Sat, Jan 31, 2026
Volume 11 - Continuous Publishing
Iran J Neurosurg 2025, 11 - Continuous Publishing: 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Davoudi-Kiakalayeh A, Yousefzade-Chabok S. Ossification of the Posterior Longitudinal Ligament: A Closer Look at The Disease. Iran J Neurosurg 2025; 11 : 19
URL: http://irjns.org/article-1-534-en.html
URL: http://irjns.org/article-1-534-en.html
1- , davoudikiakalayeh@gmail.com
Keywords: Ossification, Posterior Longitudinal Ligamen
Full Text [PDF 1447 kb]
(172 Downloads)
| Abstract (HTML) (695 Views)
Full Text: (6 Views)
Ossification of the posterior longitudinal ligament (OPLL) is due to abnormal calcification of the posterior longitudinal ligament. It primarily affects the cervical spine—various classification systems group OPLL based on its morphological properties and clinical implications.
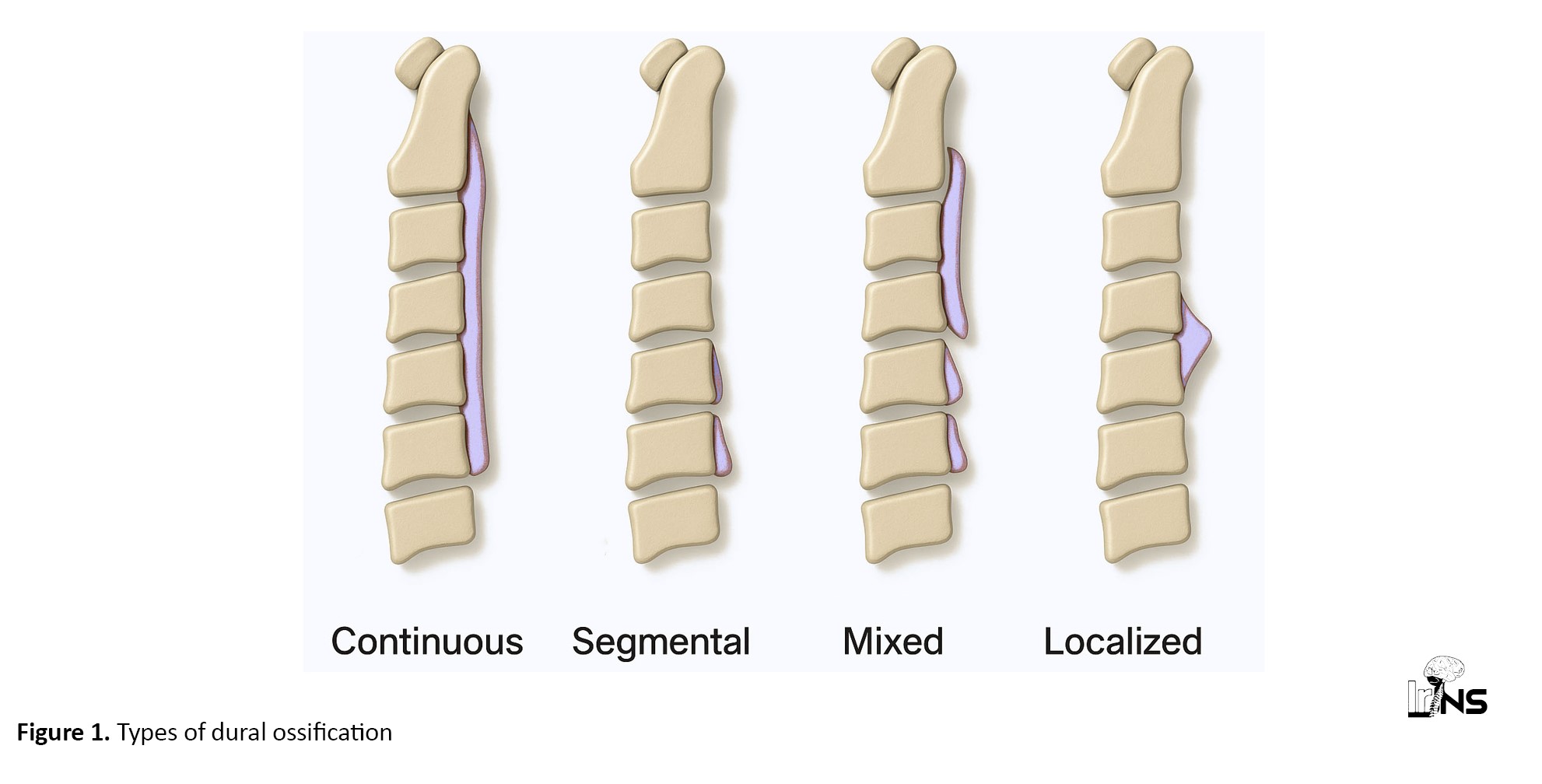
OPLL in the cervical spine is a common occurrence in cases of mild cervical spine changes. However, it is a rare pathological process of lamellar bone deposition that can result in spinal cord compression. The disease is common among the Asian population, particularly those over 50, and is caused by genetic and environmental factors. OPLL is classified into four main types: Continuous type, segmental type, mixed type, and local type (others). OPLL might involve any level, with the most common being at the C3 level, followed by C6 with 40.5%, and C7 with 36.5% (Figure 1) [1]. Risk factors associated with OPLL include various causes, such as higher levels of uric acid, higher body mass index (BMI), old age, a high-salt diet, low consumption of animal protein, glucose intolerance (diabetes), and high body mass. However, moderate amounts of sleep (6-8 hours) and regular sleeping habits were found to be associated with a decreased risk of OPLL. In addition, moderate physical exercise, smoking, alcohol consumption, and experiencing hangovers did not show any correlation with the risk of OPLL.
Today, a standard prevention or treatment of OPLL has not been established. Therefore, the management of OPLL involves various strategies, depending on symptoms and signs. Patients with incidentally discovered OPLL typically have mild symptoms and little need for medical assistance. However, once neurological symptoms appear, early surgery is desirable. Medical decisions should be based on both imaging tests and neurological symptoms. Most radiographically detectable cases are low-symptomatic or asymptomatic.
Medical management of mild and non-progressive OPLL symptoms includes pain medications, anti-inflammatory medications, anticonvulsants, non-steroidal anti-inflammatory drugs (NSAIDs), and topical opioids. Another form of medical assistance is physical therapy, which aims to improve mobility and overall function by strengthening muscles, improving flexibility, managing pain, correcting posture, and providing functional training.
Surgical intervention for OPLL depends on myelopathy symptoms such as abnormal reflexes, gait problems, radiographic evidence of injury, or persistent spinal cord compression. Surgery should be considered in these cases. Three surgical approaches are appropriate for OPLL, including the anterior cervical discectomy with fusion (ACDF), posterior method, and anterior cervical corpectomy with fusion (ACCF). If OPLL is located at the corner of the vertebral body, ACDF is recommended. However, for OPLL behind the vertebral body, ACCF is appropriate. Posterior methods are typically used for segmental or localized types and include techniques such as laminectomy (LF) and laminoplasty (LAMP and fusion). In some cases, a combined anterior and posterior approach may be necessary, depending on the patient’s K-line, canal-occupying ratio, and the size and location of the OPLL. Risk factors associated with anterior approaches include the canal occupancy ratio (Equation 1):
1. Canal occupancy ratio=maximum thickness of ossified ligament/anteroposterior spinal canal diameter×100%.
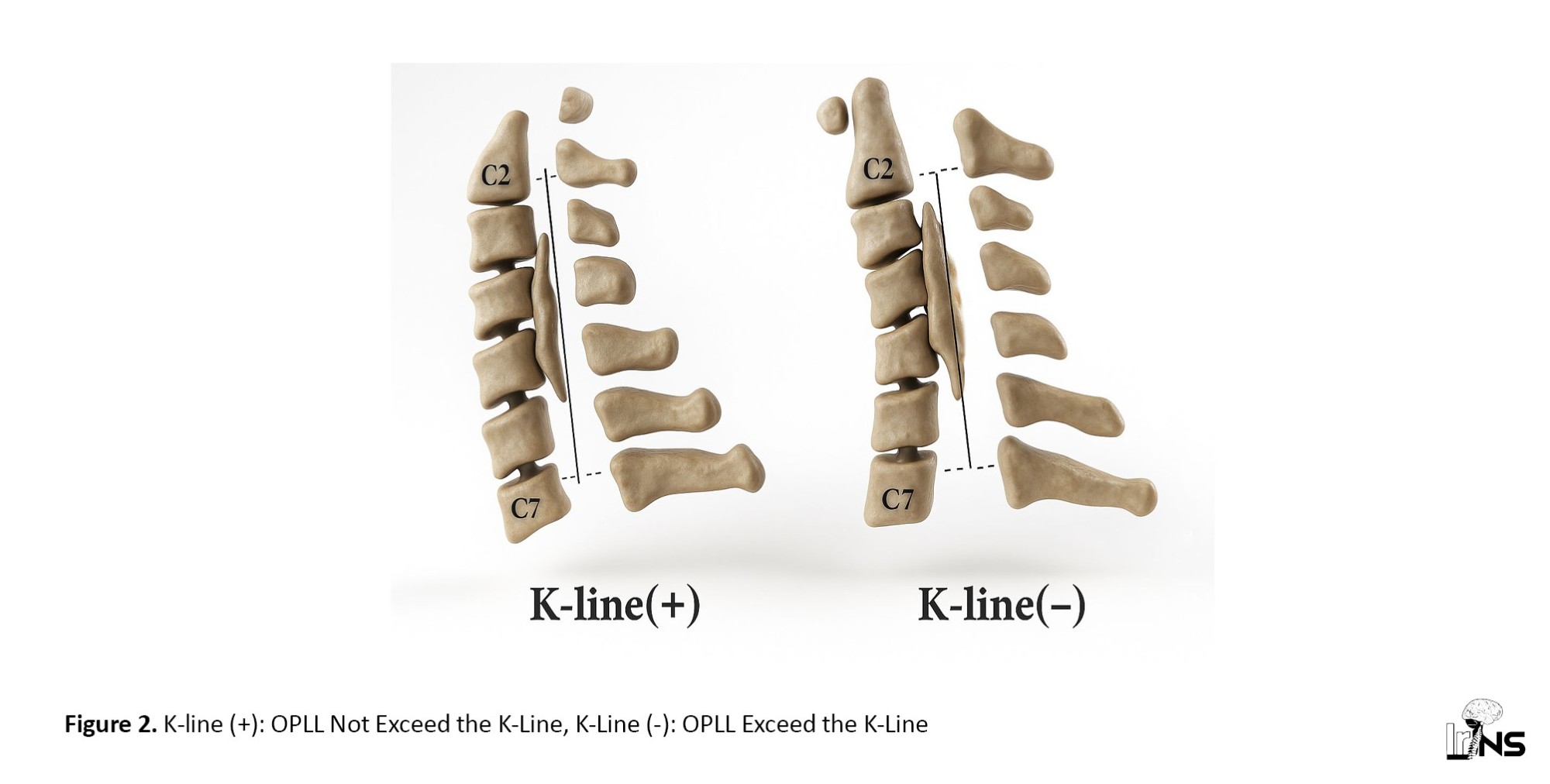
K-line (+) patients are those in whom OPLL does not cross the spinal canal midpoints at C2 and C7.
In K-line (+) patients with a canal-occupying ratio >60%, associated with higher myelopathy risk, the anterior approach (e.g. ACDF) is preferred.
The presence of SAC of less than 40% on CT, canal occupying ratio over 60%, beak-shaped OPLL, K-line (-), and C2-C7 lordosis angle under 10° favors an anterior approach, or a 360-degree fusion surgery is recommended. The ACDF techniques have been described as superior in terms of outcome, as evidenced by a higher Japanese Orthopedic Association (JOA) score.
In patients with a canal-occupying ratio greater than 60%, anterior cervical discectomy and fusion (ACDF) has been shown to provide better postoperative neurological recovery compared to posterior approaches. Additionally, the JOA recovery rates are significantly higher in this group. Conversely, for those with a canal-occupying ratio of less than 50-60%, the posterior approach is preferred if no significant local kyphosis is present.
In patients with a canal-occupying ratio below 50%, anterior and posterior approaches result in similar postoperative JOA scores and recovery rates. This outcome suggests that the decision between surgical methods is less crucial for this subgroup. Patients with a canal-occupying ratio between 50% and 60% generally show good recovery rates after surgery, especially when treated with an anterior approach. This approach is associated with better outcomes compared to posterior methods in cases of higher canal occupancy.
It has been demonstrated that posterior approaches like laminoplasty or LF do not adequately decompress patients with K-line (-). Research shows that these patients often have poor neurological outcomes after surgery, with mean recovery rates as low as 13.9%, while K-line (+) patients have a recovery rate of 66% (Figure 2). For K-line (-) patients, anterior decompression techniques are advised due to the shortcomings of posterior treatments. Better results in this group have been associated with ACDF. JOA scores were considerably higher for individuals treated with anterior techniques than for those treated with posterior approaches, according to research.
The anterior method carries a high risk of dural tear, ranging from 4.3% to 32%, whereas the posterior method poses a significantly lower risk, between 0.5% and 3%. In addition, the anterior method is associated with 15% of patients developing graft-related complications, 7% experiencing neurological deterioration, and 26% requiring additional surgical intervention.
On the other hand, the posterior method has a lower complication rate, with 9% experiencing transient upper extremity paresis, 8% experiencing neuropathic arm pain, and a 1% reoperation rate; however, posterior approaches, including LF and fusion and laminoplasty, may be well tolerated in older patients. Overall, the anterior method of OPLL surgery is much more complicated than the posterior method. Compared to the posterior surgery, OPLL patients have a higher risk of cerebrospinal fluid (CSF) leakage with anterior surgery. Symptoms of CSF leakage after anterior OPLL surgery may include pseudomeningocele, dyspnea, cutaneous CSF leakage fistula, and meningitis. Delayed wound healing, airway obstruction, and life-threatening conditions such as meningitis can also occur as secondary complications of CSF leak after cervical surgery. However, in experienced hands, the preference of the surgeon is more crucial. CT myelography, MRI, and radionuclide cisternography have been conducted to detect CSF leakage after anterior surgery in patients with OPLL.
To prevent ongoing CSF leakage and associated complications after anterior surgery for OPLL, if intraoperative adjuncts such as Gelfoam, fascia graft, or fibrin glue cannot control the CSF leak, a lumbar drain should be inserted at the time of surgery. Following this, the patient is placed on bed rest, and for 4 to 5 days, the CSF is drained at a controlled speed to enable proper dural closure. These symptoms highlight how crucial it is to identify and treat CSF leaks as soon as possible to prevent further complications and aid the patient’s recovery. Symptoms of a CSF leak include headache, nausea, and photophobia. A beta-2 transferrin test may occasionally be used to confirm the presence of CSF in drainage fluid.
Complications associated with the posterior approach
One of the main issues with posterior decompression in K-line (-) patients is that it usually fails to provide enough anterior decompression of the spinal cord. This inadequacy can lead to persistent or worsening neurological symptoms postoperatively, because the posterior shift of the spinal cord may not be enough to relieve ventral compression from the ossified ligament. A common complication associated with posterior cervical surgeries in K-line (-) patients is C5 nerve root palsy, which can occur due to nerve root injury during decompression or instrumentation, which can manifest as weakness in shoulder abduction and external rotation. After surgery, several K-line (-) patients experience persistent neurological impairments such as tingling, numbness, and weakness in the upper and lower extremities. This condition is largely due to inadequate spinal cord decompression, which is common with posterior approaches in these cases (Figure 2) [1].
Axial neck pain may result from damage to soft tissues, such as muscles and ligaments, during posterior decompression, as well as from altered cervical spine biomechanics postoperatively. Some patients may develop postoperative kyphosis due to instability or loss of curvature in the cervical spine after decompression. This condition can lead to further neurological compromise and discomfort. Patients may experience worsening or new symptoms of myelopathy, such as coordination difficulties or changes in bowel and bladder function, due to inadequate spinal cord decompression.
References
OPLL in the cervical spine is a common occurrence in cases of mild cervical spine changes. However, it is a rare pathological process of lamellar bone deposition that can result in spinal cord compression. The disease is common among the Asian population, particularly those over 50, and is caused by genetic and environmental factors. OPLL is classified into four main types: Continuous type, segmental type, mixed type, and local type (others). OPLL might involve any level, with the most common being at the C3 level, followed by C6 with 40.5%, and C7 with 36.5% (Figure 1) [1]. Risk factors associated with OPLL include various causes, such as higher levels of uric acid, higher body mass index (BMI), old age, a high-salt diet, low consumption of animal protein, glucose intolerance (diabetes), and high body mass. However, moderate amounts of sleep (6-8 hours) and regular sleeping habits were found to be associated with a decreased risk of OPLL. In addition, moderate physical exercise, smoking, alcohol consumption, and experiencing hangovers did not show any correlation with the risk of OPLL.
Today, a standard prevention or treatment of OPLL has not been established. Therefore, the management of OPLL involves various strategies, depending on symptoms and signs. Patients with incidentally discovered OPLL typically have mild symptoms and little need for medical assistance. However, once neurological symptoms appear, early surgery is desirable. Medical decisions should be based on both imaging tests and neurological symptoms. Most radiographically detectable cases are low-symptomatic or asymptomatic.
Medical management of mild and non-progressive OPLL symptoms includes pain medications, anti-inflammatory medications, anticonvulsants, non-steroidal anti-inflammatory drugs (NSAIDs), and topical opioids. Another form of medical assistance is physical therapy, which aims to improve mobility and overall function by strengthening muscles, improving flexibility, managing pain, correcting posture, and providing functional training.
Surgical intervention for OPLL depends on myelopathy symptoms such as abnormal reflexes, gait problems, radiographic evidence of injury, or persistent spinal cord compression. Surgery should be considered in these cases. Three surgical approaches are appropriate for OPLL, including the anterior cervical discectomy with fusion (ACDF), posterior method, and anterior cervical corpectomy with fusion (ACCF). If OPLL is located at the corner of the vertebral body, ACDF is recommended. However, for OPLL behind the vertebral body, ACCF is appropriate. Posterior methods are typically used for segmental or localized types and include techniques such as laminectomy (LF) and laminoplasty (LAMP and fusion). In some cases, a combined anterior and posterior approach may be necessary, depending on the patient’s K-line, canal-occupying ratio, and the size and location of the OPLL. Risk factors associated with anterior approaches include the canal occupancy ratio (Equation 1):
1. Canal occupancy ratio=maximum thickness of ossified ligament/anteroposterior spinal canal diameter×100%.
K-line (+) patients are those in whom OPLL does not cross the spinal canal midpoints at C2 and C7.
In K-line (+) patients with a canal-occupying ratio >60%, associated with higher myelopathy risk, the anterior approach (e.g. ACDF) is preferred.
The presence of SAC of less than 40% on CT, canal occupying ratio over 60%, beak-shaped OPLL, K-line (-), and C2-C7 lordosis angle under 10° favors an anterior approach, or a 360-degree fusion surgery is recommended. The ACDF techniques have been described as superior in terms of outcome, as evidenced by a higher Japanese Orthopedic Association (JOA) score.
In patients with a canal-occupying ratio greater than 60%, anterior cervical discectomy and fusion (ACDF) has been shown to provide better postoperative neurological recovery compared to posterior approaches. Additionally, the JOA recovery rates are significantly higher in this group. Conversely, for those with a canal-occupying ratio of less than 50-60%, the posterior approach is preferred if no significant local kyphosis is present.
In patients with a canal-occupying ratio below 50%, anterior and posterior approaches result in similar postoperative JOA scores and recovery rates. This outcome suggests that the decision between surgical methods is less crucial for this subgroup. Patients with a canal-occupying ratio between 50% and 60% generally show good recovery rates after surgery, especially when treated with an anterior approach. This approach is associated with better outcomes compared to posterior methods in cases of higher canal occupancy.
It has been demonstrated that posterior approaches like laminoplasty or LF do not adequately decompress patients with K-line (-). Research shows that these patients often have poor neurological outcomes after surgery, with mean recovery rates as low as 13.9%, while K-line (+) patients have a recovery rate of 66% (Figure 2). For K-line (-) patients, anterior decompression techniques are advised due to the shortcomings of posterior treatments. Better results in this group have been associated with ACDF. JOA scores were considerably higher for individuals treated with anterior techniques than for those treated with posterior approaches, according to research.
The anterior method carries a high risk of dural tear, ranging from 4.3% to 32%, whereas the posterior method poses a significantly lower risk, between 0.5% and 3%. In addition, the anterior method is associated with 15% of patients developing graft-related complications, 7% experiencing neurological deterioration, and 26% requiring additional surgical intervention.
On the other hand, the posterior method has a lower complication rate, with 9% experiencing transient upper extremity paresis, 8% experiencing neuropathic arm pain, and a 1% reoperation rate; however, posterior approaches, including LF and fusion and laminoplasty, may be well tolerated in older patients. Overall, the anterior method of OPLL surgery is much more complicated than the posterior method. Compared to the posterior surgery, OPLL patients have a higher risk of cerebrospinal fluid (CSF) leakage with anterior surgery. Symptoms of CSF leakage after anterior OPLL surgery may include pseudomeningocele, dyspnea, cutaneous CSF leakage fistula, and meningitis. Delayed wound healing, airway obstruction, and life-threatening conditions such as meningitis can also occur as secondary complications of CSF leak after cervical surgery. However, in experienced hands, the preference of the surgeon is more crucial. CT myelography, MRI, and radionuclide cisternography have been conducted to detect CSF leakage after anterior surgery in patients with OPLL.
To prevent ongoing CSF leakage and associated complications after anterior surgery for OPLL, if intraoperative adjuncts such as Gelfoam, fascia graft, or fibrin glue cannot control the CSF leak, a lumbar drain should be inserted at the time of surgery. Following this, the patient is placed on bed rest, and for 4 to 5 days, the CSF is drained at a controlled speed to enable proper dural closure. These symptoms highlight how crucial it is to identify and treat CSF leaks as soon as possible to prevent further complications and aid the patient’s recovery. Symptoms of a CSF leak include headache, nausea, and photophobia. A beta-2 transferrin test may occasionally be used to confirm the presence of CSF in drainage fluid.
Complications associated with the posterior approach
One of the main issues with posterior decompression in K-line (-) patients is that it usually fails to provide enough anterior decompression of the spinal cord. This inadequacy can lead to persistent or worsening neurological symptoms postoperatively, because the posterior shift of the spinal cord may not be enough to relieve ventral compression from the ossified ligament. A common complication associated with posterior cervical surgeries in K-line (-) patients is C5 nerve root palsy, which can occur due to nerve root injury during decompression or instrumentation, which can manifest as weakness in shoulder abduction and external rotation. After surgery, several K-line (-) patients experience persistent neurological impairments such as tingling, numbness, and weakness in the upper and lower extremities. This condition is largely due to inadequate spinal cord decompression, which is common with posterior approaches in these cases (Figure 2) [1].
Axial neck pain may result from damage to soft tissues, such as muscles and ligaments, during posterior decompression, as well as from altered cervical spine biomechanics postoperatively. Some patients may develop postoperative kyphosis due to instability or loss of curvature in the cervical spine after decompression. This condition can lead to further neurological compromise and discomfort. Patients may experience worsening or new symptoms of myelopathy, such as coordination difficulties or changes in bowel and bladder function, due to inadequate spinal cord decompression.
References
- Tetreault L, Nakashima H, Kato S, Kryshtalskyj M, Nagoshi N, Nouri A, Singh A, Fehlings MG. A systematic review of classification systems for cervical ossification of the posterior longitudinal ligament. Global Spine Journal. 2019; 9(1):85-103. [DOI:10.1177/2192568217720421]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |