Thu, Jan 29, 2026
Volume 11 - Continuous Publishing
Iran J Neurosurg 2025, 11 - Continuous Publishing: 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Abouie Mehrizi M A, Haghir A H, Ghanavizian M, Mojazi-Amiri M, Maleki-poor B, Mohazzab-Torabi S. Plasmacytoma-induced Pathological Axis Fracture: A Case Report and Literature Review. Iran J Neurosurg 2025; 11 : 7
URL: http://irjns.org/article-1-348-en.html
URL: http://irjns.org/article-1-348-en.html
Mohammad Ali Abouie Mehrizi1 

 , Amir Hossein Haghir1
, Amir Hossein Haghir1 

 , Mostafa Ghanavizian1
, Mostafa Ghanavizian1 

 , Milad Mojazi-Amiri2
, Milad Mojazi-Amiri2 

 , Bahador Maleki-poor3
, Bahador Maleki-poor3 

 , Saman Mohazzab-Torabi *4
, Saman Mohazzab-Torabi *4 




 , Amir Hossein Haghir1
, Amir Hossein Haghir1 

 , Mostafa Ghanavizian1
, Mostafa Ghanavizian1 

 , Milad Mojazi-Amiri2
, Milad Mojazi-Amiri2 

 , Bahador Maleki-poor3
, Bahador Maleki-poor3 

 , Saman Mohazzab-Torabi *4
, Saman Mohazzab-Torabi *4 


1- Department of Neurosurgery, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
2- Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
3- 3- Functional Neurosurgery Research Center, Shohada Tajrish Comprehensive Neurosurgical Center of Excellence, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4- Department of Neurosurgery, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran. ,smntrb@gmail.com
2- Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
3- 3- Functional Neurosurgery Research Center, Shohada Tajrish Comprehensive Neurosurgical Center of Excellence, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4- Department of Neurosurgery, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran. ,
Full Text [PDF 3280 kb]
(578 Downloads)
| Abstract (HTML) (2249 Views)
References
Full Text: (52 Views)
1. Background and Importance
Solitary bone plasmacytoma (SBP) is a rare hematological malignancy defined as the localized proliferation of neoplastic monoclonal plasma cells in the absence of multiple myeloma (MM) with <10% infiltration of plasma cells into the bone marrow [1, 2]. SBP is a malignant condition that often develops in the posterior arch of the lumbar spine, followed by the thoracic and less common cervical regions. Metastases to the cervical junction (C1 and C2) are unconventional and account for <1% of all spinal metastases [3, 4]. Their malignant nature tends to be locally aggressive and can result in pathological fractures and catastrophic chronic or acute neurological complications [5]. SBP should be misdiagnosed in pathognomonic conditions based on its radiological appearance, consisting of lytic bone lesions identical to other malignancies, such as MM, aneurysmal bone cyst, and metastasis [6-8]. The treatment of SBP is controversial and challenging and requires consideration of the patient’s comorbidities, quality of life, and overall survival. Multiple surgical approaches have been used with variable improvements.
We report the case of an unusual patient with SBP at C2 who presented with severe axial mechanical neck pain and craniocervical instability that was successfully treated with posterior decompression/stabilization followed by postoperative radiotherapy.
2. Case Presentation
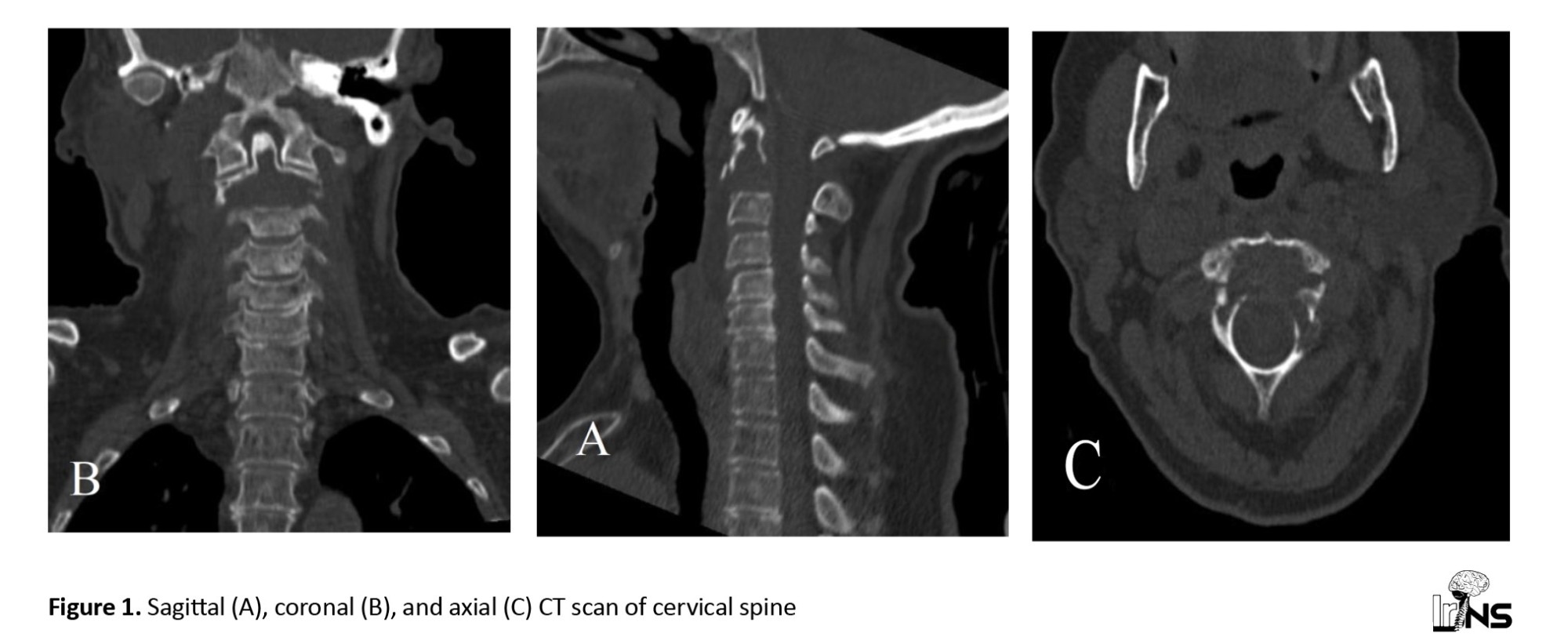
A 70-year-old woman presented with 6 months of progressive, severe axial mechanical cervical pain and “sensation” of skull instability. Primarily, she had complete concessions with intact upper and lower extremities without sensory or upper motor neuron symptoms. Computed tomography (CT) showed a lytic expansile lesion involving the body of C2 and left lamina but thinned anterior and posterior cortical borders with some disruption (Figure 1).
Solitary bone plasmacytoma (SBP) is a rare hematological malignancy defined as the localized proliferation of neoplastic monoclonal plasma cells in the absence of multiple myeloma (MM) with <10% infiltration of plasma cells into the bone marrow [1, 2]. SBP is a malignant condition that often develops in the posterior arch of the lumbar spine, followed by the thoracic and less common cervical regions. Metastases to the cervical junction (C1 and C2) are unconventional and account for <1% of all spinal metastases [3, 4]. Their malignant nature tends to be locally aggressive and can result in pathological fractures and catastrophic chronic or acute neurological complications [5]. SBP should be misdiagnosed in pathognomonic conditions based on its radiological appearance, consisting of lytic bone lesions identical to other malignancies, such as MM, aneurysmal bone cyst, and metastasis [6-8]. The treatment of SBP is controversial and challenging and requires consideration of the patient’s comorbidities, quality of life, and overall survival. Multiple surgical approaches have been used with variable improvements.
We report the case of an unusual patient with SBP at C2 who presented with severe axial mechanical neck pain and craniocervical instability that was successfully treated with posterior decompression/stabilization followed by postoperative radiotherapy.
2. Case Presentation
A 70-year-old woman presented with 6 months of progressive, severe axial mechanical cervical pain and “sensation” of skull instability. Primarily, she had complete concessions with intact upper and lower extremities without sensory or upper motor neuron symptoms. Computed tomography (CT) showed a lytic expansile lesion involving the body of C2 and left lamina but thinned anterior and posterior cortical borders with some disruption (Figure 1).
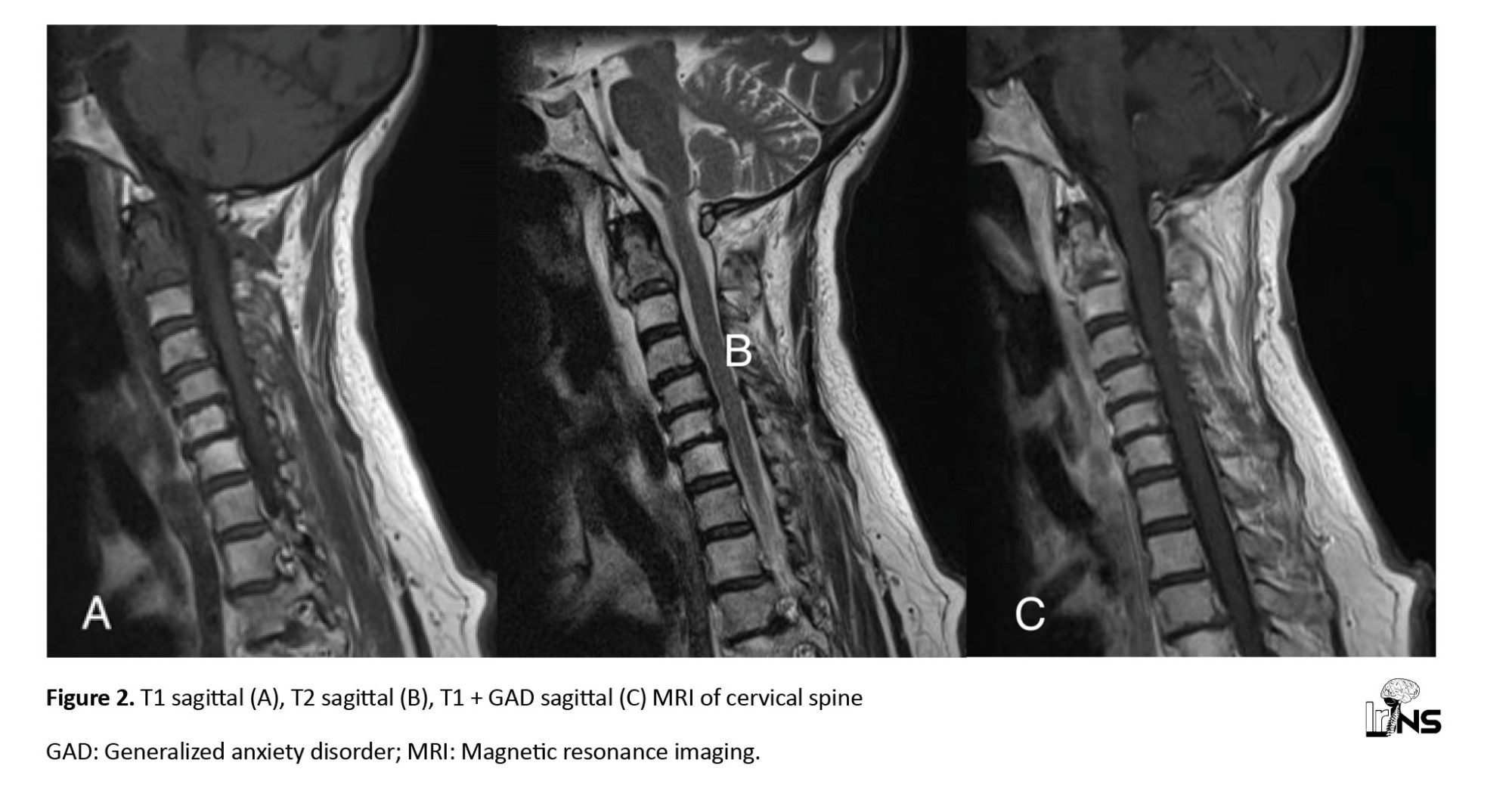
Furthermore, magnetic resonance imaging (MRI) showed hypo-signal lesions in the T1 sequence and hyper-signal in T2 with heterogenous enhancement in T1 + generalized anxiety disorder (GAD) (Figure 2).
A whole-body bone scan only showed solitary axis involvement, and no abnormalities or indications of any metastatic conditions were detected. Laboratory tests, plasma protein electrophoresis, paranoid personality disorder (PPD) test, and brucellosis markers were all normal.
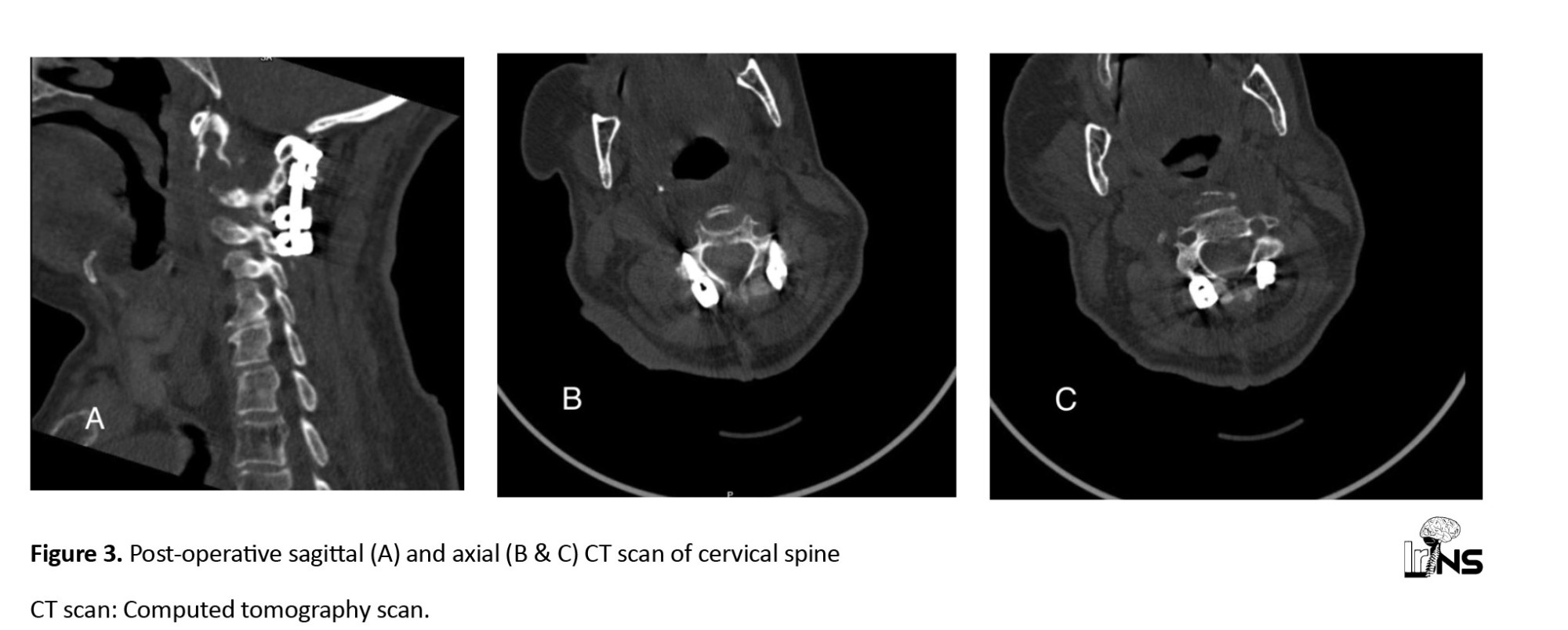
Given the symptoms, patient age, and structural instability of the craniospinal junction with the lytic C2 lesion, we decided to perform posterior cervical fusion with three main objectives: To improve the clinical symptoms, stabilize the cervical spine, and prevent devastating neurological consequences. Surgery was performed under general anesthesia and neurophysiological monitoring. The patient was premedicated with intravenous antibiotics (2 g of sodium cefazolin). The patient was placed in the prone position with an adequate cushion, and his head was fixed using a Mayfield clamp under general anesthesia. After division of the skin and posterior neck muscles, the Laminar hook on the C1 and C3-C4 lateral mass was inserted. An additional posterior transpedicular biopsy of the bone marrow was performed using the Jamshidi needle. Within 1 d postoperatively, the patient’s pain resolved without new neurological deficits, and a CT scan confirmed cervical stability (Figure 3).
Given the symptoms, patient age, and structural instability of the craniospinal junction with the lytic C2 lesion, we decided to perform posterior cervical fusion with three main objectives: To improve the clinical symptoms, stabilize the cervical spine, and prevent devastating neurological consequences. Surgery was performed under general anesthesia and neurophysiological monitoring. The patient was premedicated with intravenous antibiotics (2 g of sodium cefazolin). The patient was placed in the prone position with an adequate cushion, and his head was fixed using a Mayfield clamp under general anesthesia. After division of the skin and posterior neck muscles, the Laminar hook on the C1 and C3-C4 lateral mass was inserted. An additional posterior transpedicular biopsy of the bone marrow was performed using the Jamshidi needle. Within 1 d postoperatively, the patient’s pain resolved without new neurological deficits, and a CT scan confirmed cervical stability (Figure 3).
The patient was ambulated on the third day and discharged on the fifth postoperative day using a Miami collar.
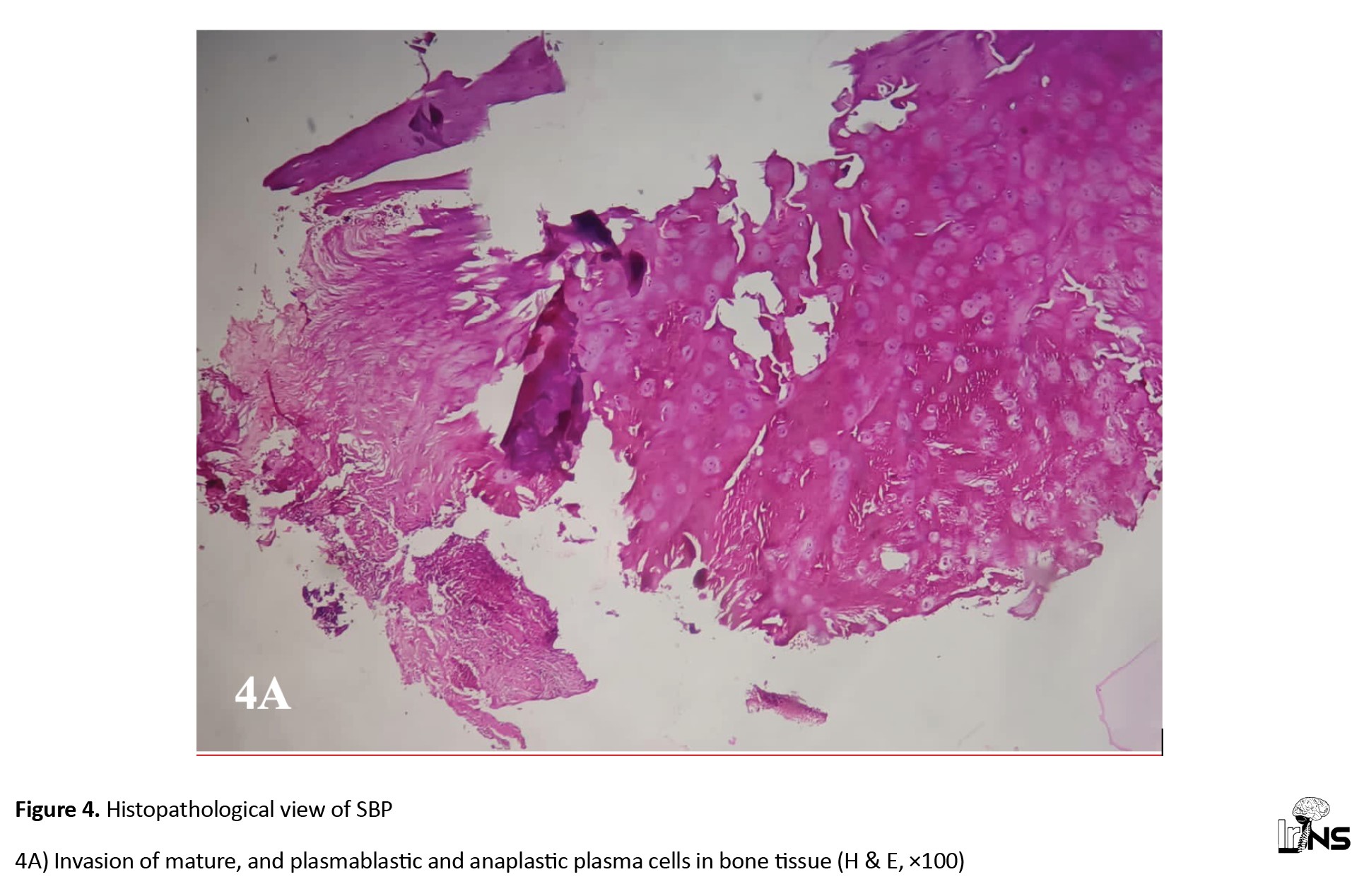
Histopathological and immunohistochemical studies of the lesion were consistent with those of the plasmacytoma. Anti-CD56, anti-CD166, anti-CXCR4, anti-Ki-67, and anti-c-MYC antibodies were used for immunohistochemical (IHC) analysis of plasmacytoma biopsies. Where staining with antibodies was observed, the following expression values were considered positive: ≥10% for CD56, ≥50% for CD166, ≥20% for CXCR4, and ≥40% for c-MYC. The level of proliferative activity was expressed as a percentage and assessed based on the expression of the Ki-67 marker in tumour cells. The diagnosis of SPB was confirmed by immunohistochemistry (IHC). Subsequently, the patient underwent radiotherapy (RT) (25 sessions [45 Gy]) with complete remission (Figure 4).
Histopathological and immunohistochemical studies of the lesion were consistent with those of the plasmacytoma. Anti-CD56, anti-CD166, anti-CXCR4, anti-Ki-67, and anti-c-MYC antibodies were used for immunohistochemical (IHC) analysis of plasmacytoma biopsies. Where staining with antibodies was observed, the following expression values were considered positive: ≥10% for CD56, ≥50% for CD166, ≥20% for CXCR4, and ≥40% for c-MYC. The level of proliferative activity was expressed as a percentage and assessed based on the expression of the Ki-67 marker in tumour cells. The diagnosis of SPB was confirmed by immunohistochemistry (IHC). Subsequently, the patient underwent radiotherapy (RT) (25 sessions [45 Gy]) with complete remission (Figure 4).
In postoperative course, conventional radiotherapy (CRT) (25 sessions: 40 Gy) was started in the fifth postoperative week. Six months later, a whole-body bone scan revealed adequate local control, no new bone lesions, and good therapeutic response. After one year of follow-up, the patient was pain-free and had a normal life. Subsequent cervical CT and whole-body scans showed stability and no evidence of recurrence.
3. Discussion
To our knowledge, cases of posterior cervical fixation for solitary plasmacytomas of the axis are rare in literature. Cervical pain in patients with metastatic lesions involving the spine can be caused by the tumor itself or by junctional instability (e.g. pathological fractures) [9]. We describe a 70-year-old woman who complained of severe chronic pain, exacerbated by range-of-motion activities, for the past 6 months.
SBP accounts for only 3% of all plasma cell neoplasms and is extremely rare (0.5%) in the craniocervical region [10]. It predominantly affects men (65%), and the mean age of patients diagnosed with SBP is 55 years [2]. Without effective preventive treatment, there is a high tendency for progression from SBP to MM.
The International Myeloma Working Group (IMWG) describes the criteria for SBP as follows: A solitary bone or soft tissue lesion, confirmed by bone biopsy showing clonal plasma cells; normal bone marrow, with no evidence of plasma cells or, at most, less than 10% involvement; no evidence of bone lesions other than the primary solitary lesion on MRI and/or CT of the spine and pelvis; and the absence of any target organ damage (e.g. hypercalcemia, renal failure, or anemia) [11].
Histological findings, including identifying monoclonal plasma cell infiltrates, are essential to establish a primary diagnosis. Our patient exhibited a lytic lesion on both MRI and CT, indicative of a malignant tumor. The CT showed expansive bone destruction, preserving the anterior and posterior borders. Patients presenting with tumor-induced pain may be good candidates for palliative therapies, such as radiation or bisphosphonate treatment, depending on the primary tumor type [12]. Our patient’s pain was mechanical and caused by craniocervical instability resulting from a pathologic fracture. After a comprehensive whole-body metastatic assessment, the primary tumor remained undiagnosed. Consequently, we opted for an invasive treatment approach as the patient was in good overall condition but symptomatic.
Moreover, the fragile outer borders of the C2 body pose a significant fracture risk, with potentially catastrophic consequences. Single-session posterior cervical fixation is rarely recommended for treating metastatic cervical instability. To our knowledge, the transpedicular approach to access the C2 body is not a safe option due to the vertebral arteries’ proximity and the axis pedicles’ small size [3]. The transoral approach provides the most straightforward access, offering the advantage of a short distance to the C2 vertebral body, thereby minimizing the risk of injury to crucial vascular structures [13, 14]. However, we decided against a second surgery with a higher risk of infection and bleeding due to the undiagnosed nature of the lesion. Therefore, posterior transpedicular biopsy via a Jamshidi needle was the optimal option for confirming the diagnosis of SBP. The posterior approach also allowed stabilization of the craniocervical junction. After careful consideration, the posterior approach was selected, and C1 laminar hooks with C3-C4 lateral mass fixation were performed along with C2 transpedicular biopsy.
Several authors have recommended injecting selective bone cement to prevent vertebral collapse [2, 3, 5, 15]. However, we considered our patient a high-risk case for cement injection due to the thinness of the vertebral borders, which could easily be disrupted, potentially leading to catastrophic neurological consequences. Cervical fixation significantly improves the patient’s quality of life. Our patient experienced a reduction in cervical pain 7 days after surgery and was able to ambulate without a soft neck collar.
Radiation therapy is the first-line treatment for SBP in several patients. However, in cases of spinal compression, neurological symptoms, or severe instability, radiation therapy should be combined with spinal stabilization. Additionally, radiation therapy during surgery helps eliminate most tumor cells and delays local recurrence, with better outcomes in managing tumor-related pain.
One of the main limitations in discussing plasmacytoma and C2 pathological fractures is the scarcity of comprehensive studies and research specifically focusing on this topic. Most available literature consists of case reports and small case series, limiting the findings’ generalizability. Due to the rarity of plasmacytoma and C2 pathological fractures, studies often have small sample sizes, making it challenging to draw definitive conclusions. Large-scale studies involving diverse populations are required to obtain a more accurate understanding of this condition. Most of the available literature is retrospective and relies on medical records and historical data. Prospective studies that follow patients over time provide more robust evidence and allow for a better characterization of disease progression and treatment outcomes. Plasmacytoma and C2 pathological fractures can manifest in various ways, leading to differences in clinical presentation, radiographic findings, and treatment approaches. The lack of standardized diagnostic criteria and treatment protocols contributes to the heterogeneity of reported cases, making it challenging to compare and synthesize available evidence. Many studies have limited follow-up periods, often ranging from months to years.
4. Conclusion
Finally, SBP involving the C2 cervical vertebral body is very rare; however, posterior cervical fixation combined with neoadjuvant radiotherapy may constitute a safe and effective treatment to stabilize SBP, compromising the stability of C2, improving mechanical pain, and improving quality of life. Lytic lesions affecting the vertebral body, especially in the upper cervical region, must be considered when making a differential diagnosis and precise surgical approach.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from the patient to publish this case report and any accompanying images. The patient were fully informed about the nature of the report and the potential for her medical information to be shared in scientific literature, with all efforts made to maintain confidentiality and privacy. The patient signed the consent before submitting or publishing case details.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conception and design: Saman Mohazzab-Torabi, Mohammad Ali Abouie Mehrizi; Data collection: Saman Mohazzab-Torabi, Mostafa Ghanavizian, Milad Mojazi-Amiri; Data analysis and interpretation: Saman Mohazzab-Torabi, Milad Mojazi-Amiri; Drafting the article: Saman Mohazzab-Torabi, Amir Hossein Haghir; Critically revising the article: Amir Hossein Haghir, Mohammad Ali Abouie Mehrizi, Bahador Maleki-poor; Reviewing the submitted version of the manuscript: Saman Mohazzab-Torabi, Amir Hossein Haghir; Final approval: All Authors.
Conflict of interest
The authors declared no conflict of interest.
3. Discussion
To our knowledge, cases of posterior cervical fixation for solitary plasmacytomas of the axis are rare in literature. Cervical pain in patients with metastatic lesions involving the spine can be caused by the tumor itself or by junctional instability (e.g. pathological fractures) [9]. We describe a 70-year-old woman who complained of severe chronic pain, exacerbated by range-of-motion activities, for the past 6 months.
SBP accounts for only 3% of all plasma cell neoplasms and is extremely rare (0.5%) in the craniocervical region [10]. It predominantly affects men (65%), and the mean age of patients diagnosed with SBP is 55 years [2]. Without effective preventive treatment, there is a high tendency for progression from SBP to MM.
The International Myeloma Working Group (IMWG) describes the criteria for SBP as follows: A solitary bone or soft tissue lesion, confirmed by bone biopsy showing clonal plasma cells; normal bone marrow, with no evidence of plasma cells or, at most, less than 10% involvement; no evidence of bone lesions other than the primary solitary lesion on MRI and/or CT of the spine and pelvis; and the absence of any target organ damage (e.g. hypercalcemia, renal failure, or anemia) [11].
Histological findings, including identifying monoclonal plasma cell infiltrates, are essential to establish a primary diagnosis. Our patient exhibited a lytic lesion on both MRI and CT, indicative of a malignant tumor. The CT showed expansive bone destruction, preserving the anterior and posterior borders. Patients presenting with tumor-induced pain may be good candidates for palliative therapies, such as radiation or bisphosphonate treatment, depending on the primary tumor type [12]. Our patient’s pain was mechanical and caused by craniocervical instability resulting from a pathologic fracture. After a comprehensive whole-body metastatic assessment, the primary tumor remained undiagnosed. Consequently, we opted for an invasive treatment approach as the patient was in good overall condition but symptomatic.
Moreover, the fragile outer borders of the C2 body pose a significant fracture risk, with potentially catastrophic consequences. Single-session posterior cervical fixation is rarely recommended for treating metastatic cervical instability. To our knowledge, the transpedicular approach to access the C2 body is not a safe option due to the vertebral arteries’ proximity and the axis pedicles’ small size [3]. The transoral approach provides the most straightforward access, offering the advantage of a short distance to the C2 vertebral body, thereby minimizing the risk of injury to crucial vascular structures [13, 14]. However, we decided against a second surgery with a higher risk of infection and bleeding due to the undiagnosed nature of the lesion. Therefore, posterior transpedicular biopsy via a Jamshidi needle was the optimal option for confirming the diagnosis of SBP. The posterior approach also allowed stabilization of the craniocervical junction. After careful consideration, the posterior approach was selected, and C1 laminar hooks with C3-C4 lateral mass fixation were performed along with C2 transpedicular biopsy.
Several authors have recommended injecting selective bone cement to prevent vertebral collapse [2, 3, 5, 15]. However, we considered our patient a high-risk case for cement injection due to the thinness of the vertebral borders, which could easily be disrupted, potentially leading to catastrophic neurological consequences. Cervical fixation significantly improves the patient’s quality of life. Our patient experienced a reduction in cervical pain 7 days after surgery and was able to ambulate without a soft neck collar.
Radiation therapy is the first-line treatment for SBP in several patients. However, in cases of spinal compression, neurological symptoms, or severe instability, radiation therapy should be combined with spinal stabilization. Additionally, radiation therapy during surgery helps eliminate most tumor cells and delays local recurrence, with better outcomes in managing tumor-related pain.
One of the main limitations in discussing plasmacytoma and C2 pathological fractures is the scarcity of comprehensive studies and research specifically focusing on this topic. Most available literature consists of case reports and small case series, limiting the findings’ generalizability. Due to the rarity of plasmacytoma and C2 pathological fractures, studies often have small sample sizes, making it challenging to draw definitive conclusions. Large-scale studies involving diverse populations are required to obtain a more accurate understanding of this condition. Most of the available literature is retrospective and relies on medical records and historical data. Prospective studies that follow patients over time provide more robust evidence and allow for a better characterization of disease progression and treatment outcomes. Plasmacytoma and C2 pathological fractures can manifest in various ways, leading to differences in clinical presentation, radiographic findings, and treatment approaches. The lack of standardized diagnostic criteria and treatment protocols contributes to the heterogeneity of reported cases, making it challenging to compare and synthesize available evidence. Many studies have limited follow-up periods, often ranging from months to years.
4. Conclusion
Finally, SBP involving the C2 cervical vertebral body is very rare; however, posterior cervical fixation combined with neoadjuvant radiotherapy may constitute a safe and effective treatment to stabilize SBP, compromising the stability of C2, improving mechanical pain, and improving quality of life. Lytic lesions affecting the vertebral body, especially in the upper cervical region, must be considered when making a differential diagnosis and precise surgical approach.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from the patient to publish this case report and any accompanying images. The patient were fully informed about the nature of the report and the potential for her medical information to be shared in scientific literature, with all efforts made to maintain confidentiality and privacy. The patient signed the consent before submitting or publishing case details.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conception and design: Saman Mohazzab-Torabi, Mohammad Ali Abouie Mehrizi; Data collection: Saman Mohazzab-Torabi, Mostafa Ghanavizian, Milad Mojazi-Amiri; Data analysis and interpretation: Saman Mohazzab-Torabi, Milad Mojazi-Amiri; Drafting the article: Saman Mohazzab-Torabi, Amir Hossein Haghir; Critically revising the article: Amir Hossein Haghir, Mohammad Ali Abouie Mehrizi, Bahador Maleki-poor; Reviewing the submitted version of the manuscript: Saman Mohazzab-Torabi, Amir Hossein Haghir; Final approval: All Authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Caers J, Paiva B, Zamagni E, Leleu X, Bladé J, Kristinsson SY, et al. Diagnosis, treatment, and response assessment in solitary plasmacytoma: updated recommendations from a European Expert Panel. Journal of hematology & oncology. 2018; 11(1):10. [DOI:10.1186/s13045-017-0549-1] [PMID]
- Pham A, Mahindra A. Solitary plasmacytoma: A review of diagnosis and management. Current Hematologic Malignancy Reports. 2019; 14(2):63-9. [DOI:10.1007/s11899-019-00499-8] [PMID]
- Quigley KJ, Cortese CM, Place HM. Cervical degenerative cyst located within the body of C2: a case report and review of the literature. Spine. 2006; 31(8):E237-40. [DOI:10.1097/01.brs.0000210251.56703.d4] [PMID]
- Yoon JY, Kim TK, Kim KH. Anterolateral percutaneous vertebroplasty at C2 for lung cancer metastasis and upper cervical facet joint block. The Clinical Journal of Pain. 2008; 24(7):641-6. [DOI:10.1097/AJP.0b013e31816c6630] [PMID]
- Wu X, Tan M, Qi Y, Yi P, Yang F, Tang X, et al. Posterior decompression and occipitocervical fixation followed by intraoperative vertebroplasty for metastatic involvement of the axis. BMC Musculoskeletal Disorders. 2018; 19(1):11. [DOI:10.1186/s12891-018-1928-7] [PMID]
- Fay LY, Wu JC, Huang WC, Shih YH, Cheng H. One-stage posterior resection is feasible for a holovertebral aneurysmal bone cyst of the axis: a case report and literature review. Surgical Neurology. 2009; 72(S 2):S80-5. [DOI:10.1016/j.wneu.2009.09.007] [PMID]
- Zwolak P, Kröber M. Acute neck pain caused by atlanto-axial instability secondary to pathologic fracture involving odontoid process and C2 vertebral body: treatment with radiofrequency thermoablation, cement augmentation and odontoid screw fixation. Archives of Orthopaedic and Trauma Surgery. 2015; 135(9):1211-5. [DOI:10.1007/s00402-015-2266-y] [PMID]
- Papp Z, Marosfői M, Szikora I, Banczerowski P. Treatment of C-2 metastatic tumors with intraoperative transoral or transpedicular vertebroplasty and occipitocervical posterior fixation. Journal of neurosurgery. Spine. 2014; 21(6):886-91. [DOI:10.3171/2014.8.SPINE13932] [PMID]
- Dores GM, Landgren O, McGlynn KA, Curtis RE, Linet MS, Devesa SS. Plasmacytoma of bone, extramedullary plasmacytoma, and multiple myeloma: incidence and survival in the United States, 1992-2004. British journal of haematology. 2009; 144(1):86-94. [DOI:10.1111/j.1365-2141.2008.07421.x] [PMID]
- Ahmadi SA, Slotty PJ, Munoz-Bendix C, Steiger HJ, Cornelius JF. Early surgical occipitocervical stabilization for plasma cell neoplasms at the craniocervical junction: Systematic review and proposal of a treatment algorithm. The Spine journal. 2016; 16(1):91-104. [DOI:10.1016/j.spinee.2015.09.032] [PMID]
- Dimopoulos M, Terpos E, Comenzo RL, Tosi P, Beksac M, Sezer O, et al. International myeloma working group consensus statement and guidelines regarding the current role of imaging techniques in the diagnosis and monitoring of multiple Myeloma. Leukemia. 2009; 23(9):1545-56. [DOI:10.1038/leu.2009.89] [PMID]
- Floeth FW, Herdmann J, Rhee S, Turowski B, Krajewski K, Steiger HJ, et al. Open microsurgical tumor excavation and vertebroplasty for metastatic destruction of the second cervical vertebra-outcome in seven cases. The spine journal. 2014; 14(12):3030-7. [DOI:10.1016/j.spinee.2014.09.018] [PMID]
- Brage L, Roldán H, Plata-Bello J, Martel D, García-Marín V. Transoral vertebroplasty for a C2 aneurysmal bone cyst. The spine journal. 2016; 16(7):e473-7. [DOI:10.1016/j.spinee.2016.02.042] [PMID]
- Monterumici DA, Narne S, Nena U, Sinigaglia R. Transoral kyphoplasty for tumors in C2. The spine journal. 2007; 7(6):666-70. [DOI:10.1016/j.spinee.2006.08.007] [PMID]
- Sachs DC, Inamasu J, Mendel EE, Guiot BH. Transoral vertebroplasty for renal cell metastasis involving the axis: case report. Spine. 2006; 31(24):E925-8. [DOI:10.1097/01.brs.0000245923.66285.71] [PMID]
Type of Study: Case report |
Subject:
Spine
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |