Tue, Feb 3, 2026
Volume 9 - Continuous Publishing
Iran J Neurosurg 2023, 9 - Continuous Publishing: 10-17 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mousavi S R, Liaghat A, Shahpari Motlagh M A, Pishjoo M, Tarokh A, farrokhi M. Launching the DCER (Distraction, Compression, Extension, and Reduction) Technique in Basilar Invagination and Atlantoaxial Dislocation: A Preliminary Report of Two Cases in Iran. Iran J Neurosurg 2023; 9 : 2
URL: http://irjns.org/article-1-341-en.html
URL: http://irjns.org/article-1-341-en.html
Seyed Reza Mousavi1 

 , Alireza Liaghat2
, Alireza Liaghat2 

 , Mohammadhadi Amir Shahpari Motlagh2
, Mohammadhadi Amir Shahpari Motlagh2 

 , Masoud Pishjoo3
, Masoud Pishjoo3 

 , Amir Tarokh2
, Amir Tarokh2 

 , Majidreza Farrokhi *4
, Majidreza Farrokhi *4 




 , Alireza Liaghat2
, Alireza Liaghat2 

 , Mohammadhadi Amir Shahpari Motlagh2
, Mohammadhadi Amir Shahpari Motlagh2 

 , Masoud Pishjoo3
, Masoud Pishjoo3 

 , Amir Tarokh2
, Amir Tarokh2 

 , Majidreza Farrokhi *4
, Majidreza Farrokhi *4 


1- Department of Neurosurgery, Shiraz University of Medical Sciences, Shiraz, Iran AND Shiraz Neuroscience Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
2- Department of Neurosurgery, Shiraz University of Medical Sciences, Shiraz, Iran
3- Department of Neurosurgery, Faculty of Medicine, Birjand University of Medical Sciences, Birjand, Iran
4- Department of Neurosurgery, Shiraz University of Medical Sciences, Shiraz, Iran AND Shiraz Neuroscience Research Center, Shiraz University of Medical Sciences, Shiraz, Iran ,farokhim@sums.ac.ir
2- Department of Neurosurgery, Shiraz University of Medical Sciences, Shiraz, Iran
3- Department of Neurosurgery, Faculty of Medicine, Birjand University of Medical Sciences, Birjand, Iran
4- Department of Neurosurgery, Shiraz University of Medical Sciences, Shiraz, Iran AND Shiraz Neuroscience Research Center, Shiraz University of Medical Sciences, Shiraz, Iran ,
Keywords: Atlantoaxial dislocation, Basilar invagination, Compression, Distraction, Extension, Reduction
Full Text [PDF 1510 kb]
(1312 Downloads)
| Abstract (HTML) (5166 Views)
Case 1
A 50-year-old man with a history of ischemic heart disease (under treatment with aspirin and clopidogrel) was referred to our neurosurgery clinic with a five-month complaint of severe pain in his hands, which was more significant on the right. He had no significant axial neck pain. On the physical examination, the muscle powers were 5/5 in all limbs except for his left foot during dorsiflexion (2/5) due to a traumatic injury five years earlier. Deep tendon reflexes (DTR) were 3/4; the plantar reflex was downward, and the Hoffman sign was positive. Neither saddle hypoesthesia nor incontinence was noted.
A cervical MRI showed severe stenosis of the craniocervical junction with a severe pressure effect on the cervicomedullary junction, causing an increased signal due to the posterior displacement of the odontoid process. At the C3–C4 level, evidence of a diffuse central osteophyte complex causing a pressure effect over the thecal sac with mild canal stenosis and mild bilateral neural foraminal stenosis touching the exiting nerve root was noted. Moreover, evidence of a mild central disc osteophyte complex at C4–C5 with minimal indentation over the thecal sac without any sign of neural foraminal stenosis or canal stenosis was observed. Using the plain x-rays and CT scans with reconstructed views, the diagnosis of BI and AAD was established, and traditional indices (McRae and Wackenheim) were used to evaluate BI severity (Figure 1 A).

A CT angiogram study was then conducted to evaluate the vertebral arteries. Following the investigations, surgery with the DCER technique was planned and discussed with the patient. First, he was positioned prone with his head fixed on a U-shaped headrest and the neck in a neutral position. After general anesthesia, a standard vertical midline incision was made from the inion to C6. Suboccipital decompression was done, followed by the insertion of a cervical occipital plate with four screws and five lateral mass screws (right C3 & C6; left C4, C5 & C6) with five nuts. One cross-link between two rods was applied, and a right C1–C2 facet joint spacer with a polyether ether ketone (PEEK)-cage was performed thereafter. A mesh plate with five mini-screws and a 20-cm rod was applied to limit graft materials contacting the dural sac; this was followed by the insertion of an autologous bone graft harvested from the right posterior iliac crest. Eventually, a C-arm was used to ensure the correct positioning of screws.
As mentioned earlier, postoperative imaging was done to evaluate the screws’ position and the extent of reduction (Figure 1). On the follow-up MRI, metallic fixation devices were seen in the posterior elements of the C3, C4, and C5 vertebral bodies. Disc osteophyte complexes were observed at C2-C3 and C3-C4 levels, causing bilateral narrowing of the neural foramina. Also, the disc space between C6-C7 is rudimentary suggestive of a block vertebra. In the 1-year follow-up, significant neurologic improvement was obvious and fusion in the cervical CT scan was detected (Figure 1 D).
Case 2
A 33-year-old man without any significant past medical history was referred with progressive right upper extremity weakness commencing a year beforehand Muscle forces were 5/5 except for the middle part of his right upper extremity (4/5), and he had hyperreflexia in the DTR evaluation (3/4). Hoffman’s sign was positive, the plantar reflex was downward, and the patient had no saddle hypoesthesia or incontinence.
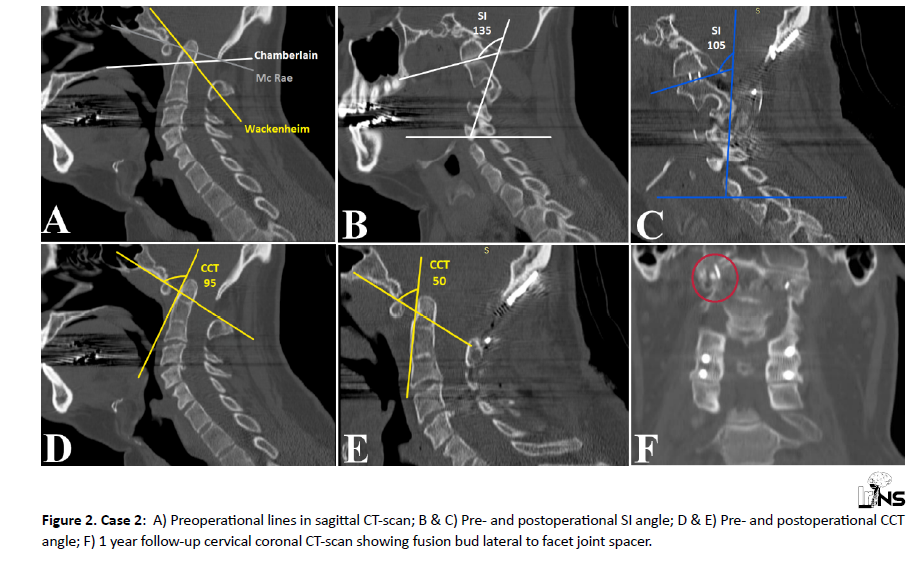
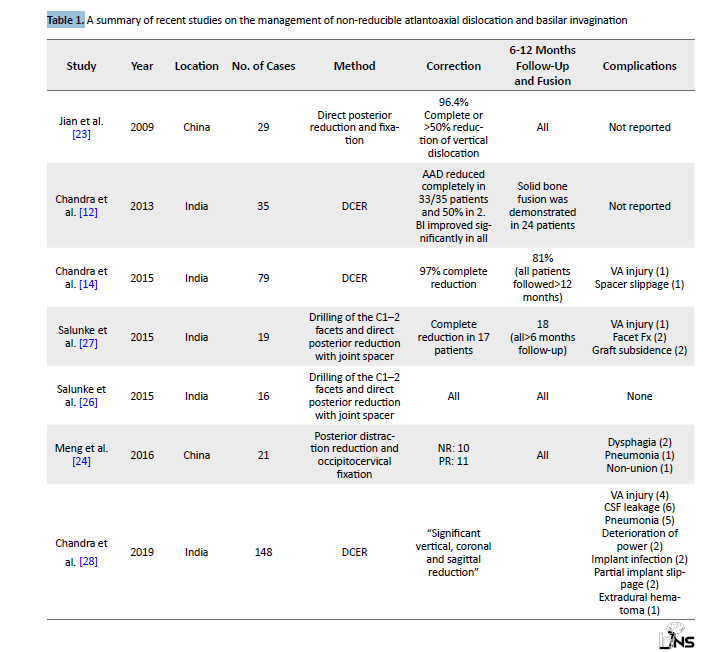
After a thorough physical and radiological assessment, BI and AAD were diagnosed for the patient. The McRae, Chamberlain, and Wackenheim lines were measured (Figure 2 A), and surgery with the DCER technique was planned thereafter.
He was placed on the operating table in the prone position with his head fixed on a U-shaped headrest and neck placed in a neutral position. A standard midline incision was made from the occipital protuberance, and an interlaminar C2 screw was inserted under C-arm control. C2 laminectomy and C1 posterior arc removal (C1 assimilated to foramen magnum) were performed, followed by suboccipital decompression. After dural opening, tonsillar shrinkage was done by bipolar coagulator, and the dura was then repaired with a dural graft from the subperiosteal tissue. The occipital plate was placed, the rod was inserted, and the spacer graft was inserted in the C1-C2 joint bilaterally.
At the final follow-up, his Hoffman remained positive, and the patient had hyperreflexia. Postoperative MRI within 12 months of surgery revealed evidence of the previous operation in the posterior fossa and occipital skull bone, as well as a significant increase in cervical spine lordosis. Furthermore, super posterior displacement of the odontoid process of C2 was noted, narrowing the foramen of Monro and placing a pressure effect on the brainstem. Herniation of the cerebellum vermis was observed inferiorly from the foramen magnum, and an elongated tubular shape fluid signal (hyposignal in T1, hypersignal in T2) was seen within the central cervical spinal cord, indicative of a syrinx. Additionally, diffuse disc bulging was evident at the C2–C3 and C3–C4 levels, with indentation of the anterior aspect of the thecal sac and bilateral mild neural foraminal narrowing without canal stenosis.
The patient underwent a second surgery for the removal of rods and interlaminar C2 screw. Then, C3–C4 lateral mass screws (4 screws and 4 nuts) were placed, and C1–C2 fusion was done with two anterior cervical cages. Subsequently, 2 rods and one cross-link in between were applied, and a graft was inserted bilaterally. Postoperative cervical MRI demonstrated herniation of the cerebellum through the foramen magnum and narrowing of the cervicomedullary junction (anteroposterior diameter =9.5 mm), associated with signal changes in the cord at this area. Also, evidence of elongated cystic dilatation with fluid signal intensity in the central part of the cervical cord was noted, suggestive of a syrinx.
3. Discussion
As complicated conditions, AAD and BI progressively cause cervicomedullary compression and neurological deficits. Treatment focuses on decreasing the compression and providing sensible stability and deformity correction [5, 6, 19, 20]. These congenital disorders usually cannot be reduced by cervical traction with dynamic x-rays. Cases are mostly associated with atlas assimilation with the occiput [4, 15]. Notably, both our patients had irreducible AAD and BI. Conventionally, BI with AAD was treated through an anterior transoral approach and removal of the odontoid process, followed by a posterior instrumented fixation [9, 10, 21, 15].
In some cases, traction reduces AAD; however, BIs cannot be reduced on traction [5, 6], and there is some consensus that such cases should be treated with decompression and stabilization without deformity correction [9-11, 21]. Before 2010, Goel et al. introduced a technique through which BIs could be realigned by distraction (using a spacer within the joint) with C1–C2 fixation [5, 6, 22]. Jian et al. [23] and Y. Meng et al. [24] reported cases of irreducible BI in China. They introduced a moderately new concept of intraoperative manipulation in which both BI and AAD were reduced in cases of BI with an assimilated C1 arch. In this technique, after direct posterior decompression and distraction, a rod was connected to a C2 pedicular screw, and occipitocervical fixation was performed. Notwithstanding their favorable outcomes, it had a weakness in providing distraction only as a method of reduction for both AAD and BI. Optimal reduction in cases with AAD can be achieved by a forward movement of the dens, whereas BI requires only a vertical distraction. Furthermore, their results showed a risk of resettling in cases where distraction was performed without spacer placement.
Hsu et al. [25] tackled this issue using a novel technique for two patients with acquired occipitocervical instability in 2010. Beyond and above that, they applied compression between the upper occipital screw and another superior screw on the rod to provide an extension of the neck, thereby correcting the AAD. According to their results, although distraction corrects BI, AAD correction can be attained by simultaneous extension and distraction.
Chandra et al. [12] described the DCER technique in 2013 in India, constituting the distraction of joint space with spacers (in the occipito-C1-C2 joint space) before compression between the occiput and C2, resulting in extension at the occipito-C1-C2 joint and causing AAD reduction. They explicated that 94% of cases with AAD and all cases with BI were reduced completely using the DCER technique. Their other case series published in 2013 and 2015 [12, 14] developed this procedure with novel devices, reporting improvements in terms of indices, fusion rates, and complications. At the same time, in India, Salunke et al. [26, 27] utilized “drilling of the C1–2 facets and direct posterior reduction with joint spacer” for 35 cases of non-reducible BI and AAD. The major principles followed were identical to Chandra et al.’s, yet they were not referred to as the DCER procedure.
Chandra et al. also reported their largest and latest series in 2019 [28], including 148 cases of BI treated with the DCER procedure. They attained a better understanding of BI, radiologic indices, indications and contraindications, and the main challenges of the DCER procedure. Based on this study, non-reducible BI is classified into three main types according to the sagittal inclination (SI) angle. This is the angle measured between the line parallel to the axis of the dense process (drawn tangential to its posterior border) and a line parallel to the C1–C2 joint surface with a normal range of 87.15±5.65°. The SI angle was classified as less than 100° (type I), 100–160° (type II), and more than 160° (type III). For each type, Chandra et al. recommended the following surgical procedure, with further details provided in their manuscript [28]:
- Type I: DCER
- Type II: Joint remodeling+DCER
- Type III: Extra-articular distraction+DCER
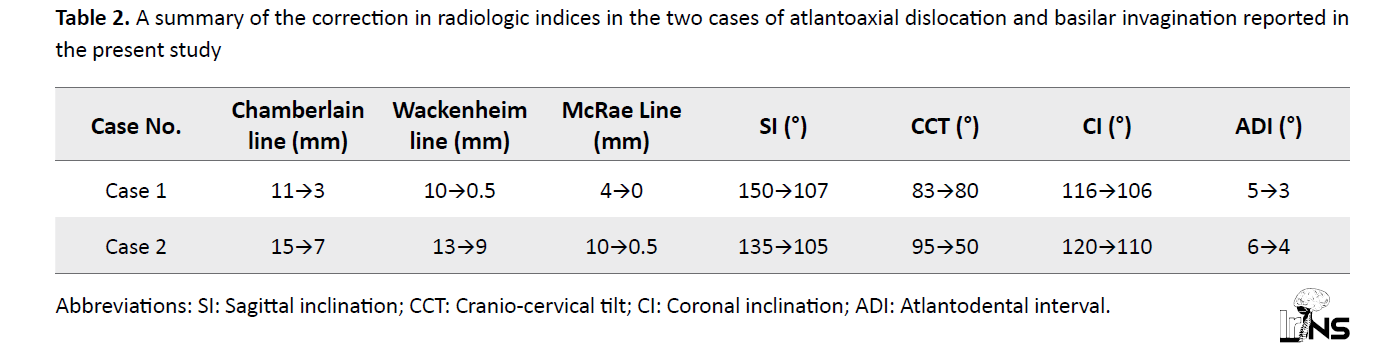
As reviewed in Table 1, recent concepts regarding non-reducible BI and AAD management can be classified into two major approaches: (i) Posterior decompression and reduction with occipitocervical fixation and (ii) the DCER procedure with C1–C2 facet joint spacer application. Fusion in both recent methods was the same and complete.
Correction of indices and reduction rates have been significantly superior in methods including the C1–C2 joint spacer and vertical reduction. Although major complications cannot be compared in detail due to the small numbers reported, in both methods, vertebral artery injury was reported as the most severe complication with a slightly higher rate in DCER procedures.
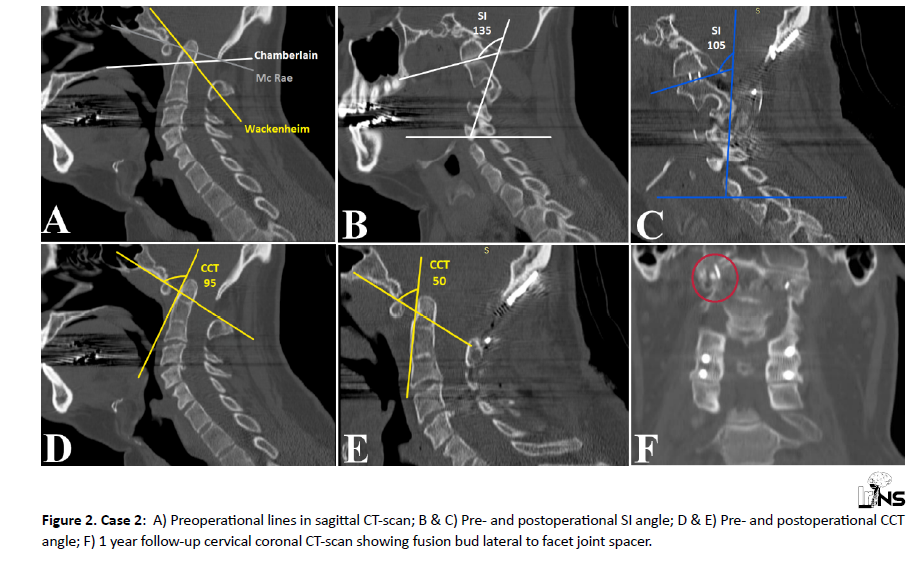
In line with the literature and the latest Chandra et al.’s data [28], we successfully treated two individuals with BI and AAD using the DCER technique for the first time in our center and reported for the first time in Iran. Both cases were type-II non-reducible BI, and achievements in correcting radiologic indices are summarized in Table 2.
In the first case, the patient’s age (causing BI to be more severe and rigid) and the lack of appropriate new devices for the DCER procedure led to the failure of the correction of CCT. Occipitocervical fusion was also an important part of this procedure due to the specific biomechanics of the craniocervical junction region [29].
4. Conclusion
The result of this research can be revised in the future with a simpler and single approach due to the small sample size and selection bias. Nonetheless, we achieved acceptable clinical improvement and vertical reduction.
Based on previous studies [12, 14, 28], it can be inferred that the DCER technique, mainly grounded upon the principle of utilizing a spacer as a fulcrum, is a safe and more effective strategy to correct AAD and BI through a single-stage posterior approach.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from all patients.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, study design and drafting the article: Majidreza farrokhi and Seyed Reza Mousavi; Data collection: Seyed Reza Mousavi; Critically revising the article and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Full Text: (2786 Views)
1. Background and Importance
The craniovertebral junction (CVJ) is a complex area providing considerable mobility while marinating biomechanical stability [1]. Developmental CVJ anomalies usually consist of irreducible atlantoaxial dislocation (AAD) and basilar invagination (BI) associated with the occipital fusion of the C1 arch [2-4]. BI is the congenital upward displacement of the upper cervical spine (particularly the odontoid process) into the foramen magnum, which can be associated with AAD [5-8].
The previous techniques mainly focused on transoral excision of the dens, followed by posterior instrumented fusion [9-11]. In 2013, the distraction, compression, extension, and reduction (DCER) technique was introduced by Chandra et al. [12] to reduce, realign, and correct BI and AAD with a posterior-only, single-stage approach [12-15]. Herein, we report two cases of BI and AAD who underwent surgery with the DCER technique instead of transoral excision for the first time in our region.
2. Case Presentation
Patients
The Institutional Review Committee approved this study, and written consent was obtained from the patients. Two patients with BI and AAD were operated on by the senior author and were followed up 12 months postoperatively.
Radiological assessment
Preoperative dynamic plain X-ray, magnetic resonance imaging (MRI), and computed tomography (CT) with sagittal, parasagittal, and coronal reconstruction were performed for both patients to thoroughly assess the joints and the severity of BI and AAD [12]. According to the plain X-ray, both patients had irreducible BI and AAD. The Chamberlain (normal being 2.3±2.6 mm below this line) [16, 17] and McRae lines (normal being 5.8±1.6 below this line) [18] were used for evaluating the BI. We measured the thickness and length of the C2 lamina to assess the suitability of screw insertion. The shape and size of the C1 lateral mass and the bilateral connection of the C1–C2 joints were also evaluated. Moreover, a CT angiogram was performed to identify the size and course of the vertebral arteries between the C1 and C2 segments. Associated syringomyelia and other intramedullary signal changes were noted pre-operatively and post-operatively.
One week after the surgery, both patients underwent imaging with plain x-rays and CT scans with reconstructed views to evaluate the screws’ position and the extent of the reduction. MRI was performed three months after the surgery to evaluate the extent of spinal cord and medulla oblongata decompression. Follow-up plain x-rays and CT scans with reconstructed views were repeated 12 months after the surgery to assess the position of the screws and the degree of bone fusion.
The craniovertebral junction (CVJ) is a complex area providing considerable mobility while marinating biomechanical stability [1]. Developmental CVJ anomalies usually consist of irreducible atlantoaxial dislocation (AAD) and basilar invagination (BI) associated with the occipital fusion of the C1 arch [2-4]. BI is the congenital upward displacement of the upper cervical spine (particularly the odontoid process) into the foramen magnum, which can be associated with AAD [5-8].
The previous techniques mainly focused on transoral excision of the dens, followed by posterior instrumented fusion [9-11]. In 2013, the distraction, compression, extension, and reduction (DCER) technique was introduced by Chandra et al. [12] to reduce, realign, and correct BI and AAD with a posterior-only, single-stage approach [12-15]. Herein, we report two cases of BI and AAD who underwent surgery with the DCER technique instead of transoral excision for the first time in our region.
2. Case Presentation
Patients
The Institutional Review Committee approved this study, and written consent was obtained from the patients. Two patients with BI and AAD were operated on by the senior author and were followed up 12 months postoperatively.
Radiological assessment
Preoperative dynamic plain X-ray, magnetic resonance imaging (MRI), and computed tomography (CT) with sagittal, parasagittal, and coronal reconstruction were performed for both patients to thoroughly assess the joints and the severity of BI and AAD [12]. According to the plain X-ray, both patients had irreducible BI and AAD. The Chamberlain (normal being 2.3±2.6 mm below this line) [16, 17] and McRae lines (normal being 5.8±1.6 below this line) [18] were used for evaluating the BI. We measured the thickness and length of the C2 lamina to assess the suitability of screw insertion. The shape and size of the C1 lateral mass and the bilateral connection of the C1–C2 joints were also evaluated. Moreover, a CT angiogram was performed to identify the size and course of the vertebral arteries between the C1 and C2 segments. Associated syringomyelia and other intramedullary signal changes were noted pre-operatively and post-operatively.
One week after the surgery, both patients underwent imaging with plain x-rays and CT scans with reconstructed views to evaluate the screws’ position and the extent of the reduction. MRI was performed three months after the surgery to evaluate the extent of spinal cord and medulla oblongata decompression. Follow-up plain x-rays and CT scans with reconstructed views were repeated 12 months after the surgery to assess the position of the screws and the degree of bone fusion.
Case 1
A 50-year-old man with a history of ischemic heart disease (under treatment with aspirin and clopidogrel) was referred to our neurosurgery clinic with a five-month complaint of severe pain in his hands, which was more significant on the right. He had no significant axial neck pain. On the physical examination, the muscle powers were 5/5 in all limbs except for his left foot during dorsiflexion (2/5) due to a traumatic injury five years earlier. Deep tendon reflexes (DTR) were 3/4; the plantar reflex was downward, and the Hoffman sign was positive. Neither saddle hypoesthesia nor incontinence was noted.
A cervical MRI showed severe stenosis of the craniocervical junction with a severe pressure effect on the cervicomedullary junction, causing an increased signal due to the posterior displacement of the odontoid process. At the C3–C4 level, evidence of a diffuse central osteophyte complex causing a pressure effect over the thecal sac with mild canal stenosis and mild bilateral neural foraminal stenosis touching the exiting nerve root was noted. Moreover, evidence of a mild central disc osteophyte complex at C4–C5 with minimal indentation over the thecal sac without any sign of neural foraminal stenosis or canal stenosis was observed. Using the plain x-rays and CT scans with reconstructed views, the diagnosis of BI and AAD was established, and traditional indices (McRae and Wackenheim) were used to evaluate BI severity (Figure 1 A).

A CT angiogram study was then conducted to evaluate the vertebral arteries. Following the investigations, surgery with the DCER technique was planned and discussed with the patient. First, he was positioned prone with his head fixed on a U-shaped headrest and the neck in a neutral position. After general anesthesia, a standard vertical midline incision was made from the inion to C6. Suboccipital decompression was done, followed by the insertion of a cervical occipital plate with four screws and five lateral mass screws (right C3 & C6; left C4, C5 & C6) with five nuts. One cross-link between two rods was applied, and a right C1–C2 facet joint spacer with a polyether ether ketone (PEEK)-cage was performed thereafter. A mesh plate with five mini-screws and a 20-cm rod was applied to limit graft materials contacting the dural sac; this was followed by the insertion of an autologous bone graft harvested from the right posterior iliac crest. Eventually, a C-arm was used to ensure the correct positioning of screws.
As mentioned earlier, postoperative imaging was done to evaluate the screws’ position and the extent of reduction (Figure 1). On the follow-up MRI, metallic fixation devices were seen in the posterior elements of the C3, C4, and C5 vertebral bodies. Disc osteophyte complexes were observed at C2-C3 and C3-C4 levels, causing bilateral narrowing of the neural foramina. Also, the disc space between C6-C7 is rudimentary suggestive of a block vertebra. In the 1-year follow-up, significant neurologic improvement was obvious and fusion in the cervical CT scan was detected (Figure 1 D).
Case 2
A 33-year-old man without any significant past medical history was referred with progressive right upper extremity weakness commencing a year beforehand Muscle forces were 5/5 except for the middle part of his right upper extremity (4/5), and he had hyperreflexia in the DTR evaluation (3/4). Hoffman’s sign was positive, the plantar reflex was downward, and the patient had no saddle hypoesthesia or incontinence.
After a thorough physical and radiological assessment, BI and AAD were diagnosed for the patient. The McRae, Chamberlain, and Wackenheim lines were measured (Figure 2 A), and surgery with the DCER technique was planned thereafter.
He was placed on the operating table in the prone position with his head fixed on a U-shaped headrest and neck placed in a neutral position. A standard midline incision was made from the occipital protuberance, and an interlaminar C2 screw was inserted under C-arm control. C2 laminectomy and C1 posterior arc removal (C1 assimilated to foramen magnum) were performed, followed by suboccipital decompression. After dural opening, tonsillar shrinkage was done by bipolar coagulator, and the dura was then repaired with a dural graft from the subperiosteal tissue. The occipital plate was placed, the rod was inserted, and the spacer graft was inserted in the C1-C2 joint bilaterally.
At the final follow-up, his Hoffman remained positive, and the patient had hyperreflexia. Postoperative MRI within 12 months of surgery revealed evidence of the previous operation in the posterior fossa and occipital skull bone, as well as a significant increase in cervical spine lordosis. Furthermore, super posterior displacement of the odontoid process of C2 was noted, narrowing the foramen of Monro and placing a pressure effect on the brainstem. Herniation of the cerebellum vermis was observed inferiorly from the foramen magnum, and an elongated tubular shape fluid signal (hyposignal in T1, hypersignal in T2) was seen within the central cervical spinal cord, indicative of a syrinx. Additionally, diffuse disc bulging was evident at the C2–C3 and C3–C4 levels, with indentation of the anterior aspect of the thecal sac and bilateral mild neural foraminal narrowing without canal stenosis.
The patient underwent a second surgery for the removal of rods and interlaminar C2 screw. Then, C3–C4 lateral mass screws (4 screws and 4 nuts) were placed, and C1–C2 fusion was done with two anterior cervical cages. Subsequently, 2 rods and one cross-link in between were applied, and a graft was inserted bilaterally. Postoperative cervical MRI demonstrated herniation of the cerebellum through the foramen magnum and narrowing of the cervicomedullary junction (anteroposterior diameter =9.5 mm), associated with signal changes in the cord at this area. Also, evidence of elongated cystic dilatation with fluid signal intensity in the central part of the cervical cord was noted, suggestive of a syrinx.
3. Discussion
As complicated conditions, AAD and BI progressively cause cervicomedullary compression and neurological deficits. Treatment focuses on decreasing the compression and providing sensible stability and deformity correction [5, 6, 19, 20]. These congenital disorders usually cannot be reduced by cervical traction with dynamic x-rays. Cases are mostly associated with atlas assimilation with the occiput [4, 15]. Notably, both our patients had irreducible AAD and BI. Conventionally, BI with AAD was treated through an anterior transoral approach and removal of the odontoid process, followed by a posterior instrumented fixation [9, 10, 21, 15].
In some cases, traction reduces AAD; however, BIs cannot be reduced on traction [5, 6], and there is some consensus that such cases should be treated with decompression and stabilization without deformity correction [9-11, 21]. Before 2010, Goel et al. introduced a technique through which BIs could be realigned by distraction (using a spacer within the joint) with C1–C2 fixation [5, 6, 22]. Jian et al. [23] and Y. Meng et al. [24] reported cases of irreducible BI in China. They introduced a moderately new concept of intraoperative manipulation in which both BI and AAD were reduced in cases of BI with an assimilated C1 arch. In this technique, after direct posterior decompression and distraction, a rod was connected to a C2 pedicular screw, and occipitocervical fixation was performed. Notwithstanding their favorable outcomes, it had a weakness in providing distraction only as a method of reduction for both AAD and BI. Optimal reduction in cases with AAD can be achieved by a forward movement of the dens, whereas BI requires only a vertical distraction. Furthermore, their results showed a risk of resettling in cases where distraction was performed without spacer placement.
Hsu et al. [25] tackled this issue using a novel technique for two patients with acquired occipitocervical instability in 2010. Beyond and above that, they applied compression between the upper occipital screw and another superior screw on the rod to provide an extension of the neck, thereby correcting the AAD. According to their results, although distraction corrects BI, AAD correction can be attained by simultaneous extension and distraction.
Chandra et al. [12] described the DCER technique in 2013 in India, constituting the distraction of joint space with spacers (in the occipito-C1-C2 joint space) before compression between the occiput and C2, resulting in extension at the occipito-C1-C2 joint and causing AAD reduction. They explicated that 94% of cases with AAD and all cases with BI were reduced completely using the DCER technique. Their other case series published in 2013 and 2015 [12, 14] developed this procedure with novel devices, reporting improvements in terms of indices, fusion rates, and complications. At the same time, in India, Salunke et al. [26, 27] utilized “drilling of the C1–2 facets and direct posterior reduction with joint spacer” for 35 cases of non-reducible BI and AAD. The major principles followed were identical to Chandra et al.’s, yet they were not referred to as the DCER procedure.
Chandra et al. also reported their largest and latest series in 2019 [28], including 148 cases of BI treated with the DCER procedure. They attained a better understanding of BI, radiologic indices, indications and contraindications, and the main challenges of the DCER procedure. Based on this study, non-reducible BI is classified into three main types according to the sagittal inclination (SI) angle. This is the angle measured between the line parallel to the axis of the dense process (drawn tangential to its posterior border) and a line parallel to the C1–C2 joint surface with a normal range of 87.15±5.65°. The SI angle was classified as less than 100° (type I), 100–160° (type II), and more than 160° (type III). For each type, Chandra et al. recommended the following surgical procedure, with further details provided in their manuscript [28]:
- Type I: DCER
- Type II: Joint remodeling+DCER
- Type III: Extra-articular distraction+DCER
As reviewed in Table 1, recent concepts regarding non-reducible BI and AAD management can be classified into two major approaches: (i) Posterior decompression and reduction with occipitocervical fixation and (ii) the DCER procedure with C1–C2 facet joint spacer application. Fusion in both recent methods was the same and complete.
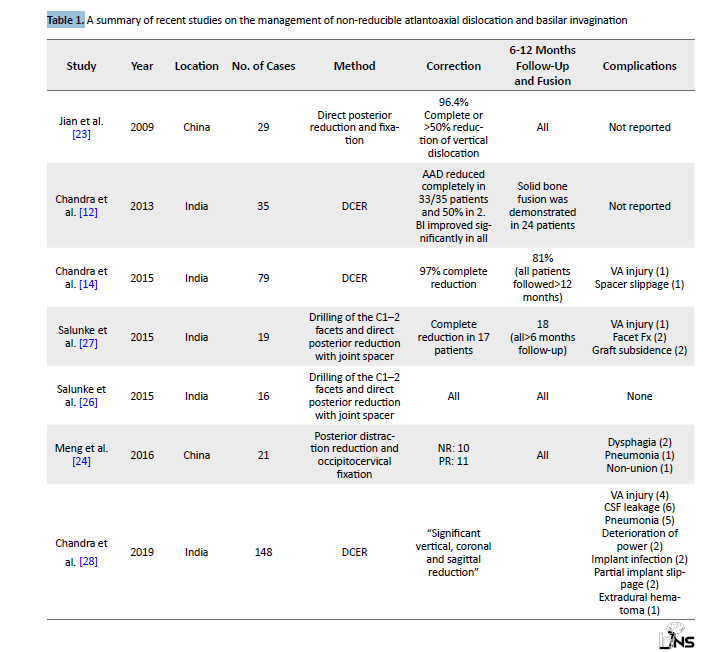
Correction of indices and reduction rates have been significantly superior in methods including the C1–C2 joint spacer and vertical reduction. Although major complications cannot be compared in detail due to the small numbers reported, in both methods, vertebral artery injury was reported as the most severe complication with a slightly higher rate in DCER procedures.
In line with the literature and the latest Chandra et al.’s data [28], we successfully treated two individuals with BI and AAD using the DCER technique for the first time in our center and reported for the first time in Iran. Both cases were type-II non-reducible BI, and achievements in correcting radiologic indices are summarized in Table 2.
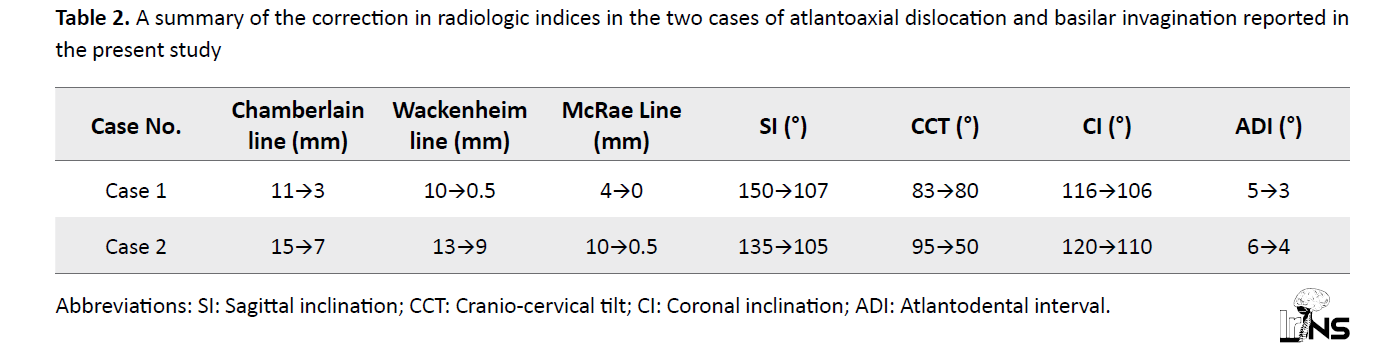
In the first case, the patient’s age (causing BI to be more severe and rigid) and the lack of appropriate new devices for the DCER procedure led to the failure of the correction of CCT. Occipitocervical fusion was also an important part of this procedure due to the specific biomechanics of the craniocervical junction region [29].
4. Conclusion
The result of this research can be revised in the future with a simpler and single approach due to the small sample size and selection bias. Nonetheless, we achieved acceptable clinical improvement and vertical reduction.
Based on previous studies [12, 14, 28], it can be inferred that the DCER technique, mainly grounded upon the principle of utilizing a spacer as a fulcrum, is a safe and more effective strategy to correct AAD and BI through a single-stage posterior approach.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from all patients.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, study design and drafting the article: Majidreza farrokhi and Seyed Reza Mousavi; Data collection: Seyed Reza Mousavi; Critically revising the article and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Gonzalez LF, Crawford NR, Chamberlain RH, Garza LEP, Preul MC, Sonntag VK, et al. Craniovertebral junction fixation with transarticular screws: biomechanical analysis of a novel technique. Journal of Neurosurgery: Spine. 2003; 98(2):202-9. [DOI:10.3171/spi.2003.98.2.0202] [PMID]
- Ahmed R, Traynelis VC, Menezes AH. Fusions at the craniovertebral junction. Child’s Nervous System. 2008; 24(10):1209-24. [DOI:10.1007/s00381-008-0607-7] [PMID]
- Bharucha E, Dastur H. Craniovertebral anomalies: A report on 40 cases. Brain. 1964; 87(3):469-80. [DOI:10.1093/brain/87.3.469] [PMID]
- Chandra PS. Irreducible basilar invagination and atlanto-axial dislocation: Are they really “irreducible”? Indian Journal of Neurosurgery. 2012; 1(02):101-4. [DOI:10.4103/2277-9167.102264]
- Goel A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. Journal of Neurosurgery: Spine. 2004; 1(3):281-6. [DOI:10.3171/spi.2004.1.3.0281] [PMID]
- Goel A. Progressive basilar invagination after transoral odontoidectomy: Treatment by atlantoaxial facet distraction and craniovertebral realignment. Spine. 2005; 30(18):E551-5. [DOI:10.1097/01.brs.0000179414.64741.7b] [PMID]
- Goel A. Double insurance atlantoaxial fixation. Surgical Neurology. 2007; 67(2):135-9. [DOI:10.1016/j.surneu.2006.05.059] [PMID]
- Ding X, Abumi K, Ito M, Sudo H, Takahata M, Nagahama K, et al. A retrospective study of congenital osseous anomalies at the craniocervical junction treated by occipitocervical plate-rod systems. European Spine Journal. 2012; 21(8):1580-9. [DOI:10.1007/s00586-012-2324-x] [PMID] [PMCID]
- Landeiro JA, Boechat S, Christoph DdH, Gonçalves MB, Castro Id, Lapenta MA, et al. Transoral approach to the craniovertebral junction. Arquivos de Neuro-Psiquiatria. 2007; 65(4):1166-71. [DOI:10.1590/S0004-282X2007000700014] [PMID]
- Lee ST, Fairholm DJ. Transoral anterior decompression for treatment of unreducible atlantoaxial dislocations. Surgical Neurology. 1985; 23(3):244-8. [DOI:10.1016/0090-3019(85)90089-8] [PMID]
- Wang T, Zeng B, Xu J. Transoral reduction of irreducible posteriorly displaced odontoid fracture. European Spine Journal. 2011; 20(Suppl 2):S227-30. [DOI:10.1007/s00586-010-1596-2] [PMID] [PMCID]
- Chandra PS, Kumar A, Chauhan A, Ansari A, Mishra NK, Sharma BS. Distraction, compression, and extension reduction of basilar invagination and atlantoaxial dislocation: A novel pilot technique. Neurosurgery. 2013; 72(6):1040-53. [DOI:10.1227/NEU.0b013e31828bf342] [PMID]
- Chandra PS, Goyal N, Chauhan A, Ansari A, Sharma BS, Garg A. The severity of basilar invagination and atlantoaxial dislocation correlates with sagittal joint inclination, coronal joint inclination, and craniocervical tilt: A description of new indexes for the craniovertebral junction. OperativeNeurosurgery. 2014; 10(4):621-30. [DOI:10.1227/NEU.0000000000000470] [PMID]
- Chandra PS, Prabhu M, Goyal N, Garg A, Chauhan A, Sharma BS. Distraction, compression, extension, and reduction combined with joint remodeling and extra-articular distraction: description of 2 new modifications for its application in basilar invagination and atlantoaxial dislocation: prospective study in 79 cases. Neurosurgery. 2015; 77(1):67-80. [DOI:10.1227/NEU.0000000000000737] [PMID]
- Joaquim AF, Tedeschi H, Chandra PS. Controversies in the surgical management of congenital craniocervical junction disorders-A critical review. Neurology India. 2018; 66(4):1003-15. [DOI:10.4103/0028-3886.237025] [PMID]
- Cronin C, Lohan D, Mhuircheartigh JN, Meehan C, Murphy J, Roche C. CT evaluation of Chamberlain’s, McGregor’s, and McRae’s skull-base lines. Clinical Radiology. 2009; 64(1):64-9. [DOI:10.1016/j.crad.2008.03.012] [PMID]
- Kwong Y, Rao N, Latief K. Craniometric measurements in the assessment of craniovertebral settling: Are they still relevant in the age of cross-sectional imaging? American Journal of Roentgenology. 2011; 196(4):W421-W5. [DOI:10.2214/AJR.10.5339] [PMID]
- McRae D. Occipitalization of atlas. American Journal of Roentgenology. 1953; 70:23-45. [Link]
- Fenoy AJ, Menezes AH, Fenoy KA. Craniocervical junction fusions in patients with hindbrain herniation and syringohydromyelia. Journal of Neurosurgery: Spine. 2008; 9(1):1-9. [DOI:10.3171/SPI/2008/9/7/001] [PMID]
- Aryan HE, Newman CB, Nottmeier EW, Acosta FL, Wang VY, Ames CP. Stabilization of the atlantoaxial complex via C-1 lateral mass and C-2 pedicle screw fixation in a multicenter clinical experience in 102 patients: Modification of the Harms and Goel techniques. Journal of Neurosurgery: Spine. 2008; 8(3):222-9. [DOI:10.3171/SPI/2008/8/3/222] [PMID]
- Mummaneni PV, Haid RW. Transoral odontoidectomy. Neurosurgery. 2005; 56(5):1045-50. [Link]
- Goel A, Pareikh S, Sharma P. Atlantoaxial joint distraction for treatment of basilar invagination secondary to rheumatoid arthritis. Neurology India. 2005; 53(2):238-40. [DOI:10.4103/0028-3886.16424] [PMID]
- Jian FZ, Chen Z, Wrede KH, Samii M, Ling F. Direct posterior reduction and fixation for the treatment of basilar invagination with atlantoaxial dislocation. Neurosurgery. 2010; 66(4):678-87. [DOI:10.1227/01.NEU.0000367632.45384.5A] [PMID]
- Meng Y, Chen H, Lou J, Rong X, Wang B, Deng Y, et al. Posterior distraction reduction and occipitocervical fixation for the treatment of basilar invagination and atlantoaxial dislocation. Clinical Neurology and Neurosurgery. 2016; 140:60-7. [DOI:10.1016/j.clineuro.2015.11.011] [PMID]
- Wesley H, Zaidi HA, Suk I, Gokaslan ZL, Wolinsky JP. A new technique for intraoperative reduction of occipitocervical instability. Operative Neurosurgery. 2010; 66(6):ons319-24. [DOI:10.1227/01.NEU.0000369925.81522.60] [PMID]
- Salunke P, Sahoo S, Khandelwal NK, Ghuman MS. Technique for direct posterior reduction in irreducible atlantoaxial dislocation: Multi-planar realignment of C1-2. Clinical Neurology and Neurosurgery. 2015; 131:47-53. [DOI:10.1016/j.clineuro.2015.01.025] [PMID]
- Salunke P, Futane S, Sharma M, Sahoo S, Kovilapu U, Khandelwal NK. ‘Pseudofacets’ or ‘supernumerary facets’ in congenital atlanto-axial dislocation: Boon or bane? European Spine Journal. 2015; 24(1):80-7. [Link]
- Sarat Chandra P, Bajaj J, Singh PK, Garg K, Agarwal D. Basilar invagination and atlantoaxial dislocation: Reduction, deformity correction and realignment using the DCER (distraction, compression, extension, and reduction) technique with customized instrumentation and implants. Neurospine. 2019; 16(2):231-50. [DOI:10.14245/ns.1938194.097] [PMID] [PMCID]
- Mousavi R, Farrokhi MR, Eghbal K, Safaee J, Dehghanian AR. Reconstruction of C1 lateral mass with an expandable cage in addition to vertebral artery preservation: presenting two cases. British Journal of Neurosurgery. 2021;16:1-6. [DOI:10.1080/02688697.2021.1978393] [PMID]
Type of Study: Case Series |
Subject:
Spine
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |



