Wed, Feb 4, 2026
Volume 10 - Continuous Publishing
Iran J Neurosurg 2024, 10 - Continuous Publishing: 229-238 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ashraf A, Yousefzadeh-Chabok S, Shakeri Boroujeni M, Fahimi A, Kaviyani Jebeli T, Eslami kenarsari H. The Relationship Between the Number of Blood Gauze Consumed and Hemoglobin Drop in Craniotomy Surgeries. Iran J Neurosurg 2024; 10 : 27
URL: http://irjns.org/article-1-434-en.html
URL: http://irjns.org/article-1-434-en.html
Ali Ashraf *1 

 , Shahrokh Yousefzadeh-Chabok2
, Shahrokh Yousefzadeh-Chabok2 

 , Mehrnoosh Shakeri Boroujeni3
, Mehrnoosh Shakeri Boroujeni3 

 , Amirhossein Fahimi3
, Amirhossein Fahimi3 

 , Talat Kaviyani Jebeli3
, Talat Kaviyani Jebeli3 

 , Habib Eslami kenarsari4
, Habib Eslami kenarsari4 




 , Shahrokh Yousefzadeh-Chabok2
, Shahrokh Yousefzadeh-Chabok2 

 , Mehrnoosh Shakeri Boroujeni3
, Mehrnoosh Shakeri Boroujeni3 

 , Amirhossein Fahimi3
, Amirhossein Fahimi3 

 , Talat Kaviyani Jebeli3
, Talat Kaviyani Jebeli3 

 , Habib Eslami kenarsari4
, Habib Eslami kenarsari4 


1- Poursina Clinical Research Development Unit, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran. , crdu_poursina@gums.ac.ir
2- Guilan Road Trauma Research Center, Trauma Institute, Guilan University of Medical Sciences, Rasht, Iran.
3- Poursina Clinical Research Development Unit, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Vice-Chancellorship of Research and Technology, Guilan University of Medical Sciences, Rasht, Iran.
2- Guilan Road Trauma Research Center, Trauma Institute, Guilan University of Medical Sciences, Rasht, Iran.
3- Poursina Clinical Research Development Unit, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Vice-Chancellorship of Research and Technology, Guilan University of Medical Sciences, Rasht, Iran.
Full Text [PDF 1486 kb]
(844 Downloads)
| Abstract (HTML) (2486 Views)
Full Text: (806 Views)
1. Introduction
Craniotomy is the removal of part of the bone from the skull to access the brain. Specialized tools called the bone flap are used to remove the bone. The bone flap is temporarily removed and replaced after brain surgery [1, 2]. Bleeding occurs after many surgeries, causing anemia and a drop in hemoglobin (Hb) levels in a person [3].
Studies have shown that patients with anemia are likely to experience a prolonged hospital stay after surgery, leading to increased resource consumption [4]. According to the conducted studies, when the hematocrit (HCT) is <39.1% or >45%, along with increasing severity of anemia and polycythemia, the risk of death 30 days after the operation increases [5]. Other studies have shown that in patients undergoing craniotomy, a small change in Hb after the operation is associated with an increased probability of death within 30 days [6].
Bleeding after craniotomy is clinically crucial and requires accurate measurement of blood loss [7, 8]. When deciding to transfuse blood to neurosurgery patients, the related risks, advantages, and disadvantages should be considered. Strong evidence shows that transfusion-related adverse events are associated with increased morbidity and mortality in children aged 18 to 20 years [9]. The neurosurgeon should be able to accurately estimate the volume of blood lost during surgery to avoid unnecessary blood transfusions [10, 11].
A study conducted on 1032 patients reported that at least one out of every 10 patients undergoing neurosurgery suffered from postoperative anemia. The same study showed that the rate of anemia in cranial surgery was higher than that in non-cranial surgery (11.8 to 10.1) [12].
Anesthesiologists must carefully assess blood loss and replace it with blood components according to clinical conditions. A large volume of fluid loading can decrease the Hb/HCT (level and the dilution effect, which can cause the patient to need more blood transfusions [13, 14].
The best way to avoid this problem is to use appropriate and accurate methods to evaluate the amount of blood loss during surgery. Currently, several methods exist for estimating blood loss. Visual estimation was one of the common methods, another used method is to compare Hb and HCT before and after the operation, and another is the weighing method (the sum of the suctioned blood weight and the blood volume of blood gauze) [15-17].
Currently, the common method of estimating the volume of blood lost in craniotomy surgery is to measure the volume of aspirated blood, and it is not customary to use the method of weighing the volume of blood and blood gauze during surgery. Due to the lack of sufficient studies on blood loss measurement methods, we decided to conduct a study with the aim of “diagnostic value of blood volume of blood gauzes compared to suctioned blood in craniotomy”. In this way, it helps surgeons and anesthesiologists to identify the best method and avoid injecting more or less blood than the patients need.
2. Methods and Materials/Patients
Our study was an analytical-cross-sectional study. The study population of this research includes patients who were admitted to Rasht’s Poursina Hospital in 2019 and underwent craniotomy surgery.
All patients with a history of craniotomy surgery at Poursina Hospital in Rasht were included in the study, and patients who suffered cardiopulmonary arrest and died during surgery were excluded from the study.
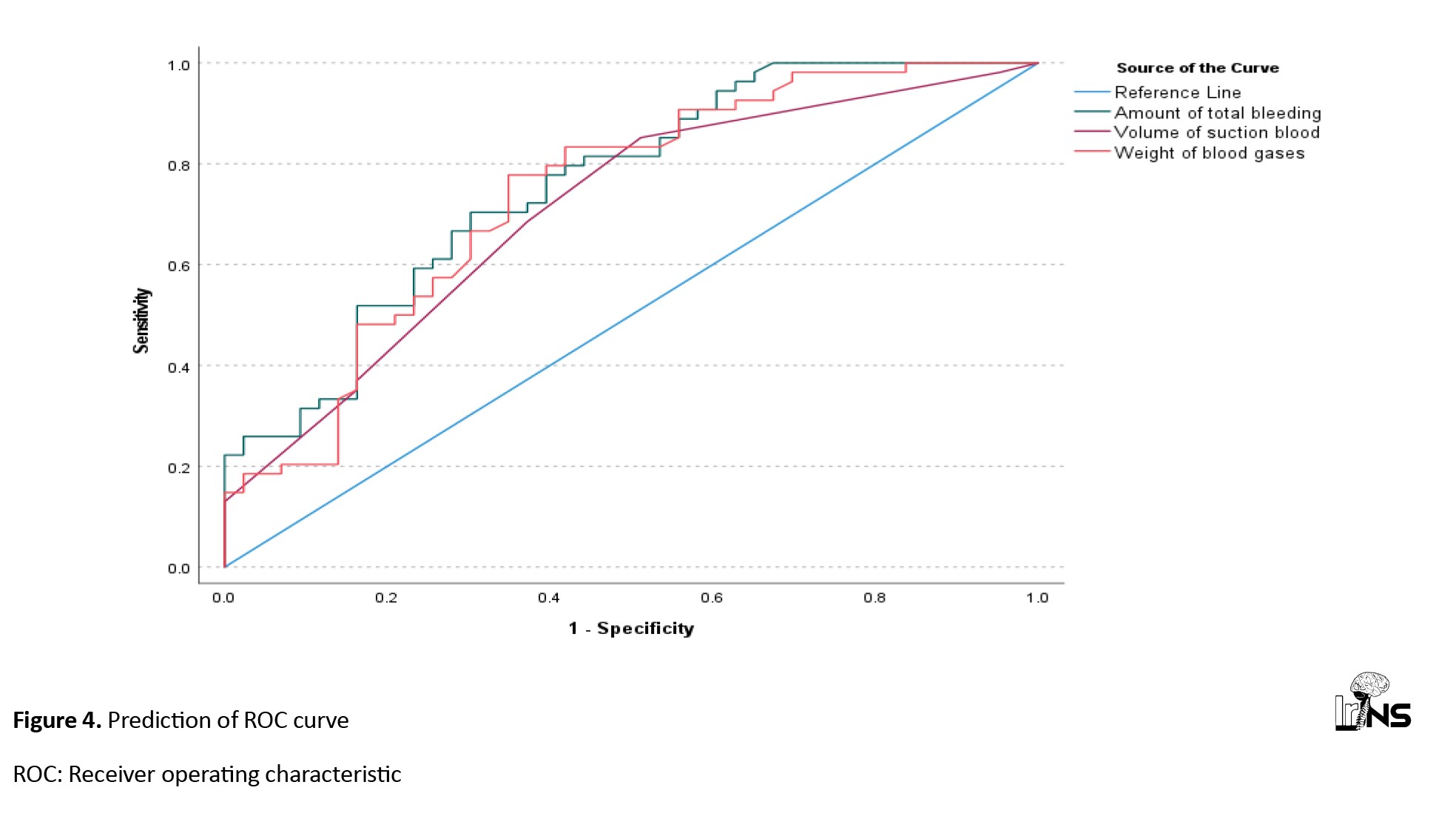
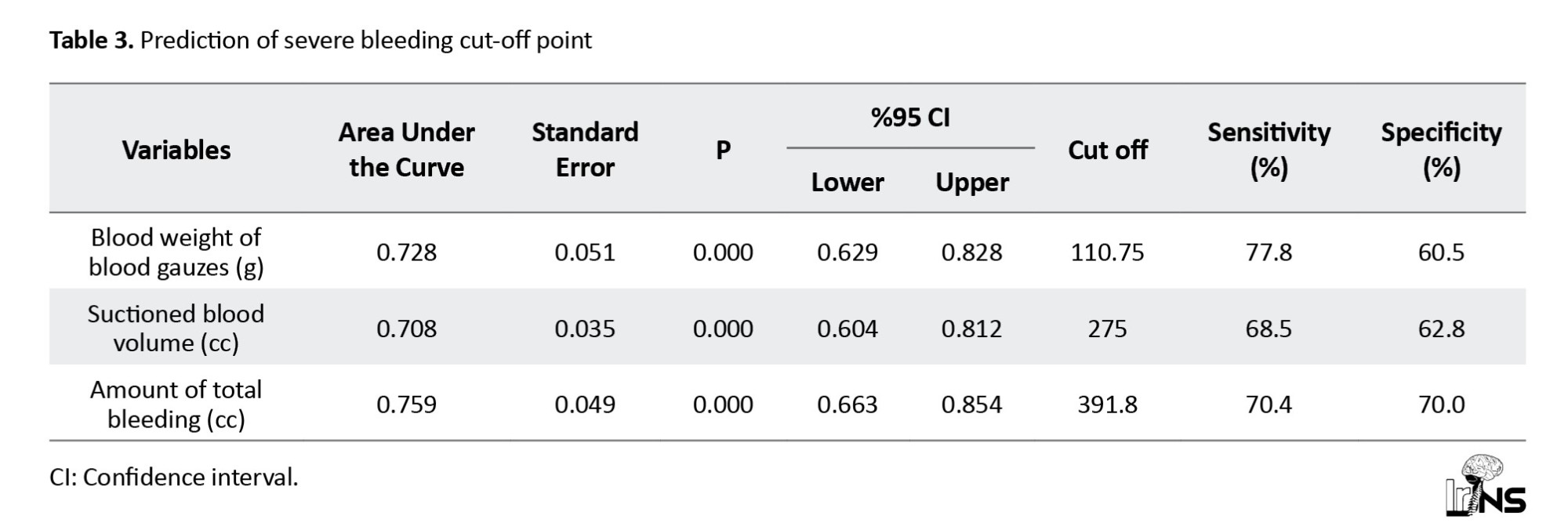
Sampling by the convenience method and based on the article by Grant et al. [18] and the following formula includes 97 patients admitted to Poursina Hospital, Rasht in 2019 who underwent craniotomy surgery. The sample size was calculated based on Equation 1.
After coordination with the university units and the approval of the Ethics Committee, the researcher collected data.
Information, such as age, gender, operation site, operation position, blood group, and history of hypertension and anemia was documented. Hb before and six hours after the surgery was measured.
The volume of blood and fluid received during the operation and the suction blood volume was recorded and blood gauzes were weighed using a scale and the difference in the weight of blood and non-blood gauze was obtained (with an electronic scale SF400).
Finally, the data were analyzed using IBM SPSS software, version 22. Quantitative data was described using Mean±SD and qualitative data was described using frequency and percentage.
We used receiver operating characteristic (ROC) curves to investigate the amount of suctioned blood and the number of blood gauzes in predicting Hb changes after craniotomy surgery in patients admitted to Poursina Hospital, Rasht in the first six months of 2019.
Moreover, to check the relationship between the variables, Pearson’s correlation test was used if the variables were normal and Spearman’s correlation was used if the variables were non-normal.
We used the Shapiro-Wilk test to check the normality of the variables. The error level was considered to be 5%.
3. Result
In this study, 97 craniotomy surgeries were evaluated in terms of suctioned blood and blood gauze numbers in predicting Hb changes after surgery.
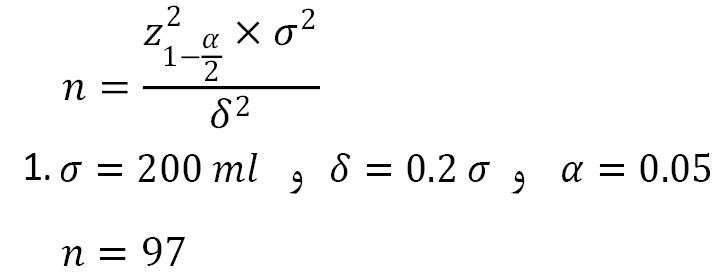
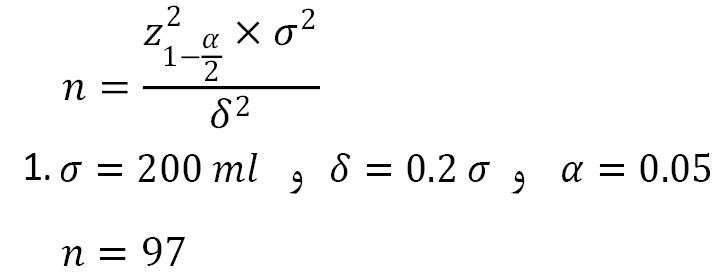
According to Table 1, most craniotomy surgeries were performed in people under 50 years old (40.2%).
In terms of gender, most samples were men (59.8%), and in terms of blood group, most patients had blood group B (32%), and most were RH positive (76.3%).
In the examination of the underlying diseases of the studied patients, (34%) of the patients had underlying diseases, most of which were hypertension (93.9%) and (21.2%) diabetes (57.6%) with coronary artery disease (CAD), and about (32%) patients received blood during surgery.
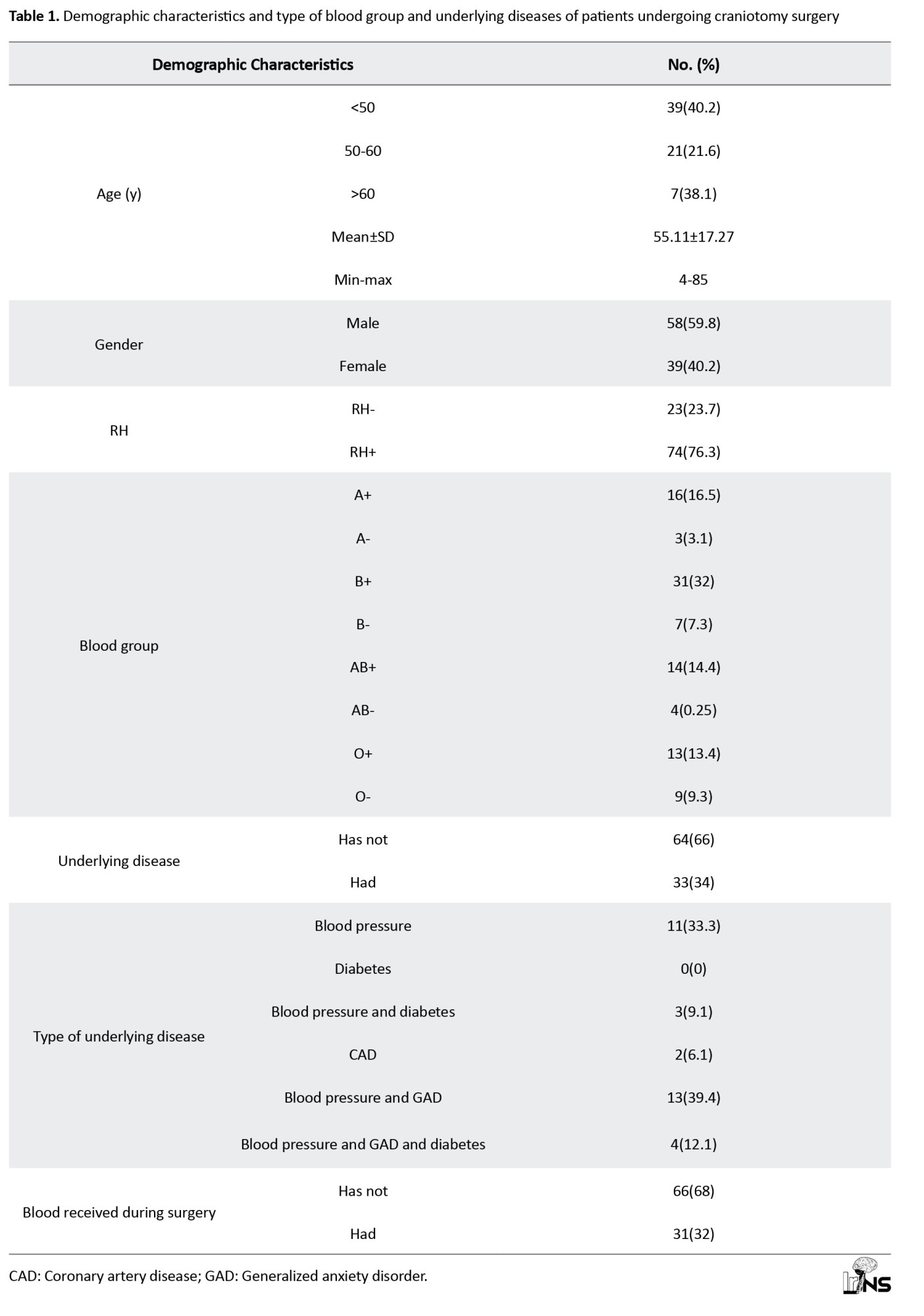
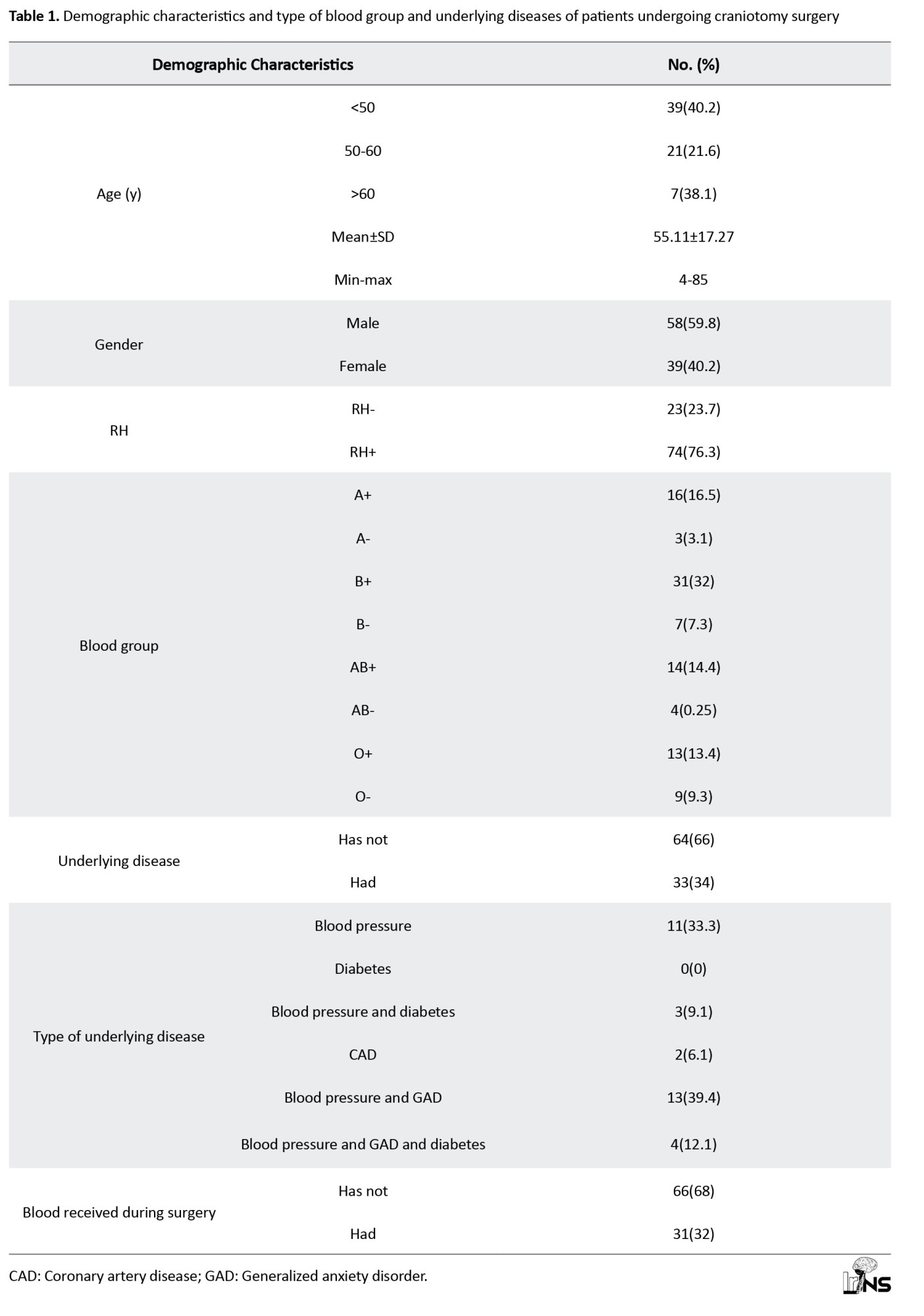
The mean percentage of suctioned blood to the total bleeding is 68.57±7.61, and the mean percentage of blood gauze to the total bleeding is 31.43±7.61 (Table 2).
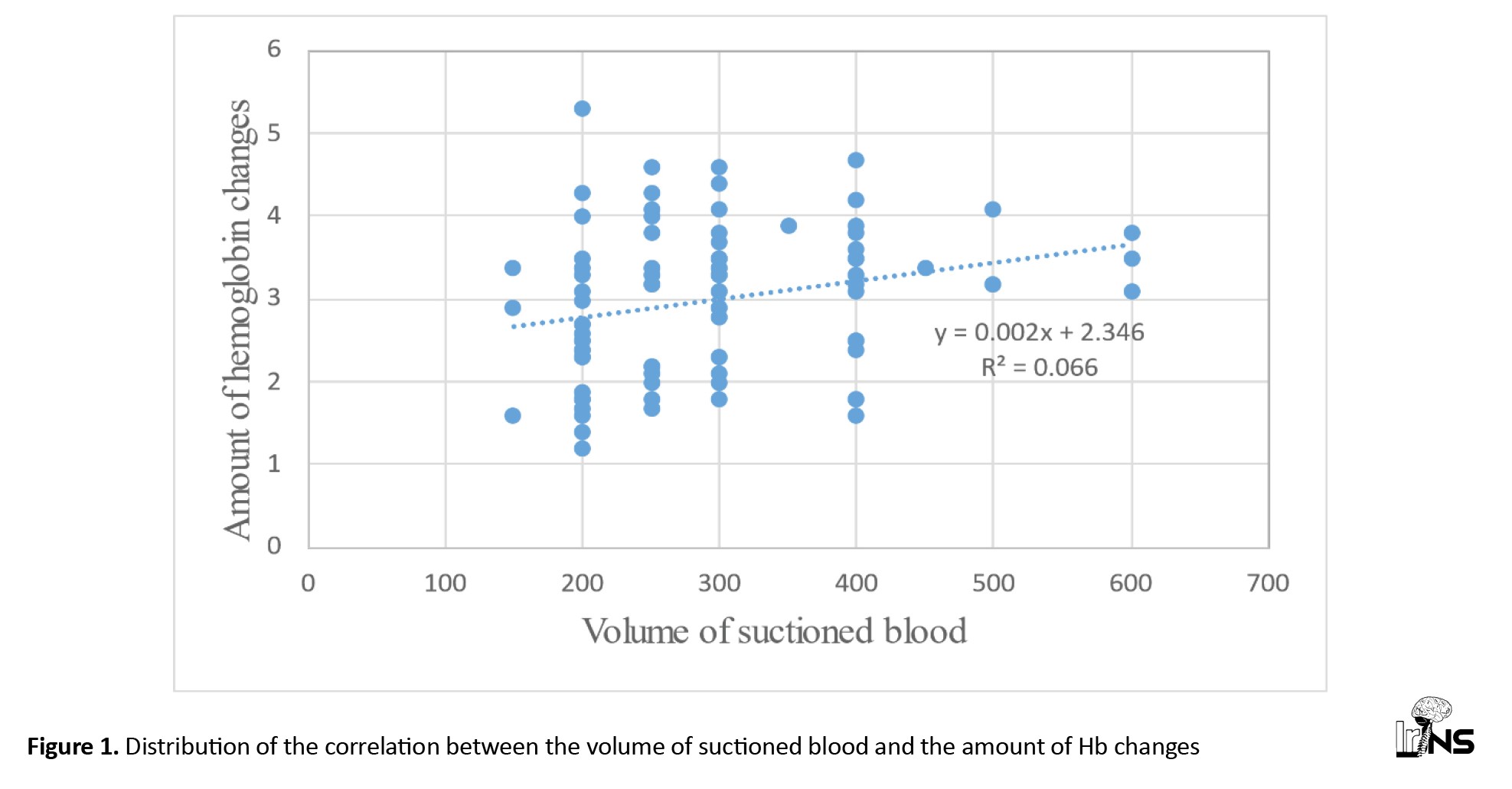
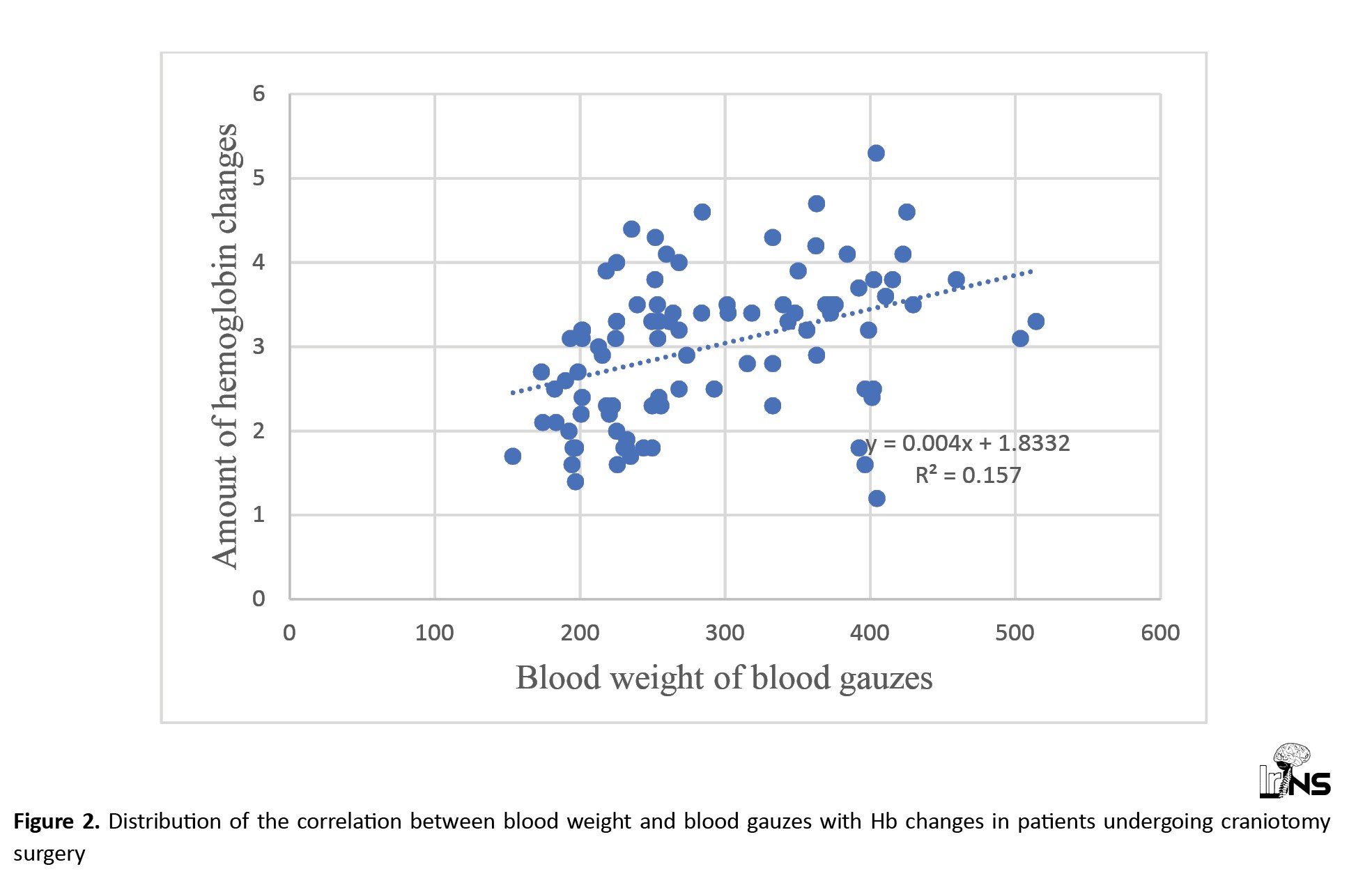
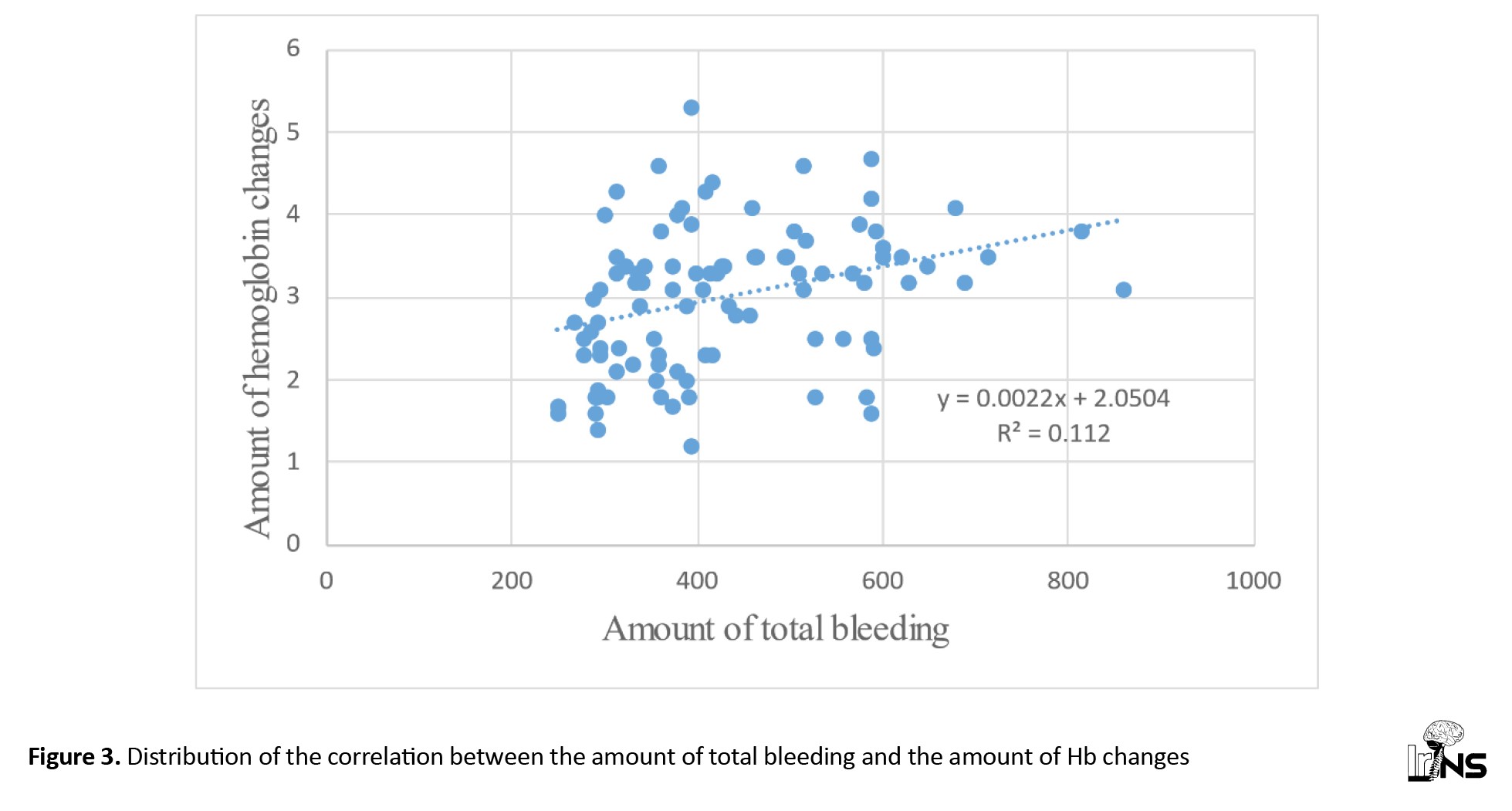
Hb changes have a significant positive linear correlation with blood weight of blood gauzes, suctioned blood volume, total bleeding amount and also with the number of blood gauzes (Figures 1, 2 and 3). This also depends on the number of gauzes and the weight of blood gauzes, which are stronger than suctioned blood.
Based on the Spearman correlation coefficient, the intensity of the correlation between the number of blood gauzes and the amount of blood from blood gauzes was greater than the change in the volume of suctioned blood and the amount of total bleeding.
For one gram increase in blood weight of blood gauzes, 7.6×0.001 units affect the decrease of Hb. Based on the coefficient of determination of blood weight from blood gauzes, on average 14.1% predicts changes in Hb.
Based on the R2 coefficient, the predictive value and effect coefficient (β) of blood weight from blood gauzes is more than whole blood and suctioned blood.
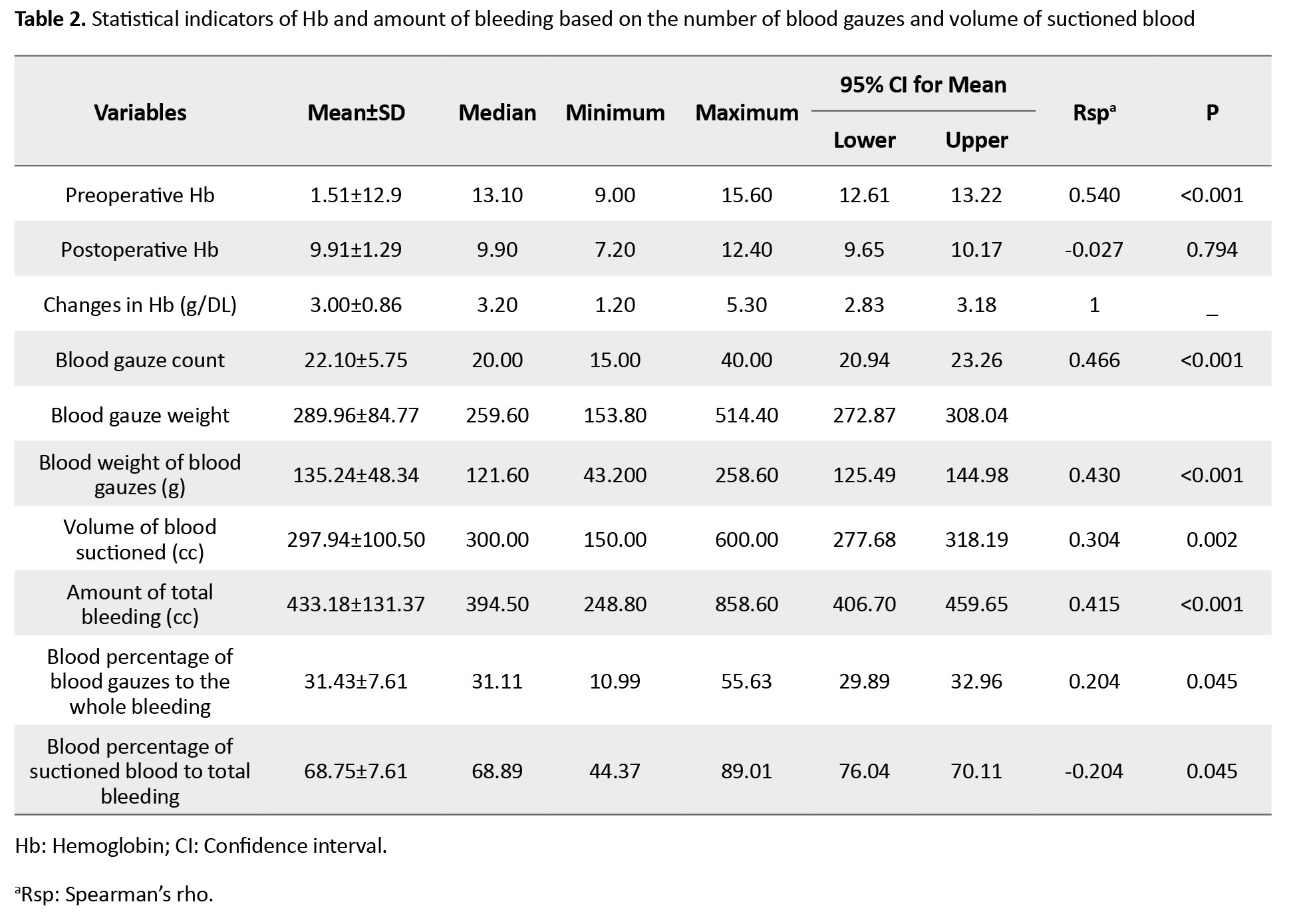
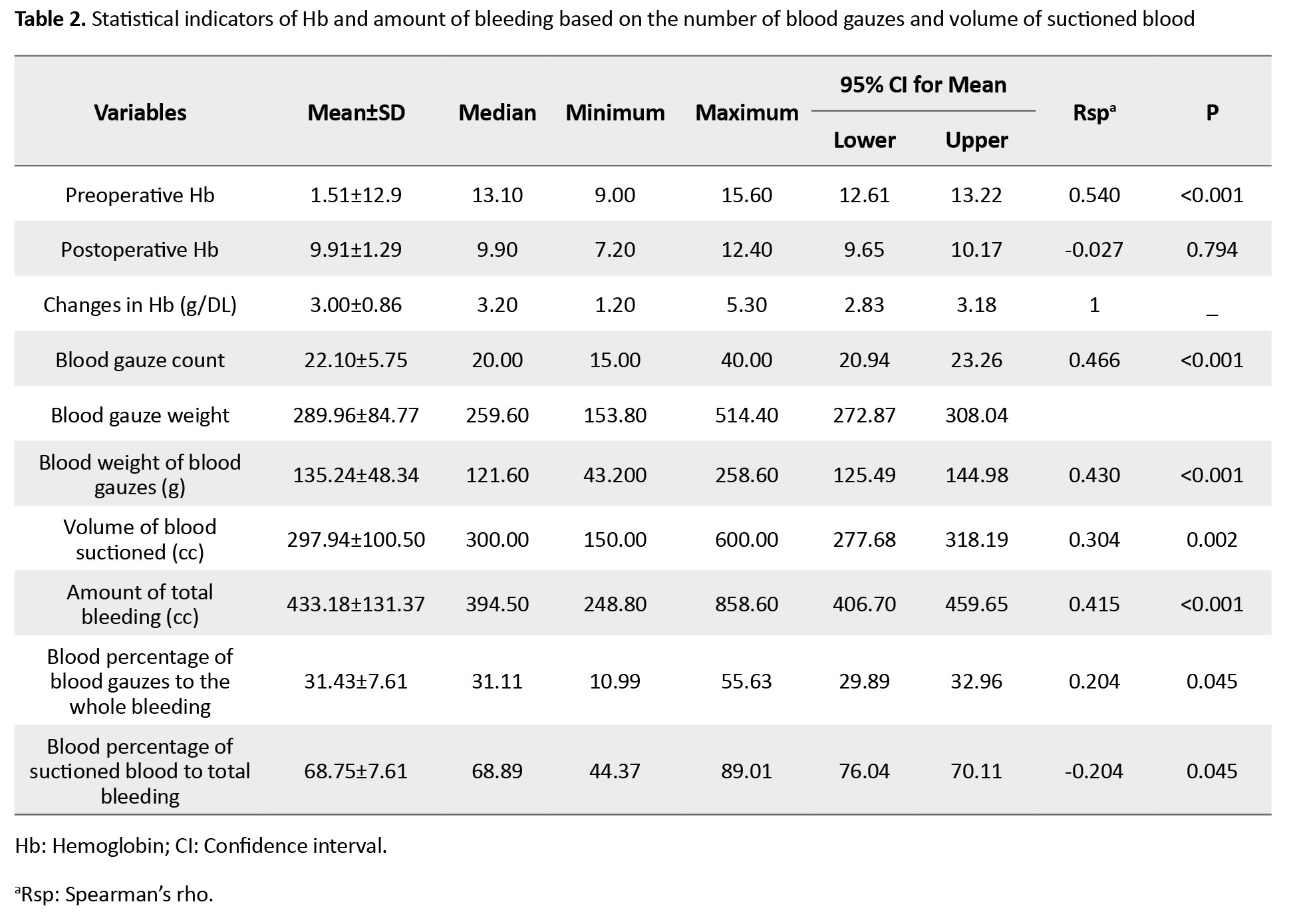
Based on the ROC diagram and information in Table 3, the level of predicting blood weight from blood gauzes (ROC=0.728±0.005) was statistically significant (Figure 4).
The best cut-off points for predicting bleeding more than normal in the volume of suctioned blood equaled to 275 cc with sensitivity and specificity of 68.5% and 62.8%.
Finally, the amount of total bleeding to predict bleeding more than normal in the craniotomy surgery community is equal to 759±0.049, which is also statistically significant (P<0.001).
The best cut off point for total bleeding to predict bleeding more than the normal society is 391.8 cc with sensitivity and specificity of 70.4% and 70%.
4. Discussion
According to the definition of anemia (<12 for women and <13 for men) by World Health Organization (WHO), about 80% to 90% of post-operative patients can be included in this definition, but clinically, we often consider Hb less than 10 as anemia after surgery [19].
Since bleeding is one of the most common complications of craniotomy surgery and it can be associated with poor clinical results, and long-term hospitalization for the patient and even death, accurate measurement of blood loss and timely injection of blood and fluids is of particular importance in these patients.
Many studies are conducted about the methods of measuring blood loss during surgery, but since few studies compare blood loss by blood gauze and suctioned blood in predicting Hb drop after surgery, we decided to investigate this issue by conducting this study so that we can predict the blood lost during the operation using its results and at the same time prevent unnecessary blood transfusion.
The strength of our study is the specific investigation of craniotomy surgeries and also the use of a combined method (weight measurement of blood gauze + aspirated blood) in the estimation of blood loss during surgery. By using this information, we can accurately estimate the amount of Hb drop and reserve blood for the patient before surgery.
All the data were obtained from the detailed information recorded in the files of patients undergoing craniotomy in Poursina Hospital. The blood volume of blood gauze and suctioned blood in the bottles was measured and analyzed with accurate weighing methods.
The results of our study showed that 32% of patients received blood during craniotomy. Shiferaw et al., on 153 patients to investigate complications after elective craniotomy, although blood loss in that study was evaluated by the EBC formula (based on Hb and HCT before and after the operation). It was calculated in patients with a lower average age, but it showed the same results as our study (36.7%) [20].
The number of changes in Hb before and after the operation in our study was on average 3+0.86, In the study of Parthiban Giribabu et al., which was conducted on 1025 patients to investigate the risk factors and the effect of anemia after neurosurgery, this amount was reported as 1 gram. The reason for this can be the difference in the amount of blood injected during the operation and the type of surgery being investigated [12].
The frequency of the underlying disease of blood pressure in our subjects was (33%) which is a higher number compared to Shiferaw et al.’s study (7.8%), the reason for this difference can be the higher average age of our study subjects and also high blood pressure statistics in our country [20].
The average amount of total bleeding in our study, which was obtained from the sum of the blood weight of blood gauzes and suctioned blood, was equal to 433.18±131.3. In Shiferaw et al.’s study, which was conducted on 153 patients undergoing elective craniotomy, the average amounts of blood lost was 1040±727 [20]. The reason for this difference can be the different blood measurement methods in this study (Hb and HCT calculation method before and after the operation) and the difference in the surgeon’s technique and skill. Also in our study, the blood on the surgical gowns and the surgical bed was not calculated, which could be one of the causes of this difference.
The results of our study revealed that the number of changes in Hb has a significant positive linear correlation with the number of blood gauzes, the weight of blood obtained from them, the volume of suctioned blood, and the amount of total bleeding, this also depends on the number of gauzes and the weight of blood gauzes, which are stronger than suctioned blood.
However, in the field of surgery, the surgeon’s concern is generally focused on the volume of suctioned blood, therefore, the volume of suctioned blood is regularly monitored and reported, but the number of blood gauzes used may be neglected.
Many studies have not been conducted on the comparison of aspirated blood and blood obtained from blood gauzes in predicting post-operative Hb drop.
Based on the data analysis, for one gram increase in blood weight from blood gauzes, Hb decreases by 6.7×0.001 units, on the other hand, suctioned blood has an average effect on Hb drop by 2.2×0.001.
This strong relationship between the blood volume of consumed gauze and Hb drop can be due to the use of a high number of gauzes used during the operation. In our study, the number of consumed gauzes was even reported up to 45.
These results indicated that although the volume of suctioned blood can be a predictor of Hb drop and the subsequent blood transfusion can prevent the decrease of Hb to some extent, if only this volume is used as the basis for blood unit injection, The risk of anemia and its complications are still relevant, especially in patients whose blood volume of consumed gauzes is greater than the volume of suctioned blood.
Therefore, it is necessary to not only rely on suctioned blood when deciding to start a blood transfusion, but the number of blood gauze consumed in the operation field should also be seriously considered in the calculations and use combined methods to calculate the amount of blood lost.
5. Conclusion
The results of our study demonstrated that both methods of measuring the volume of blood lost, i.e. suctioned blood and the blood volume of blood gauze, are effective in reducing Hb, but the effect coefficient of the blood volume of gauze consumed during craniotomy surgery can be even higher than suctioned blood.
This shows that measuring the number of gauze consumed during this surgery can be effective in predicting the amount of blood loss and Hb drop of the patient after the operation, and by accurately calculating the blood loss, it can reduce complications after the operation. It is caused by Hb drop and improves blood count and injection system to help in craniotomy surgeries.
One of the limitations of our study was the lack of examination of the blood absorbed into the surgical wounds, since a large amount of blood is lost in this way during surgical procedures, especially in cases of severe bleeding, conducting further studies to evaluate the effect of this volume of blood on Hb drop can be associated with achieving better outcomes after this type of surgery.
Our suggestion for future studies is to repeat the study with a higher sample size and investigate other types of surgeries, especially major surgeries, as well as consider the duration of surgeries in the amount of blood lost, so that using the results of those studies, a more accurate decision can be made. It should be adopted for the amount of blood transfusion in patients undergoing various surgeries and prevent further complications for patients and impose additional costs on the hospital.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Guilan, Rasht, Iran (IR.GUMS.REC.1399.168). Honesty and ethical standards were observed in the use of information, results, and their publication. The patient’s personal information was preserved and no one, except the research team, had access to the information under investigation.
Funding
This research did not receive any grant from funding agencies in the government, public, university, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Ali Ashraf, and Shahrokh Yousefzadeh-Chabok; Data collection: Amirhossein Fahimi, and Talat Kaviyani Jebeli; Data analysis and interpretation: Habib Eslami-Kenarsari; Writing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Craniotomy is the removal of part of the bone from the skull to access the brain. Specialized tools called the bone flap are used to remove the bone. The bone flap is temporarily removed and replaced after brain surgery [1, 2]. Bleeding occurs after many surgeries, causing anemia and a drop in hemoglobin (Hb) levels in a person [3].
Studies have shown that patients with anemia are likely to experience a prolonged hospital stay after surgery, leading to increased resource consumption [4]. According to the conducted studies, when the hematocrit (HCT) is <39.1% or >45%, along with increasing severity of anemia and polycythemia, the risk of death 30 days after the operation increases [5]. Other studies have shown that in patients undergoing craniotomy, a small change in Hb after the operation is associated with an increased probability of death within 30 days [6].
Bleeding after craniotomy is clinically crucial and requires accurate measurement of blood loss [7, 8]. When deciding to transfuse blood to neurosurgery patients, the related risks, advantages, and disadvantages should be considered. Strong evidence shows that transfusion-related adverse events are associated with increased morbidity and mortality in children aged 18 to 20 years [9]. The neurosurgeon should be able to accurately estimate the volume of blood lost during surgery to avoid unnecessary blood transfusions [10, 11].
A study conducted on 1032 patients reported that at least one out of every 10 patients undergoing neurosurgery suffered from postoperative anemia. The same study showed that the rate of anemia in cranial surgery was higher than that in non-cranial surgery (11.8 to 10.1) [12].
Anesthesiologists must carefully assess blood loss and replace it with blood components according to clinical conditions. A large volume of fluid loading can decrease the Hb/HCT (level and the dilution effect, which can cause the patient to need more blood transfusions [13, 14].
The best way to avoid this problem is to use appropriate and accurate methods to evaluate the amount of blood loss during surgery. Currently, several methods exist for estimating blood loss. Visual estimation was one of the common methods, another used method is to compare Hb and HCT before and after the operation, and another is the weighing method (the sum of the suctioned blood weight and the blood volume of blood gauze) [15-17].
Currently, the common method of estimating the volume of blood lost in craniotomy surgery is to measure the volume of aspirated blood, and it is not customary to use the method of weighing the volume of blood and blood gauze during surgery. Due to the lack of sufficient studies on blood loss measurement methods, we decided to conduct a study with the aim of “diagnostic value of blood volume of blood gauzes compared to suctioned blood in craniotomy”. In this way, it helps surgeons and anesthesiologists to identify the best method and avoid injecting more or less blood than the patients need.
2. Methods and Materials/Patients
Our study was an analytical-cross-sectional study. The study population of this research includes patients who were admitted to Rasht’s Poursina Hospital in 2019 and underwent craniotomy surgery.
All patients with a history of craniotomy surgery at Poursina Hospital in Rasht were included in the study, and patients who suffered cardiopulmonary arrest and died during surgery were excluded from the study.
Sampling by the convenience method and based on the article by Grant et al. [18] and the following formula includes 97 patients admitted to Poursina Hospital, Rasht in 2019 who underwent craniotomy surgery. The sample size was calculated based on Equation 1.
After coordination with the university units and the approval of the Ethics Committee, the researcher collected data.
Information, such as age, gender, operation site, operation position, blood group, and history of hypertension and anemia was documented. Hb before and six hours after the surgery was measured.
The volume of blood and fluid received during the operation and the suction blood volume was recorded and blood gauzes were weighed using a scale and the difference in the weight of blood and non-blood gauze was obtained (with an electronic scale SF400).
Finally, the data were analyzed using IBM SPSS software, version 22. Quantitative data was described using Mean±SD and qualitative data was described using frequency and percentage.
We used receiver operating characteristic (ROC) curves to investigate the amount of suctioned blood and the number of blood gauzes in predicting Hb changes after craniotomy surgery in patients admitted to Poursina Hospital, Rasht in the first six months of 2019.
Moreover, to check the relationship between the variables, Pearson’s correlation test was used if the variables were normal and Spearman’s correlation was used if the variables were non-normal.
We used the Shapiro-Wilk test to check the normality of the variables. The error level was considered to be 5%.
3. Result
In this study, 97 craniotomy surgeries were evaluated in terms of suctioned blood and blood gauze numbers in predicting Hb changes after surgery.
According to Table 1, most craniotomy surgeries were performed in people under 50 years old (40.2%).
In terms of gender, most samples were men (59.8%), and in terms of blood group, most patients had blood group B (32%), and most were RH positive (76.3%).
In the examination of the underlying diseases of the studied patients, (34%) of the patients had underlying diseases, most of which were hypertension (93.9%) and (21.2%) diabetes (57.6%) with coronary artery disease (CAD), and about (32%) patients received blood during surgery.
The mean percentage of suctioned blood to the total bleeding is 68.57±7.61, and the mean percentage of blood gauze to the total bleeding is 31.43±7.61 (Table 2).
Hb changes have a significant positive linear correlation with blood weight of blood gauzes, suctioned blood volume, total bleeding amount and also with the number of blood gauzes (Figures 1, 2 and 3). This also depends on the number of gauzes and the weight of blood gauzes, which are stronger than suctioned blood.
Based on the Spearman correlation coefficient, the intensity of the correlation between the number of blood gauzes and the amount of blood from blood gauzes was greater than the change in the volume of suctioned blood and the amount of total bleeding.
For one gram increase in blood weight of blood gauzes, 7.6×0.001 units affect the decrease of Hb. Based on the coefficient of determination of blood weight from blood gauzes, on average 14.1% predicts changes in Hb.
Based on the R2 coefficient, the predictive value and effect coefficient (β) of blood weight from blood gauzes is more than whole blood and suctioned blood.
Based on the ROC diagram and information in Table 3, the level of predicting blood weight from blood gauzes (ROC=0.728±0.005) was statistically significant (Figure 4).
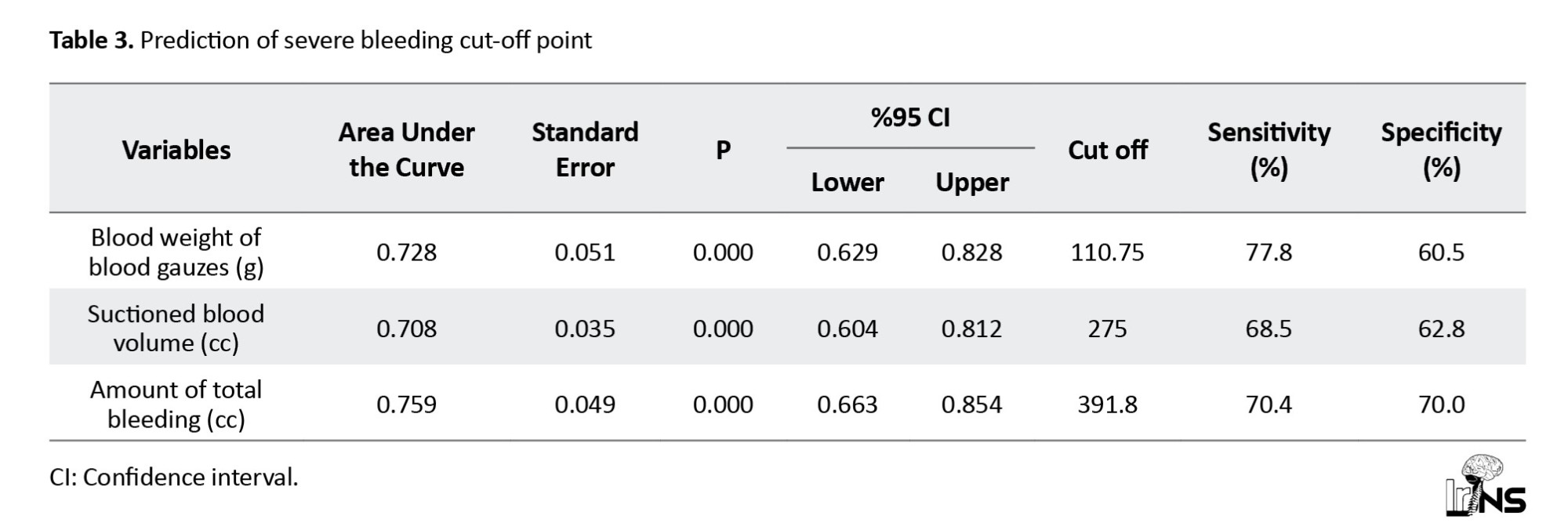
The best cut-off points for predicting bleeding more than normal in the volume of suctioned blood equaled to 275 cc with sensitivity and specificity of 68.5% and 62.8%.
Finally, the amount of total bleeding to predict bleeding more than normal in the craniotomy surgery community is equal to 759±0.049, which is also statistically significant (P<0.001).
The best cut off point for total bleeding to predict bleeding more than the normal society is 391.8 cc with sensitivity and specificity of 70.4% and 70%.
4. Discussion
According to the definition of anemia (<12 for women and <13 for men) by World Health Organization (WHO), about 80% to 90% of post-operative patients can be included in this definition, but clinically, we often consider Hb less than 10 as anemia after surgery [19].
Since bleeding is one of the most common complications of craniotomy surgery and it can be associated with poor clinical results, and long-term hospitalization for the patient and even death, accurate measurement of blood loss and timely injection of blood and fluids is of particular importance in these patients.
Many studies are conducted about the methods of measuring blood loss during surgery, but since few studies compare blood loss by blood gauze and suctioned blood in predicting Hb drop after surgery, we decided to investigate this issue by conducting this study so that we can predict the blood lost during the operation using its results and at the same time prevent unnecessary blood transfusion.
The strength of our study is the specific investigation of craniotomy surgeries and also the use of a combined method (weight measurement of blood gauze + aspirated blood) in the estimation of blood loss during surgery. By using this information, we can accurately estimate the amount of Hb drop and reserve blood for the patient before surgery.
All the data were obtained from the detailed information recorded in the files of patients undergoing craniotomy in Poursina Hospital. The blood volume of blood gauze and suctioned blood in the bottles was measured and analyzed with accurate weighing methods.
The results of our study showed that 32% of patients received blood during craniotomy. Shiferaw et al., on 153 patients to investigate complications after elective craniotomy, although blood loss in that study was evaluated by the EBC formula (based on Hb and HCT before and after the operation). It was calculated in patients with a lower average age, but it showed the same results as our study (36.7%) [20].
The number of changes in Hb before and after the operation in our study was on average 3+0.86, In the study of Parthiban Giribabu et al., which was conducted on 1025 patients to investigate the risk factors and the effect of anemia after neurosurgery, this amount was reported as 1 gram. The reason for this can be the difference in the amount of blood injected during the operation and the type of surgery being investigated [12].
The frequency of the underlying disease of blood pressure in our subjects was (33%) which is a higher number compared to Shiferaw et al.’s study (7.8%), the reason for this difference can be the higher average age of our study subjects and also high blood pressure statistics in our country [20].
The average amount of total bleeding in our study, which was obtained from the sum of the blood weight of blood gauzes and suctioned blood, was equal to 433.18±131.3. In Shiferaw et al.’s study, which was conducted on 153 patients undergoing elective craniotomy, the average amounts of blood lost was 1040±727 [20]. The reason for this difference can be the different blood measurement methods in this study (Hb and HCT calculation method before and after the operation) and the difference in the surgeon’s technique and skill. Also in our study, the blood on the surgical gowns and the surgical bed was not calculated, which could be one of the causes of this difference.
The results of our study revealed that the number of changes in Hb has a significant positive linear correlation with the number of blood gauzes, the weight of blood obtained from them, the volume of suctioned blood, and the amount of total bleeding, this also depends on the number of gauzes and the weight of blood gauzes, which are stronger than suctioned blood.
However, in the field of surgery, the surgeon’s concern is generally focused on the volume of suctioned blood, therefore, the volume of suctioned blood is regularly monitored and reported, but the number of blood gauzes used may be neglected.
Many studies have not been conducted on the comparison of aspirated blood and blood obtained from blood gauzes in predicting post-operative Hb drop.
Based on the data analysis, for one gram increase in blood weight from blood gauzes, Hb decreases by 6.7×0.001 units, on the other hand, suctioned blood has an average effect on Hb drop by 2.2×0.001.
This strong relationship between the blood volume of consumed gauze and Hb drop can be due to the use of a high number of gauzes used during the operation. In our study, the number of consumed gauzes was even reported up to 45.
These results indicated that although the volume of suctioned blood can be a predictor of Hb drop and the subsequent blood transfusion can prevent the decrease of Hb to some extent, if only this volume is used as the basis for blood unit injection, The risk of anemia and its complications are still relevant, especially in patients whose blood volume of consumed gauzes is greater than the volume of suctioned blood.
Therefore, it is necessary to not only rely on suctioned blood when deciding to start a blood transfusion, but the number of blood gauze consumed in the operation field should also be seriously considered in the calculations and use combined methods to calculate the amount of blood lost.
5. Conclusion
The results of our study demonstrated that both methods of measuring the volume of blood lost, i.e. suctioned blood and the blood volume of blood gauze, are effective in reducing Hb, but the effect coefficient of the blood volume of gauze consumed during craniotomy surgery can be even higher than suctioned blood.
This shows that measuring the number of gauze consumed during this surgery can be effective in predicting the amount of blood loss and Hb drop of the patient after the operation, and by accurately calculating the blood loss, it can reduce complications after the operation. It is caused by Hb drop and improves blood count and injection system to help in craniotomy surgeries.
One of the limitations of our study was the lack of examination of the blood absorbed into the surgical wounds, since a large amount of blood is lost in this way during surgical procedures, especially in cases of severe bleeding, conducting further studies to evaluate the effect of this volume of blood on Hb drop can be associated with achieving better outcomes after this type of surgery.
Our suggestion for future studies is to repeat the study with a higher sample size and investigate other types of surgeries, especially major surgeries, as well as consider the duration of surgeries in the amount of blood lost, so that using the results of those studies, a more accurate decision can be made. It should be adopted for the amount of blood transfusion in patients undergoing various surgeries and prevent further complications for patients and impose additional costs on the hospital.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Guilan, Rasht, Iran (IR.GUMS.REC.1399.168). Honesty and ethical standards were observed in the use of information, results, and their publication. The patient’s personal information was preserved and no one, except the research team, had access to the information under investigation.
Funding
This research did not receive any grant from funding agencies in the government, public, university, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Ali Ashraf, and Shahrokh Yousefzadeh-Chabok; Data collection: Amirhossein Fahimi, and Talat Kaviyani Jebeli; Data analysis and interpretation: Habib Eslami-Kenarsari; Writing and final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Hutchinson PJ, Kolias AG, Timofeev IS, Corteen EA, Czosnyka M, Timothy J, et al. Trial of decompressive craniectomy for traumatic intracranial hypertension. The New England Journal of Medicine. 2016; 375(12):1119-30. [DOI:10.1056/NEJMoa1605215] [PMID]
- Fernández-de Thomas RJ, Munakomi S, De Jesus O. Craniotomy. Treasure Island: StatPearls; 2023. [Link]
- Muñoz M, Acheson AG, Bisbe E, Butcher A, Gómez-Ramírez S, Khalafallah AA, et al. An international consensus statement on the management of postoperative anaemia after major surgical procedures. Anaesthesia. 2018; 73(11):1418-31. [DOI:10.1111/anae.14358] [PMID] [PMCID]
- Alan N, Seicean A, Seicean S, Neuhauser D, Weil RJ. Impact of preoperative anemia on outcomes in patients undergoing elective cranial surgery. Journal of Neurosurgery. 2014; 120(3):764-72. [DOI:10.3171/2013.10.JNS131028] [PMID]
- Xiao Y, Cheng X, Jia L, Tian Y, He J, He M, et al. Preoperative hematocrit levels and postoperative mortality in patients undergoing craniotomy for brain tumors. Frontiers in Oncology. 2023; 13:1246220. [DOI:10.3389/fonc.2023.1246220] [PMID] [PMCID]
- Zhang Y, Jia L, Tian Y, He J, He M, Chen L, et al. Association of postoperative drift in hemoglobin with mortality after brain tumor craniotomy. Neurosurgery. 2023; 93(1):168-75. [DOI:10.1227/neu.0000000000002396] [PMID]
- Seifman MA, Lewis PM, Rosenfeld JV, Hwang PY. Postoperative intracranial haemorrhage: A review. Neurosurgical Review. 2011; 34(4):393-407. [DOI:10.1007/s10143-010-0304-3] [PMID]
- Chughtai KA, Nemer OP, Kessler AT, Bhatt AA. Post-operative complications of craniotomy and craniectomy. Emergency Radiology. 2019; 26(1):99-107. [DOI:10.1007/s10140-018-1647-2] [PMID]
- Goobie SM, Haas T. Bleeding management for pediatric craniotomies and craniofacial surgery. Paediatric Anaesthesia. 2014; 24(7):678-89. [DOI:10.1111/pan.12416] [PMID]
- White JC, Whitelaw GP, Sweet WH, Hurwitt ES. Blood loss in neurosurgical operations. Annals of Surgery. 1938; 107(2):287-97. [DOI:10.1097/00000658-193802000-00012] [PMID] [PMCID]
- Cohen JA, Alan N, Seicean A, Weil RJ. Risk associated with perioperative red blood cell transfusion in cranial surgery. Neurosurgical Review. 2017; 40(4):633-42. [DOI:10.1007/s10143-017-0819-y] [PMID]
- Giribabu P, Karan N, Sriganesh K, Shukla D, Devi BI. Incidence, risk factors and impact of anemia after elective neurosurgery: A retrospective cohort study. World Neurosurgery: X. 2024; 22:100289. [DOI:10.1016/j.wnsx.2024.100289] [PMID] [PMCID]
- Sangtongjaraskul S, Sae-Phua V, Amornfa J, Tuchinda L. Risk factors of intraoperative blood transfusion in pediatric craniotomy for intracranial tumor resection: A 10-year analysis. Journal of Neurosurgery. Pediatrics. 2023; 32(1):115-23. [DOI:10.3171/2023.2.PEDS22535] [PMID]
- Suarez AD, Taicher B, Fuchs H, Marcus J, Vestal M, Homi M, et al. Predictors of blood transfusion for endoscopic assisted craniosynostosis surgery. The Journal of Craniofacial Surgery. 2022; 33(5):1327-30. [DOI:10.1097/SCS.0000000000008441] [PMID]
- Ali Algadiem E, Aleisa AA, Alsubaie HI, Buhlaiqah NR, Algadeeb JB, Alsneini HA. Blood loss estimation using gauze visual analogue. Trauma Monthly. 2016; 21(2):e34131. [DOI:10.5812/traumamon.34131] [PMID] [PMCID]
- Bala M. Estimation of blood loss in oral and maxillofacial surgery. Hamdan Medical Journal. 2023; 16(3):136-9. [DOI:10.4103/hmj.hmj_33_23]
- Kavle JA, Khalfan SS, Stoltzfus RJ, Witter F, Tielsch JM, Caulfield LE. Measurement of blood loss at childbirth and postpartum. International Journal of Gynaecology and Obstetrics. 2006; 95(1):24-8. [DOI:10.1016/j.ijgo.2006.06.010] [PMID]
- Grant MC, Whitman GJ, Savage WJ, Ness PM, Frank SM. Clinical predictors of postoperative hemoglobin drift. Transfusion. 2014; 54(6):1460-8. [DOI:10.1111/trf.12491] [PMID]
- Cappellini MD, Motta I. Anemia in clinical practice-definition and classification: Does hemoglobin change with aging? Seminars in Hematology. 2015; 52(4):261-9. [DOI:10.1053/j.seminhematol.2015.07.006] [PMID]
- Abate Shiferaw A, Negash AY, Tirsit A, Kunapaisal T, Gomez C, Theard MA, et al. Perioperative care and outcomes of patients with brain tumors undergoing elective craniotomy: Experience from an Ethiopian tertiary-care hospital. World Neurosurgery. 2024; 181:e434-46. [DOI:10.1016/j.wneu.2023.10.077] [PMID]
Type of Study: Research |
Subject:
Basic Neurosurgery
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |