Tue, Feb 3, 2026
Volume 9 - Continuous Publishing
Iran J Neurosurg 2023, 9 - Continuous Publishing: 66-71 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mahabadi A, Askariardehjani N, Rezvani M, Shafiei M, Mahmoodkhani M. Solitary Fibrous Tumor One Year After Posterior Cervical Laminectomy. Iran J Neurosurg 2023; 9 : 9
URL: http://irjns.org/article-1-345-en.html
URL: http://irjns.org/article-1-345-en.html
1- Department of Neurosurgery, School of Medicine, Kashani Hospital, Isfahan University of Medical Sciences, Isfahan, Iran , amirmahabadi@med.mui.ac.ir
2- Department of Neurosurgery, Isfahan University of Medical Sciences, Isfahan, Iran
3- Department of Neurosurgery, School of Medicine, Kashani Hospital, Isfahan University of Medical Sciences, Isfahan, IranNeurosurgery, Isfahan University of Medical Sciences, Isfahan, Iran
2- Department of Neurosurgery, Isfahan University of Medical Sciences, Isfahan, Iran
3- Department of Neurosurgery, School of Medicine, Kashani Hospital, Isfahan University of Medical Sciences, Isfahan, IranNeurosurgery, Isfahan University of Medical Sciences, Isfahan, Iran
Keywords: Solitary fibrous tumor, Cervical
laminectomy, Soft tissue
neoplasm, Postoperative
complications, Magnetic
resonance imaging
Full Text [PDF 2071 kb]
(769 Downloads)
| Abstract (HTML) (3589 Views)
Full Text: (1168 Views)
1. Background and Importance
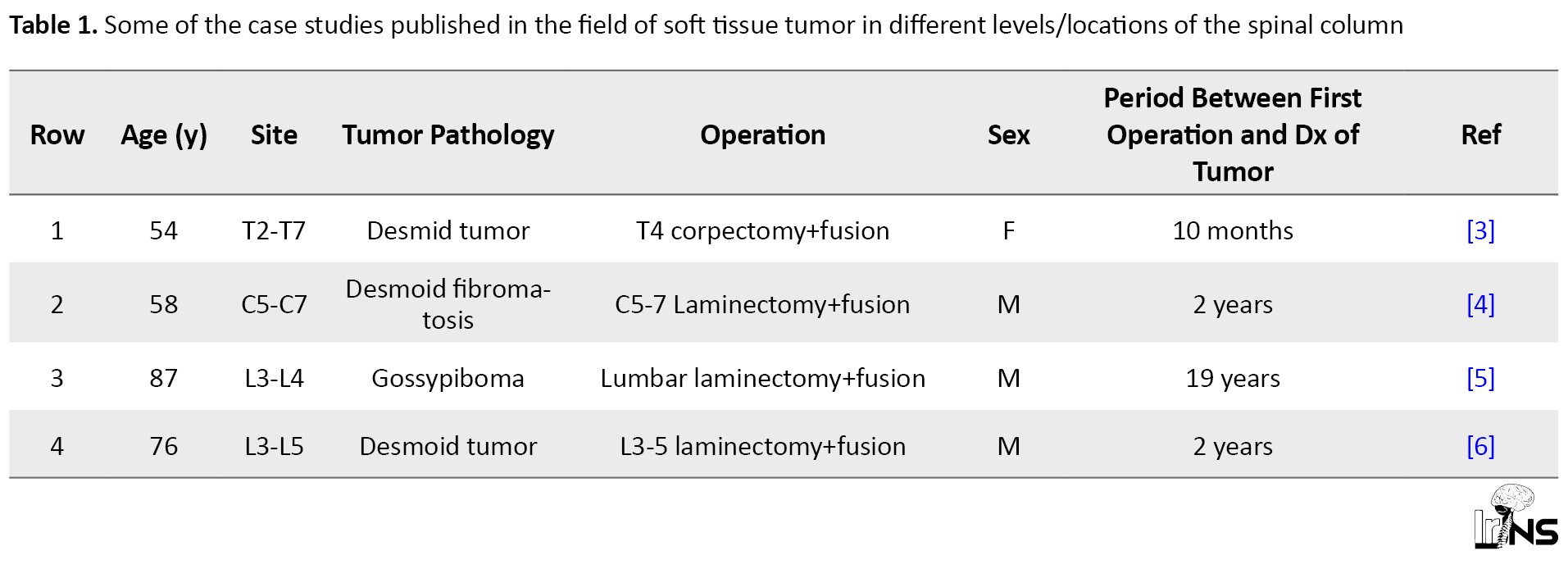
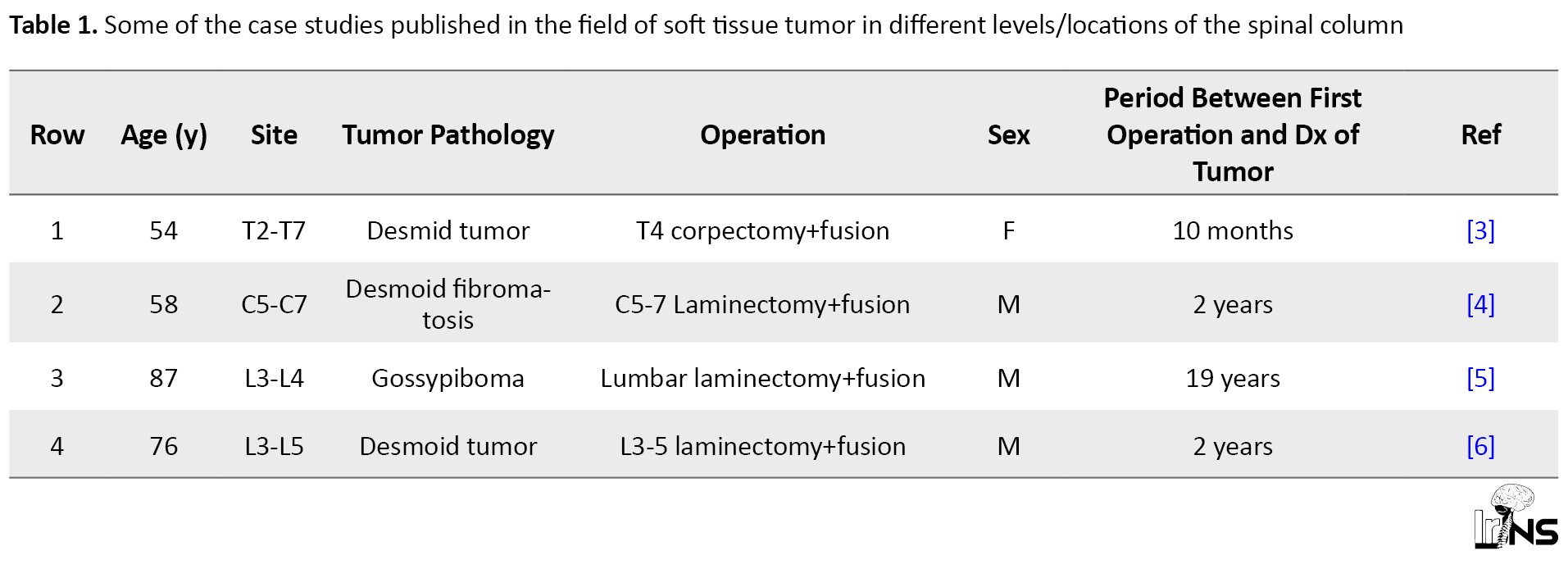
Cervical laminectomy and fixation (PCF) is one type of surgery used to treat symptomatic patients resistant to medical therapy; however, this method has serious complications that can affect patient outcomes [1]. Some of the serious complications that can occur after a posterior cervical approach include cerebrospinal fluid (CSF) leakage, surgical site infection (especially when surgery is accompanied by instrumentation), axial pain, fusion failure, graft subsidence, and epidural hematoma [2]. Although the development of a soft tissue tumor after operation is uncommon, this disorder has been reported in the literature [3, 4, 5, 6]. Table 1 lists the number of case studies published in this field.
2. Case Presentation
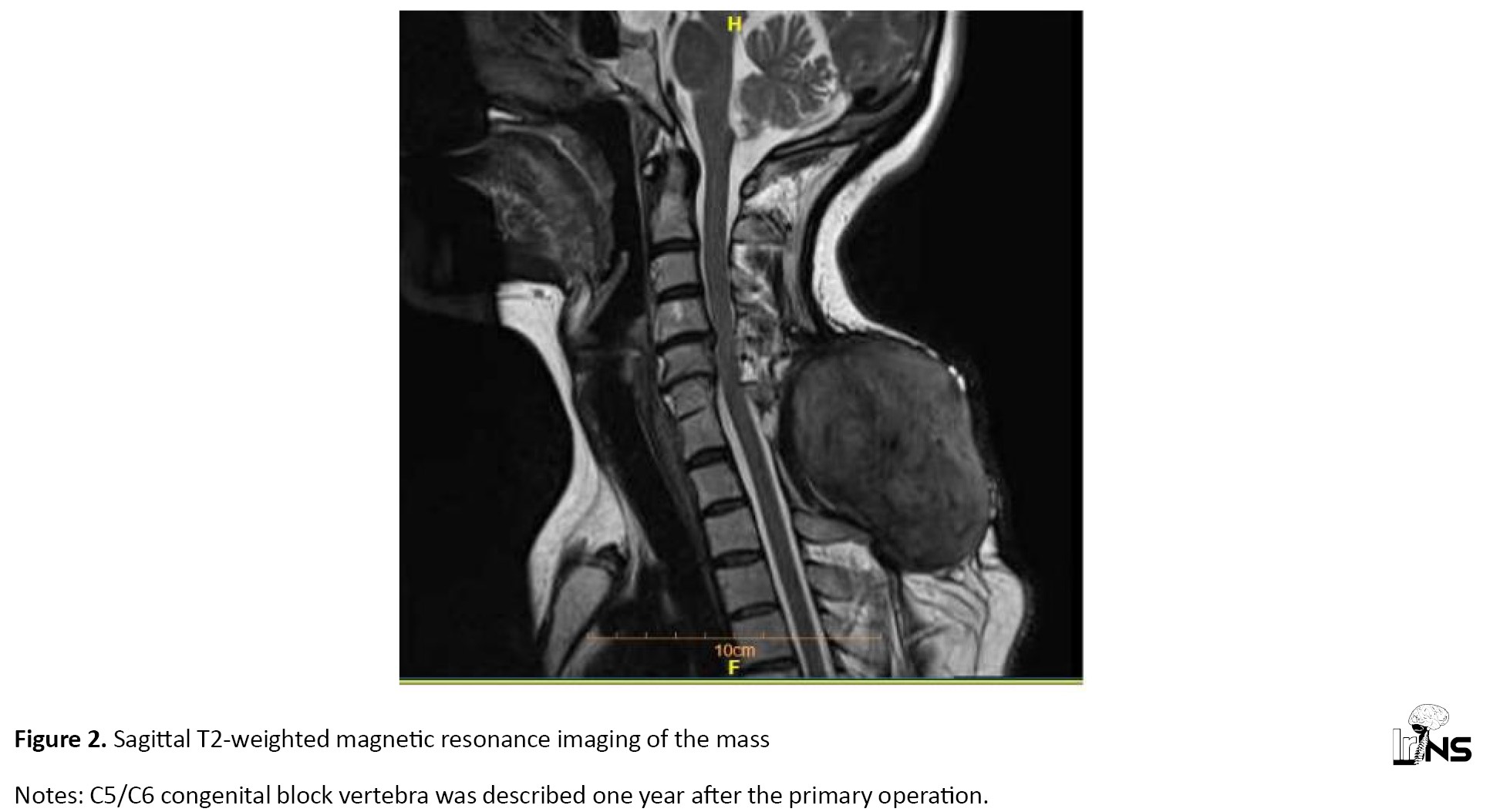
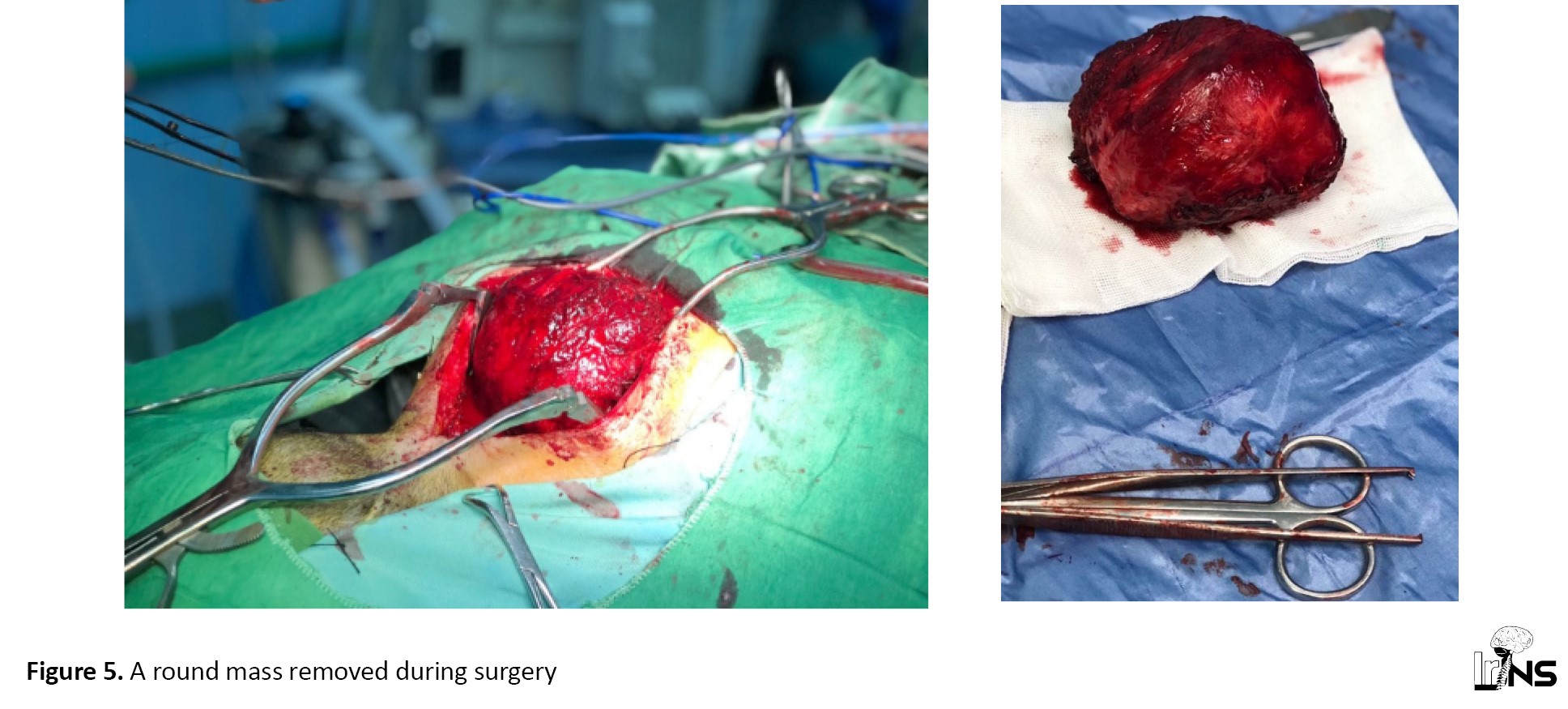
A 45-year-old woman referred to Ayatollah Kashani Hospital, Isfahan, with a major complaint of paresthesia and weakness in the upper limb 2 years ago. Cervical magnetic resonance imaging (MRI) showed spondylosis and moderate to severe cervical stenosis at C3-C6 segments (see pre-operative cervical MRI in Figure 1). Non-surgical treatment methods, such as medication, physical therapy, and cervical collars began following diagnosis. After 3 months, a follow-up examination showed no recovery. Accordingly, she was a candidate for the operation. The evaluation considered that the appropriate approach was cervical laminectomy from C3-4-5-6 without instrumentation. After general anesthesia, intubation with a GluideScope and prone position, safe laminectomy with a high-speed drill, and decompression of the spinal cord (posterior approach) were performed. The patient was discharged 3 days after the operation in good condition. Post-surgical examination and follow-up imaging demonstrated improvement in motor and sensory findings. After one year, she was referred for severe pain and swelling at the surgical site. She had no new neurological deficit. The radiological evaluation determined a large mass at the para-vertebral muscular layer. The MRI showed a large mass that was hyper-intense at T1 sequences and iso-intense at T2 sequences rather than the CSF signal (Figures 2, 3, and 4). There was no relationship between this lesion and the neural element or thecal sac. The main diagnosis that we were thinking about included organized hematoma, abscess formation, or pseudo-meningocele. Reoperation was programmed. After prone position and incision of the skin, we observed, contrary to our expectations, a large mass at the muscular layer with a thick outer layer (Figure 5). This lesion had no stickiness to the lamina or neural elements and was removed and sent to the pathology department and reviewed for detection the accurate diagnosis. Microscopic evaluation of the tumor reported fibroblastic mesenchymal cells with spindle shape cells and staghorn vascular which clearly emphasized the diagnosis of solitary fibrous tumor (the typical type). Because of further operation, we decided to extend laminectomy and fusion with a lateral mass screw. Six months later, the follow-up described no tumor recurrence.
3. Discussion
The solitary fibrous tumor was explained by Wagner for the first time at the end of the nineteenth century and further described in 1931 as a connective tissue neoplasm, such as pleura [7]. Although we might assume it is a rare soft tissue neoplasm, perhaps the developments in diagnostic modalities will change our viewpoint in the future (incidence of 0.2/100 000 annually). The solitary fibrous tumor usually accompanies mesenchymal involvement; therefore, some types of this tumor were previously called hemangiopericytoma [8]. One of the unique patterns of this tumor in histology findings was called a “patternless pattern” because of the distraction of cellular architecture [9]. Because solitary fibrous tumors originate from mesenchymal tissues, they may occur in any region, such as the pleura, abdomen, head, and neck [5]. Similar to many other tumors based on the proliferation rate (mitosis number, hypercellularity), the solitary fibrous tumor will be classified as a “typical” or “malignant” subtype [10]. One of the most important findings in the immunohistochemical evaluation of this tumor is the staining of the transducer and activator of transcription 6 (STAT6), especially in the malignant type [5]. The diagnosis is considered based on the radiologic evaluation. A computed tomography scan showed soft tissue mass with enhancement in about half of the patients. In MRI, the solitary fibrous tumor appears as a variable signal based on the location and subtypes; however, many of the solitary fibrous tumors are iso/hypo in T1 weighted images and iso/hyper in T2 [9]. The main treatment of solitary fibrous tumor is resection but for malignant types, adjuvant therapy may be considered after the operation. Usually, the average follow-up period is about 4-5 years [11]. The recurrence rate is different in the literature from about 4/110 cases (Dimico study) to 18/56 cases (Hohenforset study) [8]. Although solitary fibrous tumor is rare soft tissue cancer, secondary solitary fibrous tumor after cervical laminectomy have been reported rarely.
4. Conclusion
In this article, we aimed to provide a review of post-operative solitary fibrous tumor development after cervical laminectomy. This case report demonstrated that solitary fibrous tumor at the post-cervical segment is rare. Therefore, after cervical laminectomy, an extremely rare condition underwent tumor resection. Finally, this report states that the mesenchymal tissue injuries can be one of the risk factors for solitary fibrous tumors.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from the patient before the operation and for publishing this case report.
Funding
This article received no funding.
Authors' contributions
Conceptualization and study design: Amir Mahabadi, Majid Rezvani, Mehdi Shafiei and Mehdi Mahmoodkhani; Data collection: Navid Askariardehjani; Data analysis and interpretation: Amir Mahabadi; Drafting the article, critically revising and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The corresponding author would like to thank the Isfahan University of Medical Sciences for their support.
References
Cervical laminectomy and fixation (PCF) is one type of surgery used to treat symptomatic patients resistant to medical therapy; however, this method has serious complications that can affect patient outcomes [1]. Some of the serious complications that can occur after a posterior cervical approach include cerebrospinal fluid (CSF) leakage, surgical site infection (especially when surgery is accompanied by instrumentation), axial pain, fusion failure, graft subsidence, and epidural hematoma [2]. Although the development of a soft tissue tumor after operation is uncommon, this disorder has been reported in the literature [3, 4, 5, 6]. Table 1 lists the number of case studies published in this field.
2. Case Presentation
A 45-year-old woman referred to Ayatollah Kashani Hospital, Isfahan, with a major complaint of paresthesia and weakness in the upper limb 2 years ago. Cervical magnetic resonance imaging (MRI) showed spondylosis and moderate to severe cervical stenosis at C3-C6 segments (see pre-operative cervical MRI in Figure 1). Non-surgical treatment methods, such as medication, physical therapy, and cervical collars began following diagnosis. After 3 months, a follow-up examination showed no recovery. Accordingly, she was a candidate for the operation. The evaluation considered that the appropriate approach was cervical laminectomy from C3-4-5-6 without instrumentation. After general anesthesia, intubation with a GluideScope and prone position, safe laminectomy with a high-speed drill, and decompression of the spinal cord (posterior approach) were performed. The patient was discharged 3 days after the operation in good condition. Post-surgical examination and follow-up imaging demonstrated improvement in motor and sensory findings. After one year, she was referred for severe pain and swelling at the surgical site. She had no new neurological deficit. The radiological evaluation determined a large mass at the para-vertebral muscular layer. The MRI showed a large mass that was hyper-intense at T1 sequences and iso-intense at T2 sequences rather than the CSF signal (Figures 2, 3, and 4). There was no relationship between this lesion and the neural element or thecal sac. The main diagnosis that we were thinking about included organized hematoma, abscess formation, or pseudo-meningocele. Reoperation was programmed. After prone position and incision of the skin, we observed, contrary to our expectations, a large mass at the muscular layer with a thick outer layer (Figure 5). This lesion had no stickiness to the lamina or neural elements and was removed and sent to the pathology department and reviewed for detection the accurate diagnosis. Microscopic evaluation of the tumor reported fibroblastic mesenchymal cells with spindle shape cells and staghorn vascular which clearly emphasized the diagnosis of solitary fibrous tumor (the typical type). Because of further operation, we decided to extend laminectomy and fusion with a lateral mass screw. Six months later, the follow-up described no tumor recurrence.
3. Discussion
The solitary fibrous tumor was explained by Wagner for the first time at the end of the nineteenth century and further described in 1931 as a connective tissue neoplasm, such as pleura [7]. Although we might assume it is a rare soft tissue neoplasm, perhaps the developments in diagnostic modalities will change our viewpoint in the future (incidence of 0.2/100 000 annually). The solitary fibrous tumor usually accompanies mesenchymal involvement; therefore, some types of this tumor were previously called hemangiopericytoma [8]. One of the unique patterns of this tumor in histology findings was called a “patternless pattern” because of the distraction of cellular architecture [9]. Because solitary fibrous tumors originate from mesenchymal tissues, they may occur in any region, such as the pleura, abdomen, head, and neck [5]. Similar to many other tumors based on the proliferation rate (mitosis number, hypercellularity), the solitary fibrous tumor will be classified as a “typical” or “malignant” subtype [10]. One of the most important findings in the immunohistochemical evaluation of this tumor is the staining of the transducer and activator of transcription 6 (STAT6), especially in the malignant type [5]. The diagnosis is considered based on the radiologic evaluation. A computed tomography scan showed soft tissue mass with enhancement in about half of the patients. In MRI, the solitary fibrous tumor appears as a variable signal based on the location and subtypes; however, many of the solitary fibrous tumors are iso/hypo in T1 weighted images and iso/hyper in T2 [9]. The main treatment of solitary fibrous tumor is resection but for malignant types, adjuvant therapy may be considered after the operation. Usually, the average follow-up period is about 4-5 years [11]. The recurrence rate is different in the literature from about 4/110 cases (Dimico study) to 18/56 cases (Hohenforset study) [8]. Although solitary fibrous tumor is rare soft tissue cancer, secondary solitary fibrous tumor after cervical laminectomy have been reported rarely.
4. Conclusion
In this article, we aimed to provide a review of post-operative solitary fibrous tumor development after cervical laminectomy. This case report demonstrated that solitary fibrous tumor at the post-cervical segment is rare. Therefore, after cervical laminectomy, an extremely rare condition underwent tumor resection. Finally, this report states that the mesenchymal tissue injuries can be one of the risk factors for solitary fibrous tumors.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from the patient before the operation and for publishing this case report.
Funding
This article received no funding.
Authors' contributions
Conceptualization and study design: Amir Mahabadi, Majid Rezvani, Mehdi Shafiei and Mehdi Mahmoodkhani; Data collection: Navid Askariardehjani; Data analysis and interpretation: Amir Mahabadi; Drafting the article, critically revising and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The corresponding author would like to thank the Isfahan University of Medical Sciences for their support.
References
- Badiee RK, Mayer R, Pennicooke B, Chou D, Mummaneni PV, Tan LA. Complications following posterior cervical decompression and fusion: a review of incidence, risk factors, and prevention strategies. Journal of Spine Surgery. 2019; 6(1):323-33. [DOI:10.21037/jss.2019.11.01] [PMID] [PMCID]
- Wang T, Tian XM, Liu SK, Wang H, Zhang YZ, Ding WY. Prevalence of complications after surgery in treatment for cervical compressive myelopathy: A meta-analysis for last decade. Medicine. 2017; 96(12):e6421. [DOI:10.1097/MD.0000000000006421] [PMID] [PMCID]
- Puvanesarajah V, Lina IA, Liauw JA, Hsu W, Burger PC, Witham TF. Desmoid tumor formation following posterior spinal instrumentation placement. Evidence-Based Spine-Care Journal. 2013; 4(2): 137-42. [DOI:10.1055/s-0033-1357356] [PMID] [PMCID]
- Schlag H, Neuhoff J, Castein J, Hoffmann C, Kandziora F. Sporadic desmoid fibromatosis of the neck after dorsal spondylodesis of the cervical spine. Surgical Neurology International. 2022; 13:64. [DOI:10.25259/SNI_1240_2021] [PMID] [PMCID]
- Kobayashi T, Miyakoshi N, Abe E, Abe T, Suzuki T, Takahashi M, et al. Gossypiboma 19 years after laminectomy mimicking a malignant spinal tumour: A case report. Journal of Medical Case Reports. 2014; 8(1):311. [DOI:10.1186/1752-1947-8-311] [PMID] [PMCID]
- Yan J, Chazen JL. Postoperative lumbar fusion paraspinal desmoid tumor case report. Radiology Case Reports. 2022; 17(9):2960-2. [DOI:10.1016/j.radcr.2022.05.022] [PMID] [PMCID]
- Chick JF, Chauhan NR, Madan R. Solitary fibrous tumors of the thorax: Nomenclature, epidemiology, radiologic and pathologic findings, differential diagnoses, and management. American Journal of Roentgenology. 2013; 200(3):W238-48. [DOI:10.2214/AJR.11.8430] [PMID]
- Demicco EG, Park MS, Araujo DM, Fox PS, Bassett RL, Pollock RE, et al. Solitary fibrous tumor: A clinicopathological study of 110 cases and proposed risk assessment model. Modern Pathology. 2012; 25(9):1298-306. [DOI:10.1038/modpathol.2012.83] [PMID]
- Martin-Broto J, Mondaza-Hernandez JL, Moura DS, Hindi N. A comprehensive review on solitary fibrous tumor: New insights for new horizons. Cancers. 2021; 13(12):2913. [DOI:10.3390/cancers13122913] [PMID] [PMCID]
- Baldi, G., et al., Solitary fibrous tumor of all sites: outcome of late recurrences in 14 patients. Clin Sarcoma Res. 2013; 3: 4. doi: 10.1186. Europe PMC free article][Abstract][CrossRef][Google Scholar]. [DOI:10.1186/2045-3329-3-4] [PMID] [PMCID]
- Hohenforst-Schmidt W, Grapatsas K, Dahm M, Zarogoulidis P, Leivaditis V, Kotoulas C, et al. Solitary fibrous tumor: A center’s experience and an overview of the symptomatology, the diagnostic and therapeutic procedures of this rare tumor. Respiratory Medicine Case Reports. 2017; 21:99-104. [DOI:10.1016/j.rmcr.2017.04.007]
Type of Study: Case report |
Subject:
Spine
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |