Sun, Feb 22, 2026
Volume 10 - Continuous Publishing
Iran J Neurosurg 2024, 10 - Continuous Publishing: 173-179 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Alizadeh S D, Jalalifar M, Mehmandoost S, Reihani-Kermani H. Trends in Traumatic Spine and Spinal Cord Injuries in Southeast Iran: A Ten-year Single-center Study. Iran J Neurosurg 2024; 10 : 20
URL: http://irjns.org/article-1-395-en.html
URL: http://irjns.org/article-1-395-en.html
Trends in Traumatic Spine and Spinal Cord Injuries in Southeast Iran: A Ten-year Single-center Study
Seyed Danial Alizadeh1 

 , Mohammad-Rasoul Jalalifar1
, Mohammad-Rasoul Jalalifar1 

 , Soheil Mehmandoost2
, Soheil Mehmandoost2 

 , Hamed Reihani-Kermani *3
, Hamed Reihani-Kermani *3 




 , Mohammad-Rasoul Jalalifar1
, Mohammad-Rasoul Jalalifar1 

 , Soheil Mehmandoost2
, Soheil Mehmandoost2 

 , Hamed Reihani-Kermani *3
, Hamed Reihani-Kermani *3 


1- Faculty of Medicine, Kerman University of Medical Sciences, Kerman, Iran.
2- HIV/STI Surveillance Research Center, WHO Collaborating Center for HIV Surveillance, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran
3- Department of Neurosurgery, Kerman University of Medical Sciences, Kerman, Iran. & Neuroscience Research Center, Kerman University of Medical Sciences, Kerman, Iran. ,h_reihani@hotmail.com
2- HIV/STI Surveillance Research Center, WHO Collaborating Center for HIV Surveillance, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran
3- Department of Neurosurgery, Kerman University of Medical Sciences, Kerman, Iran. & Neuroscience Research Center, Kerman University of Medical Sciences, Kerman, Iran. ,
Full Text [PDF 812 kb]
(741 Downloads)
| Abstract (HTML) (2553 Views)
Full Text: (770 Views)
1. Introduction
Traumatic spinal injury (TSI) is a crucial public health issue worldwide; specifically, injuries sustained to the spinal cord impose devastating effects on the physical, emotional, and socioeconomic conditions of individuals and their families [1, 2]. It is estimated that the annual global incidence of TSI is 10.5 cases per 100000 people and is higher in low- and middle-income countries [3]. In Iran, several studies have been conducted on traumatic spinal cord injury (SCI), and the incidence and prevalence of this have been reported at 10.5 per million people and 4.4 per 10000 people, respectively [4, 5].
Epidemiological data on TSI vary depending on each country and region due to their differences in culture, demographics, and socioeconomic conditions [6, 7]. The results of a study conducted over 3 years on 776 cases of spine injuries have shown that in Iran, the highest rate of TSI is related to lumbar injuries, most people are men, and car accidents are the most common mechanism of injury [8].
Investigations on TSI have been restricted to a short-term period, and the data on trending over time remains few in the previous studies [9, 10]. Clinicians and health care systems should be aware of the TSI pattern in the management and rehabilitation of patients, developing practice guidelines, and injury prevention [2, 10].
Hence, a medical records study was conducted at Bahonar Academic Hospital, the main referral hospital for spine trauma in Kerman Province, Iran. This study was conducted to demonstrate TSI patients’ characteristics and describe the epidemiologic trending of TSI and SCI over ten years.
2. Methods and Materials/Patients
A retrospective analysis was conducted among patients who were admitted to the spine trauma center of Bahonar Hospital, the main referral hospital for trauma in Kerman City, Iran. The study included all patients with spine injuries between January 2013 and December 2022.
Data collection
All hospitalized patients with TSI were included in the study. We reviewed the medical records, and patient information was obtained. A TSI was considered any fracture and or dislocation. For each patient, we considered gender, age, level of injury, and neurological status using the American Spinal Injury Association (ASIA), the leading cause of injury, including falling, accidents (pedestrian, motorcycle, car, pickup truck, van, heavy transport vehicle, and bus crushed injured), location of injury (inside or outside of the city), and type of treatment (surgical or non-surgical). Some data were collected based on computerized tomography (CT) scan reports, such as injury level. SCI and neurological status were obtained based on magnetic resonance imaging (MRI) reports and clinical evaluations. The exclusion criteria included readmissions and incomplete medical records.
Definitions
Following the inclusion of all patients with TSI detected by CT scan and or MRI, SCI was identified by MRI and a standardized neurological physical examination using the international standards for neurological classification of spinal cord injury. Next, the degree of impairment reported with ASIA is the following: A is complete impairment, B is sensory incomplete impairment, C is motor incomplete impairment, D is motor incomplete impairment, and E is normal. An ASIA grade is not given to someone without a SCI [11].
Statistical analysis
To present descriptive statistics for outcome variables and covariates, they have been reported by absolute and relative frequencies with 95% confidence intervals (95% CI) with the normal method. The covariates with a P<0.2 in the chi-squered test were imported into the multivariable logistic regression model. To reach the final model, the backward elimination method was used, and a P<0.05 was considered the statistical significance level. Stata software, version 17.0 (Stata Corp., College Station, TX) was used for all of the statistical analyses.
3. Results
The medical records of 1494 patients with TSI were included over a decade. The results of the analysis were divided into four subsections, age and gender, SCI, level of TSI, etiology, location, and treatments. Table 1 summarizes the data about variables and their associations as well.
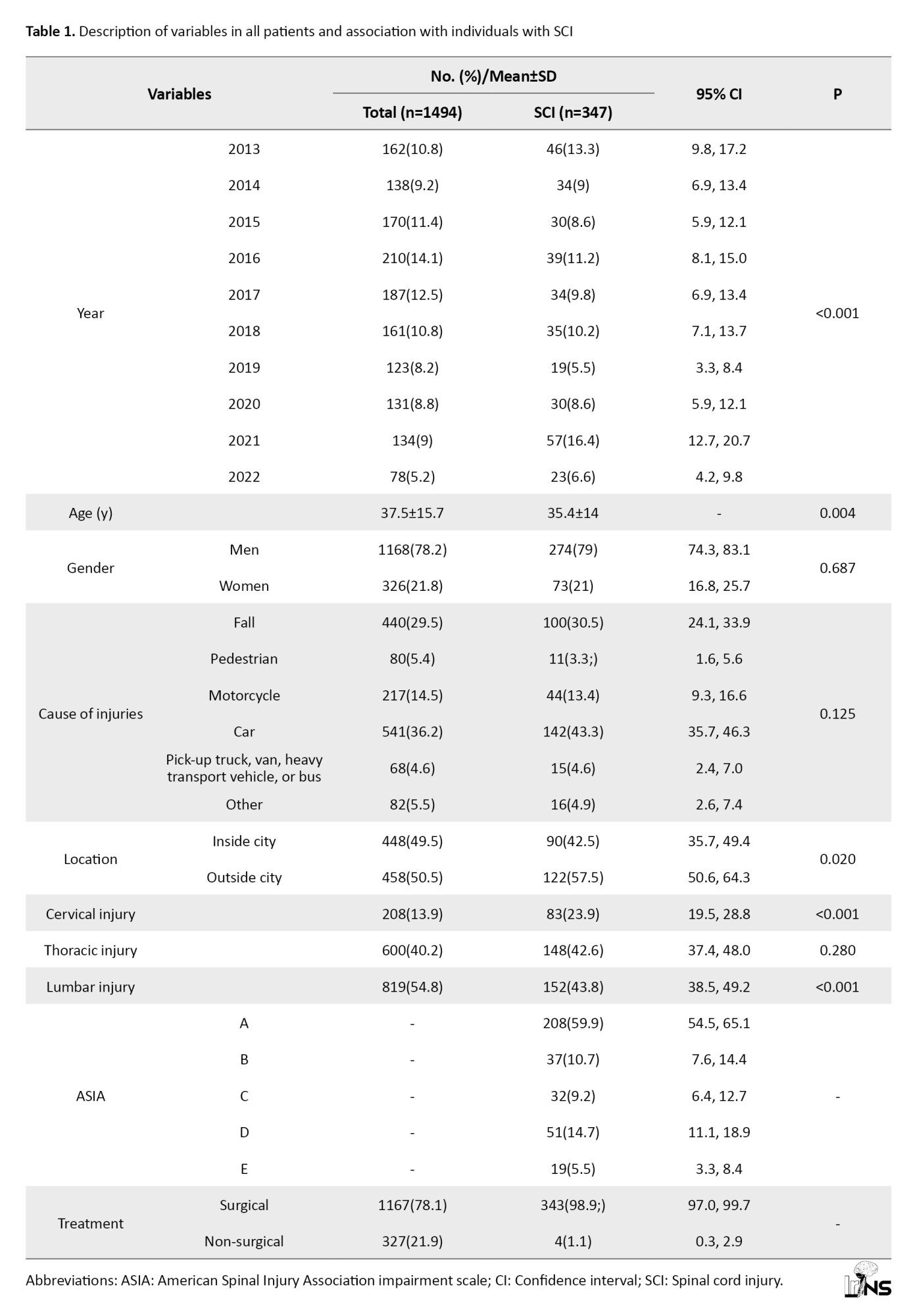
Age and gender
Of the 1494 patients with TSI, 1168(78.2%) were men; the male-to-female ratio was 3.6:1. No significant relationship was observed between gender and SCI (P=0.687). The Mean±SD of the age of the patients was 37.5±15.7 years. The Mean±SD of the age of SCI patients was 35.4±14.0 years; it was 38.2±16.2 years for those without SCI, therefore patients with SCI are younger than other group significantly (P=0.004) (Table 1). The mean male-to-female ratio remained constant over ten years and did not show any statistical significance (P=0.831).
Level of TSI and SCI
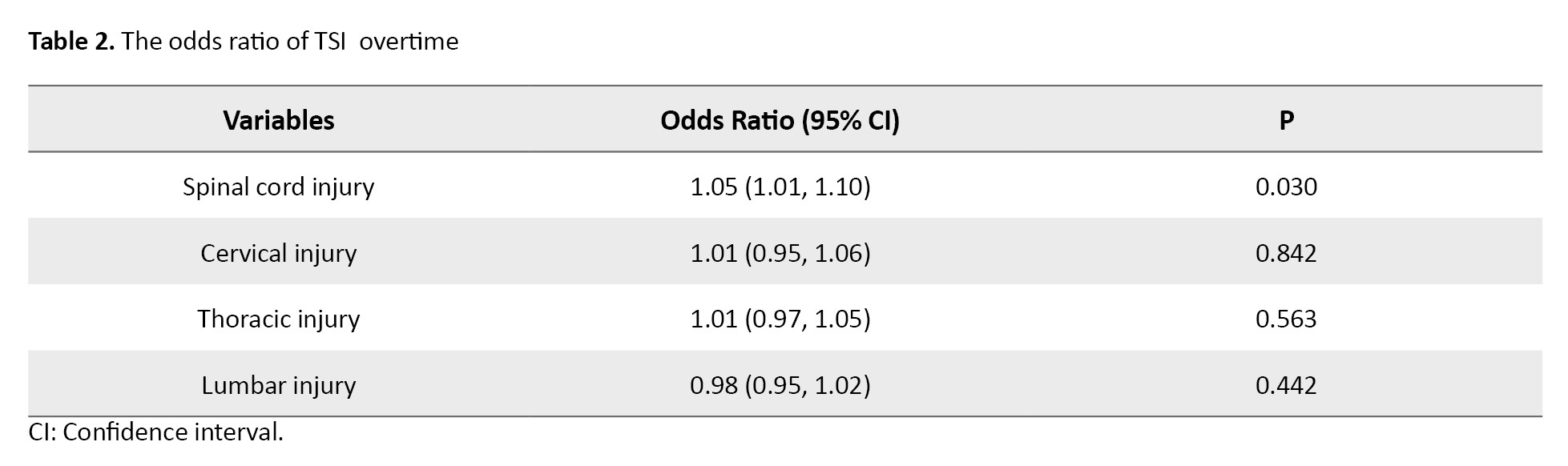
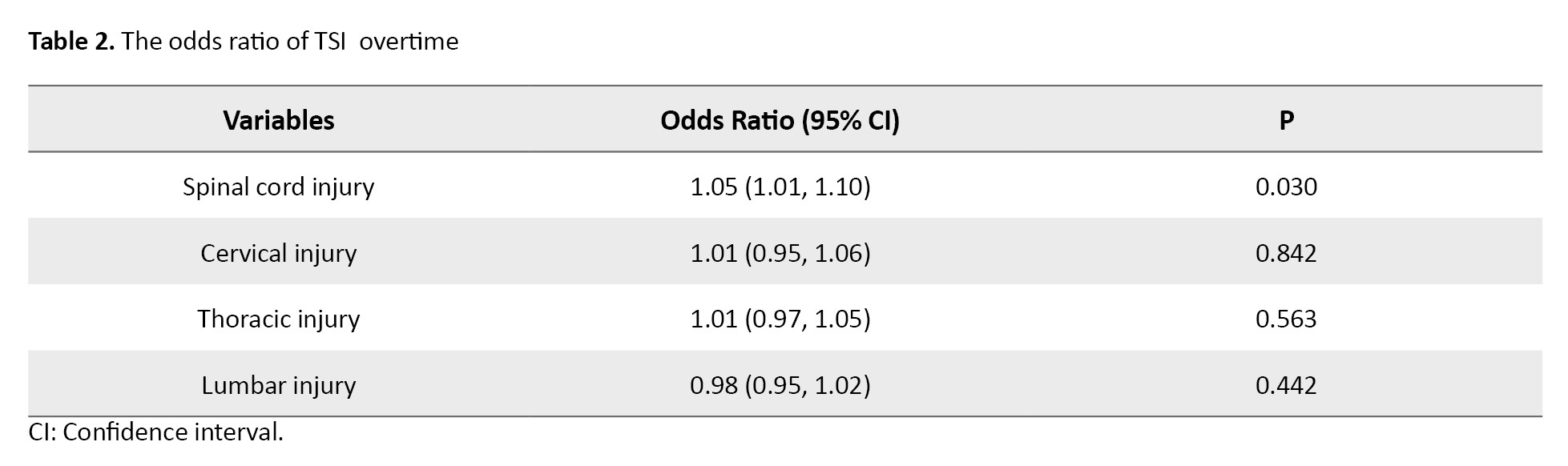
The prevalence of SCI was 23.2% (n=347). During ten years, the mean number of cervical, thoracic, and lumbar injuries is 21±6.5, 60±17·.2, and 82±21, respectively, however, no significant trend existed among cervical, thoracic, or lumbar injuries over time (P=0.842, P=0.563, and P=0.442, respectively). The lumbar spine was the most frequent site of injury (n=819, 54.8%), followed by the thoracic 40.2% (n=600) and the cervical spine 13.9% (n=208). Our analysis revealed that cervical and thoracic spine injuries were significantly correlated with SCI (P<0.001) (Table 1). Cervical and lumbar spine injuries were also more common in the group without SCI (n=125, 60%, and n=667, 81.4%, respectively) than in the SCI group (40%, n=83, and 18.6%, n=152, respectively). The odds ratio (OR) of SCI has increased over ten years by 5% (Table 2).
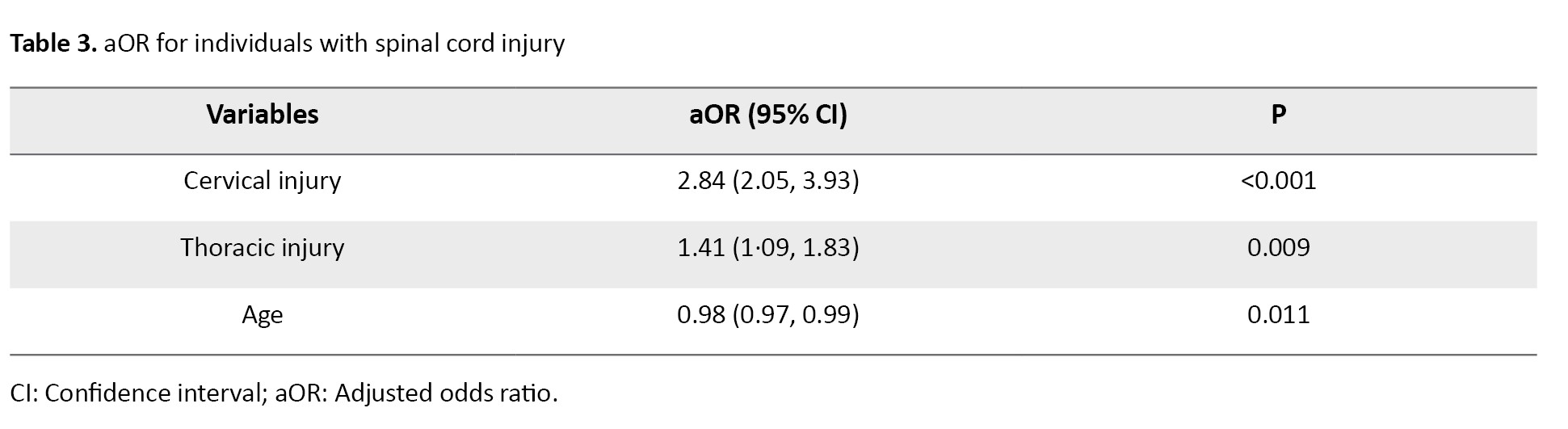
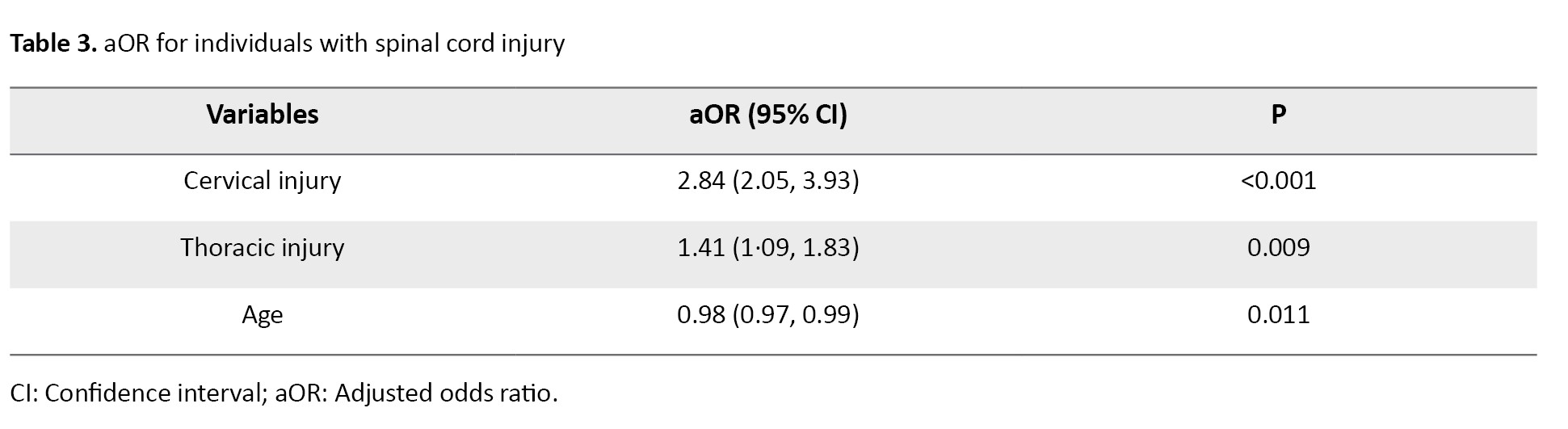
The results of the multivariable logistic regression model indicated that SCI was significantly associated with cervical injury (adjusted odds ratio [aOR]=2.84) thoracic injury (aOR=1.41), and age (aOR=0.98) (Table 3).
The ASIA was used to assess the degree of neurological deficit upon admission. A total of 208 SCI patients (59.9%) were categorized as ASIA A, and 139(40.1%) were categorized as ASIA B, C, D, or E (10.7%, 9.2%, 14.7%, and 5.5%, respectively) (Table 1).
The leading cause, location, and treatment of TSI
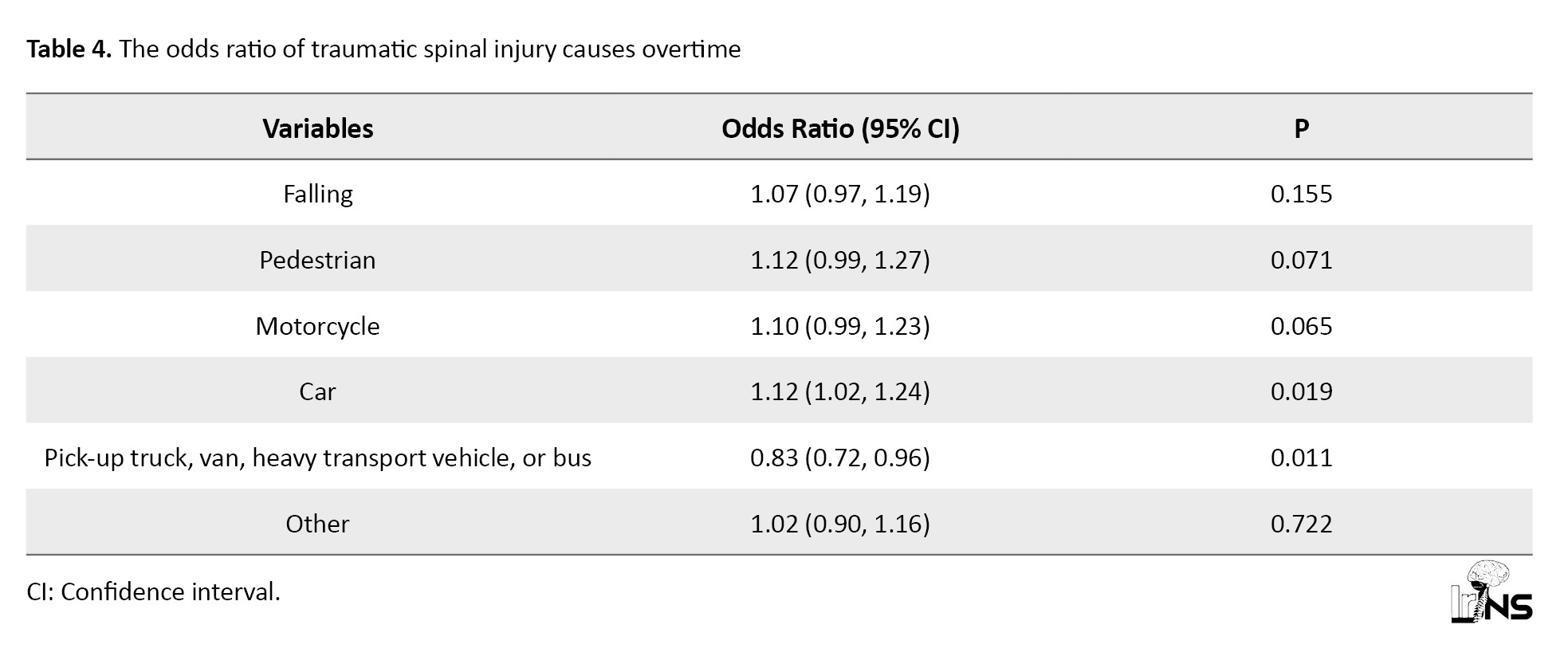
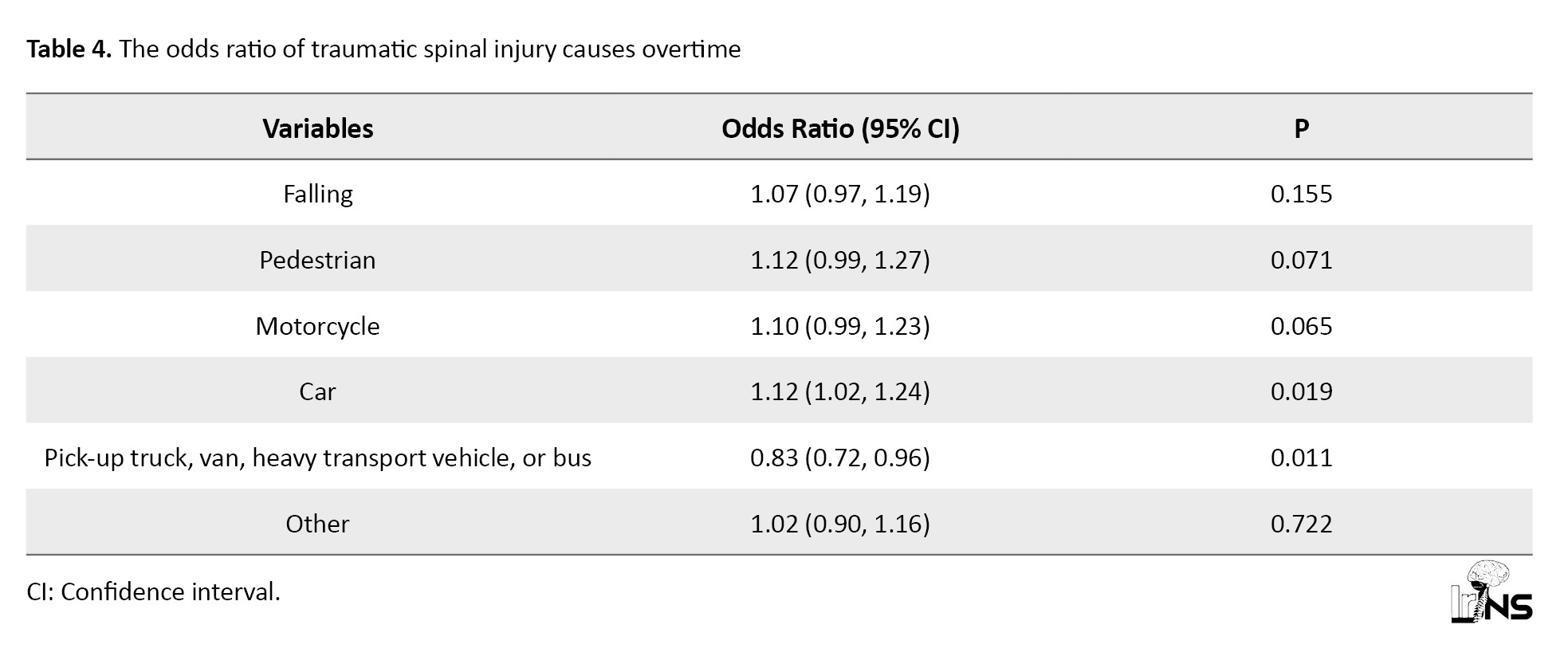
No relationship was observed between the top five leading causes of TSI and SCI (P=0.125), car accidents (36.2%), falls (29.5%), motorcycle crashes (14.5%), pedestrian (5.4%), pickup trucks, vans, heavy transport vehicles, and buses (4.6%) (Table 1). Car occupants had a higher probability of SCI over ten years by 12%, while it decreased for occupants of pickup trucks, vans, heavy transport vehicles, and buses over a decade by 7% (Table 4).
Among traffic accident causes, the location of TSI was 50.5% in the suburb and 49.5% in the city; however, SCI was significantly more common in the suburb than in the city (57.5%, n=122, P=0.020). A surgical procedure was performed for 1167 patients with TSI (78.1%). It was revealed that most TSI patients who were surgically treated (70.6%, n=824) without SCI (Table 1).
4. Discussion
This study revealed no gender-SCI correlation. Patients with SCI are much younger. In the past decade, SCI odds increased significantly. The lumbar spine was injured the most, followed by the thoracic and cervical. We found that SCI was significantly linked with cervical and thoracic spine injuries. Non-SCI patients had greater cervical and lumbar spine injuries than SCI patients. The risk of SCI is much higher for cervical and thoracic than for lumbar spine injuries. No significant trend was found in cervical, thoracic, and lumbar injuries over time. No correlation was observed between the top five TSI and SCI causes. Car occupants had a 12% higher risk of SCI over ten years, while pickup truck, van, large transport vehicle, and bus occupants had a 7% lower risk. Among traffic accident causes, SCI was more common in the suburban areas. The most surgically treated TSI patients had no SCI.
Most TSI patients were men, which is consistent with other studies due to dangerous occupations and more risky behavior [3, 5, 8]. The mean age of SCI in Iran was 35.8±1.07 years in one study [4] and 33.2±14.3 years in another study [5]. Therefore, it is crucial to pay more attention to young people. Our result regarding the leading causes was consistent with the global investigated results that traffic accidents and falls were the main causes of TSI worldwide [3]. Although another study in Iran reported that 45.7% of injuries were caused by falling, followed by road traffic crashes (40.6%), the most common cause of tetraplegia was road traffic crashes [5]. Also, as they mentioned, SCI occurred more commonly in outside of the city, as we found. In our survey, car occupants had a higher probability of TSI over the years.
The incidence rate of SCI is 10.5 cases per million in Iran [5], while the overall incidence rate of SCI in the United States is 84.9 cases per million [12]. Algahtany et al. [9] and Selassie et al. [13] reported in a similar trend study that SCI increased significantly from 2002–2017 and 1998-2012, respectively.
The in-hospital mortality following cervical SCI in patients with ASIA A was 20.6%, and the mortality for ASIA B, C, and D was 9.3%, 0.05%, and 0.2%, respectively [14].
Chen et al. mentioned that the level of SCI most frequently occurred in the cervical spine (~60%), followed by the thoracic (32%), and lumbosacral (9%) in the United States [15]. In a study conducted in South Africa, 74% involvement of the thoracic and lumbar and 26% cervical injuries were observed [16]. Most patients were treated surgically in our survey. Despite increasing acceptance of early surgery post-SCI, further research is needed to identify subgroups of patients who derive particular benefits [17].
5. Conclusion
In conclusion, our extensive ten-year investigation of TSI and SCIs in the main referral spine trauma center of Southeast Iran from 2013 to 2022 has unveiled insights into the epidemiologic trends. This research underscores the pressing public health significance of spinal injuries, particularly SCI, and the profound impact on individuals’ lives and well-being. The study’s results reveal the increasing odds of SCIs and highlight the relevance of age, level of injury, and predominant leading causes.
In this scientific article, it is crucial to acknowledge the following limitations, this study was conducted as a retrospective analysis of medical records, which may introduce potential biases and limit the ability to establish causal relationships and prevent the collection of detailed information on the long-term outcomes and quality of life for individuals with TSIs, which would be valuable for a more comprehensive understanding of the impact of these injuries. Additionally, the data were collected from a single center and limited to a specific geographic region in Southeast Iran, which may not fully represent the broader population of traumatic spinal injury cases in the region or the country. Despite these limitations, the study provides essential insights into the characteristics and trends of TSI and SCIs in the region and serves as a foundation for future research and policy development.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of the Kerman University of Medical Sciences, Kerman, Iran (Code: IR.KMU.AH.REC.1400.154).
Funding
This research received no grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Hamed Reihani-Kermani; Data collection: Mohammad-Rasoul Jalalifar, Seyed Danial Alizadeh; Data analysis and interpretation: Soheil Mehmandoost; Drafting the article: Mohammad-Rasoul Jalalifar, Seyed Danial Alizadeh; Review and editing: Hamed Reihani-Kermani, Mohammad-Rasoul Jalalifar, Seyed Danial Alizadeh, Soheil Mehmandoost; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors extend their heartfelt gratitude to the patients who participated in this study, your participation made this research possible! The authors also express their deep appreciation to the dedicated doctors, and nurses whose tireless efforts contributed to the success of this study.
References
Traumatic spinal injury (TSI) is a crucial public health issue worldwide; specifically, injuries sustained to the spinal cord impose devastating effects on the physical, emotional, and socioeconomic conditions of individuals and their families [1, 2]. It is estimated that the annual global incidence of TSI is 10.5 cases per 100000 people and is higher in low- and middle-income countries [3]. In Iran, several studies have been conducted on traumatic spinal cord injury (SCI), and the incidence and prevalence of this have been reported at 10.5 per million people and 4.4 per 10000 people, respectively [4, 5].
Epidemiological data on TSI vary depending on each country and region due to their differences in culture, demographics, and socioeconomic conditions [6, 7]. The results of a study conducted over 3 years on 776 cases of spine injuries have shown that in Iran, the highest rate of TSI is related to lumbar injuries, most people are men, and car accidents are the most common mechanism of injury [8].
Investigations on TSI have been restricted to a short-term period, and the data on trending over time remains few in the previous studies [9, 10]. Clinicians and health care systems should be aware of the TSI pattern in the management and rehabilitation of patients, developing practice guidelines, and injury prevention [2, 10].
Hence, a medical records study was conducted at Bahonar Academic Hospital, the main referral hospital for spine trauma in Kerman Province, Iran. This study was conducted to demonstrate TSI patients’ characteristics and describe the epidemiologic trending of TSI and SCI over ten years.
2. Methods and Materials/Patients
A retrospective analysis was conducted among patients who were admitted to the spine trauma center of Bahonar Hospital, the main referral hospital for trauma in Kerman City, Iran. The study included all patients with spine injuries between January 2013 and December 2022.
Data collection
All hospitalized patients with TSI were included in the study. We reviewed the medical records, and patient information was obtained. A TSI was considered any fracture and or dislocation. For each patient, we considered gender, age, level of injury, and neurological status using the American Spinal Injury Association (ASIA), the leading cause of injury, including falling, accidents (pedestrian, motorcycle, car, pickup truck, van, heavy transport vehicle, and bus crushed injured), location of injury (inside or outside of the city), and type of treatment (surgical or non-surgical). Some data were collected based on computerized tomography (CT) scan reports, such as injury level. SCI and neurological status were obtained based on magnetic resonance imaging (MRI) reports and clinical evaluations. The exclusion criteria included readmissions and incomplete medical records.
Definitions
Following the inclusion of all patients with TSI detected by CT scan and or MRI, SCI was identified by MRI and a standardized neurological physical examination using the international standards for neurological classification of spinal cord injury. Next, the degree of impairment reported with ASIA is the following: A is complete impairment, B is sensory incomplete impairment, C is motor incomplete impairment, D is motor incomplete impairment, and E is normal. An ASIA grade is not given to someone without a SCI [11].
Statistical analysis
To present descriptive statistics for outcome variables and covariates, they have been reported by absolute and relative frequencies with 95% confidence intervals (95% CI) with the normal method. The covariates with a P<0.2 in the chi-squered test were imported into the multivariable logistic regression model. To reach the final model, the backward elimination method was used, and a P<0.05 was considered the statistical significance level. Stata software, version 17.0 (Stata Corp., College Station, TX) was used for all of the statistical analyses.
3. Results
The medical records of 1494 patients with TSI were included over a decade. The results of the analysis were divided into four subsections, age and gender, SCI, level of TSI, etiology, location, and treatments. Table 1 summarizes the data about variables and their associations as well.
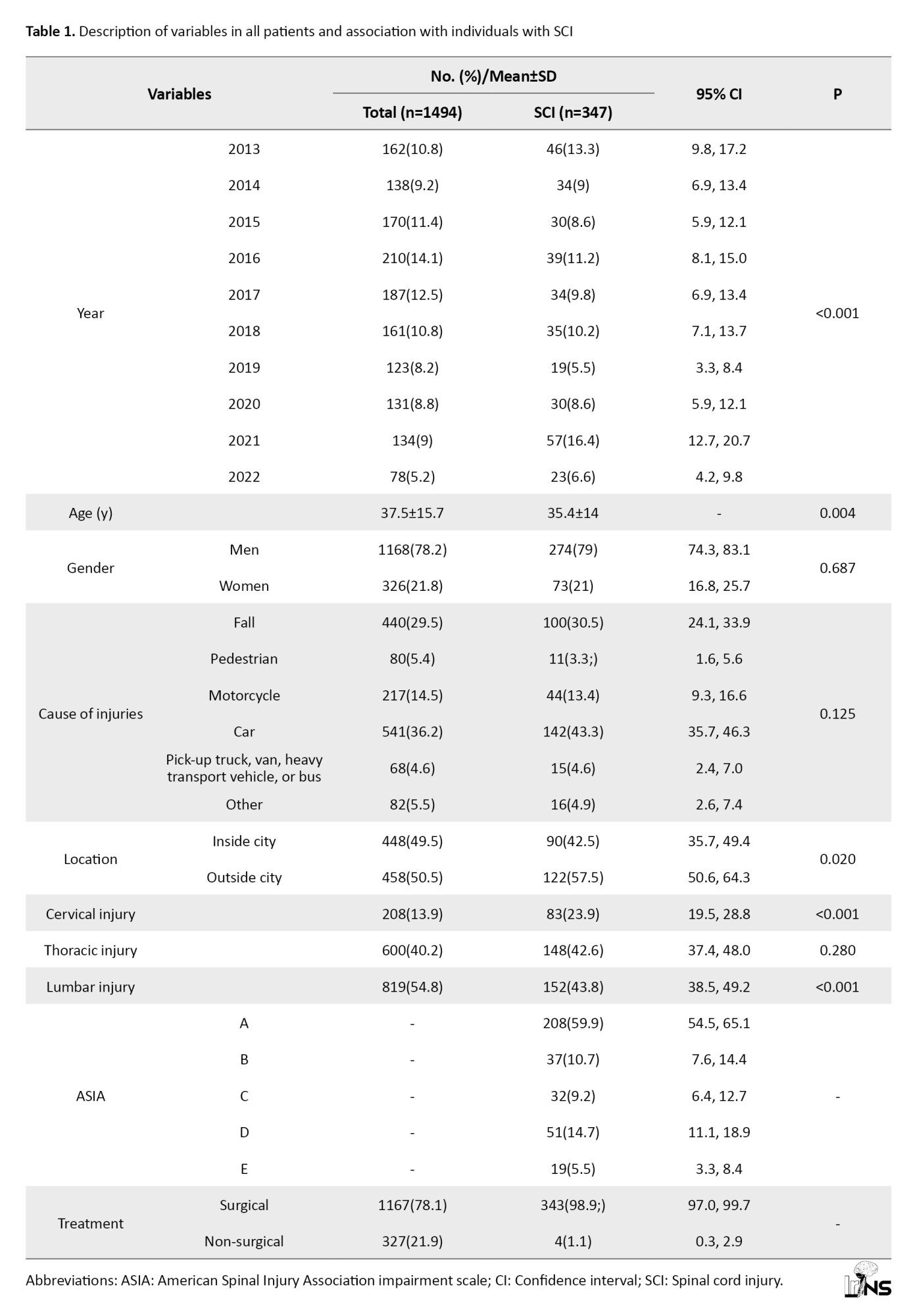
Age and gender
Of the 1494 patients with TSI, 1168(78.2%) were men; the male-to-female ratio was 3.6:1. No significant relationship was observed between gender and SCI (P=0.687). The Mean±SD of the age of the patients was 37.5±15.7 years. The Mean±SD of the age of SCI patients was 35.4±14.0 years; it was 38.2±16.2 years for those without SCI, therefore patients with SCI are younger than other group significantly (P=0.004) (Table 1). The mean male-to-female ratio remained constant over ten years and did not show any statistical significance (P=0.831).
Level of TSI and SCI
The prevalence of SCI was 23.2% (n=347). During ten years, the mean number of cervical, thoracic, and lumbar injuries is 21±6.5, 60±17·.2, and 82±21, respectively, however, no significant trend existed among cervical, thoracic, or lumbar injuries over time (P=0.842, P=0.563, and P=0.442, respectively). The lumbar spine was the most frequent site of injury (n=819, 54.8%), followed by the thoracic 40.2% (n=600) and the cervical spine 13.9% (n=208). Our analysis revealed that cervical and thoracic spine injuries were significantly correlated with SCI (P<0.001) (Table 1). Cervical and lumbar spine injuries were also more common in the group without SCI (n=125, 60%, and n=667, 81.4%, respectively) than in the SCI group (40%, n=83, and 18.6%, n=152, respectively). The odds ratio (OR) of SCI has increased over ten years by 5% (Table 2).
The results of the multivariable logistic regression model indicated that SCI was significantly associated with cervical injury (adjusted odds ratio [aOR]=2.84) thoracic injury (aOR=1.41), and age (aOR=0.98) (Table 3).
The ASIA was used to assess the degree of neurological deficit upon admission. A total of 208 SCI patients (59.9%) were categorized as ASIA A, and 139(40.1%) were categorized as ASIA B, C, D, or E (10.7%, 9.2%, 14.7%, and 5.5%, respectively) (Table 1).
The leading cause, location, and treatment of TSI
No relationship was observed between the top five leading causes of TSI and SCI (P=0.125), car accidents (36.2%), falls (29.5%), motorcycle crashes (14.5%), pedestrian (5.4%), pickup trucks, vans, heavy transport vehicles, and buses (4.6%) (Table 1). Car occupants had a higher probability of SCI over ten years by 12%, while it decreased for occupants of pickup trucks, vans, heavy transport vehicles, and buses over a decade by 7% (Table 4).
Among traffic accident causes, the location of TSI was 50.5% in the suburb and 49.5% in the city; however, SCI was significantly more common in the suburb than in the city (57.5%, n=122, P=0.020). A surgical procedure was performed for 1167 patients with TSI (78.1%). It was revealed that most TSI patients who were surgically treated (70.6%, n=824) without SCI (Table 1).
4. Discussion
This study revealed no gender-SCI correlation. Patients with SCI are much younger. In the past decade, SCI odds increased significantly. The lumbar spine was injured the most, followed by the thoracic and cervical. We found that SCI was significantly linked with cervical and thoracic spine injuries. Non-SCI patients had greater cervical and lumbar spine injuries than SCI patients. The risk of SCI is much higher for cervical and thoracic than for lumbar spine injuries. No significant trend was found in cervical, thoracic, and lumbar injuries over time. No correlation was observed between the top five TSI and SCI causes. Car occupants had a 12% higher risk of SCI over ten years, while pickup truck, van, large transport vehicle, and bus occupants had a 7% lower risk. Among traffic accident causes, SCI was more common in the suburban areas. The most surgically treated TSI patients had no SCI.
Most TSI patients were men, which is consistent with other studies due to dangerous occupations and more risky behavior [3, 5, 8]. The mean age of SCI in Iran was 35.8±1.07 years in one study [4] and 33.2±14.3 years in another study [5]. Therefore, it is crucial to pay more attention to young people. Our result regarding the leading causes was consistent with the global investigated results that traffic accidents and falls were the main causes of TSI worldwide [3]. Although another study in Iran reported that 45.7% of injuries were caused by falling, followed by road traffic crashes (40.6%), the most common cause of tetraplegia was road traffic crashes [5]. Also, as they mentioned, SCI occurred more commonly in outside of the city, as we found. In our survey, car occupants had a higher probability of TSI over the years.
The incidence rate of SCI is 10.5 cases per million in Iran [5], while the overall incidence rate of SCI in the United States is 84.9 cases per million [12]. Algahtany et al. [9] and Selassie et al. [13] reported in a similar trend study that SCI increased significantly from 2002–2017 and 1998-2012, respectively.
The in-hospital mortality following cervical SCI in patients with ASIA A was 20.6%, and the mortality for ASIA B, C, and D was 9.3%, 0.05%, and 0.2%, respectively [14].
Chen et al. mentioned that the level of SCI most frequently occurred in the cervical spine (~60%), followed by the thoracic (32%), and lumbosacral (9%) in the United States [15]. In a study conducted in South Africa, 74% involvement of the thoracic and lumbar and 26% cervical injuries were observed [16]. Most patients were treated surgically in our survey. Despite increasing acceptance of early surgery post-SCI, further research is needed to identify subgroups of patients who derive particular benefits [17].
5. Conclusion
In conclusion, our extensive ten-year investigation of TSI and SCIs in the main referral spine trauma center of Southeast Iran from 2013 to 2022 has unveiled insights into the epidemiologic trends. This research underscores the pressing public health significance of spinal injuries, particularly SCI, and the profound impact on individuals’ lives and well-being. The study’s results reveal the increasing odds of SCIs and highlight the relevance of age, level of injury, and predominant leading causes.
In this scientific article, it is crucial to acknowledge the following limitations, this study was conducted as a retrospective analysis of medical records, which may introduce potential biases and limit the ability to establish causal relationships and prevent the collection of detailed information on the long-term outcomes and quality of life for individuals with TSIs, which would be valuable for a more comprehensive understanding of the impact of these injuries. Additionally, the data were collected from a single center and limited to a specific geographic region in Southeast Iran, which may not fully represent the broader population of traumatic spinal injury cases in the region or the country. Despite these limitations, the study provides essential insights into the characteristics and trends of TSI and SCIs in the region and serves as a foundation for future research and policy development.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of the Kerman University of Medical Sciences, Kerman, Iran (Code: IR.KMU.AH.REC.1400.154).
Funding
This research received no grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Hamed Reihani-Kermani; Data collection: Mohammad-Rasoul Jalalifar, Seyed Danial Alizadeh; Data analysis and interpretation: Soheil Mehmandoost; Drafting the article: Mohammad-Rasoul Jalalifar, Seyed Danial Alizadeh; Review and editing: Hamed Reihani-Kermani, Mohammad-Rasoul Jalalifar, Seyed Danial Alizadeh, Soheil Mehmandoost; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors extend their heartfelt gratitude to the patients who participated in this study, your participation made this research possible! The authors also express their deep appreciation to the dedicated doctors, and nurses whose tireless efforts contributed to the success of this study.
References
- Choi JH, Park PJ, Din V, Sam N, Iv V, Park KB. Epidemiology and clinical management of traumatic spine injuries at a major government hospital in Cambodia. Asian Spine Journal. 2017; 11(6):908-16. [DOI:10.4184/asj.2017.11.6.908] [PMID] [PMCID]
- Kattail D, Furlan JC, Fehlings MG. Epidemiology and clinical outcomes of acute spine trauma and spinal cord injury: Experience from a specialized spine trauma center in Canada in comparison with a large national registry. The Journal of Trauma. 2009; 67(5):936-43. [DOI:10.1097/TA.0b013e3181a8b431] [PMID]
- Kumar R, Lim J, Mekary RA, Rattani A, Dewan MC, Sharif SY, et al. Traumatic spinal injury: Global epidemiology and worldwide volume. World Neurosurgery. 2018; 113:e345-63. [DOI:10.1016/j.wneu.2018.02.033] [PMID]
- Saheban Maleki M, Khedri B, Ebrahimpour Roodposhti M, Askari Majdabadi H, Seyedrezaei SO, Amanat N, et al. Epidemiology of traumatic spinal cord injuries in Iran; A systematic review and meta-analysis. Archives of Academic Emergency Medicine. 2022; 10(1):e80. [DOI:10.18502/ijph.v52i9.13565]
- Sharif-Alhoseini M, Rahimi-Movaghar V. Hospital-based incidence of traumatic spinal cord injury in Tehran, Iran. Iranian Journal of Public Health. 2014; 43(3):331-41. [PMID]
- Algahtany MA. Epidemiology, trend and in-hospital outcome of traumatic spinal injuries due to road traffic accidents. Pakistan Journal of Medical Sciences. 2022; 38(3):492-7. [DOI:10.12669/pjms.38.3.5288]
- Tee JW, Chan CH, Fitzgerald MC, Liew SM, Rosenfeld JV. Epidemiological trends of spine trauma: An Australian level 1 trauma centre study. Global Spine Journal. 2013; 3(2):75-84. [DOI:10.1055/s-0033-1337124] [PMID] [PMCID]
- Yadollahi M, Karajizadeh M, Bordbar N, Ghahramani Z. Incidence and pattern of traumatic spine injury in a single level I trauma center of southern Iran. Chinese Journal of Traumatology. 2023; 26(4):199-203. [DOI:10.1016/j.cjtee.2023.01.001] [PMID] [PMCID]
- Algahtany M, McFaull S, Chen L, Zhang S, Saarela O, Alqahtani F, et al. The changing etiology and epidemiology of traumatic spinal injury: A population-based study. World Neurosurgery. 2021; 149:e116-27. [DOI:10.1016/j.wneu.2021.02.066] [PMID]
- Pirouzmand F. Epidemiological trends of spine and spinal cord injuries in the largest Canadian adult trauma center from 1986 to 2006. Journal of Neurosurgery. Spine. 2010; 12(2):131-40. [DOI:10.3171/2009.9.SPINE0943] [PMID]
- Rupp R, Biering-Sørensen F, Burns SP, Graves DE, Guest J, Jones L, et al. International standards for neurological classification of spinal cord injury: Revised 2019. Topics in Spinal Cord Injury Rehabilitation. 2021; 27(2):1-22. [DOI:10.46292/sci2702-1] [PMID] [PMCID]
- Jazayeri SB, Maroufi SF, Mohammadi E, Dabbagh Ohadi MA, Hagen EM, Chalangari M, et al. Incidence of traumatic spinal cord injury worldwide: A systematic review, data integration, and update. World Neurosurgery: X. 2023; 18:100171. [DOI:10.1016/j.wnsx.2023.100171] [PMID] [PMCID]
- Selassie A, Cao Y, Saunders LL. Epidemiology of traumatic spinal cord injury among persons older than 21 years: A population-based study in South Carolina, 1998-2012. Topics in Spinal cord Injury Rehabilitation. 2015; 21(4):333-44. [DOI:10.1310/sci2015-313] [PMID] [PMCID]
- Sadeghi-Naini M, Yousefifard M, Ghodsi Z, Azarhomayoun A, Kermanian F, Golpayegani M, et al. In-hospital mortality rate in subaxial cervical spinal cord injury patients: A systematic review and meta-analysis. Acta Neurochirurgica. 2023; 165(9):2675-88. [DOI:10.1007/s00701-023-05720-5] [PMID]
- Chen Y, He Y, DeVivo MJ. Changing demographics and injury profile of new traumatic spinal cord injuries in the United States, 1972-2014. Archives of Physical Medicine and Rehabilitation. 2016; 97(10):1610-9. [DOI:10.1016/j.apmr.2016.03.017] [PMID]
- Velmahos GC, Degiannis E, Hart K, Souter I, Saadia R. Changing profiles in spinal cord injuries and risk factors influencing recovery after penetrating injuries. The Journal of Trauma. 1995; 38(3):334-7. [DOI:10.1097/00005373-199503000-00004] [PMID]
- Wilson JR, Witiw CD, Badhiwala J, Kwon BK, Fehlings MG, Harrop JS. Early surgery for traumatic spinal cord injury: Where are we now? Global Spine Journal. 2020; 10(1 Suppl):84S-91. [DOI:10.1177/2192568219877860] [PMID] [PMCID]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |



