Wed, Feb 4, 2026
Volume 10 - Continuous Publishing
Iran J Neurosurg 2024, 10 - Continuous Publishing: 225-228 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Akbulut B B, Bölük M S, Yurtsevewn T, Biçeroğlu H. Rare Presentation of Pilocytic Astrocytoma in the Cerebellar Tonsils of an Adult: A Case Report. Iran J Neurosurg 2024; 10 : 26
URL: http://irjns.org/article-1-440-en.html
URL: http://irjns.org/article-1-440-en.html
1- Department of Neurosurgery, Faculty of Medicine, Ege University, Izmir, Turkey. , b.bahadirakbulut@gmail.com
2- Department of Neurosurgery, Faculty of Medicine, Ege University, Izmir, Turkey.
2- Department of Neurosurgery, Faculty of Medicine, Ege University, Izmir, Turkey.
Full Text [PDF 847 kb]
(522 Downloads)
| Abstract (HTML) (2416 Views)
Full Text: (481 Views)
1. Background and Importance
Low-grade gliomas (LGGs) are World Health Organization (WHO) grade 1 and 2 tumors that are slow-growing tumors arising from glial cells [1]. Pilocytic astrocytomas are the most common virulence of childhood [2], but infratentorial pilocytic astrocytomas are rarely observed in adults [1, 3, 4]. We present a rare case of adult infratentorial pilocytic astrocytoma to add to the literature.
2. Case Presentation
A 31-year-old man presented with a 2-year history of neck pain and progressive numbness in the face and left arm. The patient’s medical history was unremarkable, with no previous surgeries, allergies, or known diseases. Neurological examination upon admission revealed no cranial nerve involvement, motor or sensory deficits, or signs of cerebellar dysfunction.
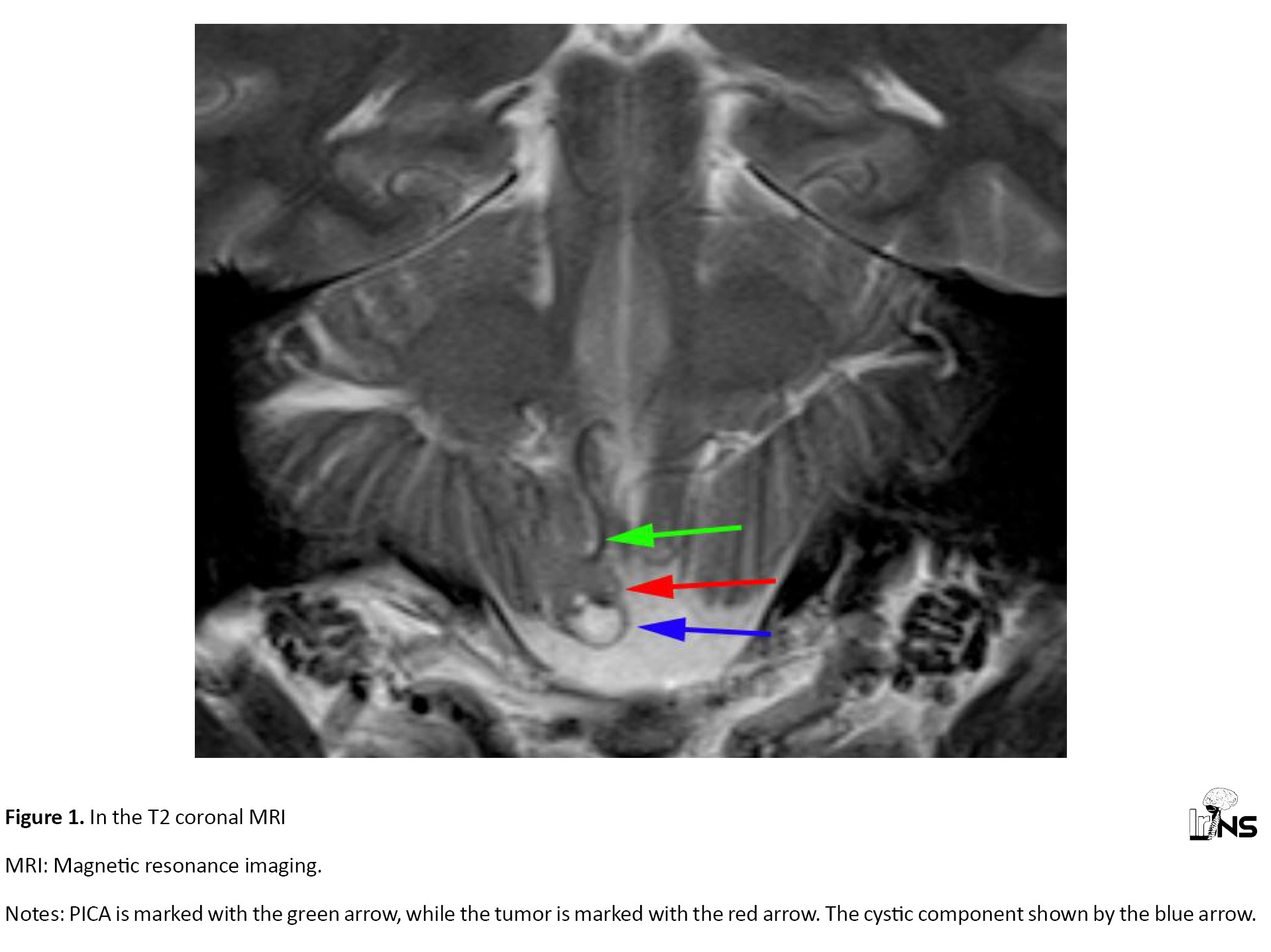
Cranial magnetic resonance imaging (MRI) was obtained, revealing a 2-cm T2 hyperintense lesion with focal cystic components in the right cerebellar tonsil (Figure 1), suggestive of a LGG. No contrast enhancement was observed on T1 gadolinium-enhanced sequences. Perfusion MRI showed no increase in the tumor’s perfusion. A spectroscopy was also obtained, but it was inconclusive due to artifacts caused by tumor adjacency to the bony structures.
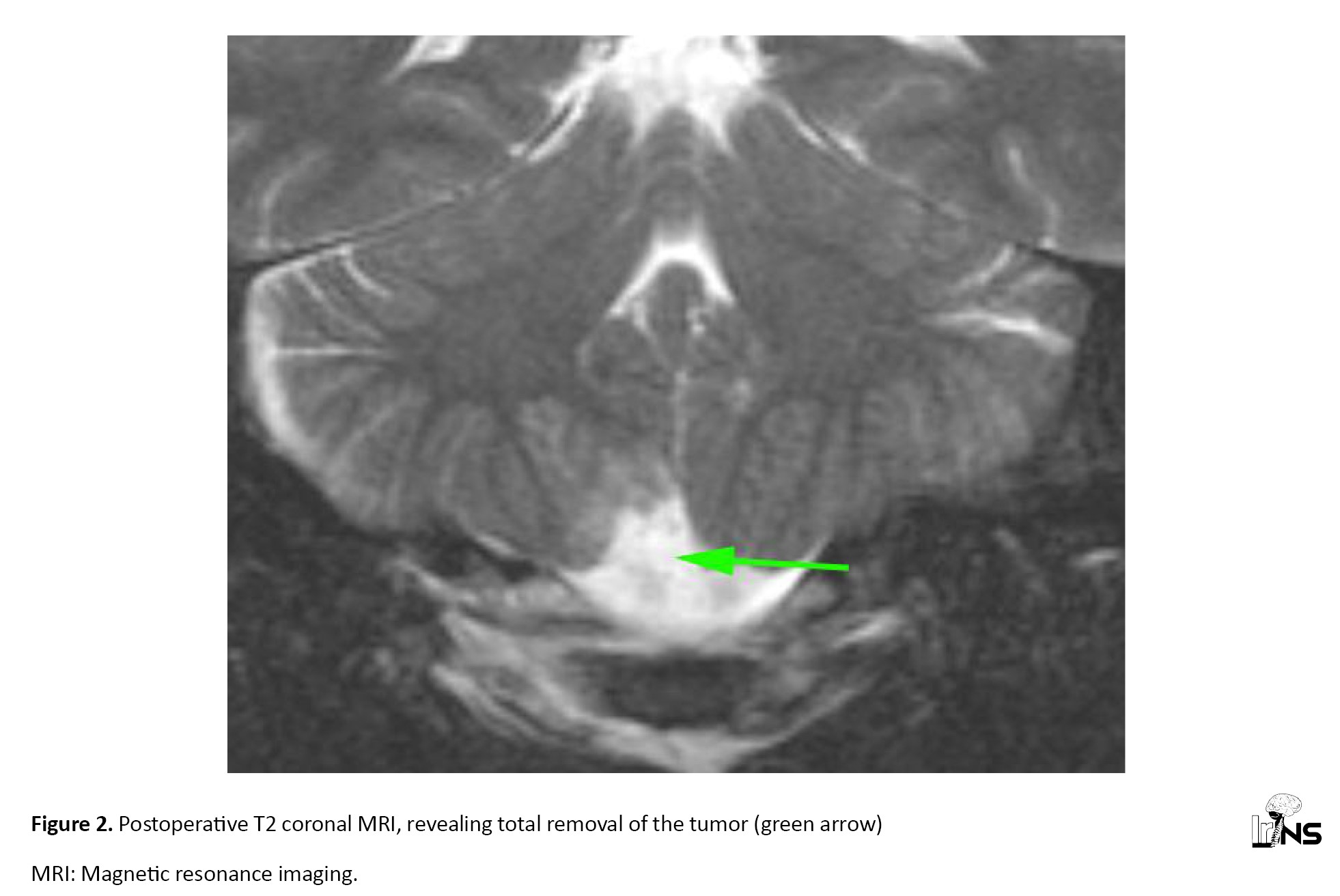
The patient was operated on after informed consent was obtained. In the prone position, a midline incision and suboccipital craniotomy were made. The tumor was removed without any complications and sent to pathology for analysis. Postoperative MRI revealed the removal of the tumor (Figure 2). The patient was discharged four days later without any significant complications.
The tumor on morphological analysis showed areas of dense fibrillary tissue with microcystic spaces in between. The tumor was ATRX loss negative, IDH-1 mutation negative, and synaptophysin negative, confirming the diagnosis of pilocytic astrocytoma. This, along with the absence of p53 mutation, commonly found in higher grade gliomas, and a low Ki-67 labeling index of 1%, suggested a low proliferative potential, consistent with the benign nature of pilocytic astrocytomas.
The patient was discussed on our multidisciplinary tumor board, and since the tumor was totally removed, only follow-up was planned with no adjuvant therapy. The patient is recurrence-free at 1-year follow-up without any symptoms.
3. Discussion
Pilocytic astrocytomas are rare tumors in the adult population, especially in the infratentorial region, with benign histologic features and a favorable prognosis [1, 3, 4]. The absence of IDH-1 mutation and P53 alteration, along with a low Ki-67 index, is typical of a benign tumor, in agreement with the literature, indicating a favorable prognosis for pilocytic astrocytomas [2]. The recurrence-free period at the 1-year follow-up that followed a successful surgical resection without adjuvant therapy demonstrates the potential for favorable outcomes in cases where complete resection is feasible [5, 6, 7].
A multidisciplinary approach is used to manage infratentorial pilocytic astrocytomas in adults. The approach is directed at maximal tumor resection with neurological function preservation. This case contributes to the growing body of evidence concerning the efficacy of surgical treatment in such cases.
4. Conclusion
This case report highlights the uncommon presentation of pilocytic astrocytoma in the cerebellar tonsils of an adult. It stresses the need to consider this diagnosis even in atypical locations. It also demonstrates the effectiveness of surgical treatment in this population.
Ethical Considerations
Compliance with ethical guidelines
This is a retrospective observational case study. The Ege University, Izmir, Turkey. Research Ethics Committee has confirmed that no ethical approval was required. The patient participating in the study provided informed consent for surgery. Consent to participate is not applicable as this is not an experimental study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Hüseyin Biçeroğlu, Mustafa Serdar Bölük, and Taşkın Yurtseven; Data collection: Bilal Bahadır Akbulut, and Mustafa Serdar Bölük; Data analysis and interpretation: Bilal Bahadır Akbulut; Drafting the article: Bilal Bahadır Akbulut, and Mustafa Serdar Bölük; Review and editing; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Low-grade gliomas (LGGs) are World Health Organization (WHO) grade 1 and 2 tumors that are slow-growing tumors arising from glial cells [1]. Pilocytic astrocytomas are the most common virulence of childhood [2], but infratentorial pilocytic astrocytomas are rarely observed in adults [1, 3, 4]. We present a rare case of adult infratentorial pilocytic astrocytoma to add to the literature.
2. Case Presentation
A 31-year-old man presented with a 2-year history of neck pain and progressive numbness in the face and left arm. The patient’s medical history was unremarkable, with no previous surgeries, allergies, or known diseases. Neurological examination upon admission revealed no cranial nerve involvement, motor or sensory deficits, or signs of cerebellar dysfunction.
Cranial magnetic resonance imaging (MRI) was obtained, revealing a 2-cm T2 hyperintense lesion with focal cystic components in the right cerebellar tonsil (Figure 1), suggestive of a LGG. No contrast enhancement was observed on T1 gadolinium-enhanced sequences. Perfusion MRI showed no increase in the tumor’s perfusion. A spectroscopy was also obtained, but it was inconclusive due to artifacts caused by tumor adjacency to the bony structures.
The patient was operated on after informed consent was obtained. In the prone position, a midline incision and suboccipital craniotomy were made. The tumor was removed without any complications and sent to pathology for analysis. Postoperative MRI revealed the removal of the tumor (Figure 2). The patient was discharged four days later without any significant complications.
The tumor on morphological analysis showed areas of dense fibrillary tissue with microcystic spaces in between. The tumor was ATRX loss negative, IDH-1 mutation negative, and synaptophysin negative, confirming the diagnosis of pilocytic astrocytoma. This, along with the absence of p53 mutation, commonly found in higher grade gliomas, and a low Ki-67 labeling index of 1%, suggested a low proliferative potential, consistent with the benign nature of pilocytic astrocytomas.
The patient was discussed on our multidisciplinary tumor board, and since the tumor was totally removed, only follow-up was planned with no adjuvant therapy. The patient is recurrence-free at 1-year follow-up without any symptoms.
3. Discussion
Pilocytic astrocytomas are rare tumors in the adult population, especially in the infratentorial region, with benign histologic features and a favorable prognosis [1, 3, 4]. The absence of IDH-1 mutation and P53 alteration, along with a low Ki-67 index, is typical of a benign tumor, in agreement with the literature, indicating a favorable prognosis for pilocytic astrocytomas [2]. The recurrence-free period at the 1-year follow-up that followed a successful surgical resection without adjuvant therapy demonstrates the potential for favorable outcomes in cases where complete resection is feasible [5, 6, 7].
A multidisciplinary approach is used to manage infratentorial pilocytic astrocytomas in adults. The approach is directed at maximal tumor resection with neurological function preservation. This case contributes to the growing body of evidence concerning the efficacy of surgical treatment in such cases.
4. Conclusion
This case report highlights the uncommon presentation of pilocytic astrocytoma in the cerebellar tonsils of an adult. It stresses the need to consider this diagnosis even in atypical locations. It also demonstrates the effectiveness of surgical treatment in this population.
Ethical Considerations
Compliance with ethical guidelines
This is a retrospective observational case study. The Ege University, Izmir, Turkey. Research Ethics Committee has confirmed that no ethical approval was required. The patient participating in the study provided informed consent for surgery. Consent to participate is not applicable as this is not an experimental study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Hüseyin Biçeroğlu, Mustafa Serdar Bölük, and Taşkın Yurtseven; Data collection: Bilal Bahadır Akbulut, and Mustafa Serdar Bölük; Data analysis and interpretation: Bilal Bahadır Akbulut; Drafting the article: Bilal Bahadır Akbulut, and Mustafa Serdar Bölük; Review and editing; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Acharya S, Lavrador JP, Sekhon PP, Visagan R, Jung J, Gullan R, Vergani F, et al. Low-grade glioma case series: Lessons learned from an evolving 10-year single-institution multidisciplinary team practice. World Neurosurgery. 2021; 151:e47-57. [DOI:10.1016/j.wneu.2021.03.101] [PMID]
- Knight J, Karsonovich T, De Jesus O. Pilocytic astrocytoma. Treasure Island: StatPearls Publishing; 2024. [Link]
- Deacu M, Popescu S, Docu Axelerad A, Topliceanu TS, Aschie M, Bosoteanu M, et al. Prognostic factors of low-grade gliomas in adults. Current Oncology. 2022; 29(10):7327-42. [DOI:10.3390/curroncol29100576] [PMID] [PMCID]
- Schomas DA, Laack NN, Rao RD, Meyer FB, Shaw EG, O'Neill BP, et al. Intracranial low-grade gliomas in adults: 30-year experience with long-term follow-up at Mayo Clinic. Neuro-Oncology. 2009; 11(4):437-45. [DOI:10.1215/15228517-2008-102] [PMID] [PMCID]
- Rossi M, Ambrogi F, Gay L, Gallucci M, Conti Nibali M, Leonetti A, et al. Is supratotal resection achievable in low-grade gliomas? Feasibility, putative factors, safety, and functional outcome. Journal of Neurosurgery. 2019; 132(6):1692-705. [DOI:10.3171/2019.2.JNS183408] [PMID]
- Duffau H. Long-term outcomes after supratotal resection of diffuse low-grade gliomas: A consecutive series with 11-year follow-up. Acta Neurochirurgica. 2016; 158(1):51-8. [DOI:10.1007/s00701-015-2621-3] [PMID]
- Brown TJ, Bota DA, van Den Bent MJ, Brown PD, Maher E, Aregawi D, et al. Management of low-grade glioma: A systematic review and meta-analysis. Neuro-Oncology Practice. 2019; 6(4):249-58. [DOI:10.1093/nop/npy034] [PMID] [PMCID]
Type of Study: Case report |
Subject:
Brain Tumors
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |