Sun, Feb 22, 2026
Volume 10 - Continuous Publishing
Iran J Neurosurg 2024, 10 - Continuous Publishing: 126-133 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Yaqoob U, Dhakal R, Karki D, Ghimire S, Ahmed N, Awan T T. Traumatic Brain Injuries in Male Soccer Players. Iran J Neurosurg 2024; 10 : 14
URL: http://irjns.org/article-1-413-en.html
URL: http://irjns.org/article-1-413-en.html
Uzair Yaqoob *1 

 , Roshan Dhakal2
, Roshan Dhakal2 

 , Deeven Karki2
, Deeven Karki2 

 , Sujha Ghimire2
, Sujha Ghimire2 

 , Naveed Ahmed3
, Naveed Ahmed3 

 , Tabeer Tanwir Awan4
, Tabeer Tanwir Awan4 




 , Roshan Dhakal2
, Roshan Dhakal2 

 , Deeven Karki2
, Deeven Karki2 

 , Sujha Ghimire2
, Sujha Ghimire2 

 , Naveed Ahmed3
, Naveed Ahmed3 

 , Tabeer Tanwir Awan4
, Tabeer Tanwir Awan4 


1- Department of Neurosurgery, Civil Hospital, SMBB Trauma Centre, Karachi, Pakistan. , ozair_91393@hotmail.com
2- Department of Internal Medicine, Nepal Medical College, Kathmandu, Nepal.
3- Department of Neurosurgery, Pakistan Institute of Medical Sciences, Islamabad, Pakistan.
4- Dow Institute of Physical Medicine and Rehabilitation, Karachi, Pakistan.
2- Department of Internal Medicine, Nepal Medical College, Kathmandu, Nepal.
3- Department of Neurosurgery, Pakistan Institute of Medical Sciences, Islamabad, Pakistan.
4- Dow Institute of Physical Medicine and Rehabilitation, Karachi, Pakistan.
Full Text [PDF 1155 kb]
(1529 Downloads)
| Abstract (HTML) (2835 Views)
Full Text: (1757 Views)
1. Introduction
Given that soccer is a globally prevalent sport with more than 224 million players worldwide, concerns about the potential for short- or long-term brain trauma have gained prominence [1, 2]. The practice of playing or hitting a ball with one’s head originated in northern England [1]. It grew in popularity following the Football Association’s adoption of the original rules in 1863. The organization quickly set up a new rule prohibiting ball interaction with hands in 1872 [3]. Since then, the so-called head-to-head play has become a staple of soccer [1]. Heading the ball, deeply ingrained in soccer, poses risks beyond the known dangers of collisions during play [4, 5]. Detailed investigations are underway to understand the level, aspect, and potential repercussions of heading, including cognitive consequences, both short- and long-term [1, 6]. A recent study revealing a link between heading the soccer ball and decreased cognitive performance within 24 hours emphasizes the need for a comprehensive examination of traumatic brain injuries (TBIs) in modern football [7]. As a result, the number of head impact accidents involving a biomechanical force communicated to the skull and brain, often known as a “sub-concussive hit”, is unknown.
Purposeful soccer headings are more common than incidental head impacts, but their severity is usually lower [8]. It is unknown whether purposeful soccer headings are harmful to the brain [9]. One controlled heading session has been linked to higher rates of reported concussion symptoms, changes in postural control, and higher levels of corticomotor inhibition along with memory impairment [7, 10]. There has been evidence of brain white matter microstructure abnormalities and cognition problems in players who self-reported long-term exposure to 885 to 1800 headers annually [11]. However, some studies have not discovered any appreciable neuropsychological or neurocognitive impairments linked to brief exposure to soccer headings. This narrative review article aims to evaluate the incidence, contact methods, impact damage, associated symptoms, and management protocols related to TBIs in soccer. By addressing the gaps in understanding the frequency and classification of TBIs in modern football, this study contributes to the broader discourse on player safety and informs potential preventive measures and management strategies.
2. Materials and Methods
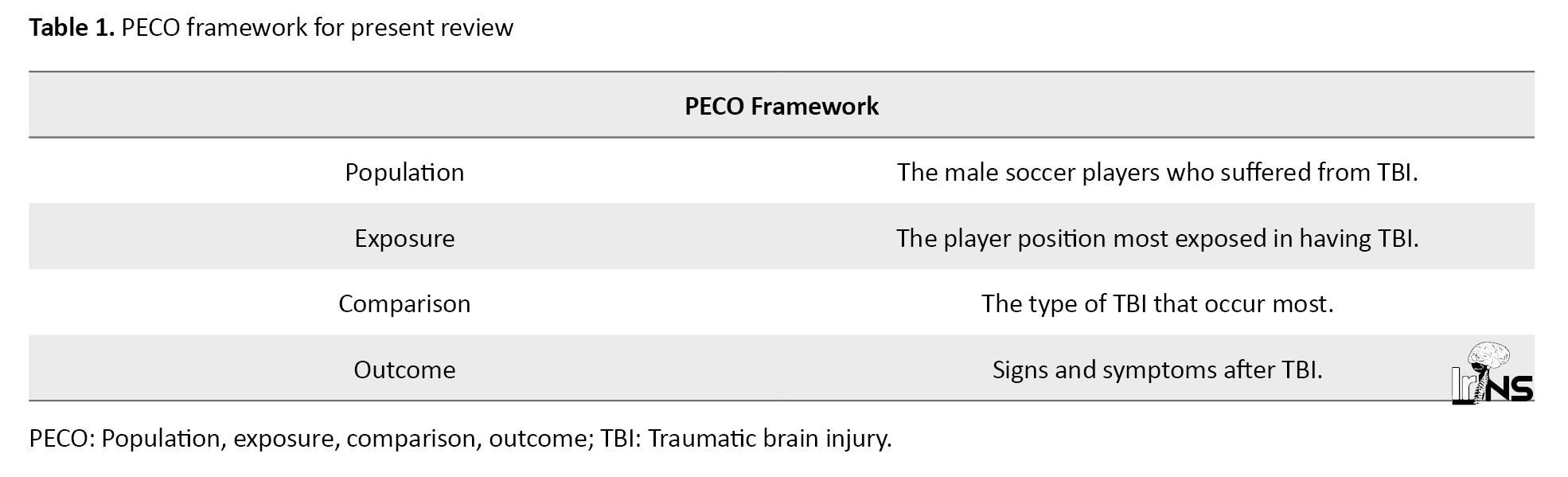
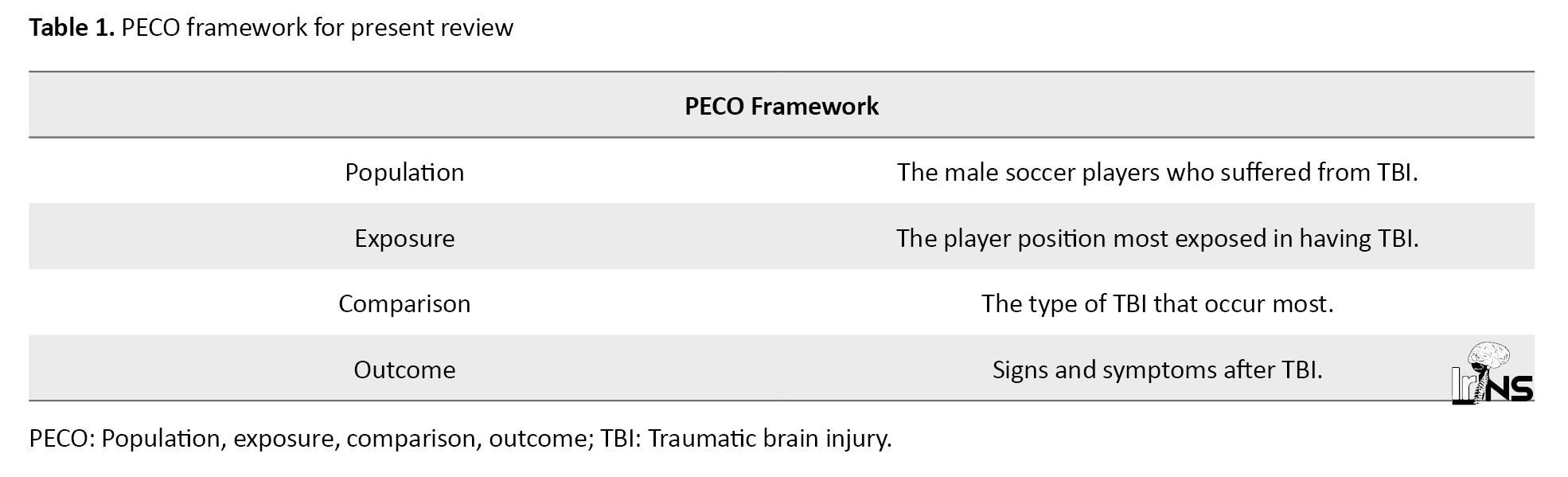
The authors went through PubMed, Scopus, and Google Scholar databases. Search terms used were as follows: “Traumatic brain injuries or TBIs”, “concussion”, “male soccer players or male soccer athletes”, “incidence”, “injury”, “cognitive impairments or changes”, and “management”. The publications from the last two decades were considered. Retrospective, prospective, and clinical studies in the English language were included in this review. The population, exposure, comparison, outcome (PECO) framework (with intervention replaced with exposure) was used to simplify the research question which is presented in Table 1.
3. Results
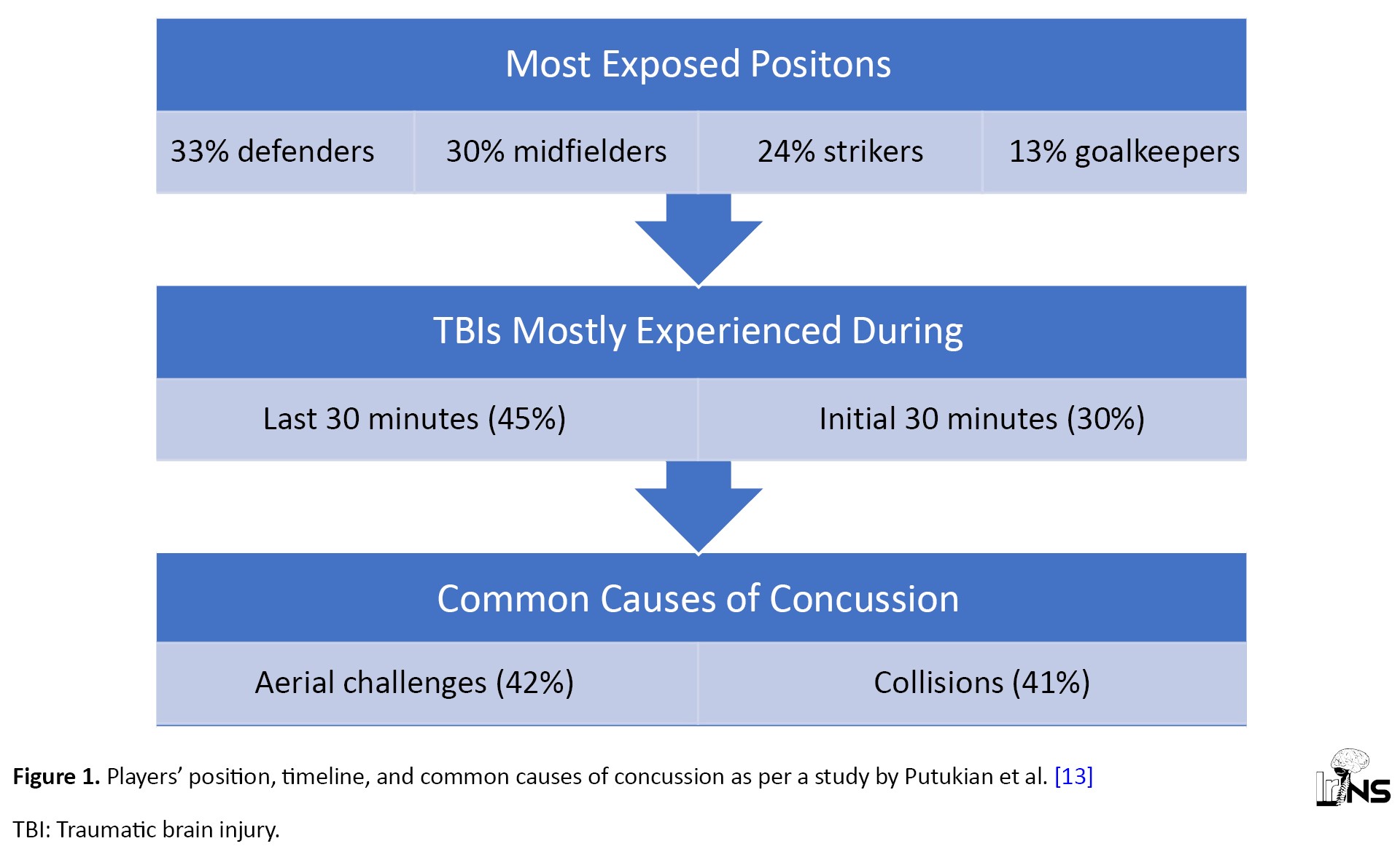
Most players knew an impact was coming [12]. It is critical to be aware of impending contact since it helps you to prepare for it [12]. Defenders were most exposed to collisions and aerial challenges common causes of concussions in the midfield (Figure 1) [13]. A frequent source of concussions in Major League Soccer (MLS) was head-to-head contact [13]. In a preliminary examination of sports-related concussion (SRC) video analysis in MLS players, visual evidence of concussion, observable signs, or both (loss of consciousness, gripping or holding the head, dropping to the floor, being sluggish to get up, or appearing disoriented or confused) were discovered in 28% of match concussions [13]. Twenty-six unintentional head hits were documented in 20 players, or 37% (95% confidence interval [CI]; 24.3%, 51.3%) of players throughout a soccer season in France, with four players being exposed to repeated blows two or three times [14]. Involuntary head hits were experienced by 60% (95% CI; 26.2%, 87.8%) of strikers and 62.5% (95% CI, 24.49%, 91.48%) of center-backs [14]. Despite this, no statistically significant difference (P=0.22) was observed in averages of hits per player based on player position. Involuntary impacts were projected to occur in 44.1/1000 player-hours (95% CI; 27.1%, 60.9%) [14]. Forwards and center-backs performed more headers than other players due to their positioning in “receiving areas” of the field [14]. Despite this, forwards showed a great deal of variation [14]. Defensive players reported being the most often to head the ball in a survey of the Norwegian professional soccer players, followed by forwards [15]. Otherwise, in a study conducted by Koerte et al. [16], center-midfielders were defined as “distance headers” who were much more habituated to heading with higher kinetics, although only headers that occurred during training were considered, and male sportsmen were pretty young (mean age of 15.7±0.7 years). Videotapes and injury data from the Norwegian soccer league were collected prospectively throughout the 2000 season [17]. Head injuries amounted to 2.0/1000 player hours, and concussions accounted for 0.5/1000 player hours [17]. Another research of players in the Norwegian elite league acquired and evaluated videotapes of all head hits throughout the 2004 and 2005 seasons [15]. There were 19.6 head accidents per 1000 playing hours (including referee stoppage time) [15].
Type of TBI seen in soccers
Understanding the type of TBIs experienced by players paves the way in the future for football federations to investigate and comprehend how and why these incidences of head injuries are observed so often. This current article reviews the occurrence of TBIs because many cases go unnoticed due to the minimal occurrence of symptoms related to TBI (Table 2).
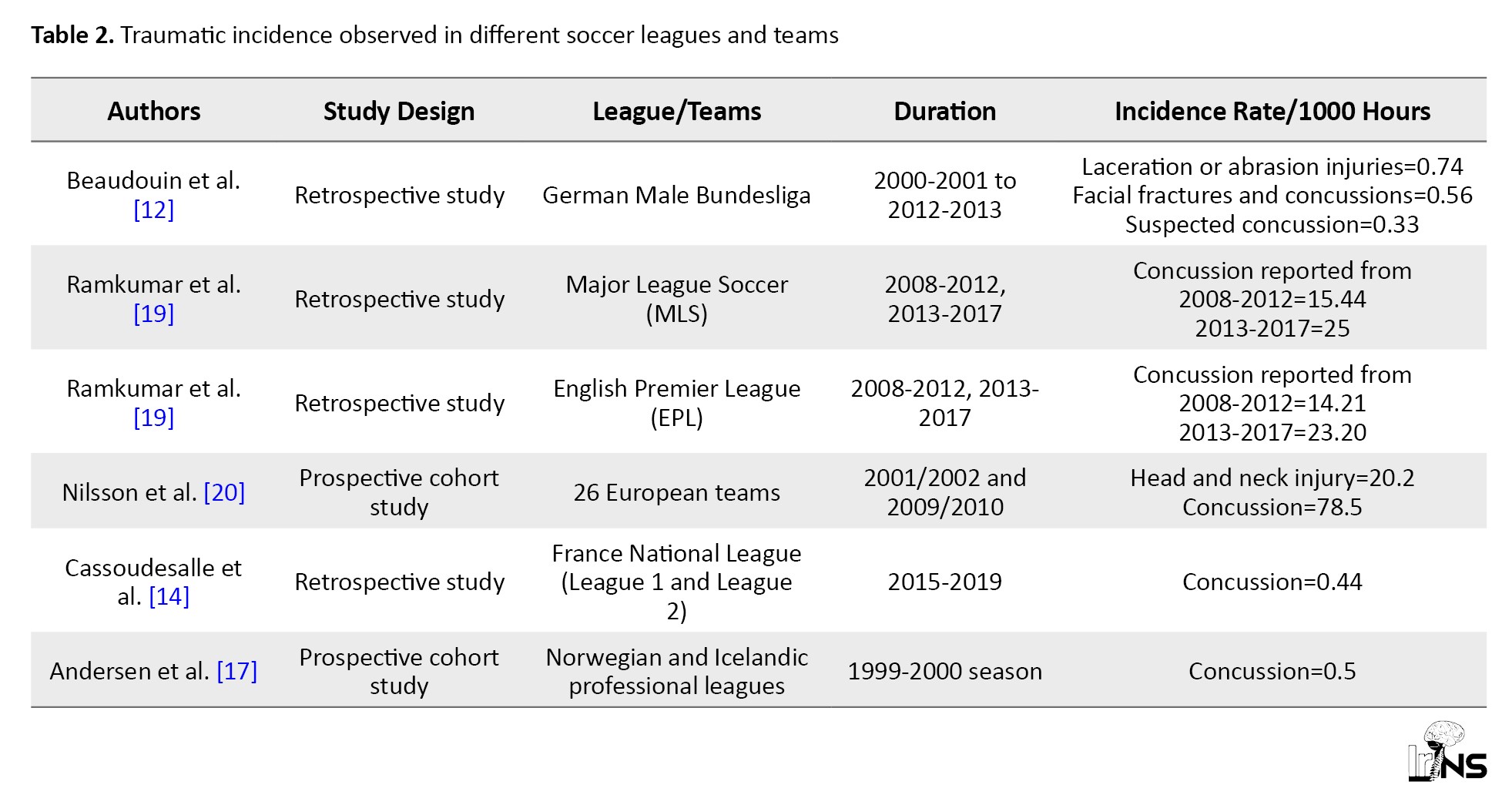
A study conducted in Germany investigated head injuries experienced by soccer players in 13 seasons in German league Bundesliga [12]. It was observed that out of 1000 match hours, the incidence rate (IR) of head injuries was 2.22 (95% CI; 2.00%, 2.26%) [12]. Laceration or abrasion injuries were observed, which were the most common type of injuries [12]. In Sweden, a descriptive retrospective study was performed to assess SRC prevalence in elite Swedish soccer players [18]. 35.3% of male players answered in the survey that they suffered from concussions [18]. Major soccer league which is the American soccer league had an IR/1000 hours of 15.44 for a concussion during the 2008 to 2012 season, whereas for the 2013 to 2017 seasons, IR/1000 hours rose to 25.00 [19]. Additionally, the English Premier League (EPL), the prime soccer league in England, had an IR/1000 hours for the 2008-2012 season of 14.21 and 2013-2017 of 23.20 [19]. Between 2001 and 2010, Nilsson et al. examined 136 neck and head trauma in 26 European professional football teams (2.2% of all injuries). Concussion was the most common type of head injury (n=48; 35.3%) [20]. From 1998 to 2012, Junge and Dvoák compiled injury data from 51 Fédération Internationale de Football Association (FIFA)-sponsored competitions and four Olympic Games. The team physicians recorded 3 944 injuries, with 577(15%) affecting the head or neck. Concussion was identified in 81 injuries (2% of all injuries) [21].
Contact mechanisms of injury seen in soccer players
There should be implications for players to be careful in performing certain tackles so that the game can be played safely. Two methods may cause TBIs in soccer [5, 22]. Unintentional head hits and hits to the head from various parts of the body of players (head-to-head, elbow-to-head), hitting the head on the floor, football goal frame, or even strikes garnered by the free-kick, when the ball flies and hits the unready player with incredible speed, are the most common causes of head injuries in football [5, 14, 22-24]. Another cause of brain injuries in soccer is forces that are not high enough to cause concussion symptoms. Microtrauma and subconcussive brain trauma are terminologies that are used in these situations [5, 20, 21]. Deliberate rebounding of the ball to manipulate, re-directing, or even speed its path toward a target causes a lot of injuries [5, 22]. Sub concussive brain injuries have a cumulative, chronic, but less severe effect. The quantity of head strikes is also crucial. Professional players were observed to smash the ball using their heads anywhere from 6 to 16 times every match. The more proficient the players are, the more high-intensity training and match frequency are required of them. This reflects a significant cumulative weight of head impacts during a footballer’s professional career, which can last up to 20 years [14, 22-24]. A retrospective study conducted in the France neurorehabilitation unit in which recorded data was obtained from the French Football Federation mentioned that 47% of players suffer from concussion through the head-to-head mechanism, with an aerial challenge (61%) being the most common playing action responsible of causing it [23]. According to the literature, aerial challenges caused well over 50% of concussions, and aerial challenges caused 94% of head-to-head concussions [12, 17, 25]. In research conducted in France, elbow-to-head injuries accounted for just 8% of concussions, confirming the results shown when a new rule in professional football for men was implemented in 2006 (red card given on deliberate elbow-to-head tackles as punishment) and indicating a reduction in concussion rates [23]. According to preliminary data from the 2014–2016 seasons, many concussions were caused by contact with a competitor (71%) but also by contact with a fellow player (16%) [13].
Symptoms acquired by the players
TBIs can be difficult to interpret since injuries with (accompanying) concussion symptoms are frequently misdiagnosed as a head contusion rather than a concussion or TBI. Due to weak symptoms or concealed post-injury signals by the player, concussions are readily disregarded by laypeople and even medical personnel [12]. A total of 41.6% of players exhibited concomitant neurological symptoms with 9.8% reporting dizziness in a study conducted in Germany, including a headache in the first 24 hours following trauma. None of the football players with midfacial fractures and or concussions showed any persisting neurologic symptoms in follow-up assessments at the moment of coming back or 6 months following trauma [26]. Both forgetfulness and unconsciousness were reported by 40.0% of elite Swedish players at the time of concussion, with both symptoms being more common in men than women (P=0.001). The most common acute symptom was dizziness, and the most common chronic symptom was a headache in Sweden. A player’s health may be jeopardized if they experience persistent symptoms. Almost 10% of the participants in the Swedish study said that their symptoms lasted more than three months. They also discovered a link between both the number of past concussions and the occurrence of symptoms that persisted. After the players’ most recent concussion episode, players with a history of concussions were more likely to feel fatigued, have concentration/memory difficulties, and have headaches. Dizziness (82%) and nausea were the two most reported acute SRC symptoms (59.2%) [18]. A total of 295 players experienced at least one symptom (concentration/memory difficulties, headache, exhaustion, nausea, and/or dizziness) lasting more than 24 hours (88.3%) [18]. The most prevalent persistent complaint among these was headache (reported by 271 players, 81.6%) [18]. For 61.3% of the participants, symptom relief took one week or less [18]. In 8.5% of the players, symptoms lasted longer than three months, and in 3.1%, it lasted longer than a year [18]. The players’ awareness was certainly lost after these three head-to-head collisions, according to a video analysis of the game played in the French football league [14]. A total of 29 head injuries exist (2.9/1000 match hours IR, 95% CI; 2.0%, 4.1%). Another study conducted in France saw concussions accounted for 48% of all injuries (IR of 1.4, 95% CI; 0.8%, 2.3%), followed by head/facial fractures (24%, IR of 0.7, 95% CI; 0.%, 1.5%), abrasions/lacerations (7%, IR of 0.2, 95% CI, 0.1%, 0.8%) and head/facial contusions (21%, IR of 0.6, 95% CI, 0.3%, 1.3%). The total number of injuries caused by headers includes 29 head injuries, which were all verified during the video analysis. The ‘suspected concussion’ subgroup accounted for 17% of all head trauma and included 1 zygomatic bone fracture and 4 head contusions.
Except for goalkeepers, footballers in the EPL performed poorly compared to minutes played, assisted, scoring chances, and overall shots following a concussion [19]. Concussions took an average of 10.5 days to heal, while 27% of concussed athletes returned to the game within 5 days [13]. Concussed EPL players averaged 0.5 fewer assists per year, 5.2 fewer games started per year, 3.5 fewer shots on goal per year, and 8.2 fewer total shots per year than non-concussed players [19]. Following a concussion, non-goalkeeper soccer players in MLS experienced no substantial declines in total games, goals, assisting, shot attempts, or total attempts in the second half of this season [19]. Further examination of professionals who retired during the abovementioned study found that the odds of performing 1, 3, and 5 years in MLS after a concussion were 52.6% versus 57.2%, 19.2% versus 25.3%, and 5.1% versus 12.7%, respectively, when compared to the healthy population [19]. Compared to healthy players in MLS, concussed players had the same survival rate (log-rank P=0.787, hazard ratio=1.03) [19]. After a concussion, the odds of playing in the EPL for 1, 3, or 5 years were 83% versus 59%, 56% versus 26%, and 27% versus 14%, respectively, compared to the healthy group [19]. Concussed players had a higher survival rate than healthy players in the EPL (log-rank P=0.0001, hazard ratio=0.414) [19].
4. Discussion
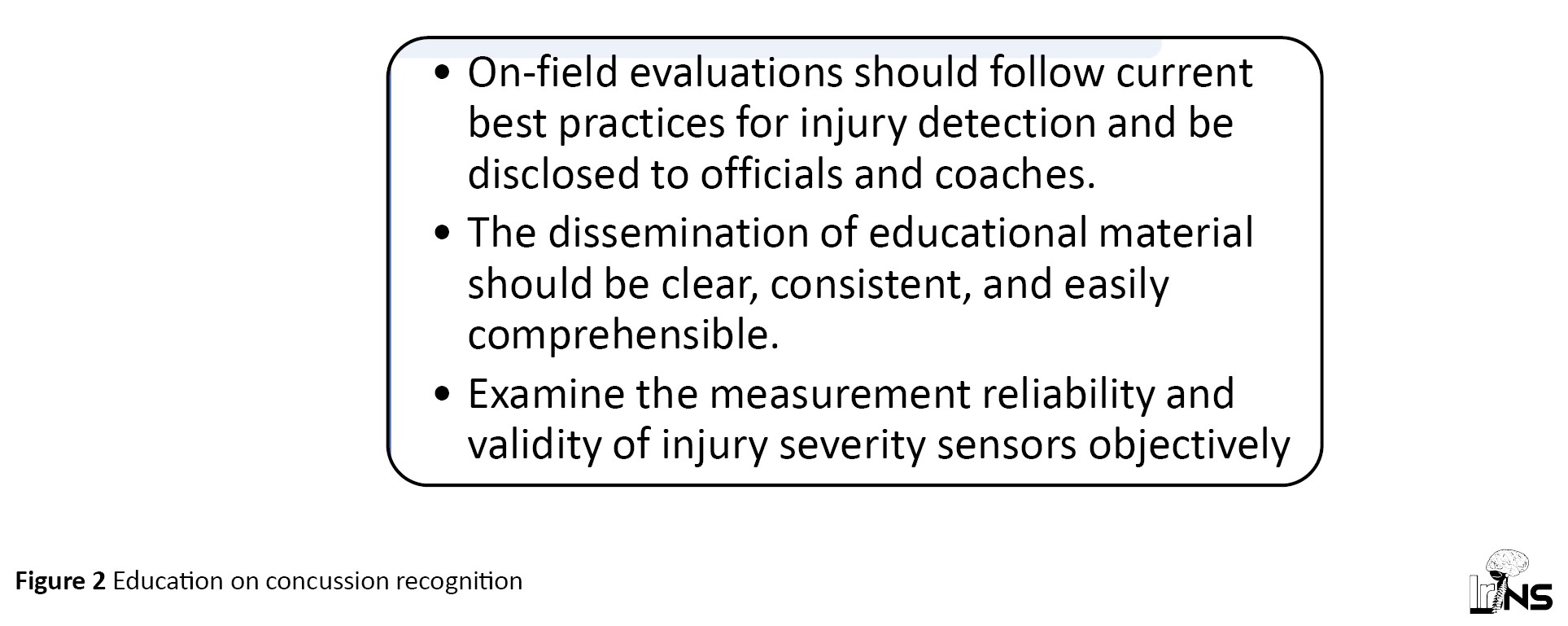
There have been conversations at several levels, including the Concussion in Sport Group (CISG), FIFA, National Governing Organizations, and National Collegiate Athletics Association (NCAA), concerning rule changes that would allow medical staff to undertake an immediate examination when an injury is suspected [13]. Any suggested amendments to soccer’s Rules of the Game should include the possibility of opportunism or tremendous pressure on medical professionals to restore a player to the pitch [13]. The precise and timely diagnosis of the probable injury is a key component of any successful concussion care approach [13]. It is critical not to overlook “red flags” during a sideline evaluation to distinguish a concussion from much more severe damage like traumatic cord injury or structural brain damage [27]. Vomiting, neck stiffness, motor or sensory deficiencies in the extremities, double vision, and seizures are all red flags that indicate a dangerous situation [27]. Referees, coaches, administrators, athletes, sports medicine physicians, athletic trainers, physical therapists, neuropsychologists, and strength and conditioning specialists are all responsible for recognizing the injury [13]. As a result, damage identification requires the education of these populations [13]. Officials’ primary role is to keep players safe, not to diagnose injuries [13]. Any modifications to on-field evaluations must take current best practices for injury detection and evaluation into account, and such modifications must be disclosed to those who teach and educate officials and coaches [13]. Education is a joint effort (Figure 2), and as members of the soccer community, we play an active role in ensuring that this demographic has access to up-to-date, scientifically based knowledge [13]. Awareness, advancement, and policy change are all aided by education [13]. Whilst sensors for non-helmeted athletics are being developed (e.g. mouthguards, earpieces, retainers, and others), none have been verified, and their usage in soccer outside of a research context is not now recommended [13]. Given the growing number of injury risk sensors entering the commercial market, it is critical to analyze the assessment validity and reliability of these systems completely and objectively [13]. While sensors for non-helmeted athletics (for example, mouthguards, earpieces, retainers, and others) are being developed, none have been confirmed, and their use in soccer except in a research context is not encouraged at this time [13]. The 2018 Football World Cup in Russia first used spotters to aid and convey potential injuries to on-field medical professionals [13]. The risks and long-term repercussions of recurrent concussions highlight the need to accurately diagnose and treat concussions to prevent athletes from experiencing long-term neurological and behavioral problems [27]. While this is visible in traditional risk sports, such as American football and ice hockey, despite soccer’s global appeal, broad recognition is only gradually happening for the sport [27]. Head injuries in soccer are typically underdiagnosed, and potential effects are overlooked, due to the heterogeneous and generally mild symptoms of trauma [27]. Another issue that can result in players being not taken out of play when they should is the truth that the medical team is under a lot of strain [18]. During the 2014 World Cup, :union: of European Football Associations (UEFA) established new guidelines for concussions, allowing the referee to call a 3-minute timeout for the injured player so that the doctor can evaluate them [18]. The following season, this was brought to Sweden [20]. It was disclosed in a prospective cohort study that on-medical personnel were mostly responsible for treating midfacial fractures in the field [26]. After suffering an injury, most players from both teams went to a trauma center right after (semi-professionals: 86.5%; amateurs: 75.8%) [26]. When athletes were diagnosed with a concussion or a serious midfacial fracture, they were only admitted to the hospital for 24 hours [26]. According to current recommendations, which include those from FIFA, athletes who are diagnosed with SRC should be taken out of the game and examined by a medical professional skilled in managing concussions; they should not return to play the same day [28]. It is advised to take a first phase of physical and mental rest [29]. A step-by-step symptom-limited development of increased physical, cognitive, work- or school-related activity is then part of the return to academic and athletic processes [28].
5. Conclusion
In summary, heading in soccer has been connected to both short- and long-term traumatic brain damage in male players. Head-to-head contact was identified as a major cause of concussions in MLS, with defense players being the most vulnerable to collisions and aerial challenges that result in concussions. It is crucial to diagnose injuries as soon as possible and officials, coaches, players, and medical personnel need to be informed. More research is needed to address the gaps in understanding regarding potential preventive measures and management strategies to enhance player safety.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Uzair Yaqoob, Roshan Dhakal, and Deeven Karki; Data collection: Sujha Ghimire, Naveed Ahmed, and Tabeer Tanwir Awan; Data analysis and interpretation: Sujha Ghimire, Naveed Ahmed, and Tabeer Tanwir Awan; Writing the original draft: Uzair Yaqoob, Roshan Dhakal, Deeven Karki; Review, editing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Given that soccer is a globally prevalent sport with more than 224 million players worldwide, concerns about the potential for short- or long-term brain trauma have gained prominence [1, 2]. The practice of playing or hitting a ball with one’s head originated in northern England [1]. It grew in popularity following the Football Association’s adoption of the original rules in 1863. The organization quickly set up a new rule prohibiting ball interaction with hands in 1872 [3]. Since then, the so-called head-to-head play has become a staple of soccer [1]. Heading the ball, deeply ingrained in soccer, poses risks beyond the known dangers of collisions during play [4, 5]. Detailed investigations are underway to understand the level, aspect, and potential repercussions of heading, including cognitive consequences, both short- and long-term [1, 6]. A recent study revealing a link between heading the soccer ball and decreased cognitive performance within 24 hours emphasizes the need for a comprehensive examination of traumatic brain injuries (TBIs) in modern football [7]. As a result, the number of head impact accidents involving a biomechanical force communicated to the skull and brain, often known as a “sub-concussive hit”, is unknown.
Purposeful soccer headings are more common than incidental head impacts, but their severity is usually lower [8]. It is unknown whether purposeful soccer headings are harmful to the brain [9]. One controlled heading session has been linked to higher rates of reported concussion symptoms, changes in postural control, and higher levels of corticomotor inhibition along with memory impairment [7, 10]. There has been evidence of brain white matter microstructure abnormalities and cognition problems in players who self-reported long-term exposure to 885 to 1800 headers annually [11]. However, some studies have not discovered any appreciable neuropsychological or neurocognitive impairments linked to brief exposure to soccer headings. This narrative review article aims to evaluate the incidence, contact methods, impact damage, associated symptoms, and management protocols related to TBIs in soccer. By addressing the gaps in understanding the frequency and classification of TBIs in modern football, this study contributes to the broader discourse on player safety and informs potential preventive measures and management strategies.
2. Materials and Methods
The authors went through PubMed, Scopus, and Google Scholar databases. Search terms used were as follows: “Traumatic brain injuries or TBIs”, “concussion”, “male soccer players or male soccer athletes”, “incidence”, “injury”, “cognitive impairments or changes”, and “management”. The publications from the last two decades were considered. Retrospective, prospective, and clinical studies in the English language were included in this review. The population, exposure, comparison, outcome (PECO) framework (with intervention replaced with exposure) was used to simplify the research question which is presented in Table 1.
3. Results
Most players knew an impact was coming [12]. It is critical to be aware of impending contact since it helps you to prepare for it [12]. Defenders were most exposed to collisions and aerial challenges common causes of concussions in the midfield (Figure 1) [13]. A frequent source of concussions in Major League Soccer (MLS) was head-to-head contact [13]. In a preliminary examination of sports-related concussion (SRC) video analysis in MLS players, visual evidence of concussion, observable signs, or both (loss of consciousness, gripping or holding the head, dropping to the floor, being sluggish to get up, or appearing disoriented or confused) were discovered in 28% of match concussions [13]. Twenty-six unintentional head hits were documented in 20 players, or 37% (95% confidence interval [CI]; 24.3%, 51.3%) of players throughout a soccer season in France, with four players being exposed to repeated blows two or three times [14]. Involuntary head hits were experienced by 60% (95% CI; 26.2%, 87.8%) of strikers and 62.5% (95% CI, 24.49%, 91.48%) of center-backs [14]. Despite this, no statistically significant difference (P=0.22) was observed in averages of hits per player based on player position. Involuntary impacts were projected to occur in 44.1/1000 player-hours (95% CI; 27.1%, 60.9%) [14]. Forwards and center-backs performed more headers than other players due to their positioning in “receiving areas” of the field [14]. Despite this, forwards showed a great deal of variation [14]. Defensive players reported being the most often to head the ball in a survey of the Norwegian professional soccer players, followed by forwards [15]. Otherwise, in a study conducted by Koerte et al. [16], center-midfielders were defined as “distance headers” who were much more habituated to heading with higher kinetics, although only headers that occurred during training were considered, and male sportsmen were pretty young (mean age of 15.7±0.7 years). Videotapes and injury data from the Norwegian soccer league were collected prospectively throughout the 2000 season [17]. Head injuries amounted to 2.0/1000 player hours, and concussions accounted for 0.5/1000 player hours [17]. Another research of players in the Norwegian elite league acquired and evaluated videotapes of all head hits throughout the 2004 and 2005 seasons [15]. There were 19.6 head accidents per 1000 playing hours (including referee stoppage time) [15].
Type of TBI seen in soccers
Understanding the type of TBIs experienced by players paves the way in the future for football federations to investigate and comprehend how and why these incidences of head injuries are observed so often. This current article reviews the occurrence of TBIs because many cases go unnoticed due to the minimal occurrence of symptoms related to TBI (Table 2).
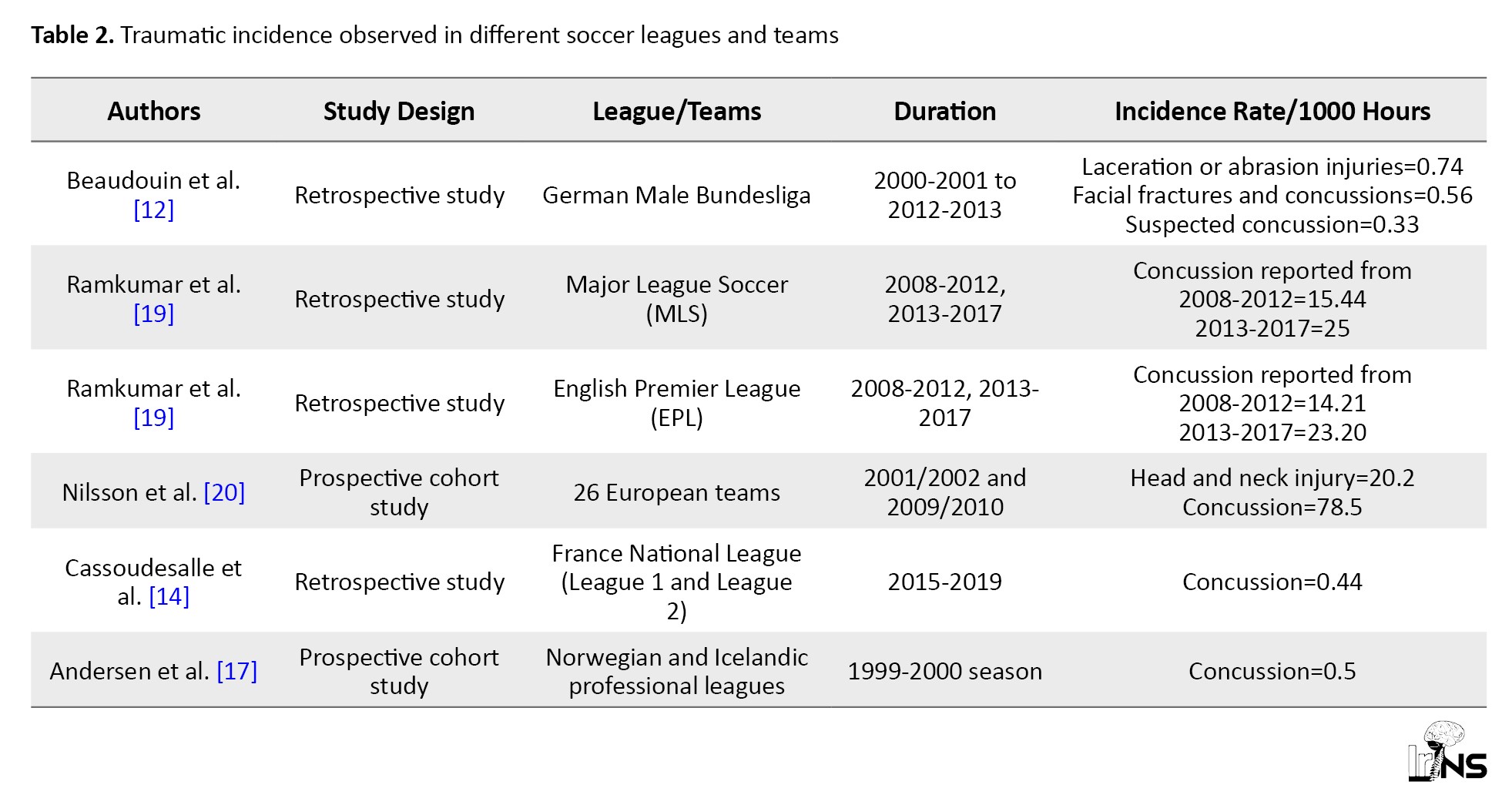
A study conducted in Germany investigated head injuries experienced by soccer players in 13 seasons in German league Bundesliga [12]. It was observed that out of 1000 match hours, the incidence rate (IR) of head injuries was 2.22 (95% CI; 2.00%, 2.26%) [12]. Laceration or abrasion injuries were observed, which were the most common type of injuries [12]. In Sweden, a descriptive retrospective study was performed to assess SRC prevalence in elite Swedish soccer players [18]. 35.3% of male players answered in the survey that they suffered from concussions [18]. Major soccer league which is the American soccer league had an IR/1000 hours of 15.44 for a concussion during the 2008 to 2012 season, whereas for the 2013 to 2017 seasons, IR/1000 hours rose to 25.00 [19]. Additionally, the English Premier League (EPL), the prime soccer league in England, had an IR/1000 hours for the 2008-2012 season of 14.21 and 2013-2017 of 23.20 [19]. Between 2001 and 2010, Nilsson et al. examined 136 neck and head trauma in 26 European professional football teams (2.2% of all injuries). Concussion was the most common type of head injury (n=48; 35.3%) [20]. From 1998 to 2012, Junge and Dvoák compiled injury data from 51 Fédération Internationale de Football Association (FIFA)-sponsored competitions and four Olympic Games. The team physicians recorded 3 944 injuries, with 577(15%) affecting the head or neck. Concussion was identified in 81 injuries (2% of all injuries) [21].
Contact mechanisms of injury seen in soccer players
There should be implications for players to be careful in performing certain tackles so that the game can be played safely. Two methods may cause TBIs in soccer [5, 22]. Unintentional head hits and hits to the head from various parts of the body of players (head-to-head, elbow-to-head), hitting the head on the floor, football goal frame, or even strikes garnered by the free-kick, when the ball flies and hits the unready player with incredible speed, are the most common causes of head injuries in football [5, 14, 22-24]. Another cause of brain injuries in soccer is forces that are not high enough to cause concussion symptoms. Microtrauma and subconcussive brain trauma are terminologies that are used in these situations [5, 20, 21]. Deliberate rebounding of the ball to manipulate, re-directing, or even speed its path toward a target causes a lot of injuries [5, 22]. Sub concussive brain injuries have a cumulative, chronic, but less severe effect. The quantity of head strikes is also crucial. Professional players were observed to smash the ball using their heads anywhere from 6 to 16 times every match. The more proficient the players are, the more high-intensity training and match frequency are required of them. This reflects a significant cumulative weight of head impacts during a footballer’s professional career, which can last up to 20 years [14, 22-24]. A retrospective study conducted in the France neurorehabilitation unit in which recorded data was obtained from the French Football Federation mentioned that 47% of players suffer from concussion through the head-to-head mechanism, with an aerial challenge (61%) being the most common playing action responsible of causing it [23]. According to the literature, aerial challenges caused well over 50% of concussions, and aerial challenges caused 94% of head-to-head concussions [12, 17, 25]. In research conducted in France, elbow-to-head injuries accounted for just 8% of concussions, confirming the results shown when a new rule in professional football for men was implemented in 2006 (red card given on deliberate elbow-to-head tackles as punishment) and indicating a reduction in concussion rates [23]. According to preliminary data from the 2014–2016 seasons, many concussions were caused by contact with a competitor (71%) but also by contact with a fellow player (16%) [13].
Symptoms acquired by the players
TBIs can be difficult to interpret since injuries with (accompanying) concussion symptoms are frequently misdiagnosed as a head contusion rather than a concussion or TBI. Due to weak symptoms or concealed post-injury signals by the player, concussions are readily disregarded by laypeople and even medical personnel [12]. A total of 41.6% of players exhibited concomitant neurological symptoms with 9.8% reporting dizziness in a study conducted in Germany, including a headache in the first 24 hours following trauma. None of the football players with midfacial fractures and or concussions showed any persisting neurologic symptoms in follow-up assessments at the moment of coming back or 6 months following trauma [26]. Both forgetfulness and unconsciousness were reported by 40.0% of elite Swedish players at the time of concussion, with both symptoms being more common in men than women (P=0.001). The most common acute symptom was dizziness, and the most common chronic symptom was a headache in Sweden. A player’s health may be jeopardized if they experience persistent symptoms. Almost 10% of the participants in the Swedish study said that their symptoms lasted more than three months. They also discovered a link between both the number of past concussions and the occurrence of symptoms that persisted. After the players’ most recent concussion episode, players with a history of concussions were more likely to feel fatigued, have concentration/memory difficulties, and have headaches. Dizziness (82%) and nausea were the two most reported acute SRC symptoms (59.2%) [18]. A total of 295 players experienced at least one symptom (concentration/memory difficulties, headache, exhaustion, nausea, and/or dizziness) lasting more than 24 hours (88.3%) [18]. The most prevalent persistent complaint among these was headache (reported by 271 players, 81.6%) [18]. For 61.3% of the participants, symptom relief took one week or less [18]. In 8.5% of the players, symptoms lasted longer than three months, and in 3.1%, it lasted longer than a year [18]. The players’ awareness was certainly lost after these three head-to-head collisions, according to a video analysis of the game played in the French football league [14]. A total of 29 head injuries exist (2.9/1000 match hours IR, 95% CI; 2.0%, 4.1%). Another study conducted in France saw concussions accounted for 48% of all injuries (IR of 1.4, 95% CI; 0.8%, 2.3%), followed by head/facial fractures (24%, IR of 0.7, 95% CI; 0.%, 1.5%), abrasions/lacerations (7%, IR of 0.2, 95% CI, 0.1%, 0.8%) and head/facial contusions (21%, IR of 0.6, 95% CI, 0.3%, 1.3%). The total number of injuries caused by headers includes 29 head injuries, which were all verified during the video analysis. The ‘suspected concussion’ subgroup accounted for 17% of all head trauma and included 1 zygomatic bone fracture and 4 head contusions.
Except for goalkeepers, footballers in the EPL performed poorly compared to minutes played, assisted, scoring chances, and overall shots following a concussion [19]. Concussions took an average of 10.5 days to heal, while 27% of concussed athletes returned to the game within 5 days [13]. Concussed EPL players averaged 0.5 fewer assists per year, 5.2 fewer games started per year, 3.5 fewer shots on goal per year, and 8.2 fewer total shots per year than non-concussed players [19]. Following a concussion, non-goalkeeper soccer players in MLS experienced no substantial declines in total games, goals, assisting, shot attempts, or total attempts in the second half of this season [19]. Further examination of professionals who retired during the abovementioned study found that the odds of performing 1, 3, and 5 years in MLS after a concussion were 52.6% versus 57.2%, 19.2% versus 25.3%, and 5.1% versus 12.7%, respectively, when compared to the healthy population [19]. Compared to healthy players in MLS, concussed players had the same survival rate (log-rank P=0.787, hazard ratio=1.03) [19]. After a concussion, the odds of playing in the EPL for 1, 3, or 5 years were 83% versus 59%, 56% versus 26%, and 27% versus 14%, respectively, compared to the healthy group [19]. Concussed players had a higher survival rate than healthy players in the EPL (log-rank P=0.0001, hazard ratio=0.414) [19].
4. Discussion
There have been conversations at several levels, including the Concussion in Sport Group (CISG), FIFA, National Governing Organizations, and National Collegiate Athletics Association (NCAA), concerning rule changes that would allow medical staff to undertake an immediate examination when an injury is suspected [13]. Any suggested amendments to soccer’s Rules of the Game should include the possibility of opportunism or tremendous pressure on medical professionals to restore a player to the pitch [13]. The precise and timely diagnosis of the probable injury is a key component of any successful concussion care approach [13]. It is critical not to overlook “red flags” during a sideline evaluation to distinguish a concussion from much more severe damage like traumatic cord injury or structural brain damage [27]. Vomiting, neck stiffness, motor or sensory deficiencies in the extremities, double vision, and seizures are all red flags that indicate a dangerous situation [27]. Referees, coaches, administrators, athletes, sports medicine physicians, athletic trainers, physical therapists, neuropsychologists, and strength and conditioning specialists are all responsible for recognizing the injury [13]. As a result, damage identification requires the education of these populations [13]. Officials’ primary role is to keep players safe, not to diagnose injuries [13]. Any modifications to on-field evaluations must take current best practices for injury detection and evaluation into account, and such modifications must be disclosed to those who teach and educate officials and coaches [13]. Education is a joint effort (Figure 2), and as members of the soccer community, we play an active role in ensuring that this demographic has access to up-to-date, scientifically based knowledge [13]. Awareness, advancement, and policy change are all aided by education [13]. Whilst sensors for non-helmeted athletics are being developed (e.g. mouthguards, earpieces, retainers, and others), none have been verified, and their usage in soccer outside of a research context is not now recommended [13]. Given the growing number of injury risk sensors entering the commercial market, it is critical to analyze the assessment validity and reliability of these systems completely and objectively [13]. While sensors for non-helmeted athletics (for example, mouthguards, earpieces, retainers, and others) are being developed, none have been confirmed, and their use in soccer except in a research context is not encouraged at this time [13]. The 2018 Football World Cup in Russia first used spotters to aid and convey potential injuries to on-field medical professionals [13]. The risks and long-term repercussions of recurrent concussions highlight the need to accurately diagnose and treat concussions to prevent athletes from experiencing long-term neurological and behavioral problems [27]. While this is visible in traditional risk sports, such as American football and ice hockey, despite soccer’s global appeal, broad recognition is only gradually happening for the sport [27]. Head injuries in soccer are typically underdiagnosed, and potential effects are overlooked, due to the heterogeneous and generally mild symptoms of trauma [27]. Another issue that can result in players being not taken out of play when they should is the truth that the medical team is under a lot of strain [18]. During the 2014 World Cup, :union: of European Football Associations (UEFA) established new guidelines for concussions, allowing the referee to call a 3-minute timeout for the injured player so that the doctor can evaluate them [18]. The following season, this was brought to Sweden [20]. It was disclosed in a prospective cohort study that on-medical personnel were mostly responsible for treating midfacial fractures in the field [26]. After suffering an injury, most players from both teams went to a trauma center right after (semi-professionals: 86.5%; amateurs: 75.8%) [26]. When athletes were diagnosed with a concussion or a serious midfacial fracture, they were only admitted to the hospital for 24 hours [26]. According to current recommendations, which include those from FIFA, athletes who are diagnosed with SRC should be taken out of the game and examined by a medical professional skilled in managing concussions; they should not return to play the same day [28]. It is advised to take a first phase of physical and mental rest [29]. A step-by-step symptom-limited development of increased physical, cognitive, work- or school-related activity is then part of the return to academic and athletic processes [28].
5. Conclusion
In summary, heading in soccer has been connected to both short- and long-term traumatic brain damage in male players. Head-to-head contact was identified as a major cause of concussions in MLS, with defense players being the most vulnerable to collisions and aerial challenges that result in concussions. It is crucial to diagnose injuries as soon as possible and officials, coaches, players, and medical personnel need to be informed. More research is needed to address the gaps in understanding regarding potential preventive measures and management strategies to enhance player safety.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Uzair Yaqoob, Roshan Dhakal, and Deeven Karki; Data collection: Sujha Ghimire, Naveed Ahmed, and Tabeer Tanwir Awan; Data analysis and interpretation: Sujha Ghimire, Naveed Ahmed, and Tabeer Tanwir Awan; Writing the original draft: Uzair Yaqoob, Roshan Dhakal, Deeven Karki; Review, editing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Bunc G, Ravnik J, Velnar T. May heading in soccer result in traumatic brain injury? A review of literature. Medical Archives (Sarajevo, Bosnia and Herzegovina). 2017; 71(5):356-9. [DOI:10.5455/medarh.2017.71.356-359]
- Guthrie RM. Emerging data on the incidence of concussion in football practice at all levels of amateur play. The Physician and sportsmedicine.. 2015; 43(4):333-5. [DOI: 10.1080/00913847.2015.1081552] [PMID]
- Bangsbo J, Norregaard L, Thorso F. Activity profile of competition soccer. Canadian Journal of Sport Sciences. 1991; 16(2):110-6. [PMID]
- Pickett W, Streight S, Simpson K, Brison RJ. Head injuries in youth soccer players presenting to the emergency department. British Journal of Sports Medicine. 2005; 39(4):226-31; discussion -31. [DOI:10.1136/bjsm.2004.013169]
- Kirkendall DT, Jordan SE, Garrett WE. Heading and head injuries in soccer. Sports Medicine. 2001; 31(5):369-86. [DOI:10.2165/00007256-200131050-00006]
- Rodrigues AC, Lasmar RP, Caramelli P. Effects of soccer heading on brain structure and function. Frontiers in Neurology. 2016; 7:38. [DOI:10.3389/fneur.2016.00038]
- Di Virgilio TG, Hunter A, Wilson L, Stewart W, Goodall S, Howatson G, et al. Evidence for acute electrophysiological and cognitive changes following routine soccer heading. eBioMedicine. 2016; 13:66-7. [DOI:10.1016/j.ebiom.2016.10.029]
- Rezaei A, Wu LC. Automated soccer head impact exposure tracking using video and deep learning. Scientific Reports. 2022; 12(1):9282. [DOI:10.1038/s41598-022-13220-2]
- Stemper BD, Shah AS, Harezlak J, Rowson S, Mihalik JP, Duma SM, et al. Comparison of head impact exposure between concussed football athletes and matched controls: Evidence for a possible second mechanism of sport-related concussion. Annals of Biomedical Engineering. 2019; 47(10):2057-72. [DOI:10.1007/s10439-018-02136-6]
- Haran FJ, Tierney R, Wright WG, Keshner E, Silter M. Acute changes in postural control after soccer heading. International Journal of Sports Medicine. 2013; 34(4):350-4. [DOI:10.1055/s-0032-1304647]
- Lipton ML, Kim N, Zimmerman ME, Kim M, Stewart WF, Branch CA, et al. Soccer heading is associated with white matter microstructural and cognitive abnormalities. Radiology. 2013; 268(3):850-7. [DOI:10.1148/radiol.13130545]
- Beaudouin F, Aus der Funten K, Tross T, Reinsberger C, Meyer T. Head injuries in professional male football (soccer) over 13 years: 29% lower incidence rates after a rule change (red card). British Journal of Sports Medicine. 2019; 53(15):948-52. [DOI:10.1136/bjsports-2016-097217]
- Putukian M, Echemendia RJ, Chiampas G, Dvorak J, Mandelbaum B, Lemak LJ, et al. Head Injury in Soccer: From Science to the Field; summary of the head injury summit held in April 2017 in New York City, New York. British Journal of Sports Medicine. 2019; 53(21):1332. [DOI:10.1136/bjsports-2018-100232]
- Cassoudesalle H, Laborde B, Orhant E, Dehail P. Video analysis of concussion mechanisms and immediate management in French men’s professional football (soccer) from 2015 to 2019. Scandinavian Journal of Medicine & Science. 2021; 31(2):465-72. [DOI:10.1111/sms.13852]
- Straume-Naesheim TM, Andersen TE, Dvorak J, Bahr R. Effects of heading exposure and previous concussions on neuropsychological performance among Norwegian elite footballers. British Journal of Sports Medicine. 2005; 39(suppl 1):i70-i7. [DOI:10.1136/bjsm.2005.019646]
- Koerte IK, Ertl-Wagner B, Reiser M, Zafonte R, Shenton ME. White matter integrity in the brains of professional soccer players without a symptomatic concussion. JAMA. 2012; 308(18):1859-61. [DOI:10.1001/jama.2012.13735]
- Andersen TE, Arnason A, Engebretsen L, Bahr R. Mechanisms of head injuries in elite football. British Journal of Sports Medicine. 2004; 38(6):690-6. [DOI:10.1136/bjsm.2003.009357]
- Hanni S, Vedung F, Tegner Y, Marklund N, Johansson J. Soccer-related concussions among swedish elite soccer players: A descriptive study of 1,030 players. Frontiers in Neurology. 2020; 11:510800. [DOI:10.3389/fneur.2020.510800]
- Ramkumar PN, Navarro SM, Haeberle HS, Luu BC, Jang A, Frangiamore SJ, et al. Concussion in American versus european professional soccer: A decade-long comparative analysis of incidence, return to play, performance, and longevity. The American Journal of Sports Medicine. 2019; 47(10):2287-93. [DOI:10.1177/0363546519859542]
- Nilsson M, Hagglund M, Ekstrand J, Walden M. Head and neck injuries in professional soccer. Clinical Journal of Sport Medicine. 2013; 23(4):255-60. [DOI:10.1097/JSM.0b013e31827ee6f8]
- Junge A, Dvorak J. Injury surveillance in the World Football Tournaments 1998-2012. British Journal of Sports Medicine. 2013; 47(12):782-8. [DOI:10.1136/bjsports-2013-092205]
- Levy ML, Ozgur BM, Berry C, Aryan HE, Apuzzo ML. Analysis and evolution of head injury in football. Neurosurgery. 2004; 55(3):649-55. [DOI:10.1227/01.NEU.0000134598.06114.89]
- Pellman EJ, Viano DC, Tucker AM, Casson I. Concussion in professional football: Location and direction of helmet impacts-Part 2. 2003; 53(6):1328-41. [DOI:10.1227/01.NEU.0000093499.20604.21]
- Viano DC, Casson IR, Pellman EJ. Concussion in professional football: Biomechanics of the struck player--part 14. Neurosurgery. 2007; 61(2):313-28; discussion 27-8. [DOI:10.1227/01.NEU.0000279969.02685.D0]
- Fuller CW, Junge A, Dvorak J. A six year prospective study of the incidence and causes of head and neck injuries in international football. British Journal of Sports Medicine. 2005; 39(Suppl 1):i3-9. [DOI:10.1136/bjsm.2005.018937]
- Krutsch V, Gesslein M, Loose O, Weber J, Nerlich M, Gaensslen A, et al. Injury mechanism of midfacial fractures in football causes in over 40% typical neurological symptoms of minor brain injuries. Knee Surgery, Sports Traumatology, Arthroscopy. 2018; 26(4):1295-302. [DOI:10.1007/s00167-017-4431-z]
- Hubertus V, Marklund N, Vajkoczy P. Management of concussion in soccer. Acta Neurochirurgica. 2019; 161(3):425-33. [DOI:10.1007/s00701-019-03807-6]
- McCrory P, Meeuwisse W, Dvořák J, Aubry M, Bailes J, Broglio S, et al. Consensus statement on concussion in sport-the 5(th) international conference on concussion in sport held in Berlin, October 2016. British Journal of Sports Medicine. 2017; 51(11):838-47. [DOI:10.1136/bjsports-2017-097699]
- Schneider KJ, Leddy JJ, Guskiewicz KM, Seifert T, McCrea M, Silverberg ND, et al. Rest and treatment/rehabilitation following sport-related concussion: A systematic review. British Journal of Sports Medicine. 2017; 51(12):930-4. [DOI:10.1136/bjsports-2016-097475]
Type of Study: Review |
Subject:
Neurotrauma
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |