Fri, Jul 11, 2025
Volume 9 - Continuous Publishing
Iran J Neurosurg 2023, 9 - Continuous Publishing: 32-37 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ebrahimi H, Azimi H, Kolahchi Z, Gholami Z, Nasseri S, Adib M, et al . The Attitude of Neurosurgeons Toward Telemedicine During COVID-19 Pandemic. Iran J Neurosurg 2023; 9 : 5
URL: http://irjns.org/article-1-340-en.html
URL: http://irjns.org/article-1-340-en.html
Hannan Ebrahimi1 

 , Hesam Azimi1
, Hesam Azimi1 

 , Zahra Kolahchi2
, Zahra Kolahchi2 

 , Zeinab Gholami1
, Zeinab Gholami1 

 , Shahin Nasseri1
, Shahin Nasseri1 

 , Maryam Adib3
, Maryam Adib3 

 , Abbas Amirjamshidi1
, Abbas Amirjamshidi1 

 , Mohammad Shirani Bidabadi2
, Mohammad Shirani Bidabadi2 

 , Ahmad Pour-Rashidi *4
, Ahmad Pour-Rashidi *4 




 , Hesam Azimi1
, Hesam Azimi1 

 , Zahra Kolahchi2
, Zahra Kolahchi2 

 , Zeinab Gholami1
, Zeinab Gholami1 

 , Shahin Nasseri1
, Shahin Nasseri1 

 , Maryam Adib3
, Maryam Adib3 

 , Abbas Amirjamshidi1
, Abbas Amirjamshidi1 

 , Mohammad Shirani Bidabadi2
, Mohammad Shirani Bidabadi2 

 , Ahmad Pour-Rashidi *4
, Ahmad Pour-Rashidi *4 


1- Department of Neurosurgery, Sina Hospital, Tehran University of Medical Sciences, Tehran, Iran
2- Department of Neurosurgery, Sina Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
3- Department of Biomedical Engineering, Central Tehran Branch, Islamic Azad University, Tehran, Iran
4- Department of Neurosurgery, Sina Hospital, Tehran University of Medical Sciences, Tehran, Iran ,ahmadpourrashidi89@gmail.com
2- Department of Neurosurgery, Sina Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
3- Department of Biomedical Engineering, Central Tehran Branch, Islamic Azad University, Tehran, Iran
4- Department of Neurosurgery, Sina Hospital, Tehran University of Medical Sciences, Tehran, Iran ,
Full Text [PDF 771 kb]
(678 Downloads)
| Abstract (HTML) (2074 Views)
Full Text: (860 Views)
1. Introduction
The COVID-19 pandemic has changed routine medical management worldwide, especially in developing countries [1]. The COVID-19 disease is transmitted through interpersonal communication, so the widespread outbreak of this disease has imposed severe restrictions on social interactions. An important aspect of these restrictions is the therapeutic activities and medical visits that forced many people not to go to the hospitals except in emergencies. In the COVID-19 era, most surgical procedures were limited to emergencies, and also periodic postoperative visits were difficult to perform. Therefore, another visiting method besides face-to-face visits seems necessary [2].
Telemedicine is gaining popularity as an effective mode of sharing medical issues between patients and physicians using audio, photo, and video devices for data transfer [3, 4]. Telemedicine can be considered a primary modality of patient visits for non-emergent conditions in the COVID-19 pandemic. It helps people with no obligation of physical presence at the clinics during the lockdown and social distancing.
During this period, neurosurgery should also provide the necessary services according to the patients’ needs outside the neurosurgical clinics. Telemedicine can be expanded with higher speed and quality in developed countries due to better accessibility to the Internet and the necessary infrastructures [5]. In developing countries, using telemedicine is challenging because of a lack of required facilities and training, lower level of education and poor socio-economic conditions, limited access to high-speed Internet and audio and video devices, and governments being negligent in providing the necessary education for different segments [6, 7].
Moreover, physicians themselves face different problems when visiting patients using telemedicine, especially in neurosurgical cases, due to the necessity of close neurological examination in diagnostic measures. Despite the existing limitations, telemedicine is developing and becoming more popular. Therefore, it is important to examine the limitations and obstacles to the development of telehealth modes of communication. This research aimed at investigating the neurosurgeons’ perspective on telemedicine in the treatment and follow-up of neurosurgical patients during the COVID-19 period.
2. Methods and Materials/Patients
This cross-sectional study was carried out in the Department of Neurosurgery, Tehran University of Medical Sciences, Tehran, Iran, from June 2021 to July 2021. An internet-based questionnaire was distributed among all postgraduate and assistant neurosurgeons at the University. Neurosurgeons who did not fill out the questionnaire for any reason were excluded from the study. The questionnaire was extracted from a study by Mohanty et al. (2020) and the validity of this questionnaire was surveyed. This questionnaire consisted of two sections; demographic and attitude data. The demographic variables included age, sex, educational level, history of using telemedicine, and the reasons for unimplemented telemedicine. The attitude section included nine questions asking one question about convenience, two questions about adequate time, three questions about the applicability of telemedicine in the future, and three questions about the effectiveness of the non-physical visit. The answers were according to the Likert scale in 5 steps: Strongly agree, agree, undecided, disagree, and strongly disagree.
Statistical analysis was performed using SPSS software, version 24 (IBM SPSS statistics for windows, IBM corp; 2016). Descriptive statistics were Mean±SD for the quantitative variables and frequencies for the qualitative variables.
3. Results
This study included 74 neurosurgeons who were mainly male (89.2%). The mean age was 33.16±5.69 years (ranging from 27 to 62 years), and most participants were neurosurgical residents (75.6 %). The mean of previous medical experience and using telemedicine were 1.11+517 and 1.16+1.65 years, respectively. Thirty-seven precipitants (50%) had no previous experience of using telemedicine. Nevertheless, it was commonly used by some others through online messengers (73%) and voice calls (35.1%), respectively. Most participants preferred telemedicine for follow-up (93.24%).
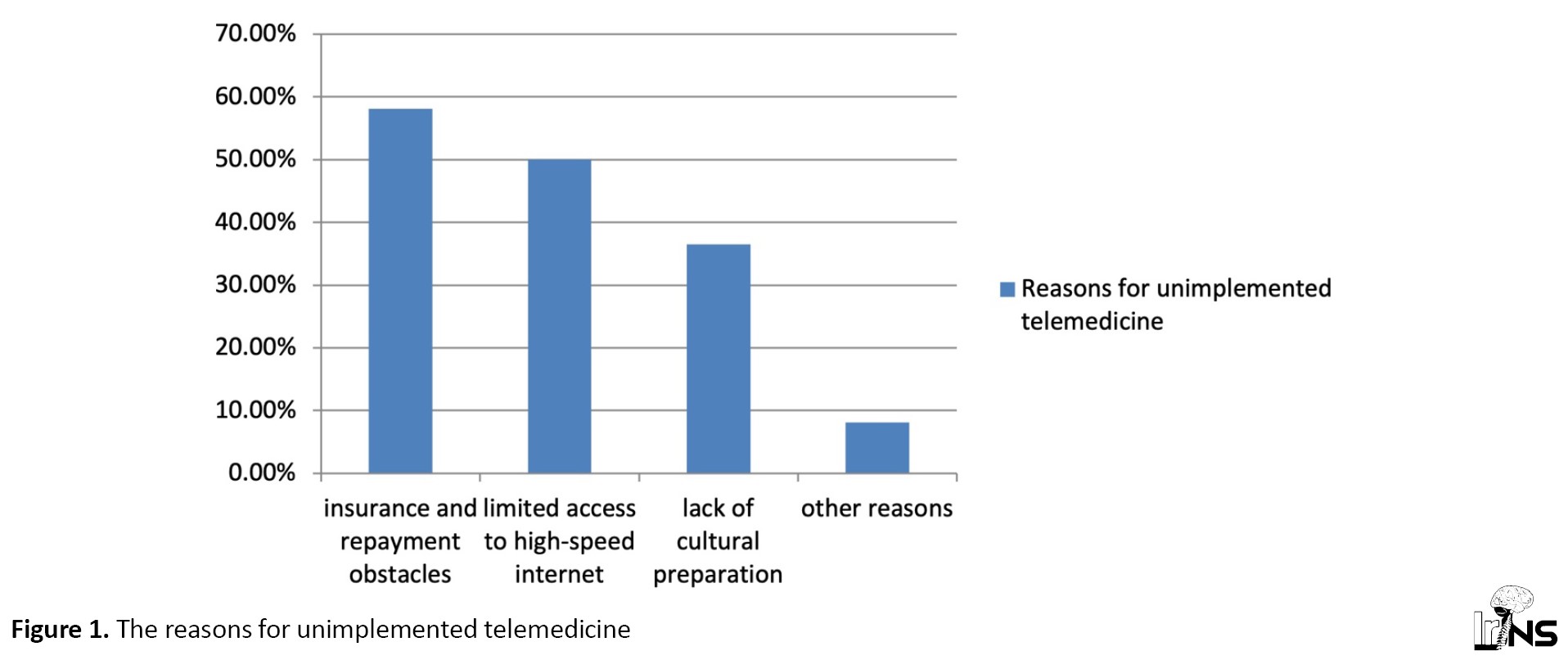
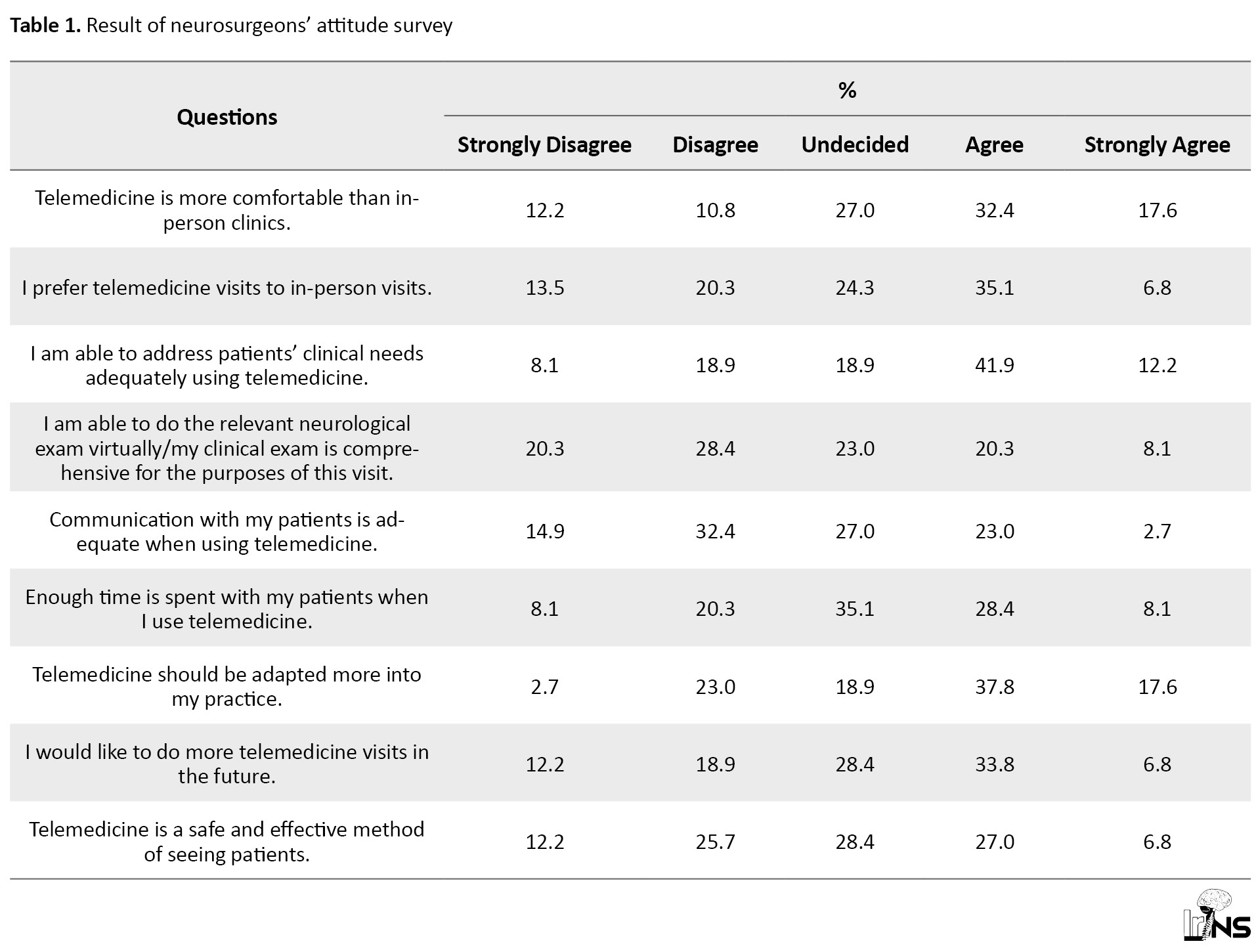
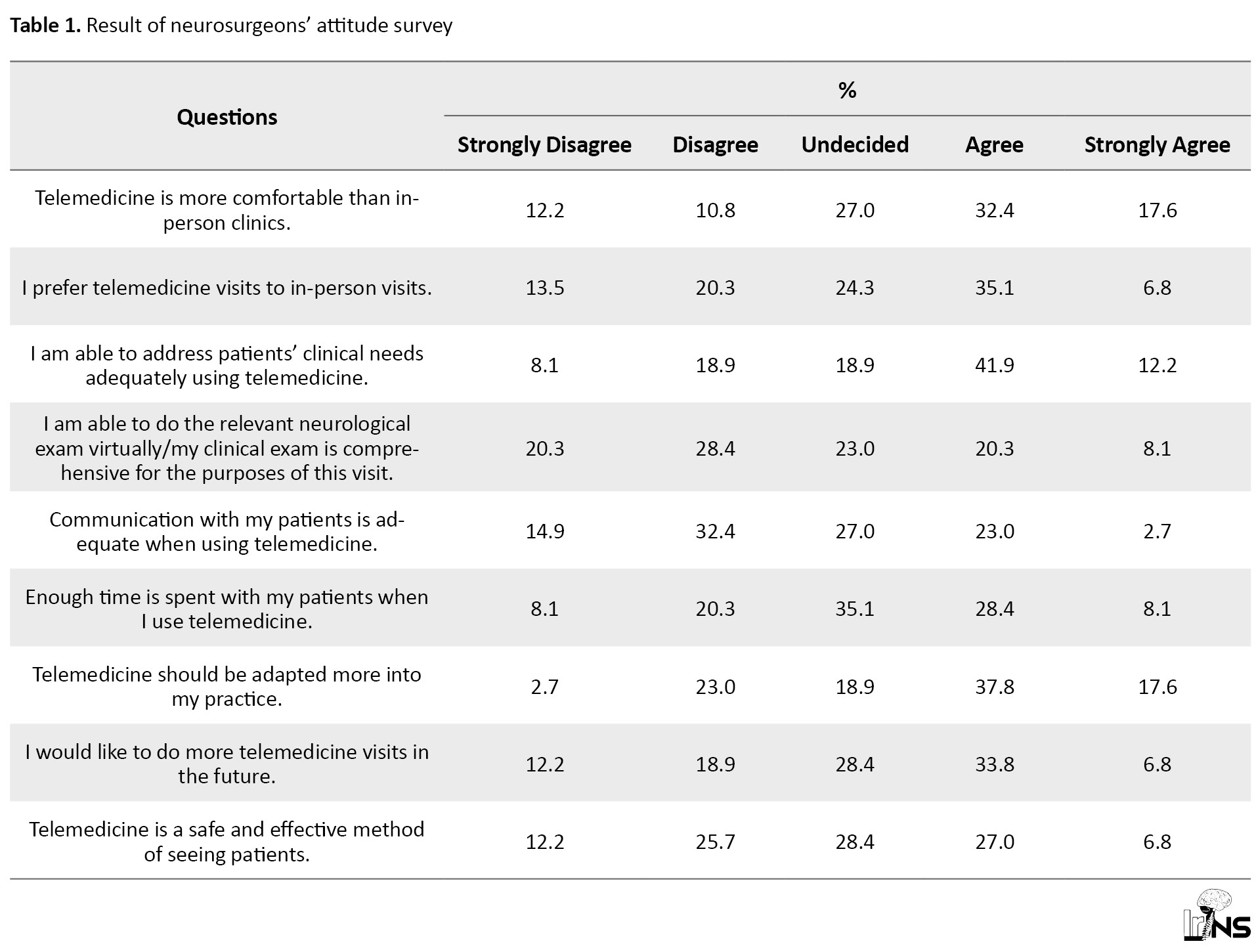
The common reasons for unimplemented telemedicine were insurance and repayment obstacles (58.11%), limited access to high-speed internet (50.05%), and lack of cultural preparation (36.48%), respectively (Figure 1). Most neurosurgeons demonstrated that telemedicine is more comfortable and can meet the patient’s needs, so they preferred it; however, the neurological examination is incomprehensive by telemedicine. Although neurosurgeons spend enough time per patient via telemedicine, physician-patient communication was not adequate. Most of the participants stated that telemedicine should be adapted to working condition and local setting first and then used extensively in the future. The effectiveness of telemedicine was still challenging in most neurosurgeons’ opinions (Table 1).
4. Discussion
The need to provide health and medical service over a distance has a long history, but telemedicine is developing rapidly nowadays, mainly resulting from the fast growth of technology [3]. Moreover, after the COVID-19 outbreak in 2021 and the necessity of social distancing, the implantation and usage of telehealth increased rapidly. Furthermore, telemedicine is a cost-effective alternative considering transportation costs and absence from work [8].
Among neurologists, telemedicine has been widely used, particularly for stroke evaluations and subsequent thrombolytic prescriptions. According to the previous studies, the remote physician could assess CT scans accurately, and tissue plasminogen activator (t-PA) would be delivered appropriately to patients in 4.5 hours timeframe [9, 10]. Tele-stroke is notably helpful when the time from door to the needle is more prolonged, such as in a rural area with limited available stroke centers [10]. Given that the most common cause of rt-PA ineligibility is the time more than 4.5 hours from the beginning of the stroke, the TRUST-tPA study found that telemedicine enhanced accessibility to rt-PA by five times more than routine care [9]. Additionally, telemedicine has been used in other neurological disorders such as Parkinson’s disease, epilepsy, and dementia [11]. Physical examination through a modified form of the unified parkinson’s disease rating scale (UPDRS) can be done virtually [12, 13], and even patients’ candidates for deep brain stimulation (DBS) can be selected appropriately [14].
The utilization of telemedicine in neurosurgery started many years ago [15], but a recent report showed that neurosurgery is among the 15 least specialties that use telemedicine [16]. Most of the studies that evaluated telemedicine in neurosurgical patients have been conducted in post-neurosurgical care settings. Thaker et al. assessed telemedicine efficacy and cost-effectiveness in 1200 patients in 52 months for follow-up visits after neurosurgical service, reporting that telemedicine has more efficacy besides lower costs for patients [8]. Furthermore, a study by Reider-Demer et al. that utilized telemedicine for post-neurosurgical care follow-up, found that emergency room visits or readmission rates had no significant difference between patients in face-to-face visits and patients with telemedicine care. In addition, 100% of patients were satisfied with their telemedicine appointment, and 85% were willing to set future visits in telemedicine form rather than face-to-face meetings [17].
Similarly, Yoon et al.’s study demonstrated high satisfaction in patients after telemedicine visits [2]. In addition to patients’ satisfaction, Mohanty et al. studied providers’ opinions regarding telemedicine; similar to our results, only 42% believed in telemedicine rather than a face-to-face meeting [18]. Also, in concordance with Mohanty et al., about 72% of participants in our study disagreed or were undecided about performing an adequate physical examination through telemedicine. The physical examination can be performed virtually, but it highly depends on patients’ cooperation and the type of tests. Besides, it is challenging to notice muscle changes and cranial nerve deficits that are subtle [19]. It is more convenient and feasible to do physical examinations in non-first and post-surgery visits. Furthermore, patients and physicians tend to meet each other at least once and then pursue visits virtually, and this is mainly because of making a trustful relationship between patients and physicians.
Dadlani et al. assessed the data from follow-up visits of more than 1500 neurosurgical patients and 3000 teleconsultations in their study. They represented that telemedicine has detected postoperative complications with 94% specificity and 100% sensitivity [20]. In parallel to Dadlani et al., about 54% of our participants agreed that they could address patients’ clinical needs adequately using telemedicine.
The common reasons for unimplemented telemedicine found in the present study were mainly related to governmental and health policy issues and may be seen in other countries as well. The most common problem was insurance and repayment issues. Blue et al. reported that one of the main obstacles to telemedicine development and widespread utilization of telemedicine was reimbursement issues before the COVID-19 pandemic in the United States. However, after the emerging COVID-19, the government removed the restriction on telemedicine for rural areas and organized the repayment system which led to the rapid implantation of telemedicine and physicians’ willingness, including neurosurgeons, to telemedicine utilization [19]. Limited access to high-speed internet was the second common reason, and a recent systematic review showed that the primary cause of telemedicine failure is technological issues [6]. These problems will be solved in the future by emphasizing more on the necessity and benefits of telemedicine and technological developments. That can be the reason for the agreement of 55.4% of our participants with more implementation of telemedicine programs in the future.
As a limitation, this study was done among postgraduates of a high-quality neurosurgery training center; a multi-center study can be used to decrease this selection bias. Also, it is suggested to compare our findings with the results of studies performed in the post-COVID-19 setting. Moreover, this study was presented as only a survey of medical professionals in a specific field. Unfortunately, the category of telemedicine and its various dimensions have never been designed in the form of appropriate questionnaires to intelligently identify the intellectual angles and practical concerns of neurosurgeons in this field. Not addressing the use of telemedicine in the field of medical consultation and between two doctors, which is also important and practical, especially for the management of trauma patients, whether in accidents or military encounters, is one of our shortcomings that can be addressed by future researchers.
5. Conclusion
This study revealed that neurosurgeons have a high tendency to use telemedicine. They considered telemedicine as a comfortable alternative but the effectiveness of telemedicine is still controversial in certain medical situations. It needs to be adapted primarily and then used extensively in the future. Comparing the results of our study with studies performed after the COVID-19 pandemic are worth to be noted by other researchers.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the local ethics committee of Department of Neurosurgery, Tehran University of Medical Sciences, Tehran, Iran. Ethical issues (including plagiarism, informed consent, misconduct, data fabrication and or falsification, double publication and or submission, redundancy, etc.) have been completely observed by the authors.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Hannan Ebrahimi, Maryam Adib and Abbas Amirjamshidi; Data collection: Hesam Azimi, Zeinab Gholami and Shahin Nasseri; Data analysis, interpretation and drafting the article: Hannan Ebrahimi and Zahra Kolahchi; Critically revising the article and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
All authors would like to thank the assistance of all people who helped us in preparing and composing the paper.
References
The COVID-19 pandemic has changed routine medical management worldwide, especially in developing countries [1]. The COVID-19 disease is transmitted through interpersonal communication, so the widespread outbreak of this disease has imposed severe restrictions on social interactions. An important aspect of these restrictions is the therapeutic activities and medical visits that forced many people not to go to the hospitals except in emergencies. In the COVID-19 era, most surgical procedures were limited to emergencies, and also periodic postoperative visits were difficult to perform. Therefore, another visiting method besides face-to-face visits seems necessary [2].
Telemedicine is gaining popularity as an effective mode of sharing medical issues between patients and physicians using audio, photo, and video devices for data transfer [3, 4]. Telemedicine can be considered a primary modality of patient visits for non-emergent conditions in the COVID-19 pandemic. It helps people with no obligation of physical presence at the clinics during the lockdown and social distancing.
During this period, neurosurgery should also provide the necessary services according to the patients’ needs outside the neurosurgical clinics. Telemedicine can be expanded with higher speed and quality in developed countries due to better accessibility to the Internet and the necessary infrastructures [5]. In developing countries, using telemedicine is challenging because of a lack of required facilities and training, lower level of education and poor socio-economic conditions, limited access to high-speed Internet and audio and video devices, and governments being negligent in providing the necessary education for different segments [6, 7].
Moreover, physicians themselves face different problems when visiting patients using telemedicine, especially in neurosurgical cases, due to the necessity of close neurological examination in diagnostic measures. Despite the existing limitations, telemedicine is developing and becoming more popular. Therefore, it is important to examine the limitations and obstacles to the development of telehealth modes of communication. This research aimed at investigating the neurosurgeons’ perspective on telemedicine in the treatment and follow-up of neurosurgical patients during the COVID-19 period.
2. Methods and Materials/Patients
This cross-sectional study was carried out in the Department of Neurosurgery, Tehran University of Medical Sciences, Tehran, Iran, from June 2021 to July 2021. An internet-based questionnaire was distributed among all postgraduate and assistant neurosurgeons at the University. Neurosurgeons who did not fill out the questionnaire for any reason were excluded from the study. The questionnaire was extracted from a study by Mohanty et al. (2020) and the validity of this questionnaire was surveyed. This questionnaire consisted of two sections; demographic and attitude data. The demographic variables included age, sex, educational level, history of using telemedicine, and the reasons for unimplemented telemedicine. The attitude section included nine questions asking one question about convenience, two questions about adequate time, three questions about the applicability of telemedicine in the future, and three questions about the effectiveness of the non-physical visit. The answers were according to the Likert scale in 5 steps: Strongly agree, agree, undecided, disagree, and strongly disagree.
Statistical analysis was performed using SPSS software, version 24 (IBM SPSS statistics for windows, IBM corp; 2016). Descriptive statistics were Mean±SD for the quantitative variables and frequencies for the qualitative variables.
3. Results
This study included 74 neurosurgeons who were mainly male (89.2%). The mean age was 33.16±5.69 years (ranging from 27 to 62 years), and most participants were neurosurgical residents (75.6 %). The mean of previous medical experience and using telemedicine were 1.11+517 and 1.16+1.65 years, respectively. Thirty-seven precipitants (50%) had no previous experience of using telemedicine. Nevertheless, it was commonly used by some others through online messengers (73%) and voice calls (35.1%), respectively. Most participants preferred telemedicine for follow-up (93.24%).
The common reasons for unimplemented telemedicine were insurance and repayment obstacles (58.11%), limited access to high-speed internet (50.05%), and lack of cultural preparation (36.48%), respectively (Figure 1). Most neurosurgeons demonstrated that telemedicine is more comfortable and can meet the patient’s needs, so they preferred it; however, the neurological examination is incomprehensive by telemedicine. Although neurosurgeons spend enough time per patient via telemedicine, physician-patient communication was not adequate. Most of the participants stated that telemedicine should be adapted to working condition and local setting first and then used extensively in the future. The effectiveness of telemedicine was still challenging in most neurosurgeons’ opinions (Table 1).
4. Discussion
The need to provide health and medical service over a distance has a long history, but telemedicine is developing rapidly nowadays, mainly resulting from the fast growth of technology [3]. Moreover, after the COVID-19 outbreak in 2021 and the necessity of social distancing, the implantation and usage of telehealth increased rapidly. Furthermore, telemedicine is a cost-effective alternative considering transportation costs and absence from work [8].
Among neurologists, telemedicine has been widely used, particularly for stroke evaluations and subsequent thrombolytic prescriptions. According to the previous studies, the remote physician could assess CT scans accurately, and tissue plasminogen activator (t-PA) would be delivered appropriately to patients in 4.5 hours timeframe [9, 10]. Tele-stroke is notably helpful when the time from door to the needle is more prolonged, such as in a rural area with limited available stroke centers [10]. Given that the most common cause of rt-PA ineligibility is the time more than 4.5 hours from the beginning of the stroke, the TRUST-tPA study found that telemedicine enhanced accessibility to rt-PA by five times more than routine care [9]. Additionally, telemedicine has been used in other neurological disorders such as Parkinson’s disease, epilepsy, and dementia [11]. Physical examination through a modified form of the unified parkinson’s disease rating scale (UPDRS) can be done virtually [12, 13], and even patients’ candidates for deep brain stimulation (DBS) can be selected appropriately [14].
The utilization of telemedicine in neurosurgery started many years ago [15], but a recent report showed that neurosurgery is among the 15 least specialties that use telemedicine [16]. Most of the studies that evaluated telemedicine in neurosurgical patients have been conducted in post-neurosurgical care settings. Thaker et al. assessed telemedicine efficacy and cost-effectiveness in 1200 patients in 52 months for follow-up visits after neurosurgical service, reporting that telemedicine has more efficacy besides lower costs for patients [8]. Furthermore, a study by Reider-Demer et al. that utilized telemedicine for post-neurosurgical care follow-up, found that emergency room visits or readmission rates had no significant difference between patients in face-to-face visits and patients with telemedicine care. In addition, 100% of patients were satisfied with their telemedicine appointment, and 85% were willing to set future visits in telemedicine form rather than face-to-face meetings [17].
Similarly, Yoon et al.’s study demonstrated high satisfaction in patients after telemedicine visits [2]. In addition to patients’ satisfaction, Mohanty et al. studied providers’ opinions regarding telemedicine; similar to our results, only 42% believed in telemedicine rather than a face-to-face meeting [18]. Also, in concordance with Mohanty et al., about 72% of participants in our study disagreed or were undecided about performing an adequate physical examination through telemedicine. The physical examination can be performed virtually, but it highly depends on patients’ cooperation and the type of tests. Besides, it is challenging to notice muscle changes and cranial nerve deficits that are subtle [19]. It is more convenient and feasible to do physical examinations in non-first and post-surgery visits. Furthermore, patients and physicians tend to meet each other at least once and then pursue visits virtually, and this is mainly because of making a trustful relationship between patients and physicians.
Dadlani et al. assessed the data from follow-up visits of more than 1500 neurosurgical patients and 3000 teleconsultations in their study. They represented that telemedicine has detected postoperative complications with 94% specificity and 100% sensitivity [20]. In parallel to Dadlani et al., about 54% of our participants agreed that they could address patients’ clinical needs adequately using telemedicine.
The common reasons for unimplemented telemedicine found in the present study were mainly related to governmental and health policy issues and may be seen in other countries as well. The most common problem was insurance and repayment issues. Blue et al. reported that one of the main obstacles to telemedicine development and widespread utilization of telemedicine was reimbursement issues before the COVID-19 pandemic in the United States. However, after the emerging COVID-19, the government removed the restriction on telemedicine for rural areas and organized the repayment system which led to the rapid implantation of telemedicine and physicians’ willingness, including neurosurgeons, to telemedicine utilization [19]. Limited access to high-speed internet was the second common reason, and a recent systematic review showed that the primary cause of telemedicine failure is technological issues [6]. These problems will be solved in the future by emphasizing more on the necessity and benefits of telemedicine and technological developments. That can be the reason for the agreement of 55.4% of our participants with more implementation of telemedicine programs in the future.
As a limitation, this study was done among postgraduates of a high-quality neurosurgery training center; a multi-center study can be used to decrease this selection bias. Also, it is suggested to compare our findings with the results of studies performed in the post-COVID-19 setting. Moreover, this study was presented as only a survey of medical professionals in a specific field. Unfortunately, the category of telemedicine and its various dimensions have never been designed in the form of appropriate questionnaires to intelligently identify the intellectual angles and practical concerns of neurosurgeons in this field. Not addressing the use of telemedicine in the field of medical consultation and between two doctors, which is also important and practical, especially for the management of trauma patients, whether in accidents or military encounters, is one of our shortcomings that can be addressed by future researchers.
5. Conclusion
This study revealed that neurosurgeons have a high tendency to use telemedicine. They considered telemedicine as a comfortable alternative but the effectiveness of telemedicine is still controversial in certain medical situations. It needs to be adapted primarily and then used extensively in the future. Comparing the results of our study with studies performed after the COVID-19 pandemic are worth to be noted by other researchers.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the local ethics committee of Department of Neurosurgery, Tehran University of Medical Sciences, Tehran, Iran. Ethical issues (including plagiarism, informed consent, misconduct, data fabrication and or falsification, double publication and or submission, redundancy, etc.) have been completely observed by the authors.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Hannan Ebrahimi, Maryam Adib and Abbas Amirjamshidi; Data collection: Hesam Azimi, Zeinab Gholami and Shahin Nasseri; Data analysis, interpretation and drafting the article: Hannan Ebrahimi and Zahra Kolahchi; Critically revising the article and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
All authors would like to thank the assistance of all people who helped us in preparing and composing the paper.
References
- Szmuda T, Ali S, Słoniewski P, Group NW. Telemedicine in neurosurgery during the novel coronavirus (COVID-19) pandemic. Polish Journal of Neurology and Neurosurgery. 2020; 54(2):207-8. [Link]
- Yoon EJ, Tong D, Anton GM, Jasinski JM, Claus CF, Soo TM, et al. Patient satisfaction with neurosurgery telemedicine visits during the coronavirus disease 2019 pandemic: A prospective cohort study. World Neurosurgery. 2021; 145:e184-91 [DOI:10.1016/j.wneu.2020.09.170] [PMID] [PMCID]
- Waller M, Stotler C. Telemedicine: A Primer. Current Allergy and Asthma Reports. 2018; 18(10):54. [DOI:10.1007/s11882-018-0808-4] [PMID]
- Salehahmadi Z, Hajialiasghari F. Telemedicine in Iran: Chances and challenges. World Journal of Plastic Surgery. 2013; 2(1):18-25. [PMCID]
- Ashry AH, Soffar HM, Alsawy MF. Neurosurgical education during COVID-19: Challenges and lessons learned in Egypt. The Egyptian Journal of Neurology, Psychiatry and Neurosurgery. 2020; 56(1):110 [DOI:10.1186/s41983-020-00242-8] [PMID] [PMCID]
- Eichberg DG, Basil GW, Di L, Shah AH, Luther EM, Lu VM, et al. Telemedicine in neurosurgery: Lessons learned from a systematic review of the literature for the COVID-19 era and beyond. Neurosurgery. 2021; 88(1):E1-12. [DOI:10.1093/neuros/nyaa306] [PMID] [PMCID]
- Ahmadi M, Meraji M, Mashoof Jafarabad E. [Evidence on telemedicine in Iran - systematic review (Persian)]. Journal of Paramedical Sciences & Rehabilitation. 2018; 7(1):112-24. [DOI:10.22038/JPSR.2018.21592.1551]
- Thakar S, Rajagopal N, Mani S, Shyam M, Aryan S, Rao AS, et al. Comparison of telemedicine with in-person care for follow-up after elective neurosurgery: Results of a cost-effectiveness analysis of 1200 patients using patient-perceived utility scores. Neurosurgical Focus. 2018; 44(5):E17. [DOI:10.3171/2018.2.FOCUS17543] [PMID]
- Mazighi M, Meseguer E, Labreuche J, Miroux P, Le Gall C, Roy P, et al. TRUST-tPA trial: Telemedicine for remote collaboration with urgentists for stroke-tPA treatment. Journal of Telemedicine and Telecare. 2017; 23(1):174-80 [DOI:10.1177/1357633X15615762] [PMID]
- Patel UK, Malik P, DeMasi M, Lunagariya A, Jani VB. Multidisciplinary approach and outcomes of tele-neurology: A review. Cureus. 2019; 11(4):e4410-e. [DOI:10.7759/cureus.4410]
- Schneider RB, Biglan KM. The promise of telemedicine for chronic neurological disorders: The example of Parkinson’s disease. The Lancet Neurology. 2017; 16(7):541-51. [DOI:10.1016/S1474-4422(17)30167-9] [PMID]
- Cubo E, Trejo Gabriel-Galán JM, Seco Martínez J, Rioja Alcubilla C, Yang C, Fernández Arconada O, et al. Comparison of office-based versus home Web-based clinical assessments for Parkinson’s disease. Movement Disorders. 2012; 27(2):308-311 [DOI:10.1002/mds.24028] [PMID]
- Abdolahi A, Scoglio N, Killoran A, Dorsey ER, Biglan KM. Potential reliability and validity of a modified version of the Unified Parkinson’s Disease Rating Scale that could be administered remotely. Parkinsonism & Related Disorders. 2013; 19(2):218-21 [DOI:10.1016/j.parkreldis.2012.10.008] [PMID] [PMCID]
- Witek N, Heath SL, Ouyang B, Tanner CM, Galifianakis NB. Remote telemedicine evaluation of deep brain stimulation candidacy: Retrospective cohort analysis. Neurology. Clinical Practice. 2020; 10(3):199-205. [DOI:10.1212/CPJ.0000000000000723] [PMID] [PMCID]
- Ionita CC, Sharma J, Janicke DM, Levy EI, Siddiqui AH, Agrawal S, et al. Acute ischemic stroke and thrombolysis location: Comparing telemedicine and stroke center treatment outcomes. Hospital Practice. 2009; 37(1):33-9. [DOI:10.3810/hp.2009.12.252] [PMID]
- Doximity. telemedicine and locum tenens opportunities study-measuring physician interest in emerging employment areas [Internet]. 2019 [Updated July 2019]. Available from: [Link]
- Reider-Demer M, Raja P, Martin N, Schwinger M, Babayan D. Prospective and retrospective study of videoconference telemedicine follow-up after elective neurosurgery: Results of a pilot program. Neurosurgical Review. 20018; 41:497-501. [Link]
- Mohanty A, Srinivasan VM, Burkhardt JK, Johnson J, Patel AJ, Sheth SA, et al. Ambulatory neurosurgery in the COVID-19 era: Patient and provider satisfaction with telemedicine. Neurosurgical Focus. 2020; 49(6):E13. [DOI:10.3171/2020.9.FOCUS20596] [PMID]
- Blue R, Yang AI, Zhou C, De Ravin E, Teng CW, Arguelles GR, et al. Telemedicine in the era of coronavirus disease 2019 (covid-19): A neurosurgical perspective. World Neurosurgery. 2020; 139:549-57 [DOI:10.1016/j.wneu.2020.05.066] [PMID] [PMCID]
- Dadlani R, Mani S, AU JG, Mohan D, Rajgopalan N, Thakar S, et al. The impact of telemedicine in the postoperative care of the neurosurgery patient in an outpatient clinic: a unique perspective of this valuable resource in the developing world--an experience of more than 3000 teleconsultations. World Neurosurgery. 2014; 82(3-4):270-83. [DOI:10.1016/j.wneu.2014.05.027] [PMID]
Type of Study: Research |
Subject:
Basic Neurosurgery
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |