Sun, Feb 22, 2026
Volume 10 - Continuous Publishing
Iran J Neurosurg 2024, 10 - Continuous Publishing: 149-156 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rahimizadeh A, Williamson W, Malekmohammadi Z, Rahimizadeh S, Amirzadeh M, Homae M et al . Thoracolumbar Extradural Arachnoid Cysts: Report of Two Adult Cases. Iran J Neurosurg 2024; 10 : 17
URL: http://irjns.org/article-1-431-en.html
URL: http://irjns.org/article-1-431-en.html
Abolfazl Rahimizadeh1 

 , Walter Williamson *2
, Walter Williamson *2 

 , Zahed Malekmohammadi3
, Zahed Malekmohammadi3 

 , Shaghayegh Rahimizadeh4
, Shaghayegh Rahimizadeh4 

 , Mahan Amirzadeh3
, Mahan Amirzadeh3 

 , Mohsen Homae3
, Mohsen Homae3 
 , Sayed Ali Ahmadi5
, Sayed Ali Ahmadi5 




 , Walter Williamson *2
, Walter Williamson *2 

 , Zahed Malekmohammadi3
, Zahed Malekmohammadi3 

 , Shaghayegh Rahimizadeh4
, Shaghayegh Rahimizadeh4 

 , Mahan Amirzadeh3
, Mahan Amirzadeh3 

 , Mohsen Homae3
, Mohsen Homae3 
 , Sayed Ali Ahmadi5
, Sayed Ali Ahmadi5 


1- Pars Advanced and Minimally Invasive Medical Manners Research Center, Iran University of Medical Sciences, Tehran, Iran
2- The Office of Clinical Research (OCR), Baylor College of Medicine, Houston, USA. ,walter.williamson@bcm.edu
3- Pars Advanced and Minimally Invasive Medical Manners Research Center, Iran University of Medical Sciences, Tehran, Iran.
4- Anderson Cancer Research Center, University of Texas, USA.
5- Department of Pathology, Sina Hospital, Tehran University of Medical Sciences, Tehran, Iran.
2- The Office of Clinical Research (OCR), Baylor College of Medicine, Houston, USA. ,
3- Pars Advanced and Minimally Invasive Medical Manners Research Center, Iran University of Medical Sciences, Tehran, Iran.
4- Anderson Cancer Research Center, University of Texas, USA.
5- Department of Pathology, Sina Hospital, Tehran University of Medical Sciences, Tehran, Iran.
Keywords: Extradural arachnoid cyst
(EDAC), Laminectomy, Paraparesis, Spinal arachnoid
cyst, Thoracolumbar spine
Full Text [PDF 3263 kb]
(506 Downloads)
| Abstract (HTML) (2845 Views)
Full Text: (1335 Views)
1. Background and Importance
Spinal arachnoid cysts are uncommon, benign lesions that were first described by Spiller in 1903 [1-3]. These cysts are cerebrospinal fluid (CSF)-containing masses lined by the arachnoid mater and account for about 1% of all primary spinal mass lesions. Spinal arachnoid cysts are most often located in extradural and intradural spaces while their intramedullary location is extremely rare [3-9]. Spinal extradural arachnoid cysts (EDAC) are thought to arise from a tiny defect in the dura mater, leading to subsequent herniation of the arachnoid layer into the extradural space and gradual enlargement over time [1-3, 9]. This pathology typically becomes symptomatic in the second to fourth decade of life and its discovery in older adults is much less frequent [1-3, 9]. Before significant enlargement, an EDAC may remain asymptomatic for a long period. The mainstay of surgery for symptomatic EDACs is the closure of the fistula between the subarachnoid space and the cystic outgrowth [1-3, 9]. Herein, we present two new symptomatic adult cases located at the thoracolumbar spinal level.
2. Cases Presentation
Case 1
A 22-year-old woman presented with bilateral lower limb weakness and paresthesia for one year. Her symptoms had noticeably worsened within the last 2 months. Neurological examination demonstrated paraparesis with hyperactive reflexes and a positive Babinski sign. A sensory level with hypesthesia to pinprick and light touch was noted up to the umbilicus.
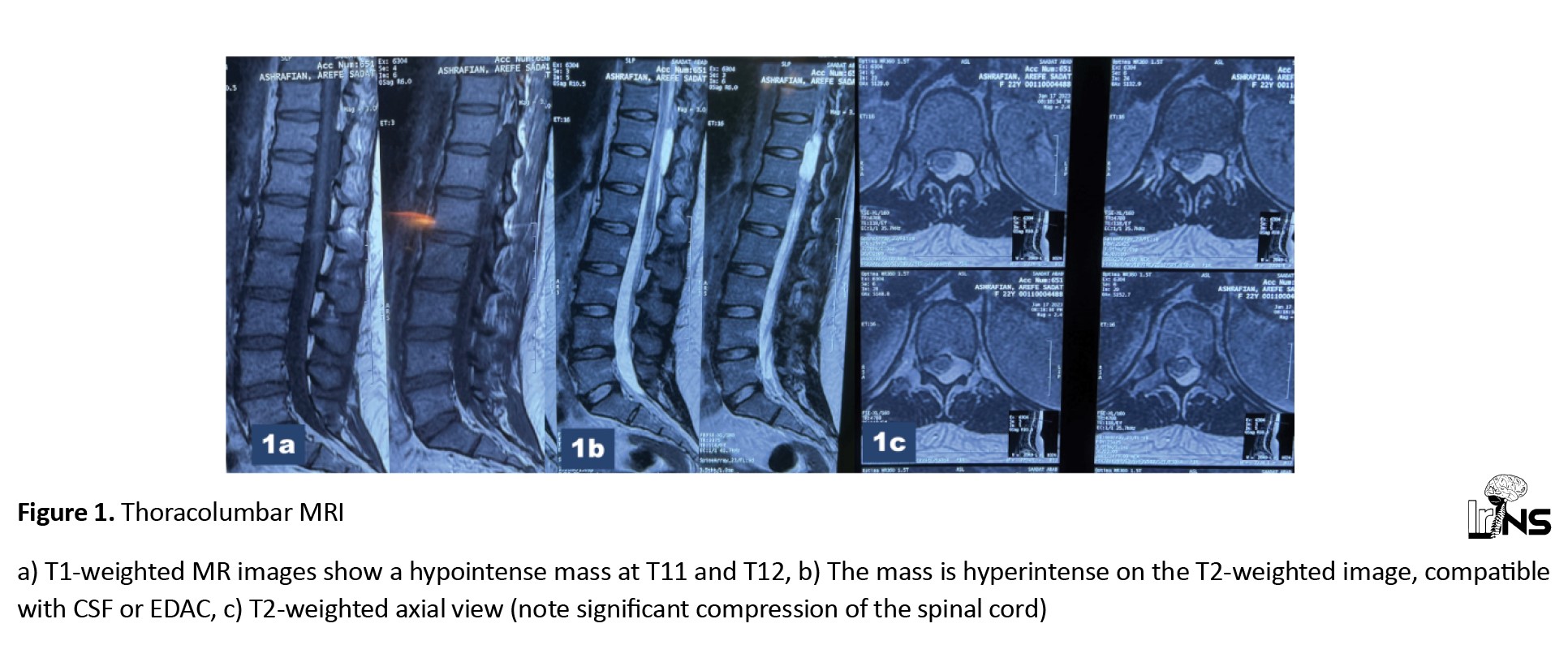
T1-weighted (A) and T2-weighted (B) sagittal MRI of the thoracolumbar spine revealed an extradural cystic lesion extending from the T11 to T12 levels. The cyst was hypointense on T1-weighted MRI and hyperintense on T2-weighted MRI, consistent with an extradural arachnoid cyst. The cyst displayed a compressive effect on the thinned, ventrally compressed cord in the axial views (Figure 1). Following the performance of an appropriate 2-level laminectomy, an extra-dural cystic lesion was exposed. The cyst was meticulously dissected and separated from the dura until a left-sided ostia was discovered and closed utilizing silk sutures.
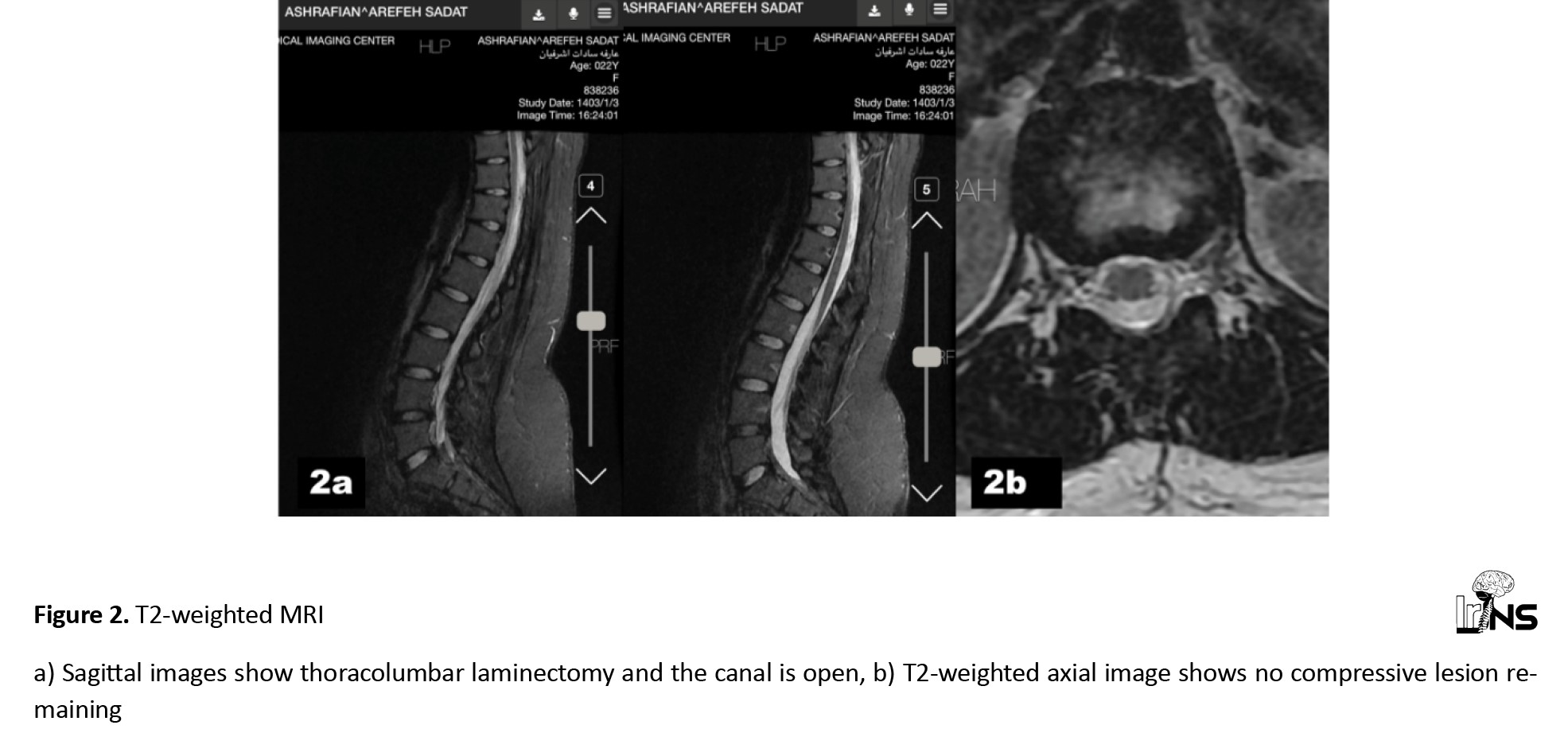
During a three-months follow-up encounter, the patient was able to ambulate with some difficulty, but by the 6-month mark, she could walk normally. In the control thoracolumbar MRI at the one-year follow-up encounter, the arachnoid cyst was no longer detectable (Figure 2).
Case 2
A 38-year-old man was admitted to the hospital for numbness and weakness in the left lower limb for two years, along with similar symptoms in the right lower limb for six months. The lower limb weakness had been exacerbated bilaterally in the last three months. His neurological examination revealed asymmetric paraparesis with hyperactive reflexes and a bilateral Babinski sign.
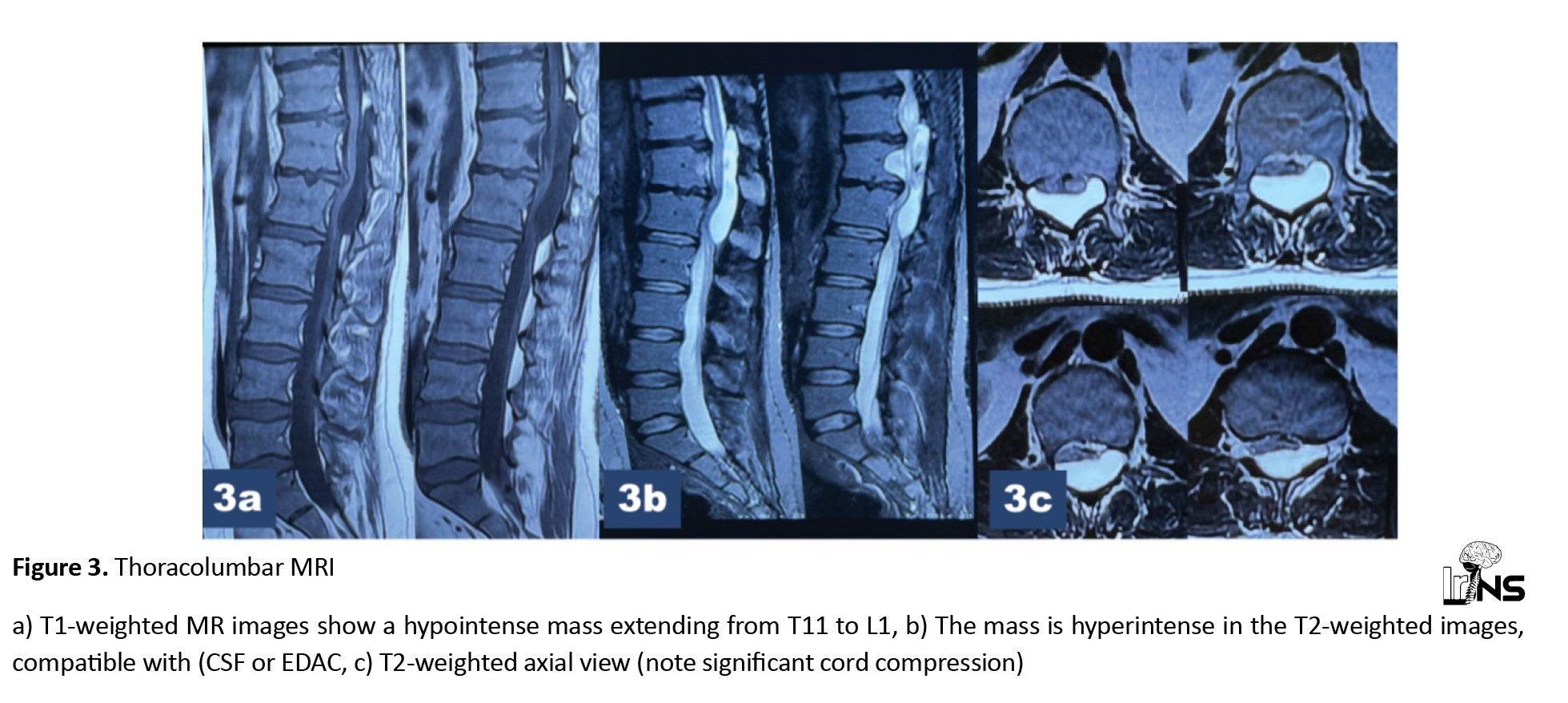
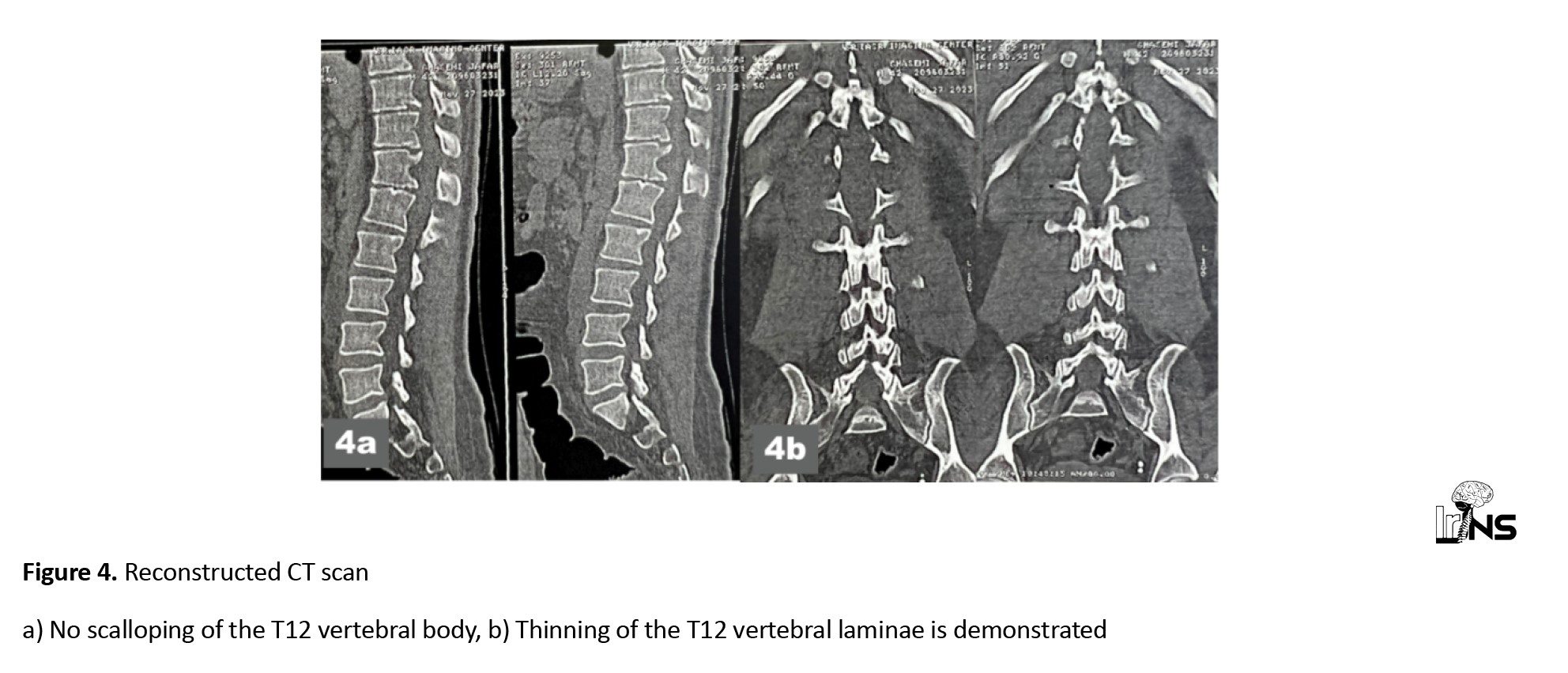
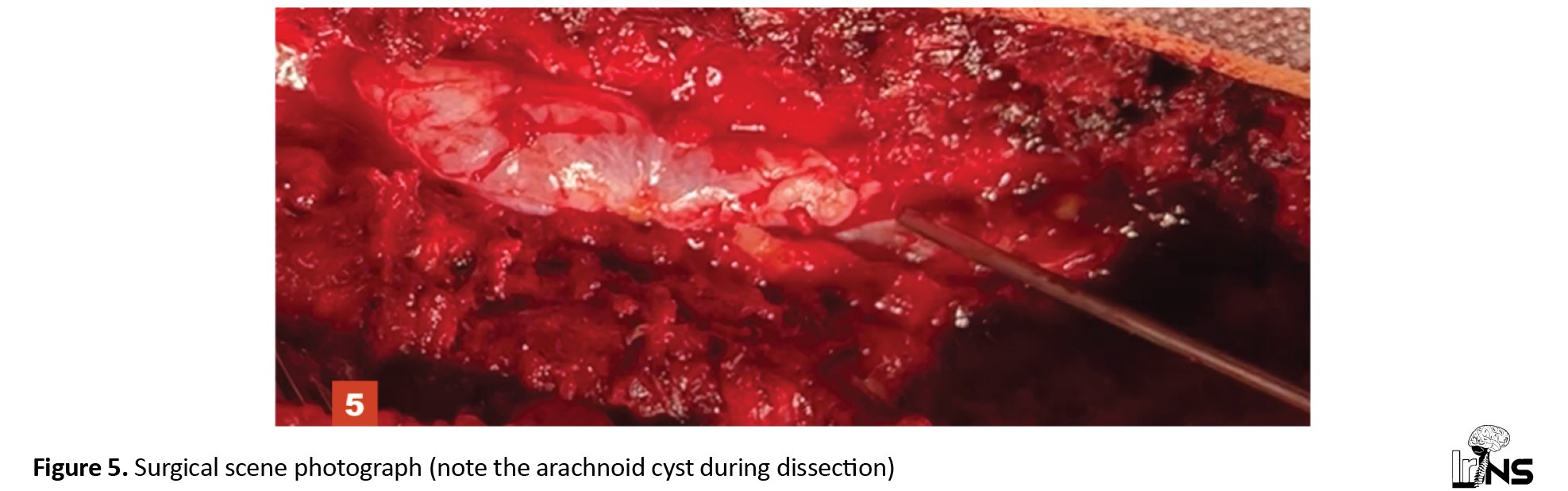
In the sagittal thoracolumbar MRI, a large fluid-containing epidural mass extending from T11 to L1 was demonstrated. The cystic mass exhibited low signal intensity onT1 weighted images and high signal intensity on T2-weighted sagittal images, consistent with an extradural arachnoid cyst. In the axial images, the dural sac was significantly compressed by the arachnoid cyst (Figure 3). The computerized tomography scan also showed erosion of the T12 pedicle and scalloping of the L1 vertebral body (Figure 4). Following a three-level laminectomy, the transparent cyst was separated from the dura mater and completely excised (Figure 5). Subsequently, the communicating dural fistula was visualized on the left side at the T12 level and was closed using a combination of silk sutures and silver clips.
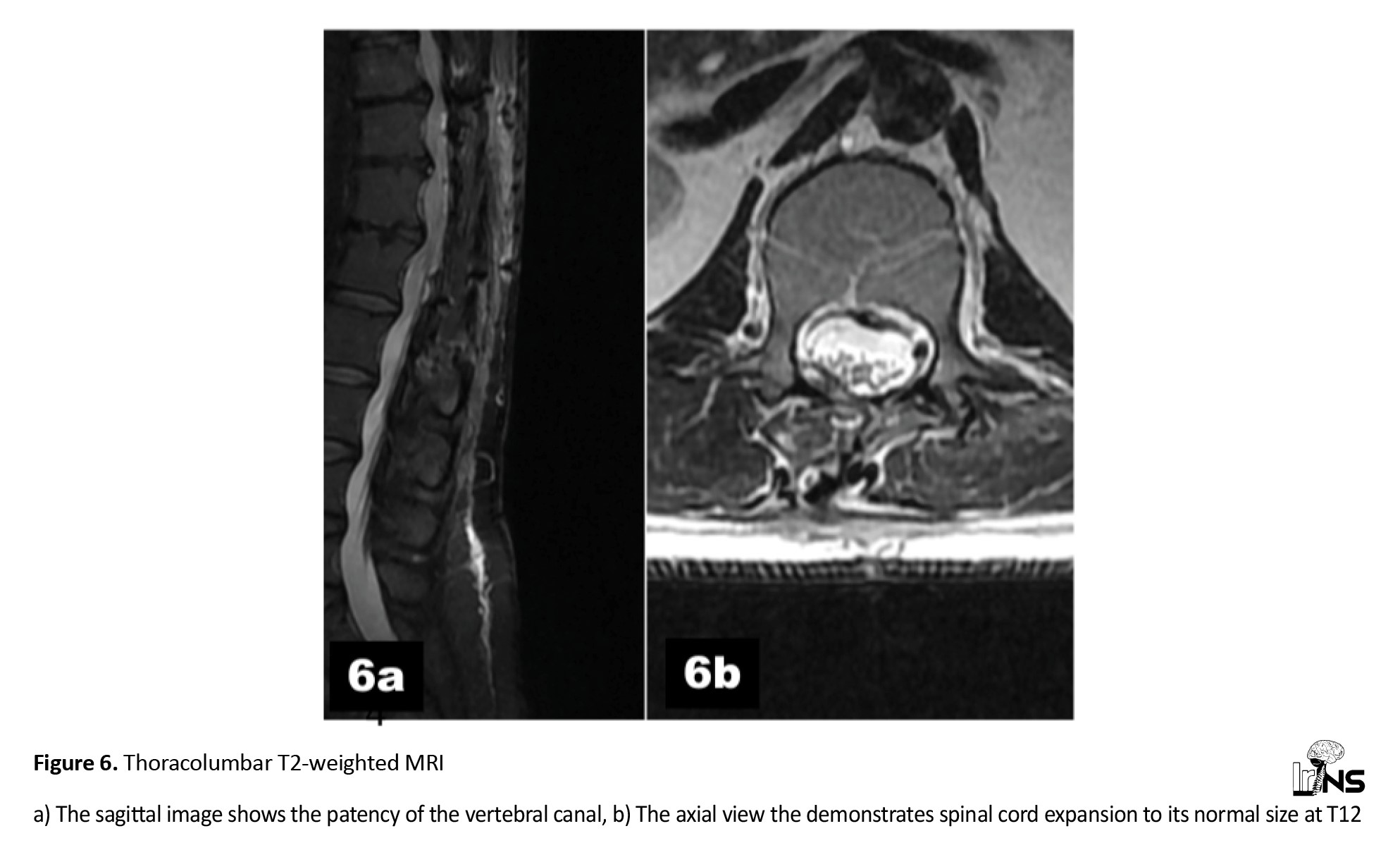
The postoperative course was uneventful. At a six-month follow-up encounter, he was found to be doing very well with a normal neurological examination. His control MRI showed no signs of cord compression (Figure 6).
3. Discussion
EDACs are thin-walled, CSF-containing masses lined by a layer of arachnoid [1-3]. The exact pathogenesis is still being debated. Yet herniation of the arachnoid layer into the extradural space through a tiny dural defect and its gradual enlargement via a one-way valve mechanism is the most accepted among many likely scenarios. These cysts are commonly observed in patients aged 20 to 50 years, with a slight male predominance [1-3, 9]. The cause of the tiny dural holes remains unclear, but it is widely believed to be congenital. The familial occurrence of EDACs supports this theory [9-12]. Rarely, in a patient with EDAC, the primary dural hole may be secondary to closed, penetrating, or iatrogenic trauma and may develop as a result of arachnoiditis or post-hemorrhagic events [13-16].
Location and numbers
These lesions are predominantly located on the posterior aspect of the spinal cord and within the thoracic and thoracolumbar regions in about 77% of cases [1-3, 13-16]. The lumbosacral and sacral regions, with a prevalence of 20%, are the next most frequent locations for the occurrence EDACs. Cervical spine EDACs, with an occurrence of 3%, are the rarest subtype [1-3, 13-16]. In rare instances, spinal EDACs may be present in multiple spinal areas and display a slight predominance in females [9-12].
Clinical picture
The location and size of the cyst determines the specific symptoms and the severity of such symptoms [1-3, 9-12, 17-19]. The duration of symptoms is shorter in cysts that originate within the thoracic spine due to the smaller diameter of the spinal canal in this region [1-3, 9-12, 17-19]. The clinical manifestation of an EDAC depends on its size and location within the spinal column. This means that the symptoms in a cervical EDAC may vary from upper limb radicular pain or paresthesia to quadriparesis [1-3, 9-12, 17-19]. In contrast, thoracic examples typically present with symptoms that commence as intercostal pain or dysesthesia and ultimately result in spastic paraparesis. Lumbosacral EDACs most often emerge as radicular pain and weakness [1-3, 9-12, 17-19]. They may also manifest as urinary dysfunction [17-19]. On one rare occasion, a positive urinary Valsalva maneuver and intermittent priapism were reported in an extradural arachnoid cyst of the lumbar spine [20]. In patients who are either asymptomatic or present with mild symptoms, rapid deterioration can occur which may include the development of paraplegia and spontaneous posterior spinal cord herniation into the extradural space. In such cases, an arachnoid cyst should be suspected and ruled out [21].
Diagnosis
EDACs are best diagnosed based on their characteristic MRI findings. An EDAC exhibits characteristic signals identical to CSF on T1- and T2-weighted images. In addition to accurate diagnosis, delineation of the cystic dimensions can be calculated using MRI [1-3, 9-12, 17-19, 21, 22, 23]. Several studies have employed specialized MR imaging techniques, such as cine-MRI and time-spatial labeling inversion pulse (T-SLIP) MRI, to locate the causative defect between the cyst and the subarachnoid space [24, 25]. This can be also detected with cine MRI by observing pulsating flow voids [24, 25]. The location of the connection between the subarachnoid space and the cyst may also be suspected in an MR myelogram [25]. Digital subtraction cystography can be used to detect the communicating hole in EDAC [26, 27].
Treatment
Treatment varies and depends on whether the patient is symptomatic. With the increasing use of MRI, it is not unusual to find asymptomatic EDACs incidentally. In such cases, conservative treatment involving periodic clinical examination and evaluations of the cyst size with control MRI is recommended [1-3, 16-19].
Laminectomy or laminoplasty, followed by excision of the cyst and subsequent closure of the ostia, has been the most popular approach to treatment [1-3, 12-19]. It should be noted that the mainstay of surgery for symptomatic EDACs is the closure of the communicating fistula between the subarachnoid space and the cyst [23-29]. Therefore, if the site of ostia can be identified preoperatively using cine MRI, MR myelogram, or CT myelography, selective closure of the communicating hole with focal laminectomy or minimally invasive surgery yields excellent results in terms of surgery duration and extent [23-27, 29, 30]. This approach also helps avoid spinal instability and malalignment associated with laminectomy [23-27, 29, 30]. However, it is important to remember that the preoperative identification of communicating ostia is very challenging. Consequently, if the communicating fistula is not discovered, decompressive laminectomy/laminoplasty, excision of the cyst, and closure of the ostia will be the intervention of choice [1-3, 31, 32]. The exception would be children near puberty, in whom even multilevel laminoplasty might result in a late kyphotic deformity. In such cases, postponing surgery may be advisable.
It should be noted that in multiple arachnoid cysts, each cyst typically has its own ostia, therefore closure of all dural defects will be required during a surgical intervention.
Outcome
Postoperatively, all patients with EDACs will benefit from a decompressive laminectomy/laminoplasty, removal of the cyst, and closure of the ostia. However, with extensive laminectomy and even laminoplasty, the possibility of kyphotic deformity should be kept in mind. In such cases, periodic clinical examinations and radiological surveys are necessary. If spinal deformity appears, particularly in children and adolescents, appropriate temporary or permanent instrumentation for the correction of the deformity may become necessary.
4. Conclusion
An EDAC can develop due to outpouchings or entrapment of the arachnoid membrane through a tiny dural defect resulting in gradual enlargement due to a ball-valve mechanism within the cystic opening. MRI is the diagnostic modality of choice, although computed tomography myelography may be superior in detecting the location of the tiny dural defect. Symptomatic arachnoid cysts should be treated surgically. Surgery aims to decompress the spinal cord or cauda equina and restore CSF flow dynamics with appropriate closure of the ostia. However, if the exact site of the fistula between the arachnoid space and EDAC is identified preoperatively, mini laminectomy and selective closure of the fistula at the ostia may then be considered the treatment of choice. Otherwise, laminectomy or laminoplasty, excision of the cyst, and closure of the communicating hole will remain the treatment of choice.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contribute to preparing all parts of the research.
Conflict of interest
The authors declared no conflict of interest.
References
Spinal arachnoid cysts are uncommon, benign lesions that were first described by Spiller in 1903 [1-3]. These cysts are cerebrospinal fluid (CSF)-containing masses lined by the arachnoid mater and account for about 1% of all primary spinal mass lesions. Spinal arachnoid cysts are most often located in extradural and intradural spaces while their intramedullary location is extremely rare [3-9]. Spinal extradural arachnoid cysts (EDAC) are thought to arise from a tiny defect in the dura mater, leading to subsequent herniation of the arachnoid layer into the extradural space and gradual enlargement over time [1-3, 9]. This pathology typically becomes symptomatic in the second to fourth decade of life and its discovery in older adults is much less frequent [1-3, 9]. Before significant enlargement, an EDAC may remain asymptomatic for a long period. The mainstay of surgery for symptomatic EDACs is the closure of the fistula between the subarachnoid space and the cystic outgrowth [1-3, 9]. Herein, we present two new symptomatic adult cases located at the thoracolumbar spinal level.
2. Cases Presentation
Case 1
A 22-year-old woman presented with bilateral lower limb weakness and paresthesia for one year. Her symptoms had noticeably worsened within the last 2 months. Neurological examination demonstrated paraparesis with hyperactive reflexes and a positive Babinski sign. A sensory level with hypesthesia to pinprick and light touch was noted up to the umbilicus.
T1-weighted (A) and T2-weighted (B) sagittal MRI of the thoracolumbar spine revealed an extradural cystic lesion extending from the T11 to T12 levels. The cyst was hypointense on T1-weighted MRI and hyperintense on T2-weighted MRI, consistent with an extradural arachnoid cyst. The cyst displayed a compressive effect on the thinned, ventrally compressed cord in the axial views (Figure 1). Following the performance of an appropriate 2-level laminectomy, an extra-dural cystic lesion was exposed. The cyst was meticulously dissected and separated from the dura until a left-sided ostia was discovered and closed utilizing silk sutures.
During a three-months follow-up encounter, the patient was able to ambulate with some difficulty, but by the 6-month mark, she could walk normally. In the control thoracolumbar MRI at the one-year follow-up encounter, the arachnoid cyst was no longer detectable (Figure 2).
Case 2
A 38-year-old man was admitted to the hospital for numbness and weakness in the left lower limb for two years, along with similar symptoms in the right lower limb for six months. The lower limb weakness had been exacerbated bilaterally in the last three months. His neurological examination revealed asymmetric paraparesis with hyperactive reflexes and a bilateral Babinski sign.
In the sagittal thoracolumbar MRI, a large fluid-containing epidural mass extending from T11 to L1 was demonstrated. The cystic mass exhibited low signal intensity onT1 weighted images and high signal intensity on T2-weighted sagittal images, consistent with an extradural arachnoid cyst. In the axial images, the dural sac was significantly compressed by the arachnoid cyst (Figure 3). The computerized tomography scan also showed erosion of the T12 pedicle and scalloping of the L1 vertebral body (Figure 4). Following a three-level laminectomy, the transparent cyst was separated from the dura mater and completely excised (Figure 5). Subsequently, the communicating dural fistula was visualized on the left side at the T12 level and was closed using a combination of silk sutures and silver clips.
The postoperative course was uneventful. At a six-month follow-up encounter, he was found to be doing very well with a normal neurological examination. His control MRI showed no signs of cord compression (Figure 6).
3. Discussion
EDACs are thin-walled, CSF-containing masses lined by a layer of arachnoid [1-3]. The exact pathogenesis is still being debated. Yet herniation of the arachnoid layer into the extradural space through a tiny dural defect and its gradual enlargement via a one-way valve mechanism is the most accepted among many likely scenarios. These cysts are commonly observed in patients aged 20 to 50 years, with a slight male predominance [1-3, 9]. The cause of the tiny dural holes remains unclear, but it is widely believed to be congenital. The familial occurrence of EDACs supports this theory [9-12]. Rarely, in a patient with EDAC, the primary dural hole may be secondary to closed, penetrating, or iatrogenic trauma and may develop as a result of arachnoiditis or post-hemorrhagic events [13-16].
Location and numbers
These lesions are predominantly located on the posterior aspect of the spinal cord and within the thoracic and thoracolumbar regions in about 77% of cases [1-3, 13-16]. The lumbosacral and sacral regions, with a prevalence of 20%, are the next most frequent locations for the occurrence EDACs. Cervical spine EDACs, with an occurrence of 3%, are the rarest subtype [1-3, 13-16]. In rare instances, spinal EDACs may be present in multiple spinal areas and display a slight predominance in females [9-12].
Clinical picture
The location and size of the cyst determines the specific symptoms and the severity of such symptoms [1-3, 9-12, 17-19]. The duration of symptoms is shorter in cysts that originate within the thoracic spine due to the smaller diameter of the spinal canal in this region [1-3, 9-12, 17-19]. The clinical manifestation of an EDAC depends on its size and location within the spinal column. This means that the symptoms in a cervical EDAC may vary from upper limb radicular pain or paresthesia to quadriparesis [1-3, 9-12, 17-19]. In contrast, thoracic examples typically present with symptoms that commence as intercostal pain or dysesthesia and ultimately result in spastic paraparesis. Lumbosacral EDACs most often emerge as radicular pain and weakness [1-3, 9-12, 17-19]. They may also manifest as urinary dysfunction [17-19]. On one rare occasion, a positive urinary Valsalva maneuver and intermittent priapism were reported in an extradural arachnoid cyst of the lumbar spine [20]. In patients who are either asymptomatic or present with mild symptoms, rapid deterioration can occur which may include the development of paraplegia and spontaneous posterior spinal cord herniation into the extradural space. In such cases, an arachnoid cyst should be suspected and ruled out [21].
Diagnosis
EDACs are best diagnosed based on their characteristic MRI findings. An EDAC exhibits characteristic signals identical to CSF on T1- and T2-weighted images. In addition to accurate diagnosis, delineation of the cystic dimensions can be calculated using MRI [1-3, 9-12, 17-19, 21, 22, 23]. Several studies have employed specialized MR imaging techniques, such as cine-MRI and time-spatial labeling inversion pulse (T-SLIP) MRI, to locate the causative defect between the cyst and the subarachnoid space [24, 25]. This can be also detected with cine MRI by observing pulsating flow voids [24, 25]. The location of the connection between the subarachnoid space and the cyst may also be suspected in an MR myelogram [25]. Digital subtraction cystography can be used to detect the communicating hole in EDAC [26, 27].
Treatment
Treatment varies and depends on whether the patient is symptomatic. With the increasing use of MRI, it is not unusual to find asymptomatic EDACs incidentally. In such cases, conservative treatment involving periodic clinical examination and evaluations of the cyst size with control MRI is recommended [1-3, 16-19].
Laminectomy or laminoplasty, followed by excision of the cyst and subsequent closure of the ostia, has been the most popular approach to treatment [1-3, 12-19]. It should be noted that the mainstay of surgery for symptomatic EDACs is the closure of the communicating fistula between the subarachnoid space and the cyst [23-29]. Therefore, if the site of ostia can be identified preoperatively using cine MRI, MR myelogram, or CT myelography, selective closure of the communicating hole with focal laminectomy or minimally invasive surgery yields excellent results in terms of surgery duration and extent [23-27, 29, 30]. This approach also helps avoid spinal instability and malalignment associated with laminectomy [23-27, 29, 30]. However, it is important to remember that the preoperative identification of communicating ostia is very challenging. Consequently, if the communicating fistula is not discovered, decompressive laminectomy/laminoplasty, excision of the cyst, and closure of the ostia will be the intervention of choice [1-3, 31, 32]. The exception would be children near puberty, in whom even multilevel laminoplasty might result in a late kyphotic deformity. In such cases, postponing surgery may be advisable.
It should be noted that in multiple arachnoid cysts, each cyst typically has its own ostia, therefore closure of all dural defects will be required during a surgical intervention.
Outcome
Postoperatively, all patients with EDACs will benefit from a decompressive laminectomy/laminoplasty, removal of the cyst, and closure of the ostia. However, with extensive laminectomy and even laminoplasty, the possibility of kyphotic deformity should be kept in mind. In such cases, periodic clinical examinations and radiological surveys are necessary. If spinal deformity appears, particularly in children and adolescents, appropriate temporary or permanent instrumentation for the correction of the deformity may become necessary.
4. Conclusion
An EDAC can develop due to outpouchings or entrapment of the arachnoid membrane through a tiny dural defect resulting in gradual enlargement due to a ball-valve mechanism within the cystic opening. MRI is the diagnostic modality of choice, although computed tomography myelography may be superior in detecting the location of the tiny dural defect. Symptomatic arachnoid cysts should be treated surgically. Surgery aims to decompress the spinal cord or cauda equina and restore CSF flow dynamics with appropriate closure of the ostia. However, if the exact site of the fistula between the arachnoid space and EDAC is identified preoperatively, mini laminectomy and selective closure of the fistula at the ostia may then be considered the treatment of choice. Otherwise, laminectomy or laminoplasty, excision of the cyst, and closure of the communicating hole will remain the treatment of choice.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contribute to preparing all parts of the research.
Conflict of interest
The authors declared no conflict of interest.
References
- Garg K, Borkar SA, Kale SS, Sharma BS. Spinal arachnoid cysts - our experience and review of literature. British Journal of Neurosurgery. 2017; 31(2):172-8. [DOI:10.1080/02688697.2016.1229747]
- Lee SW, Foo A, Tan CL, Tan T, Lwin S, Yeo TT, et al. Spinal extradural cyst: Case report and review of literature. World Neurosurgery. 2018; 116:343-6. [DOI:10.1016/j.wneu.2018.05.199]
- Rahimizadeh A, Kaghazchi M, Shariati M, Abdolkhani E, Abbasnejad E, Rahimizadeh S. Spinal extradural arachnoid cysts, Coluna/Columna 2013; 12(2):112-8. [DOI:10.1590/S1808-18512013000200004]
- Tomii M, Mizuno J, Takeda M, Matsushima T, Itoh Y, Numazawa S, et al. Thoracolumbar extradural arachnoid cyst-three surgical case reports. Neurologia Medico-Chirurgica. 2013; 53(2):129-33. [DOI:10.2176/nmc.53.129]
- Wang MY, Levi AD, Green BA. Intradural spinal arachnoid cysts in adults. Surgical Neurology. 2003; 60(1):49-55. [DOI:10.1016/S0090-3019(03)00149-6]
- Rahimizadeh A, Sharifi G. Anterior cervical arachnoid cyst. Asian Spine Journal. 2013; 7(2): 119-25. [DOI:10.4184/asj.2013.7.2.119]
- Schmutzer M, Tonn JC, Zausinger S. Spinal intradural extramedullary arachnoid cysts in adults-operative therapy and clinical outcome. Acta Neurochirurgica. 2020; 162:691-702. [DOI:10.1007/s00701-019-04156-0]
- Rahimizadeh A, Soufiani H. Intramedullary arachnoid cyst in association with cervical spondylosis: Case report. The Spine Journal. 2013; 13(10):e21-5. [DOI:10.1016/j.spinee.2013.05.014]
- Bergland RM. Congenital intraspinal extradural cyst: Report of three cases in one family. Journal of Neurosurgery. 1968; 28(5):495-9. [DOI:10.3171/jns.1968.28.5.0495]
- Takagaki T, Nomura T, Toh E, Watanabe M, Mochida J. Multiple extradural arachnoid cysts at the spinal cord and cauda equina levels in the young. Spinal Cord. 2006; 44(1):59-62. [Link]
- Suryaningtyas W, Arifin M. Multiple spinal extradural arachnoid cysts occurring in a child. Journal of Neurosurgery. 2007; 106(2):158-61. [DOI:10.3171/ped.2007.106.2.158]
- Kahraman S, Anik I, Gocmen S, Sirin S. Departm Extradural giant multiloculated arachnoid cyst causing spinal cord compression in a child.The Journal of Spinal Cord Medicine. 2016; 31(3):306-8. [DOI:10.1080/10790268.2008.11760728]
- Rahimizadeh A, Ehteshami. Yazdi T, Rahimizadeh S. Remote paraparesis due to a traumatic extradural arachnoid cyst developing 2 years after brachial plexus root avulsion injury: Case report and review of the literature. Journal of Brachial Plexus and Peripheral Nerve Injury. 2015; 10(1):e43-9. [DOI:10.1055/s-0035-1558426]
- Hoffman EP, Garner JT, Johnson D, Shelden CH. Traumatic arachnoidal diverticulum associated with paraplegia. Case report. Journal f Neurosurgery. 1973; 38(1):81-5. [DOI:10.3171/jns.1973.38.1.0081]
- Rahimizadeh A, Javadi SA. Symptomatic intraspinal lumbosacral pseudomeningocele, a late consequence of root avulsion injury secondary to gunshot wound. North American Spine Society Journal (NASS J). 2020; 3:100025. [DOI:10.1016/j.xnsj.2020.100025]
- Mao HQ, Yang HL, Geng DC, Bao ZH, Tang TS. Spinal extradural arachnoid cyst following percutaneous vertebroplasty. European Spine Journal. 2011; 20:206-10. [Link]
- Liu JK, Cole CD, Kan P, Schmidt MH. Spinal extradural arachnoid cysts: Clinical, radiological, and surgical features. Neurosurgical Focus. 2007; 22(2):1-5. [DOI:10.3171/foc.2007.22.2.6]
- Lin L, Jason R. A rare case of spinal extradural arachnoid cyst with cord compression. Asian Journal of Neurosurgery. 2018; 13(2):468-70. [DOI:10.4103/ajns.AJNS_310_16]
- Oh JK, Lee DY, Kim TY, Yi S, Ha Y, Kim KN, et al. Thoracolumbar extradural arachnoid cysts: A study of 14 consecutive cases. Acta Neurochirurgica. 2012; 154:341-8. [DOI:10.1007/s00701-011-1110-6]
- Chen WL, Tsai WC,Tsao YT. Valsalva maneuver-induced priapism: A hidden culprit. The Journal of Sexual Medicine. 2009; 6(4):1181-4. [DOI:10.1111/j.1743-6109.2008.01175.x]
- Nejat F, Cigarchi SZ, Kazemi SS. Spinal cord herniation into an extradural thoracic arachnoid cyst: Surgical treatment. Journal of Neurosurgery. 2006; 104(3):210-1. [DOI:10.3171/ped.2006.104.3.210]
- Netra R, Min L, Hui MS, Wang JC, Bin Y, Ming Z. Spinal extradural meningeal cysts: An MRI evaluation of a case series and literature review. Journal of Spinal Disorders & Techniques. 2011; 24(2):132-6. [Link]
- Doita M, Nishida K, Miura J, Takada T, Kurosaka M, Fujii M. Kinematic magnetic resonance imaging of a thoracic spinal extradural arachnoid cyst: An alternative suggestion for exacerbation of symptoms during straining. Spine (Phila Pa 1976) 2003; 28(12):E229-33. [DOI:10.1097/01.BRS.0000065490.71054.2C]
- Neo M, Koyama T, Sakamoto T, Fujibayashi S, Nakamura T. Detection of a dural defect by cinematic magnetic resonance imaging and its selective closure as a treatment for a spinal extradural arachnoid cyst. Spine (Phila Pa 1976). 2004; 29(19):E426-30. [DOI:10.1097/01.brs.0000141189.41705.70]
- Miyamoto M, Kim K, Matsumoto R, Isobe M, Isu T. Utility of preoperative magnetic resonance imaging myelography for identifying dural defects in patients with spinal extradural arachnoid cysts: Case report. Neurosurgery. 2006; 59(4):E941-3. [DOI:10.1227/01.NEU.0000232659.56174.28]
- Gu K, Kwon JW, Kim ES. Digital subtraction cystography for detection of communicating holes of spinal extradural arachnoid cysts. Korean Journal of Radiology. 2016; 17(1):111-6. [DOI:10.3348/kjr.2016.17.1.111]
- Ishibe T, Senzoku F, Ikeda N, Kamba Y, Mikawa Y. Detection of the communicating hole(s) of spinal extradural arachnoid cysts using time-spatial labeling inversion pulse magnetic resonance imaging. Spine (Phila Pa 1976). 2014; 39(23):E1394-7. [DOI:10.1097/BRS.0000000000000591]
- DiSclafani A, Canale DJ. Communicating spinal arachnoid cysts: Diagnosis by delayed metrizamide computed tomography. Surgical Neurology. 1985; 23(4):428-30. [DOI:10.1016/0090-3019(85)90224-1]
- Lee SW, Choi SW, Lim J, Youm JY, Kwon HJ, Koh HS, et al. How to fnd dural defect of spinal extradural arachnoid cyst. Korean Journal of Neurotrauma. 2020; 16(2):360-6. [DOI:10.13004/kjnt.2020.16.e27]
- Ying GY, Chang KS, Tang YJ, Cheng CY, Zhu YJ, Chen CM. Utilizing real-time contrast medium to detect the fistula of giant spinal arachnoid cyst and treat with minimal invasive surgery. BMC Surgery. 2019; 19:11. [DOI:10.1186/s12893-019-0475-y]
- Funao H, Nakamura M, Hosogane N, Watanabe K, Tsuji T, Ishii K, et al. Surgical treatment of spinal extradural arachnoid cysts in the thoracolumbar spine. Neurosurgery. 2012; 71(2):278-84. [DOI:10.1227/NEU.0b013e318257bf74]
- Qi W, Zhao L, Fang J, Chang X, Xu Y. Clinical characteristics and treatment strategies for idiopathic spinal extradural arachnoid cysts: A single-center experience. Acta Neurochirurgica. 2015; 157:539-45. [DOI:10.1007/s00701-014-2278-3]
Type of Study: Case report |
Subject:
Basic Neurosurgery
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |