Thu, Feb 5, 2026
Volume 10 - Continuous Publishing
Iran J Neurosurg 2024, 10 - Continuous Publishing: 180-187 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sanie Jahromi M S, Zarei M, Taheri L, Deylami M, Kalani N. Tracheal Tube Cuff Pressure Measurement Methods in Lumbar Disc Surgery. Iran J Neurosurg 2024; 10 : 21
URL: http://irjns.org/article-1-403-en.html
URL: http://irjns.org/article-1-403-en.html
Mohammad Sadegh Sanie Jahromi1 

 , Meysam Zarei2
, Meysam Zarei2 

 , Lohrasb Taheri3
, Lohrasb Taheri3 

 , Mansour Deylami4
, Mansour Deylami4 

 , Navid Kalani *5
, Navid Kalani *5 




 , Meysam Zarei2
, Meysam Zarei2 

 , Lohrasb Taheri3
, Lohrasb Taheri3 

 , Mansour Deylami4
, Mansour Deylami4 

 , Navid Kalani *5
, Navid Kalani *5 


1- Department of Anesthesiology, Jahrom University of medical sciences, Jahrom, Iran.
2- Student Research Committee, Jahrom University of Medical Sciences, Jahrom, Iran.
3- Department of Surgery, Jahrom University of Medical Sciences, Jahrom, Iran.
4- Department of Anesthesiology and Critical Care, Faculty of Medicine, Golestan University of Medical Sciences, Gorgan, Iran.
5- Department of Anesthesiology, Jahrom University of medical sciences, Jahrom, Iran. ,navidkalani@ymail.com
2- Student Research Committee, Jahrom University of Medical Sciences, Jahrom, Iran.
3- Department of Surgery, Jahrom University of Medical Sciences, Jahrom, Iran.
4- Department of Anesthesiology and Critical Care, Faculty of Medicine, Golestan University of Medical Sciences, Gorgan, Iran.
5- Department of Anesthesiology, Jahrom University of medical sciences, Jahrom, Iran. ,
Full Text [PDF 941 kb]
(641 Downloads)
| Abstract (HTML) (2299 Views)
Full Text: (157 Views)
1. Introduction
Tracheal tubes are designed to establish a secure airway in adult patients, featuring a distal cuff that, when inflated, acts as a barrier to the tracheal wall. This inflation prevents pulmonary aspiration, ensuring the delivery of the intended flow volume to the lungs. The tracheal tube size is determined by its inner diameter, measured in millimeters; however, the relationship with the outer diameter varies across different production designs. The inflation of the tracheal tube cuff forms a barrier between the tube and the tracheal wall, eliminating air leakage during positive pressure ventilation and safeguarding the lungs against aspiration. Earlier tracheal tube cuffs, characterized by high pressure, exerted considerable force on tracheal mucus, leading to ischemia. Contemporary endotracheal tubes incorporate low-pressure cuffs to minimize pressure on the trachea, consequently reducing the risk of ischemia [1]. Maintaining cuff pressure within the range of 20-30 cm of water is crucial to minimize air leakage, preserve flow volume, and prevent damage to the tracheal mucosa [2]. Studies indicate that at a cuff pressure of 25 cm of water, tracheal blood flow remains normal, while pressures of 40 cm and 50 cm result in pale and white tracheal mucosa, respectively. A cuff pressure of 60 cm halts tracheal blood flow [3]. A linear relationship is observed between cuff volume and pressure, and insufficient cuff expansion (below 18 cm of water) can lead to pulmonary aspiration of upper airway secretions. To mitigate complications, it is imperative to periodically record the pressure inside the tracheal tube cuff and determine the optimal pressure with the appropriate volume [4-6]. Various methods, such as manual techniques (finger palpation and minimal leak) and automated approaches (direct manometry and continuous monitoring), are employed to assess tracheal tube cuff pressure. Common methods to assess cuff pressure accuracy include the manual minimal leak method and direct manometry [2]. Improper cuff pressure is considered a significant factor contributing to tracheal injury among various factors [8]. Some studies suggest that changing from a supine to a prone position affects cuff pressure, but the impact of lateral decubitus and prone positions on tracheal cuff pressure during surgery remains unexplored. Alterations in tracheal tube position or movement may influence cuff pressure due to the non-circular nature of the trachea along its length [7-11]. Hence, this study was conducted to investigate and compare tracheal tube cuff pressure using two instrumental methods (manometer) and manual methods in patients positioned prone during surgery.
2. Methods and Materials/Patients
This prospective analytical study included 60 patients who underwent lumbar disc surgery in the prone position. The sample included all eligible patients referred to Peymaniyeh Hospital in Jahrom City, Iran, who underwent lumbar disc surgery in a prone position in 2022. The inclusion criteria included individuals aged 18 and above, undergoing general anesthesia in the prone position. The exclusion criteria included refusal to participate, head and neck injuries preventing bending, and inability to obtain consent. Induction of anesthesia involved midazolam (0.03-0.06 mg/kg), fentanyl (2-4 mg/kg), thiopental (5 mg/kg), and atracurium (0.06 mg/kg), with a subsequent administration of 0.1 mg/kg morphine. Intubation was conducted using a single attempt with an appropriately sized tracheal tube. Initially, in the supine position, cuff pressure inside the high-volume, low-pressure tracheal tube was recorded manually and then using a manometric method. Data, including demographic information and cuff pressure changes measured via manometry and manual methods, were collected using a researcher-made checklist. After positioning the patient in the prone position, the cuff pressure was immediately recorded and adjusted using manometry. Subsequent recordings were made every 15 minutes until the surgery’s completion, utilizing only the manometric method. A German-made manometer (Mallinckrodt) was employed, connected to the tracheal tube cuff, and used to inflate the cuff. The pressure gauge displayed the pressure within the cuff, with the normal range being 20 to 30 cm of water. The tracheal tubes, low-pressure and high-volume, were manufactured by Iran’s Supa factory and underwent pre-insertion testing for cuff leakage. Tracheal tube No. 8 was used for male patients, and 7.5 mm in internal diameter for female patients. An anesthetist proficient with the manometer conducted cuff pressure measurements. Data analysis utilized descriptive statistics (mean and percentage) and relevant statistical tests (repeated measurement and analysis of variance (ANOVA) through SPSS software, version 16.
3. Results
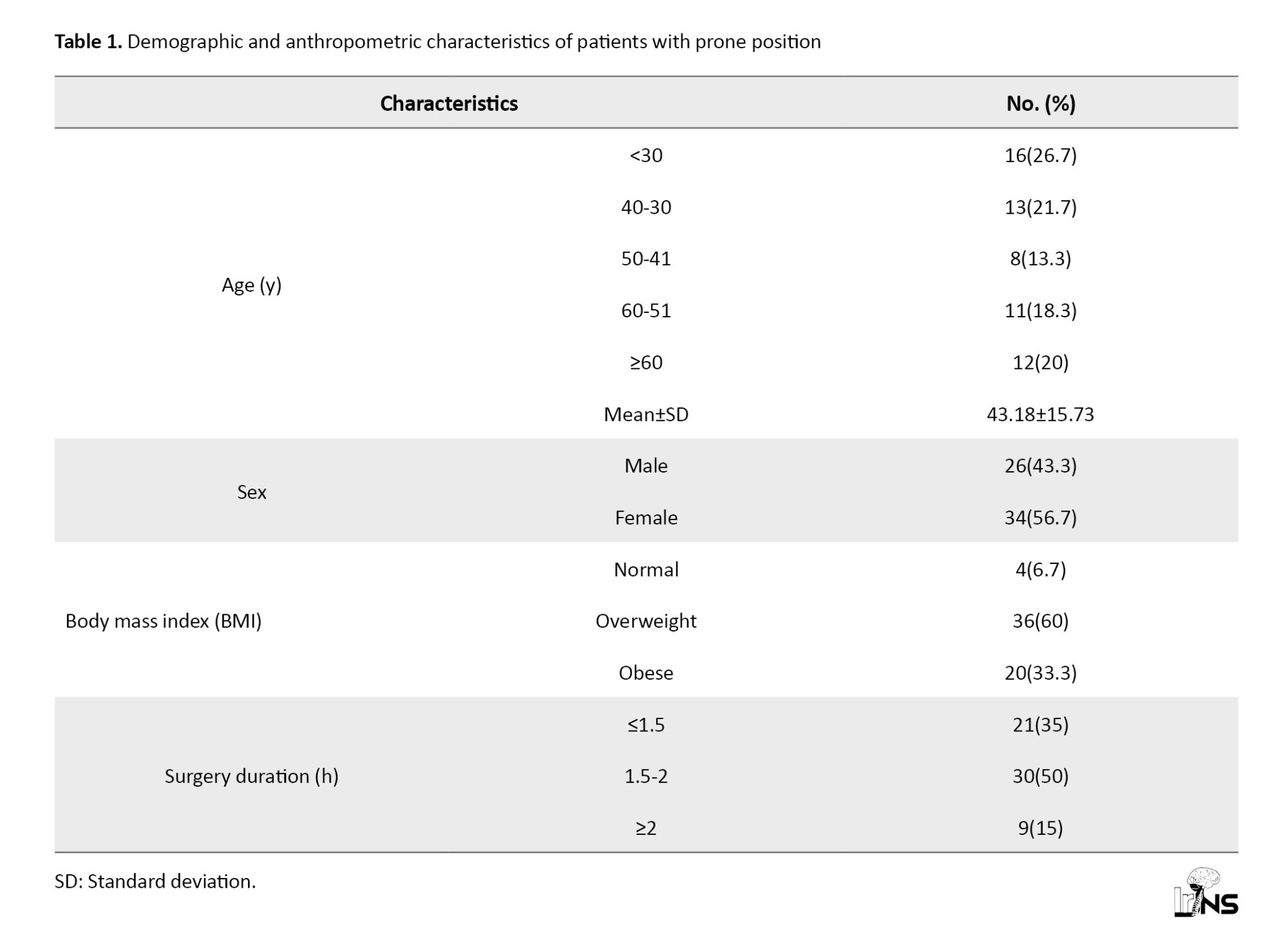
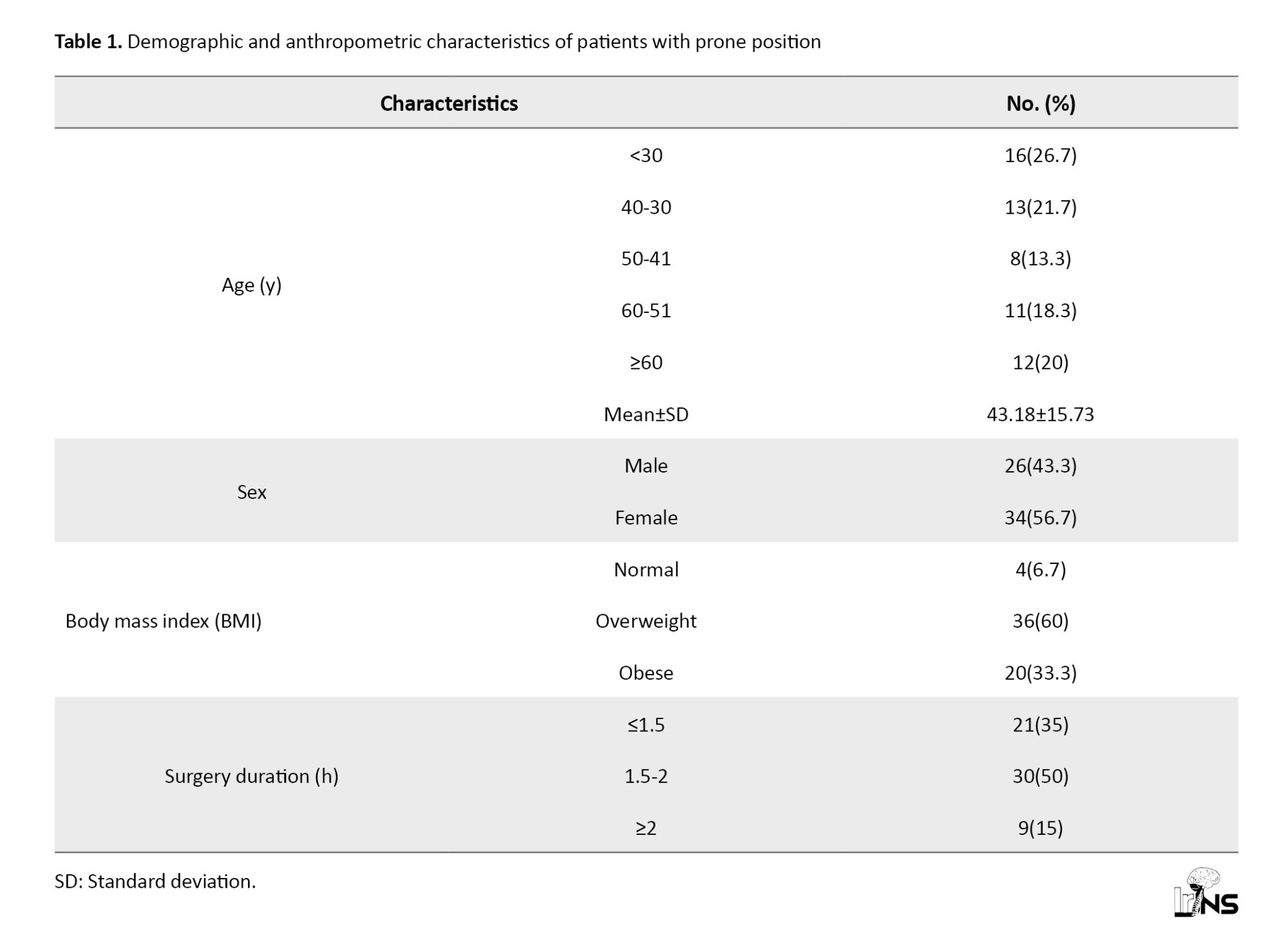
The present study encompassed a cohort of 60 patients ranging in age from 21 to 70 years undergoing lumbar disc surgery in the prone position. The mean age of the patients was 43.18±15.73 years, with nearly half of them falling below the age of thirty years old (48.4%). Most participants were women, constituting 56.7%, while the remaining were men. Regarding body mass index, 60% of the patients were classified in the overweight range. The duration of surgery for half of the patients fell within the range of 1.5 to 2 hours (Table 1).
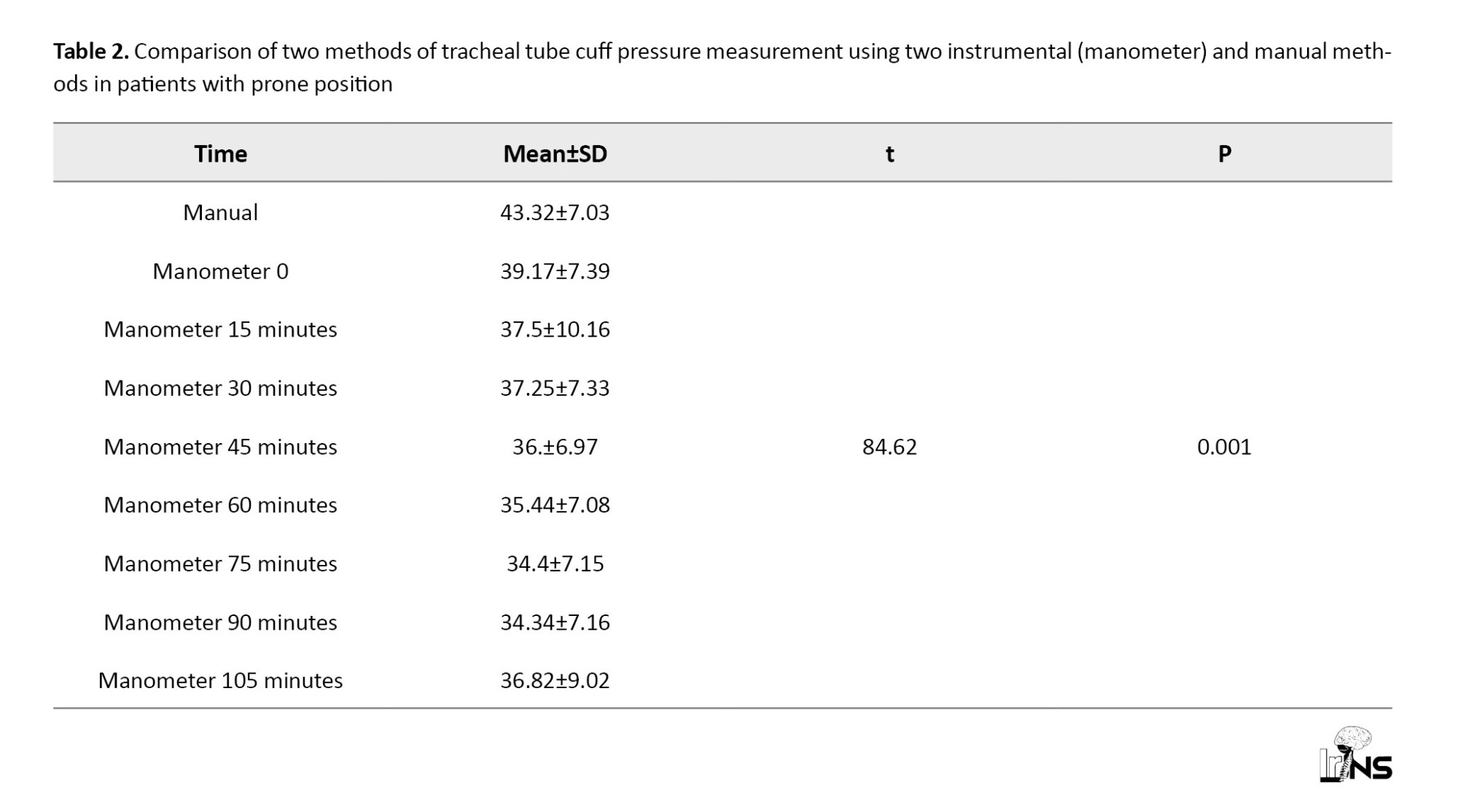
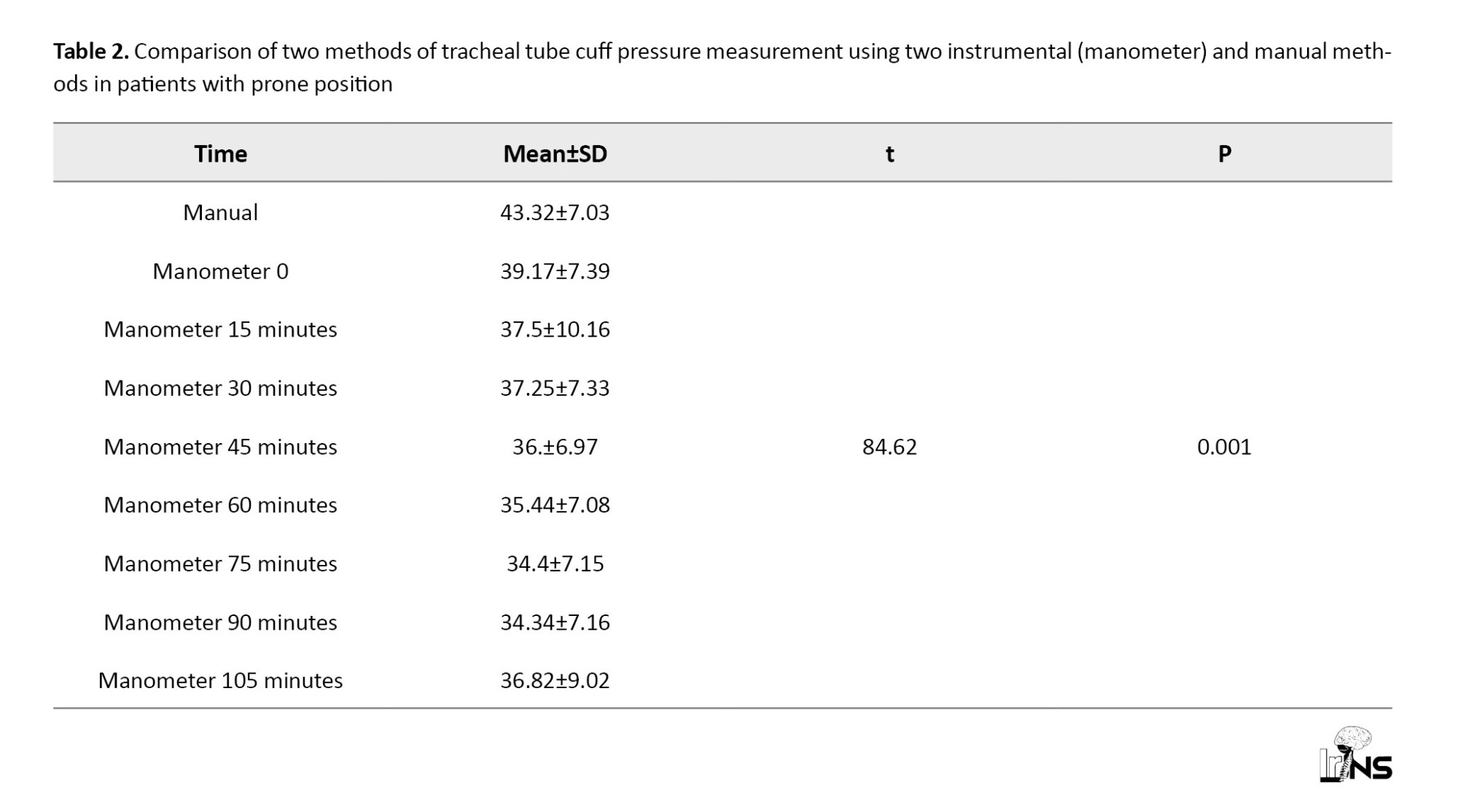
The tracheal tube cuff pressure at various time points did not adhere to a normal distribution (P<0.05). Consequently, Friedman’s test was employed to compare the two methods of tracheal tube cuff pressure measurement, utilizing instrumental (manometer) and manual methods in patients positioned prone. Pairwise comparisons were conducted using the Wilcoxon test with Bonferroni correction. The results of Friedman’s test revealed a significant difference between the two methods of measuring tracheal tube cuff pressure, employing both instrumental (manometer) and manual methods in patients in the prone position (P<0.001). Specifically, the pressure of the tracheal tube cuff measured instrumentally (manometer) was consistently lower than the manual prone position, exhibiting a decrease from 0 to 105 minutes post-operation. Further comparisons using the Wilcoxon test with Bonferroni correction demonstrated that tracheal tube cuff pressure in the manual method was significantly higher than the tracheal tube cuff pressure at 30 minutes (t=2.258, P=0.005), 45 minutes (t=3.091, P=0.001), 60 minutes (t=3.409, P=0.001), 75 minutes (t=4.621, P=0.001), 90 minutes (t=0.045, P=0.001), and 105 minutes (t=4.57, P=0.001) when measured using the manometer (Table 2).
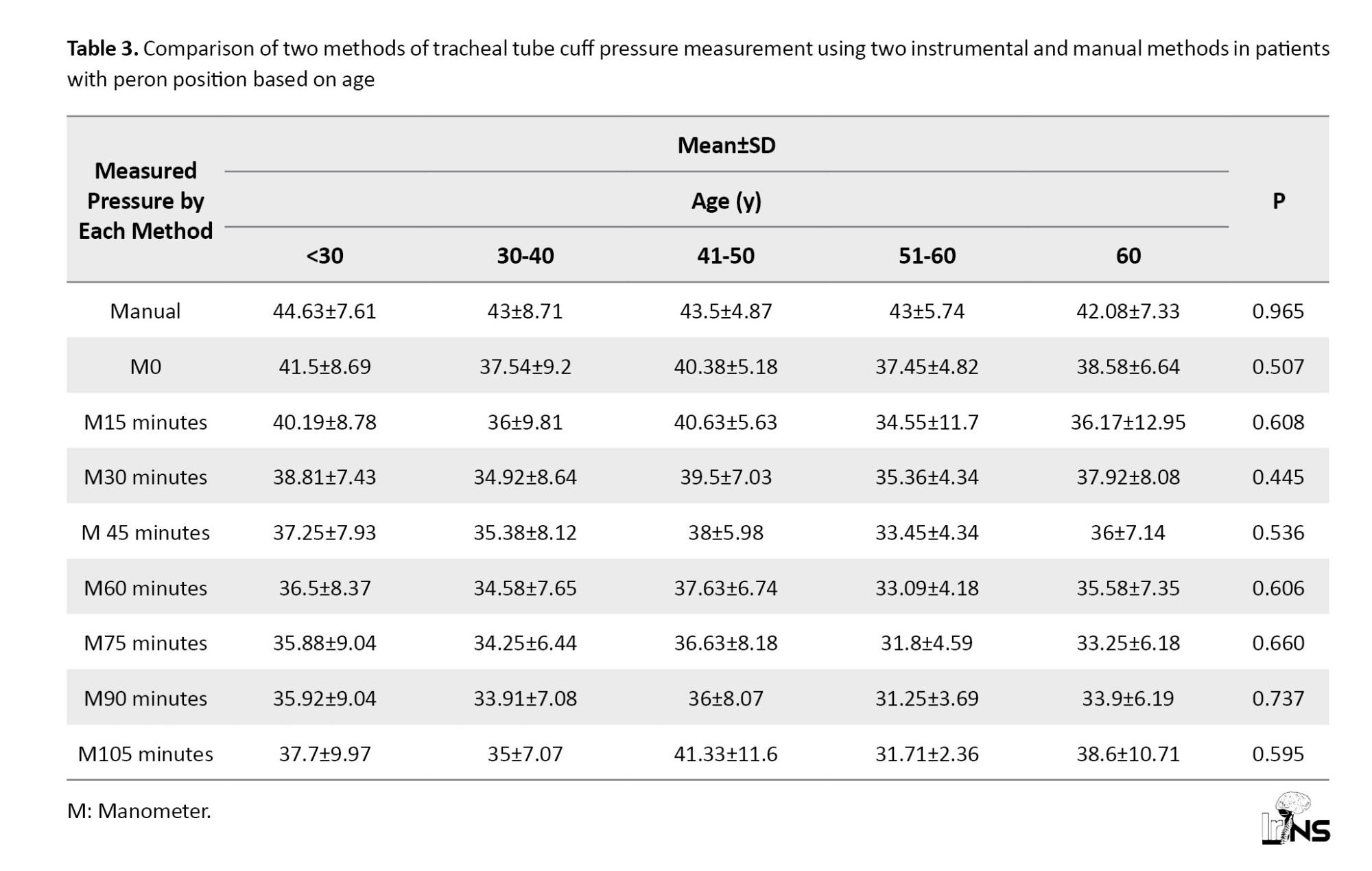
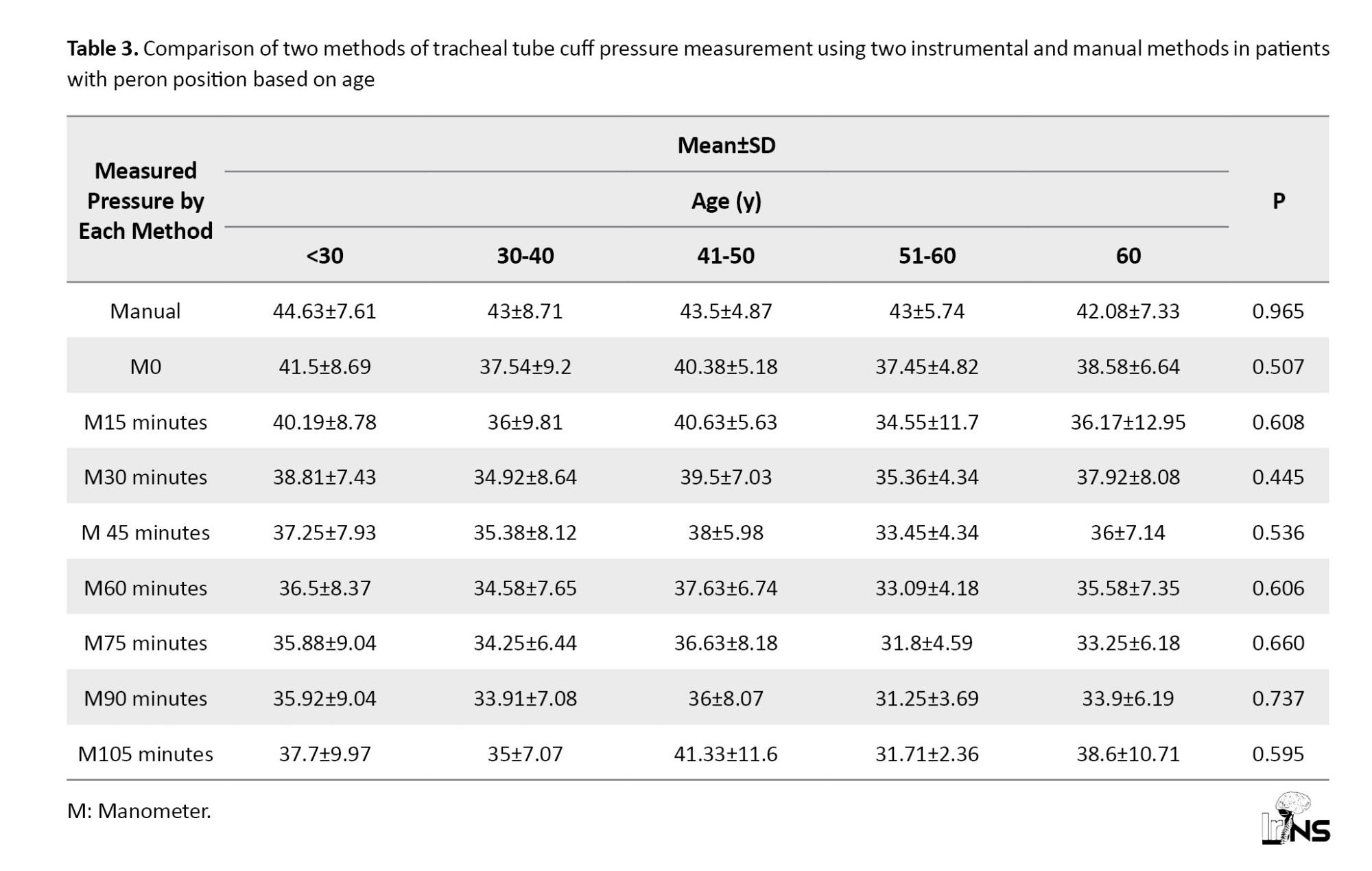
The results of the Kruskal-Wallis test showed no significant difference between the two methods of measuring tracheal tube cuff pressure using two instrumental and manual methods in patients with Peron positions at different ages (P>0.05) (Table 3).
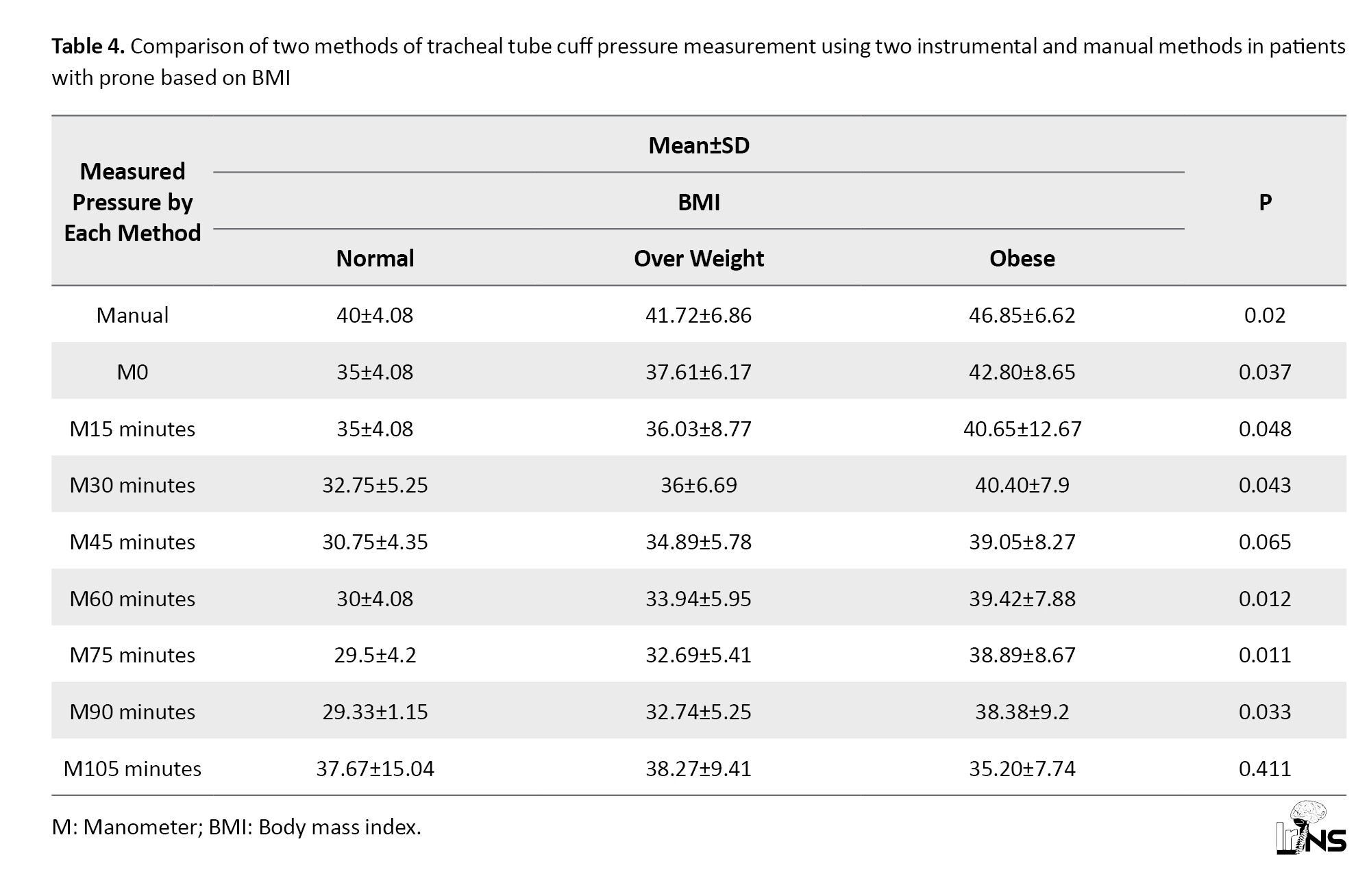
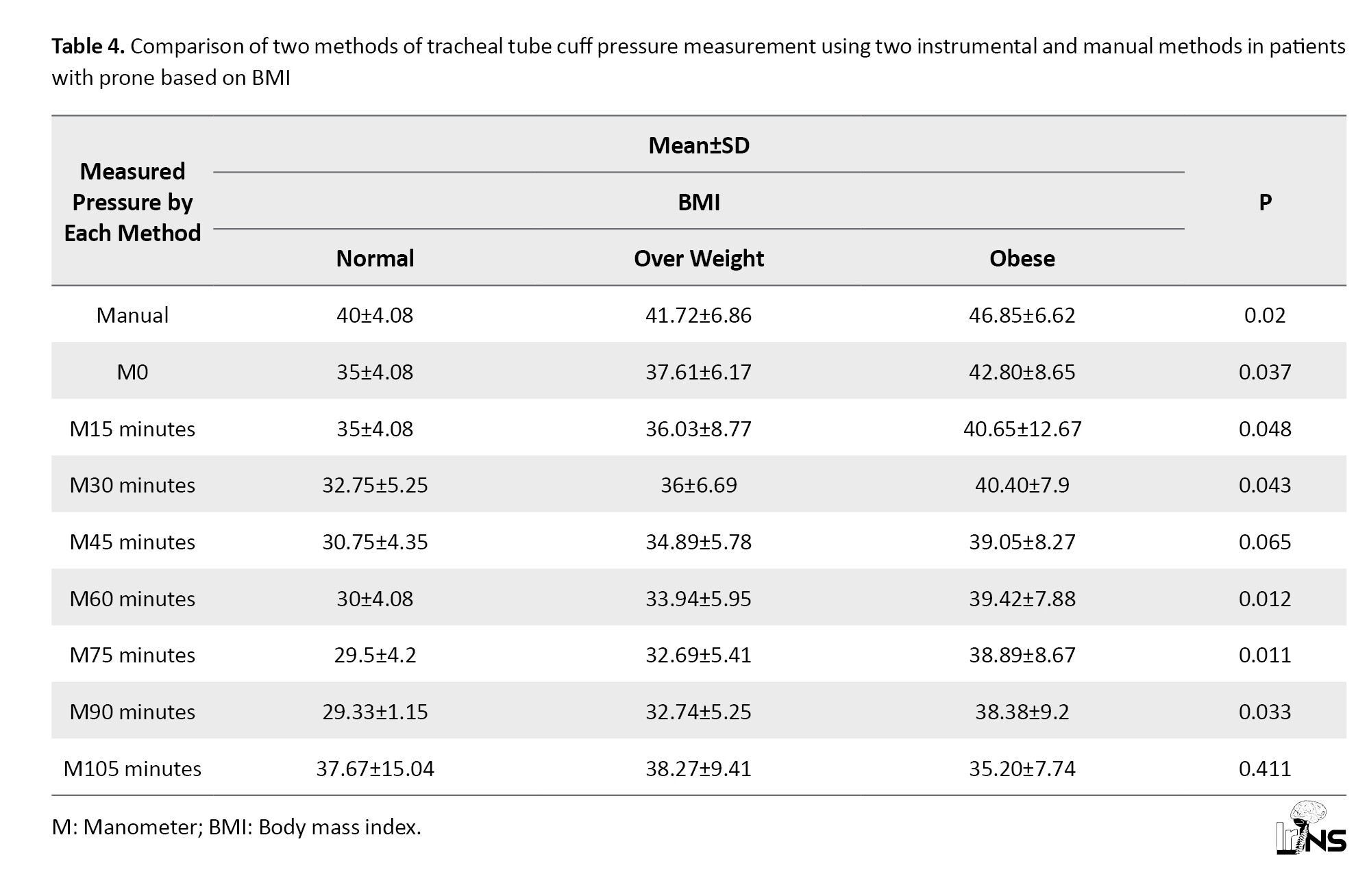
The results of the Kruskal-Wallis test showed a significant difference in tracheal tube cuff pressure by two instrumental methods (manometer) (at zero, 15 minutes, 30 minutes, 60 minutes, 90 minutes) and manual methods in patients with prone position according to body mass index (P<0.05). In manual and manometer methods at zero, 15 minutes, 30 minutes, 60 minutes, and 90 minutes, the highest tracheal tube cuff pressure was higher in obese patients than in other patients (Table 4).
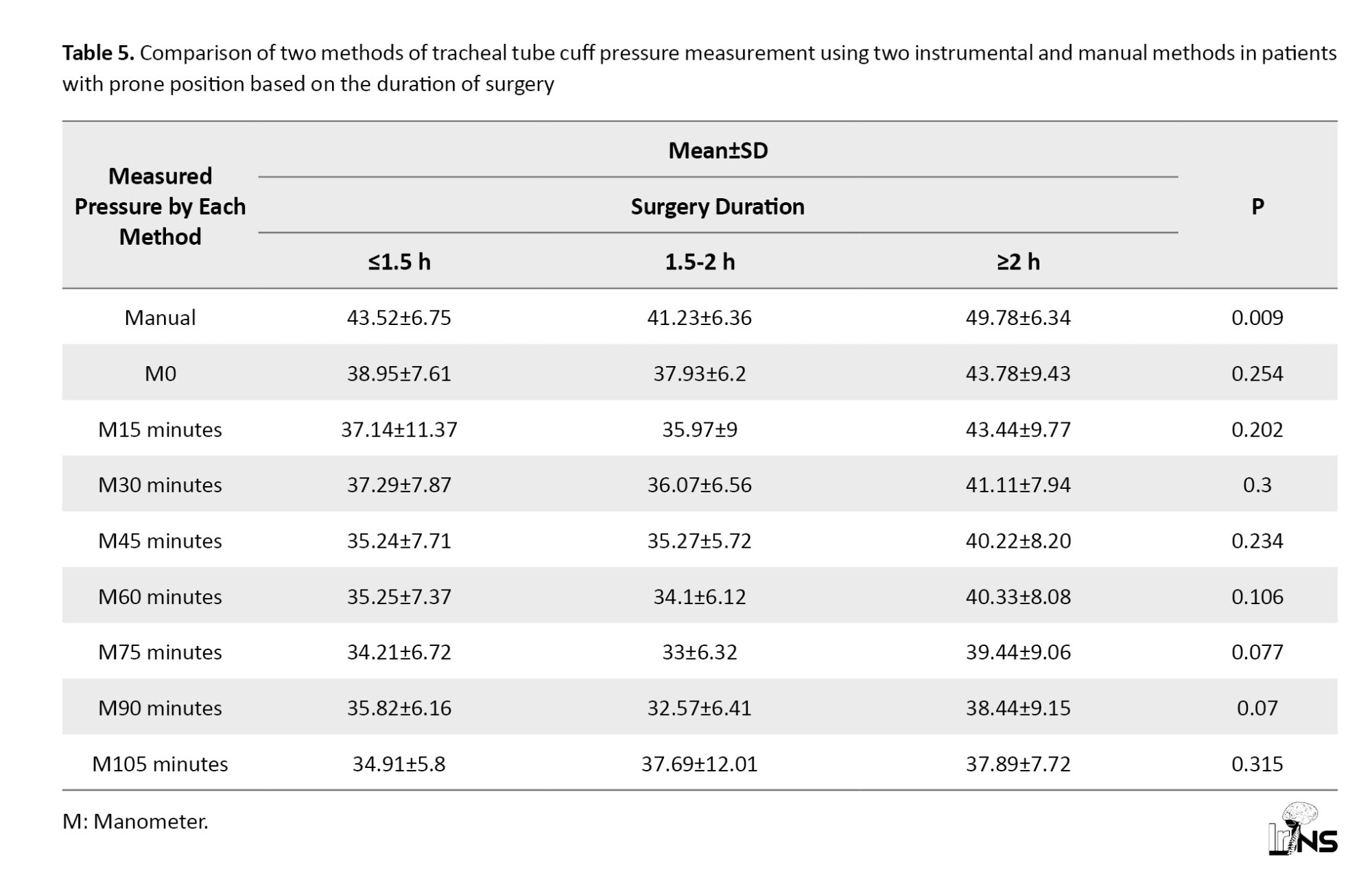
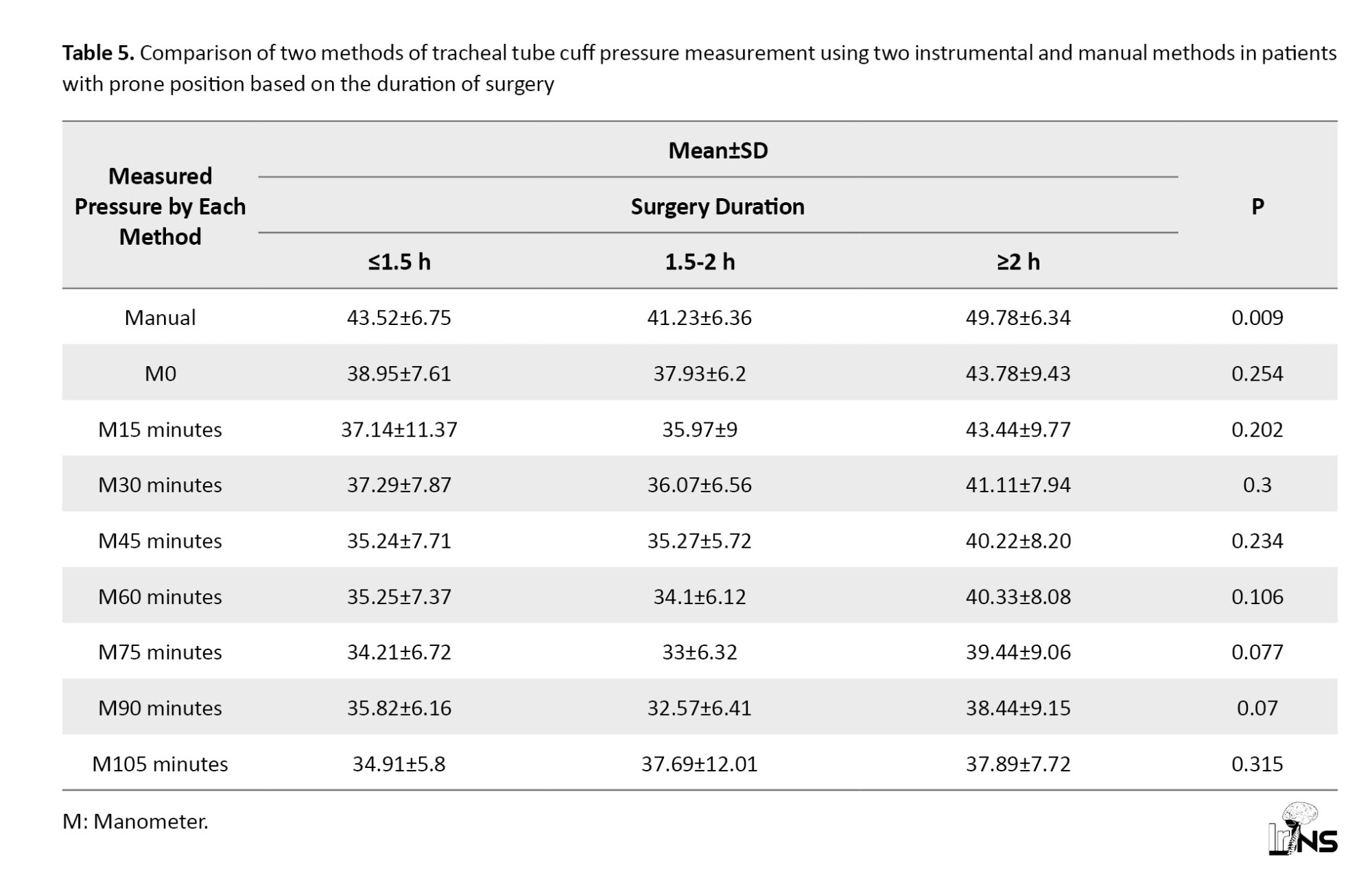
The results of the Kruskal-Wallis test showed a significant difference in the tracheal tube cuff pressure in the traditional prone position method according to the length of surgery (P<0.05). In the manual method, the highest tracheal tube cuff pressure was in patients with a duration of surgery of 2 hours or more (Table 5).
4. Discussion
Tracheal tube cuff pressure management plays a pivotal role in airway management post endotracheal intubation, particularly in critically ill patients undergoing mechanical ventilation. Inadequate cuff pressure may lead to pulmonary aspiration, while excessive pressure can compromise tracheal capillary perfusion [12-15]. This study was conducted to compare two methods of tracheal tube cuff pressure measurement, using instrumental (manometer) and manual methods, on 60 patients aged 21 to 70 years in the prone position. A comparison of the two instrumental and manual methods in patients in the prone position revealed a significant difference in measuring tracheal tube cuff pressure. The instrumental method (manometer) demonstrated lower cuff pressure than the manual method in prone position patients, decreasing from 0 to 105 minutes post-operation. Various techniques, including manual and manual methods (minimal leak and finger palpation) and automatic methods (direct manometry and continuous monitoring), are used to check tracheal cuff pressure [2]. Studies exploring different methods of tracheal tube cuff pressure measurement have reported varying results. Sanaie et al. compared tracheal tube cuff pressure using constant volume techniques and the minimal leakage test method, both resulting in excessive intra-cuff pressure. However, the minimum leakage test method produced more acceptable pressure than constant volume techniques [16]. In the present study, cuff pressure measured by the manual method tended to be higher than manometer pressure, although both methods often recorded pressures higher than the normal range. White et al. compared four tracheal tube cuff pressure inflation techniques, favoring the use of a digital syringe over other methods and recommending the incorporation of a cuff manometer when employing alternative techniques [17]. Rahmani et al. found that touching the cuff balloon or using constant volume techniques was unsuitable for evaluating cuff pressure, emphasizing the need for control through a manometer [18]. In our study, the manometry method consistently measured and recorded tracheal tube cuff pressure throughout the procedure. Factors influencing tracheal tube cuff pressure include patient-related factors, environmental conditions, and care interventions, such as changes in position and therapeutic interventions. Studies have indicated that 25% to 80% of pressure in the abdominal and chest cavities can be transferred between them. Increased intra-abdominal pressure may elevate intra-thoracic pressure, resulting in increased airway pressure and endotracheal tube cuff pressure [19, 20, 10]. In our study, the highest tracheal tube cuff pressure was observed in obese patients, indicating elevated intra-abdominal and chest pressure. Furthermore, measuring cuff pressure by the manual method in the prone position revealed the highest cuff pressure in patients with a surgery duration of 2 hours or more. Research suggests that tracheal tube cuff pressure fluctuates over time. Diffusion of nitrous oxide into the endotracheal cuff during anesthesia leads to an immediate increase, while long-term surgical procedures (>4 hours) result in significant pressure changes [21, 22]. In our study, the surgical position used contributed to higher cuff pressure in a shorter timeframe.
5. Conclusion
According to the results of the current study, it is evident that the tracheal tube cuff pressure measured by the instrumental method (manometer) was consistently lower than that measured by the manual method in patients placed in the prone position. This underscores the importance of utilizing the manometry measurement method to accurately assess tracheal tube cuff pressure in various patient scenarios. The superiority of the manometer in maintaining cuff pressures within the normal range suggests its critical role in airway management, particularly in situations where prone positioning is involved. Thus, it is recommended to adopt manometry as a standard practice for tracheal tube cuff pressure measurement to enhance precision and mitigate potential complications associated with improper cuff pressures.
Ethical Considerations
Compliance with ethical guidelines
This study was approved and registered by the Research Ethics Committee of Jahrom University of Medical Sciences, Jahrom, Iran (Code: IIR.JUMS.REC.1400.090).
Funding
This study was extracted from the doctoral residency dissertation of Meysam Zarei approved by the Department of Anesthesiology, Faculty of Medicine, Jahrom University of Medical Sciences, Jahrom, Iran.
Authors' contributions
Conceptualization and study design: Mohammad Sadegh Sanie Jahromi, and Navid Kalani; Data collection and writing the original draft: Mohammad Sadegh Sanie Jahromi, Lohrasb Taheri, Navid Kalani, and Meysam Zarei; Statistical analysis: Mansour Deylami and Navid Kalani Final approval: Mohammad Sadegh Sanie Jahromi and Navid Kalani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the Clinical Research Development Unit of Peymanieh Educational and Research and Therapeutic Center of Jahrom University of Medical Sciences, Jahrom, Iran for their help in revising the manuscript.
References
Tracheal tubes are designed to establish a secure airway in adult patients, featuring a distal cuff that, when inflated, acts as a barrier to the tracheal wall. This inflation prevents pulmonary aspiration, ensuring the delivery of the intended flow volume to the lungs. The tracheal tube size is determined by its inner diameter, measured in millimeters; however, the relationship with the outer diameter varies across different production designs. The inflation of the tracheal tube cuff forms a barrier between the tube and the tracheal wall, eliminating air leakage during positive pressure ventilation and safeguarding the lungs against aspiration. Earlier tracheal tube cuffs, characterized by high pressure, exerted considerable force on tracheal mucus, leading to ischemia. Contemporary endotracheal tubes incorporate low-pressure cuffs to minimize pressure on the trachea, consequently reducing the risk of ischemia [1]. Maintaining cuff pressure within the range of 20-30 cm of water is crucial to minimize air leakage, preserve flow volume, and prevent damage to the tracheal mucosa [2]. Studies indicate that at a cuff pressure of 25 cm of water, tracheal blood flow remains normal, while pressures of 40 cm and 50 cm result in pale and white tracheal mucosa, respectively. A cuff pressure of 60 cm halts tracheal blood flow [3]. A linear relationship is observed between cuff volume and pressure, and insufficient cuff expansion (below 18 cm of water) can lead to pulmonary aspiration of upper airway secretions. To mitigate complications, it is imperative to periodically record the pressure inside the tracheal tube cuff and determine the optimal pressure with the appropriate volume [4-6]. Various methods, such as manual techniques (finger palpation and minimal leak) and automated approaches (direct manometry and continuous monitoring), are employed to assess tracheal tube cuff pressure. Common methods to assess cuff pressure accuracy include the manual minimal leak method and direct manometry [2]. Improper cuff pressure is considered a significant factor contributing to tracheal injury among various factors [8]. Some studies suggest that changing from a supine to a prone position affects cuff pressure, but the impact of lateral decubitus and prone positions on tracheal cuff pressure during surgery remains unexplored. Alterations in tracheal tube position or movement may influence cuff pressure due to the non-circular nature of the trachea along its length [7-11]. Hence, this study was conducted to investigate and compare tracheal tube cuff pressure using two instrumental methods (manometer) and manual methods in patients positioned prone during surgery.
2. Methods and Materials/Patients
This prospective analytical study included 60 patients who underwent lumbar disc surgery in the prone position. The sample included all eligible patients referred to Peymaniyeh Hospital in Jahrom City, Iran, who underwent lumbar disc surgery in a prone position in 2022. The inclusion criteria included individuals aged 18 and above, undergoing general anesthesia in the prone position. The exclusion criteria included refusal to participate, head and neck injuries preventing bending, and inability to obtain consent. Induction of anesthesia involved midazolam (0.03-0.06 mg/kg), fentanyl (2-4 mg/kg), thiopental (5 mg/kg), and atracurium (0.06 mg/kg), with a subsequent administration of 0.1 mg/kg morphine. Intubation was conducted using a single attempt with an appropriately sized tracheal tube. Initially, in the supine position, cuff pressure inside the high-volume, low-pressure tracheal tube was recorded manually and then using a manometric method. Data, including demographic information and cuff pressure changes measured via manometry and manual methods, were collected using a researcher-made checklist. After positioning the patient in the prone position, the cuff pressure was immediately recorded and adjusted using manometry. Subsequent recordings were made every 15 minutes until the surgery’s completion, utilizing only the manometric method. A German-made manometer (Mallinckrodt) was employed, connected to the tracheal tube cuff, and used to inflate the cuff. The pressure gauge displayed the pressure within the cuff, with the normal range being 20 to 30 cm of water. The tracheal tubes, low-pressure and high-volume, were manufactured by Iran’s Supa factory and underwent pre-insertion testing for cuff leakage. Tracheal tube No. 8 was used for male patients, and 7.5 mm in internal diameter for female patients. An anesthetist proficient with the manometer conducted cuff pressure measurements. Data analysis utilized descriptive statistics (mean and percentage) and relevant statistical tests (repeated measurement and analysis of variance (ANOVA) through SPSS software, version 16.
3. Results
The present study encompassed a cohort of 60 patients ranging in age from 21 to 70 years undergoing lumbar disc surgery in the prone position. The mean age of the patients was 43.18±15.73 years, with nearly half of them falling below the age of thirty years old (48.4%). Most participants were women, constituting 56.7%, while the remaining were men. Regarding body mass index, 60% of the patients were classified in the overweight range. The duration of surgery for half of the patients fell within the range of 1.5 to 2 hours (Table 1).
The tracheal tube cuff pressure at various time points did not adhere to a normal distribution (P<0.05). Consequently, Friedman’s test was employed to compare the two methods of tracheal tube cuff pressure measurement, utilizing instrumental (manometer) and manual methods in patients positioned prone. Pairwise comparisons were conducted using the Wilcoxon test with Bonferroni correction. The results of Friedman’s test revealed a significant difference between the two methods of measuring tracheal tube cuff pressure, employing both instrumental (manometer) and manual methods in patients in the prone position (P<0.001). Specifically, the pressure of the tracheal tube cuff measured instrumentally (manometer) was consistently lower than the manual prone position, exhibiting a decrease from 0 to 105 minutes post-operation. Further comparisons using the Wilcoxon test with Bonferroni correction demonstrated that tracheal tube cuff pressure in the manual method was significantly higher than the tracheal tube cuff pressure at 30 minutes (t=2.258, P=0.005), 45 minutes (t=3.091, P=0.001), 60 minutes (t=3.409, P=0.001), 75 minutes (t=4.621, P=0.001), 90 minutes (t=0.045, P=0.001), and 105 minutes (t=4.57, P=0.001) when measured using the manometer (Table 2).
The results of the Kruskal-Wallis test showed no significant difference between the two methods of measuring tracheal tube cuff pressure using two instrumental and manual methods in patients with Peron positions at different ages (P>0.05) (Table 3).
The results of the Kruskal-Wallis test showed a significant difference in tracheal tube cuff pressure by two instrumental methods (manometer) (at zero, 15 minutes, 30 minutes, 60 minutes, 90 minutes) and manual methods in patients with prone position according to body mass index (P<0.05). In manual and manometer methods at zero, 15 minutes, 30 minutes, 60 minutes, and 90 minutes, the highest tracheal tube cuff pressure was higher in obese patients than in other patients (Table 4).
The results of the Kruskal-Wallis test showed a significant difference in the tracheal tube cuff pressure in the traditional prone position method according to the length of surgery (P<0.05). In the manual method, the highest tracheal tube cuff pressure was in patients with a duration of surgery of 2 hours or more (Table 5).
4. Discussion
Tracheal tube cuff pressure management plays a pivotal role in airway management post endotracheal intubation, particularly in critically ill patients undergoing mechanical ventilation. Inadequate cuff pressure may lead to pulmonary aspiration, while excessive pressure can compromise tracheal capillary perfusion [12-15]. This study was conducted to compare two methods of tracheal tube cuff pressure measurement, using instrumental (manometer) and manual methods, on 60 patients aged 21 to 70 years in the prone position. A comparison of the two instrumental and manual methods in patients in the prone position revealed a significant difference in measuring tracheal tube cuff pressure. The instrumental method (manometer) demonstrated lower cuff pressure than the manual method in prone position patients, decreasing from 0 to 105 minutes post-operation. Various techniques, including manual and manual methods (minimal leak and finger palpation) and automatic methods (direct manometry and continuous monitoring), are used to check tracheal cuff pressure [2]. Studies exploring different methods of tracheal tube cuff pressure measurement have reported varying results. Sanaie et al. compared tracheal tube cuff pressure using constant volume techniques and the minimal leakage test method, both resulting in excessive intra-cuff pressure. However, the minimum leakage test method produced more acceptable pressure than constant volume techniques [16]. In the present study, cuff pressure measured by the manual method tended to be higher than manometer pressure, although both methods often recorded pressures higher than the normal range. White et al. compared four tracheal tube cuff pressure inflation techniques, favoring the use of a digital syringe over other methods and recommending the incorporation of a cuff manometer when employing alternative techniques [17]. Rahmani et al. found that touching the cuff balloon or using constant volume techniques was unsuitable for evaluating cuff pressure, emphasizing the need for control through a manometer [18]. In our study, the manometry method consistently measured and recorded tracheal tube cuff pressure throughout the procedure. Factors influencing tracheal tube cuff pressure include patient-related factors, environmental conditions, and care interventions, such as changes in position and therapeutic interventions. Studies have indicated that 25% to 80% of pressure in the abdominal and chest cavities can be transferred between them. Increased intra-abdominal pressure may elevate intra-thoracic pressure, resulting in increased airway pressure and endotracheal tube cuff pressure [19, 20, 10]. In our study, the highest tracheal tube cuff pressure was observed in obese patients, indicating elevated intra-abdominal and chest pressure. Furthermore, measuring cuff pressure by the manual method in the prone position revealed the highest cuff pressure in patients with a surgery duration of 2 hours or more. Research suggests that tracheal tube cuff pressure fluctuates over time. Diffusion of nitrous oxide into the endotracheal cuff during anesthesia leads to an immediate increase, while long-term surgical procedures (>4 hours) result in significant pressure changes [21, 22]. In our study, the surgical position used contributed to higher cuff pressure in a shorter timeframe.
5. Conclusion
According to the results of the current study, it is evident that the tracheal tube cuff pressure measured by the instrumental method (manometer) was consistently lower than that measured by the manual method in patients placed in the prone position. This underscores the importance of utilizing the manometry measurement method to accurately assess tracheal tube cuff pressure in various patient scenarios. The superiority of the manometer in maintaining cuff pressures within the normal range suggests its critical role in airway management, particularly in situations where prone positioning is involved. Thus, it is recommended to adopt manometry as a standard practice for tracheal tube cuff pressure measurement to enhance precision and mitigate potential complications associated with improper cuff pressures.
Ethical Considerations
Compliance with ethical guidelines
This study was approved and registered by the Research Ethics Committee of Jahrom University of Medical Sciences, Jahrom, Iran (Code: IIR.JUMS.REC.1400.090).
Funding
This study was extracted from the doctoral residency dissertation of Meysam Zarei approved by the Department of Anesthesiology, Faculty of Medicine, Jahrom University of Medical Sciences, Jahrom, Iran.
Authors' contributions
Conceptualization and study design: Mohammad Sadegh Sanie Jahromi, and Navid Kalani; Data collection and writing the original draft: Mohammad Sadegh Sanie Jahromi, Lohrasb Taheri, Navid Kalani, and Meysam Zarei; Statistical analysis: Mansour Deylami and Navid Kalani Final approval: Mohammad Sadegh Sanie Jahromi and Navid Kalani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the Clinical Research Development Unit of Peymanieh Educational and Research and Therapeutic Center of Jahrom University of Medical Sciences, Jahrom, Iran for their help in revising the manuscript.
References
- Henderson J. Airway Management in the Adult. In: Miller RD. Millers Anesthesia. Edinburgh: Elsevier; 2020. [DOI:10.1016/B978-0-443-06959-8.00050-9]
- Letvin A, Kremer P, Silver PC, Samih N, Reed-Watts P, Kollef MH. Frequent versus infrequent monitoring of endotracheal tube cuff pressures. Respiratory Care. 2018; 63(5):495-501. [DOI:10.4187/respcare.05926] [PMID]
- Nikbakhsh N, Alijanpour E, Mortazavi Y, Organji N. [Evaluation of tracheal tube cuff pressure complications in icu patients of Shahid Beheshti Hospital, 2007-2008 (Persian)]. Journal of Babol University of Medical Sciences. 2010; 12(2):30-4. [Link]
- Saleh Moghaddam A.R, Malekzadeh J, Mesbahi Z, Esmaeli H. [Relationship between temperature and cuff pressure in mechanically ventilated patients with endotracheal Tube (Persian)]. Quarterly of the Horizon of Medical Sciences. 2013; 19(2):105-9. [Link]
- Sharyfy A, Khatony A, Rezaey M. Is there a relationship between core body temperature and changes of endotracheal tube cuff pressure? Iranian Journal of Critical Care Nursing. 2014; 6(3):102-9. [Link]
- Rokamp KZ, Secher NH, Møller AM, Nielsen HB. Tracheal tube and laryngeal mask cuff pressure during anesthesia- mandatory monitoring is in need. BMC Anesthesiology. 2014; 10(20):20. [DOI:10.1186/1471-2253-10-20]
- Godoy AC, Vieira RJ, Capitani EM. [Endotracheal tube cuff pressure alteration after changes in position in patients under mechanical ventilation (Portuguese)]. Jornal Brasileiro de Pneumologia. 2008 May;34(5):294-7. [DOI:10.1590/S1806-37132008000500008] [PMID]
- Minonishi T, Kinoshita H, Hirayama M, Kawahito S, Azma T, Hatakeyama N, et al. The supine-to-prone position change induces modification of endotracheal tube cuff pressure accompanied by tube displacement. Journal of Clinical Anesthesia. 2013; 25(1):28-31. [DOI:10.1016/j.jclinane.2012.05.007] [PMID]
- Rigini N, Boaz M, Ezri T, Evron S, Trigub D, Jackobashvilli S, Izakson A. Prompt correction of endotracheal tube positioning after intubation prevents further inappropriate positions. Journal of Clinical Anesthesia. 2011; 23(5):367-71. [DOI:10.1016/j.jclinane.2010.11.002] [PMID]
- Kim D, Jeon B, Son JS, Lee JR, Ko S, Lim H. The changes of endotracheal tube cuff pressure by the position changes from supine to prone and the flexion and extension of head. Korean Journal of Anesthesiology. 2015; 68(1):27-31. [DOI:10.4097/kjae.2015.68.1.27] [PMID] [PMCID]
- Otoch JP, Minamoto H, Perini M, Carneiro FO, de Almeida Artifon EL. Is there a correlation between right bronchus length and diameter with age? Journal of Thoracic Disease. 2013; 5(3):306-9. [DOI:10.3978/j.issn.2072-1439.2013.03.12] [PMID]
- Abramson ZR, Susarla S, Tagoni JR, Kaban L. Three-dimensional computed tomographic analysis of airway anatomy. Journal of Oral and Maxillofacial Surgery. 2010; 68(2):363-71. [DOI:10.1016/j.joms.2009.09.086] [PMID]
- Sengupta P, Sessler DI, Maglinger P, Wells S, Vogt A, Durrani J, et al. Endotracheal tube cuff pressure in three hospitals, and the volume required to produce an appropriate cuff pressure. BMC Anesthesiology. 2004; 4(1):8. [DOI:10.1186/1471-2253-4-8] [PMID] [PMCID]
- Sole ML, Su X, Talbert S, Penoyer DA, Kalita S, Jimenez E, et al. Evaluation of an intervention to maintain endotracheal tube cuff pressure within therapeutic range. American Journal of Critical Care. 2011; 20(2):109-17. [DOI:10.4037/ajcc2011661] [PMID] [PMCID]
- Mahmoodpoor A, Hamishehkar H, Hamidi M, Shadvar K, Sanaie S, Golzari SE, et al. A prospective randomized trial of tapered-cuff endotracheal tubes with intermittent subglottic suctioning in preventing ventilator-associated pneumonia in critically ill patients. Journal of Critical Care. 2017; 38:152-6. [DOI:10.1016/j.jcrc.2016.11.007] [PMID]
- Mahmoodpoor A, Peyrovi-far A, Hamishehkar H, Bakhtyiari Z, Mirinezhad MM, Hamidi M, et al. Comparison of prophylactic effects of polyurethane cylindrical or tapered cuff and polyvinyl chloride cuff endotracheal tubes on ventilator-associated pneumonia. Acta Medica Iranica. 2013; 51(7):461-6. [Link]
- Sanaie S, Rahmani F, Chokhachian S, Mahmoodpoor A, Rahimi Panahi J, Mehdizadeh Esfanjani R, et al. Comparison of tracheal tube cuff pressure with two technique: Fixed volume and minimal leak test techniques. Journal of Cardiovascular and Thoracic Research. 2019; 11(1):48-52. [DOI:10.15171/jcvtr.2019.08] [PMID] [PMCID]
- White DM, Makara M, Martinez-Taboada F. Comparison of four inflation techniques on endotracheal tube cuff pressure using a feline airway simulator. Journal of Feline Medicine and Surgery. 2020; 22(7):641-7. [DOI:10.1177/1098612X19871701] [PMID] [PMCID]
- Rahmani F, Soleimanpour H, Zeynali A, Mahmoodpoor A, Shahsavari Nia K, Rahimi Panahi J, et al. Comparison of tracheal tube cuff pressure with two techniques: Fixed volume versus pilot balloon palpation. Journal of Cardiovascular and Thoracic Research. 2017; 9(4):196-9. [DOI:10.15171/jcvtr.2017.34] [PMID] [PMCID]
- Kim E, Kim HC, Lim YJ, Kim CH, Sohn S, Chung CK, et al. Comparison of intra-abdominal pressure among 3 prone positional apparatuses after changing from the supine to the prone position and applying positive end-expiratory pressure in healthy euvolemic patients: A prospective observational study. Journal of Neurosurgical Anesthesiology. 2017; 29(1):14-20. [DOI:10.1097/ANA.0000000000000257] [PMID]
- Telias I, Katira BH, Brochard L. Is the prone position helpful during spontaneous breathing in patients with COVID-19? JAMA. 2020; 323(22):2265-7. [DOI:10.1001/jama.2020.8539] [PMID]
- Combes X, Schauvliege F, Peyrouset O, Motamed C, Kirov K, Dhonneur G, et al. Intracuff pressure and tracheal morbidity: Influence of filling with saline during nitrous oxide anesthesia. Anesthesiology. 2001; 95(5):1120-4. [DOI:10.1097/00000542-200111000-00015] [PMID]
- Kako H, Goykhman A, Ramesh AS, Krishna SG, Tobias JD. Changes in intracuff pressure of a cuffed endotracheal tube during prolonged surgical procedures. International Journal of Pediatric Otorhinolaryngology. 2015; 79(1):76-9. [DOI:10.1016/j.ijporl.2014.11.017] [PMID]
Type of Study: Research |
Subject:
Neurotrauma
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |



