Thu, Jan 29, 2026
Volume 11 - Continuous Publishing
Iran J Neurosurg 2025, 11 - Continuous Publishing: 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Akhbari M, Akbulut B B, Bölük M S, Yurtseven T, Biçeroğlu H. Endoscopic Endonasal Management of Cavernous Sinus Hemangioma: A Case Report. Iran J Neurosurg 2025; 11 : 15
URL: http://irjns.org/article-1-480-en.html
URL: http://irjns.org/article-1-480-en.html
Matin Akhbari *1 

 , Bilal Bahadır Akbulut2
, Bilal Bahadır Akbulut2 

 , Mustafa Serdar Bölük2
, Mustafa Serdar Bölük2 

 , Taşkın Yurtseven2
, Taşkın Yurtseven2 

 , Hüseyin Biçeroğlu2
, Hüseyin Biçeroğlu2 




 , Bilal Bahadır Akbulut2
, Bilal Bahadır Akbulut2 

 , Mustafa Serdar Bölük2
, Mustafa Serdar Bölük2 

 , Taşkın Yurtseven2
, Taşkın Yurtseven2 

 , Hüseyin Biçeroğlu2
, Hüseyin Biçeroğlu2 


1- Department of Neurosurgery, Faculty of Medicine, Ege University Izmir, Turkey. , mat.akhbari@gmail.com
2- Department of Neurosurgery, Faculty of Medicine, Ege University Izmir, Turkey.
2- Department of Neurosurgery, Faculty of Medicine, Ege University Izmir, Turkey.
Full Text [PDF 1156 kb]
(295 Downloads)
| Abstract (HTML) (1080 Views)
Full Text: (199 Views)
Background and Importance
Cavernous sinus hemangiomas (CSH) are rare vascular lesions accounting for approximately 3% of all benign tumors within the cavernous sinus [1]. These lesions are clinically significant due to their proximity to critical neurovascular structures, which often result in symptoms, such as headaches, visual disturbances, and cranial nerve palsies [2].
The management of these tumors is also complex, with options including surgical resection, radiosurgery, and adjuvant therapies. Surgical intervention carries a high risk of intraoperative bleeding and postoperative complications due to the vascular nature of the tumor [3]. However, in the last decades, endoscopic techniques (ET) have emerged as one of the surgical methods for resecting CSH, offering a less invasive approach with promising outcomes [4].
This report aims to present a case of CSH, highlighting the diagnostic challenges and treatment considerations involved.
Case Presentation
A 56-year-old female presented with a 3-month headache and blurred vision to our neurosurgery department. She had no previous surgeries, allergies, or known diseases.
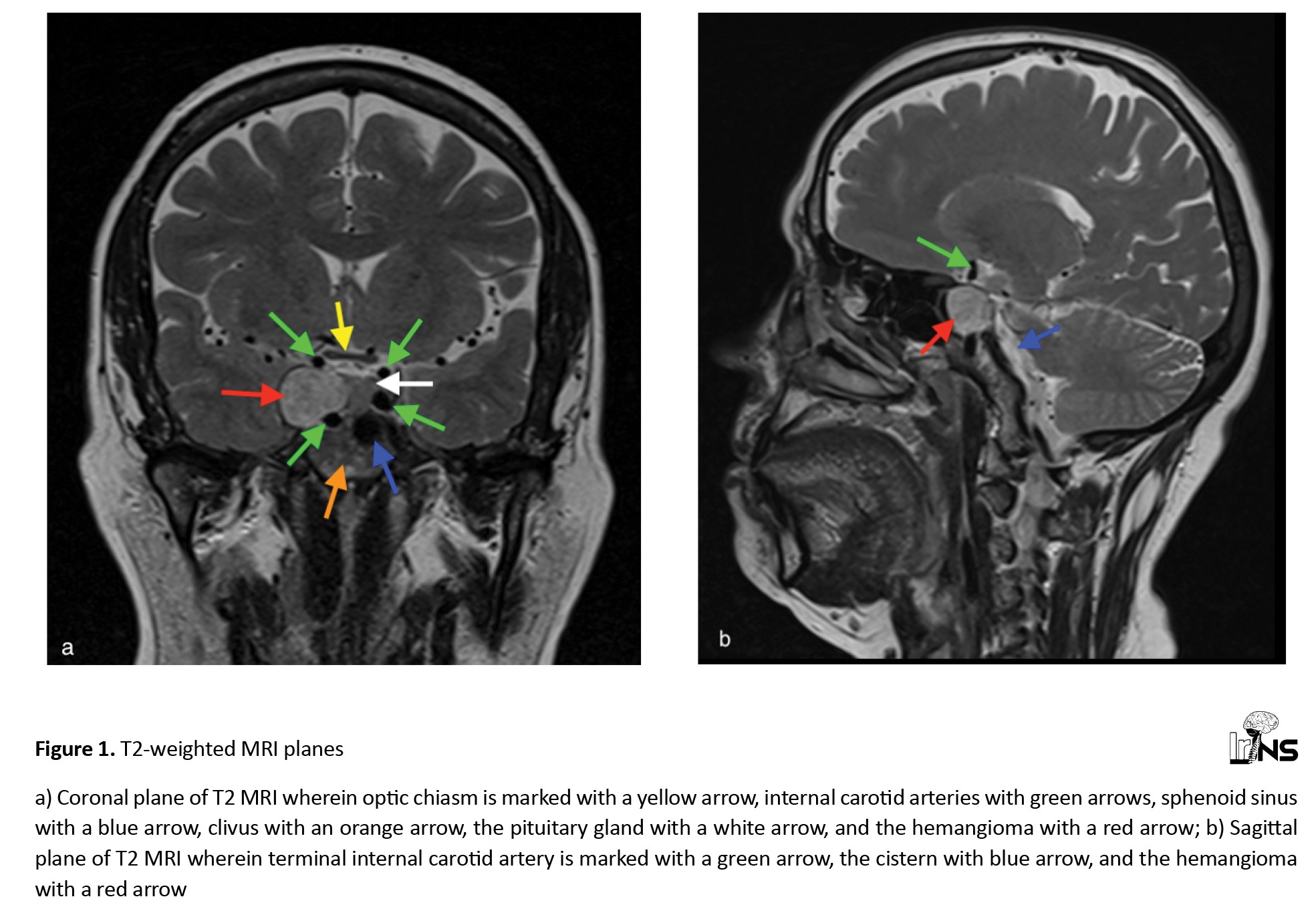
Neurological examination upon admission revealed no cranial nerve involvement, motor or sensory deficits, or other vision disturbances. A cranial magnetic resonance imaging (MRI) was obtained, revealing an 18×16×20 mm T2 hyperintense lesion in the cavernous sinus (Figure 1).
Cavernous sinus hemangiomas (CSH) are rare vascular lesions accounting for approximately 3% of all benign tumors within the cavernous sinus [1]. These lesions are clinically significant due to their proximity to critical neurovascular structures, which often result in symptoms, such as headaches, visual disturbances, and cranial nerve palsies [2].
The management of these tumors is also complex, with options including surgical resection, radiosurgery, and adjuvant therapies. Surgical intervention carries a high risk of intraoperative bleeding and postoperative complications due to the vascular nature of the tumor [3]. However, in the last decades, endoscopic techniques (ET) have emerged as one of the surgical methods for resecting CSH, offering a less invasive approach with promising outcomes [4].
This report aims to present a case of CSH, highlighting the diagnostic challenges and treatment considerations involved.
Case Presentation
A 56-year-old female presented with a 3-month headache and blurred vision to our neurosurgery department. She had no previous surgeries, allergies, or known diseases.
Neurological examination upon admission revealed no cranial nerve involvement, motor or sensory deficits, or other vision disturbances. A cranial magnetic resonance imaging (MRI) was obtained, revealing an 18×16×20 mm T2 hyperintense lesion in the cavernous sinus (Figure 1).
She had nothing of significance in her laboratory results.
The patient underwent surgical intervention after obtaining informed consent. An endoscopic endonasal transsphenoidal surgery (EETS) method was performed for the removal of the tumor.
The tumor was removed without any complications and sent to pathology for analysis. The histopathological examination revealed a tumor with the characteristics of CSH. Postoperative MRI and computed tomography demonstrated the complete excision of the tumor. The patient was discharged four days later without experiencing any notable complications. There were no complications or recurrences during the 6-month follow-up.
Discussion
CSH comprises approximately 3% of all cavernous sinus lesions. It is more commonly observed in women aged 40 to 60 years. Clinical symptoms, such as headaches and cranial nerve deficits, typically arise from the progressive enlargement of the tumor [5].
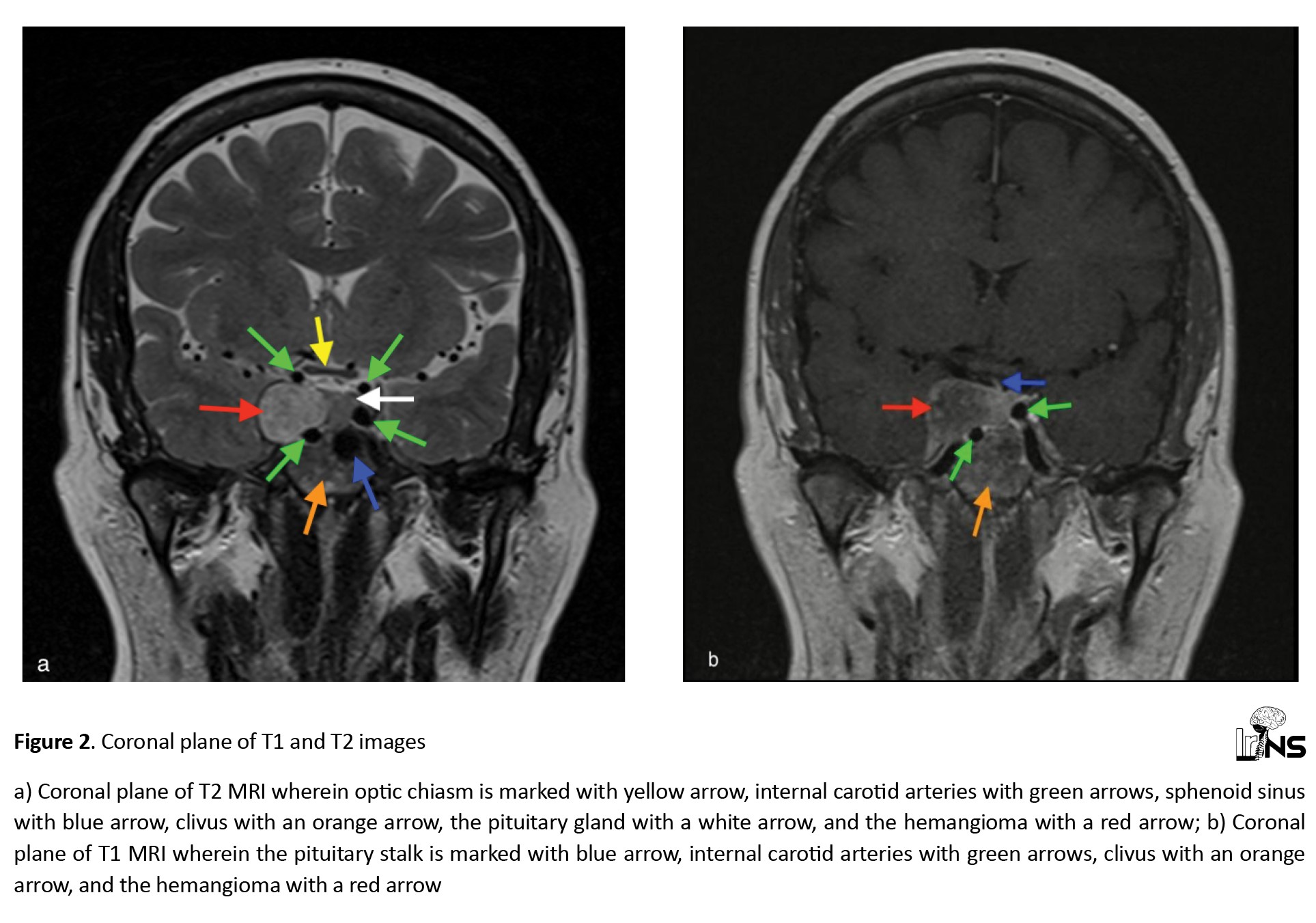
In our case, the MRI findings of the patient’s CSH were consistent with those reported in the literature. Specifically, the lesion exhibited hyperintensity on T2-weighted images and hypointensity on T1-weighted images (Figure 2).
The patient underwent surgical intervention after obtaining informed consent. An endoscopic endonasal transsphenoidal surgery (EETS) method was performed for the removal of the tumor.
The tumor was removed without any complications and sent to pathology for analysis. The histopathological examination revealed a tumor with the characteristics of CSH. Postoperative MRI and computed tomography demonstrated the complete excision of the tumor. The patient was discharged four days later without experiencing any notable complications. There were no complications or recurrences during the 6-month follow-up.
Discussion
CSH comprises approximately 3% of all cavernous sinus lesions. It is more commonly observed in women aged 40 to 60 years. Clinical symptoms, such as headaches and cranial nerve deficits, typically arise from the progressive enlargement of the tumor [5].
In our case, the MRI findings of the patient’s CSH were consistent with those reported in the literature. Specifically, the lesion exhibited hyperintensity on T2-weighted images and hypointensity on T1-weighted images (Figure 2).
These imaging characteristics align with previously reported findings, reinforcing the diagnostic value of MRI in identifying CSH [6-8]. The consistency of these findings across multiple studies underscores the reliability of MRI as a crucial tool in diagnosing and managing this rare vascular tumor.
In this case, the patient’s gender and clinical symptoms align with the findings reported in the literature on CSH. Specifically, this patient, a female, presented with headaches and visual disturbances, which are consistent with the symptoms described in several studies [6, 7, 9]. Montoya et al. [6] and Mahajan et al. [7] noted a significant female preponderance in their studies, each reporting 11 female patients. This consistency in gender distribution and clinical presentation across multiple studies underscores the typical demographic and symptomatic profile of CSH, reinforcing these findings’ diagnostic and clinical relevance.
According to the review conducted by Zhu et al., it is evident that the frontotemporal craniotomy (FC) method has been performed more frequently, achieving a gross total resection (GTR) rate of 78.97% (154 out of 195 cases) [10]. In contrast, the EETS method has been utilized less often, with a GTR rate of 57.14% (8 out of 14 cases). However, the GTR rate for EETS could be higher if it were applied to a larger number of cases. Additionally, this study highlights that the rates of postoperative short-term and long-term newly developed or deteriorative cranial-nerve function complications are significantly lower in the EETS group compared to the FC group. Specifically, the EETS group reported 0% (0 out of 7) for short-term and 0% (0 out of 6) for long-term complications, whereas the FC group reported 57% (57 out of 100) for short-term and 18.18% (18 out of 99) for long-term complications [10].
We utilized the EETS approach, successfully achieving GTR. Remarkably, our patient did not experience any postoperative short-term or long-term newly developed or deteriorative cranial-nerve function complications. This outcome further supports the potential advantages of the EETS method in minimizing postoperative complications and achieving successful resection.
Conclusion
This case report presents a cavernous sinus hemangioma, a rare benign vascular tumor within the cavernous sinus. Gross tumor resection was successfully achieved through the EET surgical method without any post-operative complications, which highlights the high efficacy of this surgical method.
Ethical Considerations
Compliance with ethical guidelines
This is a retrospective case study at Ege University. The Research Ethics Committee of Ege University, Izmir, Turkey, has confirmed that no ethical approval was required. The patient participating in the study provided informed consent for surgery.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Hüseyin Biçeroğlu, Mustafa Serdar Bölük, and Taşkın Yurtseven; Data collection: Matin Akhbari and Bilal Bahadır Akbulut; Data analysis and interpretation: Matin Akhbari and Bilal Bahadır Akbulut; Writing the original draft: Matin Akhbari, Bilal Bahadır Akbulut, and Mustafa Serdar Bölük; Review and editing: Matin Akhbari and Bilal Bahadır Akbulut; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors acknowledge the support and contributions that facilitated the completion of this work.
References
In this case, the patient’s gender and clinical symptoms align with the findings reported in the literature on CSH. Specifically, this patient, a female, presented with headaches and visual disturbances, which are consistent with the symptoms described in several studies [6, 7, 9]. Montoya et al. [6] and Mahajan et al. [7] noted a significant female preponderance in their studies, each reporting 11 female patients. This consistency in gender distribution and clinical presentation across multiple studies underscores the typical demographic and symptomatic profile of CSH, reinforcing these findings’ diagnostic and clinical relevance.
According to the review conducted by Zhu et al., it is evident that the frontotemporal craniotomy (FC) method has been performed more frequently, achieving a gross total resection (GTR) rate of 78.97% (154 out of 195 cases) [10]. In contrast, the EETS method has been utilized less often, with a GTR rate of 57.14% (8 out of 14 cases). However, the GTR rate for EETS could be higher if it were applied to a larger number of cases. Additionally, this study highlights that the rates of postoperative short-term and long-term newly developed or deteriorative cranial-nerve function complications are significantly lower in the EETS group compared to the FC group. Specifically, the EETS group reported 0% (0 out of 7) for short-term and 0% (0 out of 6) for long-term complications, whereas the FC group reported 57% (57 out of 100) for short-term and 18.18% (18 out of 99) for long-term complications [10].
We utilized the EETS approach, successfully achieving GTR. Remarkably, our patient did not experience any postoperative short-term or long-term newly developed or deteriorative cranial-nerve function complications. This outcome further supports the potential advantages of the EETS method in minimizing postoperative complications and achieving successful resection.
Conclusion
This case report presents a cavernous sinus hemangioma, a rare benign vascular tumor within the cavernous sinus. Gross tumor resection was successfully achieved through the EET surgical method without any post-operative complications, which highlights the high efficacy of this surgical method.
Ethical Considerations
Compliance with ethical guidelines
This is a retrospective case study at Ege University. The Research Ethics Committee of Ege University, Izmir, Turkey, has confirmed that no ethical approval was required. The patient participating in the study provided informed consent for surgery.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Hüseyin Biçeroğlu, Mustafa Serdar Bölük, and Taşkın Yurtseven; Data collection: Matin Akhbari and Bilal Bahadır Akbulut; Data analysis and interpretation: Matin Akhbari and Bilal Bahadır Akbulut; Writing the original draft: Matin Akhbari, Bilal Bahadır Akbulut, and Mustafa Serdar Bölük; Review and editing: Matin Akhbari and Bilal Bahadır Akbulut; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors acknowledge the support and contributions that facilitated the completion of this work.
References
- Lombardi D, Giovanelli M, de Tribolet N. Sellar and parasellar extra-axial cavernous hemangiomas. Acta Neurochirurgica. 1994; 130(1-4):47-54. [DOI:10.1007/BF01405502] [PMID]
- Linskey ME, Sekhar LN. Cavernous sinus hemangiomas: A series, a review, and an hypothesis. Neurosurgery. 1992; 30(1):101-8. [DOI:10.1227/00006123-199201000-00018] [PMID]
- Hashimoto M, Yokota A, Ohta H, Urasaki E. Intratumoral injection of plastic adhesive material for removal of cavernous sinus hemangioma. Technical note. Journal of Neurosurgery. 2000; 93(6):1078-81. [DOI:10.3171/jns.2000.93.6.1078] [PMID]
- Fraser JF, Mass AY, Brown S, Anand VK, Schwartz TH. Transnasal endoscopic resection of a cavernous sinus hemangioma: Technical note and review of the literature. Skull Base. 2008; 18(5):309-15. [DOI:10.1055/s-0028-1086059] [PMID] [PMCID]
- Nishimura F, Park YS, Nakagawa I, Yamada S, Nakase H, Nagatomo Y. Hemorrhagic cavernous sinus hemangioma with sudden-onset abducens palsy. World Neurosurgery. 2018; 112:1-5. [DOI:10.1016/j.wneu.2018.01.016] [PMID]
- Montoya F, Vidal A, Sepulveda F, Marileo R, Caro J, Castillo M. Cavernous Sinus Hemangioma: Imaging diagnosis and surgical considerations. World Neurosurgery. 2021; 146:e30-e7. [DOI:10.1016/j.wneu.2020.09.153] [PMID]
- Mahajan A, Rao VRK, Anantaram G, Polnaya AM, Desai S, Desai P, et al. Clinical-radiological-pathological correlation of cavernous sinus hemangioma: Incremental value of diffusion-weighted imaging. World Journal of Radiology. 2017; 9(8):330-8. [DOI:10.4329/wjr.v9.i8.330] [PMID] [PMCID]
- Esteves C, Berhanu D, Guerreiro C. Radiologic clue to cavernous sinus hemangioma diagnosis. World Neurosurgery. 2025; 194:123440. [DOI:10.1016/j.wneu.2024.11.023] [PMID]
- Rasband JM, Alfattal R, Patel AJ, Fuller GN, Perry A, Lu HC. Cavernous sinus hemangioma: Histopathological spectrum of 8 cases. Journal of Neuropathology and Experimental Neurology. 2023; 82(10):884-6. [DOI:10.1093/jnen/nlad058] [PMID]
- Zhu J, Cong Z, Ma C. Endoscopic endonasal transsphenoidal surgery for the cavernous sinus hemangioma: Surgical application and review of the literature. World Neurosurgery X. 2023; 18:100179. [DOI:10.1016/j.wnsx.2023.100179] [PMID] [PMCID]
Type of Study: Case report |
Subject:
Skull Base
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |