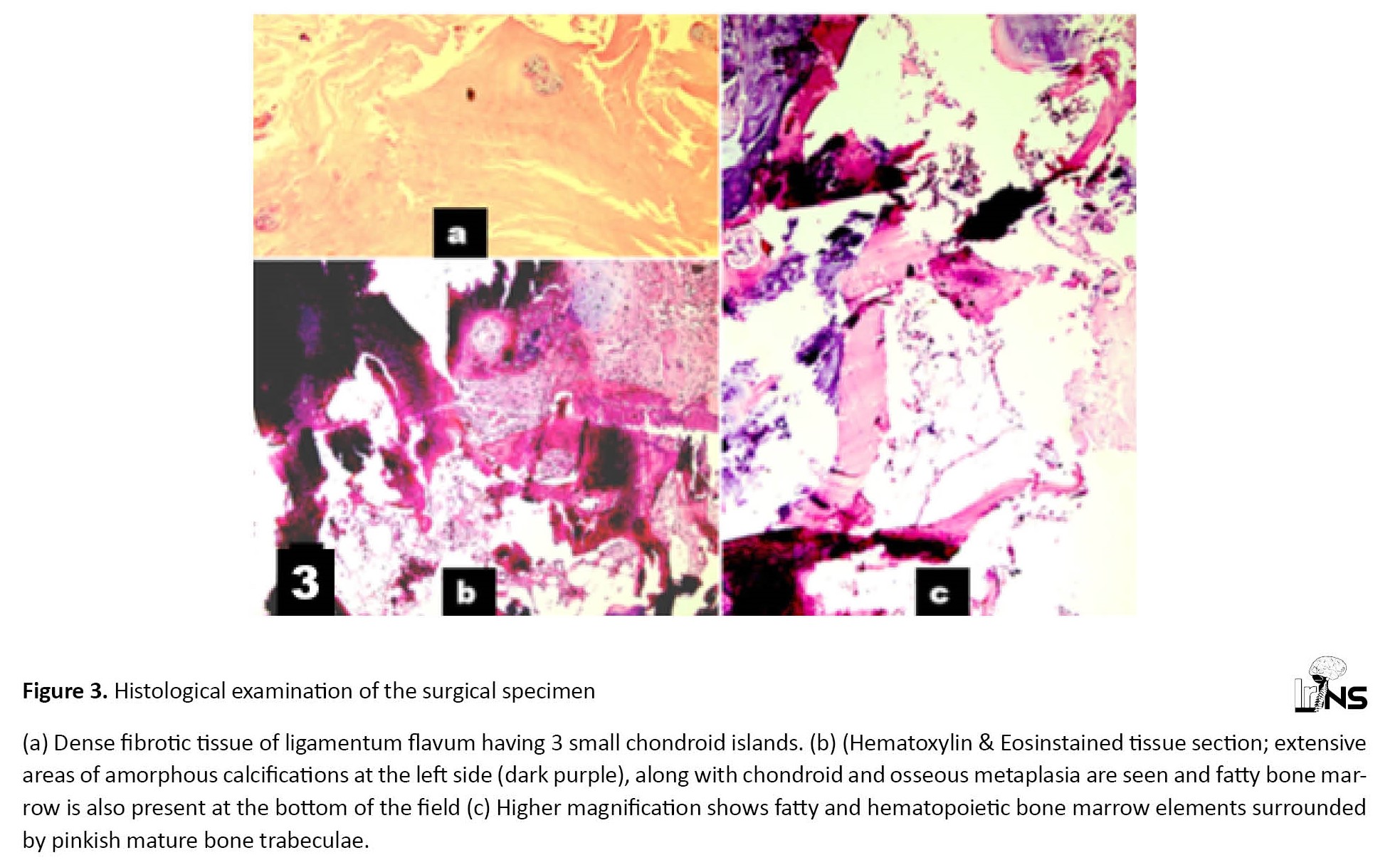
Histological examination of the surgical specimens revealed islands of endochondral ossification within the elastic ligament fibers which were compatible with the diagnosis of OLF (Figure 3). The post-operative course recovery was uneventful and the patient showed some evidence of regained function immediately following the surgical intervention. At one-year follow-up, her mJOA reached a scale score of 15, and surprisingly the mid-cervical myelopathic patch was resolved in the control MRI (Figure 4).
3. Discussion
Incidence
OLF most often affects the thoracic and lumbar regions whereas effect of the cervical spine leading to a resultant myeloradiculopathy remains a much infrequent occurrence [9-12]. The prevalence of asymptomatic OLF in East Asian populations is 38.5% and 26.5% in the thoracic and lumbar regions respectively, where its occurrence within the cervical spine is less than 1% [10, 13-16].
In a study conducted by Hiraoka et al., the incidence of OLF was found to be 34% in the postmortem autopsies of a large group of aged patients [17]. Accordingly, all discovered OLFs were overwhelmingly confined to the thoracic or lumbar spinal regions and not a single patient possessed such an anomaly within the cervical spine [17].
Fujimori et al. conducted a research study involving 1500 Japanese patients utilizing a multi-detector computed tomography scan [13]. While the prevalence of asymptomatic OLF within the thoracic spine was found to be 12%, its prevalence within the cervical spine was 0.3% [18].
The high rate of OLF within the thoracic spine is the direct result of the constant tension placed on the ligamentum flavum induced through the presence of thoracic kyphosis [9-14]. Contrarily, the exposure of the ligamentum flavum at the cervical spine to tension is shown to be less than that displayed within other regions of the vertebral column. Moreover, lordotic curvature of the cervical spine and the difference in the thickness of the yellow ligaments compared to the thoracic segments may also help to explain the overall low prevalence of COLF [3-8].
Ethnicity
Most of the published cases with cervical OLF are of East Asian ethnic descent [1-8]. However, its occurrence in Caucasians is not as infrequent as it was once supposed [3].
Clinical picture
Typical clinical features of COLFs at the time of diagnosis include an unsteady gait, decreased muscle strength, sensory disturbances, and urinary dysfunction. Such findings are noted to be indistinguishable from cord compressions seen within cervical spondylotic myelopathies [3-8]. The interval from the onset of the disease to the correct diagnosis is usually very lengthy and can range from one to several years.
Imaging
The exact location and shape of the OLF, the number of affected levels, as well as the degrees of cord compression and the associated myelopathies can be best demonstrated by utilization of MRI [3-8]. A typical cervical OLF is visualized as a hypointense signal intensity mass at the level of the posterior margin of the spinal canal when viewed using T1-weighted sagittal MR images. A patient with cervical OLF myelopathy is observed as an intramedullary hyper-intense spot within T-2 weighted sagittal views at the time of diagnosis [3-8].
Most cervical OLFs are located within the subaxial segments and their occurrence in the upper cervical region is rare [3-8].
It is important to assess the exact size, shape, and extent of the ossified lesions before surgical intervention. To accomplish this goal, computerized tomography should be performed. On axial CT scans, the lesions are visualized as ossified masses from the facet joint to the base of the spinal process and can be either unilateral or bilateral [19, 20]. Reconstructed images of an OLF are primarily shown as an ossified mass at the posterior aspect of the spinal column at the site of the ligamentum flavum [3-8, 18-20].
Treatment
Symptomatic cases with cervical OLF should be followed closely with periodic examinations and MRI scans. A decompressive laminectomy and excision of the ossified masses are the mainstay of treatment in symptomatic sub-types [3-8]. The indications for surgery are cervical radiculopathy, myelopathy, or myeloradiculopathy. Bilateral occurrences usually display a tight adherence to the dura. Unilateral nodular OLF sub-types typically show a minimal amount of adhesion to the dura mater. A dural tear is not considered a frequent complication during the surgical removal of a cervical OLF.
Differential
Cervical OLF and cervical ligamentum flavum calcification (CLF) which are separate unique entities are sometimes confused with one another due to the many similarities they present [20, 21]. Imaging features and intraoperative findings will likewise mirror each other [20, 21]. The calcification of the ligamentum flavum, pseudogout, and calcium pyrophosphate dehydrate crystal deposition disease (CPPD), all belong to a single sub-category and can only truly be differentiated from OLF histopathologically [21, 22].
Outcome: The outcome after surgery depends on the duration of the symptoms, the anteroposterior diameter of the lesion, the degree of cord compression observed, the presence of myelopathy, and the specific type of OLF discovered. Our review has shown that surgical intervention for a cervical OLF is associated with a better prognosis when compared to thoracic subtypes.
4. Conclusion
COLF, although rare within non-East Asian populations, should be considered a possible cause of cervical myeloradiculopathy. Surgical excision of COLF is quite easier in the cervical spine with less adhesion and dural tear compared with the thoracic and lumbar OLFs, probably due to the rarity of concomitant dural ossification. Detection of this illusive condition requires a careful and concise neurological exam, the utilization of specific imaging features, a high level of adequate suspicion, and a solid working knowledge of the unique pathological features of this clinical presentation. As a whole, this rare phenomenon is markedly different from a simple calcification of the yellow ligament itself.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from the patient for publishing this report and the corresponding images.
Funding
The authors received no financial support.
Authors' contributions
All authors contributed equally to preparing this report.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
The authors appreciate Dr. Asgari (PhD) for his assistance.
References
The first example of cervical OLF was described in 1962 by Koizumi who reported this pathology in an autopsy of a 55-year-old man who had progressive quadriparesis for the last two years of his life [1]. The second instance was described by Kirita in 1973 in a woman with cervical myelopathy [2]. Since then, with the inclusion of the current presentation, 75 additional cases have been published so far [3-8]. Herein, we present an elderly Iranian woman with symptomatic cervical OLF who was managed by our team’s practice.
2. Case Presentation
A 68-year-old old woman was admitted due to an unsteady gait and weakness within all four limbs. Her neurological examination revealed alertness with spastic quadriparesis more prominent within the lower extremities. The tendon reflexes were hyperactive with positive Hoffmann and Babinski signs bilaterally. Her modified Japanese Orthopedic Association (mJOA) score at the time of admission was noted to be 10. MRI revealed a set of 2-level, bilaterally and posteriorly located masses compressing the dural sac at the C4-C5, and C5-C6 levels. Both were hypointense on T1- and T2-weighted images, compatible with the ossification of the ligamentum flavum (Figure 1a). A myelopathic patch was also demonstrated at the C4-C5 spinal level (Figure 1b). Axial computed tomography (CT scan) demonstrated elliptical, immense, and ossified masses, at both levels (Figure 2). With the diagnosis of a 2-level bilateral OLF, the patient underwent a C4 to C6 laminectomy. After making a longitudinal groove on the side of the lateral masses, laminectomy with a high-speed air drill was undertaken. It was at this time that a level of dural sac compression was noted to be produced by overtly large ossified masses. Subsequently, the masses displayed a mild adhesion to the dura and could be mobilized and then removed. After resection of the mass, the dural sac showed the expected re-expansion and adequate pulsation.
Histological examination of the surgical specimens revealed islands of endochondral ossification within the elastic ligament fibers which were compatible with the diagnosis of OLF (Figure 3). The post-operative course recovery was uneventful and the patient showed some evidence of regained function immediately following the surgical intervention. At one-year follow-up, her mJOA reached a scale score of 15, and surprisingly the mid-cervical myelopathic patch was resolved in the control MRI (Figure 4).
3. Discussion
Incidence
OLF most often affects the thoracic and lumbar regions whereas effect of the cervical spine leading to a resultant myeloradiculopathy remains a much infrequent occurrence [9-12]. The prevalence of asymptomatic OLF in East Asian populations is 38.5% and 26.5% in the thoracic and lumbar regions respectively, where its occurrence within the cervical spine is less than 1% [10, 13-16].
In a study conducted by Hiraoka et al., the incidence of OLF was found to be 34% in the postmortem autopsies of a large group of aged patients [17]. Accordingly, all discovered OLFs were overwhelmingly confined to the thoracic or lumbar spinal regions and not a single patient possessed such an anomaly within the cervical spine [17].
Fujimori et al. conducted a research study involving 1500 Japanese patients utilizing a multi-detector computed tomography scan [13]. While the prevalence of asymptomatic OLF within the thoracic spine was found to be 12%, its prevalence within the cervical spine was 0.3% [18].
The high rate of OLF within the thoracic spine is the direct result of the constant tension placed on the ligamentum flavum induced through the presence of thoracic kyphosis [9-14]. Contrarily, the exposure of the ligamentum flavum at the cervical spine to tension is shown to be less than that displayed within other regions of the vertebral column. Moreover, lordotic curvature of the cervical spine and the difference in the thickness of the yellow ligaments compared to the thoracic segments may also help to explain the overall low prevalence of COLF [3-8].
Ethnicity
Most of the published cases with cervical OLF are of East Asian ethnic descent [1-8]. However, its occurrence in Caucasians is not as infrequent as it was once supposed [3].
Clinical picture
Typical clinical features of COLFs at the time of diagnosis include an unsteady gait, decreased muscle strength, sensory disturbances, and urinary dysfunction. Such findings are noted to be indistinguishable from cord compressions seen within cervical spondylotic myelopathies [3-8]. The interval from the onset of the disease to the correct diagnosis is usually very lengthy and can range from one to several years.
Imaging
The exact location and shape of the OLF, the number of affected levels, as well as the degrees of cord compression and the associated myelopathies can be best demonstrated by utilization of MRI [3-8]. A typical cervical OLF is visualized as a hypointense signal intensity mass at the level of the posterior margin of the spinal canal when viewed using T1-weighted sagittal MR images. A patient with cervical OLF myelopathy is observed as an intramedullary hyper-intense spot within T-2 weighted sagittal views at the time of diagnosis [3-8].
Most cervical OLFs are located within the subaxial segments and their occurrence in the upper cervical region is rare [3-8].
It is important to assess the exact size, shape, and extent of the ossified lesions before surgical intervention. To accomplish this goal, computerized tomography should be performed. On axial CT scans, the lesions are visualized as ossified masses from the facet joint to the base of the spinal process and can be either unilateral or bilateral [19, 20]. Reconstructed images of an OLF are primarily shown as an ossified mass at the posterior aspect of the spinal column at the site of the ligamentum flavum [3-8, 18-20].
Treatment
Symptomatic cases with cervical OLF should be followed closely with periodic examinations and MRI scans. A decompressive laminectomy and excision of the ossified masses are the mainstay of treatment in symptomatic sub-types [3-8]. The indications for surgery are cervical radiculopathy, myelopathy, or myeloradiculopathy. Bilateral occurrences usually display a tight adherence to the dura. Unilateral nodular OLF sub-types typically show a minimal amount of adhesion to the dura mater. A dural tear is not considered a frequent complication during the surgical removal of a cervical OLF.
Differential
Cervical OLF and cervical ligamentum flavum calcification (CLF) which are separate unique entities are sometimes confused with one another due to the many similarities they present [20, 21]. Imaging features and intraoperative findings will likewise mirror each other [20, 21]. The calcification of the ligamentum flavum, pseudogout, and calcium pyrophosphate dehydrate crystal deposition disease (CPPD), all belong to a single sub-category and can only truly be differentiated from OLF histopathologically [21, 22].
Outcome: The outcome after surgery depends on the duration of the symptoms, the anteroposterior diameter of the lesion, the degree of cord compression observed, the presence of myelopathy, and the specific type of OLF discovered. Our review has shown that surgical intervention for a cervical OLF is associated with a better prognosis when compared to thoracic subtypes.
4. Conclusion
COLF, although rare within non-East Asian populations, should be considered a possible cause of cervical myeloradiculopathy. Surgical excision of COLF is quite easier in the cervical spine with less adhesion and dural tear compared with the thoracic and lumbar OLFs, probably due to the rarity of concomitant dural ossification. Detection of this illusive condition requires a careful and concise neurological exam, the utilization of specific imaging features, a high level of adequate suspicion, and a solid working knowledge of the unique pathological features of this clinical presentation. As a whole, this rare phenomenon is markedly different from a simple calcification of the yellow ligament itself.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from the patient for publishing this report and the corresponding images.
Funding
The authors received no financial support.
Authors' contributions
All authors contributed equally to preparing this report.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
The authors appreciate Dr. Asgari (PhD) for his assistance.
References
- Kubota M, Baba I, Sumida I. Myelopathy due to ossification of the ligamentum flavum of the cervical spine. A report of two cases. Spine. 1981; 6(6):553-9. [PMID]
- Kirita Y, Miyazaki K, Lin D, Nosaka K, Shima M, Yamamura H, et al. Surgical treatment for the ossification of the ligamentum flavum. Chubu Nippon Seikeigeka Saigaigeka Gakkai Zasshi. 1973; 16:814-7. [Link]
- Rahimizadeh A, Asgari N, Soufiani H, Rahimizadeh S. Ossification of the cervical ligamentum flavum and case report with myelopathy. Surgical Neurology International. 2018; 9:263. [PMID]
- Oh JY, Wang VT, Teo TWW, Kaliya-Perumal AK, Hee HT. Ossification of the yellow ligament in the cervical spine-an unusual location. Biomedicine (Taipei) 2019; :9(2):14. [DOI:10.1051/bmdcn/2019090214] [PMID] [PMCID]
- He R, Fang H. Ossification of the ligamentum flavum in the upper cervical spine: A report of two cases and literature review. Experimental and Therapeutic Medicine. 2020; 20(2):1734-8. [DOI:10.3892/etm.2020.8834] [PMID] [PMCID]
- Iftekhar N, Rasool A, Khan I. Cervical cord compression due to ossification of the ligamentum flavum - A case report and literature review. Surgical Neurology International. 2020; 11:37. [DOI:10.25259/SNI_605_2019] [PMID] [PMCID]
- Sing RD, Arts MP, de Ruiter GCW. Delayed onsetwhite cord syndrome after anterior and posterior cervical decompression surgery for symptomatic ossification of spinal ligaments: Illustrative cases. Journal of Neurosurgery: Case Lessons. 2113. 2021; 1(19):CASE2113 [DOI:10.3171/CASE2113]
- Ishikawa Y, Miyakoshi N, Hongo M, Kasukawa Y, Kudo D, Sato C, et al. Thin cervical spinal cord between ossifications of ligamentum flavum and the posterior longitudinal ligament: Case report and literature review. World Neurosurgery. 2021; 145:83-8 [DOI:10.1016/j.wneu.2020.09.033] [PMID]
- Rahimizadeh A, Soufiani H, Amirzadeh M, Rahimizadeh S. Ossification of the ligamentum flavum of the lumbar spine in Caucasians: Case series.Journal of Spine & Neurosurgery. 2017; 6:5. [DOI:10.4172/2325-9701.1000283]
- Aizawa T, Sato T, Sasaki H, Kusakabe T, Morozumi N, Kokubun S. Thoracic myelopathy caused by ossification of the ligamentum flavum: Clinical features and surgical results in the Japanese population. Journal of Neurosurgery. Spine. 2006; 5(6):514-9. [DOI:10.3171/spi.2006.5.6.514] [PMID]
- Rahimizadeh A. Isolated proximal thoracic ossified ligamentum flavum causing paraparesis in a Caucasian: A case report and review of literature. 2146-5622 - World spinal column Journal. 2012; 3(1):38-43. [Link]
- Hur H, Lee JK, Lee JH, Kim JH, Kim SH. Thoracic myelopathy caused by ossification of the ligamentum flavum. Journal of Korean Neurosurgical Society. 2009; 46(3):189-94 [DOI:10.3340/jkns.2009.46.3.189] [PMID] [PMCID]
- Fujimori T Watabe T, Iwamoto Y, Hamada S, Iwasaki M, Oda T. Prevalence, concomitance, and distribution of ossification of the spinal ligamentsresults of whole spine CT Scans in 1500 Japanese patients. Spine. 2016; 41(21):1668-76. [DOI:10.1097/BRS.0000000000001643] [PMID]
- Guo JJ, Luk KD, Karppinen J, Yang H, Cheung KM. Prevalence, distribution, and morphology of ossification of the ligamentum flavum: A population study of one thousand seven hundred thirty-six magnetic resonance imaging scans. Spine (Phila Pa 1976). 2010; 35(1):51-6. [DOI:10.1097/BRS.0b013e3181b3f779] [PMID]
- Liang H, Liu G, Lu S, Chen S, Jiang D, Shi H, et al. Epidemiology of ossification of the spinal ligaments and associated factors in the Chinese population: A cross-sectional study of 2000 consecutive individuals. BMC Musculoskeletal Disorders. 2019; 20(1):253. [DOI:10.1186/s12891-019-2569-1] [PMID] [PMCID]
- Moon BJ, Kuh SU, Kim S, Kim KS, Cho YE, Chin DK. Prevalence, distribution, and significance of incidental thoracic ossification of the ligamentum flavum in Korean patients with back or leg pain : MR-based cross sectional study. Journal of Korean Neurosurgical Society. 2015; 58(2):112-8. [DOI:10.3340/jkns.2015.58.2.112] [PMID] [PMCID]
- Kobayashi S, Okada K, Onoda K, Horikoshi S. Ossification of the cervical ligamentum flavum. Surgical Neurology. 1991; 35(3):234-8. [PMID]
- Otani K,Ahara T, Takana A, Shibazaki S. Ossification of the ligamentum falvum of the thoracic spine in adult kyphosis. International Orthopaedics. 1986,10(2):135-9. [PMID]
- Rahimizadeh A, Habibollahzadeh P, Williamson WL, Soufiani H, Amirzadeh M, Rahimizadeh S. Symptomatic thoracic ossification of the ligamentum flavum in a patient with ankylosing spondylitis: Report of a case and review. Surgical Neurology International. 2021; 12:596. [DOI:10.25259/SNI_1067_2021] [PMID] [PMCID]
- Rahimizadeh A, Sami SH, Amirzadeh M, Rahimizadeh S, Asgari N. Symptomatic thoracic ossified ligamentum flavum in achondroplasia: A case report and literature review. Surgical Neurology International. 2022; 13:70. [DOI:10.25259/SNI_101_2022] [PMID] [PMCID]
- Iwasaki Y, Akino M, Abe H, Tsuru M, Tashiro K, Miyasaka K, et al. Calcification of the ligamentum flavum of the cervical spine: Report of four cases. Journal of Neurosurgery. 1983; 59(3):531-4. [DOI:10.3171/jns.1983.59.3.0531] [PMID]
- Khan MH, Smith PN, Donaldson WF 3rd. Acute quadriparesis caused by calcification of the entire cervical ligamentum flavum in a white female-report of an unusual case and a brief review of the literature: Case report. Spine. 2005; 30(22):E687-91. [DOI:10.1097/01.brs.0000186472.88141.38] [PMID]
Type of Study: Case report |
Subject:
Spine
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |