Sun, Feb 22, 2026
Volume 10 - Continuous Publishing
Iran J Neurosurg 2024, 10 - Continuous Publishing: 168-172 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Doostabadi H, Talimkhani M M, Arjipour M. A Dangerous Acute Presentation of Hemorrhagic Meningioma. Iran J Neurosurg 2024; 10 : 19
URL: http://irjns.org/article-1-427-en.html
URL: http://irjns.org/article-1-427-en.html
1- Department of Neurosurgery, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran.
2- Department of Neurosurgery, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran
3- Department of Neurosurgery, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran ,mahdiarjipour@yahoo.com
2- Department of Neurosurgery, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran
3- Department of Neurosurgery, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran ,
Full Text [PDF 1436 kb]
(658 Downloads)
| Abstract (HTML) (2696 Views)
Full Text: (606 Views)
1. Background and Importance
While most meningiomas are diagnosed accidentally, they usually cause focal headaches, convulsions, dizziness, or neurological deficits in symptomatic patients. Various clinical characteristics may occur depending on their size, location, and invasion.
Most of these tumors are benign and therefore the risk of bleeding is low. The most common form of hemorrhaging due to meningioma is subdural hematoma (SDH) [1].
Although malignant tumors, such as glioma are associated with spontaneous bleeding, this phenomenon is rare in benign tumors, such as meningioma [1]. The mechanism of hemorrhage in these tumors is not yet fully understood. Hemorrhagic brain tumors, which can cause intracranial hemorrhages, are responsible for 1%-11% of intracranial hemorrhages. Brain tumor-related subarachnoid hemorrhage (SAH) accounts for 0.4% of all SAH cases. Moreover, 1.7% to 10% of brain tumors cause an intracerebral hemorrhage. Intertumoral hemorrhage typically occurs in 11% of head tumors, and its occurrence in glioblastoma multiforme, choriocarcinomas, oligodendrogliomas, pituitary adenomas, choroid plexus papilloma, and meningioma is also prevalent [2].
In this article, we present a case in which meningioma is accompanied by subdural and IPH hematomas.
2. Case Presentation
A 69-year-old woman with a history of hypertension was admitted to the emergency department with a severe and sudden headache complaint.
On computed tomography (CT) scan, a heterogeneous hyperdense area was observed in the right frontoparietal area. The lesion has two components, an iso-intense portion in the anterolateral (tumor) and a hyperdense portion in the posteromedial and compression over brain tissue and there was a mild midline shift.
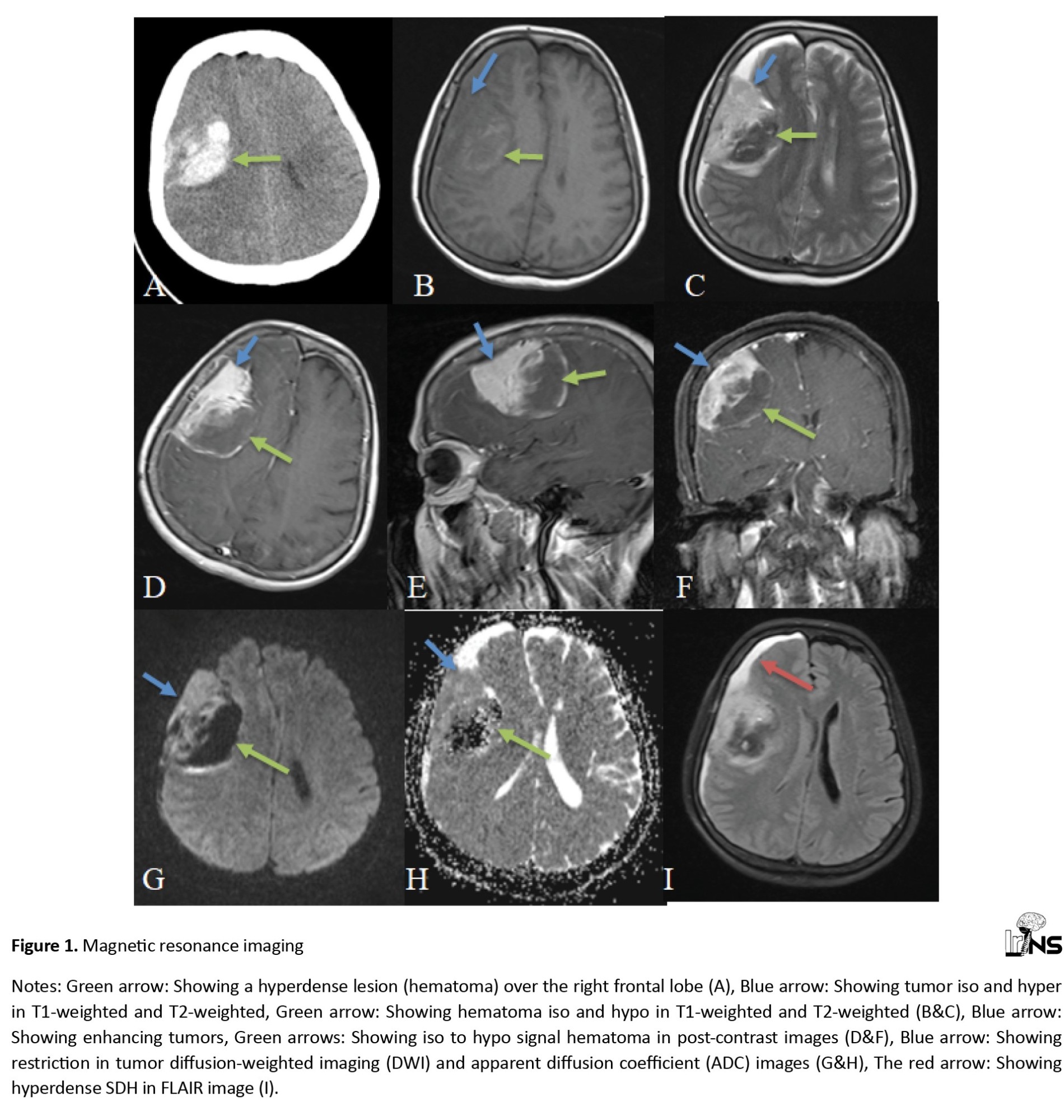
In magnetic resonance imaging (MRI), it was found that the lesion was heterogeneous and anterolateral portion (tumor) was hypointense on T1-weighted images and hyperintense on T2-weighted images and the posteromedial portion (hematoma) was iso-hypo on T1-weighted and hypo on T2-weighted images. At post-contrast images, the anterolateral portion (tumor) displayed homogenous dense enhancement, and no enhancement was observed at the posteromedial portion (hematoma). Also, crescent shape extension of hematoma was observed in subdural space (free component) which was iso on T1-weighted and hyper on T2, and no enhancement was observed (Figure 1). The mentioned results were supportive of peri-tumoral hematoma.
Operation
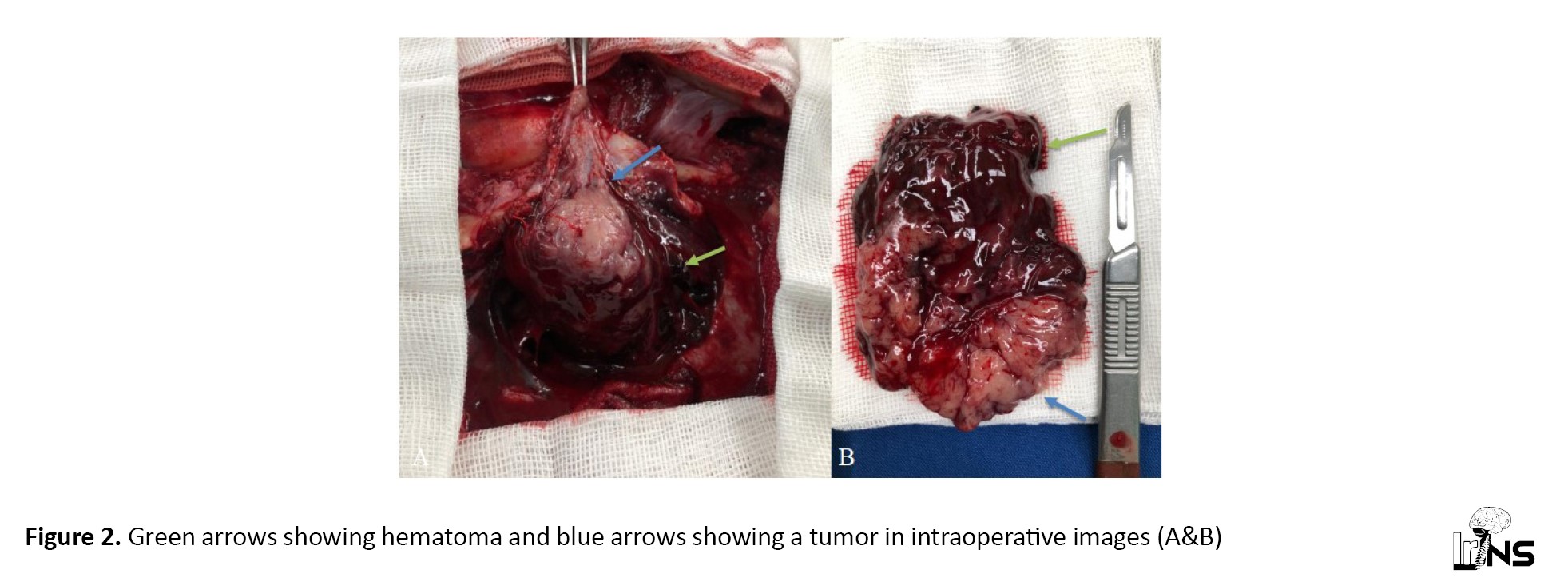
The patient underwent an emergent frontoparietal craniotomy. After the dura opening, a SDH was observed and evacuated, and then a mass with a dura base in favor of meningioma was identified, along with IPH hematoma in posteromedial to the tumor. The tumor was resected and the hematoma was evacuated and washed. Ultimately, the duraplasty was performed and a drain was placed at the end (Figure 2).
Postoperative outcome
The patient was admitted to the intensive care unit (ICU). Twenty-four hours later, a post-operative brain CT scan was performed for the patient. No trace of hematoma or tumor tissue was observed on the brain CT therefore we started the anticoagulants. On the second day, the patient was admitted to the ward and got out of bed. The patient was discharged on the third day in good condition. Control MRI showed complete removal of the tumor (Figure 3).
Pathology
Macroscopy
The received sample of the first container (brain mass) contains numerous pieces of cream-brown tissue with a soft to elastic consistency, dimensions of (6×6×2) cm, and a nodular growth pattern. On the surface of the cut, the cream is brown and non-uniform. It contains numerous blood clots attached to it. The received sample of the second container contains a piece of brown cream texture with dimensions of 2×1×0.5.
Microscopy
Sections of neoplastic tissue with meningothelial appearance can be observed under the microscope. The neoplastic cells are characterized by round to oval nuclei with vesicular chromatin patterns, sometimes small eosinophilic nuclei are found in dense sheets of cells with a syncytial appearance. A collagenous field has been established. Vascular field of neoplastic tissue and few cystic spaces along with edema vascular congestion and bleeding are evident. No evidence of tissue necrosis increased mitotic activity and patternless and heterogeneous differentiation is observed. Meningioma meningotheliomatous type grade I with intertumoral hemorrhage.
3. Discussion
Primary metastatic and malignant tumors are the most prone to bleeding due to their histological characteristics and association with coagulopathy. However, sometimes benign tumors, such as meningioma and schwannoma can also lead to bleeding. Convexity and intraventricular meningiomas and, fibroblastic or angioblastic subtypes are more likely to bleed. Bleeding raises the mortality rate of benign meningioma. As a result, early diagnosis and surgical treatment by hematoma evacuation with underlying tumor resection are required as we did in our case [1].
Hemorrhage due to meningioma is relatively rare, with an incidence of 1.3% to 2.4%, and 120 cases reported in the literature between 1980-2021, mostly SDH (41%), intraparenchymal (IPH) (37%), SAH (18%), intraventricular hemorrhage (IVH) (4%) [3]. The risk of rebleeding in patients who were not operated on for resection and hematoma evacuation was 74% with a median time of 120 days, thus the rebleeding risk is high and it could be dangerous, consequently, prompt surgery is justified. SAH and IVH types and hindbrain location had an association with early rebleeding. Therefore, SDH and IPH in meningioma are rare (reported cases were 49 and 44 respectively) [4-6] and their association as in our case is extremely rare. Ventricular and hindbrain location and IPH can worsen prognosis and outcomes [3].
The most reported histologic subtypes of meningioma are meningothelial and angiomatosis [7]. Hemorrhage in the meningothelial subtype is probably related to the presence of vasoactive substances released by the tumor, which can induce vasodilation and bleeding [1].
In this case, SDH and IPH were both associated with meningioma, which is extremely rare. It may have occurred accidentally or as a result of minor head trauma.
Most patients diagnosed with meningioma are covered without any complication but about 7.5% of the patients died despite proper treatment and also 10% were left with neurological sequelae [1].
4. Conclusion
Each acute SDH and IPH is a rare presentation of meningiomas and their association as in this case is extremely rare. Due to the high risk of rebleeding in similar reported cases, prompt surgical treatment is recommended. Precise pathogenesis understanding needs a more intentional evaluation of these cases.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from the patient.
Funding
The study was funded by Hamadan University of Medical Sciences, Hamadan, Iran.
Authors' contributions
Conceptualization and study design: Mahdi Arjipour; Data collection: Mohammad Mahdi Talimkhani; Data analysis and interpretation: Hamidreza Doostabadi; Writing the original draft: Mahdi Arjipour and Hamidreza Doostabadi; Review and editing: Mahdi Arjipour.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors appreciate the financial assistance provided by the departments of Neurosurgery at Hamadan University of Medical Sciences, Hamadan, Iran.
References
While most meningiomas are diagnosed accidentally, they usually cause focal headaches, convulsions, dizziness, or neurological deficits in symptomatic patients. Various clinical characteristics may occur depending on their size, location, and invasion.
Most of these tumors are benign and therefore the risk of bleeding is low. The most common form of hemorrhaging due to meningioma is subdural hematoma (SDH) [1].
Although malignant tumors, such as glioma are associated with spontaneous bleeding, this phenomenon is rare in benign tumors, such as meningioma [1]. The mechanism of hemorrhage in these tumors is not yet fully understood. Hemorrhagic brain tumors, which can cause intracranial hemorrhages, are responsible for 1%-11% of intracranial hemorrhages. Brain tumor-related subarachnoid hemorrhage (SAH) accounts for 0.4% of all SAH cases. Moreover, 1.7% to 10% of brain tumors cause an intracerebral hemorrhage. Intertumoral hemorrhage typically occurs in 11% of head tumors, and its occurrence in glioblastoma multiforme, choriocarcinomas, oligodendrogliomas, pituitary adenomas, choroid plexus papilloma, and meningioma is also prevalent [2].
In this article, we present a case in which meningioma is accompanied by subdural and IPH hematomas.
2. Case Presentation
A 69-year-old woman with a history of hypertension was admitted to the emergency department with a severe and sudden headache complaint.
On computed tomography (CT) scan, a heterogeneous hyperdense area was observed in the right frontoparietal area. The lesion has two components, an iso-intense portion in the anterolateral (tumor) and a hyperdense portion in the posteromedial and compression over brain tissue and there was a mild midline shift.
In magnetic resonance imaging (MRI), it was found that the lesion was heterogeneous and anterolateral portion (tumor) was hypointense on T1-weighted images and hyperintense on T2-weighted images and the posteromedial portion (hematoma) was iso-hypo on T1-weighted and hypo on T2-weighted images. At post-contrast images, the anterolateral portion (tumor) displayed homogenous dense enhancement, and no enhancement was observed at the posteromedial portion (hematoma). Also, crescent shape extension of hematoma was observed in subdural space (free component) which was iso on T1-weighted and hyper on T2, and no enhancement was observed (Figure 1). The mentioned results were supportive of peri-tumoral hematoma.
Operation
The patient underwent an emergent frontoparietal craniotomy. After the dura opening, a SDH was observed and evacuated, and then a mass with a dura base in favor of meningioma was identified, along with IPH hematoma in posteromedial to the tumor. The tumor was resected and the hematoma was evacuated and washed. Ultimately, the duraplasty was performed and a drain was placed at the end (Figure 2).
Postoperative outcome
The patient was admitted to the intensive care unit (ICU). Twenty-four hours later, a post-operative brain CT scan was performed for the patient. No trace of hematoma or tumor tissue was observed on the brain CT therefore we started the anticoagulants. On the second day, the patient was admitted to the ward and got out of bed. The patient was discharged on the third day in good condition. Control MRI showed complete removal of the tumor (Figure 3).
Pathology
Macroscopy
The received sample of the first container (brain mass) contains numerous pieces of cream-brown tissue with a soft to elastic consistency, dimensions of (6×6×2) cm, and a nodular growth pattern. On the surface of the cut, the cream is brown and non-uniform. It contains numerous blood clots attached to it. The received sample of the second container contains a piece of brown cream texture with dimensions of 2×1×0.5.
Microscopy
Sections of neoplastic tissue with meningothelial appearance can be observed under the microscope. The neoplastic cells are characterized by round to oval nuclei with vesicular chromatin patterns, sometimes small eosinophilic nuclei are found in dense sheets of cells with a syncytial appearance. A collagenous field has been established. Vascular field of neoplastic tissue and few cystic spaces along with edema vascular congestion and bleeding are evident. No evidence of tissue necrosis increased mitotic activity and patternless and heterogeneous differentiation is observed. Meningioma meningotheliomatous type grade I with intertumoral hemorrhage.
3. Discussion
Primary metastatic and malignant tumors are the most prone to bleeding due to their histological characteristics and association with coagulopathy. However, sometimes benign tumors, such as meningioma and schwannoma can also lead to bleeding. Convexity and intraventricular meningiomas and, fibroblastic or angioblastic subtypes are more likely to bleed. Bleeding raises the mortality rate of benign meningioma. As a result, early diagnosis and surgical treatment by hematoma evacuation with underlying tumor resection are required as we did in our case [1].
Hemorrhage due to meningioma is relatively rare, with an incidence of 1.3% to 2.4%, and 120 cases reported in the literature between 1980-2021, mostly SDH (41%), intraparenchymal (IPH) (37%), SAH (18%), intraventricular hemorrhage (IVH) (4%) [3]. The risk of rebleeding in patients who were not operated on for resection and hematoma evacuation was 74% with a median time of 120 days, thus the rebleeding risk is high and it could be dangerous, consequently, prompt surgery is justified. SAH and IVH types and hindbrain location had an association with early rebleeding. Therefore, SDH and IPH in meningioma are rare (reported cases were 49 and 44 respectively) [4-6] and their association as in our case is extremely rare. Ventricular and hindbrain location and IPH can worsen prognosis and outcomes [3].
The most reported histologic subtypes of meningioma are meningothelial and angiomatosis [7]. Hemorrhage in the meningothelial subtype is probably related to the presence of vasoactive substances released by the tumor, which can induce vasodilation and bleeding [1].
In this case, SDH and IPH were both associated with meningioma, which is extremely rare. It may have occurred accidentally or as a result of minor head trauma.
Most patients diagnosed with meningioma are covered without any complication but about 7.5% of the patients died despite proper treatment and also 10% were left with neurological sequelae [1].
4. Conclusion
Each acute SDH and IPH is a rare presentation of meningiomas and their association as in this case is extremely rare. Due to the high risk of rebleeding in similar reported cases, prompt surgical treatment is recommended. Precise pathogenesis understanding needs a more intentional evaluation of these cases.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from the patient.
Funding
The study was funded by Hamadan University of Medical Sciences, Hamadan, Iran.
Authors' contributions
Conceptualization and study design: Mahdi Arjipour; Data collection: Mohammad Mahdi Talimkhani; Data analysis and interpretation: Hamidreza Doostabadi; Writing the original draft: Mahdi Arjipour and Hamidreza Doostabadi; Review and editing: Mahdi Arjipour.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors appreciate the financial assistance provided by the departments of Neurosurgery at Hamadan University of Medical Sciences, Hamadan, Iran.
References
- Nam JW, Park ES, Park JB, Seo JH, Kim M, Jung NY. Benign meningioma manifesting with acute subdural hematoma and cerebral edema: A case report and review of the literature. Journal of Medical Case Reports. 2021; 15(1):335. [DOI:10.1186/s13256-021-02935-x] [PMID] [PMCID]
- Shahbazi T, Sabahi M, Arjipour M, Adada B, Borghei-Razavi H. Hemorrhagic vestibular schwannoma: Case report and literature review of incidence and risk factors. Cureus. 2020; 12(9):e10183. [DOI:10.7759/cureus.10183] [PMID] [PMCID]
- Leclerc A, Gohel H, Malczuk J, Anzalone L, Emery E, Gaberel T. Systematic review of meningiomas revealed by spontaneous intracranial hemorrhage: Clinicopathological features, outcomes, and rebleeding rate. World Neurosurgery. 2023; 172:e625-39. [DOI:10.1016/j.wneu.2023.01.100] [PMID]
- Moriyama E, Beck H, Takayama K, Okamoto T. Acute traumatic subdural hematoma originating from a convexity meningioma--case report. Neurologia Medico-Chirurgica. 1998; 38(1):20-3. [DOI:10.2176/nmc.38.20] [PMID]
- Shimizu J, Tazawa T, Park-Matsumoto YC, Katano T, Akiba Y, Kuroiwa T. [Meningioma associated with acute subdural hematoma: A case report (Japanese)]. No shinkei geka. Neurological Surgery. 1998; 26(8):743-7. [PMID]
- Mitsuhara T, Ikawa F, Ohbayashi N, Imada Y, Abiko M, Inagawa T. [A case of petrotentorial meningioma presented as an acute subdural hemorrhage (Japanese)]. No Shinkei Geka. Neurological Surgery. 2006; 34(8):827-32. [PMID]
- Kohli CM, Crouch RL. Meningioma with intracerebral hematoma. Neurosurgery. 1984; 15(2):237-40. [DOI:10.1227/00006123-198408000-00014] [PMID]
Type of Study: Case report |
Subject:
Brain Tumors
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |