Tue, Feb 3, 2026
Volume 9 - Continuous Publishing
Iran J Neurosurg 2023, 9 - Continuous Publishing: 133-138 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
S. Chandran R, Sathyababu A, Mohammed Haneefa S, Bhanu Prabhakar R. Microlumbar Discectomy vs Minimally Invasive Tubular Microdiscectomy: A Prospective Comparative Analysis. Iran J Neurosurg 2023; 9 : 18
URL: http://irjns.org/article-1-356-en.html
URL: http://irjns.org/article-1-356-en.html
1- Department of Neurosurgery, Government Medical College, Thiruvananthapuram, Kerala, India , rajschandran@gmail.com
2- Department of Neurosurgery, Government Medical College, Thiruvananthapuram, Kerala, India
2- Department of Neurosurgery, Government Medical College, Thiruvananthapuram, Kerala, India
Full Text [PDF 2070 kb]
(1071 Downloads)
| Abstract (HTML) (3513 Views)
Full Text: (1626 Views)
1. Introduction
Prolapse of the lumbar disc is a common cause of low backache and radiculopathy. In cases where conservative treatment is unsuccessful and progressive neurological deterioration, surgery is indicated. Since the surgical description provided by Mixter and Barr [1], different techniques have evolved. The classical open-wide laminectomy and discectomy gave way to microsurgical procedures or microdiscectomy by Caspar and Yasergill [2, 3]. Microlumbar discectomy (MLD) involves the removal of a small portion of the lamina and the removal of ligamentum flavum on one side under a microscope. Newer techniques with smaller incisions, serial dilatation using tubular retractors, and discectomy through 16 to 18-mm tubes changed the concept of discectomy from “open” to “keyhole” daycare surgery. The principles of surgery in both MLD and minimally invasive surgery (MIS) using a tube include laminotomy, medial facetectomy, flavum excision, exposing the Kambin’s triangle, and discectomy, while minimally invasive through the tubular retractors in the second group. Both procedures are performed in our institution and we try to compare and analyze the results of the two procedures.
2. Methods and Materials/Patients
This prospective, observational study was conducted on patients who underwent surgical treatment for lumbar disc herniation by either MLD or MIS using a tubular retractor system during one year in the department of neurosurgery.
Inclusion criteria
All patients, irrespective of age, socioeconomic status, or duration of symptoms who presented with lumbar radicular pain, sensory or motor deficit, and radiologically documented single-level intervertebral disc prolapse in magnetic resonance imaging (MRI), underwent surgery by either MLD or MIS using tubular retractor system.
Exclusion criteria
1. Patients who had already undergone lumbar surgery.
2. Scoliosis more than 15 ̊
3. Segmental instability
4. Vertebral fractures, spine infection, tumor, inflammatory, spondyloarthropathy
5. Patients who underwent other procedures for lumbar disc prolapse
MRI scans were taken for all patients. Dynamic X-rays were taken in flexion and extension to rule out segmental instability. Patients with degenerative lumbar canal stenosis were not involved in the study group. Investigations, such as computerized tomography (CT) scan, nerve conduction velocity (NCV), and electromyography (EMG) are not routinely done in cases with clinical and radiological diagnoses of lumbar intervertebral disc prolapse in our center.
The records of the patients included the patient’s age, sex, the onset of symptoms, the symptoms of low backache, radicular pain, motor, sensory, straight leg raise (SLR) test, bowel or bladder involvement, comorbidities, MRI level, type of herniation, operating time, estimated blood loss, opioid use in post-op period, complications and outcome based on MacNab scale.
All patients were followed up for at least 6 months. The satisfaction status was graded as excellent, good, fair, or poor. “Excellent result” meant that the patient had no complaints and was able to return to full working capacity. “Good result” indicated that the patient had full working capacity but slight low backache and leg pain. “Excellent results” or “good results” were regarded as satisfactory outcomes. “Fair results” indicated that the patient did not have normal working capacity; low back and leg pain reduced but the patient still required the administration of analgesics. “Poor result” meant that the degree of pain was unchanged or worse and the patient required regular administration of analgesics [4].
Statistical analysis
All clinical data were entered into Excel sheets and analyzed using SPSS software, version 18. The mean values, percentages, and P were calculated.
3. Results
Among the 99 patients included in the study based on the inclusion criteria, 27 patients were in the age group of 21 to 30 years (27.3%), 35 patients in the age group of 31 to 40 years (35.4%), 27 patients in the age group of 41 to 50 years (27.3%), 7 patients in the age group of 51 to 60 years (7.07%) and 3 patients were aged above 60 years (3.03%).
In this study, out of 99 patients, 59.99 (59.6%) were men, of whom 31 men underwent MLD and 28 men underwent MIS; 40.200 patients (40.4%) were women, of whom 27 women underwent MLD and 13 women underwent MIS.
Observations of the onset of symptoms in the subjects showed that 43 of 200 patients (43.4%) had insidious onset of symptoms (28 in MLD and 15 in MIS group); 37.99 patients (37.4%) had a history of increased weight before the onset of the symptoms (15 in MLD and 28 in MIS group) and trauma was the initiating factor in 19.99 patients (19.2%) (15 and 4, respectively).
Low backache was present in 91 patients (91.9% of the total). Radicular pain was seen in 92.99 patients (55 and 37 in MLD and MIS groups). Sensory symptoms were present in 73 cases (73.7%) (42 and 31 in each group); motor symptoms in 49 patients (49.5%) (29 and 20 in each group); 5.05% of patients presented with bowel and bladder symptoms, and all underwent MLD.
Clinical examination revealed that the SLR test was positive in 91 patients, and crossed SLR was positive in 27 cases. The motor deficit was present in 75.5% of the cases (40 and 34 in each group), and sensory deficit in 73.5% of patients (37 and 31 cases in each).
Among the 99 patients, the majority had involvement of L4-L5 spinal level in 55 cases (24 and 31) (55.6%) followed by L5-S1 in 37 cases (29 and 8) (37.4%), L3-L4 spinal in 7 cases (7.07%).
The average operating time was 90 minutes for MLD, while it was 110 minutes for MIS discectomy.
Estimated blood loss was about 100 mL in MLD and about 60 mL in MIS discectomy.
Prolonged opioid treatment was required for pain relief for more than 24 hours in 7 cases of MLD, while none of the MIS discectomy patients required prolonged post-op opioids for pain relief.
Dural injury and intraoperative cerebrospinal fluid (CSF) leak occurred in 2 cases of MIS discectomy, both settled with fat and tissue glue. Recurrent disc occurred at follow-up in 5 cases of MLD and 4 cases of MIS discectomy.
Six months after surgery, all the patients were followed up to assess for relief of symptoms and recovery of sensory and motor deficits.
On follow-up, 85.4% of the MIS group had an excellent outcome compared to 77.6% of patients in the MLD group. Poor outcome was recorded in 2 patients in the MLD group (3.45%) and 3 patients in the MIS group (7.32%).
4. Discussion
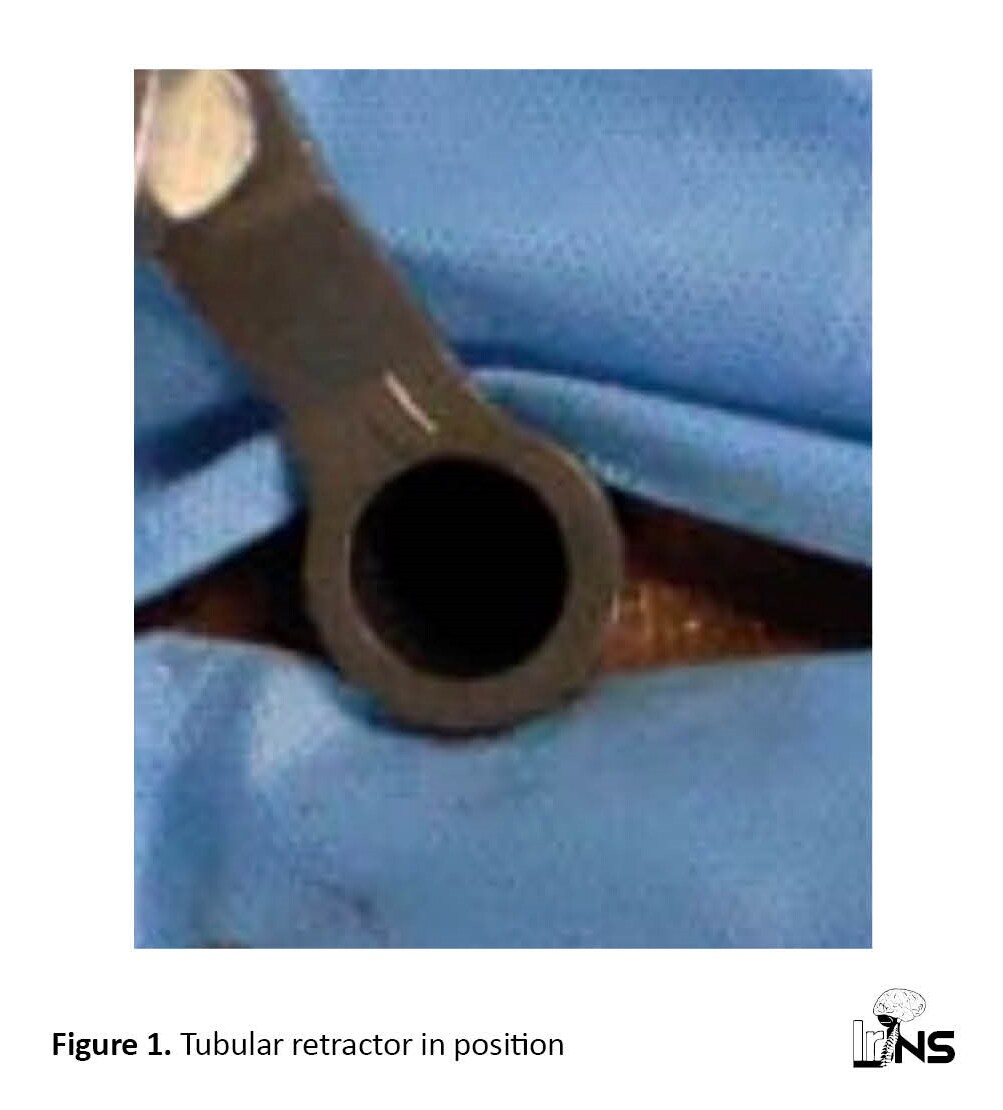
The literature shows that about 80% of adults experience low back pain at some time, and it is one of the common causes of physical activity restriction in the age group of less than 45 years old [5]. Patients with lumbar disc prolapse present with low back pain, radicular pain, numbness, weakness, bowel/bladder disturbances, and paresthesia. Mixter and Barr were the first to describe the first surgical method to treat ruptured intervertebral discs [2]. Many procedures evolved since then. This includes open laminectomy and discectomy, MLD, in which minimal bone and ligamentum flavum removal is performed, followed by removal of the prolapsed or bulged disc through a small incision, removal of the disc material using a tubular retractor system (Figure 1), endoscopic discectomy, etc.
In a minimally invasive tubular discectomy, the prolapsed disc material is visualized through the tube under high magnification using an operating microscope (Figure 2) and removed till the dura and root are lax (Figure 3).


The recovery from pain and neurological deficits following surgical techniques shows striking variations, depending on factors, such as patient selection and examination and surgical techniques [6].
In classical MLD, subperiosteal retraction of muscles is performed using specialized retractors. In MIS, serial dilators are used through a muscle-splitting approach using a tubular retractor system.
In a study conducted by German et al., minimally invasive surgery (MIS) using tubular retractors had an operating time of 165.5±5.75 and open microsurgical discectomy had an operating time of 169.8±4.37, but the difference was statistically insignificant [7]. It was 110 and 90 minutes, respectively, in our series.
According to German et al, MIS estimated blood loss of 59.3±12.0 mL and open microsurgical discectomy estimated blood loss of 90.4±8.1 mL, which was statistically significant [7]; the results were almost similar to our series.
In a similar comparative study conducted by Grenier-Perth et al., MIS had an operating time of 69 minutes and open microsurgical discectomy had an operating time of 63 minutes. MIS estimated blood loss of 30 mL and open microsurgical discectomy had estimated blood loss of 90 mL [8].
The results were almost similar to our series. Post-operative use of opioid analgesics was less in MIS patients compared to the MLD group.
Muramatsu et al. documented that 100% of open microsurgical discectomy patients used morphine in the post-op period while only 52% used opioids in the MIS group [9]. Brock et al. also commented that post-operative analgesic usage was significantly lower in the tubular group [10].
The main complications studied included inadvertent injury to the dura and CSF leak. Recurrence of disc prolapse was another concern when opting for a minimally invasive technique compared to the accepted open technique. The trial conducted by Ryang et al. used the tubular technique as originally described and demonstrated no difference in recurrent disc herniation or CSF leak, whereas, in our series, recurrence was similar but intraoperative injury to the dura and CSF leak was more in the MIS group [11].
Teli et al. demonstrated no difference in overall complications in the tubular microdiscectomy group but showed increased CSF leaks [12].
In describing the technique of tubular discectomy and review, Clark et al. found that complication profiles for tubular MIS and MLD are similar [4]. Intraoperative injury to dura is the most common complication; rates range from 7%-10%.
Other factors analyzed were the length of hospitalization, blood loss, and functional outcome at follow-up. Overdevest et al. showed no difference in functional or clinical outcome between patients randomly allocated to tubular discectomy and MLD at 5 years of follow-up. Only the length of hospitalization and blood loss were significantly reduced with tubular discectomy [13]. In short, no significant difference was observed between the two procedures in terms of functional outcome, complications, or recurrence rate. Decreased blood loss, lower post-operative analgesic requirement, and early return-to-work can place MIS with a tubular retractor system in an advantageous position compared to classical MLD, though the cost of the tubular retractor system and instruments are high.Moreover, MIS, considered “keyhole surgery”, gives more satisfaction to patients than “open” surgery.
5. Conclusion
There has been a shift from open to keyhole surgery in all fields of surgery. However, the advantages and disadvantages should be carefully analyzed. In our study, comparing MLD and minimally invasive surgery using a tubular retractor system, the functional outcome and complications and recurrence are almost the same. However, less blood loss and less analgesic requirement in the postoperative period are the definite advantages of tube discectomy.
Limitations
Only cases of single-level lumbar disc prolapse were included in the study. The outcome was assessed for up to six months but the long-term outcome should be studied since failures and recurrences may occur later.
Ethical Considerations
Compliance with ethical guidelines
The study was conducted after obtaining approval from the Institutional Research Board and Ethical Committee of Government Medical College Thiruvananthapuram, (IEC No.: 06/20/2017/MCT dated 17/04/2017). Informed written consent was obtained from the participants. Confidentiality was ensured and maintained throughout the study. Complications, when observed, were dealt with accordingly.
Funding
The article was extracted from the MCh in Neurosurgery dissertation submitted to the Kerala University of Health Sciences.
Authors' contributions
Conception, study design, data analysis and interpretation: All authors; Data collection: Raj S Chandran, Arun Sathyababu and Sharmad Mohammed Haneefa; Drafting the article: Raj S Chandran, Arun Sathyababu and Sharmad Mohammed Haneefa; Critically revising the article: Raj S Chandran, Arun Sathyababu and Rajmohan Bhanu Prabhakar; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors wish to express their gratitude to Ajith Nair, the former associate professor of Neurosurgery, Government Medical College Thiruvananthapuram for his help.
References
Prolapse of the lumbar disc is a common cause of low backache and radiculopathy. In cases where conservative treatment is unsuccessful and progressive neurological deterioration, surgery is indicated. Since the surgical description provided by Mixter and Barr [1], different techniques have evolved. The classical open-wide laminectomy and discectomy gave way to microsurgical procedures or microdiscectomy by Caspar and Yasergill [2, 3]. Microlumbar discectomy (MLD) involves the removal of a small portion of the lamina and the removal of ligamentum flavum on one side under a microscope. Newer techniques with smaller incisions, serial dilatation using tubular retractors, and discectomy through 16 to 18-mm tubes changed the concept of discectomy from “open” to “keyhole” daycare surgery. The principles of surgery in both MLD and minimally invasive surgery (MIS) using a tube include laminotomy, medial facetectomy, flavum excision, exposing the Kambin’s triangle, and discectomy, while minimally invasive through the tubular retractors in the second group. Both procedures are performed in our institution and we try to compare and analyze the results of the two procedures.
2. Methods and Materials/Patients
This prospective, observational study was conducted on patients who underwent surgical treatment for lumbar disc herniation by either MLD or MIS using a tubular retractor system during one year in the department of neurosurgery.
Inclusion criteria
All patients, irrespective of age, socioeconomic status, or duration of symptoms who presented with lumbar radicular pain, sensory or motor deficit, and radiologically documented single-level intervertebral disc prolapse in magnetic resonance imaging (MRI), underwent surgery by either MLD or MIS using tubular retractor system.
Exclusion criteria
1. Patients who had already undergone lumbar surgery.
2. Scoliosis more than 15 ̊
3. Segmental instability
4. Vertebral fractures, spine infection, tumor, inflammatory, spondyloarthropathy
5. Patients who underwent other procedures for lumbar disc prolapse
MRI scans were taken for all patients. Dynamic X-rays were taken in flexion and extension to rule out segmental instability. Patients with degenerative lumbar canal stenosis were not involved in the study group. Investigations, such as computerized tomography (CT) scan, nerve conduction velocity (NCV), and electromyography (EMG) are not routinely done in cases with clinical and radiological diagnoses of lumbar intervertebral disc prolapse in our center.
The records of the patients included the patient’s age, sex, the onset of symptoms, the symptoms of low backache, radicular pain, motor, sensory, straight leg raise (SLR) test, bowel or bladder involvement, comorbidities, MRI level, type of herniation, operating time, estimated blood loss, opioid use in post-op period, complications and outcome based on MacNab scale.
All patients were followed up for at least 6 months. The satisfaction status was graded as excellent, good, fair, or poor. “Excellent result” meant that the patient had no complaints and was able to return to full working capacity. “Good result” indicated that the patient had full working capacity but slight low backache and leg pain. “Excellent results” or “good results” were regarded as satisfactory outcomes. “Fair results” indicated that the patient did not have normal working capacity; low back and leg pain reduced but the patient still required the administration of analgesics. “Poor result” meant that the degree of pain was unchanged or worse and the patient required regular administration of analgesics [4].
Statistical analysis
All clinical data were entered into Excel sheets and analyzed using SPSS software, version 18. The mean values, percentages, and P were calculated.
3. Results
Among the 99 patients included in the study based on the inclusion criteria, 27 patients were in the age group of 21 to 30 years (27.3%), 35 patients in the age group of 31 to 40 years (35.4%), 27 patients in the age group of 41 to 50 years (27.3%), 7 patients in the age group of 51 to 60 years (7.07%) and 3 patients were aged above 60 years (3.03%).
In this study, out of 99 patients, 59.99 (59.6%) were men, of whom 31 men underwent MLD and 28 men underwent MIS; 40.200 patients (40.4%) were women, of whom 27 women underwent MLD and 13 women underwent MIS.
Observations of the onset of symptoms in the subjects showed that 43 of 200 patients (43.4%) had insidious onset of symptoms (28 in MLD and 15 in MIS group); 37.99 patients (37.4%) had a history of increased weight before the onset of the symptoms (15 in MLD and 28 in MIS group) and trauma was the initiating factor in 19.99 patients (19.2%) (15 and 4, respectively).
Low backache was present in 91 patients (91.9% of the total). Radicular pain was seen in 92.99 patients (55 and 37 in MLD and MIS groups). Sensory symptoms were present in 73 cases (73.7%) (42 and 31 in each group); motor symptoms in 49 patients (49.5%) (29 and 20 in each group); 5.05% of patients presented with bowel and bladder symptoms, and all underwent MLD.
Clinical examination revealed that the SLR test was positive in 91 patients, and crossed SLR was positive in 27 cases. The motor deficit was present in 75.5% of the cases (40 and 34 in each group), and sensory deficit in 73.5% of patients (37 and 31 cases in each).
Among the 99 patients, the majority had involvement of L4-L5 spinal level in 55 cases (24 and 31) (55.6%) followed by L5-S1 in 37 cases (29 and 8) (37.4%), L3-L4 spinal in 7 cases (7.07%).
The average operating time was 90 minutes for MLD, while it was 110 minutes for MIS discectomy.
Estimated blood loss was about 100 mL in MLD and about 60 mL in MIS discectomy.
Prolonged opioid treatment was required for pain relief for more than 24 hours in 7 cases of MLD, while none of the MIS discectomy patients required prolonged post-op opioids for pain relief.
Dural injury and intraoperative cerebrospinal fluid (CSF) leak occurred in 2 cases of MIS discectomy, both settled with fat and tissue glue. Recurrent disc occurred at follow-up in 5 cases of MLD and 4 cases of MIS discectomy.
Six months after surgery, all the patients were followed up to assess for relief of symptoms and recovery of sensory and motor deficits.
On follow-up, 85.4% of the MIS group had an excellent outcome compared to 77.6% of patients in the MLD group. Poor outcome was recorded in 2 patients in the MLD group (3.45%) and 3 patients in the MIS group (7.32%).
4. Discussion
The literature shows that about 80% of adults experience low back pain at some time, and it is one of the common causes of physical activity restriction in the age group of less than 45 years old [5]. Patients with lumbar disc prolapse present with low back pain, radicular pain, numbness, weakness, bowel/bladder disturbances, and paresthesia. Mixter and Barr were the first to describe the first surgical method to treat ruptured intervertebral discs [2]. Many procedures evolved since then. This includes open laminectomy and discectomy, MLD, in which minimal bone and ligamentum flavum removal is performed, followed by removal of the prolapsed or bulged disc through a small incision, removal of the disc material using a tubular retractor system (Figure 1), endoscopic discectomy, etc.
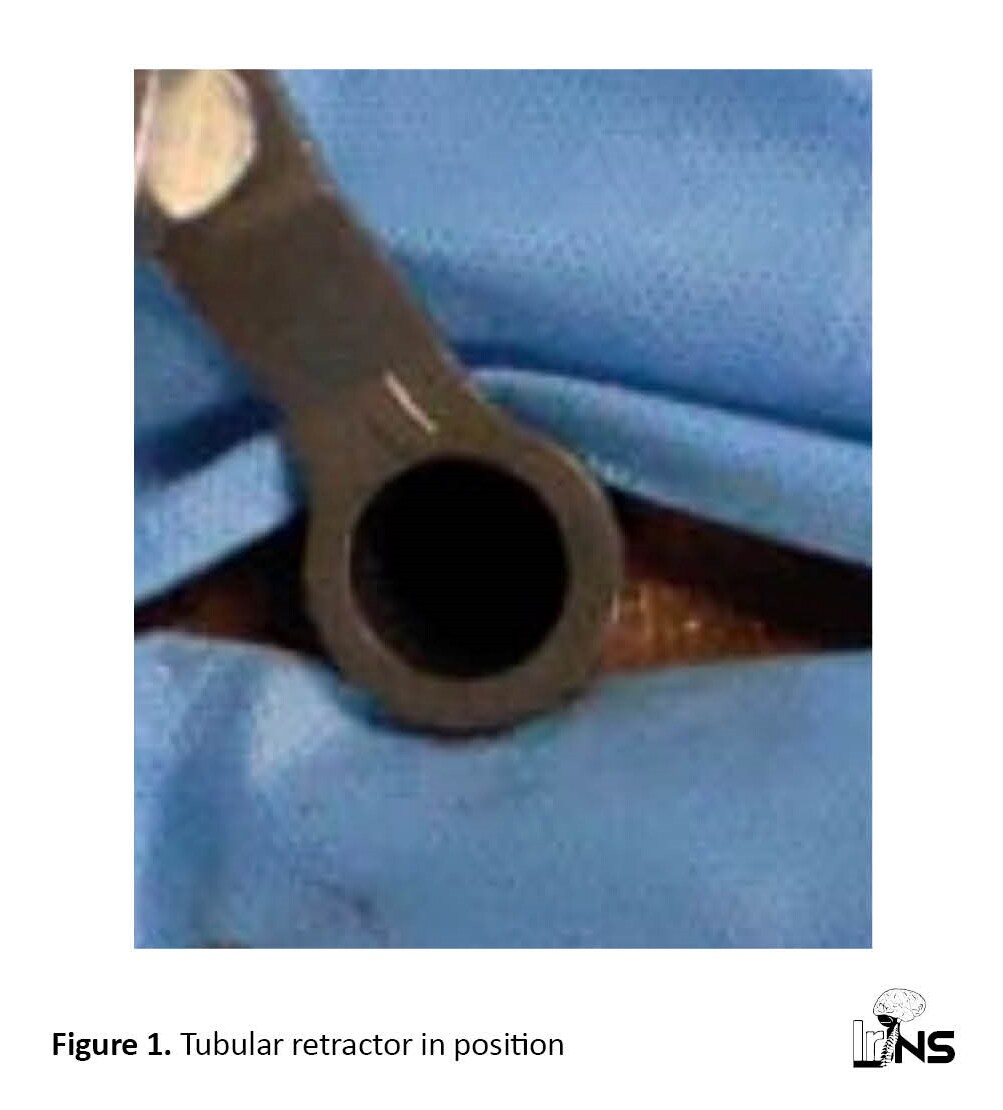
In a minimally invasive tubular discectomy, the prolapsed disc material is visualized through the tube under high magnification using an operating microscope (Figure 2) and removed till the dura and root are lax (Figure 3).


The recovery from pain and neurological deficits following surgical techniques shows striking variations, depending on factors, such as patient selection and examination and surgical techniques [6].
In classical MLD, subperiosteal retraction of muscles is performed using specialized retractors. In MIS, serial dilators are used through a muscle-splitting approach using a tubular retractor system.
In a study conducted by German et al., minimally invasive surgery (MIS) using tubular retractors had an operating time of 165.5±5.75 and open microsurgical discectomy had an operating time of 169.8±4.37, but the difference was statistically insignificant [7]. It was 110 and 90 minutes, respectively, in our series.
According to German et al, MIS estimated blood loss of 59.3±12.0 mL and open microsurgical discectomy estimated blood loss of 90.4±8.1 mL, which was statistically significant [7]; the results were almost similar to our series.
In a similar comparative study conducted by Grenier-Perth et al., MIS had an operating time of 69 minutes and open microsurgical discectomy had an operating time of 63 minutes. MIS estimated blood loss of 30 mL and open microsurgical discectomy had estimated blood loss of 90 mL [8].
The results were almost similar to our series. Post-operative use of opioid analgesics was less in MIS patients compared to the MLD group.
Muramatsu et al. documented that 100% of open microsurgical discectomy patients used morphine in the post-op period while only 52% used opioids in the MIS group [9]. Brock et al. also commented that post-operative analgesic usage was significantly lower in the tubular group [10].
The main complications studied included inadvertent injury to the dura and CSF leak. Recurrence of disc prolapse was another concern when opting for a minimally invasive technique compared to the accepted open technique. The trial conducted by Ryang et al. used the tubular technique as originally described and demonstrated no difference in recurrent disc herniation or CSF leak, whereas, in our series, recurrence was similar but intraoperative injury to the dura and CSF leak was more in the MIS group [11].
Teli et al. demonstrated no difference in overall complications in the tubular microdiscectomy group but showed increased CSF leaks [12].
In describing the technique of tubular discectomy and review, Clark et al. found that complication profiles for tubular MIS and MLD are similar [4]. Intraoperative injury to dura is the most common complication; rates range from 7%-10%.
Other factors analyzed were the length of hospitalization, blood loss, and functional outcome at follow-up. Overdevest et al. showed no difference in functional or clinical outcome between patients randomly allocated to tubular discectomy and MLD at 5 years of follow-up. Only the length of hospitalization and blood loss were significantly reduced with tubular discectomy [13]. In short, no significant difference was observed between the two procedures in terms of functional outcome, complications, or recurrence rate. Decreased blood loss, lower post-operative analgesic requirement, and early return-to-work can place MIS with a tubular retractor system in an advantageous position compared to classical MLD, though the cost of the tubular retractor system and instruments are high.Moreover, MIS, considered “keyhole surgery”, gives more satisfaction to patients than “open” surgery.
5. Conclusion
There has been a shift from open to keyhole surgery in all fields of surgery. However, the advantages and disadvantages should be carefully analyzed. In our study, comparing MLD and minimally invasive surgery using a tubular retractor system, the functional outcome and complications and recurrence are almost the same. However, less blood loss and less analgesic requirement in the postoperative period are the definite advantages of tube discectomy.
Limitations
Only cases of single-level lumbar disc prolapse were included in the study. The outcome was assessed for up to six months but the long-term outcome should be studied since failures and recurrences may occur later.
Ethical Considerations
Compliance with ethical guidelines
The study was conducted after obtaining approval from the Institutional Research Board and Ethical Committee of Government Medical College Thiruvananthapuram, (IEC No.: 06/20/2017/MCT dated 17/04/2017). Informed written consent was obtained from the participants. Confidentiality was ensured and maintained throughout the study. Complications, when observed, were dealt with accordingly.
Funding
The article was extracted from the MCh in Neurosurgery dissertation submitted to the Kerala University of Health Sciences.
Authors' contributions
Conception, study design, data analysis and interpretation: All authors; Data collection: Raj S Chandran, Arun Sathyababu and Sharmad Mohammed Haneefa; Drafting the article: Raj S Chandran, Arun Sathyababu and Sharmad Mohammed Haneefa; Critically revising the article: Raj S Chandran, Arun Sathyababu and Rajmohan Bhanu Prabhakar; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors wish to express their gratitude to Ajith Nair, the former associate professor of Neurosurgery, Government Medical College Thiruvananthapuram for his help.
References
- Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of the spinal canal. The New England Journal of Medicine. 1934; 211(5):210-5. [Link]
- Caspar W. A new surgical procedure for lumbar disc herniation causing less tissue damage through a microsurgical. Approach. Advances in Neurosurgery 4. Lumbar disc. Adult Hydrocephalus. 1977. [Link]
- Yasargil MG. Microsurgical operations of herniated lumbar disc. In: Wüllenweber R, Brock M, Hamer J, Klinger M, Spoerri O, editors. Adv Neurosurg. Advances in Neurosurgery. Berlin: Springer; 1977. [Link]
- Clark AJ, Safaee MM, Khan NR, Brown MT, Foley KT. Tubular microdiscectomy: Techniques, complication avoidance, and review of the literature. Neurosurgical Focus. 2017; 43(2):E7. [DOI: 10.3171/2017.5.FOCUS17202] [PMID]
- Mittal A, Chandrasekhar A, Mohan R, Rallapalli R, Prasad S. Analysis of the functional outcome of discectomy in lumbar disc prolapse. IOSR Journal of Dental and Medical Sciences. 2015; 14(5):73-80. [Link]
- Knight RQ, Scribani M, Krupa N, Grainger S, Goldberg G, Spivak C, et al. Lumbar Decompressive laminectomy or laminotomy for degenerative conditions: “Outcome comparison of traditional open versus less invasive techniques”. Journal of Spine. 2013; 1-10. [Link]
- German JW, Adamo MA, Hoppenot RG, Blossom JH, Nagle HA. Perioperative results following lumbar discectomy: Comparison of minimally invasive discectomy and standard microdiscectomy. Neurosurgery Focus. 2008; 25(2):E20.[DOI:10.3171/FOC/2008/25/8/E20] [PMID]
- Greiner-Perth R, Böhm H, El Saghir H. Microscopically assisted percutaneous nucleotomy, an alternative minimally invasive procedure for the operative treatment of lumbar disc herniation: Preliminary results. Neurosurgical Review. 2002; 25(4):225-7. [DOI:10.1007/s10143-002-0220-2] [PMID]
- Muramatsu K, Hachiya Y, Morita C. Postoperative magnetic resonance imaging of lumbar disc herniation: Comparison of microendoscopic discectomy and Love’s method. Spine. 2001; 26(14):1599-605. [DOI:10.1097/00007632-200107150-00022] [PMID]
- Brock M, Kunkel P, Papavero L. Lumbar microdiscectomy: Subperiosteal versus transmuscular approach and influence on the early postoperative analgesic consumption. European Spine Journal. 2008; 17(4):518-522.[DOI:10.1007/s00586-008-0604-2] [PMID] [PMCID]
- Ryang YM, Oertel MF, Mayfrank L, Gilsbach JM, Rohde V. Standard open microdiscectomy versus minimal access trocar microdiscectomy: Results of a prospective randomized study. Neurosurgery. 2008; 62(1):174-81.[DOI:10.1227/01.NEU.0000311075.56486.C5] [PMID]
- Teli M, Lovi A, Brayda-Bruno M, Zagra A, Corriero A, Giudici F, et al. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. European Spine Journal. 2010; 19(3):443-50. [DOI:10.1007/s00586-010-1290-4] [PMID] [PMCID]
- Overdevest GM, Peul WC, Brand R, Koes BW, Bartels RH, Tan WF, et al. Tubular discectomy versus conventional microdiscectomy for the treatment of lumbar disc herniation: Long-term results of a randomised controlled trial. Journal of Neurology Neurosurgery & Psychiatry. 2017; 88(12):1008-16. [DOI:10.1136/jnnp-2016-315306] [PMID]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






