Fri, May 3, 2024
Volume 9 - Continuous Publishing
Iran J Neurosurg 2023, 9 - Continuous Publishing: 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Karimian F, Saadat S, Hosseininezhad M. Chronic Pain and Psychological Interventions: A Systematic Review. Iran J Neurosurg 2023; 9 : 8
URL: http://irjns.org/article-1-343-en.html
URL: http://irjns.org/article-1-343-en.html
1- Department of Psychology, University of Guilan, Guilan, Iran
2- Neuroscience Research Center, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
3- Department of Neurology, Neuroscience Research Center, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran , hosseininezhadm@gmail.com
2- Neuroscience Research Center, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
3- Department of Neurology, Neuroscience Research Center, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran , hosseininezhadm@gmail.com
Full Text [PDF 932 kb]
(488 Downloads)
| Abstract (HTML) (1266 Views)
Full Text: (625 Views)
1. Introduction
The recognition of pain as a pathologic entity remains controversial [1]. Chronic pain is an emotional experience and is defined as pain that lasts longer than 6 months. Understanding the neurophysiology of pain is necessary to treat it as it is a common, complex, and distressing problem with profound implications for individuals and societies [2, 3]. Pain is associated with reduced mobility, activity avoidance, falls, depression and anxiety, sleep disturbances, and significant disability from isolation. The negative effects extend beyond the patient, disrupting both family and social relationships [4].
Chronic pain can have a significant impact on the quality of life. Many patients develop depression, anxiety, or sleep disturbances, or develop stress, pain-related anxiety, devastating situations, significant pain intensity, general loss of enthusiasm for life, poor emotional health, fatigue, weakness, and sleep-related problems [5, 6, 7]. Chronic pain often causes significant difficulties in personal and social life and negatively impacts the ability to work and participate in the labor market along with negative individual consequences, such as low quality of life and mental health [8].
Psychotherapy focuses on skillful coping responses and cognitive-behavioral techniques. Some treatments such as cognitive behavioral therapy (CBT) are relatively focused on acceptance- and experience (ACT)-based treatment methods, committed behavior, and patient values. Other treatments, such as ACT, aim to help individuals in coping and suffering openly without futile resistance or struggle, which is also known as acceptance [8]. Psychological interventions can directly improve self-management knowledge and stress management skills, enhance coping skills and emotional regulation, and help people adapt to chronic illness [9].
Numerous studies show that interventions such as CBT, ACT, mindfulness, restricted environmental stimulation therapy (REST), improving pain during addiction treatment (IMPAT), and so on can increase patients’ functioning and coping skills, emotional management, interpersonal functioning, and improve communications with peers and family members [10]. Also, the self-efficacy scale, quality of life, self-esteem, emotional state, pain, pain intensity, pain control, pain destruction, pain interference, life satisfaction, positive emotions, and symptom control for depression and pain management were significantly improved [11, 12].
Extensive research exists on chronic pain, and by selecting and reviewing them, the nature of pain and the importance of psychological interventions in the field of pain control, improving quality of life, and increasing positive emotions can be comprehended. This review aims to examine patients with chronic pain and the psychological interventions or psychotherapies that are done for the recovery of these patients.
2. Methods and Materials/Patients
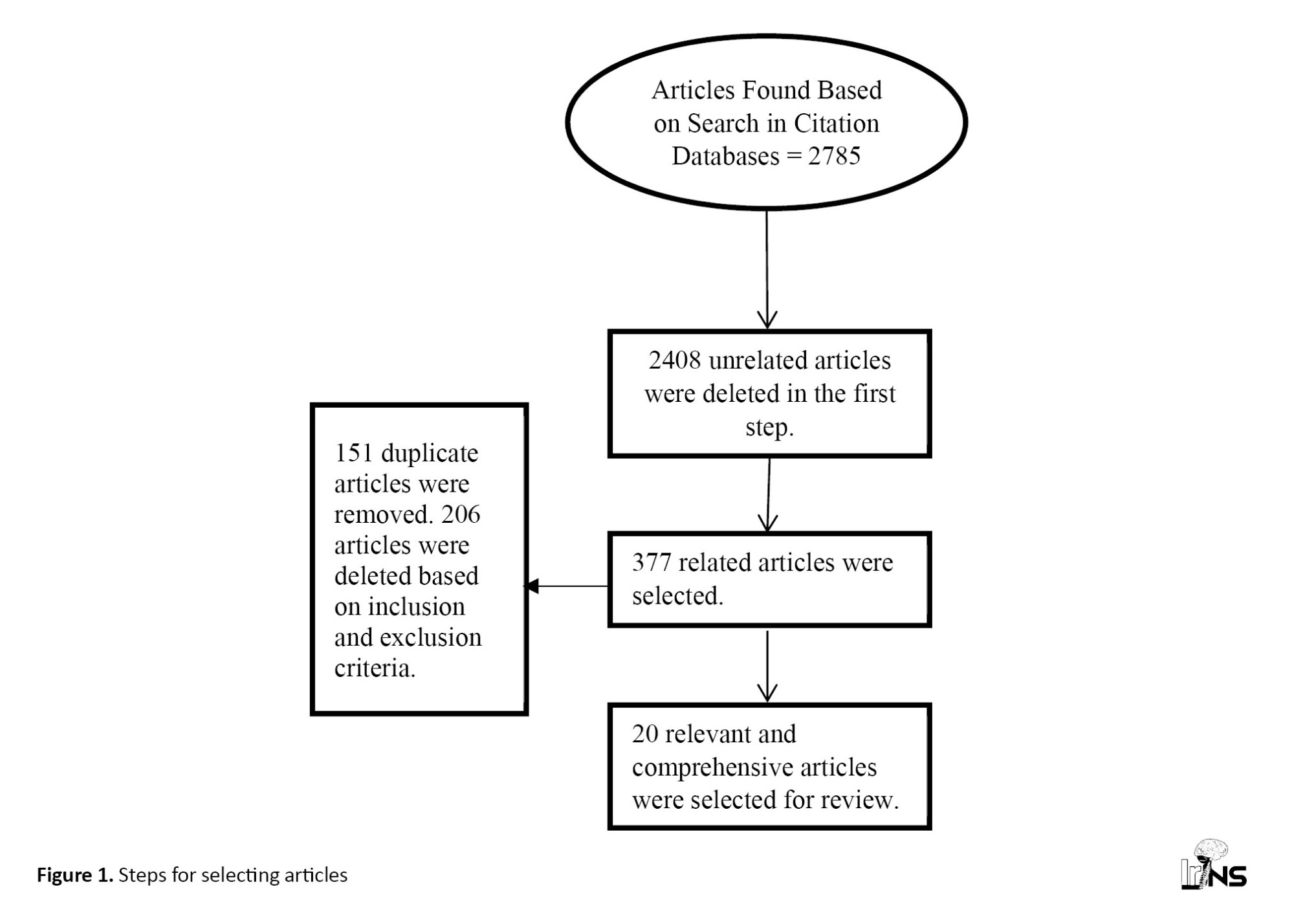
This was a systematic review of published studies from January 2018 to November 2022. The search was conducted on Scopus, PubMed, and Google Scholar databases. To search for articles, the following keywords were used for the online search: Chronic pain, psychological interventions, psychotherapy, psychology, clinical trials, and randomized clinical trials. To carefully select the keywords, all keywords related to chronic pain were searched. A total of 2785 articles with the keyword in the title or article content were found. Article titles and abstracts were reviewed by two investigators and a large number of articles were excluded from the review because of being repetitive, unrelated, or failing to meet the inclusion criteria. Finally, 20 articles were selected and reviewed. Figure 1 demonstrates the steps for checking the sources.
The recognition of pain as a pathologic entity remains controversial [1]. Chronic pain is an emotional experience and is defined as pain that lasts longer than 6 months. Understanding the neurophysiology of pain is necessary to treat it as it is a common, complex, and distressing problem with profound implications for individuals and societies [2, 3]. Pain is associated with reduced mobility, activity avoidance, falls, depression and anxiety, sleep disturbances, and significant disability from isolation. The negative effects extend beyond the patient, disrupting both family and social relationships [4].
Chronic pain can have a significant impact on the quality of life. Many patients develop depression, anxiety, or sleep disturbances, or develop stress, pain-related anxiety, devastating situations, significant pain intensity, general loss of enthusiasm for life, poor emotional health, fatigue, weakness, and sleep-related problems [5, 6, 7]. Chronic pain often causes significant difficulties in personal and social life and negatively impacts the ability to work and participate in the labor market along with negative individual consequences, such as low quality of life and mental health [8].
Psychotherapy focuses on skillful coping responses and cognitive-behavioral techniques. Some treatments such as cognitive behavioral therapy (CBT) are relatively focused on acceptance- and experience (ACT)-based treatment methods, committed behavior, and patient values. Other treatments, such as ACT, aim to help individuals in coping and suffering openly without futile resistance or struggle, which is also known as acceptance [8]. Psychological interventions can directly improve self-management knowledge and stress management skills, enhance coping skills and emotional regulation, and help people adapt to chronic illness [9].
Numerous studies show that interventions such as CBT, ACT, mindfulness, restricted environmental stimulation therapy (REST), improving pain during addiction treatment (IMPAT), and so on can increase patients’ functioning and coping skills, emotional management, interpersonal functioning, and improve communications with peers and family members [10]. Also, the self-efficacy scale, quality of life, self-esteem, emotional state, pain, pain intensity, pain control, pain destruction, pain interference, life satisfaction, positive emotions, and symptom control for depression and pain management were significantly improved [11, 12].
Extensive research exists on chronic pain, and by selecting and reviewing them, the nature of pain and the importance of psychological interventions in the field of pain control, improving quality of life, and increasing positive emotions can be comprehended. This review aims to examine patients with chronic pain and the psychological interventions or psychotherapies that are done for the recovery of these patients.
2. Methods and Materials/Patients
This was a systematic review of published studies from January 2018 to November 2022. The search was conducted on Scopus, PubMed, and Google Scholar databases. To search for articles, the following keywords were used for the online search: Chronic pain, psychological interventions, psychotherapy, psychology, clinical trials, and randomized clinical trials. To carefully select the keywords, all keywords related to chronic pain were searched. A total of 2785 articles with the keyword in the title or article content were found. Article titles and abstracts were reviewed by two investigators and a large number of articles were excluded from the review because of being repetitive, unrelated, or failing to meet the inclusion criteria. Finally, 20 articles were selected and reviewed. Figure 1 demonstrates the steps for checking the sources.
Publication of articles in a certain period, publication in English, and studies implemented on patients with chronic pain were among the criteria for the inclusion of articles. Qualitative and single-case articles, case reports, and articles based on pharmaceutical and medical interventions were considered the exclusion criteria. The framework of the standard review of health articles [13], the Sidant and Braden approach, was used to review and evaluate behavioral interventions [14]. To analyze the articles, authors’ names, the year of publication, the type of intervention or theoretical framework, the country in which the study was conducted, the number of study participants, the intervention implementation method, and the results of the study were considered.
3. Results
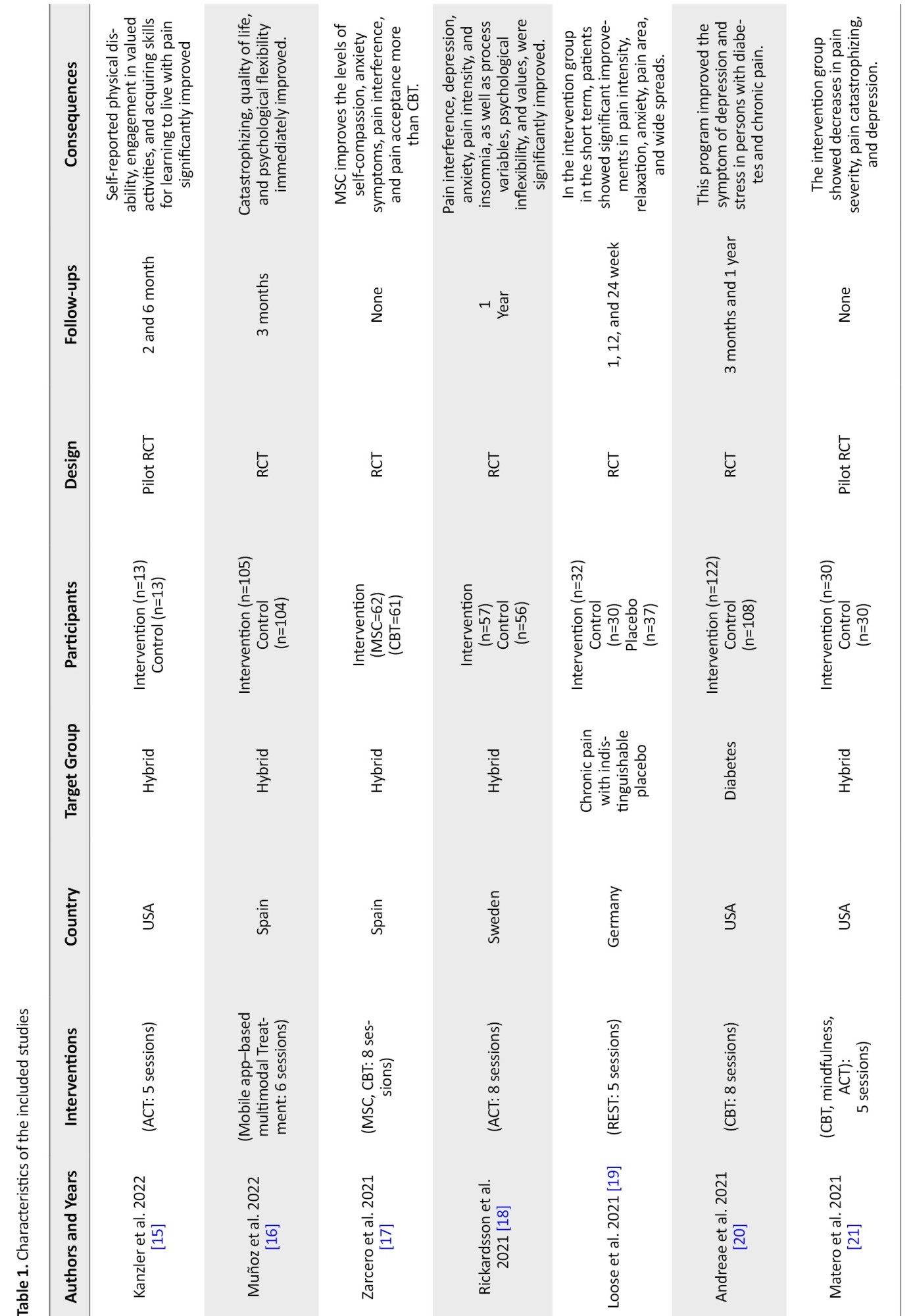
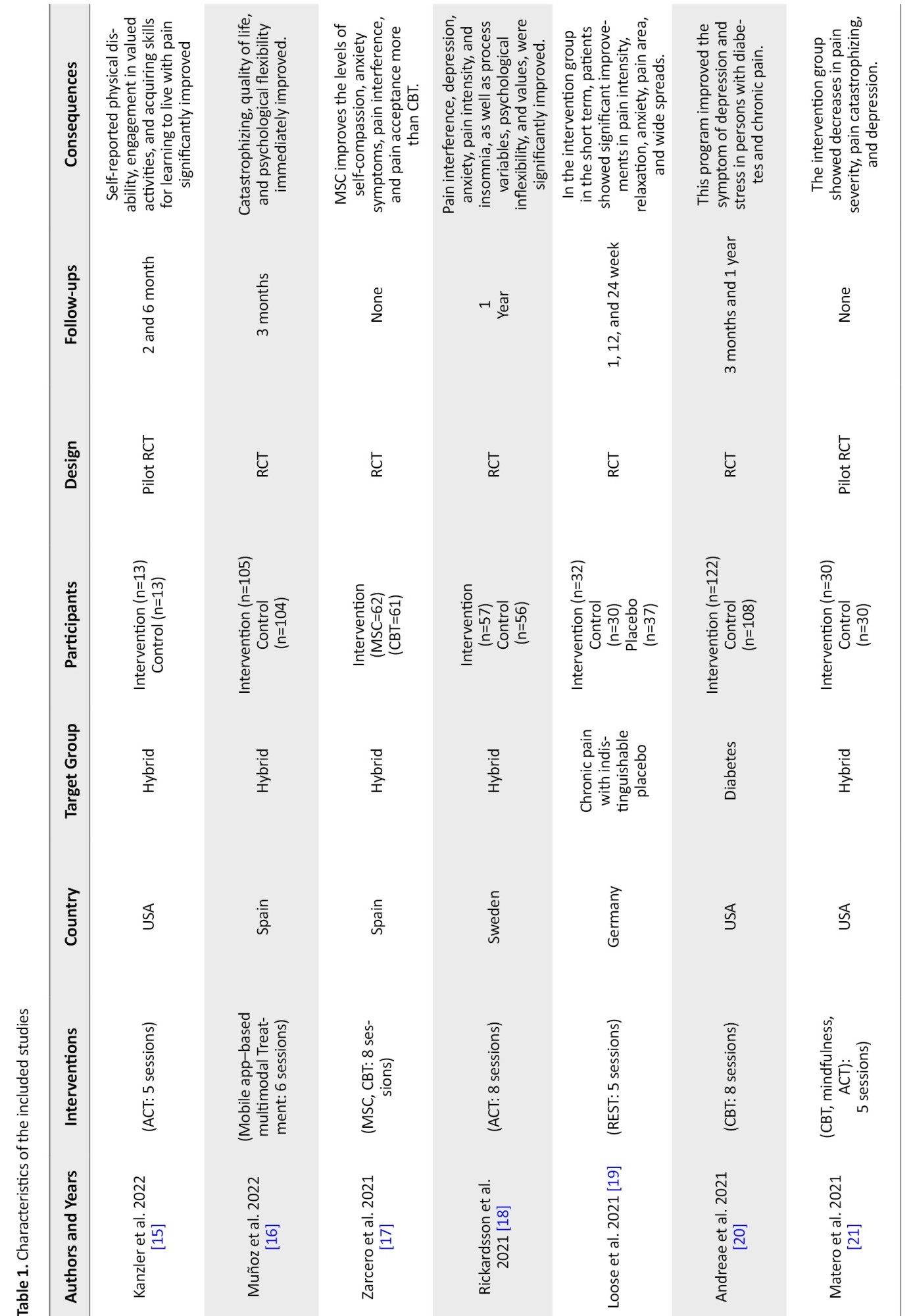
Based on inclusion criteria, 20 articles were selected for this section and analyzed in the following aspects (Table 1): Type of intervention, participants, country, study design, follow-up, and results.


A total of 2078 people participated in these studies. From the review of previous studies, it was found that psychological interventions such as CBT [17, 20, 21, 22, 32], ACT [15, 18], and then the treatment models derived from mindfulness [17, 34] were the most used methods in improving the psychological performance of people with chronic pain. The results of a review of various therapeutic interventions indicate that these treatments have the greatest effect on pain reduction [17-24, 26, 28], quality of life [15, 16], depression [18, 20, 21] and stress [16, 17, 18, 19, 23].
4. Discussion
This study aimed to show the nature of chronic pain, examine patients with this problem, and the interventions that were used to improve the process of their disorder. In this study, 20 articles were reviewed and all of them were from different countries. According to the results, the most used treatment in the studies was CBT [20, 21, 22, 32], ACT [15, 18], and mindfulness [17, 34], respectively, in patients with chronic pain. These treatments lead to cognitive restructuring and increasing access and engagement in behavioral pain management services. Patients exhibited improved pain outcomes [20, 21, 32].
Chronic pain can be the result of a complex health condition that has negative multi-dimensional effects on performance [27]. If there are factors such as improved pain management, improved psychological well-being, and the development of meaningful connections, these individuals can build resilience in the face of life’s challenges [29]. Also, some studies showed non-pharmacological treatments, such as physical therapy and psychoeducational therapy to promote active participation that works well in combination with pharmacological strategies, and that such interventions are effective for patients with chronic pain. It has also been shown to improve independence and help manage pain effectively [16].
Psychological interventions were most effective in pain control and management, quality of life, pain intensity, pain destruction, depression, anxiety, and social and emotional connection. Among all these interventions, the role of CBT was more important. Given its role in improving depressive symptoms and stress in individuals with chronic pain, this method was also effective in reducing pain severity and disability [20, 21, 22]. CBT can be used in multidisciplinary pain management programs. It can directly intervene in the excessive thoughts, worries, feelings, and behaviors associated with physical symptoms and are the most common psychotherapy for chronic pain [22].
We suggest that for the effectiveness and better quality of the treatment frameworks considered for chronic pain, more combined treatments, such as the combination of CBT, ACT, and mindfulness should be used, and the existence of long-term follow-ups will help in this process. It is also possible to use meta-diagnostic approaches.
5. Conclusion
Considering that the etiology of chronic pain can be explained based on biological and psychological factors, medical and psychological interventions are suggested to be provided in an integrated manner by the medical team in treatment centers to improve the psychological health of these people.
Ethical Considerations
Compliance with ethical guidelines
There was no animal or human research reported in this study so there was no need for obtaining the approval of any Ethics Committee.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
The authors declared no conflict of interest.
Conflict of interest
Conceptualization and study design: Fatemeh Karimian and Sajjad Saadat; Critically revising: Sajjad Saadat and Mozaffar Hosseininezhad; Data collection, data analysis and interpretation, drafting and final approving: All authors
Acknowledgements
The authors appreciate all the researchers whose papers were examined in this study.
References
3. Results
Based on inclusion criteria, 20 articles were selected for this section and analyzed in the following aspects (Table 1): Type of intervention, participants, country, study design, follow-up, and results.


A total of 2078 people participated in these studies. From the review of previous studies, it was found that psychological interventions such as CBT [17, 20, 21, 22, 32], ACT [15, 18], and then the treatment models derived from mindfulness [17, 34] were the most used methods in improving the psychological performance of people with chronic pain. The results of a review of various therapeutic interventions indicate that these treatments have the greatest effect on pain reduction [17-24, 26, 28], quality of life [15, 16], depression [18, 20, 21] and stress [16, 17, 18, 19, 23].
4. Discussion
This study aimed to show the nature of chronic pain, examine patients with this problem, and the interventions that were used to improve the process of their disorder. In this study, 20 articles were reviewed and all of them were from different countries. According to the results, the most used treatment in the studies was CBT [20, 21, 22, 32], ACT [15, 18], and mindfulness [17, 34], respectively, in patients with chronic pain. These treatments lead to cognitive restructuring and increasing access and engagement in behavioral pain management services. Patients exhibited improved pain outcomes [20, 21, 32].
Chronic pain can be the result of a complex health condition that has negative multi-dimensional effects on performance [27]. If there are factors such as improved pain management, improved psychological well-being, and the development of meaningful connections, these individuals can build resilience in the face of life’s challenges [29]. Also, some studies showed non-pharmacological treatments, such as physical therapy and psychoeducational therapy to promote active participation that works well in combination with pharmacological strategies, and that such interventions are effective for patients with chronic pain. It has also been shown to improve independence and help manage pain effectively [16].
Psychological interventions were most effective in pain control and management, quality of life, pain intensity, pain destruction, depression, anxiety, and social and emotional connection. Among all these interventions, the role of CBT was more important. Given its role in improving depressive symptoms and stress in individuals with chronic pain, this method was also effective in reducing pain severity and disability [20, 21, 22]. CBT can be used in multidisciplinary pain management programs. It can directly intervene in the excessive thoughts, worries, feelings, and behaviors associated with physical symptoms and are the most common psychotherapy for chronic pain [22].
We suggest that for the effectiveness and better quality of the treatment frameworks considered for chronic pain, more combined treatments, such as the combination of CBT, ACT, and mindfulness should be used, and the existence of long-term follow-ups will help in this process. It is also possible to use meta-diagnostic approaches.
5. Conclusion
Considering that the etiology of chronic pain can be explained based on biological and psychological factors, medical and psychological interventions are suggested to be provided in an integrated manner by the medical team in treatment centers to improve the psychological health of these people.
Ethical Considerations
Compliance with ethical guidelines
There was no animal or human research reported in this study so there was no need for obtaining the approval of any Ethics Committee.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
The authors declared no conflict of interest.
Conflict of interest
Conceptualization and study design: Fatemeh Karimian and Sajjad Saadat; Critically revising: Sajjad Saadat and Mozaffar Hosseininezhad; Data collection, data analysis and interpretation, drafting and final approving: All authors
Acknowledgements
The authors appreciate all the researchers whose papers were examined in this study.
References
- Raffaeli W, Arnaudo E. Pain as a disease: An overview. Journal of Pain Research. 2017; 10:2003-8. [DOI:10.2147/JPR.S138864] [PMID] [PMCID]
- Mills SEE, Nicolson KP, Smith BH. Chronic pain: A review of its epidemiology and associated factors in population-based studies. British Journal of Anaesthesia. 2019; 123(2):e273-83. [DOI:10.1016/j.bja.2019.03.023] [PMID] [PMCID]
- Russo CM, Brose WG. Chronic pain. Annual Review of Medicine. 1998; 49:123-33. [DOI:10.1146/annurev.med.49.1.123] [PMID]
- Bicket MC, Mao J. Chronic pain in older adults. Anesthesiology Clinics. 2015; 33(3):577-90. [DOI:10.1016/j.anclin.2015.05.011] [PMID]
- Poli P, Crestani F, Salvadori C, Valenti I, Sannino C. Medical cannabis in patients with chronic pain: Effect on pain relief, pain disability, and psychological aspects. A prospective non randomized single arm clinical trial. La Clinica Terapeutica. 2018; 169(3):e102-7. [Link]
- Bromley Milton M, Börsbo B, Rovner G, Lundgren-Nilsson Å, Stibrant-Sunnerhagen K, Gerdle B. Is pain intensity really that important to assess in chronic pain patients? A study based on the Swedish Quality Registry for Pain Rehabilitation (SQRP). PLoS One. 2013; 8(6):e65483. [DOI:10.1371/journal.pone.0065483] [PMID] [PMCID]
- DasMahapatra P, Chiauzzi E, Pujol LM, Los C, Trudeau KJ. Mediators and moderators of chronic pain outcomes in an online self-management program. The Clinical Journal of Pain. 2015; 31(5):404-13. [DOI:10.1097/AJP.0000000000000125] [PMID] [PMCID]
- Linnemørken LT, Sveinsdottir V, Knutzen T, Rødevand L, Hernæs KH, Reme SE. Protocol for the Individual Placement and Support (IPS) in pain trial: A randomized controlled trial investigating the effectiveness of IPS for patients with chronic pain. BMC Musculoskeletal Disorders. 2018; 19(1):47. [DOI:10.1186/s12891-018-1962-5] [PMID] [PMCID]
- Saadat S, Hosseininezhad M, Khatami SS, Ghasemi Jobaneh R. Psychological Interventions in chronic low back pain: A systematic review. Iranian Journal of Neurosurgery. 2021; 7(2):67-74. [DOI:10.32598/irjns.7.2.1]
- Gauntlett-Gilbert J, Connell H, Clinch J, McCracken LM. Acceptance and values-based treatment of adolescents with chronic pain: Outcomes and their relationship to acceptance. Journal of Pediatric Psychology. 2013; 38(1):72-81. [DOI:10.1093/jpepsy/jss098] [PMID]
- García-Dasí M, Pérez-Alenda S, Carrasco JJ, Marques-Sule E, Aguilar-Rodríguez M, Moreno-Segura N, et al. Effects of a non-pharmacological approach for chronic pain management in patients with haemophilia: Efficacy of cognitive-behavioural therapy associated with physiotherapy. Haemophilia. 2021; 27(3):e357-67. [DOI:10.1111/hae.14284] [PMID]
- Müller R, Gertz KJ, Molton IR, Terrill AL, Bombardier CH, Ehde DM, et al. Effects of a tailored positive psychology intervention on well-being and pain in individuals with chronic pain and a physical disability: A feasibility trial. The Clinical Journal of Pain. 2016; 32(1):32-44. [DOI:10.1097/AJP.0000000000000225] [PMID]
- Yarmohamadian M, Mohammadi E, Movahedi F. Standards for writing review articles. Health Inf Manage 2011; 8(8): 1226-34. [Link]
- Sidani S, Braden C. Evaluating nursing interventions: A theory-driven approach. Ravensdale, WA: Sage Publications; 1998. [DOI:10.4135/9781452232942]
- Kanzler KE, Robinson PJ, McGeary DD, Mintz J, Kilpela LS, Finley EP, et al. Addressing chronic pain with Focused Acceptance and Commitment Therapy in integrated primary care: Findings from a mixed methods pilot randomized controlled trial. BMC Primary Care. 2022; 23(1):77. [DOI:10.1186/s12875-022-01690-2] [PMID] [PMCID]
- Morcillo-Muñoz Y, Sánchez-Guarnido AJ, Calzón-Fernández S, Baena-Parejo I. Multimodal chronic pain therapy for adults via smartphone: Randomized controlled clinical trial. Journal of Medical Internet Research. 2022; 24(5):e36114. [DOI:10.2196/36114] [PMID] [PMCID]
- Torrijos-Zarcero M, Mediavilla R, Rodríguez-Vega B, Del Río-Diéguez M, López-Álvarez I, Rocamora-González C, et al. Mindful self-compassion program for chronic pain patients: A randomized controlled trial. European Journal of Pain. 2021; 25(4):930-44. [DOI:10.1002/ejp.1734] [PMID]
- Rickardsson J, Gentili C, Holmström L, Zetterqvist V, Andersson E, Persson J, et al. Internet-delivered acceptance and commitment therapy as microlearning for chronic pain: A randomized controlled trial with 1-year follow-up. European Journal of Pain. 2021; 25(5):1012-30. [DOI:10.1002/ejp.1723] [PMID]
- Loose LF, Manuel J, Karst M, Schmidt LK, Beissner F. Flotation restricted environmental stimulation therapy for chronic pain: a randomized clinical trial. JAMA Network Open. 2021; 4(5):e219627. [DOI:10.1001/jamanetworkopen.2021.9627] [PMID] [PMCID]
- Andreae SJ, Andreae LJ, Richman JS, Cherrington AL, Safford MM. Peer-delivered cognitive behavioral therapy-based intervention reduced depression and stress in community dwelling adults with diabetes and chronic pain: a cluster randomized trial. Annals of Behavioral Medicine. 2021; 55(10):970-80. [DOI:10.1093/abm/kaab034] [PMID]
- Miller-Matero LR, Hecht LM, Miller MK, Autio K, Pester BD, Tobin ET, et al. A brief psychological intervention for chronic pain in primary care: A pilot randomized controlled trial. Pain Medicine. 2021; 22(7):1603-11. [DOI:10.1093/pm/pnaa444] [PMID]
- Taguchi K, Numata N, Takanashi R, Takemura R, Yoshida T, Kutsuzawa K, et al. Integrated cognitive behavioral therapy for chronic pain: An open-labeled prospective single-arm trial. Medicine. 2021; 100(6):e23859. [DOI:10.1097/MD.0000000000023859] [PMID] [PMCID]
- Ziadni MS, Gonzalez-Castro L, Anderson S, Krishnamurthy P, Darnall BD. Efficacy of a single-session “empowered relief” zoom-delivered group intervention for chronic pain: Randomized controlled trial conducted during the COVID-19 pandemic. Journal of Medical Internet Research. 2021; 23(9):e29672. [DOI:10.2196/29672] [PMID] [PMCID]
- Zanca JM, Gilchrist C, Ortiz CE, Dyson-Hudson TA. Pilot clinical trial of a clinical meditation and imagery intervention for chronic pain after spinal cord injury. The Journal of Spinal Cord Medicine. 2022; 45(3):339-53. [DOI:10.1080/10790268.2021.1970894] [PMID] [PMCID]
- Eaton LH, Beck SL, Jensen MP. An audio-recorded hypnosis intervention for chronic pain management in cancer survivors: A randomized controlled pilot study. International Journal of Clinical and Experimental Hypnosis. 2021; 69(4):422-40. [DOI:10.1080/00207144.2021.1951119] [PMID] [PMCID]
- Palermo TM, de la Vega R, Murray C, Law E, Zhou C. A digital health psychological intervention (WebMAP Mobile) for children and adolescents with chronic pain: Results of a hybrid effectiveness-implementation stepped-wedge cluster randomized trial. Pain. 2020; 161(12):2763-74. [PMID] [PMCID]
- Vowles KE, Witkiewitz K, Cusack KJ, Gilliam WP, Cardon KE, Bowen S, et al. Integrated behavioral treatment for veterans with co-morbid chronic pain and hazardous opioid use: A randomized controlled pilot trial. The Journal of Pain. 2020; 21(7-8):798-807. [DOI:10.1016/j.jpain.2019.11.007] [PMID] [PMCID]
- Ilgen MA, Coughlin LN, Bohnert AS, Chermack S, Price A, Kim HM, et al. Efficacy of a psychosocial pain management intervention for men and women with substance use disorders and chronic pain: A randomized clinical trial. JAMA Psychiatry. 2020; 77(12):1225-34. [DOI:10.1001/jamapsychiatry.2020.2369] [PMID] [PMCID]
- Low MY, Lacson C, Zhang F, Kesslick A, Bradt J. Vocal music therapy for chronic pain: A mixed methods feasibility study. Journal of Alternative and Complementary Medicine. 2020; 26(2):113-22. [DOI:10.1089/acm.2019.0249] [PMID] [PMCID]
- Schmid AA, Van Puymbroeck M, Fruhauf CA, Bair MJ, Portz JD. Yoga improves occupational performance, depression, and daily activities for people with chronic pain. Work. 2019; 63(2):181-9. [DOI:10.3233/WOR-192919] [PMID]
- Boersma K, Södermark M, Hesser H, Flink IK, Gerdle B, Linton SJ. Efficacy of a transdiagnostic emotion-focused exposure treatment for chronic pain patients with comorbid anxiety and depression: A randomized controlled trial. Pain. 2019; 160(8):1708-18. [DOI:10.1097/j.pain.0000000000001575] [PMID] [PMCID]
- Barry DT, Beitel M, Cutter CJ, Fiellin DA, Kerns RD, Moore BA, et al. An evaluation of the feasibility, acceptability, and preliminary efficacy of cognitive-behavioral therapy for opioid use disorder and chronic pain. Drug and Alcohol Dependence. 2019; 194:460-7. [DOI:10.1016/j.drugalcdep.2018.10.015] [PMID] [PMCID]
- Hoffman JM, Ehde DM, Dikmen S, Dillworth T, Gertz K, Kincaid C, et al. Telephone-delivered cognitive behavioral therapy for veterans with chronic pain following traumatic brain injury: Rationale and study protocol for a randomized controlled trial study. Contemporary Clinical Trials. 2019; 76:112-9. [DOI:10.1016/j.cct.2018.12.004] [PMID]
- De Jong M, Peeters F, Gard T, Ashih H, Doorley J, Walker R, et al. A randomized controlled pilot study on mindfulness-based cognitive therapy for unipolar depression in patients with chronic pain. The Journal of Clinical Psychiatry. 2017; 79(1):15m10160. [DOI:10.4088/JCP.15m10160] [PMID] [PMCID]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |