Thu, May 2, 2024
Volume 9 - Continuous Publishing
Iran J Neurosurg 2023, 9 - Continuous Publishing: 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Goswami P, S. Chandran R, Mohammed Haneefa S, Sathyababu A, Bhanu Prabhakar R. Clinical and Radiological Changes at the Adjacent Segments Following Cervical Spine Surgery: A Retrospective Study. Iran J Neurosurg 2023; 9 : 12
URL: http://irjns.org/article-1-349-en.html
URL: http://irjns.org/article-1-349-en.html
Prakash Goswami1 

 , Raj S. Chandran *
, Raj S. Chandran * 

 2, Sharmad Mohammed Haneefa1
2, Sharmad Mohammed Haneefa1 

 , Arun Sathyababu1
, Arun Sathyababu1 

 , Rajmohan Bhanu Prabhakar1
, Rajmohan Bhanu Prabhakar1 




 , Raj S. Chandran *
, Raj S. Chandran * 

 2, Sharmad Mohammed Haneefa1
2, Sharmad Mohammed Haneefa1 

 , Arun Sathyababu1
, Arun Sathyababu1 

 , Rajmohan Bhanu Prabhakar1
, Rajmohan Bhanu Prabhakar1 


1- Department of Neurosurgery, Government Medical College, Thiruvananthapuram, Kerala, India
2- Department of Neurosurgery, Government Medical College, Thiruvananthapuram, Kerala, India , rajschandran@gmail.com
2- Department of Neurosurgery, Government Medical College, Thiruvananthapuram, Kerala, India , rajschandran@gmail.com
Full Text [PDF 2457 kb]
(229 Downloads)
| Abstract (HTML) (926 Views)
Full Text: (197 Views)
1. Introduction
Various cervical spine surgeries via both anterior and posterior approaches, such as anterior cervical discectomy or corpectomy and fixation with plates and screws, fusion with a graft taken from the iliac crest or other osteogenesis-enhancing materials, and posterior fixation using lateral mass screws have been performed for different pathologies of the cervical spine at our institution and in the centers across the globe. Pathological changes can occur at the adjacent motion segments cranially or caudally, which can be demonstrated radiologically and may manifest clinically with symptoms of myelopathy, radiculopathy, or mechanical pain, defined as adjacent segment disease (ASD). This occurs in a minority of patients with X-ray/computerized tomography (CT)/MRI evidence of adjacent segment degeneration.
In approximately 25% to 45% of patients, these changes are demonstrated on follow-up radiological evaluation, usually at levels above or below the fused segment [1-10] reported as high as 60% to 90% in certain studies [11-16]. But all of them may not present with symptoms, the incidence reported in the literature ranges from 6% to 26% on long-term follow-up [3, 4, 12, 16-18].
Common surgical interventions at our institution are anterior cervical discectomy and fusion (ACDF), anterior cervical corpectomy and fusion, circumferential fusion, and posterior-lateral mass fixation.
2. Methods and Materials/Patients
The primary objective of the study was to evaluate the proportion of the patients’ developing changes at adjacent segments following cervical spine fusion surgery 2-5 years ago in the Department of Neurosurgery.
The secondary objectives were to study the extent, pattern, and severity of these degenerative changes radiologically and to determine the sites and patterns of adjacent segment disease (ASD).
A descriptive study was conducted in the Department of Neurosurgery, Government Medical College, Trivandrum, India on patients in the age group 18-80 years who had undergone a previous cervical arthrodesis procedure (ACDF/corpectomy/posterior fixation/circumferential fusion) in the last 2-5 years and continued follow-up in neurosurgery.
Inclusion criteria included all cases in the age group 18-80 years, who underwent cervical spine fusion/fixation surgery 2-5 years ago in the Department of Neurosurgery, patients who underwent X-ray, CT, or MRI of index surgery, and patients who were willing to investigate the current status of the cervical spine after the index surgery. Dead patients and those who were unwilling to participate in the study or had a malignancy were excluded from the study.
The sample size was estimated using the following formula:
Sample Size = {Z2*(p)*(q)}/Δ2
Substituting the values-where Z value for the confidence level chosen = 1.96 (for 95% confidence level from the standard normal distribution); P= 4.8% = 0 [3];
P= prevalence
q= 1-P = 1-0.048 = 0.952
Δ= acceptable margin of error = 0.05,
All patients who had the inclusion criteria were included in the study. Those who underwent surgery for at least 2-5 years are being followed up at the Department of Neurosurgery. Clinical assessment included examining neck pain at rest position or during movements and/or radicular pain in the upper limbs with sensory or motor deficits. The radiological examination included an X-ray cervical spine anteroposterior (AP) and lateral views of the patient with the neck in neutral, flexion, and extension position. A comparison of these X-rays with those taken before surgery, mainly sagittal X-rays was done to assess the displacement of the vertebral body. The postero-inferior and postero-superior angles of the vertebral body and the distance between the two points were noted, related to the sagittal diameter of the sub-adjacent vertebra, using the formula: x=sagittal displacement (mm) x 100/sagittal diameter (mm). This is graded into four based on the percentage of displacement and independent of any magnification grade I (0-25%), II (25-50%), III (50-75%), and IV (75-100%). The height of an adjacent disc was normal if it was equal to the height of the disc located at a higher or lower level, on the condition that no evidence of degeneration was found. The next level was chosen to compare disc height in case of degeneration. Disc height decrease was graded as mild, moderate, and severe degeneration depending on the percentage of loss of disc height; mild (75%–100%), moderate (50%-75%), and severe (< 50%) of the normal disc height. The term “symptomatic ASD” was given when evidence of new radicular or myelopathic symptoms referable to an adjacent degenerated level on two consecutive visits was found. The management of symptomatic adjacent level is the same as any other cervical spine disease; conservative management with cervical orthosis, and analgesics done initially. Evaluation with MRI, CT, and dynamic X-rays was performed in the event of non-resolution of radiculopathy or new onset myelopathy, to rule out any compressive lesion. Based on the radiological findings, degenerative changes at the adjacent levels are grouped into four grades (Table 1).

3. Results
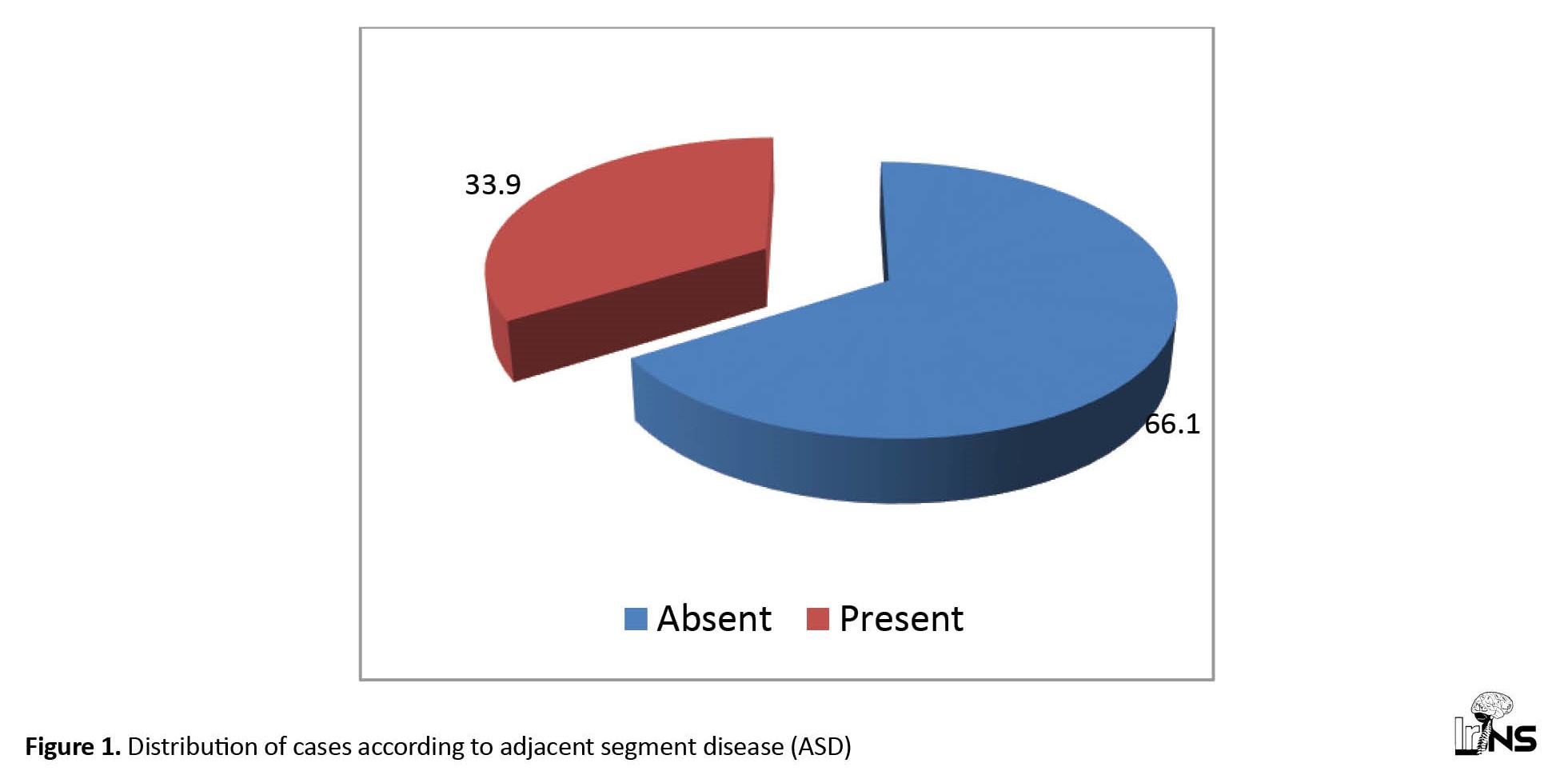
Fifty-nine patients who qualified for the inclusion criteria for the study were analyzed. The mean age group of the sample was 45.7±11.9 years. Forty-five cases (76.3%) were men and 14 cases (23.7%) were women. Sixteen patients (27.1%) were smokers and 43 (72.9%) were non-smokers. Diabetes was seen in 33% of the population.Forty-two cases (71.2%) had degenerative disease suggestive of the most common pathology behind cervical spine cases presenting at our Institution. Sixteen (27.1%) cases were trauma-related and 1 case was infectious (1.7%). The adjacent level disease was observed in 33.9% of cases and absent in 66.1% of cases (Figure 1).
Various cervical spine surgeries via both anterior and posterior approaches, such as anterior cervical discectomy or corpectomy and fixation with plates and screws, fusion with a graft taken from the iliac crest or other osteogenesis-enhancing materials, and posterior fixation using lateral mass screws have been performed for different pathologies of the cervical spine at our institution and in the centers across the globe. Pathological changes can occur at the adjacent motion segments cranially or caudally, which can be demonstrated radiologically and may manifest clinically with symptoms of myelopathy, radiculopathy, or mechanical pain, defined as adjacent segment disease (ASD). This occurs in a minority of patients with X-ray/computerized tomography (CT)/MRI evidence of adjacent segment degeneration.
In approximately 25% to 45% of patients, these changes are demonstrated on follow-up radiological evaluation, usually at levels above or below the fused segment [1-10] reported as high as 60% to 90% in certain studies [11-16]. But all of them may not present with symptoms, the incidence reported in the literature ranges from 6% to 26% on long-term follow-up [3, 4, 12, 16-18].
Common surgical interventions at our institution are anterior cervical discectomy and fusion (ACDF), anterior cervical corpectomy and fusion, circumferential fusion, and posterior-lateral mass fixation.
2. Methods and Materials/Patients
The primary objective of the study was to evaluate the proportion of the patients’ developing changes at adjacent segments following cervical spine fusion surgery 2-5 years ago in the Department of Neurosurgery.
The secondary objectives were to study the extent, pattern, and severity of these degenerative changes radiologically and to determine the sites and patterns of adjacent segment disease (ASD).
A descriptive study was conducted in the Department of Neurosurgery, Government Medical College, Trivandrum, India on patients in the age group 18-80 years who had undergone a previous cervical arthrodesis procedure (ACDF/corpectomy/posterior fixation/circumferential fusion) in the last 2-5 years and continued follow-up in neurosurgery.
Inclusion criteria included all cases in the age group 18-80 years, who underwent cervical spine fusion/fixation surgery 2-5 years ago in the Department of Neurosurgery, patients who underwent X-ray, CT, or MRI of index surgery, and patients who were willing to investigate the current status of the cervical spine after the index surgery. Dead patients and those who were unwilling to participate in the study or had a malignancy were excluded from the study.
The sample size was estimated using the following formula:
Sample Size = {Z2*(p)*(q)}/Δ2
Substituting the values-where Z value for the confidence level chosen = 1.96 (for 95% confidence level from the standard normal distribution); P= 4.8% = 0 [3];
P= prevalence
q= 1-P = 1-0.048 = 0.952
Δ= acceptable margin of error = 0.05,
All patients who had the inclusion criteria were included in the study. Those who underwent surgery for at least 2-5 years are being followed up at the Department of Neurosurgery. Clinical assessment included examining neck pain at rest position or during movements and/or radicular pain in the upper limbs with sensory or motor deficits. The radiological examination included an X-ray cervical spine anteroposterior (AP) and lateral views of the patient with the neck in neutral, flexion, and extension position. A comparison of these X-rays with those taken before surgery, mainly sagittal X-rays was done to assess the displacement of the vertebral body. The postero-inferior and postero-superior angles of the vertebral body and the distance between the two points were noted, related to the sagittal diameter of the sub-adjacent vertebra, using the formula: x=sagittal displacement (mm) x 100/sagittal diameter (mm). This is graded into four based on the percentage of displacement and independent of any magnification grade I (0-25%), II (25-50%), III (50-75%), and IV (75-100%). The height of an adjacent disc was normal if it was equal to the height of the disc located at a higher or lower level, on the condition that no evidence of degeneration was found. The next level was chosen to compare disc height in case of degeneration. Disc height decrease was graded as mild, moderate, and severe degeneration depending on the percentage of loss of disc height; mild (75%–100%), moderate (50%-75%), and severe (< 50%) of the normal disc height. The term “symptomatic ASD” was given when evidence of new radicular or myelopathic symptoms referable to an adjacent degenerated level on two consecutive visits was found. The management of symptomatic adjacent level is the same as any other cervical spine disease; conservative management with cervical orthosis, and analgesics done initially. Evaluation with MRI, CT, and dynamic X-rays was performed in the event of non-resolution of radiculopathy or new onset myelopathy, to rule out any compressive lesion. Based on the radiological findings, degenerative changes at the adjacent levels are grouped into four grades (Table 1).

3. Results
Fifty-nine patients who qualified for the inclusion criteria for the study were analyzed. The mean age group of the sample was 45.7±11.9 years. Forty-five cases (76.3%) were men and 14 cases (23.7%) were women. Sixteen patients (27.1%) were smokers and 43 (72.9%) were non-smokers. Diabetes was seen in 33% of the population.Forty-two cases (71.2%) had degenerative disease suggestive of the most common pathology behind cervical spine cases presenting at our Institution. Sixteen (27.1%) cases were trauma-related and 1 case was infectious (1.7%). The adjacent level disease was observed in 33.9% of cases and absent in 66.1% of cases (Figure 1).
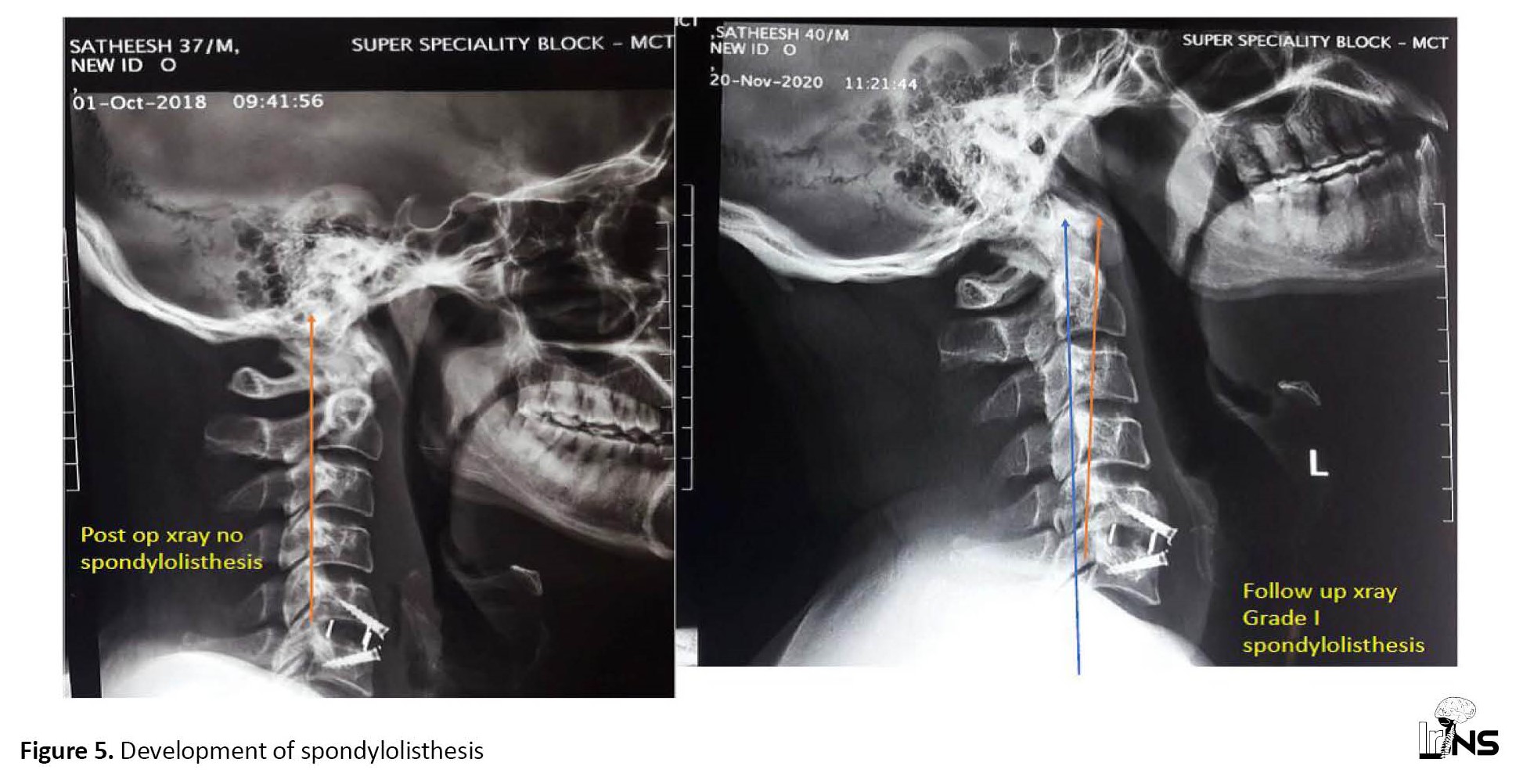
The most common level operated at index surgery was C5-C6 with 23 patients (39%), the second most common level was C6-C7 with 10 patients (16.9%), and C4-C5 with 10 patients (16.9%). Among all cervical spine surgeries done, ACDF was the most common one, performed on 39 cases (66%), anterior cervical corpectomy and cage fixation was performed in 14 patients (23.7%), circumferential fusion was performed in 5 patients (8.5%), and laminectomy and lateral mass fixation performed in 1 case (1.7%). Single-level spine fixation was commonly performed with sample size (54.2%, n=32) then two levels (42.4%, n=25) and three levels (3.4%, n=2). Adjacent segment degeneration was present in the spine fixation level subgroup at a single level of 9 cases (28.12%), two levels of 9 cases (36%), and three-level fixation of 2 cases (100%) (Table 2).

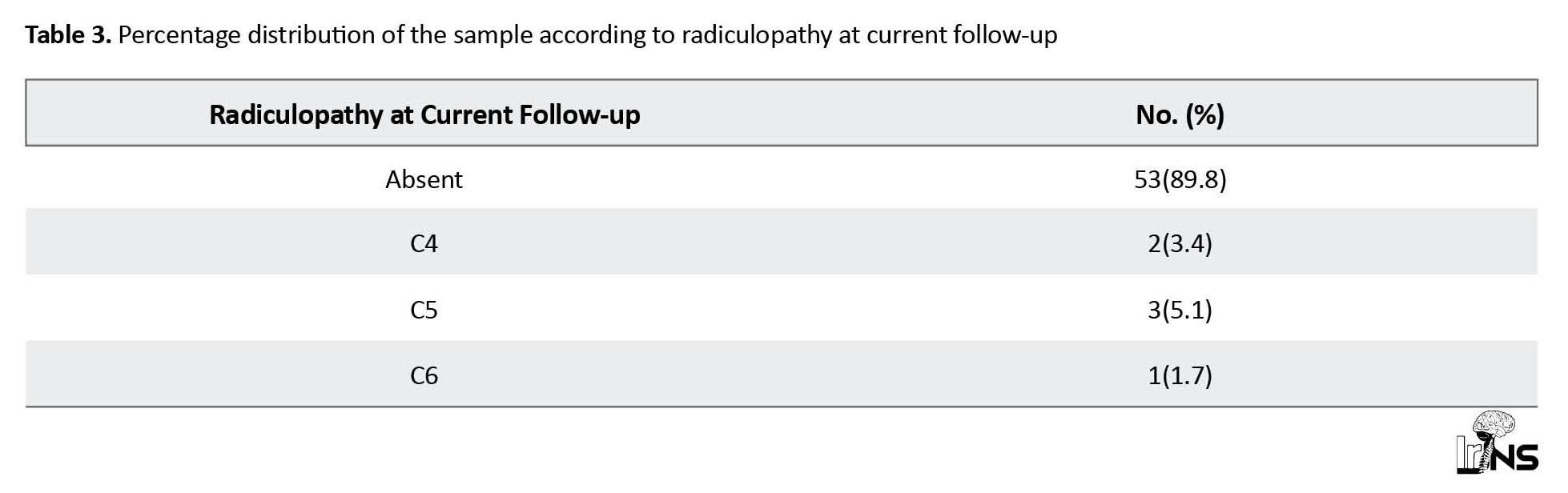
Six (10.2%) out of 59 patients developed radiculopathy due to adjacent segment changes and were considered as clinical adjacent segment pathology/ASD, which would be 10.2%. Most patients developed C5 radiculopathy (Table 3).
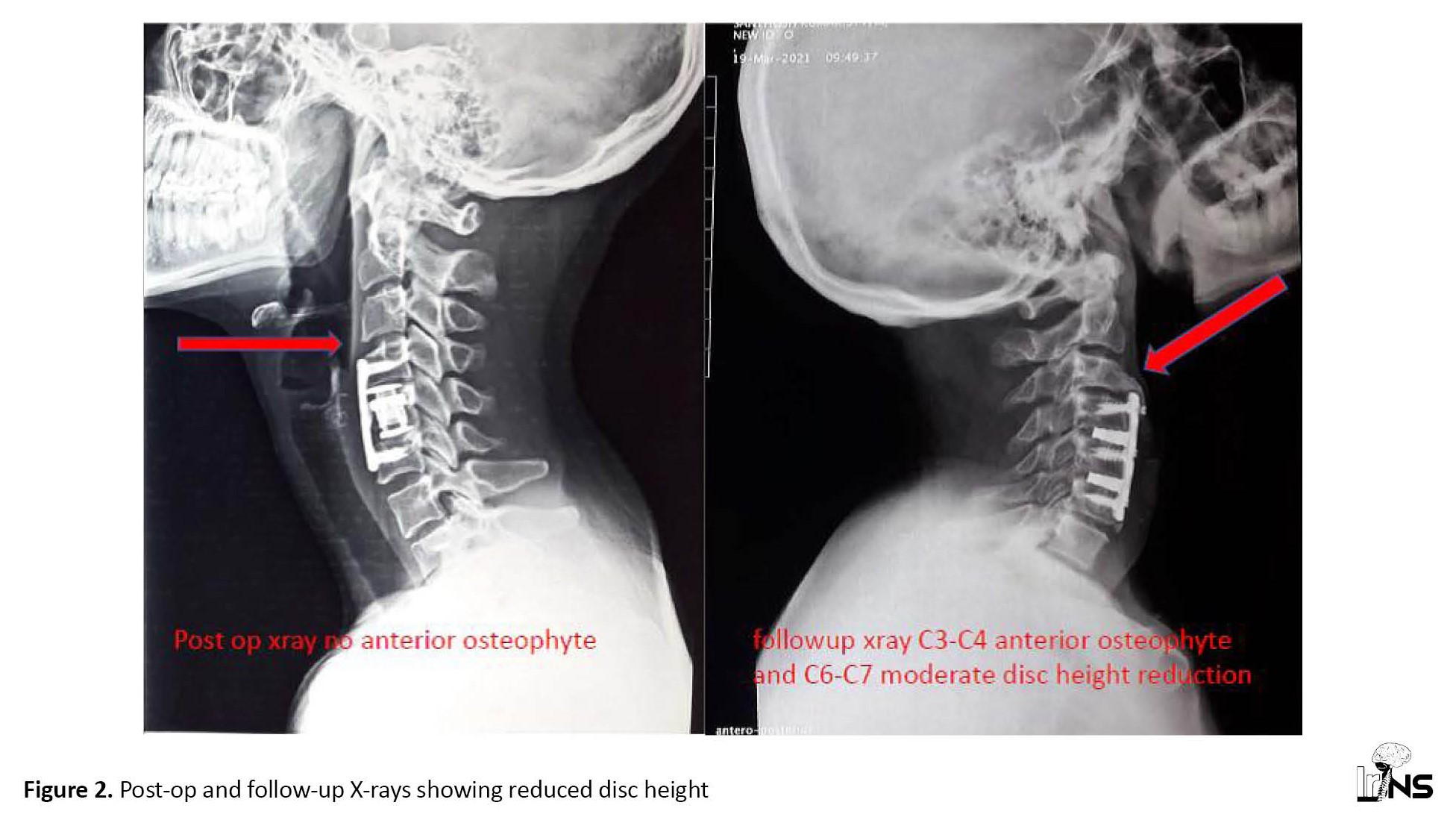
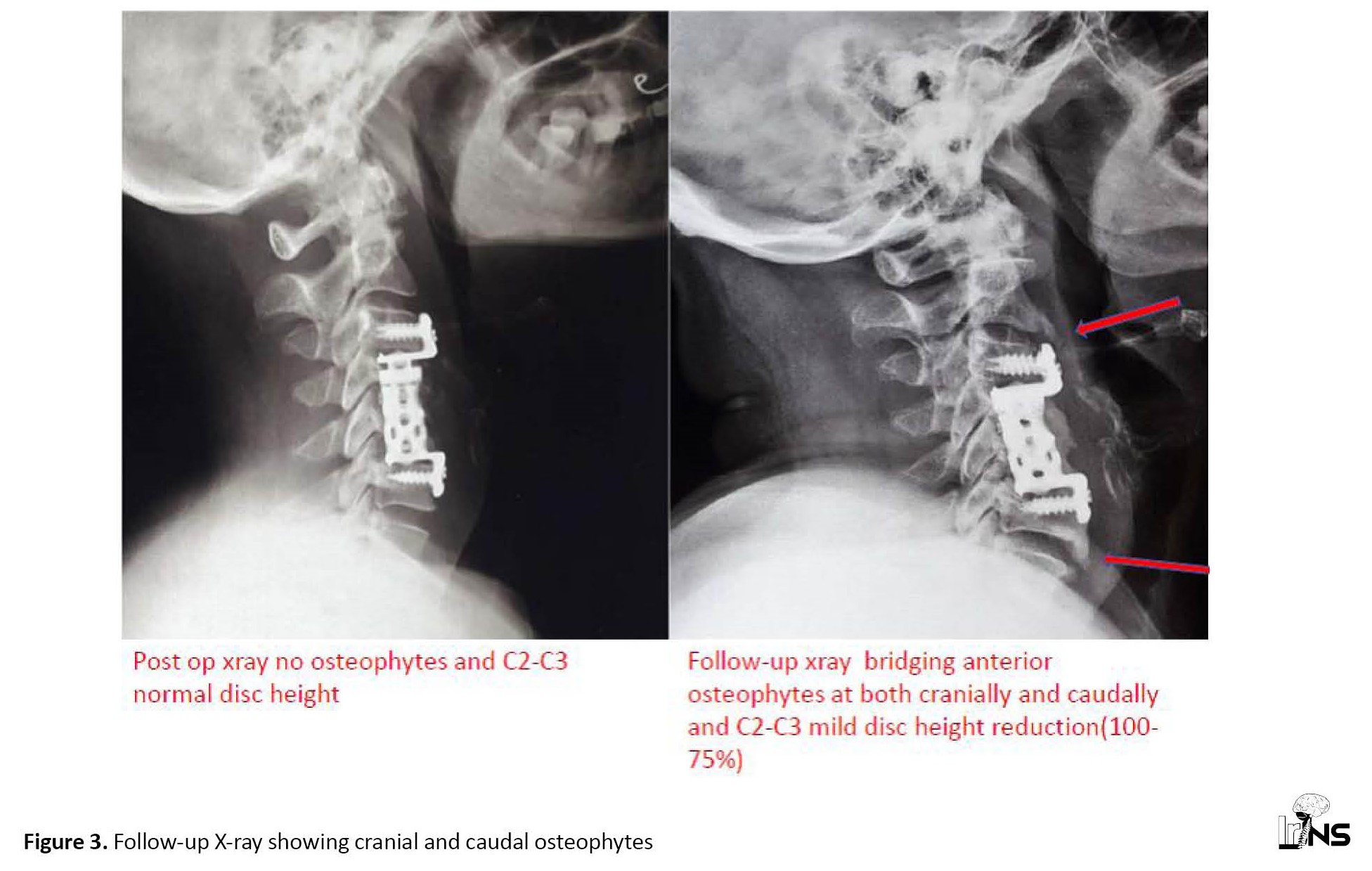
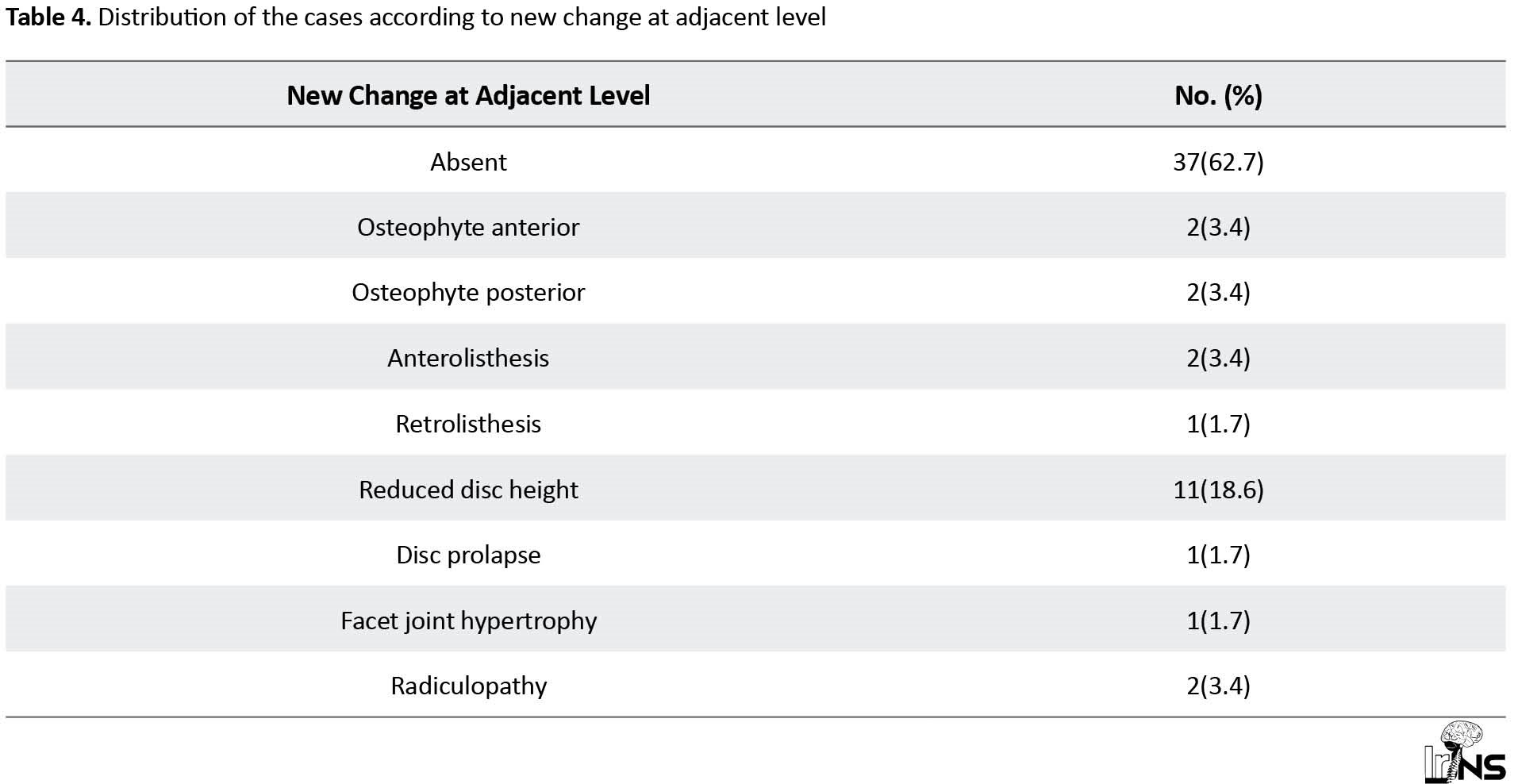
Twenty-two cases (37.3%) with new changes at adjacent levels were the most common pattern identified as reduced disc height in 11 cases (18.6%) (Figures 2 and 3).

Six (10.2%) out of 59 patients developed radiculopathy due to adjacent segment changes and were considered as clinical adjacent segment pathology/ASD, which would be 10.2%. Most patients developed C5 radiculopathy (Table 3).
Twenty-two cases (37.3%) with new changes at adjacent levels were the most common pattern identified as reduced disc height in 11 cases (18.6%) (Figures 2 and 3).
Anterior and posterior osteophytes were found along with reduced disc height in 2 cases (Figure 4), therefore actual new changes were observed in only 20 cases (Table 4).
In our study, the most common level of C4-C5 for the development of ASD was observed in 8 cases (13.6%) and at a C3-C4 level in 5 cases (8.5%).
In our study, ASD developed at cranial to fusion in 13 cases (22%), caudal to fusion in 5 cases (8.5%), and at both levels in 2 cases (Table 5).

4. Discussion
Anterior cervical discectomy and fusion for cervical radiculopathy and/or myelopathy were first described by Robinson and Smith [19] and by Cloward [20, 21]. Changes occurring at the disc levels above and below the level of fusion are described in the literature [1, 2, 11, 18, 22-23]. Various types of degenerative changes are observed, including X-ray and CT evidence, such as mechanical instability, disc degeneration, facet arthropathy, hypertrophy of ligaments, or bony osteophyte of the segments cranial or caudal to a fusion [3].
The exact cause of these degenerative changes is still a matter of debate, increased biomechanical stress leading to increased mobility of segments above and below the level of fusion is a possible explanation [11, 34-39]. Biomechanical causes include increased load at the level of facets, elevated tension in the disc, and entire fused segments acting as a single long unit and hence redistributing the movements to the levels cranial and caudal to the fused segment. In addition to this, these patients may have a background of degenerative disease of the spine and a tendency for stenosis of the spinal canal. This natural progression along with the biomechanical stress described above can lead to exaggerated degeneration at adjacent levels [2, 3, 5, 13, 40].
The radiological changes following fusion surgeries of the cervical spine may vary from 25% to 90% [1, 11, 12, 32, 35, 41-47]. However, the number of patients who are symptomatic due to these adjacent levels are much less, ranging from 6% to 26% in long-term follow-up [3, 4, 12, 16-18]. The incidence of symptomatic cases is 2.9% per year in 10 years following anterior cervical fusion according to Hilibrand et al. [3]. They also concluded that degenerative changes, such as canal stenosis or disk protrusion adjacent to the level of fusion if present, are associated with accelerated degeneration at other levels nearby. In a study conducted by Baba et al. [1], consisting of 106 patients who underwent cervical fixation, 25% developed new spinal canal stenosis cranial to fusion in 8.5 years of follow-up. Nunley et al. [42] conducted a prospective study of a 7-year follow-up of patients treated with either ACDF or cervical disc arthroplasty (CDA) and analyzed clinical and radiological adjacent level changes in them by grouping them into two. They concluded that patients treated with CDA have a lower incidence of clinically significant adjacent level changes than patients treated with ACDF. The risk is more in patients treated with ACDF and young age. In a similar study, Tuanjing et al. [43] conducted a meta-analysis of 29 randomized control trials to study the efficacy of cervical disc arthroplasty (CDA) compared with ACDF and investigated the adjacent segment motion, degeneration, disease, and reoperation of CDA compared with ACDF. They failed to find a significant statistical difference in degenerative changes of adjacent levels between CDA and ACDF within 24 months of follow-up.
A prospective cohort study by Maldonado et al. [44] including both fusion and motion-preserving surgeries showed no statistical difference between the two in terms of adjacent level changes. This emphasizes the importance of studying other risk factors, such as increased propensity in some patients for disc degeneration, and sagittal profile of the cervical spine in patients as etiological factors which lead to such changes.
Tasiou et al. [45] reported adjacent intervertebral disc degeneration in 2.7% of cases. Lunsford et al. [46] reported no significant difference in incidence between patients undergoing ACDF and patients having discectomy only.
Many studies have not documented that the cranial or caudal level is more prone to degeneration than the surgical level. Our study has demonstrated that the level cranial to fixation has more chance of developing adjacent level degeneration. Also, no clear evidence exists in the literature as to what percentage of patients with radiologically demonstrated adjacent degeneration become clinically symptomatic. In our series, 6 out of 20 radiologically significant patients developed clinical symptoms. The type of surgery and the number of levels fused did not show much statistical significance.
5. Conclusion
The proportion of ASD in postoperative cases of cervical spine arthrodesis surgery is 33.9% of 20 cases. However, symptomatic ASD was diagnosed in 6 cases (10.2%). The disease affecting the adjacent segment is more common in degenerative disease cases. Reduced disc height (degenerative changes in disc grade) at follow-up is significantly associated with the development of ASD. Level cranial to fixation was the site of adjacent segment degeneration in the majority of patients as compared with the caudal level. As the number of fixation levels increased, the proportion of adjacent segment degeneration increased; however, the difference was not significant.
Ethical Considerations
Compliance with ethical guidelines
The study started after obtaining approval from the Institutional Research Board and Ethical Committee of Government Medical College Thiruvananthapuram, under Kerala University of Health Sciences, and obtaining informed written consent from the patients (Ethical confirmation code (12) HEC.No.04/48/2020/MCT).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Data collection: Prakash Goswami, Raj S Chandran, Sharmad Mohammed Haneefa; Data analysis and interpretation: All authors; Drafting the article: Prakash Goswami, Raj S Chandran, Sharmad Mohammed Haneefa; Critically revising the article: Prakash Goswami, Raj S Chandran, Arun Sathyababu, Rajmohan Bhanu Prabhakar; Reviewing submitted version of manuscript: All authors; Approving the final version of the manuscript: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
In our study, ASD developed at cranial to fusion in 13 cases (22%), caudal to fusion in 5 cases (8.5%), and at both levels in 2 cases (Table 5).

4. Discussion
Anterior cervical discectomy and fusion for cervical radiculopathy and/or myelopathy were first described by Robinson and Smith [19] and by Cloward [20, 21]. Changes occurring at the disc levels above and below the level of fusion are described in the literature [1, 2, 11, 18, 22-23]. Various types of degenerative changes are observed, including X-ray and CT evidence, such as mechanical instability, disc degeneration, facet arthropathy, hypertrophy of ligaments, or bony osteophyte of the segments cranial or caudal to a fusion [3].
The exact cause of these degenerative changes is still a matter of debate, increased biomechanical stress leading to increased mobility of segments above and below the level of fusion is a possible explanation [11, 34-39]. Biomechanical causes include increased load at the level of facets, elevated tension in the disc, and entire fused segments acting as a single long unit and hence redistributing the movements to the levels cranial and caudal to the fused segment. In addition to this, these patients may have a background of degenerative disease of the spine and a tendency for stenosis of the spinal canal. This natural progression along with the biomechanical stress described above can lead to exaggerated degeneration at adjacent levels [2, 3, 5, 13, 40].
The radiological changes following fusion surgeries of the cervical spine may vary from 25% to 90% [1, 11, 12, 32, 35, 41-47]. However, the number of patients who are symptomatic due to these adjacent levels are much less, ranging from 6% to 26% in long-term follow-up [3, 4, 12, 16-18]. The incidence of symptomatic cases is 2.9% per year in 10 years following anterior cervical fusion according to Hilibrand et al. [3]. They also concluded that degenerative changes, such as canal stenosis or disk protrusion adjacent to the level of fusion if present, are associated with accelerated degeneration at other levels nearby. In a study conducted by Baba et al. [1], consisting of 106 patients who underwent cervical fixation, 25% developed new spinal canal stenosis cranial to fusion in 8.5 years of follow-up. Nunley et al. [42] conducted a prospective study of a 7-year follow-up of patients treated with either ACDF or cervical disc arthroplasty (CDA) and analyzed clinical and radiological adjacent level changes in them by grouping them into two. They concluded that patients treated with CDA have a lower incidence of clinically significant adjacent level changes than patients treated with ACDF. The risk is more in patients treated with ACDF and young age. In a similar study, Tuanjing et al. [43] conducted a meta-analysis of 29 randomized control trials to study the efficacy of cervical disc arthroplasty (CDA) compared with ACDF and investigated the adjacent segment motion, degeneration, disease, and reoperation of CDA compared with ACDF. They failed to find a significant statistical difference in degenerative changes of adjacent levels between CDA and ACDF within 24 months of follow-up.
A prospective cohort study by Maldonado et al. [44] including both fusion and motion-preserving surgeries showed no statistical difference between the two in terms of adjacent level changes. This emphasizes the importance of studying other risk factors, such as increased propensity in some patients for disc degeneration, and sagittal profile of the cervical spine in patients as etiological factors which lead to such changes.
Tasiou et al. [45] reported adjacent intervertebral disc degeneration in 2.7% of cases. Lunsford et al. [46] reported no significant difference in incidence between patients undergoing ACDF and patients having discectomy only.
Many studies have not documented that the cranial or caudal level is more prone to degeneration than the surgical level. Our study has demonstrated that the level cranial to fixation has more chance of developing adjacent level degeneration. Also, no clear evidence exists in the literature as to what percentage of patients with radiologically demonstrated adjacent degeneration become clinically symptomatic. In our series, 6 out of 20 radiologically significant patients developed clinical symptoms. The type of surgery and the number of levels fused did not show much statistical significance.
5. Conclusion
The proportion of ASD in postoperative cases of cervical spine arthrodesis surgery is 33.9% of 20 cases. However, symptomatic ASD was diagnosed in 6 cases (10.2%). The disease affecting the adjacent segment is more common in degenerative disease cases. Reduced disc height (degenerative changes in disc grade) at follow-up is significantly associated with the development of ASD. Level cranial to fixation was the site of adjacent segment degeneration in the majority of patients as compared with the caudal level. As the number of fixation levels increased, the proportion of adjacent segment degeneration increased; however, the difference was not significant.
Ethical Considerations
Compliance with ethical guidelines
The study started after obtaining approval from the Institutional Research Board and Ethical Committee of Government Medical College Thiruvananthapuram, under Kerala University of Health Sciences, and obtaining informed written consent from the patients (Ethical confirmation code (12) HEC.No.04/48/2020/MCT).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Data collection: Prakash Goswami, Raj S Chandran, Sharmad Mohammed Haneefa; Data analysis and interpretation: All authors; Drafting the article: Prakash Goswami, Raj S Chandran, Sharmad Mohammed Haneefa; Critically revising the article: Prakash Goswami, Raj S Chandran, Arun Sathyababu, Rajmohan Bhanu Prabhakar; Reviewing submitted version of manuscript: All authors; Approving the final version of the manuscript: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine. 1993; 18(15):2167-73. [DOI:10.1097/00007632-199311000-00004] [PMID]
- Gore DR, Sepic SB. Anterior cervical fusion for degenerated or protruded discs. A review of one hundred forty-six patients. Spine. 1984; 9(7):667-71. [DOI:10.1097/00007632-198410000-00002] [PMID]
- Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. The Journal of Bone and Joint Surgery. American Volume. 1999; 81(4):519-28. [DOI:10.2106/00004623-199904000-00009] [PMID]
- Gore DR, Sepic SB. Anterior discectomy and fusion for painful cervical disc disease. A report of 50 patients with an average follow-up of 21 years. Spine. 1998; 23(19):2047-51.[DOI:10.1097/00007632-199810010-00002] [PMID]
- Wai EK, Santos ER, Morcom RA, Fraser RD. Magnetic resonance imaging 20 years after anterior lumbar interbody fusion. Spine. 2006; 31(17):1952-6. [DOI:10.1097/01.brs.0000228849.37321.a8] [PMID]
- Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG. Adjacent segment degeneration in the lumbar spine. The Journal of Bone and Joint Surgery. American Volume. 2004; 86(7):1497-503. [DOI:10.2106/00004623-200407000-00020] [PMID]
- Lehmann TR, Spratt KF, Tozzi JE, Weinstein JN, Reinarz SJ, el-Khoury GY, et al. Long-term follow-up of lower lumbar fusion patients. Spine. 1987; 12(2):97-104.[DOI:10.1097/00007632-198703000-00004] [PMID]
- Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine. 1988; 13(3):375-7. [DOI:10.1097/00007632-198803000-00029] [PMID]
- Okuda S, Iwasaki M, Miyauchi A, Aono H, Morita M, Yamamoto T. Risk factors for adjacent segment degeneration after PLIF. Spine. 2004; 29(14):1535-40. [DOI:10.1097/01.BRS.0000131417.93637.9D] [PMID]
- Cheh G, Bridwell KH, Lenke LG, Buchowski JM, Daubs MD, Kim Y, et al. Adjacent segment disease following lumbar/ thoracolumbar fusion with pedicle screw instrumentation: A minimum 5-year follow-up. Spine. 2007; 32(20):2253-7. [DOI:10.1097/BRS.0b013e31814b2d8e] [PMID]
- Döhler JR, Kahn MR, Hughes SP. Instability of the cervical spine after anterior interbody fusion. A study on its incidence and clinical significance in 21 patients. Archives of Orthopaedic and Traumatic Surgery. 1985; 104(4):247-50. [DOI:10.1007/BF00450219] [PMID]
- Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B, et al. Long-term follow-up after interbody fusion of the cervical spine. Journal of Spinal Disorders & Techniques. 2004; 17(2):79-85. [DOI:10.1097/00024720-200404000-00001] [PMID]
- Hunter LY, Braunstein EM, Bailey RW. Radiographic changes following anterior cervical fusion. Spine. 1980; 5(5):399-401. [DOI:10.1097/00007632-198009000-00002] [PMID]
- Kulkarni V, Rajshekhar V, Raghuram L. Accelerated spondylotic changes adjacent to the fused segment following central cervical corpectomy: Magnetic resonance imaging study evidence. Journal of Neurosurgery, 100(1 Suppl Spine). 2004; 100(1 suppl Spine):2-6. [DOI:10.3171/spi.2004.100.1.0002] [PMID]
- Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: Review of the literature. Spine. 2004; 29(17):1938-44.[DOI:10.1097/01.brs.0000137069.88904.03] [PMID]
- Ishihara H, Kanamori M, Kawaguchi Y, Nakamura H, Kimura T. Adjacent segment disease after anterior cervical interbody fusion. The Spine Journal. 2004; 4(6):624-8.[DOI:10.1016/j.spinee.2004.04.011] [PMID]
- Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating: A 5- to 11-year radiologic and clinical follow-up study. Spine. 2005; 30(19):2138-44. [DOI:10.1097/01.brs.0000180479.63092.17] [PMID]
- Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. The Journal of Bone and Joint Surgery. American Volume. 1993; 75(9):1298-307.[DOI:10.2106/00004623-199309000-00005] [PMID]
- Robinson RA, Smith GW. Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull John Hopkins Hosp. 1955; 96:223–4. [Link]
- CLOWARD RB. The anterior approach for removal of ruptured cervical disks. Journal of Neurosurgery. 1958; 15(6):602-17. [DOI:10.3171/jns.1958.15.6.0602] [PMID]
- Cloward RB. Complications of anterior cervical disc operation and their treatment. Surgery. 1971; 69(2):175-82. [PMID]
- Boni M, Denaro V. [Surgical treatment of cervical arthrosis. Follow-up review (2-13 years) of the 1st 100 cases operated on by anterior approach (French)]. Revue de Chirurgie Orthopedique et Reparatrice de L'appareil Moteur. 1982; 68(4):269-80. [PMID]
- Braunstein EM, Hunter LY, Bailey RW. Long term radiographic changes following anterior cervical fusion. Clinical Radiology. 1980; 1(2):201-3. [DOI:10.1016/S0009-9260(80)80160-7] [PMID]
- DePalma AF, Rothman RH, Lewinnek GE, Canale ST. Anterior interbody fusion for severe cervical disc degeneration. Surgery, Gynecology & Obstetrics. 1972; 134(5):755-8. [PMID]
- Goffin J, van Loon J, Van Calenbergh F, Plets C. Long-term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. Journal of Spinal Disorders. 1995; 8(6):500-8; discussion 499.[DOI:10.1097/00002517-199512000-00014] [PMID]
- Gore DR, Gardner GM, Sepic SB, Murray MP. Roentgenographic findings following anterior cervical fusion. Skeletal Radiology. 1986; 15(7):556-9. [DOI:10.1007/BF00361055] [PMID]
- Gruss P, Tannenbaum H. Stress exertion on adjacent segments after ventral cervical fusion. Archives of Orthopaedic And Traumatic Surgery. 1983; 101(4):283-6. [DOI:10.1007/BF00379944] [PMID]
- Hilibrand AS, Yoo JU, Carlson GD, Bohlman HH. The success of anterior cervical arthrodesis adjacent to a previous fusion. Spine. 1997; 22(14):1574-9. [DOI:10.1097/00007632-199707150-00009] [PMID]
- Mähring M. [Segment changes in the cervical spine following cervical spondylodeses of unstable injuries (German)]. 1988; 14(5):247-58. [DOI:10.1007/BF02807981] [PMID]
- Matsunaga S, Kabayama S, Yamamoto T, Yone K, Sakou T, Nakanishi K. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine. 1999; 24(7):670-5. [DOI:10.1097/00007632-199904010-00011] [PMID]
- McGrory BJ, Klassen RA. Arthrodesis of the cervical spine for fractures and dislocations in children and adolescents. A long-term follow-up study. The Journal of Bone and Joint Surgery. American Volume 1994; 76(11):1606-16. [DOI:10.2106/00004623-199411000-00003] [PMID]
- Woesner ME, Mitts MG. The evaluation of cervical spine motion below C2: A comparison of cineroentgenographic and conventional roentgenographic methods. The American Journal of Roentgenology, Radium Therapy, and Nuclear Medicine. 1972; 115(1):148-54. [DOI:10.2214/ajr.115.1.148] [PMID]
- Yamamoto I, Ikeda A, Shibuya N, Tsugane R, Sato O. Clinical long-term results of anterior discectomy without interbody fusion for cervical disc disease. Spine. 1991; 16(3):272-9. [DOI:10.1097/00007632-199103000-00004] [PMID]
- Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine. 2002; 27(22):2431-4. [DOI:10.1097/00007632-200211150-00003] [PMID]
- Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. European Spine Journal. 2001; 10(4):320-4.[DOI:10.1007/s005860000243] [PMID] [PMCID]
- Cheng JS, Liu F, Komistek RD, Mahfouz MR, Sharma A, Glaser D. Comparison of cervical spine kinematics using a fluoroscopic model for adjacent segment degeneration. Invited submission from the Joint Section on Disorders of the Spine and Peripheral Nerves, March 2007. Journal of neurosurgery. Spine, 2007; 7(5):509-13. [DOI:10.3171/SPI-07/11/509] [PMID]
- Park DH, Ramakrishnan P, Cho TH, Lorenz E, Eck JC, Humphreys SC, et al. Effect of lower two-level anterior cervical fusion on the superior adjacent level. Journal of Neurosurgery. Spine. 2007; 7(3):336-40. [DOI:10.3171/SPI-07/09/336] [PMID]
- Levin DA, Hale JJ, Bendo JA. Adjacent segment degeneration following spinal fusion for degenerative disc disease. Bulletin of the NYU Hospital for Joint Diseases. 2007; 65(1):29-36. [PMID]
- Dmitriev AE, Kuklo TR, Lehman RA Jr, Rosner MK. Stabilizing potential of anterior, posterior, and circumferential fixation for multilevel cervical arthrodesis: An in vitro human cadaveric study of the operative and adjacent segment kinematics. Spine. 2007; 32(6):E188-96. [DOI:10.1097/01.brs.0000257577.70576.07] [PMID]
- Hilibrand AS, Robbins M. Adjacent segment degeneration and adja¬cent segment disease: The consequences of spinal fusion? The Spine Journal 2004; 4(suppl 6):190S-194S. [DOI:10.1016/j.spinee.2004.07.007] [PMID]
- Herkowitz HN, Kurz LT, Overholt DP. Surgical management of cervical soft disc herniation. A comparison between the anterior and posterior approach. Spine. 1990; 15(10):1026-30. [DOI:10.1097/00007632-199010000-00009] [PMID]
- Nunley PD, Kerr EJ 3rd, Cavanaugh DA, Utter PA, Campbell PG, Wadhwa R, et al. Adjacent segment pathology after treatment with cervicaldisc arthroplasty or anterior cervical discectomy and fusion, part 2: Clinical results at 7-year follow-up. International Journal of Spine Surgery. 2020; 14(3):278-85. [DOI:10.14444/7037] [PMID] [PMCID]
- Dong L, Xu Z, Chen X, Wang D, Li D, Liu T, et al. The change of adjacent segment after cervical disc arthroplasty compared with anterior cervical discectomy and fusion: A meta-analysis of randomized controlled trials. The Spine Journal. 2017; 17(10):1549-58. [DOI:10.1016/j.spinee.2017.06.010] [PMID]
- Maldonado CV, Paz RD, Martin CB. Adjacent-level degeneration after cervical disc arthroplasty versus fusion. European Spine Journal. 2011; 20 Suppl 3(Suppl 3):403-7. [DOI:10.1007/s00586-011-1916-1] [PMID] [PMCID]
- Tasiou A, Giannis T, Brotis AG, Siasios I, Georgiadis I, Gatos H, et al. Anterior cervical spine surgery-associated complications in a retrospective case-control study. Journal of Spine Surgery (Hong Kong). 2017; 3(3):444-59. [DOI:10.21037/jss.2017.08.03] [PMID] [PMCID]
- Lunsford LD, Bissonette DJ, Jannetta PJ, Sheptak PE, Zorub DS. Anterior surgery for cervical disc disease. Part 1: Treatment of lateral cervical disc herniation in 253 cases. Journal of Neurosurgery.1980; 53(1):1-11. [PMID]
- Kawakami M, Tamaki T, Yoshida M, Hayashi N, Ando M, Yamada H. Axial symptoms and cervical alignments after cervical anterior spinal fusion for patients with cervical myelopathy. Journal of Spinal Disorders. 1999; 12(1):50-6. [PMID
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |