Wed, Jan 28, 2026
Volume 11 - Continuous Publishing
Iran J Neurosurg 2025, 11 - Continuous Publishing: 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Thavara B D, Parambil R M, Jose B V, Sasi P K, Cholakkal S, Sebastian E et al . A Rare Case of Multiple Wasp Stings Causing Bilateral Ischemic Stroke. Iran J Neurosurg 2025; 11 : 8
URL: http://irjns.org/article-1-444-en.html
URL: http://irjns.org/article-1-444-en.html
Binoy Damodar Thavara1 

 , Rajeev Mandaka Parambil *1
, Rajeev Mandaka Parambil *1 

 , Byjo Valiyaveetil Jose1
, Byjo Valiyaveetil Jose1 

 , Prem kumar Sasi1
, Prem kumar Sasi1 

 , Shanavas Cholakkal1
, Shanavas Cholakkal1 

 , Ebby Sebastian1
, Ebby Sebastian1 

 , Atul Kale Keshavrao1
, Atul Kale Keshavrao1 




 , Rajeev Mandaka Parambil *1
, Rajeev Mandaka Parambil *1 

 , Byjo Valiyaveetil Jose1
, Byjo Valiyaveetil Jose1 

 , Prem kumar Sasi1
, Prem kumar Sasi1 

 , Shanavas Cholakkal1
, Shanavas Cholakkal1 

 , Ebby Sebastian1
, Ebby Sebastian1 

 , Atul Kale Keshavrao1
, Atul Kale Keshavrao1 


1- Department of Neurosurgery, Government Medical College, Kozhikode, India.
Full Text [PDF 2022 kb]
(1183 Downloads)
| Abstract (HTML) (3043 Views)
Full Text: (1038 Views)
1. Background and Importance
Honeybees and wasps are hymenopterans. Only 19 cases of wasp stings causing proven ischemic stroke have been reported.
Local reactions due to wasps and bee stings are self-limiting and settle within a few hours. Multiple stings can lead to vomiting, diarrhea, dyspnea, generalized edema, hypotension, syncope, acute renal failure, and death. Rarely, they cause vasculitis, serum sickness, neuritis, or encephalitis. Wani et al. reported a case of multiple wasp stings causing right hemiparesis. Magnetic resonance imaging (MRI) revealed multiple bilateral infarcts. Patient was discharged in a vegetative state on oral steroids and antibiotics [1]. Cerebral infarction in wasp stings could be due to vasculitis, hypoperfusion, retrograde stimulation of the superior cervical ganglion, coagulopathy, or vasospasm. However, the exact pathophysiology is unknown [2].
The authors reported a rare case of bilateral ischemic stroke due to multiple wasp stings that led to increased brain edema and required decompressive craniectomy to reduce intracranial pressure.
2. Case Presentation
A 49-year-old man presented with multiple (>50) wasp stings (Figure 1) all over the body at 8.30 AM. The patient developed a loss of consciousness (LOC) due to an anaphylactic reaction. Bite marks were considered for the face, trunk, and limbs. The patient was treated with antihistaminic and steroid medications. The patient regained consciousness without any neurological deficits and returned home. At 8 PM, he was brought back due to LOC and right hemiparesis.
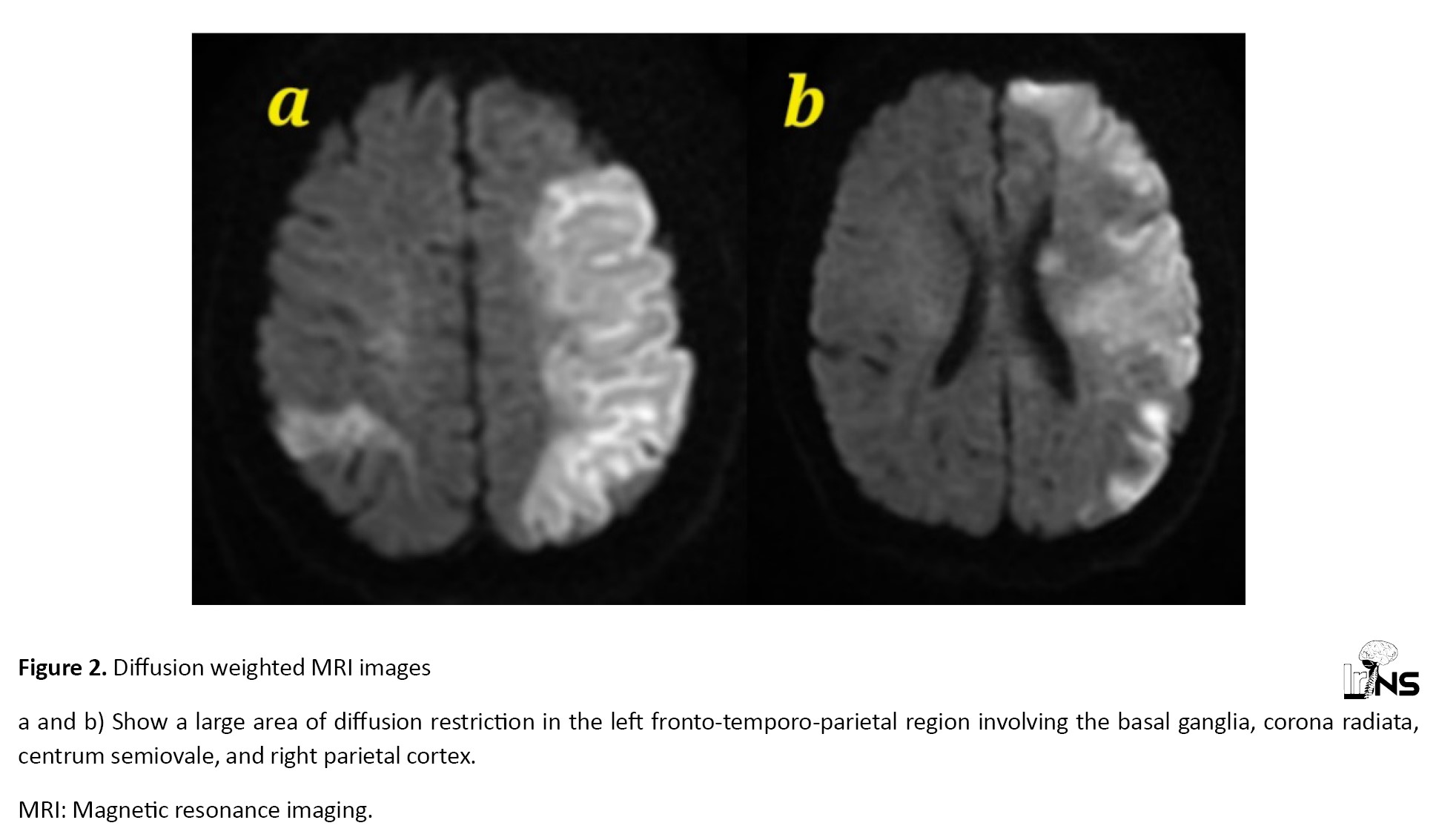
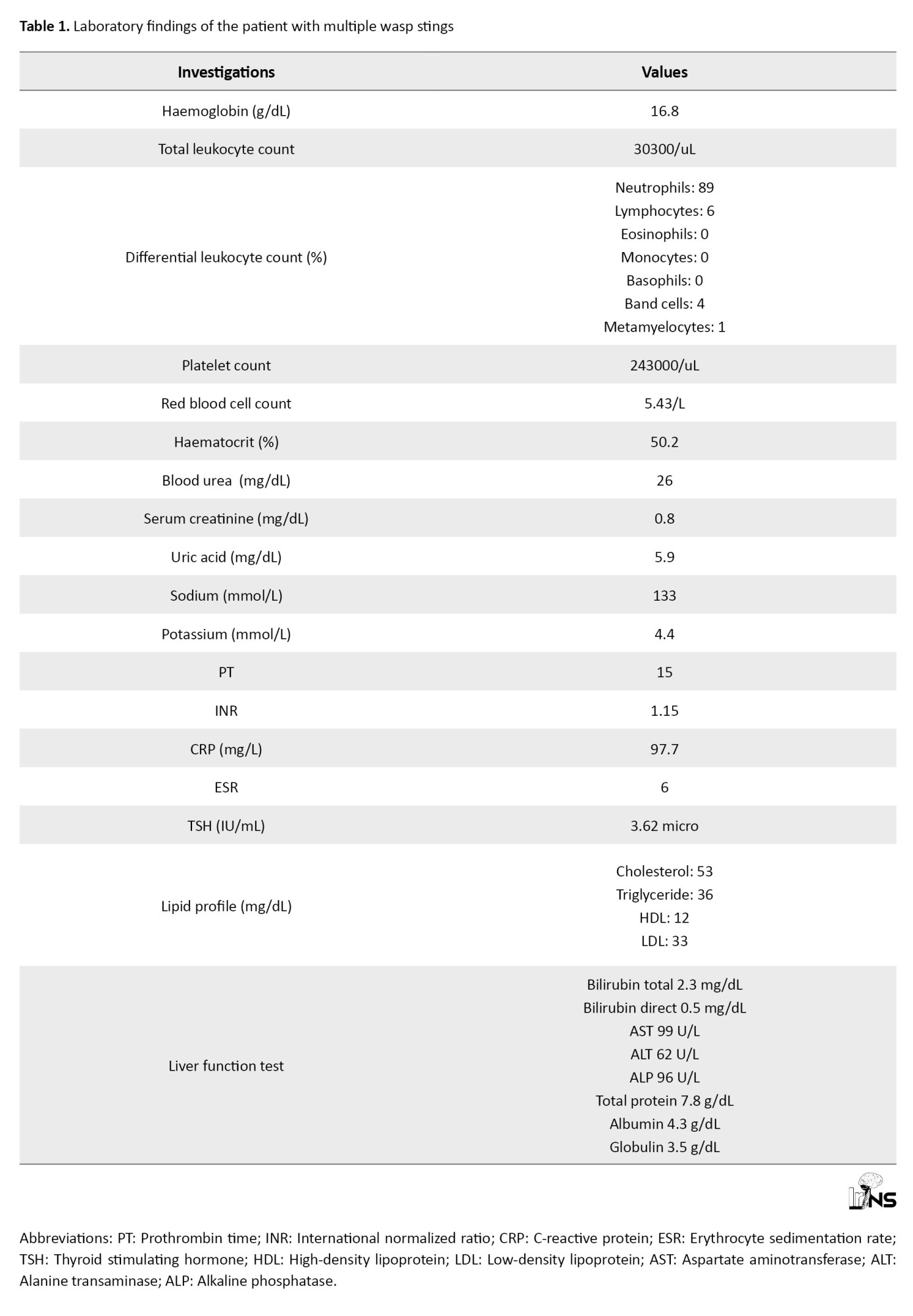
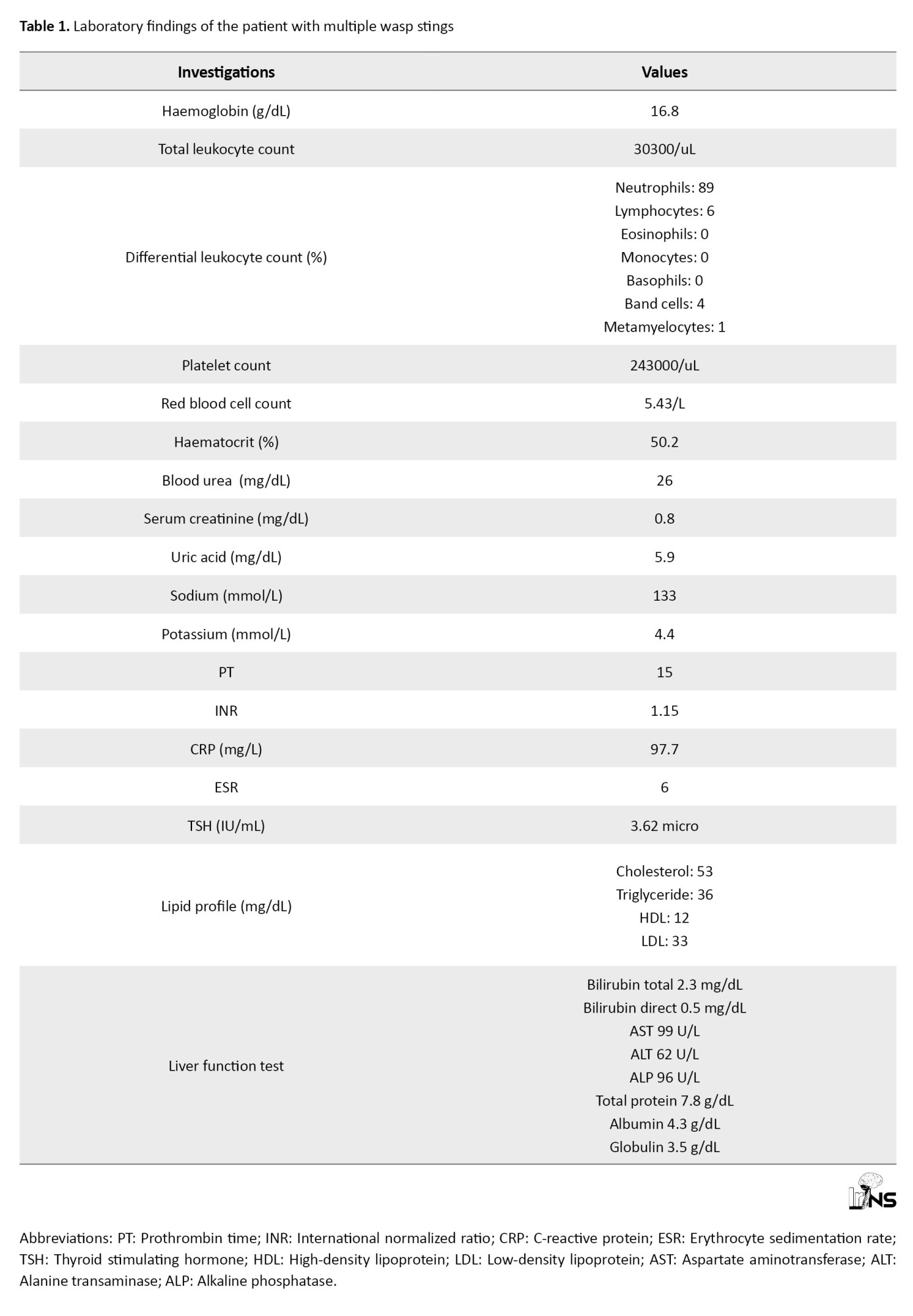
MRI of the brain taken at 10.15 PM revealed a large area of diffusion restriction in the left front-temporal-parietal region involving basal ganglia, corona radiata, centrum semiovale, and in the right parietal cortex (Figure 2). He had a Glasgow coma scale (GCS) score of E1V1M5 (E-Eye, V-Verbal, M-Motor), bilateral equal reacting pupil, and right hemiparesis with Medical Research Council (MRC) grade 1 power. His pulse rate was 88/minute, his blood pressure (BP) 180/100 mm Hg, and he was afebrile. The patient was intubated and ventilated with a low GCS score. MR angiogram taken at 1.20 AM the next day revealed luminal narrowing of the distal segment of bilateral common carotid arteries (CCA) and bilateral cervical internal cerebral artery (ICA) (Figure 3), along with attenuated cortical branches of bilateral middle cerebral arteries (MCAs). Cardiological evaluation using echocardiography revealed no abnormalities. Table 1 presents blood parameters.
The patient was a non-smoker and had no comorbidities. No history of wasps or bee stings was observed. The patient was treated with antiplatelet agents, antibiotics, steroids, antiepileptics, anti-edema measures, and ventilation. Computed tomography (CT) scan taken at 11.40 AM showed significant increase in brain oedema with midline shift to right side (Figure 4). The patient underwent a left fronto-temporoparietal decompressive craniectomy. The dura was opened, and duraplasty was performed using the pericranium. Antihypertensives were started owing to increased BP. The patient underwent tracheostomy on postoperative day (POD) 4 and was weaned off the ventilator. His GCS score was E2VtM5, pupils were bilaterally reactive, and he had right hemiparesis. Multiple wasp stings and edema of the upper limbs were noted (Figure 5). A Venous Doppler study did not reveal any deep vein thrombosis in the upper limbs. Arterial Doppler showed normal blood flow patterns in both the upper limb arteries. A CT scan obtained on POD 13 showed left-sided craniectomy decreased brain edema, and multiple infarcts (Figure 6). The patient’s condition gradually improved, and he started obeying commands on POD 14. The tracheostomy was closed, and the patient was discharged on POD 17. He underwent cranioplasty after 5 months, during which his GCS score was E4V4M6, right upper limb power was MRC grade 2, and right lower limb power improved to MRC grade 4. No weakness was observed in the left upper or lower limbs.
3. Discussion
Wasps, bees, and hornets belong to the order of insects called “Hymenoptera”. Millions of Hymenoptera stings occur annually. They usually cause local inflammatory reactions and, less commonly, severe systemic allergic reactions [3]. Local reactions include itching, swelling of lips, and urticaria [4]. Systemic reactions include hypotension or anaphylactic shock, generalized edema, respiratory failure, or even multiple organ failures. Neurological complications, including stroke, are rare [3].
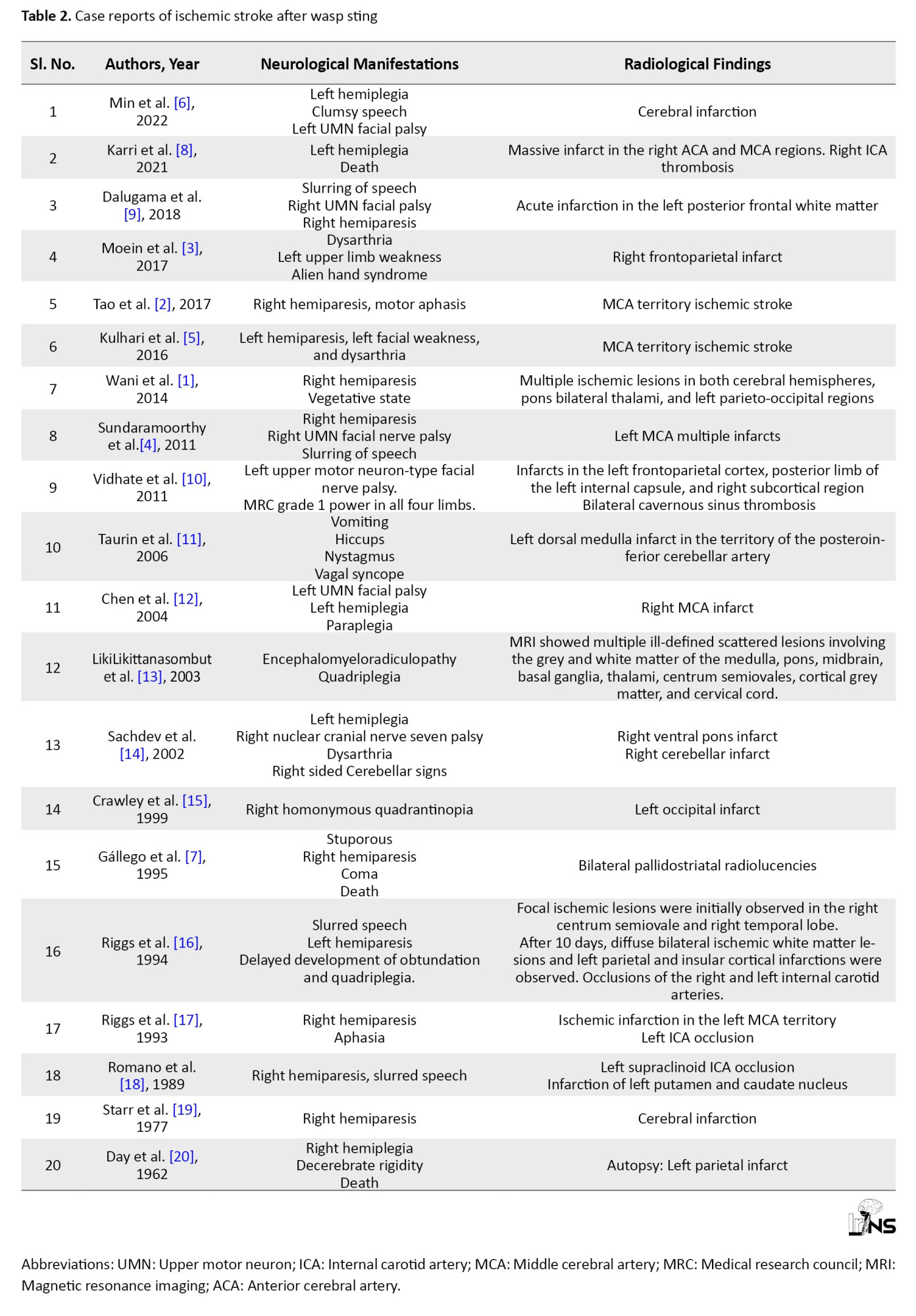
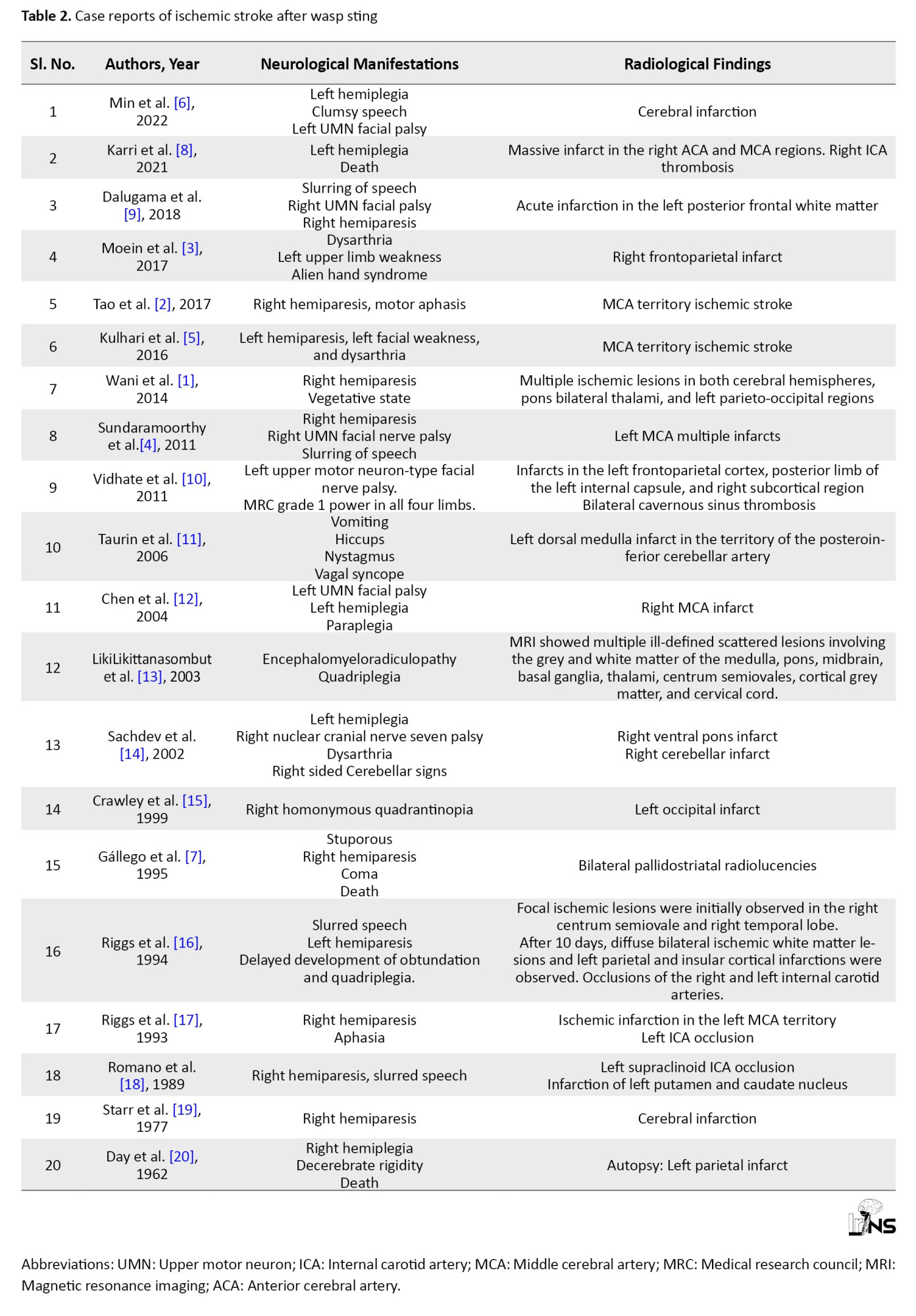
Wasp sting can present with sudden onset hemiparesis, facial weakness, and dysarthria due to MCA territory infarct. Serum wasp immunoglobulin E may be raised in such cases [5]. Min et al. reported a patient with wasp stings on his head and right shoulder. He developed left-sided hemiplegia, clumsy speech, and left facial droop due to acute progressive cerebral infarction. However, magnetic resonance angiography (MRA) showed normal blood vessels. Venom-induced vasospasm was suspected in this case [6]. Sundaramoorthy et al. reported a case of left MCA infarcts due to multiple wasp stings (about 40 to 50 wasps). He had 4-5 episodes of wasp stings in the past. However, no history of reactions from previous wasp stings was observed. Larger venom dose of multiple wasp stings was considered as the cause in this case [4]. A patient developed right hemiparesis and acute encephalopathy with coma after a single wasp sting. The patient died 72 h after the wasp sting. An autopsy revealed bilateral pallidostriatal necrosis and diffuse neuronal damage in the frontal, temporal, and parietal cortices. This occurred due to the neurotoxic effect of the poison and hypersensitivity [7]. A 40-year-old male presented with left hemiplegia after 6 hours of massive wasp stings. MRI showed right internal carotid artery (ICA) thrombosis causing massive infarct in anterior cerebral artery (ACA) and MCA territory [8]. In the authors’ case, larger venom dose of multiple wasp stings and luminal narrowing of carotid arteries, along with attenuated cortical branches of bilateral MCAs, are the causes of bilateral cerebral infarcts in their case. Table 2 describes the previously published cases of ischemic stroke after wasp sting.”
The mechanism underlying the neurotoxic effects of wasp stings remains unclear. Some authors believed that the mechanism of stroke was cerebral vasoconstriction caused by the vasoactive peptides [5]. Others suggested that venom had induced vasospasm and stimulated the superior cervical sympathetic ganglion, leading to cerebral infarction [6]. Sundaramoorthy et al. considered that severe reactions, such as cerebral infarcts, occur due to the larger volume of venom of multiple wasp stings [4]. However, Gállego et al. noted that a single wasp sting can cause neurotoxic effects and hypersensitivity, leading to encephalopathy and death [7].
Management starts with the stabilization of the airway, breathing, and circulation. Antihistamines, steroids, and epinephrine have been used to control allergic responses. No guidelines are available for the management of ischemic stroke after wasp stings due to the limited number of cases. Intravenous tissue plasminogen activator showed good outcomes in one report. To prevent cerebral vasoconstriction, the intravascular volume and hemodynamic status should be closely monitored. Aggressive BP augmentation and fluid resuscitation is crucial in these patients [5].
4. Conclusion
Multiple wasp stings can cause bilateral cerebral infarctions. Even if the initial symptoms are insignificant, wasp stings require close monitoring. Public and healthcare personnel awareness of wasp-sting complications is crucial. Multiple wasp stings causing a large ischemic insult to the brain can cause increased brain edema and require decompressive craniectomy to save the patient. Early radiological evaluation of suspicious cases and prompt medical and surgical intervention are key to the successful treatment of cerebral infarction due to wasp sting.
Ethical Considerations
Compliance with ethical guidelines
Informed consent was obtained from the patient.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization or design of the work: Binoy Damodar Thavara and Rajeev Mandaka Parambil; Data collection: Binoy Damodar Thavara, Prem Kumar Sasi, and Atul Kale Keshavrao; Data analysis and interpretation: Binoy Damodar Thavara, Byjo Valiyaveetil Jose, and Ebby Sebastian; Drafting the article: Binoy Damodar Thavara, Rajeev Mandaka Parambil, and Byjo Valiyaveetil Jose; Critical revision of the article: Rajeev Mandaka Parambil, Binoy Damodar Thavara, and Shanavas Cholakkal; Study supervision: Rajeev Mandaka Parambil; Review of results and approval of the final version of the manuscript: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors gratefully acknowledge the support of the Department of Neurosurgery, Government Medical College, Kozhikode, India.
References
Honeybees and wasps are hymenopterans. Only 19 cases of wasp stings causing proven ischemic stroke have been reported.
Local reactions due to wasps and bee stings are self-limiting and settle within a few hours. Multiple stings can lead to vomiting, diarrhea, dyspnea, generalized edema, hypotension, syncope, acute renal failure, and death. Rarely, they cause vasculitis, serum sickness, neuritis, or encephalitis. Wani et al. reported a case of multiple wasp stings causing right hemiparesis. Magnetic resonance imaging (MRI) revealed multiple bilateral infarcts. Patient was discharged in a vegetative state on oral steroids and antibiotics [1]. Cerebral infarction in wasp stings could be due to vasculitis, hypoperfusion, retrograde stimulation of the superior cervical ganglion, coagulopathy, or vasospasm. However, the exact pathophysiology is unknown [2].
The authors reported a rare case of bilateral ischemic stroke due to multiple wasp stings that led to increased brain edema and required decompressive craniectomy to reduce intracranial pressure.
2. Case Presentation
A 49-year-old man presented with multiple (>50) wasp stings (Figure 1) all over the body at 8.30 AM. The patient developed a loss of consciousness (LOC) due to an anaphylactic reaction. Bite marks were considered for the face, trunk, and limbs. The patient was treated with antihistaminic and steroid medications. The patient regained consciousness without any neurological deficits and returned home. At 8 PM, he was brought back due to LOC and right hemiparesis.
MRI of the brain taken at 10.15 PM revealed a large area of diffusion restriction in the left front-temporal-parietal region involving basal ganglia, corona radiata, centrum semiovale, and in the right parietal cortex (Figure 2). He had a Glasgow coma scale (GCS) score of E1V1M5 (E-Eye, V-Verbal, M-Motor), bilateral equal reacting pupil, and right hemiparesis with Medical Research Council (MRC) grade 1 power. His pulse rate was 88/minute, his blood pressure (BP) 180/100 mm Hg, and he was afebrile. The patient was intubated and ventilated with a low GCS score. MR angiogram taken at 1.20 AM the next day revealed luminal narrowing of the distal segment of bilateral common carotid arteries (CCA) and bilateral cervical internal cerebral artery (ICA) (Figure 3), along with attenuated cortical branches of bilateral middle cerebral arteries (MCAs). Cardiological evaluation using echocardiography revealed no abnormalities. Table 1 presents blood parameters.
The patient was a non-smoker and had no comorbidities. No history of wasps or bee stings was observed. The patient was treated with antiplatelet agents, antibiotics, steroids, antiepileptics, anti-edema measures, and ventilation. Computed tomography (CT) scan taken at 11.40 AM showed significant increase in brain oedema with midline shift to right side (Figure 4). The patient underwent a left fronto-temporoparietal decompressive craniectomy. The dura was opened, and duraplasty was performed using the pericranium. Antihypertensives were started owing to increased BP. The patient underwent tracheostomy on postoperative day (POD) 4 and was weaned off the ventilator. His GCS score was E2VtM5, pupils were bilaterally reactive, and he had right hemiparesis. Multiple wasp stings and edema of the upper limbs were noted (Figure 5). A Venous Doppler study did not reveal any deep vein thrombosis in the upper limbs. Arterial Doppler showed normal blood flow patterns in both the upper limb arteries. A CT scan obtained on POD 13 showed left-sided craniectomy decreased brain edema, and multiple infarcts (Figure 6). The patient’s condition gradually improved, and he started obeying commands on POD 14. The tracheostomy was closed, and the patient was discharged on POD 17. He underwent cranioplasty after 5 months, during which his GCS score was E4V4M6, right upper limb power was MRC grade 2, and right lower limb power improved to MRC grade 4. No weakness was observed in the left upper or lower limbs.
3. Discussion
Wasps, bees, and hornets belong to the order of insects called “Hymenoptera”. Millions of Hymenoptera stings occur annually. They usually cause local inflammatory reactions and, less commonly, severe systemic allergic reactions [3]. Local reactions include itching, swelling of lips, and urticaria [4]. Systemic reactions include hypotension or anaphylactic shock, generalized edema, respiratory failure, or even multiple organ failures. Neurological complications, including stroke, are rare [3].
Wasp sting can present with sudden onset hemiparesis, facial weakness, and dysarthria due to MCA territory infarct. Serum wasp immunoglobulin E may be raised in such cases [5]. Min et al. reported a patient with wasp stings on his head and right shoulder. He developed left-sided hemiplegia, clumsy speech, and left facial droop due to acute progressive cerebral infarction. However, magnetic resonance angiography (MRA) showed normal blood vessels. Venom-induced vasospasm was suspected in this case [6]. Sundaramoorthy et al. reported a case of left MCA infarcts due to multiple wasp stings (about 40 to 50 wasps). He had 4-5 episodes of wasp stings in the past. However, no history of reactions from previous wasp stings was observed. Larger venom dose of multiple wasp stings was considered as the cause in this case [4]. A patient developed right hemiparesis and acute encephalopathy with coma after a single wasp sting. The patient died 72 h after the wasp sting. An autopsy revealed bilateral pallidostriatal necrosis and diffuse neuronal damage in the frontal, temporal, and parietal cortices. This occurred due to the neurotoxic effect of the poison and hypersensitivity [7]. A 40-year-old male presented with left hemiplegia after 6 hours of massive wasp stings. MRI showed right internal carotid artery (ICA) thrombosis causing massive infarct in anterior cerebral artery (ACA) and MCA territory [8]. In the authors’ case, larger venom dose of multiple wasp stings and luminal narrowing of carotid arteries, along with attenuated cortical branches of bilateral MCAs, are the causes of bilateral cerebral infarcts in their case. Table 2 describes the previously published cases of ischemic stroke after wasp sting.”
The mechanism underlying the neurotoxic effects of wasp stings remains unclear. Some authors believed that the mechanism of stroke was cerebral vasoconstriction caused by the vasoactive peptides [5]. Others suggested that venom had induced vasospasm and stimulated the superior cervical sympathetic ganglion, leading to cerebral infarction [6]. Sundaramoorthy et al. considered that severe reactions, such as cerebral infarcts, occur due to the larger volume of venom of multiple wasp stings [4]. However, Gállego et al. noted that a single wasp sting can cause neurotoxic effects and hypersensitivity, leading to encephalopathy and death [7].
Management starts with the stabilization of the airway, breathing, and circulation. Antihistamines, steroids, and epinephrine have been used to control allergic responses. No guidelines are available for the management of ischemic stroke after wasp stings due to the limited number of cases. Intravenous tissue plasminogen activator showed good outcomes in one report. To prevent cerebral vasoconstriction, the intravascular volume and hemodynamic status should be closely monitored. Aggressive BP augmentation and fluid resuscitation is crucial in these patients [5].
4. Conclusion
Multiple wasp stings can cause bilateral cerebral infarctions. Even if the initial symptoms are insignificant, wasp stings require close monitoring. Public and healthcare personnel awareness of wasp-sting complications is crucial. Multiple wasp stings causing a large ischemic insult to the brain can cause increased brain edema and require decompressive craniectomy to save the patient. Early radiological evaluation of suspicious cases and prompt medical and surgical intervention are key to the successful treatment of cerebral infarction due to wasp sting.
Ethical Considerations
Compliance with ethical guidelines
Informed consent was obtained from the patient.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization or design of the work: Binoy Damodar Thavara and Rajeev Mandaka Parambil; Data collection: Binoy Damodar Thavara, Prem Kumar Sasi, and Atul Kale Keshavrao; Data analysis and interpretation: Binoy Damodar Thavara, Byjo Valiyaveetil Jose, and Ebby Sebastian; Drafting the article: Binoy Damodar Thavara, Rajeev Mandaka Parambil, and Byjo Valiyaveetil Jose; Critical revision of the article: Rajeev Mandaka Parambil, Binoy Damodar Thavara, and Shanavas Cholakkal; Study supervision: Rajeev Mandaka Parambil; Review of results and approval of the final version of the manuscript: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors gratefully acknowledge the support of the Department of Neurosurgery, Government Medical College, Kozhikode, India.
References
- Wani M, Saleem S, Verma S, Yousuf I, Wani M, Asimi R, et al. Multiple cerebral infarctions with severe multi-organ dysfunction following multiple wasp stings. Annals of Indian Academy of Neurology. 2014; 17(1):125-7. [DOI:10.4103/0972-2327.128581] [PMID]
- Tao X, Huang L, Fang C, Liu C, Qing L, Cai H. Ischemic stroke due to wasp sting: A case report. Clinical Toxicology. 2017; 55(7):682-3. [DOI:10.1080/15563650.2017.1306072] [PMID]
- Moein P, Zand R. Cerebral infarction as a rare complication of Wasp sting. Journal of Vascular and Interventional Neurology. 2017; 9(4):13-6. [PMID][PMCID]
- Sundaramoorthy K, Viswanathan S, Arulneyam J. Wasp stings-related cerebral infarction in a toddy tapper with multiple previous stings. European Neurological Journal. 2011; 18:1-3. [Link]
- Kulhari A, Rogers A, Wang H, Kumaraswamy VM, Xiong W, DeGeorgia M. Ischemic stroke after Wasp sting. The Journal of Emergency Medicine. 2016; 51(4):405-10. [DOI:10.1016/j.jemermed.2016.06.016] [PMID]
- Min L, Wenning Z, Wei W, Wei T. Acute progressive large-area cerebral infarction caused by wasp sting: A case report. Neurocase. 2022; 28(4):364-8. [DOI:10.1080/13554794.2022.2129027]
- Gállego J, Tuñón T, Soriano G, Delgado G, Lacruz F, Villanueva JA. Bilateral pallidostriatal necrosis caused by a wasp sting: a clinical and pathological study. Journal of neurology, neurosurgery, and psychiatry. 1995; 58(4):474-6. [DOI:10.1136/jnnp.58.4.474] [PMID]
- Karri M, Ramasamy B, Perumal S, Kannan KT. Wasp sting - causing a fatal menace. Brain circulation. 2021; 7(2):132-4. [DOI:10.4103/bc.bc_33_20] [PMID]
- Dalugama C, Gawarammana IB. Ischemic stroke following a wasp sting - a rare complication: A case report. Journal of Medical Case Reports. 2018; 12(1):294. [DOI:10.1186/s13256-018-1839-0] [PMID]
- Vidhate MR, Sharma P, Verma R, Yadav R. Bilateral cavernous sinus syndrome and bilateral cerebral infarcts: A rare combination after wasp sting. Journal of the neurological Sciences. 2011; 301(1-2):104-6. [DOI:10.1016/j.jns.2010.10.020] [PMID]
- Taurin G, Canneva-Bourel ML, Delafosse JM, Poirier J, Merienne M. [Dorsal medulla oblongata stroke after a wasp sting (French)]. Revue Neurologique. 2006; 162(3):371-3. [DOI:10.1016/S0035-3787(06)75024-X] [PMID]
- Chen DM, Lee PT, Chou KJ, Fang HC, Chung HM, Chen DM, et al. Descending aortic thrombosis and cerebral infarction after massive wasp stings. The American journal of medicine. 2004; 116(8):567-9. [DOI:10.1016/j.amjmed.2003.08.036] [PMID]
- LikiLikittanasombut P, Witoonpanich R, Viranuvatti K. Encephalomyeloradiculopathy associated with wasp sting. Journal of Neurology, Neurosurgery, and Psychiatry. 2003; 74(1):134-5. [DOI:10.1136/jnnp.74.1.134-a] [PMID]
- Sachdev A, Mahapatra M, D'Cruz S, Kumar A, Singh R, Lehl SS. Wasp sting induced neurological manifestations. Neurology India. 2002; 50(3):319-21. [PMID]
- Crawley F, Schon F, Brown MM. Cerebral infarction: a rare complication of wasp sting. Journal of Neurology, Neurosurgery, and Psychiatry. 1999; 66(4):550-1. [DOI:10.1136/jnnp.66.4.550] [PMID]
- Riggs JE, Ketonen LM, Wymer JP, Barbano RL, Valanne LK, Bodensteiner JB. Acute and delayed cerebral infarction after wasp sting anaphylaxis. Clinical Neuropharmacology. 1994; 17(4):384-8. [DOI:10.1097/00002826-199408000-00011] [PMID]
- Riggs JE, Ketonen LM, Bodensteiner JB, Benesch CG. Wasp sting-associated cerebral infarction: a role for cerebrovascular sympathetic innervation. Clinical Neuropharmacology. 1993; 16(4):362-5. [DOI:10.1097/00002826-199308000-00009] [PMID]
- Romano JT, Riggs JE, Bodensteiner JB, Gutmann L. Wasp sting-associated occlusion of the supraclinoid internal carotid artery: implications regarding the pathogenesis of moyamoya syndrome. Archives of Neurology. 1989; 46(6):607-8. [DOI:10.1001/archneur.1989.00520420025018] [PMID]
- Starr JC, Brasher GW. Wasp sting anaphylaxis with cerebral infarction. Annals of allergy. 1977; 39(6):431-3. [PMID]
- Day JM. Death due to cerebral infarction after wasp stings. Archives of Neurology. 1962; 7:184-6. [DOI:10.1001/archneur.1962.04210030022003] [PMID]
Type of Study: Case report |
Subject:
Basic Neurosurgery
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |