Sun, Feb 22, 2026
Volume 10 - Continuous Publishing
Iran J Neurosurg 2024, 10 - Continuous Publishing: 98-104 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Chanideh I, Ghadiri M, Madani S H, Shoghi A, Alaghemand S, Mohammadi Majd T et al . Investigating Delayed Surgical Management of a Giant Rhabdomyomatous Meningioma: A Case Report. Iran J Neurosurg 2024; 10 : 11
URL: http://irjns.org/article-1-417-en.html
URL: http://irjns.org/article-1-417-en.html
Iran Chanideh1 

 , Masoud Ghadiri2
, Masoud Ghadiri2 

 , Seyed Hamid Madani3
, Seyed Hamid Madani3 

 , Ali Shoghi1
, Ali Shoghi1 

 , Sasan Alaghemand1
, Sasan Alaghemand1 

 , Tahereh Mohammadi Majd1
, Tahereh Mohammadi Majd1 

 , Saeed Gharooee Ahangar *4
, Saeed Gharooee Ahangar *4 




 , Masoud Ghadiri2
, Masoud Ghadiri2 

 , Seyed Hamid Madani3
, Seyed Hamid Madani3 

 , Ali Shoghi1
, Ali Shoghi1 

 , Sasan Alaghemand1
, Sasan Alaghemand1 

 , Tahereh Mohammadi Majd1
, Tahereh Mohammadi Majd1 

 , Saeed Gharooee Ahangar *4
, Saeed Gharooee Ahangar *4 


1- Clinical Research Development Center, Taleghani and Imam Ali Hospital, Kermanshah University of Medical Sciences, Kermanshah, Iran
2- Students Research Committee, School of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran
3- Molecular Pathology Research Center, Imam Reza Hospital, Kermanshah Universitiy of Medical Science, Kermanshah, Iran
4- Clinical Research Development Center, Taleghani and Imam Ali Hospital, Kermanshah University of Medical Sciences, Kermanshah, Iran ,saied_gharooee@yahoo.com
2- Students Research Committee, School of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran
3- Molecular Pathology Research Center, Imam Reza Hospital, Kermanshah Universitiy of Medical Science, Kermanshah, Iran
4- Clinical Research Development Center, Taleghani and Imam Ali Hospital, Kermanshah University of Medical Sciences, Kermanshah, Iran ,
Full Text [PDF 2535 kb]
(706 Downloads)
| Abstract (HTML) (2871 Views)
References
Full Text: (1036 Views)
1. Introduction
Meningioma is one of the most common benign tumors of the central nervous system (CNS), which usually arises from the meningeal layers of the brain or spinal cord [1]. These tumors are divided into three grades. About 80% of meningiomas are considered benign or grade I, while 17% to 18% are grade II and approximately 1.7% of meningiomas turn into grade III tumors [2-4]. According to the 2021 classification of the World Health Organization (WHO) for CNS tumors, rhabdoid meningioma (RM) is a subtype of meningiomas and a grade III tumor that usually consists of rhabdoid, i.e. round to ovoid cells with eccentric nuclei, paranuclear eosinophilic inclusions, and prominent nucleoli [5, 6]. The term rhabdoid is applied to this tumor due to the similarity of its cells to rhabdomyoblasts that have not fully differentiated into skeletal muscle cells. RM has a malignant nature with a high proliferative capability and poor prognosis and was first defined in 2000 as a new subtype of meningiomas with an aggressive nature and extreme rarity [7, 8]. In most cases (nearly 80%), surgery and complete excision of meningioma is the treatment of choice [9]; however, when it is not possible to completely remove the tumor or in patients with recurrent malignancy, radiotherapy, along with surgery is also used [10]. However, it should be investigated whether late surgery of RM tumor causes the death of patients.
2. Case Presentation
A 67-year-old male who lived in Kermanshah City, Iran, presented to neurosurgery with a chief complaint of a large, slow-growing scalp mass and neck pain. Past medical history included heart failure, hypertension, and hyperlipidemia, managed with medications like β-blockers, diuretics and statins. Meanwhile, the patient denied headaches, blurred vision, diplopia, dizziness, or seizures. Despite the large size of the mass, neurological examination revealed normal sensory and motor function. However, the weight of the mass significantly impacted his daily activities and head balance, requiring constant hand support. This functional limitation and resulting psychological distress led to suicidal ideation.
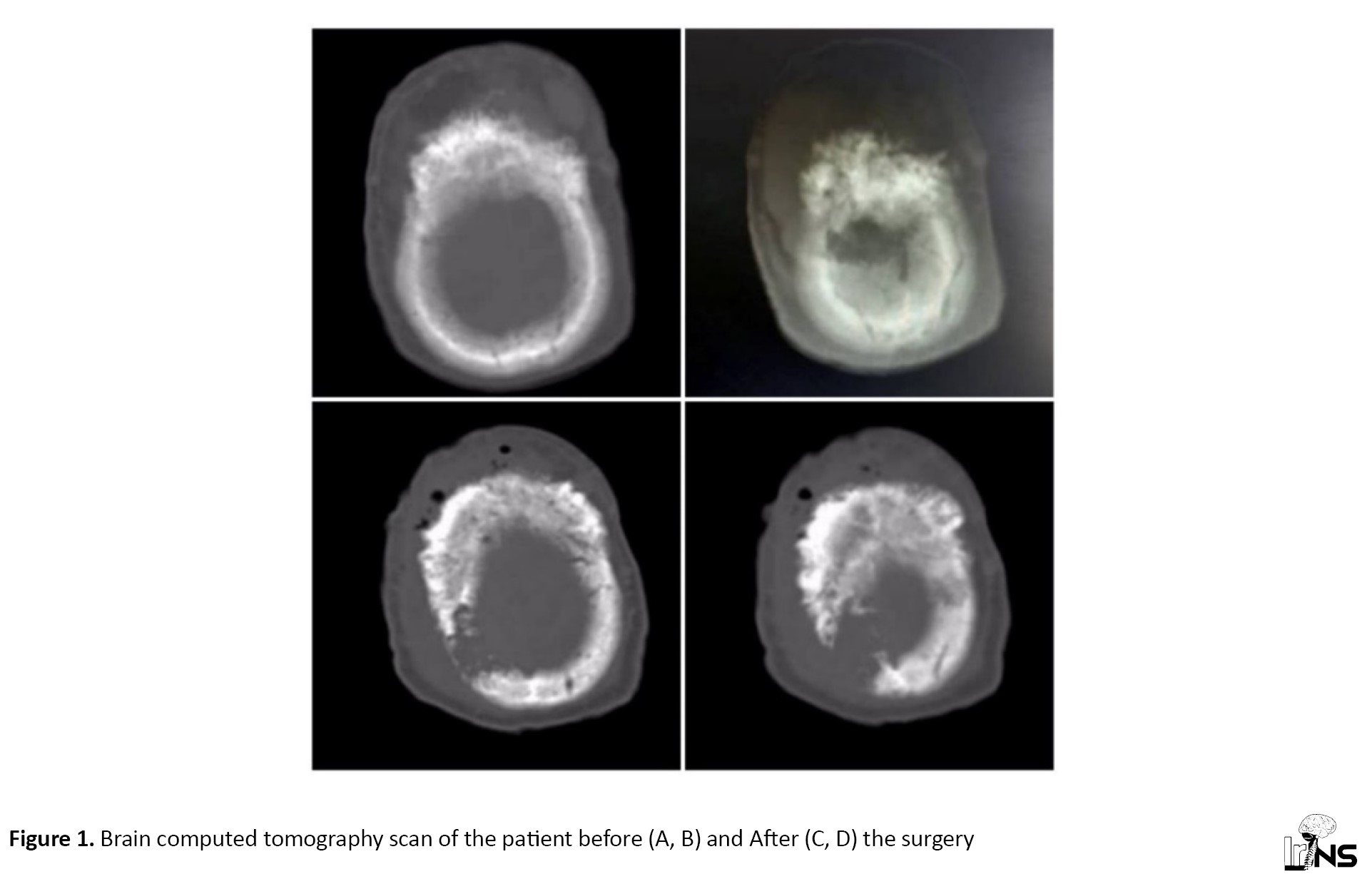
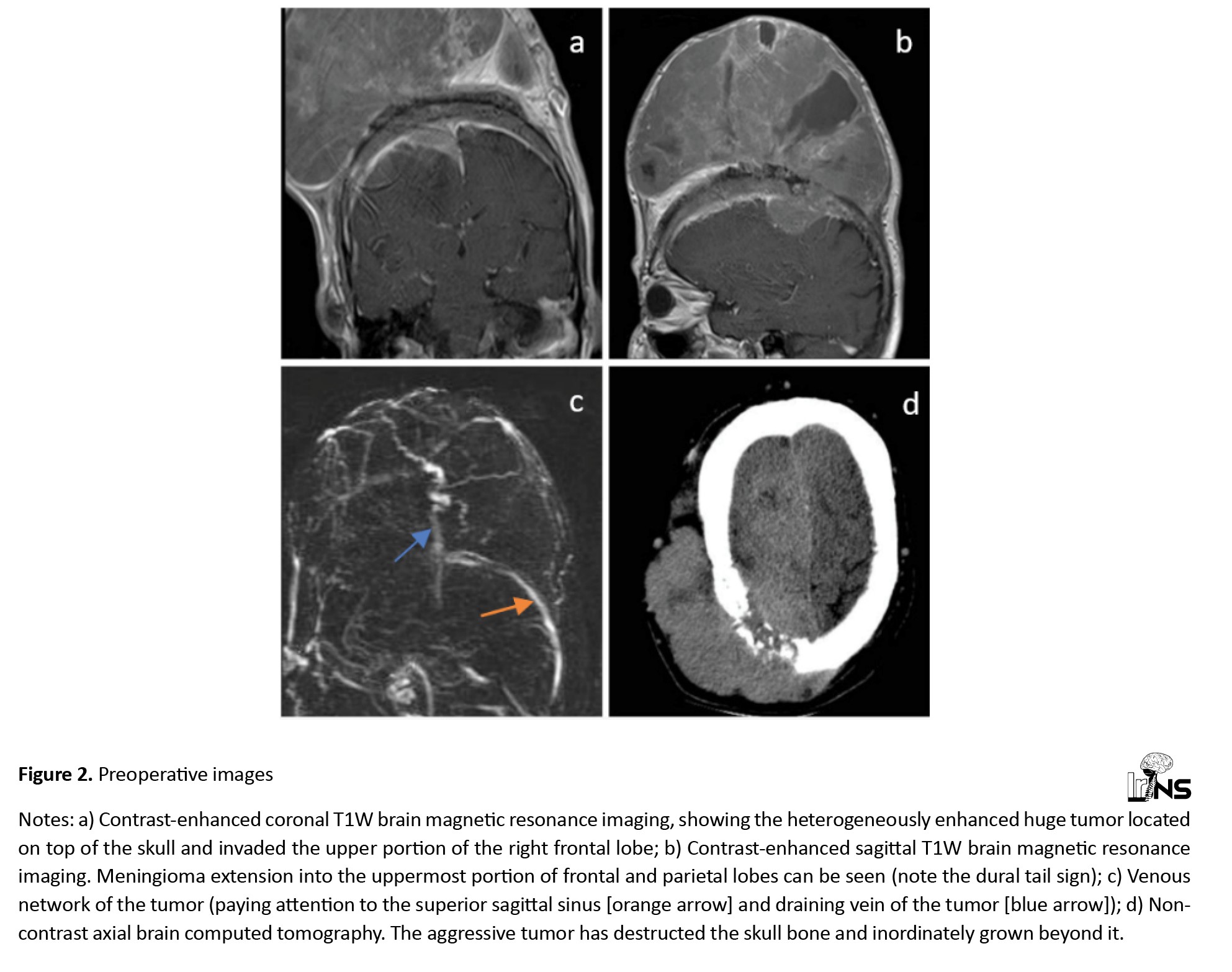
Magnetic resonance imaging of the brain revealed a large mass with a smooth border and an unusual, irregular shape on the top of the skull in the frontal and parietal regions. This mass had two connected parts as follows: An extracranial portion outside the skull and an intracranial portion inside the skull. The extracranial portion is connected through a hole created by erosion of the skull bone. After contrast injection, the extracranial part showed solid areas with signal intensity similar to gray matter and cystic areas with varied enhancement. However, the intracranial portion showed uniform enhancement, suggesting possible involvement of the dura mater in the right frontal and parietal lobe (Figures 1 and 2).
Meningioma is one of the most common benign tumors of the central nervous system (CNS), which usually arises from the meningeal layers of the brain or spinal cord [1]. These tumors are divided into three grades. About 80% of meningiomas are considered benign or grade I, while 17% to 18% are grade II and approximately 1.7% of meningiomas turn into grade III tumors [2-4]. According to the 2021 classification of the World Health Organization (WHO) for CNS tumors, rhabdoid meningioma (RM) is a subtype of meningiomas and a grade III tumor that usually consists of rhabdoid, i.e. round to ovoid cells with eccentric nuclei, paranuclear eosinophilic inclusions, and prominent nucleoli [5, 6]. The term rhabdoid is applied to this tumor due to the similarity of its cells to rhabdomyoblasts that have not fully differentiated into skeletal muscle cells. RM has a malignant nature with a high proliferative capability and poor prognosis and was first defined in 2000 as a new subtype of meningiomas with an aggressive nature and extreme rarity [7, 8]. In most cases (nearly 80%), surgery and complete excision of meningioma is the treatment of choice [9]; however, when it is not possible to completely remove the tumor or in patients with recurrent malignancy, radiotherapy, along with surgery is also used [10]. However, it should be investigated whether late surgery of RM tumor causes the death of patients.
2. Case Presentation
A 67-year-old male who lived in Kermanshah City, Iran, presented to neurosurgery with a chief complaint of a large, slow-growing scalp mass and neck pain. Past medical history included heart failure, hypertension, and hyperlipidemia, managed with medications like β-blockers, diuretics and statins. Meanwhile, the patient denied headaches, blurred vision, diplopia, dizziness, or seizures. Despite the large size of the mass, neurological examination revealed normal sensory and motor function. However, the weight of the mass significantly impacted his daily activities and head balance, requiring constant hand support. This functional limitation and resulting psychological distress led to suicidal ideation.
Magnetic resonance imaging of the brain revealed a large mass with a smooth border and an unusual, irregular shape on the top of the skull in the frontal and parietal regions. This mass had two connected parts as follows: An extracranial portion outside the skull and an intracranial portion inside the skull. The extracranial portion is connected through a hole created by erosion of the skull bone. After contrast injection, the extracranial part showed solid areas with signal intensity similar to gray matter and cystic areas with varied enhancement. However, the intracranial portion showed uniform enhancement, suggesting possible involvement of the dura mater in the right frontal and parietal lobe (Figures 1 and 2).
Following initial medical optimization and a high-risk heart consultation, the patient underwent surgery. Under general anesthesia, the patient’s head was secured with a band and a bi-coronal incision with a T-shaped extension parallel to the midline was made. A large, firm, yellowish-brown mass measuring approximately 20×15×10 cm was revealed. Due to the extensive surgery and the patient’s cardiac risk, a piecemeal resection approach was used to remove the total extracranial portion, which comprised about 85% of the entire tumor. Hemostasis was achieved, and a drainage tube was placed before closure. A tissue sample was sent for pathology to determine the tumor type (Figures 3 and 4).
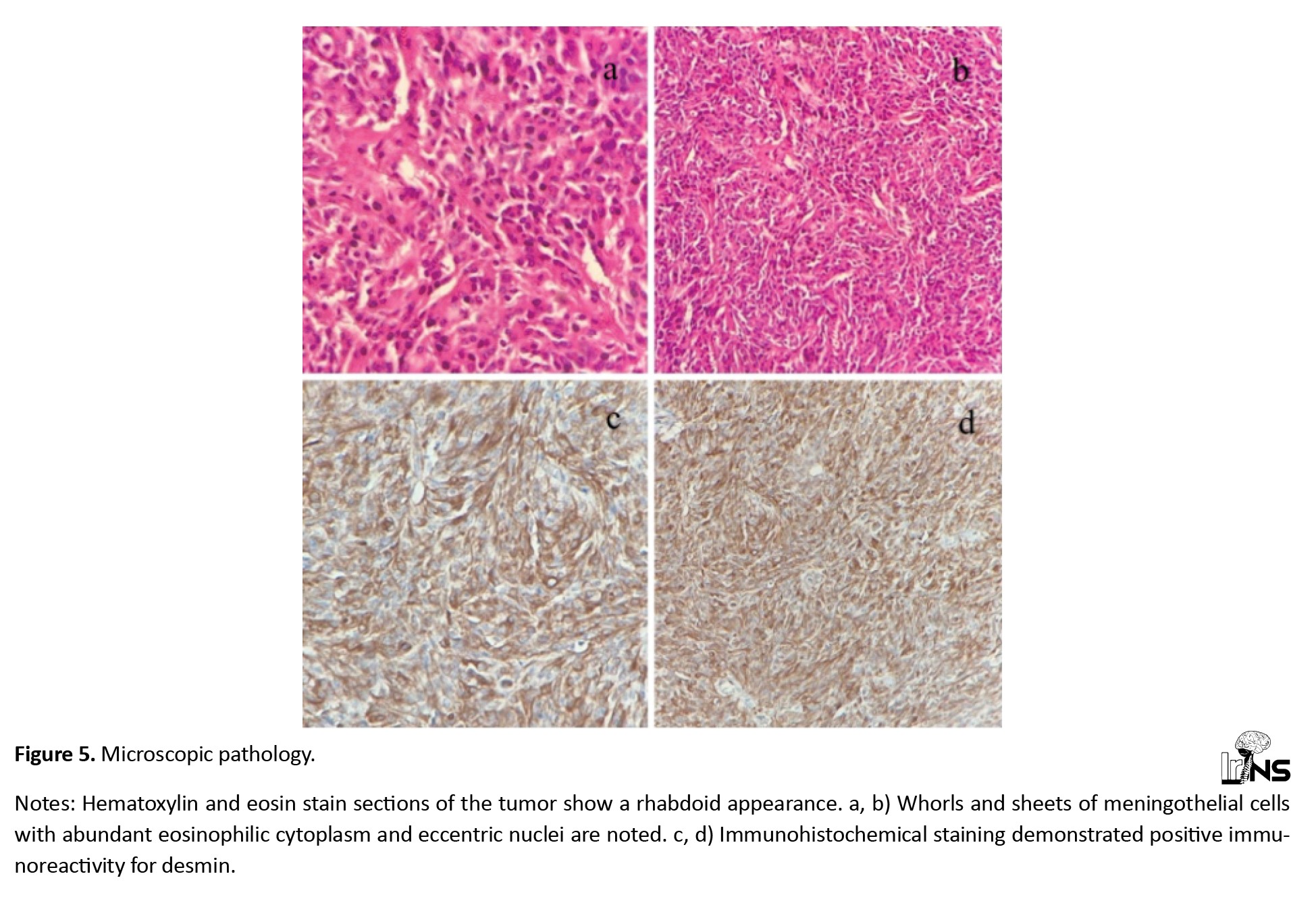
Microscopic examination revealed sheets and whorls of meningothelial rhabdoid cells, round to oval cells with abundant pink cytoplasm and off-center nuclei. Some cells contained pink inclusions within their cytoplasm, and areas of cell death were also evident (Figure 5).
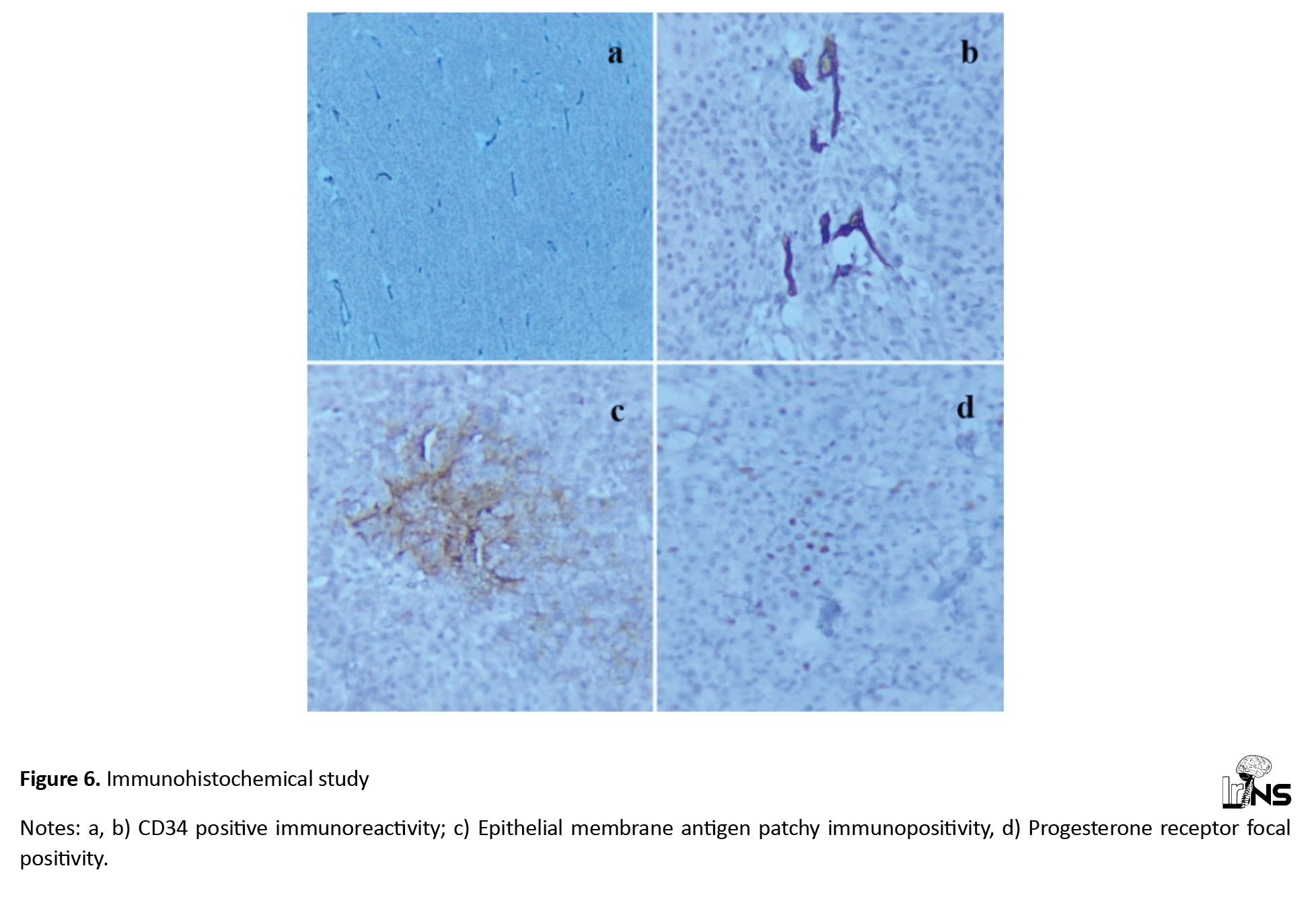
Immunohistochemical staining showed positive reactivity for desmin and focal positivity for epithelial membrane antigen, vimentin, CD34 and progesterone receptor, while negative for neuroendocrine and melanocytic markers (Figure 6).
Based on these findings, the final diagnosis of grade III WHO RM was established. The decision regarding the remaining intracranial portion was deferred until pathology results were available. Despite neurosurgeons’ recommendations for further evaluation with magnetic resonance imaging and magnetic resonance venography scans, followed by surgery to address the remaining intracranial tumor, the patient declined the second surgery. He recovered well initially and returned home. However, three months later, he was hospitalized for deep vein thrombosis in his left leg and passed away. Follow-up was carried out from the time of surgery (2023 December) until death (2024 March).
3. Discussion
RM is considered a subset of grade III tumors that are usually composed of rhabdoid cells and have a malignant nature with high proliferation [5, 6]. The extracranial type, with a prevalence of 2%, is one of the rarest subtypes of meningiomas, which are either caused by primary intracranial meningioma invasion of the extracranial area, or as a true primary extracranial tumor due to the growth of ectopic arachnoid cells [4].
In a review study, Garrido Ruiz et al. (2023) examined 233 cases of RM, as well as 23 patients studied in their laboratory. Of these, in different studies, 204 cases (75%) occurred in adults and 29 cases (10%) occurred in children. The median ages of adults were 52 years (the range of 20-85 years). Also, among the 23 cases in their laboratory, 10 men and 5 women were reported with a median age of 65 years (ranged 34-79 years) [11]. Our patient was a 67-year-old male, which matched the median age of the mentioned studies.
Inami et al. (2023) reported a case with RM, whose tumor measured 8.2×6.5×7 cm and was located in the region of the right frontal convexity [12]. Of the 11 cases of RM reported in the study of Birua et al. (2021), four lesions were located at the base of the skull, three in the convexity, and four in the parasagittal region [1]. The location of our reported tumor was mainly the right frontal region with a slight extension to the left frontal lobe, which had penetrated the extracranial region by destroying an area of the skull and growing extraordinarily on top of the calvarium. Also, the dimensions of the tumor were approximately 20×15×10 cm. In the study by Zeng et al. magnetic resonance imaging of the patient’s head showed a space-occupying lesion in his left frontotemporal lobe with approximate dimensions of 4.4×4.6×4.9 cm [13]. The tumor reported in our study was exceptionally very larger than the tumors reported in previous articles, which could indicate the aggressive nature and extensive growth capability of this RM.
Our patient had presented with neck pain which was due to the heavy weight of the tumor. In different studies, the patient’s symptoms and signs have varied depending on the location and size of the tumor and its mass effect on the adjacent normal structures, for example, in the study by Zeng et al. the RM lesion was located in the left frontotemporal region and the patient had symptoms of dizziness, headache, nausea, vomiting, and gradual blurring of vision and diplopia [13].
Marked peritumoral edema, cystic components, and bony involvement have been documented ::as char::acteristic neuroimaging findings of RMs. In Inami et al.’s study, the patient’s tumor had mild peritumoral edema with cysts and no dural tail. In addition, the patient presented with focal erosion of the skull instead of hyperostosis [12]. In a study carried out by Kim et al. on 15 patients with RM, tumors had characteristics of prominent peritumoral edema, cystic components, and bone involvement [14]. In the brain magnetic resonance imaging examination of our patient, no peritumoral edema was observed. However, cystic components and skull bone erosion were among the significant imaging features of this case.
This case report had several characteristics that can convey important findings to researchers in this field. Among the most important points of this case report, we mention the high growth rate of the tumor and the absence of symptoms of the disease. Based on the results of this study and similar studies, if the tumor is outside the skull, it will not have specific clinical symptoms such as headache, dizziness, blurred vision and double nose, and the most important clinical symptom is neck pain due to the heaviness of the head. Several reasons have been mentioned for the delay in the surgery, the most important of which are heart disease and anesthesia problems during the surgery, noting that many specialists are not willing to accept the risk of the surgery. Considering the results of the surgery and the absence of special problems during the surgery, it is strongly recommended that the operation of such patients should not be delayed in any way. Due to the lack of treatment of the patient, the results showed that if the RM disease is not treated, the growth rate is high, which will increase to 10 cm3 in approximately one year.
4. Conclusion
The tumor in the case study was one of the rare meningiomas that had a high growth rate. The surgery time of the patient was delayed for various reasons and the appearance of the patient’s head was getting worse gradually, so when the tumor is growing fast, surgery should be done faster. Although tumor location has a pivotal role in determining treatment strategy. Additionally, while various clinical symptoms such as headache, dizziness and blurred vision have been identified as symptoms of this disease; however, in this case, the tumor can manifest without any evident clinical symptoms.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Kermanshah University of Medical Sciences (Code: IR.KUMS.REC.1403.104).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contribution
Study design: Iran Chanideh, Saeed Gharooee Ahangar, Seyed Hamid Madani; Conceptualization: Iran Chanideh, Saeed Gharooee Ahangar, Sasan Alaghemand, Ali Shoghi; Writing–original draft: Masoud Ghadiri and Tahereh Mohammadi Majd; Critically revising: Iran Chanideh; Review, editing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors express their gratitude to the Radiology Department, school of medicine, Kermanshah University of Medical Sciences and Medical Records Department of Imam Reza Hospital in Kermanshah City, Iran, for their invaluable cooperation and assistance during the entire study period.
3. Discussion
RM is considered a subset of grade III tumors that are usually composed of rhabdoid cells and have a malignant nature with high proliferation [5, 6]. The extracranial type, with a prevalence of 2%, is one of the rarest subtypes of meningiomas, which are either caused by primary intracranial meningioma invasion of the extracranial area, or as a true primary extracranial tumor due to the growth of ectopic arachnoid cells [4].
In a review study, Garrido Ruiz et al. (2023) examined 233 cases of RM, as well as 23 patients studied in their laboratory. Of these, in different studies, 204 cases (75%) occurred in adults and 29 cases (10%) occurred in children. The median ages of adults were 52 years (the range of 20-85 years). Also, among the 23 cases in their laboratory, 10 men and 5 women were reported with a median age of 65 years (ranged 34-79 years) [11]. Our patient was a 67-year-old male, which matched the median age of the mentioned studies.
Inami et al. (2023) reported a case with RM, whose tumor measured 8.2×6.5×7 cm and was located in the region of the right frontal convexity [12]. Of the 11 cases of RM reported in the study of Birua et al. (2021), four lesions were located at the base of the skull, three in the convexity, and four in the parasagittal region [1]. The location of our reported tumor was mainly the right frontal region with a slight extension to the left frontal lobe, which had penetrated the extracranial region by destroying an area of the skull and growing extraordinarily on top of the calvarium. Also, the dimensions of the tumor were approximately 20×15×10 cm. In the study by Zeng et al. magnetic resonance imaging of the patient’s head showed a space-occupying lesion in his left frontotemporal lobe with approximate dimensions of 4.4×4.6×4.9 cm [13]. The tumor reported in our study was exceptionally very larger than the tumors reported in previous articles, which could indicate the aggressive nature and extensive growth capability of this RM.
Our patient had presented with neck pain which was due to the heavy weight of the tumor. In different studies, the patient’s symptoms and signs have varied depending on the location and size of the tumor and its mass effect on the adjacent normal structures, for example, in the study by Zeng et al. the RM lesion was located in the left frontotemporal region and the patient had symptoms of dizziness, headache, nausea, vomiting, and gradual blurring of vision and diplopia [13].
Marked peritumoral edema, cystic components, and bony involvement have been documented ::as char::acteristic neuroimaging findings of RMs. In Inami et al.’s study, the patient’s tumor had mild peritumoral edema with cysts and no dural tail. In addition, the patient presented with focal erosion of the skull instead of hyperostosis [12]. In a study carried out by Kim et al. on 15 patients with RM, tumors had characteristics of prominent peritumoral edema, cystic components, and bone involvement [14]. In the brain magnetic resonance imaging examination of our patient, no peritumoral edema was observed. However, cystic components and skull bone erosion were among the significant imaging features of this case.
This case report had several characteristics that can convey important findings to researchers in this field. Among the most important points of this case report, we mention the high growth rate of the tumor and the absence of symptoms of the disease. Based on the results of this study and similar studies, if the tumor is outside the skull, it will not have specific clinical symptoms such as headache, dizziness, blurred vision and double nose, and the most important clinical symptom is neck pain due to the heaviness of the head. Several reasons have been mentioned for the delay in the surgery, the most important of which are heart disease and anesthesia problems during the surgery, noting that many specialists are not willing to accept the risk of the surgery. Considering the results of the surgery and the absence of special problems during the surgery, it is strongly recommended that the operation of such patients should not be delayed in any way. Due to the lack of treatment of the patient, the results showed that if the RM disease is not treated, the growth rate is high, which will increase to 10 cm3 in approximately one year.
4. Conclusion
The tumor in the case study was one of the rare meningiomas that had a high growth rate. The surgery time of the patient was delayed for various reasons and the appearance of the patient’s head was getting worse gradually, so when the tumor is growing fast, surgery should be done faster. Although tumor location has a pivotal role in determining treatment strategy. Additionally, while various clinical symptoms such as headache, dizziness and blurred vision have been identified as symptoms of this disease; however, in this case, the tumor can manifest without any evident clinical symptoms.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Kermanshah University of Medical Sciences (Code: IR.KUMS.REC.1403.104).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contribution
Study design: Iran Chanideh, Saeed Gharooee Ahangar, Seyed Hamid Madani; Conceptualization: Iran Chanideh, Saeed Gharooee Ahangar, Sasan Alaghemand, Ali Shoghi; Writing–original draft: Masoud Ghadiri and Tahereh Mohammadi Majd; Critically revising: Iran Chanideh; Review, editing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors express their gratitude to the Radiology Department, school of medicine, Kermanshah University of Medical Sciences and Medical Records Department of Imam Reza Hospital in Kermanshah City, Iran, for their invaluable cooperation and assistance during the entire study period.
References
- Birua GJS, Sadashiva N, Konar S, Rao S, Shukla D, Krishna U, et al. Rhabdoid meningiomas: Clinicopathological analysis of a rare variant of meningioma. Clinical Neurology and Neurosurgery. 2021; 207:106778. [DOI:10.1016/j.clineuro.2021.106778] [PMID]
- Buerki RA, Horbinski CM, Kruser T, Horowitz PM, James CD, Lukas RV. An overview of meningiomas. Future oncology. 2018; 14(21):2161-77. [DOI:10.2217/fon-2018-0006] [PMID] [PMCID]
- Ostrom QT, Cioffi G, Gittleman H, Patil N, Waite K, Kruchko C, et al. CBTRUS statistical report: Primary brain and other central nervous system tumors diagnosed in the United States in 2012-2016. Neuro-oncology. 2019; 21(Suppl 5):v1-v100. [DOI:10.1093/neuonc/noz150] [PMID] [PMCID]
- Rege ICC, Garcia RR, Mendonça EF. Primary extracranial meningioma: A rare location. Head and Neck Pathology. 2017; 11(4):561-6. [DOI:10.1007/s12105-017-0813-2] [PMID] [PMCID]
- Vaubel RA, Chen SG, Raleigh DR, Link MJ, Chicoine MR, Barani I, et al. Meningiomas with rhabdoid features lacking other histologic features of malignancy: A study of 44 cases and review of the literature. Journal of Neuropathology and Experimental Neurology. 2016; 75(1):44-52. [DOI:10.1093/jnen/nlv006] [PMID] [PMCID]
- Wu YT, Ho JT, Lin YJ, Lin JW. Rhabdoid papillary meningioma: A clinicopathologic case series study. Neuropathology. 2011; 31(6):599-605. [DOI:10.1111/j.1440-1789.2011.01201.x] [PMID]
- Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathologica. 2007; 114(2):97-109. [DOI:10.1007/s00401-007-0278-6] [PMID] [PMCID]
- Mondal S, Pradhan R, Pal S, Chatterjee S, Bandyapadhyay A, Bhattacharyya D. Rhabdoid meningioma of brain-A rare aggressive tumor. Indian Journal of Medical and Paediatric Oncology. 2017; 38(2):218-9. [PMID] [PMCID]
- Marosi C, Hassler M, Roessler K, Reni M, Sant M, Mazza E, et al. Meningioma. Critical Reviews in Oncology/Hematology. 2008; 67(2):153-71. [DOI:10.1016/j.critrevonc.2008.01.010] [PMID]
- Goldbrunner R, Minniti G, Preusser M, Jenkinson MD, Sallabanda K, Houdart E, et al. EANO guidelines for the diagnosis and treatment of meningiomas. The Lancet Oncology. 2016; 17(9):e383-91. [DOI:10.1016/S1470-2045(16)30321-7] [PMID]
- Garrido Ruiz PA, González-Tablas M, Pasco Peña A, Zelaya Huerta MV, Ortiz J, Otero Á, et al. Clinical, histopathologic and genetic features of rhabdoid meningiomas. International Journal of Molecular Sciences. 2023; 24(2):1116. [DOI:10.3390/ijms24021116] [PMID] [PMCID]
- Inami K, Tsutsumi S, Hashizume A, Yoshida K, Sugiyama N, Ueno H, et al. Large rhabdoid meningioma presenting prominent hyperintensity in the optic nerve: An indicator of visual disturbance on constructive interference steady-state sequence? Surgical Neurology International. 2023; 14:248. [DOI:10.25259/SNI_364_2023] [PMID] [PMCID]
- Zeng Y, Zhang J, Jian W, Zhang Y, Yang Y, Li R, et al. Rhabdoid meningioma with a history of Budd-Chiari syndrome: A case report and review of the literature. Frontiers in Oncology. 2023; 13:1209244. [DOI:10.3389/fonc.2023.1209244] [PMID] [PMCID]
- Kim EY, Weon YC, Kim ST, Kim HJ, Byun HS, Lee JI, et al. Rhabdoid meningioma: Clinical features and MR imaging findings in 15 patients. American Journal of Neuroradiology. 2007; 28(8):1462-5. [DOI:10.3174/ajnr.A0601] [PMID] [PMCID]
Type of Study: Case report |
Subject:
Brain Tumors
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |