Thu, May 2, 2024
Volume 9 - Continuous Publishing
Iran J Neurosurg 2023, 9 - Continuous Publishing: 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rezaei S, Jafroudi M. Emotion Dysregulation Following Traumatic Brain Injury: A Systematic Review. Iran J Neurosurg 2023; 9 : 20
URL: http://irjns.org/article-1-359-en.html
URL: http://irjns.org/article-1-359-en.html
1- Department of Psychology, Faculty of Literature and Humanities, University of Guilan, Rasht, Iran , Rezaei_psy@hotmail.com
2- Department of Psychology, Faculty of Literature and Humanities, University of Guilan, Rasht, Iran
2- Department of Psychology, Faculty of Literature and Humanities, University of Guilan, Rasht, Iran
Full Text [PDF 1566 kb]
(250 Downloads)
| Abstract (HTML) (1091 Views)
Full Text: (305 Views)
1. Introduction
Traumatic brain injury (TBI), known as a “silent epidemic” [1] with an approximate annual incidence rate of 69 million worldwide cases [2], is presumed to be one of the three major causes of injury-related deaths and disabilities by 2030 [3]. According to the Centers for Disease Control and Prevention (CDC), TBI is caused by a bump, blow, or jolt to the head, contusion, or head-penetrating injury, disrupting the normal structure and function of the brain temporarily or permanently [4, 5]. In other words, TBI includes a heterogeneous group of pathologies with various onset mechanisms leading to different adverse outcomes [6] with acute (days to weeks) and chronic (months to years) symptoms [7]. In addition to physical complications caused by TBI, serious outcomes associated with alteration in brain function are disruptions in cognitive, emotional, and behavioral functions needed in both personal life and social life [8]. Accordingly, patients with TBI impose a heavy burden on the healthcare system and economy of societies worldwide [9].
Although acute symptoms are presumed to be caused by a brain injury, computerized tomography (CT) scan or magnetic resonance imaging (MRI) do not show traumatic anomalies in some cases. Even if the anomalies are identified, they present a weak correlation with the intensity of persistent symptoms [10]. Nevertheless, a significant correlation is observed between post-injury outcomes caused by TBI (e.g. neuronal death, white matter damage, and neuroinflammation), emotional response to trauma, and distress caused by physical and psychological symptoms [11]. Regardless of a prior psychological record, the risks of psychological disorders substantially increase after TBI. These disorders, psychological conditions, and related cognitive, behavioral, and emotional outcomes are probably caused by acute and chronic emotional dysregulation resulting from post-traumatic physical or emotional insults [11].
Emotion regulation refers to complex internal and external neuropsychological processes. It is the ability to control, assess, express, and modify affects and emotional responses according to their particular characteristics and time. Hence, to achieve goals, emotion regulation is manifested in individual behavior [12–16]. Modifying the expression of affects and emotions, known as the key element of emotion regulation, is controlled by the prefrontal cortex, which is the main region for emotional cognitive control [17]. Anatomically, forceps minor, uncinate fasciculus, and cingulum bundle are major pathways for white matter, connecting prefrontal and limbic regions in the emotion regulation circuit. Due to their locations at the front of the skull, they are vulnerable to brain injuries [18-20]. Thus, since brain injuries can disrupt emotions leading to persistent symptoms [21], emotional dysregulation is one of the most common and disabling outcomes of TBI [22].
Emotion dysregulation (ED) can exacerbate a wide range of symptoms, including problems in restraining emotions and behaviors (e.g. aggression, inappropriate social behavior, irritability, and impulsivity), executive function disorders (e.g. in problem-solving or purposeful behavior), and diminished emotional awareness and expression (e.g. passivity and indifference) [23, 24]. In other words, the inability to decode feelings in others not only prevents socially-adjusted responses in people with TBI but also disrupts recognizing one’s emotional states as the first stage of appropriate and optimal regulation of emotions [22]. Accordingly, ED can challenge the ability to cope with everyday situations, intensifying disrupted cognitive processes [25]. Moreover, post-TBI recovery is highly affected by a person’s capacity to regulate negative emotions, something which determines the ability to deal with injury consequences (e.g. symptoms or temporary changes in daily performance) [17–19].
With the rising occurrence and prevalence of TBI, healthcare providers increasingly encounter people with TBI following their injury [26]. Despite its clinical importance, many studies have addressed TBI management in medical fields other than psychiatry [27]. Researchers have not sufficiently emphasized the outcomes of ED in people with TBI with limited attention to post-TBI emotional disorders. Thus, this review was performed to analyze the perception of post-TBI emotional dysregulation.
2. Methods and Materials/Patients
The systematic review was conducted according to a predetermined protocol and established guidelines (preferred reporting items for systematic reviews and meta-analyses) [28].
Eligibility criteria
Studies were included if, articles were published in the English language, reported as a completed study, were published from 1997 onward to the first of January 2023, participants had at least 16 years of age (this was done to avoid confounds associated with the development of emotion regulation), and evidence of TBI were determined using one or more of the following methods including Glasgow Coma Scale (GCS), reported the loss of consciousness or evidence of post-traumatic amnesia, clinical or neuroimaging diagnosis.
Studies or papers that did not meet the above criteria were excluded. No geographical limitations were applied. Moreover, study protocols, literature reviews, methodological papers, or conference abstracts were excluded (after conducting additional searches to ensure that full papers had not been subsequently published). Articles not measuring aspects of emotional expression or regulation and longitudinal studies where the sample consisted of participants who were children at the time of TBI were not eligible to enter the study.
Search strategy
The primary search was conducted in December 2022 and an updated search was conducted on February 1, 2023. Titles and abstracts were screened using PubMed, Web of Science, Scopus as well as Google Scholar to comprise two concepts of TBI and emotion regulation. Moreover, a manual search of the articles or reference lists was performed to identify either keywords or keyword combinations. The following keywords or MeSH terms (medical subject headings) were used to search the database, emotional regulation, emotions, brain injuries, and TBI. Moreover, the subject-specific keywords [TBI OR traumatic brain injury OR head trauma OR brain trauma OR contusion OR brain injuries] AND [emotional affect OR emotion regulation, OR positive affect OR negative affect or positive mood or negative mood OR emotional expression OR emotional problem OR emotional dysregulation OR emotions] were combined separately to help identify relevant papers.
The completed search results were downloaded into Endnote X9 (Clarivate, USA) for citation management and deduplication. Screening was done in a web-based screening program, called Rayyan QCRI intelligent systematic review [29]. Rayyan (Rayyan Systems, Inc., USA) allows abstract and full-text screening of studies depending on custom inclusion and exclusion criteria. Duplicate reports were initially eliminated; then, studies were screened based on title and abstract only using the inclusion/exclusion criteria outlined in the previous section. Moreover, studies that were borderline for inclusion were more thoroughly screened by examining their full text. In addition, the reference lists of the studies were checked for any related studies that were not picked up by the search. In the initial step, both reviewers screened all references by title and abstract and then retained suitable articles. Then the full-text manuscripts of papers that remained after abstract screening were assessed for eligibility by the reviewers. While the final articles were identified for inclusion, the extraction of relevant data was conducted by both reviewers autonomously. If any discrepancies existed at each section of the review proceeding, they were resolved through consensus.
Data extraction
Table 1 presents the information extracted from each paper.

3. Results
A total of 773 articles were identified, 305 from Google Scholar, 193 from PubMed, 171 from Web of Science, and 88 from Scopus. After removing the duplicate studies, 361 studies remained and the abstracts were carefully screened and evaluated. Of these, 303 were excluded (16 were non-English articles; 88 included another type of brain injury; 145 did not measure emotional regulation; 54 were conference abstracts) (Figure 1).
Traumatic brain injury (TBI), known as a “silent epidemic” [1] with an approximate annual incidence rate of 69 million worldwide cases [2], is presumed to be one of the three major causes of injury-related deaths and disabilities by 2030 [3]. According to the Centers for Disease Control and Prevention (CDC), TBI is caused by a bump, blow, or jolt to the head, contusion, or head-penetrating injury, disrupting the normal structure and function of the brain temporarily or permanently [4, 5]. In other words, TBI includes a heterogeneous group of pathologies with various onset mechanisms leading to different adverse outcomes [6] with acute (days to weeks) and chronic (months to years) symptoms [7]. In addition to physical complications caused by TBI, serious outcomes associated with alteration in brain function are disruptions in cognitive, emotional, and behavioral functions needed in both personal life and social life [8]. Accordingly, patients with TBI impose a heavy burden on the healthcare system and economy of societies worldwide [9].
Although acute symptoms are presumed to be caused by a brain injury, computerized tomography (CT) scan or magnetic resonance imaging (MRI) do not show traumatic anomalies in some cases. Even if the anomalies are identified, they present a weak correlation with the intensity of persistent symptoms [10]. Nevertheless, a significant correlation is observed between post-injury outcomes caused by TBI (e.g. neuronal death, white matter damage, and neuroinflammation), emotional response to trauma, and distress caused by physical and psychological symptoms [11]. Regardless of a prior psychological record, the risks of psychological disorders substantially increase after TBI. These disorders, psychological conditions, and related cognitive, behavioral, and emotional outcomes are probably caused by acute and chronic emotional dysregulation resulting from post-traumatic physical or emotional insults [11].
Emotion regulation refers to complex internal and external neuropsychological processes. It is the ability to control, assess, express, and modify affects and emotional responses according to their particular characteristics and time. Hence, to achieve goals, emotion regulation is manifested in individual behavior [12–16]. Modifying the expression of affects and emotions, known as the key element of emotion regulation, is controlled by the prefrontal cortex, which is the main region for emotional cognitive control [17]. Anatomically, forceps minor, uncinate fasciculus, and cingulum bundle are major pathways for white matter, connecting prefrontal and limbic regions in the emotion regulation circuit. Due to their locations at the front of the skull, they are vulnerable to brain injuries [18-20]. Thus, since brain injuries can disrupt emotions leading to persistent symptoms [21], emotional dysregulation is one of the most common and disabling outcomes of TBI [22].
Emotion dysregulation (ED) can exacerbate a wide range of symptoms, including problems in restraining emotions and behaviors (e.g. aggression, inappropriate social behavior, irritability, and impulsivity), executive function disorders (e.g. in problem-solving or purposeful behavior), and diminished emotional awareness and expression (e.g. passivity and indifference) [23, 24]. In other words, the inability to decode feelings in others not only prevents socially-adjusted responses in people with TBI but also disrupts recognizing one’s emotional states as the first stage of appropriate and optimal regulation of emotions [22]. Accordingly, ED can challenge the ability to cope with everyday situations, intensifying disrupted cognitive processes [25]. Moreover, post-TBI recovery is highly affected by a person’s capacity to regulate negative emotions, something which determines the ability to deal with injury consequences (e.g. symptoms or temporary changes in daily performance) [17–19].
With the rising occurrence and prevalence of TBI, healthcare providers increasingly encounter people with TBI following their injury [26]. Despite its clinical importance, many studies have addressed TBI management in medical fields other than psychiatry [27]. Researchers have not sufficiently emphasized the outcomes of ED in people with TBI with limited attention to post-TBI emotional disorders. Thus, this review was performed to analyze the perception of post-TBI emotional dysregulation.
2. Methods and Materials/Patients
The systematic review was conducted according to a predetermined protocol and established guidelines (preferred reporting items for systematic reviews and meta-analyses) [28].
Eligibility criteria
Studies were included if, articles were published in the English language, reported as a completed study, were published from 1997 onward to the first of January 2023, participants had at least 16 years of age (this was done to avoid confounds associated with the development of emotion regulation), and evidence of TBI were determined using one or more of the following methods including Glasgow Coma Scale (GCS), reported the loss of consciousness or evidence of post-traumatic amnesia, clinical or neuroimaging diagnosis.
Studies or papers that did not meet the above criteria were excluded. No geographical limitations were applied. Moreover, study protocols, literature reviews, methodological papers, or conference abstracts were excluded (after conducting additional searches to ensure that full papers had not been subsequently published). Articles not measuring aspects of emotional expression or regulation and longitudinal studies where the sample consisted of participants who were children at the time of TBI were not eligible to enter the study.
Search strategy
The primary search was conducted in December 2022 and an updated search was conducted on February 1, 2023. Titles and abstracts were screened using PubMed, Web of Science, Scopus as well as Google Scholar to comprise two concepts of TBI and emotion regulation. Moreover, a manual search of the articles or reference lists was performed to identify either keywords or keyword combinations. The following keywords or MeSH terms (medical subject headings) were used to search the database, emotional regulation, emotions, brain injuries, and TBI. Moreover, the subject-specific keywords [TBI OR traumatic brain injury OR head trauma OR brain trauma OR contusion OR brain injuries] AND [emotional affect OR emotion regulation, OR positive affect OR negative affect or positive mood or negative mood OR emotional expression OR emotional problem OR emotional dysregulation OR emotions] were combined separately to help identify relevant papers.
The completed search results were downloaded into Endnote X9 (Clarivate, USA) for citation management and deduplication. Screening was done in a web-based screening program, called Rayyan QCRI intelligent systematic review [29]. Rayyan (Rayyan Systems, Inc., USA) allows abstract and full-text screening of studies depending on custom inclusion and exclusion criteria. Duplicate reports were initially eliminated; then, studies were screened based on title and abstract only using the inclusion/exclusion criteria outlined in the previous section. Moreover, studies that were borderline for inclusion were more thoroughly screened by examining their full text. In addition, the reference lists of the studies were checked for any related studies that were not picked up by the search. In the initial step, both reviewers screened all references by title and abstract and then retained suitable articles. Then the full-text manuscripts of papers that remained after abstract screening were assessed for eligibility by the reviewers. While the final articles were identified for inclusion, the extraction of relevant data was conducted by both reviewers autonomously. If any discrepancies existed at each section of the review proceeding, they were resolved through consensus.
Data extraction
Table 1 presents the information extracted from each paper.

3. Results
A total of 773 articles were identified, 305 from Google Scholar, 193 from PubMed, 171 from Web of Science, and 88 from Scopus. After removing the duplicate studies, 361 studies remained and the abstracts were carefully screened and evaluated. Of these, 303 were excluded (16 were non-English articles; 88 included another type of brain injury; 145 did not measure emotional regulation; 54 were conference abstracts) (Figure 1).
A final 58 studies were retrieved for full-text screening. Of these, 24 were excluded because, after further review, it was determined that they did not include or report emotion regulation assessment and that the participants did not have traumatic brain injuries. Finally, 34 studies were included in this review.
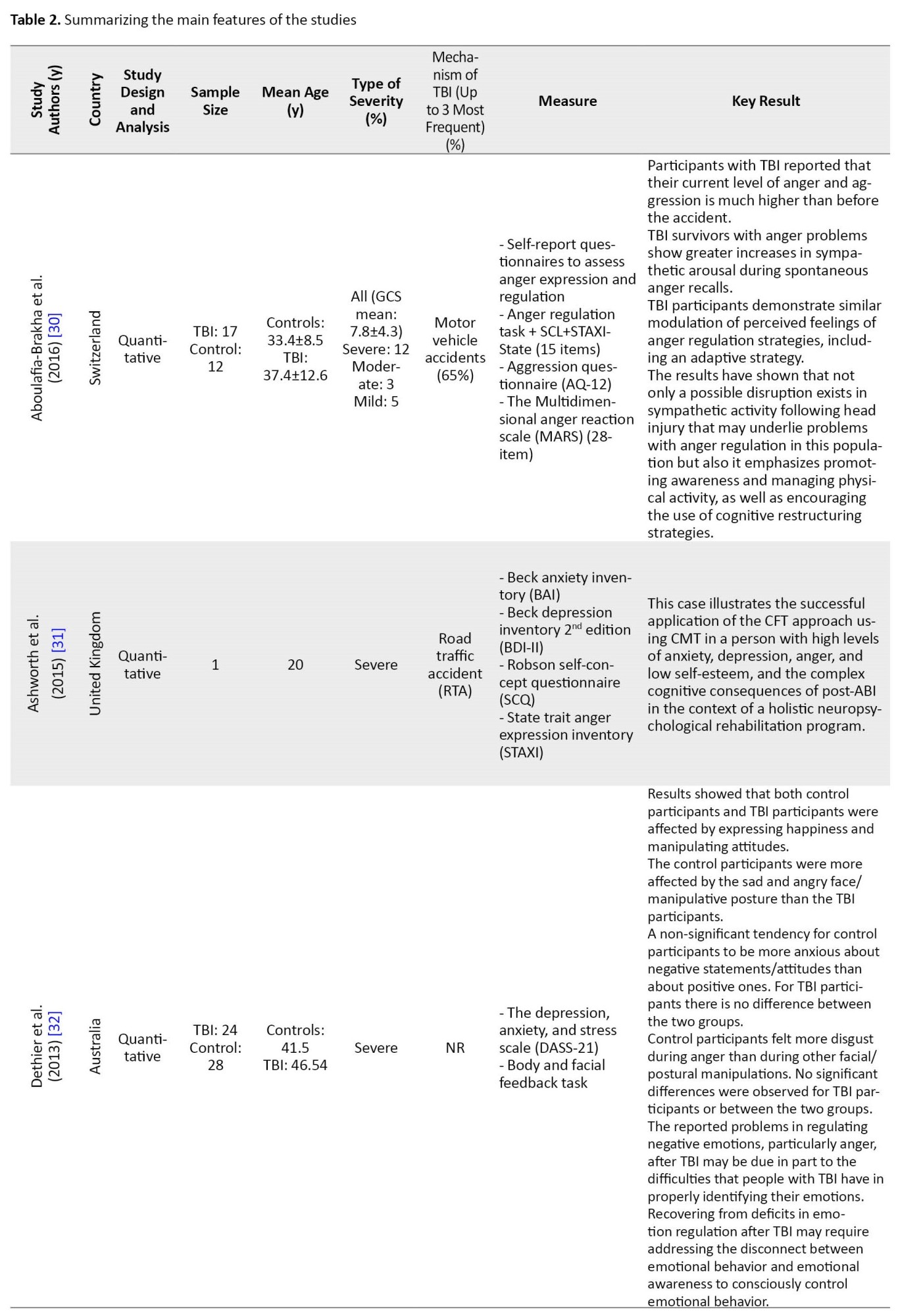
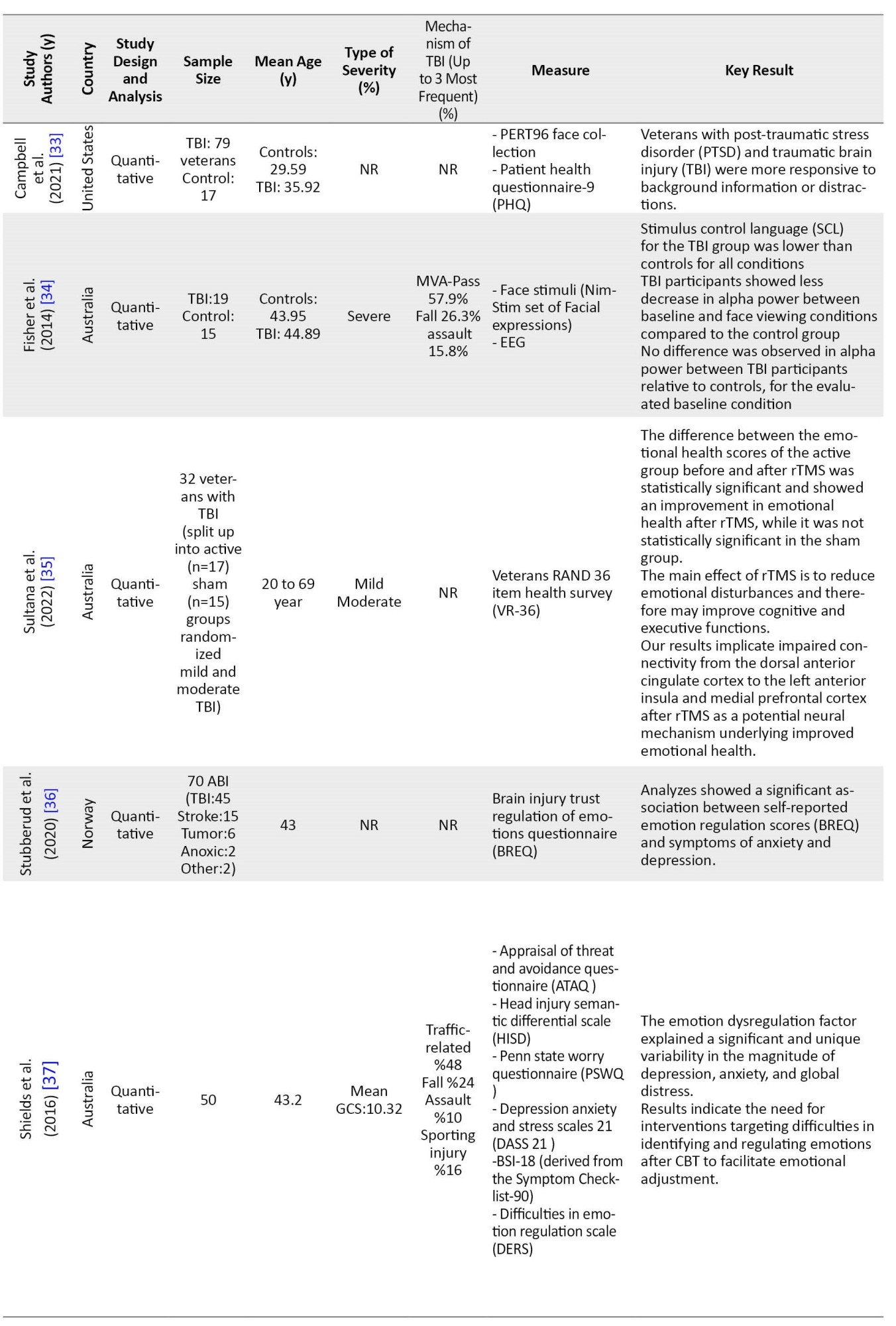
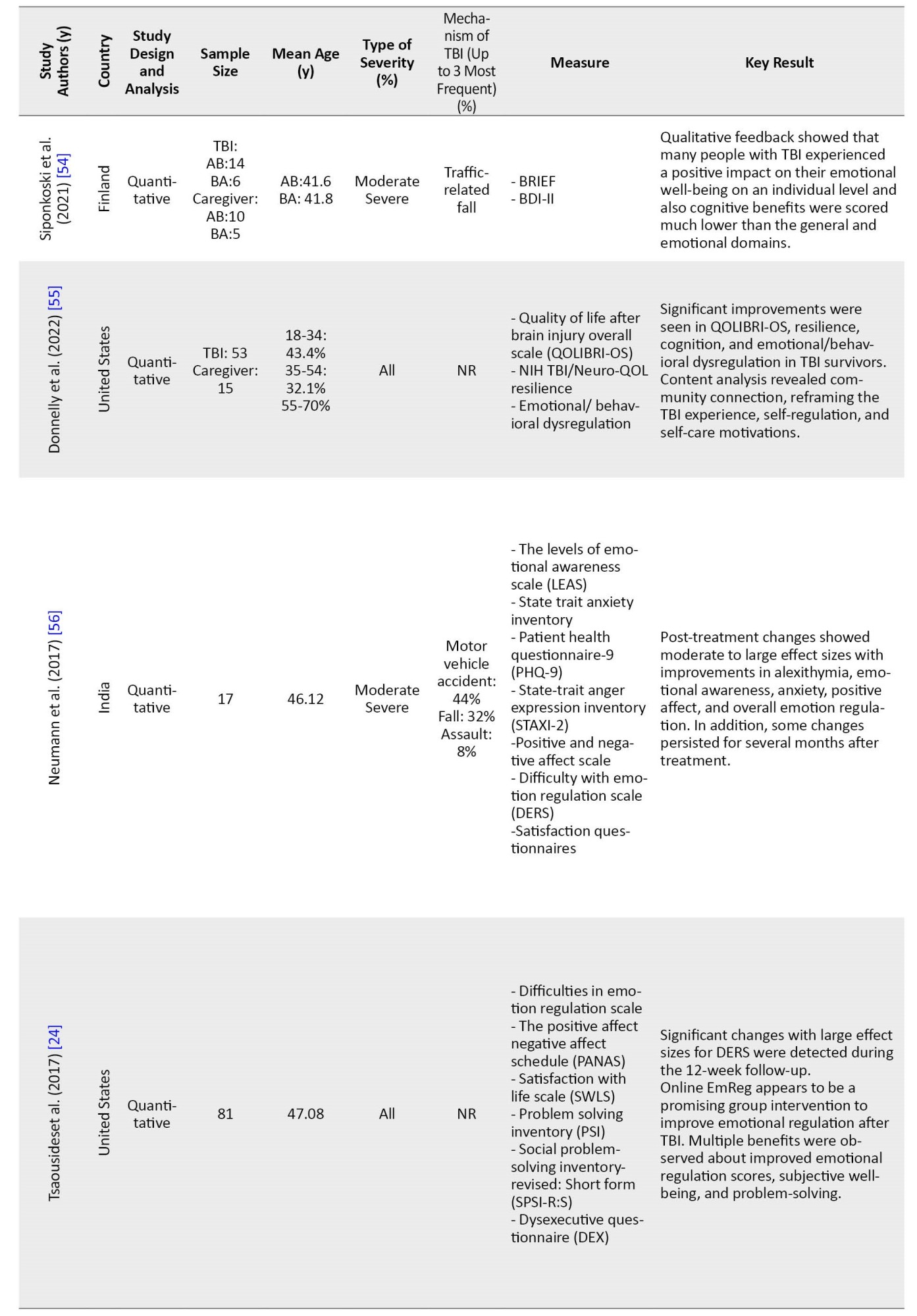
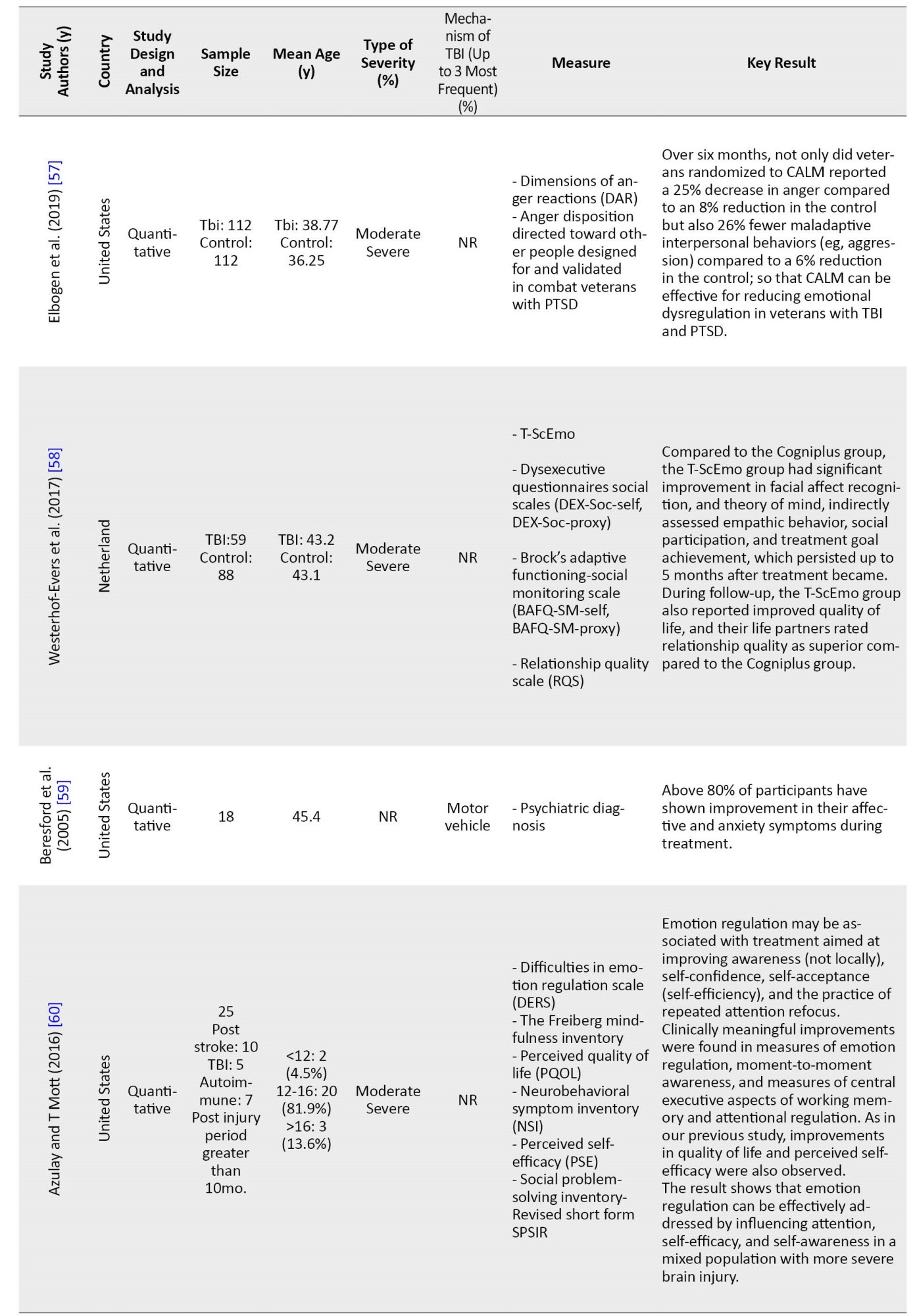
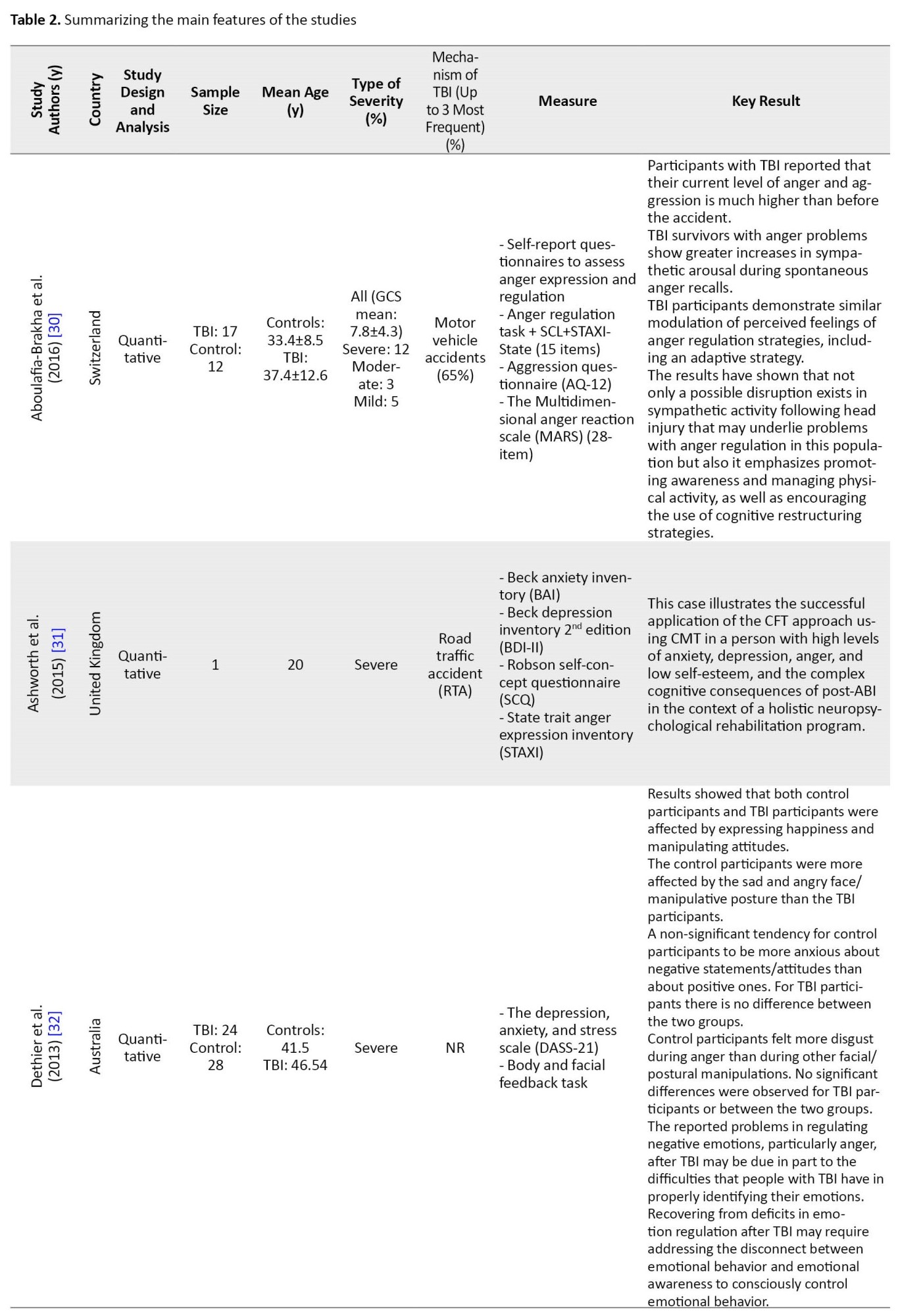
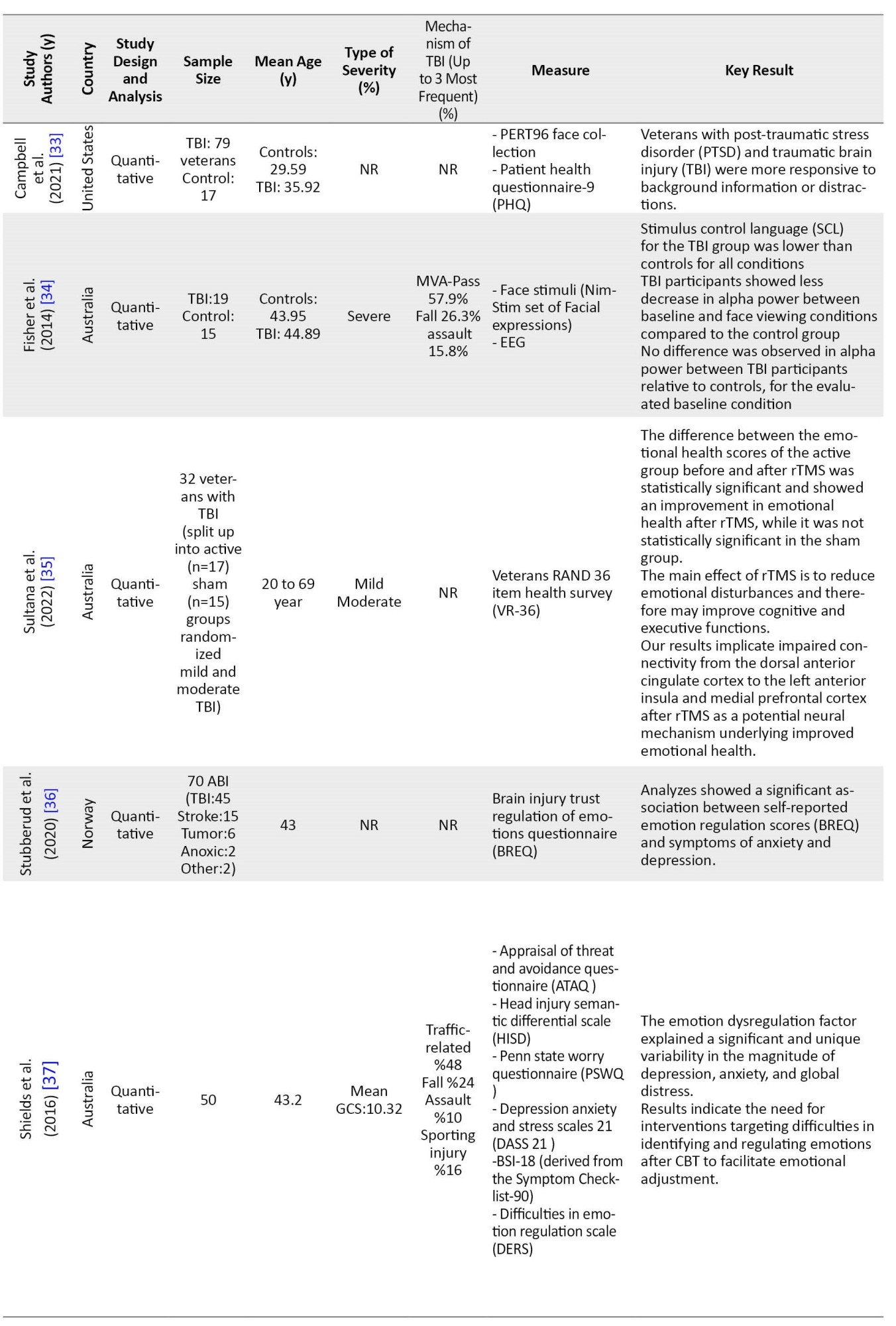
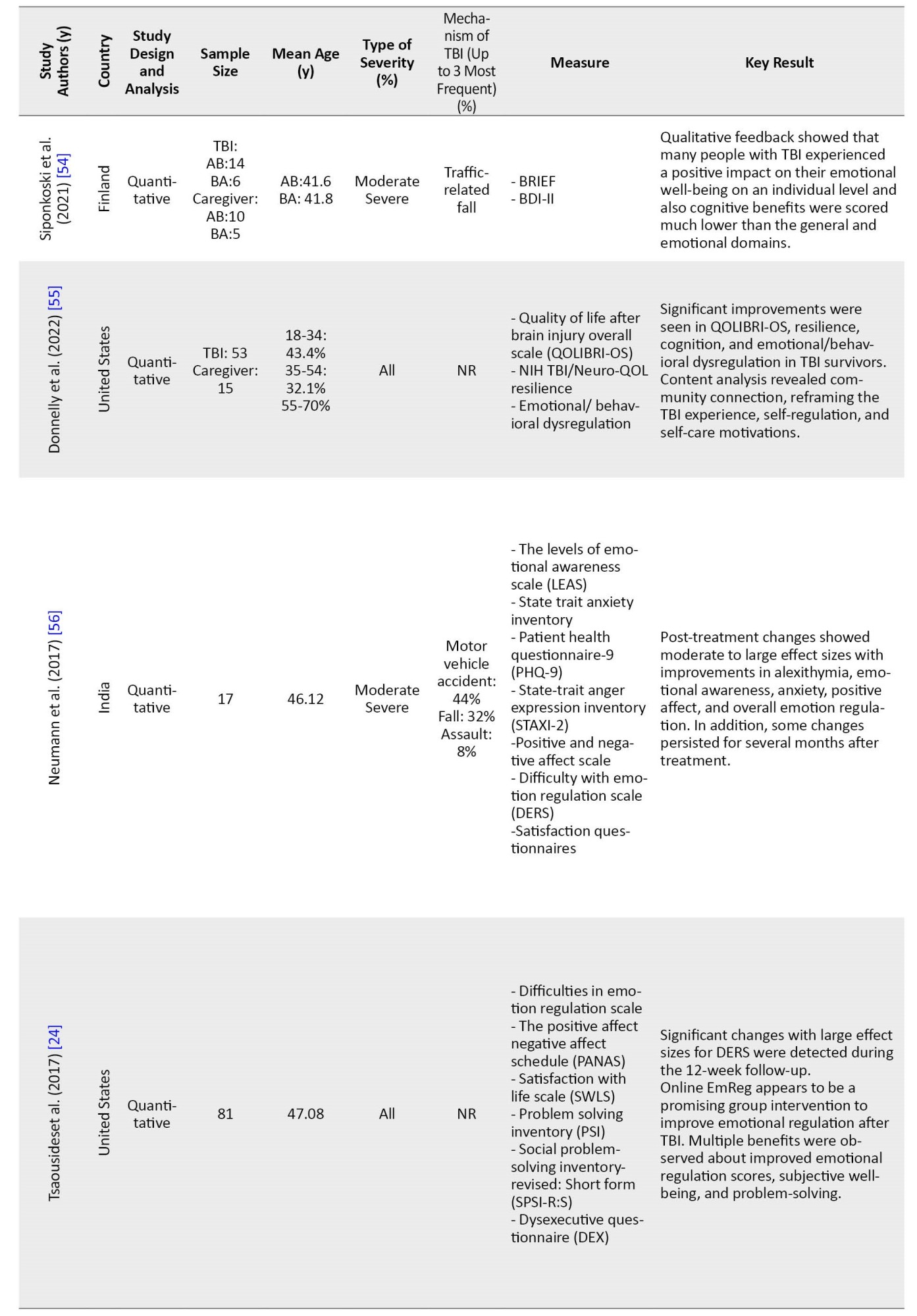
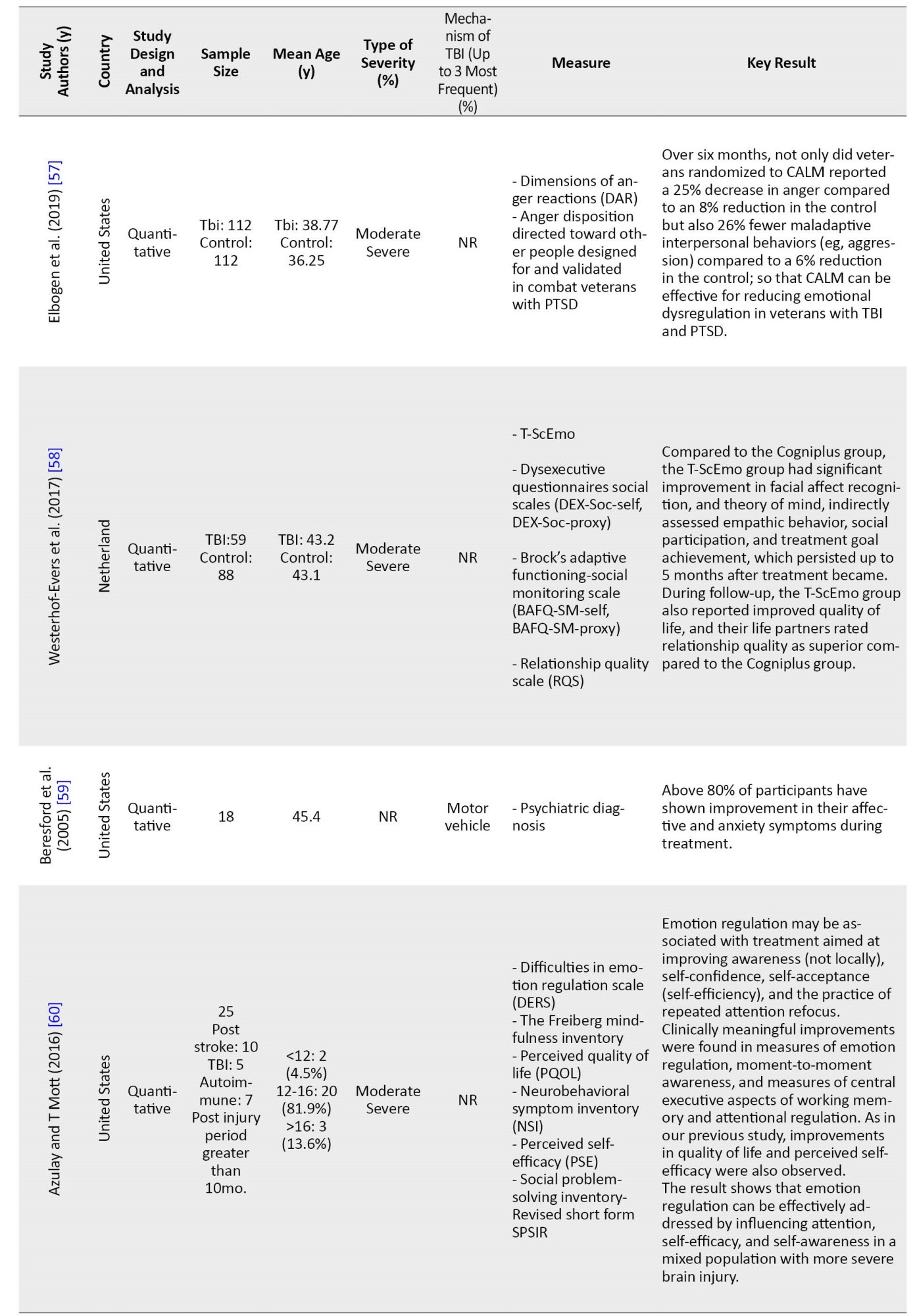
Table 2 presents the main features of the studies included in the systematic review.





Moreover, the pooled sample size was 2676, and the individual sample size varied from 1 to 636 in different studies. In addition, 23 studies (93%) were published between 2013 and 2023. Another 2 studies (7%) were published before 2010 (Figure 2).
Table 2 presents the main features of the studies included in the systematic review.





Moreover, the pooled sample size was 2676, and the individual sample size varied from 1 to 636 in different studies. In addition, 23 studies (93%) were published between 2013 and 2023. Another 2 studies (7%) were published before 2010 (Figure 2).
The countries in which the studies were conducted were geographically dispersed, 15 studies were conducted in the United States (41%) and 1 study was conducted in Europe, specifically 1 in the United Kingdom (2%), 4 in the Netherlands (11%), 2 in Norway (5%), 1 in Finland (2%), and 1 in Switzerland (2%). Five studies were conducted in Asia, 3 in Iran (8%), 1 in Korea (2%), 1 in India (2%), and 5 in Australia (14%). Moreover, TBI severity prevalence in the studies used in our research is reported as follows, 8 studies included a mixed sample of spectrum of TBI (mild, moderate, and severe) (23%). Four studies included severe types of traumatic brain injuries (10%). Three studies included mild types of traumatic brain injuries (8%). Seven studies included moderate and severe types of traumatic brain injuries (20%). One study included moderate and mild types of traumatic brain injuries (2%).
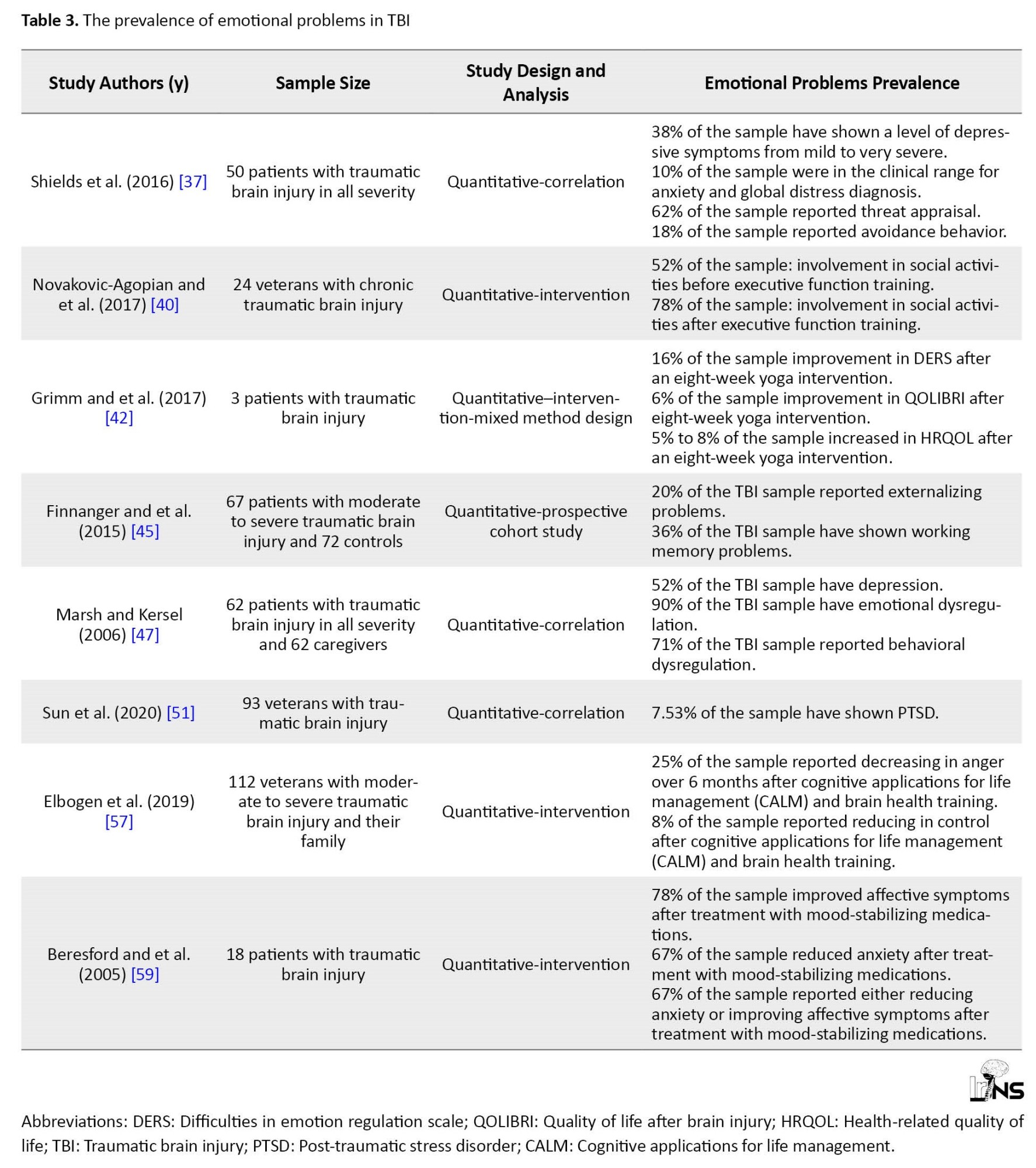
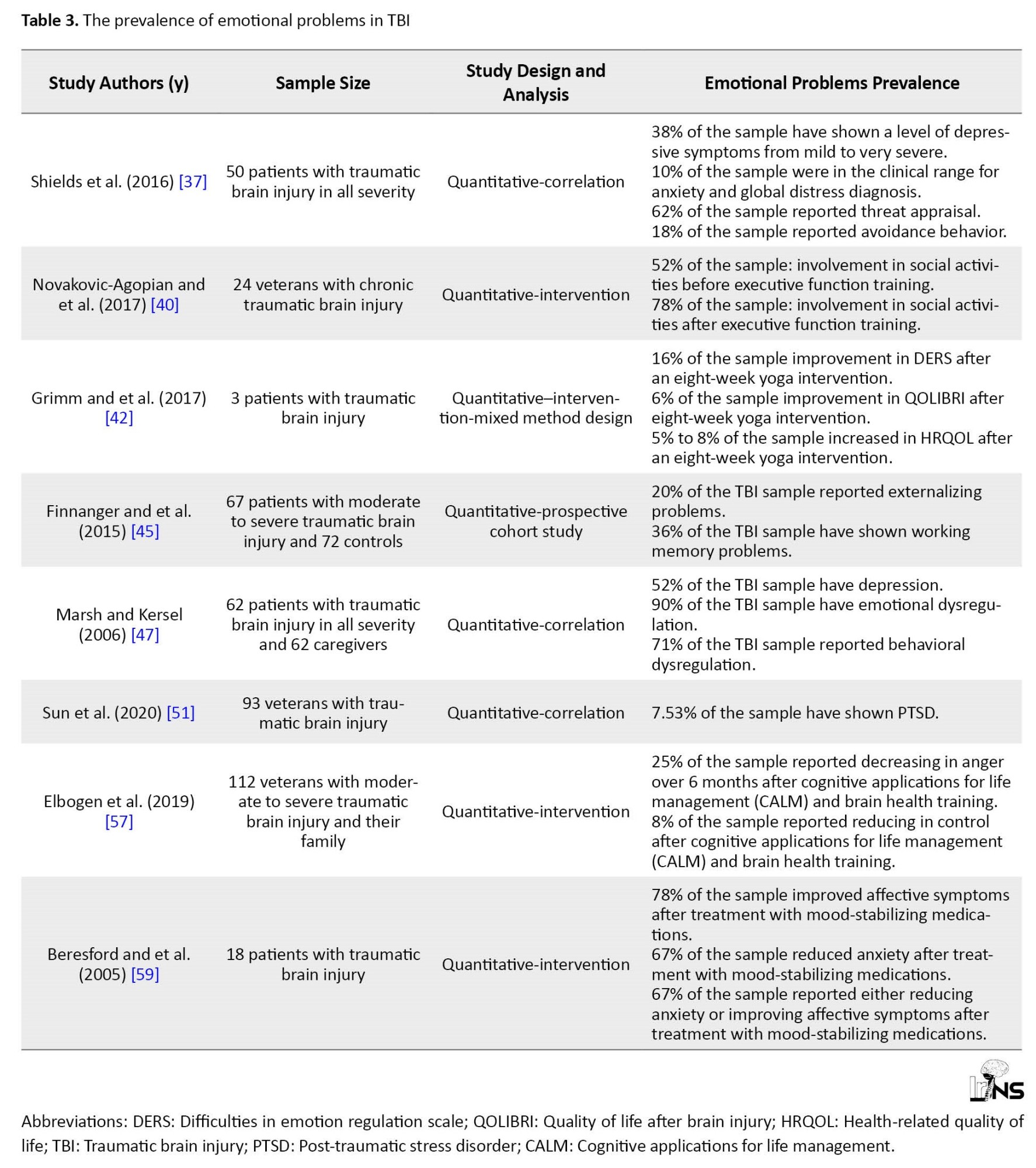
A total of 17 studies included TBI survivors and their caregivers, families, or the control healthy group (50%). Two studies included a mixed sample of brain injuries (e.g. TBI, stroke, autoimmune, and others) (5%). Furthermore, Table 3 presents the prevalence of emotional problems and their consequences in people with TBI.
4. Discussion
This study was conducted to systematically review the existing studies on emotion regulation in people with TBI. The results indicated that patients with TBI report persistent problems associated with mood disorders and ED following their injury [43, 50]. The evidence indicated that people with TBI dedicate more mental and physiological resources to preserve stable cognitive functioning over time due to their cognitive, social, and behavioral problems in daily life [44, 47, 57]. This can lead to mood disorders [43] because patients may experience difficulties in controlling their emotions despite normal CT scan results, even until 6 months after the injuries [49]. Thus, increased psychological disorders can reduce social activities, and ultimately further pressure on the health care system, society, and the patient’s family [62].
Neuroimaging studies have also shown that different cortical and subcortical regions are involved in emotion regulation processes [63]. Numerous TBI-caused molecular and cellular alterations in subcortical structures, including the amygdala and hippocampus [64] and consequently, disruption in regulating the hypothalamic-pituitary-adrenal (HPA) axis can lead to problems in the adaptive response to stress [65]. Over time, this unnatural response to stress can be correlated with post-TBI neuroinflammation and acute psychological and neurological outcomes [65]. In this regard, disrupted neural circuits, including the insular cortex and amygdala prompt compensatory and unusual functional relations of the remaining neural structures and arousal [34]. As a result, amygdala activity escalates in these patients due to emotional reactions, such as stress and anxiety [35, 51].
Previous studies have reported higher physiological arousal during anger expression in people with TBI compared to normal people [30, 37, 41]. According to Scherer’s emotion appraisal theory, emotional responses to internal and external events are manifested through physiological and cognitive appraisal processes [67]. Since the activation of the sympathetic system can substantially affect the cognitive and behavioral manifestations of anger [30], this pattern of response can be a sign of disruptions in the activity of the autonomic nervous system following TBI and may result from injury to the prefrontal cortex and limbic system structures [39, 52, 57]. In this regard, studies have reported that frontal lobe vulnerability [18-20, 52] and prefrontal cortex and posterior cingulate cortex (as well as precuneus) dysfunction cause psychological and mood disorders [46]. So that people with TBI show symptoms of ED in the form of depression and anxiety [36, 45, 46, 48, 56], which can affect their recovery from trauma [49].
Furthermore, interpersonal differences in coping styles can influence the continuation of post-injury mood complaints [68]. People with TBI experience more problems in processing emotional reactions to negative facial emotional signs compared to others’ positive facial emotional signs [32, 49]. This reduces their ability to imitate negative faces andautonomous reactions to negative faces, recognize negative faces [69], and control negative emotions [49].
Moreover, disruptions in higher-level cognitive functions (e.g. response inhibition and cognitive flexibility), following TBI, possibly imperil impulse control and reevaluation of emotional events [37]. When patients experience more negative effects, they face amplified problems, such as loss of concentration in purposeful activities [70] and problem-solving with diminished flexibility to manage these emotions. The intensity of these changes depends on a patient’s ability to organize affects and show flexibility in utilizing their potential [49]. Since emotional knowledge has a crucial role in emotion regulation [71] and people with TBI experience problems in recognizing and processing unconscious emotions (physiological or bodily affects) and conscious affects, they encounter difficulties in regulating their emotions [32].
5. Conclusion
Although the recovery in clinical and medical care has significantly reduced TBI-related fatality [72], long-term outcomes associated with post-injury emotional and mental distress and dysregulation have rarely been analyzed in terms of TBI treatment. The nature of brain injury is very complicated, and effective factors, such as demographic, biological, medical, and psychological aspects should not be neglected [49]. ED notably contributes to TBI-caused outcomes, and research is yet to determine whether physical injuries continue mental symptoms or vice versa. Therefore, medical and clinical psychology care should be equally considered for people with TBI, and a more comprehensive approach can be adapted to treat people with TBI and improve their quality of life.
Limitation
The first limitation of this study was the absence of divided groups in terms of TBI severity (mild/moderate/severe). Moreover, because mild traumatic injuries (mTBIs) are more prevalent than other TBIs worldwide, it is essential to analyze the effects of mTBI on emotional dysregulation. Accordingly, future studies are recommended to use standardized TBI intensity measures and report the correlation between intensity and performance at individual levels. Such an approach can be more helpful in determining the existence of a correlation between TBI intensity and emotion recognition disorder. Furthermore, it is recommended to design and test intervention protocols in the form of randomized clinical trials to resolve post-TBI emotional dysregulation. A main limitation of this study is that no gold standard for diagnosing emotional dysregulation existed, in other words, it included a spectrum of emotional problems in this study. Although the findings showed the existence of post-TBI emotional dysregulation, this study cannot accurately confirm whether TBI exclusively leads to ED or whether other problems following TBI may cause dysregulation. Hence, future studies can help develop certain interventions and rehabilitation methods by utilizing general diagnostic criteria while assessing ED. Moreover, since pre-morbidity disorders were not considered in this study, it is recommended to emphasize pre-morbidities in future studies.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Biomedical Research Ethics Committee of University of Guilan (Code: IR.GUILAN.REC.1400.038). All patients participating in this study filled out the written informed consent form.
Funding
This study was funded by the Department of Psychology, Faculty of Literature and Humanities, University of Guilan.
Authors' contributions
Conception and design: Sajjad Rezaei; Data collection: Maryam Jafroudi; Data analysis, data interpretation and critically revising the article: Maryam Jafroudi and Sajjad Rezaei; Drafting the article: Maryam Jafroudi; Review and final approval: Sajjad Rezaei.
Conflict of interest
The authors declared no conflict of interest.
References
A total of 17 studies included TBI survivors and their caregivers, families, or the control healthy group (50%). Two studies included a mixed sample of brain injuries (e.g. TBI, stroke, autoimmune, and others) (5%). Furthermore, Table 3 presents the prevalence of emotional problems and their consequences in people with TBI.
4. Discussion
This study was conducted to systematically review the existing studies on emotion regulation in people with TBI. The results indicated that patients with TBI report persistent problems associated with mood disorders and ED following their injury [43, 50]. The evidence indicated that people with TBI dedicate more mental and physiological resources to preserve stable cognitive functioning over time due to their cognitive, social, and behavioral problems in daily life [44, 47, 57]. This can lead to mood disorders [43] because patients may experience difficulties in controlling their emotions despite normal CT scan results, even until 6 months after the injuries [49]. Thus, increased psychological disorders can reduce social activities, and ultimately further pressure on the health care system, society, and the patient’s family [62].
Neuroimaging studies have also shown that different cortical and subcortical regions are involved in emotion regulation processes [63]. Numerous TBI-caused molecular and cellular alterations in subcortical structures, including the amygdala and hippocampus [64] and consequently, disruption in regulating the hypothalamic-pituitary-adrenal (HPA) axis can lead to problems in the adaptive response to stress [65]. Over time, this unnatural response to stress can be correlated with post-TBI neuroinflammation and acute psychological and neurological outcomes [65]. In this regard, disrupted neural circuits, including the insular cortex and amygdala prompt compensatory and unusual functional relations of the remaining neural structures and arousal [34]. As a result, amygdala activity escalates in these patients due to emotional reactions, such as stress and anxiety [35, 51].
Previous studies have reported higher physiological arousal during anger expression in people with TBI compared to normal people [30, 37, 41]. According to Scherer’s emotion appraisal theory, emotional responses to internal and external events are manifested through physiological and cognitive appraisal processes [67]. Since the activation of the sympathetic system can substantially affect the cognitive and behavioral manifestations of anger [30], this pattern of response can be a sign of disruptions in the activity of the autonomic nervous system following TBI and may result from injury to the prefrontal cortex and limbic system structures [39, 52, 57]. In this regard, studies have reported that frontal lobe vulnerability [18-20, 52] and prefrontal cortex and posterior cingulate cortex (as well as precuneus) dysfunction cause psychological and mood disorders [46]. So that people with TBI show symptoms of ED in the form of depression and anxiety [36, 45, 46, 48, 56], which can affect their recovery from trauma [49].
Furthermore, interpersonal differences in coping styles can influence the continuation of post-injury mood complaints [68]. People with TBI experience more problems in processing emotional reactions to negative facial emotional signs compared to others’ positive facial emotional signs [32, 49]. This reduces their ability to imitate negative faces andautonomous reactions to negative faces, recognize negative faces [69], and control negative emotions [49].
Moreover, disruptions in higher-level cognitive functions (e.g. response inhibition and cognitive flexibility), following TBI, possibly imperil impulse control and reevaluation of emotional events [37]. When patients experience more negative effects, they face amplified problems, such as loss of concentration in purposeful activities [70] and problem-solving with diminished flexibility to manage these emotions. The intensity of these changes depends on a patient’s ability to organize affects and show flexibility in utilizing their potential [49]. Since emotional knowledge has a crucial role in emotion regulation [71] and people with TBI experience problems in recognizing and processing unconscious emotions (physiological or bodily affects) and conscious affects, they encounter difficulties in regulating their emotions [32].
5. Conclusion
Although the recovery in clinical and medical care has significantly reduced TBI-related fatality [72], long-term outcomes associated with post-injury emotional and mental distress and dysregulation have rarely been analyzed in terms of TBI treatment. The nature of brain injury is very complicated, and effective factors, such as demographic, biological, medical, and psychological aspects should not be neglected [49]. ED notably contributes to TBI-caused outcomes, and research is yet to determine whether physical injuries continue mental symptoms or vice versa. Therefore, medical and clinical psychology care should be equally considered for people with TBI, and a more comprehensive approach can be adapted to treat people with TBI and improve their quality of life.
Limitation
The first limitation of this study was the absence of divided groups in terms of TBI severity (mild/moderate/severe). Moreover, because mild traumatic injuries (mTBIs) are more prevalent than other TBIs worldwide, it is essential to analyze the effects of mTBI on emotional dysregulation. Accordingly, future studies are recommended to use standardized TBI intensity measures and report the correlation between intensity and performance at individual levels. Such an approach can be more helpful in determining the existence of a correlation between TBI intensity and emotion recognition disorder. Furthermore, it is recommended to design and test intervention protocols in the form of randomized clinical trials to resolve post-TBI emotional dysregulation. A main limitation of this study is that no gold standard for diagnosing emotional dysregulation existed, in other words, it included a spectrum of emotional problems in this study. Although the findings showed the existence of post-TBI emotional dysregulation, this study cannot accurately confirm whether TBI exclusively leads to ED or whether other problems following TBI may cause dysregulation. Hence, future studies can help develop certain interventions and rehabilitation methods by utilizing general diagnostic criteria while assessing ED. Moreover, since pre-morbidity disorders were not considered in this study, it is recommended to emphasize pre-morbidities in future studies.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Biomedical Research Ethics Committee of University of Guilan (Code: IR.GUILAN.REC.1400.038). All patients participating in this study filled out the written informed consent form.
Funding
This study was funded by the Department of Psychology, Faculty of Literature and Humanities, University of Guilan.
Authors' contributions
Conception and design: Sajjad Rezaei; Data collection: Maryam Jafroudi; Data analysis, data interpretation and critically revising the article: Maryam Jafroudi and Sajjad Rezaei; Drafting the article: Maryam Jafroudi; Review and final approval: Sajjad Rezaei.
Conflict of interest
The authors declared no conflict of interest.
References
- Dewan MC, Rattani A, Gupta S, Baticulon RE, Hung YC, Punchak M, et al. Estimating the global incidence of traumatic brain injury. Journal of Neurosurgery. 2018; 130(4):1080-97. [DOI:10.3171/2017.10.JNS17352] [PMID]
- Herrero Babiloni A, Exposto FG, Bouferguene Y, Costa Y, Lavigne GJ, Arbour C. Temporomandibular disorders in traumatic brain injury patients: A chronic pain condition requiring further attention. Pain Medicine. 2020; 21(12):3260-2. Available [DOI:10.1093/pm/pnaa234] [PMID]
- Maas AIR, Menon DK, Manley GT, Abrams M, Åkerlund C, Andelic N, et al. Traumatic brain injury: Progress and challenges in prevention, clinical care, and research. The Lancet. Neurology. 2022; ;21(11):1004-60. [DOI:10.1016/S1474-4422(22)00309-X] [PMID]
- Peterson AB, Xu L, Daugherty J, Breiding MJ. Control and prevention surveillance report of traumatic brain injury-related emergency department visits, hospitalizations, and deaths. Atlanta: Centers for Disease Control and Prevention; 2014. [Link]
- Kline AE, Leary JB, Radabaugh HL, Cheng JP, Bondi CO. Combination therapies for neurobehavioral and cognitive recovery after experimental traumatic brain injury: Is more better? Progress in Neurobiology. 2016; 142:45-67. [DOI:10.1016/j.pneurobio.2016.05.002] [PMID] [PMCID]
- Crupi R, Cordaro M, Cuzzocrea S, Impellizzeri D. Management of traumatic brain injury: From present to future. Antioxidants. 2020; 9(4):297. [DOI:10.3390/antiox9040297] [PMID] [PMCID]
- National Institute of Neurological Disorders and Stroke. Traumatic brain injury information. Maryland: National Institute of Neurological Disorders and Stroke; 2019. [Link]
- Padgett CR, Summers MJ, Vickers JC, McCormack GH, Skilbeck CE. Exploring the effect of the apolipoprotein E (APOE) gene on executive function, working memory, and processing speed during the early recovery period following traumatic brain injury. Journal of Clinical and Experimental Neuropsychology. 2016; 38(5):551-60. [DOI:10.1080/13803395.2015.1137557] [PMID]
- van der Horn HJ, Out ML, de Koning ME, Mayer AR, Spikman JM, Sommer IE, et al. An integrated perspective linking physiological and psychological consequences of mild traumatic brain injury. Journal of Neurology. 2020; 267(9):2497-506. [DOI:10.1007/s00415-019-09335-8] [PMID] [PMCID]
- van der Horn HJ, de Haan S, Spikman JM, de Groot JC, van der Naalt J. Clinical relevance of microhemorrhagic lesions in subacute mild trau matic brain injury. Brain Imaging and Behavio. 2018; 12(3):912-6. [DOI:10.1007/s11682-017-9743-6] [PMID] [PMCID]
- Weis CN, Webb EK, deRoon-Cassini TA, Larson CL. Emotion dysregulation following trauma: Shared neurocircuitry of traumatic brain injury and trauma-related psychiatric disorders. Biological Psychiatry. 2022; 91(5):470-7. [DOI:10.1016/j.biopsych.2021.07.023] [PMID] [PMCID]
- Fitzgerald JM, DiGangi JA, Phan KL. Functional neuroanatomy of emotion and its regulation in PTSD. Harvard Review of Psychiatry. 2018; 26(3):116-28. [DOI:10.1097/HRP.0000000000000185] [PMID] [PMCID]
- Gross JJ. The emerging field of emotion regulation: An integrative review. Review of General Psychology. 1998; 2(3):271-99. [DOI:10.1037/1089-2680.2.3.271]
- Thompson RA. Emotion regulation: A theme in search of definition. The Development of Emotion Regulation: Biological and Behavioral Considerations. 1994; 59(2/3):25-52. [Link]
- Campos JJ, Frankel CB, Camras L. On the nature of emotion regulation. Child Development.2004; 75(2):377-94. [DOI:10.1111/j.1467-8624.2004.00681.x] [PMID]
- Brandão T, Tavares R, Schulz MS, Matos PM. Measuring emotion regulation and emotional expression in breast cancer patients: A systematic review. Clinical Psychology Review. 2016; 43:114-27. [DOI:10.1016/j.cpr.2015.10.002] [PMID]
- Ochsner KN, Silvers JA, Buhle JT. Functional imaging studies of emotion regulation: A synthetic review and evolving model of the cognitive control of emotion. Annals of The New York Academy of Sciences. 2012; 1251:E1-24. [DOI:10.1111/j.1749-6632.2012.06751.x] [PMID] [PMCID]
- Versace A, Acuff H, Bertocci MA, Bebko G, Almeida JR, Perlman SB, et al. White matter structure in youth with behavioral and emotional dysregulation disorders: A probabilistic tractographic study. JAMA Psychiatry. 2015; 72(4):367-76. [DOI:10.1001/jamapsychiatry.2014.2170] [PMID] [PMCID]
- Wallace EJ, Mathias JL, Ward L, Fripp J, Rose S, Pannek K. A fixel-based analysis of micro- and macro-structural changes to white matter following adult traumatic brain injury. Human Brain Mapping. 2020; 41(8):2187-97. [DOI:10.1002/hbm.24939] [PMID] [PMCID]
- Hellstrøm T, Westlye LT, Kaufmann T, Trung Doan N, Søberg HL, Sigurdardottir S, et al. White matter microstructure is associated with functional, cognitive and emotional symptoms 12 months after mild traumatic brain injury. Scientific Reports. 2017; 7(1):13795. [DOI:10.1038/s41598-017-13628-1] [PMID] [PMCID]
- van der Horn HJ, Mangina NR, Rakers SE, Kok JG, Timmerman ME, Leemans A, et al. White matter microstructure of the neural emotion regulation circuitry in mild traumatic brain injury. The European Journal of Neuroscience. 2021; 53(10):3463-75. [DOI:10.1111/ejn.15199] [PMID] [PMCID]
- Salas CE, Gross JJ, Turnbull OH. Using the process model to understand emotion regulation changes after brain injury. Psychology & Neuroscience. 2019; 12(4):430-50. [DOI:10.1037/pne0000174]
- Spikman JM, Boelen DH, Pijnenborg GH, Timmerman ME, van der Naalt J, Fasotti L. Who benefits from treatment for executive dysfunction after brain injury? Negative effects of emotion recognition deficits. Neuropsychological Rehabilitation. 2013; 23(6):824-45. [DOI:10.1080/09602011.2013.826138] [PMID]
- Tsaousides T, Spielman L, Kajankova M, Guetta G, Gordon W, Dams-O-Connor K. Improving emotion regulation following web-based group intervention for individuals with traumatic brain injury. Journal of Head Trauma Rehabilitation. 2017; 32(5):354-65. [DOI:10.1097/HTR.0000000000000345] [PMID]
- Tornås S, Løvstad M, Solbakk AK, Schanke AK, Stubberud J. Goal management training combined with external cuing as a means to improve emotional regulation, psychological functioning, and quality of life in patients with acquired brain injury: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 2016; 97(11):1841-52.e3. [DOI:10.1016/j.apmr.2016.06.014] [PMID]
- Centers for Disease Control and Prevention. Report to congress on traumatic brain injury in the United States: Epidemiology and rehabilitation. Atlanta: National Center for Injury Prevention and Control; Division of Unintentional Injury Prevention; 2015. [Link]
- Nash RP, Weinberg MS, Laughon SL, McCall RC, Bateman JR, Rosenstein DL. Acute pharmacological management of behavioral and emotional dysregulation following a traumatic brain injury: A systematic review of the literature. Psychosomatics. 2019; 60(2):139-52. [DOI:10.1016/j.psym.2018.11.009] [PMID] [PMCID]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. International Journal of Surgery. 2021; 88:105906. [DOI:10.1016/j.ijsu.2021.105906] [PMID]
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Systematic Reviews. 2016; 5(1):210. [DOI:10.1186/s13643-016-0384-4] [PMID] [PMCID]
- Aboulafia-Brakha T, Allain P, Ptak R. Emotion regulation after traumatic brain injury: Distinct patterns of sympathetic activity during anger expression and recognition. The Journal of Head Trauma Rehabilitation. 2016; 31(3):E21-31. [DOI:10.1097/HTR.0000000000000171] [PMID]
- Ashworth F, Gracey F, Gilbert P. Compassion focused therapy after traumatic brain injury: Theoretical foundations and a case illustration. Brain Impairment. 2012; 12(2):128-39. [DOI:10.1375/brim.12.2.128]
- Dethier M, Blairy S, Rosenberg H, McDonald S. Emotional regulation impairments following severe traumatic brain injury: An investigation of the body and facial feedback effects. Journal of the International Neuropsychological Society. 2013; 19(4):367-79. [DOI:10.1017/S1355617712001555] [PMID]
- Campbell AM, Elbogen EB, Johnson JL, Hamer RM, Belger A. Event related potentials indexing the influence of emotion on cognitive processing in veterans with comorbid post-traumatic stress disorder and traumatic brain injury. Clinical Neurophysiology. 2021; 132(7):1389-97. [DOI:10.1016/j.clinph.2021.03.017] [PMID]
- Fisher AC, Rushby JA, McDonald S, Parks N, Piguet O. Neurophysiological correlates of dysregulated emotional arousal in severe traumatic brain injury. Clinical Neurophysiology. 2015; 126(2):314-24. [DOI:10.1016/j.clinph.2014.05.033] [PMID]
- Sultana T, Hasan MA, Kang X, Liou-Johnson V, Adamson MM, Razi, A. Neural mechanisms of emotional health in traumatic brain injury patients undergoing rTMS treatment. Molecular Psychiatry. 2023. [DOI:10.1101/2022.09.29.22280447]
- Stubberud J, Løvstad M, Solbakk AK, Schanke AK, Tornås S. Emotional regulation following acquired brain injury: Associations with executive functioning in daily life and symptoms of anxiety and depression. Frontiers in Neurology. 2020; 11:1011. [DOI:10.3389/fneur.2020.01011] [PMID] [PMCID]
- Shields C, Ownsworth T, O'Donovan A, Fleming J. A transdiagnostic investigation of emotional distress after traumatic brain injury. Neuropsychological Rehabilitation. 2016; 26(3):410-45. [DOI:10.1080/09602011.2015.1037772] [PMID]
- Choi EB, Jang SH. Degeneration of core neural tracts for emotional regulation in a patient with traumatic brain injury: A case report. Medicine. 2021; 100(4):e24319. [DOI:10.1097/MD.0000000000024319] [PMID] [PMCID]
- Dretsch MN, Daniel TA, Goodman AM, Katz JS, Denney T, Deshpande G, et al. Differential neural activation when voluntarily regulating emotions in service members with chronic mild traumatic brain injury. Applied neuropsychology. Adult. 2019; 26(1):76-88. [DOI:10.1080/23279095.2017.1362406] [PMID]
- Novakovic-Agopian T, Kornblith E, Abrams G, McQuaid JR, Posecion L, Burciaga J, et al. Long-term effects of executive function training among veterans with chronic TBI. Brain Injury. 2019; 33(12):1513-21. [DOI:10.1080/02699052.2019.1645357] [PMID]
- Fishbein D, Dariotis JK, Ferguson PL, Pickelsimer EE. Relationships between traumatic brain injury and illicit drug use and their association with aggression in inmates. International Journal of Offender Therapy and Comparative Criminology. 2016; 60(5):575-97. [DOI:10.1177/0306624X14554778] [PMID]
- Grimm LA, Van Puymbroeck M, Miller KK, Fisher T, Schmid AA. Yoga after traumatic brain injury: Changes in emotional regulation and health-related quality of life in a case study. International Journal of Complementary & Alternative Medicine. 2017; 8(1):00247. [DOI:10.15406/ijcam.2017.08.00247]
- Killgore WDS, Singh P, Kipman M, Pisner D, Fridman A, Weber M. Gray matter volume and executive functioning correlate with time since injury following mild traumatic brain injury. Neuroscience Letters. 2016; 612:238-44.[DOI:10.1016/j.neulet.2015.12.033] [PMID]
- Westerhof-Evers HJ, Visser-Keizer AC, Fasotti L, Spikman JM. Social cognition and emotion regulation: A multifaceted treatment (T-ScEmo) for patients with traumatic brain injury. Clinical Rehabilitation. 2019; 33(5):820-33.[DOI:10.1177/0269215519829803] [PMID] [PMCID]
- Finnanger TG, Olsen A, Skandsen T, Lydersen S, Vik A, Evensen KA, et al. Life after adolescent and adult moderate and severe traumatic brain injury: Self-reported executive, emotional, and behavioural function 2-5 years after injury. Behavioural Neurology. 2015; 2015:329241. [DOI:10.1155/2015/329241] [PMID] [PMCID]
- van der Horn HJ, Liemburg EJ, Scheenen ME, de Koning ME, Marsman JB, Spikman JM, et al. Brain network dysregulation, emotion, and complaints after mild traumatic brain injury. Human Brain Mapping. 2016; 37(4):1645-54. [DOI:10.1002/hbm.23126] [PMID] [PMCID]
- Marsh NV, Kersel DA. Frequency of behavioural problems at one year following traumatic brain injury: Correspondence between patient and caregiver reports. Neuropsychological Rehabilitation. 2006; 16(6):684-94. [DOI:10.1080/09602010500220290] [PMID]
- Novakovic-Agopian T, Posecion L, Kornblith E, Abrams G, McQuaid JR, Neylan TC, et al. Goal-Oriented Attention Self-Regulation Training improves executive functioning in veterans with post-traumatic stress disorder and mild traumatic brain injury. Journal of Neurotrauma. 2021; 38(5):582-92. [DOI:10.1089/neu.2019.6806] [PMID]
- Shafiei E, Fakharian E, Nademi A, Omidi A, Sharifi A, Akbari H. A comparison of difficulties in emotional regulations of patients with mild traumatic brain injury and normal controls. Archives of Trauma Research. 2018; 7(2):45-9. [DOI:10.4103/atr.atr_7_17]
- Nemattavousi M, Soltaninia S. [The mediating role of experiential avoidance in the relationship between Alexithymia and emotion regulation in patients with major depression disorder after traumatic brain injury (Persian)]. Shenakht Journal of Psychology and Psychiatry. 2020; 7(2):140-52. [DOI:10.52547/shenakht.7.2.140]
- Sun M, Marquardt CA, Disner SG, Burton PC, Davenport ND, Lissek S, et al. Posttraumatic stress symptomatology and abnormal neural responding during emotion regulation under cognitive demands: Mediating effects of personality. Personality Neuroscience. 2020; 3:e9. [DOI:10.1017/pen.2020.10] [PMID] [PMCID]
- Ebrahimi SAA. The effectiveness of mindfulness-based therapy and positive thinking on emotion regulation and defense mechanisms in people with borderline personality disorder in improving post-traumatic brain injury. Journal of Assessment and Research in Applied Counseling. 2022; 4(1):6-10. [DOI:10.52547/jarac.4.2.13]
- Tsaousides T, D'Antonio E, Varbanova V, Spielman L. Delivering group treatment via videoconference to individuals with traumatic brain injury: A feasibility study. Neuropsychological Rehabilitation. 2014; 24(5):784-803. [DOI:10.1080/09602011.2014.907186] [PMID]
- Siponkoski ST, Koskinen S, Laitinen S, Holma M, Ahlfors M, Jordan-Kilkki P, et al. Effects of neurological music therapy on behavioural and emotional recovery after traumatic brain injury: A randomized controlled cross-over trial. Neuropsychological Rehabilitation. 2022; 32(7):1356-88. [DOI:10.1080/09602011.2021.1890138] [PMID]
- Donnelly KZ, Nelson J, Zeller S, Davey A, Davis D. The feasibility, acceptability, and effectiveness of the multimodal, community-based LoveYourBrain Retreat program for people with traumatic brain injury and caregivers. Disability and Rehabilitation. 2022; 28:1-11. [DOI:10.1080/09638288.2022.2159547] [PMID]
- Neumann D, Malec JF, Hammond FM. Reductions in alexithymia and emotion dysregulation after training emotional self-awareness following traumatic brain injury: A phase I trial. The Journal of Head Trauma Rehabilitation. 2017; 32(5):286-95. [DOI:10.1097/HTR.0000000000000277] [PMID] [PMCID]
- Elbogen EB, Dennis PA, Van Voorhees EE, Blakey SM, Johnson JL, Johnson SC, et al. Cognitive rehabilitation with mobile technology and social support for veterans with TBI and PTSD: A randomized clinical trial. The Journal of Head Trauma Rehabilitation. 2019; 34(1):1-10. [DOI:10.1097/HTR.0000000000000435] [PMID] [PMCID]
- Westerhof-Evers HJ, Visser-Keizer AC, Fasotti L, Schönherr MC, Vink M, van der Naalt J, et al. Effectiveness of a treatment for impairments in social cognition and emotion regulation (T-ScEmo) after traumatic brain injury: A randomized controlled trial. Journal of Head Trauma Rehabilitation. 2017; 32(5):296-307. [DOI:10.1097/HTR.0000000000000332] [PMID]
- Beresford TP, Arciniegas D, Clapp L, Martin B, Alfers J. Reduction of affective lability and alcohol use following traumatic brain injury: A clinical pilot study of anti-convulsant medications. Brain Injury. 2005; 19(4):309-13. [DOI:10.1080/02699050410001720121] [PMID]
- Azulay J, Mott T. Using mindfulness attention meditation (MAP) with a mixed brain injury population to enhance awareness and improve emotional regulation. Journal of Psychology and Clinical Psychiatry. 2016; 6(5):00372. [Link]
- Cantor J, Ashman T, Dams-O'Connor K, Dijkers MP, Gordon W, Spielman L, et al. Evaluation of the short-term executive plus intervention for executive dysfunction after traumatic brain injury: A randomized controlled trial with minimization. Archives of Physical Medicine and Rehabilitation. 2014; 95(1):1-9.e3. [DOI:10.1016/j.apmr.2013.08.005] [PMID]
- Bardeen JR, Kumpula MJ, Orcutt HK. Emotion regulation difficulties as a prospective predictor of posttraumatic stress symptoms following a mass shooting. Journal of Anxiety Disorders. 2013; 27(2):188-96. [DOI:10.1016/j.janxdis.2013.01.003] [PMID] [PMCID]
- Kohn N, Eickhoff SB, Scheller M, Laird AR, Fox PT, Habel U. Neural network of cognitive emotion regulation - An ALE meta-analysis and MACM analysis. NeuroImage. 2014; 87:345-55. [PMID] [PMCID]
- Meyer DL, Davies DR, Barr JL, Manzerra P, Forster GL. Mild traumatic brain injury in the rat alters neuronal number in the limbic system and increases conditioned fear and anxiety-like behaviors. Experimental Neurology. 2012; 235(2):574-87. [DOI:10.1016/j.expneurol.2012.03.012] [PMID]
- Russell AL, Tasker JG, Lucion AB, Fiedler J, Munhoz CD, Wu TJ, et al. Factors promoting vulnerability to dysregulated stress reactivity and stress-related disease. Journal of Neuroendocrinology. 2018; 30(10):e12641. [DOI:10.1111/jne.12641] [PMID] [PMCID]
- Tapp ZM, Godbout JP, Kokiko-Cochran ON. A tilted axis: Maladaptive inflammation and HPA axis dysfunction contribute to consequences of TBI. Frontiers in Neurology. 2019; 10:345. [DOI:10.3389/fneur.2019.00345] [PMID] [PMCID]
- Israel, L. The cognitive emotion process: Examining appraisal theory using theoretical modeling and machine learning [PhD dissertation]. München: Ludwig-Maximilians-Universität; 2020. [Link]
- Bohnen N, Jolles J, Twijnstra A, Mellink R, Sulon J. Coping styles, cortisol reactivity, and performance in a vigilance task of patients with persistent postconcussive symptoms after a mild head injury. International Journal of Neuroscience. 1992; 64(1-4):97-105. [DOI:10.3109/00207459209000536] [PMID]
- de Sousa A, McDonald S, Rushby J, Li S, Dimoska A, James C. Understanding deficits in empathy after traumatic brain injury: The role of affective responsivity. Cortex. 2011; 47(5):526-35. [DOI:10.1016/j.cortex.2010.02.004] [PMID]
- Pineau H, Marchand A, Guay S. Specificity of cognitive and behavioral complaints in post-traumatic stress disorder and mild traumatic brain injury. Behavioral Sciences. 2015; 5(1):43-58. [DOI:10.3390/bs5010043] [PMID] [PMCID]
- Maas AIR, Menon DK, Adelson PD, Andelic N, Bell MJ, Belli A, et al. Traumatic brain injury: Integrated approaches to improve prevention, clinical care, and research. The Lancet Neurology. 2017; 16(12):987-1048. [DOI:10.1016/S1474-4422(17)30371-X]
- Herwig U, Kaffenberger T, Jäncke L, Brühl AB. Self-related awareness and emotion regulation. NeuroImage. 2010; 50(2):734-41. [DOI:10.1016/j.neuroimage.2009.12.089] [PMID]
Type of Study: Review |
Subject:
Neuroscience
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








