Wed, Jan 28, 2026
Volume 11 - Continuous Publishing
Iran J Neurosurg 2025, 11 - Continuous Publishing: 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Siddiqui O A, nasreen F, Siddiqui S M, Khalid A. A Retrospective Analysis of Head Injury Patients Admitted in an Indian Tertiary Hospital During the COVID 19 Pandemic. Iran J Neurosurg 2025; 11 : 3
URL: http://irjns.org/article-1-386-en.html
URL: http://irjns.org/article-1-386-en.html
1- Department of Anaesthesiology, Jawaharlal Nehru Medical College, Aligarh Muslim University (AMU), Aligarh, India.
Keywords: Intensive Care Unit, Traumatic Brain Injury, Head injury, Road Traffic Accidents, COVID-19
Full Text [PDF 938 kb]
(701 Downloads)
| Abstract (HTML) (3185 Views)
References
Full Text: (1106 Views)
1. Introduction
The COVID-19 pandemic has affected the entire world in an unprecedented manner. During the initial period, a lockdown occurred with complete movement restrictions. Gradual unlocking in a phased manner was performed after the first wave, and travel and routine work were allowed with necessary precautions [1, 2]. There were worries that the containment measures and lockdown may have negatively affected public health and the outcomes of other conditions [3, 4]. Owing to various social and economic reasons, a complete lockdown was not feasible after that, and limited movement was allowed. With the gradual unlocking and subsequent movement on the road, an increase in the number of patients with road traffic accidents (RTA) and head injuries was expected. Reduced traffic congestion, empty lanes, and excessive vehicle speed may have increased the occurrence of RTA during lockdown.
Head injury, or acquired brain injury, is a broad term used to describe various injuries to the scalp, skull, brain, or underlying blood vessels. This occurs when an external force impacts the brain in the form of a bump, jolt, or blow to the head, the head violently hits a surface, or an item pierces the skull and enters the brain [5]. Traumatic brain injury (TBI) does not generally result in evident motor dysfunction. Most people who experience these symptoms are invisible and do not express their concerns. The consequences of TBI and related conditions are often misunderstood. All these factors have contributed to the term “silent epidemic” [6].
Head injury with subsequent TBI is a major cause of morbidity and mortality, specifically in low- and middle-income countries, and poses a challenge in the intensive care unit (ICU). The altered behavior of the population may have substantially affected the epidemiology of TBI cases, with many countries reporting changes in the incidence as well as the outcome during vs before the pandemic [7]. There are not many such studies on the Indian subcontinent.
This study was conducted to evaluate TBI cases admitted to the emergency trauma ICU in our hospital during the COVID-19 outbreak. We discussed the management and challenges faced in the ICU care of patients with TBI during the second wave of the pandemic in a tertiary care hospital in northern India.
2. Methods and Materials
The study was conducted on patients admitted to the ICU in the Emergency Department at Jawaharlal Nehru Medical College after obtaining approval from the Institutional Ethical Committee. The ICU is a level III, nine-bed multidisciplinary unit that caters to emergency patients. Consultants and residents of the Department of Anesthesiology and Critical Care manage the care of these patients.
This retrospective study included patients admitted to the ICU between January 2021 and December 2021. Patient data were retrieved from an electronic database maintained in the ICU. Sociodemographic parameters, causes of TBI, therapeutic interventions, and outcomes in terms of Glasgow coma scale (GCS) score and mortality, tracheostomy, and extubation were all evaluated. Rotterdam computed tomography (CT) scores were noted on the non-contrast CT scan of patient's head, which was done at the time of admission (done within 4 hours of admission).
Rotterdam CT scores are classified as follows:
Basal cisterns:
• 0: Normal
• 1: Compressed
• 2: Absent
Midline shift:
• 0: No shift or ≤5 mm
• 1: Shift >5 mm
Epidural mass lesion:
• 0: Present
• 1: Absent
Intraventricular blood or traumatic subarachnoid hemorrhage (SAH):
• 0: Absent
• 1: Present
3. Results
Over a year, 76 patients with TBI were admitted to the trauma ICU.
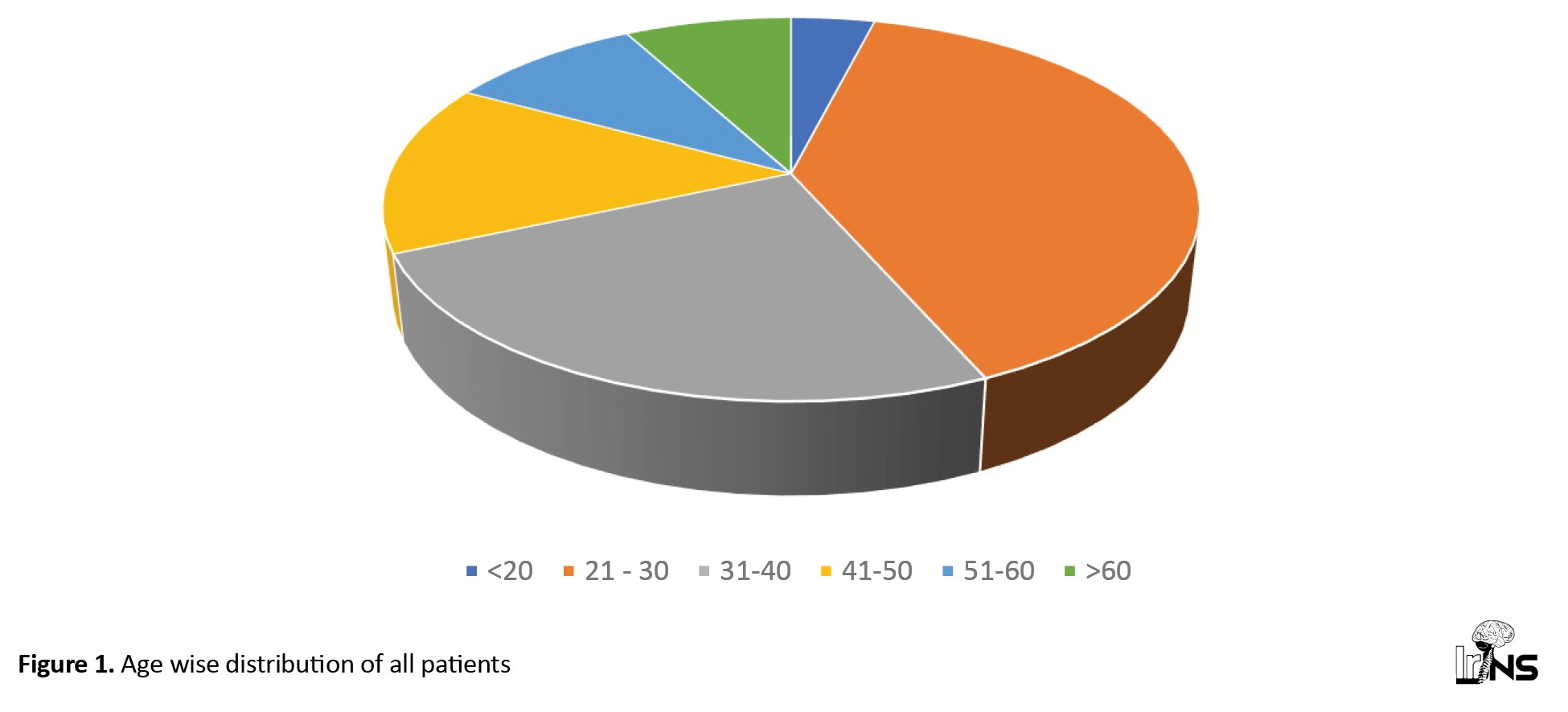
Age: These patients were between 18 and 75, with a mean age of 37.09±14.64 years. The maximum number of patients was between the ages of 21 and 30 (39.5%), followed by 31 and 40(25%). Elderly patients aged >70 account for 2.6% of the total population (Figure 1).
The COVID-19 pandemic has affected the entire world in an unprecedented manner. During the initial period, a lockdown occurred with complete movement restrictions. Gradual unlocking in a phased manner was performed after the first wave, and travel and routine work were allowed with necessary precautions [1, 2]. There were worries that the containment measures and lockdown may have negatively affected public health and the outcomes of other conditions [3, 4]. Owing to various social and economic reasons, a complete lockdown was not feasible after that, and limited movement was allowed. With the gradual unlocking and subsequent movement on the road, an increase in the number of patients with road traffic accidents (RTA) and head injuries was expected. Reduced traffic congestion, empty lanes, and excessive vehicle speed may have increased the occurrence of RTA during lockdown.
Head injury, or acquired brain injury, is a broad term used to describe various injuries to the scalp, skull, brain, or underlying blood vessels. This occurs when an external force impacts the brain in the form of a bump, jolt, or blow to the head, the head violently hits a surface, or an item pierces the skull and enters the brain [5]. Traumatic brain injury (TBI) does not generally result in evident motor dysfunction. Most people who experience these symptoms are invisible and do not express their concerns. The consequences of TBI and related conditions are often misunderstood. All these factors have contributed to the term “silent epidemic” [6].
Head injury with subsequent TBI is a major cause of morbidity and mortality, specifically in low- and middle-income countries, and poses a challenge in the intensive care unit (ICU). The altered behavior of the population may have substantially affected the epidemiology of TBI cases, with many countries reporting changes in the incidence as well as the outcome during vs before the pandemic [7]. There are not many such studies on the Indian subcontinent.
This study was conducted to evaluate TBI cases admitted to the emergency trauma ICU in our hospital during the COVID-19 outbreak. We discussed the management and challenges faced in the ICU care of patients with TBI during the second wave of the pandemic in a tertiary care hospital in northern India.
2. Methods and Materials
The study was conducted on patients admitted to the ICU in the Emergency Department at Jawaharlal Nehru Medical College after obtaining approval from the Institutional Ethical Committee. The ICU is a level III, nine-bed multidisciplinary unit that caters to emergency patients. Consultants and residents of the Department of Anesthesiology and Critical Care manage the care of these patients.
This retrospective study included patients admitted to the ICU between January 2021 and December 2021. Patient data were retrieved from an electronic database maintained in the ICU. Sociodemographic parameters, causes of TBI, therapeutic interventions, and outcomes in terms of Glasgow coma scale (GCS) score and mortality, tracheostomy, and extubation were all evaluated. Rotterdam computed tomography (CT) scores were noted on the non-contrast CT scan of patient's head, which was done at the time of admission (done within 4 hours of admission).
Rotterdam CT scores are classified as follows:
Basal cisterns:
• 0: Normal
• 1: Compressed
• 2: Absent
Midline shift:
• 0: No shift or ≤5 mm
• 1: Shift >5 mm
Epidural mass lesion:
• 0: Present
• 1: Absent
Intraventricular blood or traumatic subarachnoid hemorrhage (SAH):
• 0: Absent
• 1: Present
3. Results
Over a year, 76 patients with TBI were admitted to the trauma ICU.
Age: These patients were between 18 and 75, with a mean age of 37.09±14.64 years. The maximum number of patients was between the ages of 21 and 30 (39.5%), followed by 31 and 40(25%). Elderly patients aged >70 account for 2.6% of the total population (Figure 1).
Sex: Male patients comprised 72.4% of the total, and females accounted for 27.6%. A total of 56.4% of male patients recovered, 43.6% died, 47.6% of female patients recovered, and 52.4% died.
Cause: 73.6% of the patients had TBI due to a road traffic accident; 18.4% had a fall from height with a head injury; 6.5% had an assault with a head injury; and 1.3% had a slip and fall with a head injury.
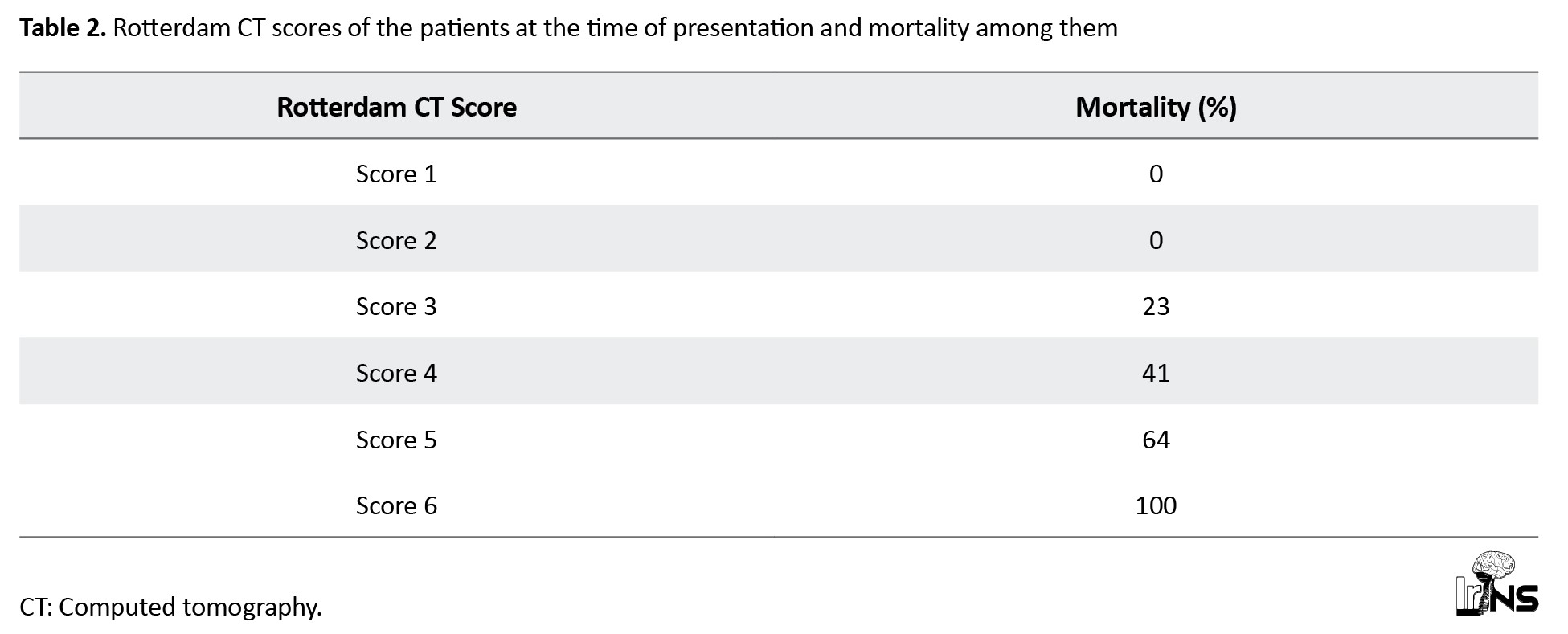
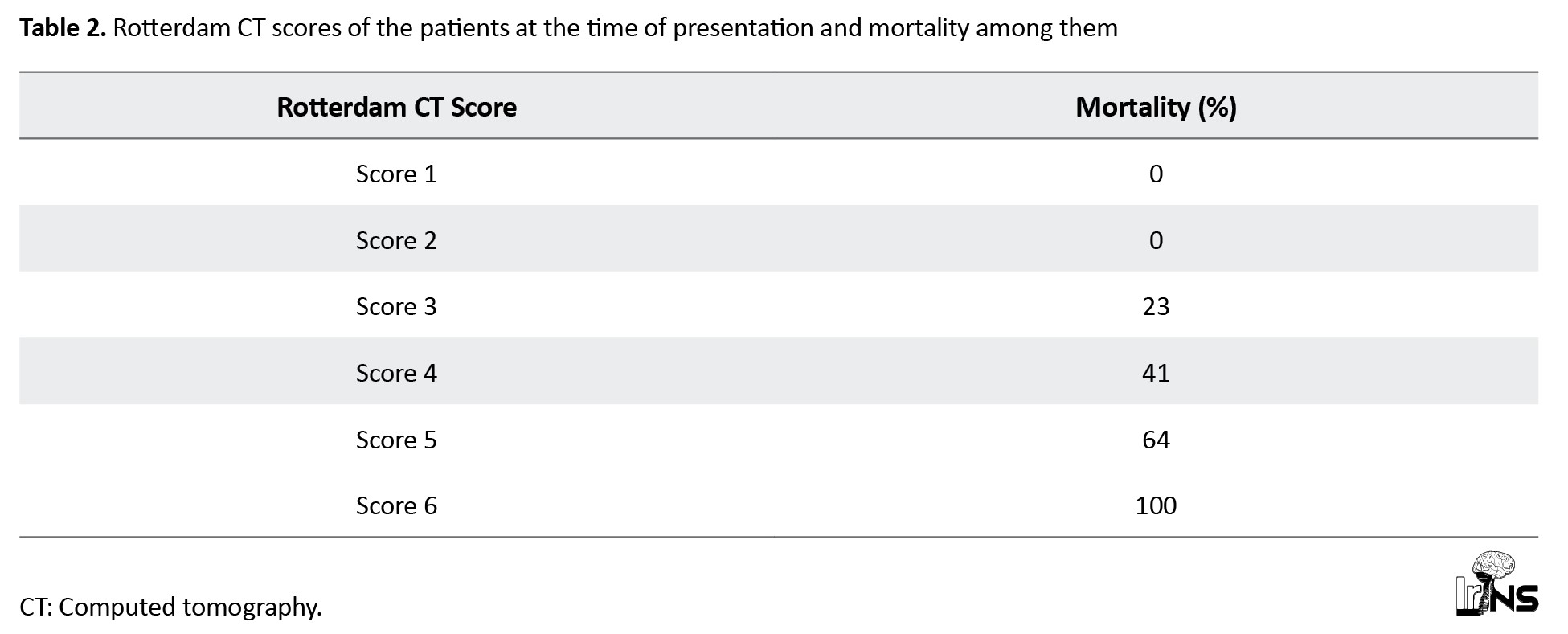
Rotterdam CT score: Patients having a CT scan at the time of presentation to the emergency department (done within 4 hours). Mortality was high among patients with a higher Rotterdam CT score and low among patients with a lower Rotterdam CT score (Table 1).
Intervention: 18.4% of patients underwent surgery. Many of them (57.14%) recovered, and 42.86% died.
Mechanical ventilation: Mechanical ventilation following TBI was required in 84.2% of patients. Of these, 31.25% were extubated, 14.06% were tracheostomized and shifted out, and the rest expired (54.69%).
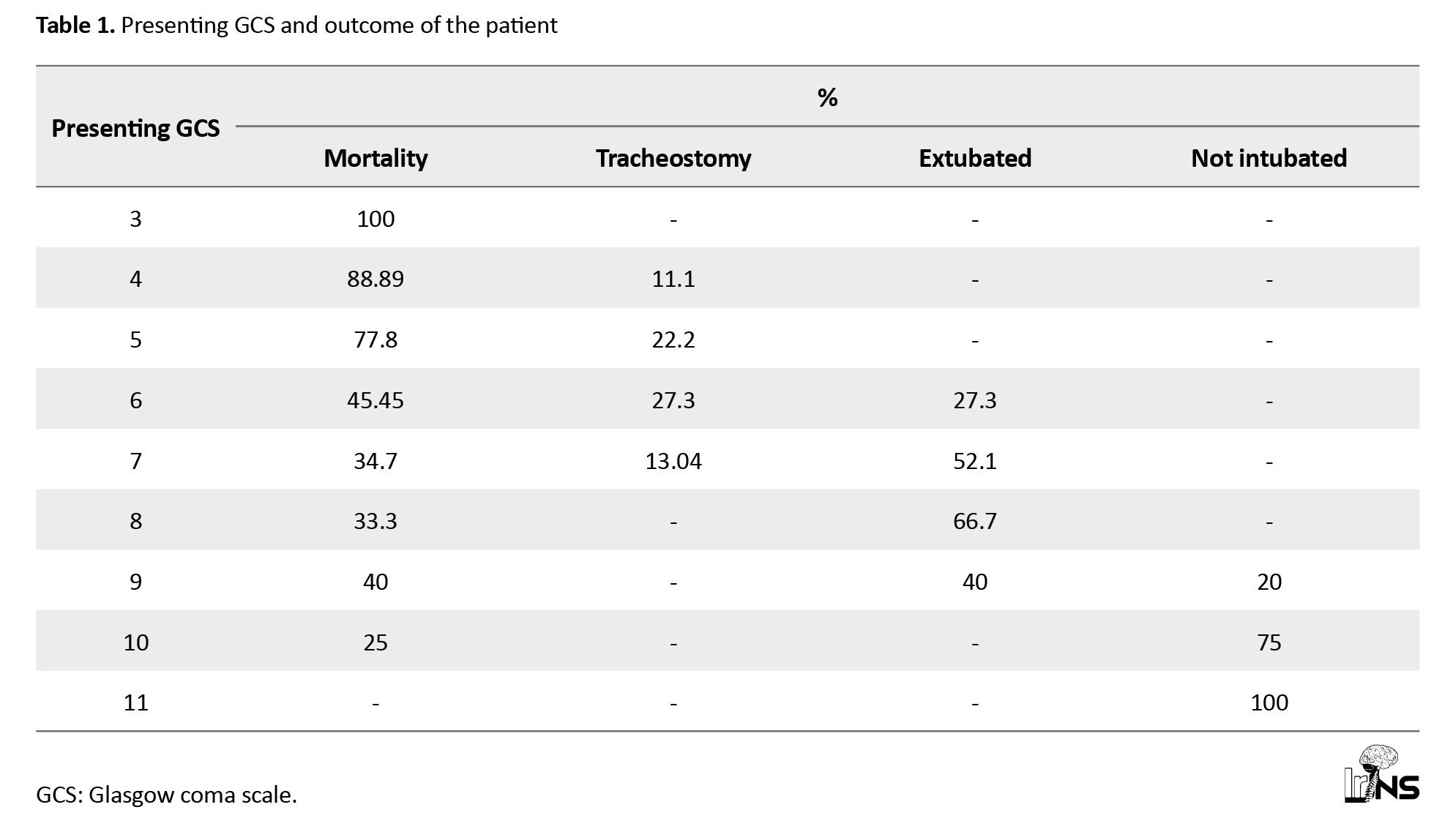
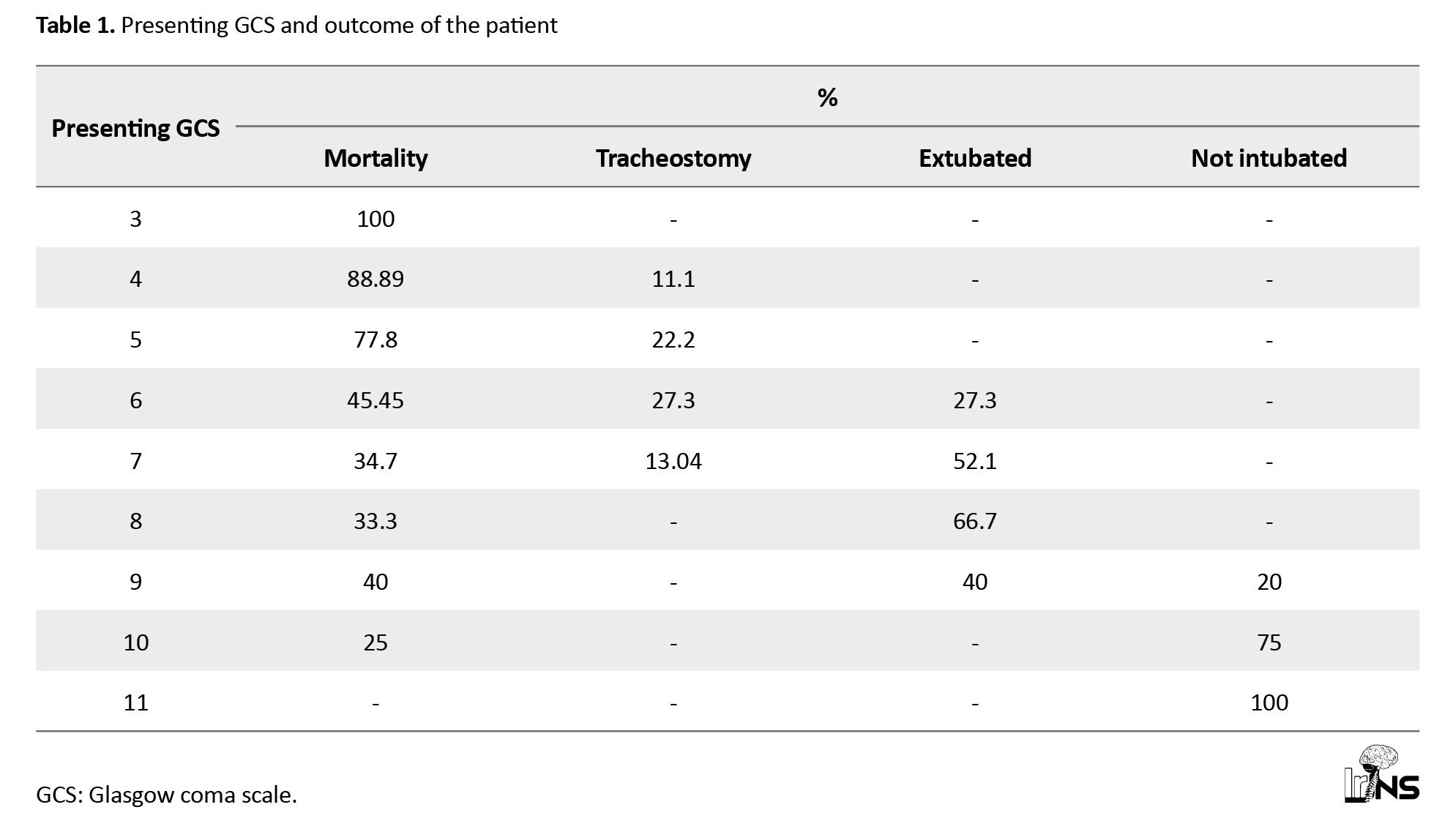
Outcome: Mortality following TBI was high, with 46.05% of all patients dying. A total of 26.3% were extubated, 11.8% were shifted out after tracheostomy, and 15.8% were not intubated. Table 2 presents the relationship between patient GCS score and outcome.
4. Discussion
This study analyzed the impact of the second wave of COVID-19 on patients with TBI admitted to the Emergency Trauma Center (ETC) ICU of our hospital. Our study indicated a high mortality rate of 46.05% in patients with TBI, despite a decrease in the number of admissions over one year during the second wave of COVID-19. In April 2020, our hospital was recognized as a level 2 COVID-19 care facility. Due to the sudden increment in critical patients and COVID-19 patients presenting with a variety of symptoms, a COVID-19 suspect area and a COVID-19 suspect ICU were required, rather than an isolation ICU where all patients presenting to the emergency room and requiring ICU care were managed until the reverse transcription polymerase chain reaction (RT-PCR) results were obtained. It was difficult to create a COVID-19 suspect ICU in an emergency and trauma hospital in a relatively short time. As a result, we were forced to convert the ETC ICU into a COVID-19 suspect ICU, considering that all patients were COVID-19 suspects unless proven differently by RT-PCR [8].
Based on the RT-PCR report, patients were shifted to a dedicated COVID-19 ICU, or main ICU. Since our hospital is a tertiary care center, patients continued to encounter various other non-COVID-19 emergencies during the COVID-19 pandemic. The main aim was to contain the outbreak and limit its spread while continuing with the hospital’s emergency services. As we did not have a dedicated neurosurgery ICU, all patients presenting with TBI who required ICU care were kept in the Trauma ICU, which was chosen as the interim COVID-19 suspect ICU for critical patients. This poses numerous challenges regarding resource planning, infection control, patient care, and training and safety of healthcare workers. After the first wave subsided, things gradually returned to normal when the deadly second wave occurred. This was a much larger outbreak with widespread infection. The management of patients with severe TBI is a continuous process, starting from the pre-hospital period and continuing through management in the emergency department and operating rooms before admission to the ICU.
Our study indicated a death rate of 46.05% in patients with head injuries during the COVID-19 pandemic (Table 1). This high mortality rate is by the study by Miękisiak et al., which also shows a 26.75% increase in the in-house mortality rate in the COVID period as compared to the pre-covid era. However, the incidence of TBI decreased during the COVID-19 period [9]. No comparable data existed at our hospital because no such study had been conducted before COVID-19. Some of the potential causes of the increased mortality in patients with head injury during the COVID-19 era were increased head injury severity, insufficient ICU beds, undertrained staff, lack of experience in managing pandemic situations, mismanagement of neurotrauma patients due to an overcrowded hospital, and cross-infection with COVID-19 patients since our ICU was a combined COVID-19 and trauma ICU. The number of patients with severe head injuries may have increased as mild to moderate head injuries were not reported to the hospital because of lockdown and concerns about patients visiting hospitals at the peak of the pandemic. Public reports also revealed that the severity of head injuries was higher during the COVID-19 pandemic [10, 11]. Possible reasons that have been cited for increased mortality in head injury patients during lockdown include an increased injury severity score and a low GCS at the time of trauma presentation [10]. Goyal et al. reported an increase in mortality from 12.4% to 22.5% in head injury patients during the COVID-19 pandemic as compared to the pre-COVID-19 period [12]. An increase in the severity of head traumas and related injuries caused this surge in mortality.
A study by Bagheri et al. observed an increase in the in-hospital mortality of elderly patients presenting with moderate to severe head injuries [13]. They noticed coronavirus and GCS as independent risk factors for in-hospital mortality. Damara et al., in their systemic review and analysis of 13 studies, found high mortality due to TBI in low- and middle-income countries. However, no change was observed in mortality in high-income countries during the COVID-19 pandemic [14]. This variation can be attributed to the relatively higher number of COVID-19 cases in underdeveloped nations and insufficient medical resources, which eventually burdened the healthcare system.
In contrast to our findings, Weber et al.’s observational cohort study revealed no significant difference in mortality during the pandemic compared to the pre-pandemic period [7]. The number of patients with severe traumatic brain injuries did not decrease during the pandemic, according to their study, which was conducted in the affluent nation of Norway. The same standard of care was provided throughout the pandemic, possibly due to better infrastructure. A study by Luostarinen et al. in Finland also revealed similar results in patients with TBI during the COVID-19 era, perhaps due to their advanced public health system and presumably improved care [15].
The results of the present study about demographic data revealed that TBI was more common in the economically productive age group [16, 17] (Figure 1). The average age was 37±14. It is well known that there are sex-related differences in TBI incidence. Of the patients in our study, 72.4% were men. Men are more likely to be exposed to injuries than women because they are more likely to engage in injury-prone work or dangerous behaviour. These results are consistent with the multicenter descriptive study by Eom et al., which found that 68.8% of all males had TBI [18].
RTA were the most common mode of injury, accounting for approximately 73.6% of cases. With the issuance of unlocking orders by the government, the movement of people on the road was permitted; thus, the incidence of RTA increased significantly. Other studies have also cited RTA as a major cause of TBI during pandemics [19-21].
Regarding management, most of the patients with TBI were treated conservatively, with only 18% requiring surgical intervention. A literature review also highlights similar findings, with many patients with TBI being managed conservatively during the COVID-19 pandemic [22]. Thinly stretched hospital resources, with most facilities diverted to COVID-19 ICUs and wards. A shortage of staff, equipment, and surgical facilities may have been the primary reasons for decreased surgical interventions during the pandemic.
5. Conclusion
The COVID-19 pandemic has had a significant impact on the management of patients with TBI. Despite a decrease in the number of admissions, high mortality rates have been noted in patients with TBI during the COVID-19 pandemic.
Limitations
This was a retrospective study of TBI patients during the COVID-19 pandemic. The analysis would have been better if we had compared it with pre-COVID-19 data. However, the same could not be done, as no such study was conducted during the pre-COVID-19 period. Since the data were retrieved from a single center, the results of the study cannot be generalized. However, our data might provide insights for larger multicenter trials exploring the pandemic’s impact on TBI patterns.
Ethical Considerations
Compliance with ethical guidelines
The study was conducted after obtaining approval from the Institutional Ethical Committee of Jawaharlal Nehru Medical College, Aligarh, India (Code: IEC/JNMC/2022/429).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, study design, data collection, data analysis and interpretation: Sobia Manaal Siddiqui; Drafting the article: Obaid Ahmad Siddiqui; Review and editing: Farah Nasreen; fina; approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Cause: 73.6% of the patients had TBI due to a road traffic accident; 18.4% had a fall from height with a head injury; 6.5% had an assault with a head injury; and 1.3% had a slip and fall with a head injury.
Rotterdam CT score: Patients having a CT scan at the time of presentation to the emergency department (done within 4 hours). Mortality was high among patients with a higher Rotterdam CT score and low among patients with a lower Rotterdam CT score (Table 1).
Intervention: 18.4% of patients underwent surgery. Many of them (57.14%) recovered, and 42.86% died.
Mechanical ventilation: Mechanical ventilation following TBI was required in 84.2% of patients. Of these, 31.25% were extubated, 14.06% were tracheostomized and shifted out, and the rest expired (54.69%).
Outcome: Mortality following TBI was high, with 46.05% of all patients dying. A total of 26.3% were extubated, 11.8% were shifted out after tracheostomy, and 15.8% were not intubated. Table 2 presents the relationship between patient GCS score and outcome.
4. Discussion
This study analyzed the impact of the second wave of COVID-19 on patients with TBI admitted to the Emergency Trauma Center (ETC) ICU of our hospital. Our study indicated a high mortality rate of 46.05% in patients with TBI, despite a decrease in the number of admissions over one year during the second wave of COVID-19. In April 2020, our hospital was recognized as a level 2 COVID-19 care facility. Due to the sudden increment in critical patients and COVID-19 patients presenting with a variety of symptoms, a COVID-19 suspect area and a COVID-19 suspect ICU were required, rather than an isolation ICU where all patients presenting to the emergency room and requiring ICU care were managed until the reverse transcription polymerase chain reaction (RT-PCR) results were obtained. It was difficult to create a COVID-19 suspect ICU in an emergency and trauma hospital in a relatively short time. As a result, we were forced to convert the ETC ICU into a COVID-19 suspect ICU, considering that all patients were COVID-19 suspects unless proven differently by RT-PCR [8].
Based on the RT-PCR report, patients were shifted to a dedicated COVID-19 ICU, or main ICU. Since our hospital is a tertiary care center, patients continued to encounter various other non-COVID-19 emergencies during the COVID-19 pandemic. The main aim was to contain the outbreak and limit its spread while continuing with the hospital’s emergency services. As we did not have a dedicated neurosurgery ICU, all patients presenting with TBI who required ICU care were kept in the Trauma ICU, which was chosen as the interim COVID-19 suspect ICU for critical patients. This poses numerous challenges regarding resource planning, infection control, patient care, and training and safety of healthcare workers. After the first wave subsided, things gradually returned to normal when the deadly second wave occurred. This was a much larger outbreak with widespread infection. The management of patients with severe TBI is a continuous process, starting from the pre-hospital period and continuing through management in the emergency department and operating rooms before admission to the ICU.
Our study indicated a death rate of 46.05% in patients with head injuries during the COVID-19 pandemic (Table 1). This high mortality rate is by the study by Miękisiak et al., which also shows a 26.75% increase in the in-house mortality rate in the COVID period as compared to the pre-covid era. However, the incidence of TBI decreased during the COVID-19 period [9]. No comparable data existed at our hospital because no such study had been conducted before COVID-19. Some of the potential causes of the increased mortality in patients with head injury during the COVID-19 era were increased head injury severity, insufficient ICU beds, undertrained staff, lack of experience in managing pandemic situations, mismanagement of neurotrauma patients due to an overcrowded hospital, and cross-infection with COVID-19 patients since our ICU was a combined COVID-19 and trauma ICU. The number of patients with severe head injuries may have increased as mild to moderate head injuries were not reported to the hospital because of lockdown and concerns about patients visiting hospitals at the peak of the pandemic. Public reports also revealed that the severity of head injuries was higher during the COVID-19 pandemic [10, 11]. Possible reasons that have been cited for increased mortality in head injury patients during lockdown include an increased injury severity score and a low GCS at the time of trauma presentation [10]. Goyal et al. reported an increase in mortality from 12.4% to 22.5% in head injury patients during the COVID-19 pandemic as compared to the pre-COVID-19 period [12]. An increase in the severity of head traumas and related injuries caused this surge in mortality.
A study by Bagheri et al. observed an increase in the in-hospital mortality of elderly patients presenting with moderate to severe head injuries [13]. They noticed coronavirus and GCS as independent risk factors for in-hospital mortality. Damara et al., in their systemic review and analysis of 13 studies, found high mortality due to TBI in low- and middle-income countries. However, no change was observed in mortality in high-income countries during the COVID-19 pandemic [14]. This variation can be attributed to the relatively higher number of COVID-19 cases in underdeveloped nations and insufficient medical resources, which eventually burdened the healthcare system.
In contrast to our findings, Weber et al.’s observational cohort study revealed no significant difference in mortality during the pandemic compared to the pre-pandemic period [7]. The number of patients with severe traumatic brain injuries did not decrease during the pandemic, according to their study, which was conducted in the affluent nation of Norway. The same standard of care was provided throughout the pandemic, possibly due to better infrastructure. A study by Luostarinen et al. in Finland also revealed similar results in patients with TBI during the COVID-19 era, perhaps due to their advanced public health system and presumably improved care [15].
The results of the present study about demographic data revealed that TBI was more common in the economically productive age group [16, 17] (Figure 1). The average age was 37±14. It is well known that there are sex-related differences in TBI incidence. Of the patients in our study, 72.4% were men. Men are more likely to be exposed to injuries than women because they are more likely to engage in injury-prone work or dangerous behaviour. These results are consistent with the multicenter descriptive study by Eom et al., which found that 68.8% of all males had TBI [18].
RTA were the most common mode of injury, accounting for approximately 73.6% of cases. With the issuance of unlocking orders by the government, the movement of people on the road was permitted; thus, the incidence of RTA increased significantly. Other studies have also cited RTA as a major cause of TBI during pandemics [19-21].
Regarding management, most of the patients with TBI were treated conservatively, with only 18% requiring surgical intervention. A literature review also highlights similar findings, with many patients with TBI being managed conservatively during the COVID-19 pandemic [22]. Thinly stretched hospital resources, with most facilities diverted to COVID-19 ICUs and wards. A shortage of staff, equipment, and surgical facilities may have been the primary reasons for decreased surgical interventions during the pandemic.
5. Conclusion
The COVID-19 pandemic has had a significant impact on the management of patients with TBI. Despite a decrease in the number of admissions, high mortality rates have been noted in patients with TBI during the COVID-19 pandemic.
Limitations
This was a retrospective study of TBI patients during the COVID-19 pandemic. The analysis would have been better if we had compared it with pre-COVID-19 data. However, the same could not be done, as no such study was conducted during the pre-COVID-19 period. Since the data were retrieved from a single center, the results of the study cannot be generalized. However, our data might provide insights for larger multicenter trials exploring the pandemic’s impact on TBI patterns.
Ethical Considerations
Compliance with ethical guidelines
The study was conducted after obtaining approval from the Institutional Ethical Committee of Jawaharlal Nehru Medical College, Aligarh, India (Code: IEC/JNMC/2022/429).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, study design, data collection, data analysis and interpretation: Sobia Manaal Siddiqui; Drafting the article: Obaid Ahmad Siddiqui; Review and editing: Farah Nasreen; fina; approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Venkataram T, Goyal N, Kalita D, Bahurupi Y, Gangotri, Sadhasivam S, Set al. Deployment of neurosurgeons at the warfront against Coronavirus Disease of 2019 (COVID-19). World Neurosurgery. 2020; 144:e561-7. [doi:10.1016/j.wneu.2020.09.009] [PMID] [PMCID]
- Goyal N, Gupta K, Chaturvedi J, Swain SK, Tomy A. Getting neurosurgery services back on its feet: "learning to live" with COVID-19. Asian Journal of Neurosurgery. 2021; 16(2):340-8. [DOI:10.4103/ajns.AJNS_497_20] [PMID]
- Bavli I, Sutton B, Galea S. Harms of public health interventions against covid-19 must not be ignored. BMJ. 2020; 371:m4074. [DOI:10.1136/bmj.m4074] [PMID]
- Rosenbaum L. The untold toll - the pandemic's effects on patients without Covid-19. The New England Journal of Medicine. 2020; 382(24):2368-71. [DOI:10.1056/NEJMms2009984] [PMID]
- Menon DK, Schwab K, Wright DW, Maas AI. Position statement: Definition of traumatic brain injury. Archives of Physical Medicine and Rehabilitation. 2010; 91(11):1637-40. [DOI:10.1016/j.apmr.2010.05.017] [PMID]
- Peeters W, van den Brande R, Polinder S, Brazinova A, Steyerberg EW, Lingsma HF, et al. Epidemiology of traumatic brain injury in Europe. Acta Neurochirurgica. 2015; 157(10):1683-96. [DOI:10.1007/s00701-015-2512-7] [PMID]
- Weber C, Werner D, Thorsen K, Søreide K. Health care implications of the Covid-19 pandemic for patients with severe traumatic brain injury-a nationwide, observational cohort study. World Neurosurgery. 2022; 165:e452-6. [DOI:10.1016/j.wneu.2022.06.066] [PMID]
- Amir SH, Zafar L, Siddiqui OA, Nasreen F. Challenges in managing an emergency and trauma ICU during COVID-19 pandemic: Perspective from a tertiary care centre in western Uttar Pradesh (India). Bangladesh Journal of Medical Science. 2021; 20(Special Issue on Covid19):S26-31. [DOI:10.3329/bjms.v20i5.55397]
- Miękisiak G, Szarek D, Pettersson SD, Pezowicz C, Morasiewicz P, Kubaszewski Ł, et al. The increased mortality rate with lower incidence of traumatic brain injury during the Covid-19 pandemic: A national study. Healthcare. 2022; 10(10):1954. [DOI:10.3390/healthcare10101954] [PMID]
- Dash DD. Covid lockdown saved nearly 9,000 lives, 26,000 injuries on roads [internet]. 2020. [Updated 2025 March 8]. Available from: [Link]
- Yasin YJ, Grivna M, Abu-Zidan FM. Global impact of COVID-19 pandemic on road traffic collisions. World Journal of Emergency Surgery. 2021; 16(1):51. [DOI:10.1186/s13017-021-00395-8] [PMID]
- Goyal N, Swain SK, Gupta K, Chaturvedi J, Arora RK, Sharma SK. "Locked up inside home" - Head injury patterns during coronavirus disease of 2019 pandemic. Surgical Neurology International. 2020; 11:395. [DOI:10.25259/SNI_675_2020] [PMID]
- Reza Bagheri S, Abdi A, Benson J, Naghdi N, Eden SV, Arjmand M, et al. The significant impact of Coronavirus disease 2019 (COVID-19) on in-hospital mortality of elderly patients with moderate to severe traumatic brain injury: A retrospective observational study. Journal of clinical Neuroscience. 2021; 93:241-6. [DOI:10.1016/j.jocn.2021.09.029] [PMID]
- Damara FA, Muchamad GR, Anton A, Ramdhani AN, Channel IC, Faried A. Epidemiological pattern of traumatic brain injury in the Covid-19 pandemic: A systematic review and meta-analysis. World Neurosurgery. 2022; 161:e698-709. [DOI:10.1016/j.wneu.2022.02.081] [PMID]
- Luostarinen T, Virta J, Satopää J, Bäcklund M, Kivisaari R, Korja M, et al. Intensive care of traumatic brain injury and aneurysmal subarachnoid hemorrhage in Helsinki during the Covid-19 pandemic. Acta Neurochirurgica. 2020; 162(11):2715-24. [DOI:10.1007/s00701-020-04583-4] [PMID]
- Kirankumar MR, Satri V, Satyanarayana V, Ramesh Chandra VV, Madhusudan M, Sowjanya J. Demographic profile, clinical features, imaging and outcomes in patients with traumatic brain injury presenting to emergency room. Journal of Clinical and Scientific Research. 2019; 8(3):132-6. [DOI:10.4103/JCSR.JCSR_65_19]
- Lee KK, Seow WT, Ng I. Demographical profiles of adult severe traumatic brain injury patients: implications for healthcare planning. Singapore Medical Journal. 2006; 47(1):31-6. [PMID]
- Eom KS, Kim JH, Yoon SH, Lee SJ, Park KJ, Ha SK, et al. Gender differences in adult traumatic brain injury according to the Glasgow coma scale: A multicenter descriptive study. Chinese Journal of Traumatology. 2021; 24(6):333-43. [DOI:10.1016/j.cjtee.2021.06.004] [PMID]
- Lara-Reyna J, Yaeger KA, Rossitto CP, Camara D, Wedderburn R, Ghatan S, et al. "staying home"-early changes in patterns of Neurotrauma in new York City during the Covid-19 pandemic. World Neurosurgery. 2020; 143:e344-50. [DOI:10.1016/j.wneu.2020.07.155] [PMID]
- Goyal N, Venkataram T, Singh V, Chaturvedi J. Collateral damage caused by COVID-19: Change in volume and spectrum of neurosurgery patients. Journal of Clinical Neuroscience. 2020; 80:156-61. [DOI:10.1016/j.jocn.2020.07.055] [PMID]
- Inada H, Ashraf L, Campbell S. COVID-19 lockdown and fatal motor vehicle collisions due to speed-related traffic violations in Japan: A time-series study. Injury Prevention. 2021; 27(1):98-100. [DOI:10.1136/injuryprev-2020-043947] [PMID]
- Manivannan S, Sharouf F, Mayo I, Albaqer H, Mehrez M, Jaber H, et al. Management of neurotrauma during COVID-19: A single centre experience and lessons for the future. Brain injury. 2021; 35(8):957-63. [DOI:10.1080/02699052.2021.1934731] [PMID]
Type of Study: Research |
Subject:
Neurotrauma
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |