Wed, Jul 16, 2025
Volume 1, Issue 1 (6-2015)
Iran J Neurosurg 2015, 1(1): 47-52 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bahrami E, Rahatlou H, Fattahi A, Astaraki S, Khani M, Shirvani M et al . The Real Story of the Fifth Nerve Neurinoma: A Review of Our Learning Curve about Surgical Approaches and Associated Shortcomings. Iran J Neurosurg 2015; 1 (1) :47-52
URL: http://irjns.org/article-1-7-en.html
URL: http://irjns.org/article-1-7-en.html
Eshagh Bahrami 
 , Hessam Rahatlou *1
, Hessam Rahatlou *1 

 , Arash Fattahi
, Arash Fattahi 
 , Shahrzad Astaraki
, Shahrzad Astaraki 
 , Mohammad-Reza Khani
, Mohammad-Reza Khani 
 , Massood Shirvani
, Massood Shirvani 
 , Mohammad-Jafar Ghaempanah
, Mohammad-Jafar Ghaempanah 


 , Hessam Rahatlou *1
, Hessam Rahatlou *1 

 , Arash Fattahi
, Arash Fattahi 
 , Shahrzad Astaraki
, Shahrzad Astaraki 
 , Mohammad-Reza Khani
, Mohammad-Reza Khani 
 , Massood Shirvani
, Massood Shirvani 
 , Mohammad-Jafar Ghaempanah
, Mohammad-Jafar Ghaempanah 

1- , Rahatlou@gmail.com
Keywords: Corneal anesthesia, Iatrogenic, Combined approach, Cerebello Pontine Angle tumor, Vidian nerve, Painless corneal perforation, Herpes ophthalmicus, Neurinoma, Interdurall location
Full Text [PDF 615 kb]
(1789 Downloads)
| Abstract (HTML) (7792 Views)
Full Text: (1688 Views)
Background and Importance
The clinical presentation of the fifth nerve neurinoma includes a wide range from trigeminal neuralgia to generalized neurologic manifestations. The main presenting signs and symptoms detected in large neurinomas or neurinomas associated with large cystic components are divided into focal and generalized manifestations (1). Focal presentations of these neurinomas include unilateral craniofacial headache in the fifth nerve territory, classic unilateral trigeminal neuralgia (V1,V2,V3) or any combination of them. Decreased corneal sensation, asymmetric jaw jerk accompanying cranial nerve defects such as hemifacial spasm, unilateral 6th nerve paresis are some of the other focal manifestations of the fifth nerve neurinoma (2). The Generalized symptoms are intracranial pressure (ICP) raising which can be presented with headache or vomiting, Papilledema, binocular diplopia, unsteadiness and drowsiness due to hydrocephalus. Long-Tract signs as spastic hemiparesis or quadriparesis and also convulsion as a rare symptom are also other generalized symptoms which the fifth nerve neurinoma can be presented with them (2). Case-based approach is one of the best methods to discuss and explain the interesting points for management of complicated cases in practical neurosurgery; so we would be glad to express our practical experiences in two different fifth nerve neurinoma cases. In the first case (solid tumor), A combined cerebellopontine angle (CPA) subtemporal approach in the lateral park-bench position was used and in the second one (the cystic tumor) retrosigmoid CPA suprameatal approach in the semisitting position was used.
Case Presentation
Case 1
A 31 year old man presented with long-lasting headache, binocular diplopia, unsteadiness ataxia and quadriparesis which have been progressed for about 6 months. Bilateral papilledema was detected during physical examination. His corneal sensation was intact (corneal Reflex had not been examined) (Figure 1). We operated on the patient in lateral Park-bench position using a combined subtemporal and retrosigmoid approach. Craniectomy was performed and drilling of petrous bone was done as much as possible to reach the widest extradural exposure. Then the dura of the posterior fossa opened which revealed no intradural tumor. Subtemporaldural opening was also negative for intraduraltumor.
It was concluded that the tumor should be located interdurally and so the most probable tumor was the fifth nerve neurinoma. The mass was fleshy in texture and relatively hemorrhagic. We were lucky to extract the entire tumor when we reached the distal branches of the fifth nerve. Patient recovered from anesthesia in 24 hours post-op without any major neurological deficit but it was found that Lt corneal anesthesia on the second post-op day. Vision was intact and the patient was warned about corneal anesthesia under strict corneal protection with transparent moisturizing eye ointment.
Frequent corneal exam by ophthalmologist revealed persistent corneal epithelial defect.Tarsoraphy was done for 2 weeks. Patient’s cornea recovered completely but he developed paradoxical CSF leakage from the mastoid air cell origin in the third week of post-op period which sealed by fat and glue successfully. Now the patient is intact except Lt facial paresthesia and Lt corneal anesthesia. Serial CT scan and MRI (±GAD) one year after operation is accompanied which is clear for tumor remnant (Figure 2).
The clinical presentation of the fifth nerve neurinoma includes a wide range from trigeminal neuralgia to generalized neurologic manifestations. The main presenting signs and symptoms detected in large neurinomas or neurinomas associated with large cystic components are divided into focal and generalized manifestations (1). Focal presentations of these neurinomas include unilateral craniofacial headache in the fifth nerve territory, classic unilateral trigeminal neuralgia (V1,V2,V3) or any combination of them. Decreased corneal sensation, asymmetric jaw jerk accompanying cranial nerve defects such as hemifacial spasm, unilateral 6th nerve paresis are some of the other focal manifestations of the fifth nerve neurinoma (2). The Generalized symptoms are intracranial pressure (ICP) raising which can be presented with headache or vomiting, Papilledema, binocular diplopia, unsteadiness and drowsiness due to hydrocephalus. Long-Tract signs as spastic hemiparesis or quadriparesis and also convulsion as a rare symptom are also other generalized symptoms which the fifth nerve neurinoma can be presented with them (2). Case-based approach is one of the best methods to discuss and explain the interesting points for management of complicated cases in practical neurosurgery; so we would be glad to express our practical experiences in two different fifth nerve neurinoma cases. In the first case (solid tumor), A combined cerebellopontine angle (CPA) subtemporal approach in the lateral park-bench position was used and in the second one (the cystic tumor) retrosigmoid CPA suprameatal approach in the semisitting position was used.
Case Presentation
Case 1
A 31 year old man presented with long-lasting headache, binocular diplopia, unsteadiness ataxia and quadriparesis which have been progressed for about 6 months. Bilateral papilledema was detected during physical examination. His corneal sensation was intact (corneal Reflex had not been examined) (Figure 1). We operated on the patient in lateral Park-bench position using a combined subtemporal and retrosigmoid approach. Craniectomy was performed and drilling of petrous bone was done as much as possible to reach the widest extradural exposure. Then the dura of the posterior fossa opened which revealed no intradural tumor. Subtemporaldural opening was also negative for intraduraltumor.
It was concluded that the tumor should be located interdurally and so the most probable tumor was the fifth nerve neurinoma. The mass was fleshy in texture and relatively hemorrhagic. We were lucky to extract the entire tumor when we reached the distal branches of the fifth nerve. Patient recovered from anesthesia in 24 hours post-op without any major neurological deficit but it was found that Lt corneal anesthesia on the second post-op day. Vision was intact and the patient was warned about corneal anesthesia under strict corneal protection with transparent moisturizing eye ointment.
Frequent corneal exam by ophthalmologist revealed persistent corneal epithelial defect.Tarsoraphy was done for 2 weeks. Patient’s cornea recovered completely but he developed paradoxical CSF leakage from the mastoid air cell origin in the third week of post-op period which sealed by fat and glue successfully. Now the patient is intact except Lt facial paresthesia and Lt corneal anesthesia. Serial CT scan and MRI (±GAD) one year after operation is accompanied which is clear for tumor remnant (Figure 2).
Case 2
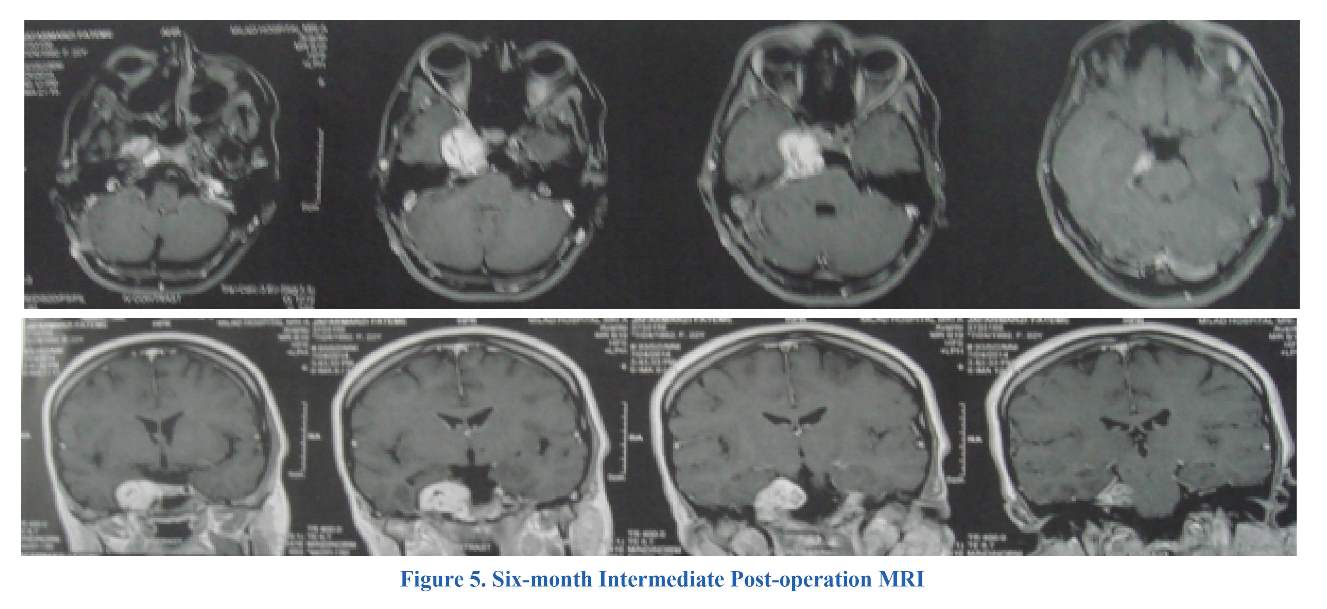
A 21 years old woman presented with unilateral craniofacial headache of long duration. She complained of binocular diplopia and atypical trigeminal neuralgia which have been progressed for about 3 months. Ipsilateral sixth nerve palsy and symmetric corneal reflex were also detected and her corneal sensation was also intact (Figure 3,4). In this patient due to the presence of large cystic component, we operated on semi-sitting position with standard retrosigmoid-subtentorial approach (Figure 5). The tumor exposed from CPA then we extended suprameatal corridor by cyst-evacuation and piecemeal evacuation of the tumor. At last we reached the small solid portion of the tumor attached to external side of the carotid artery extending to subtemporal fossa which we left it alone. The patient had quiet post-operative period and after recovery from anesthesia, we found corneal anesthesia in the right eye. Six months postoperative MRI (±GAD) revealed a small solid tumor remnant which was expected and also was out of access from the CPA approach. The patient is now neurologically intact except right facial paresthesia, Rt sixth nerve palsy and right corneal anesthesia. The patient was not warned of her corneal anesthesia.
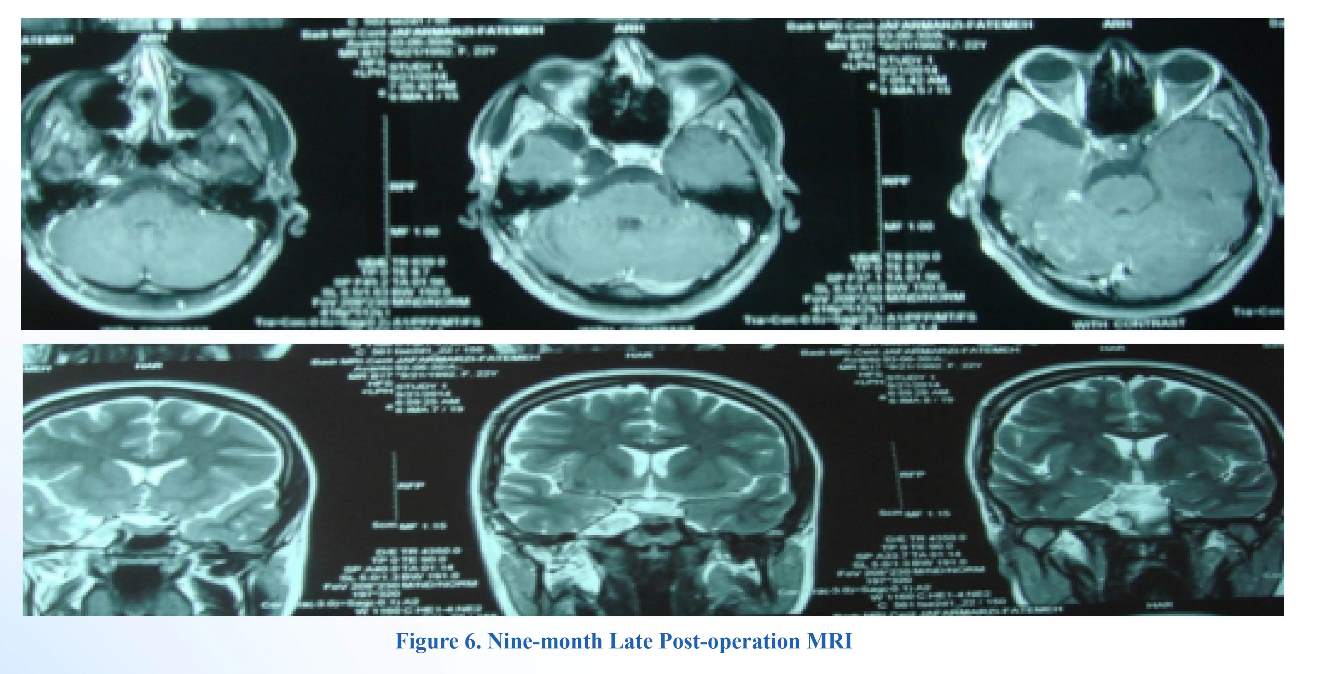
The MRI revealed tumor remnant which was getting larger in the 6 month post-operation. We decided to operate on via right Pterional approach reaching anterior subtemporal fossa and so the entire tumor remnant was removed successfully (Figure 6).
A 21 years old woman presented with unilateral craniofacial headache of long duration. She complained of binocular diplopia and atypical trigeminal neuralgia which have been progressed for about 3 months. Ipsilateral sixth nerve palsy and symmetric corneal reflex were also detected and her corneal sensation was also intact (Figure 3,4). In this patient due to the presence of large cystic component, we operated on semi-sitting position with standard retrosigmoid-subtentorial approach (Figure 5). The tumor exposed from CPA then we extended suprameatal corridor by cyst-evacuation and piecemeal evacuation of the tumor. At last we reached the small solid portion of the tumor attached to external side of the carotid artery extending to subtemporal fossa which we left it alone. The patient had quiet post-operative period and after recovery from anesthesia, we found corneal anesthesia in the right eye. Six months postoperative MRI (±GAD) revealed a small solid tumor remnant which was expected and also was out of access from the CPA approach. The patient is now neurologically intact except right facial paresthesia, Rt sixth nerve palsy and right corneal anesthesia. The patient was not warned of her corneal anesthesia.
The MRI revealed tumor remnant which was getting larger in the 6 month post-operation. We decided to operate on via right Pterional approach reaching anterior subtemporal fossa and so the entire tumor remnant was removed successfully (Figure 6).
Discussion
Corneal anesthesia is a major threat regarding corneal preservation, so some questions may be posed as follows: 1) Is it wise to warn a neurosurgical patient about the lack of corneal sensation which was intact pre-operatively and the motor division of VII nerve is functional post-operatively? 2) Is the corneal nutrition impaired in iatrogenic corneal anesthesia cases? 3) Is the corneal preservation dependent on facial nerve function (intact vidian nerve) or the corneal somatic sensation is the only major determinant?
Secretion and production of tear:
Although the cornea is clear and seems to lack substance, it is actually a highly organized group of cells and proteins. Unlike most tissues in the body, the Cornea contains no blood vessels to nourish or protect it against infection. Instead, the cornea receives its nourishment from the tears and aqueous humor (a fluid in the anterior portion of the eye) that fills the chamber behind it (3). As we know, the secretion and production of tear is completely dependent on intact vidian nerve (a parasympathetic component of VII nerve) (4) Therefore it must be considered that in the cases of combined (Subtemporal + Retrosigmoid) approaches we should drill some of the basi temporal petrous bone where the vidian nerve may be injured inadvertently. (5) The least believable result of such a nerve injury would be xerophthalmia which the patient with intact corneal sensation complains of dry eye and burning sensation unilaterally but in the cases of iatrogenic post-op corneal anesthesia the patient may develop corneal ulceration without any painful complaint (6). In the cases of patients with 5th nerve neurinomas who undergo combined approach, we are exposed with iatrogenic post-op corneal anesthesia and at the same time we have no tear production due to vidian nerve damage which is in part approach dependent. Although the VII nerve motor function is intact but we have no enough tear to nourish and protect the cornea. On the other hand in the cases of retrosigmoid approach alone we should have intact vidian nerve and sufficient tear production to nourish the cornea is ensured (7). The role of intact V and VII nerve functions are the cornerstone of corneal preservation and protection (nutritional and mechanical view point). In preoperative period, the patient with intact corneal sensation and intact facial motor function should have intact blinking reflex. We recommend strictly to check corneal sensation, facial nerve function and preserved tearing post-operatively in order to protect the cornea (8). In the combined approach when the tumor located in pre-ganglionic or ganglionic portion, the injury of corneal sensation during operation is more likely to develop but when the tumor is located in post-ganglionic divisions, only those one involving the v1 division are likely to injure the corneal sensation (7). One extraordinary threat which we have had exposed with was the occurrence of Herpes ophthalmicus and corneal perforation without painful complaint (9). Finally the ambulated patients would have face wash and sweating so water and sweat exposure to cornea is a real danger to an anesthetic cornea in everyday activities.
Advantages and disadvantages of the approaches:
Better following of the proximal portion of the5th nerve, better handling of subtentorial component, preparing a trans-lesional window to petroclinoidal junction in the case of cystic lesions are the advantages of Retrosigmoid (Suprameatal) approach and the threat to the vidian nerve damage is less probable than combined approach. On the other hand better visualization of all of the mass and neighboring structures, better access to interdurally entrapped solid masses and also better handling of the neighboring vessels are the advantages of the combined (Retrosigmoid + Subtemporal)approach while the threat of simultaneous damage to V and VII nerves is considerable in this approach.
Complications
Corneal anesthesia CSF leakage (direct, paradoxical), cranial nerve damage (other than fifth) and vascular injuries are some of the surgical complications. We have been exposed with two of them in our cases.
CSF leak after a retromastoid approach can drain through open mastoid air cells into the middle ear cavity and then through the Eustachian tube to present as CSF rhinorrhea. This type of leak has been referred to as paradoxical CSF rhinorrhea (5). Watertight dural closure should be the goal following any posterior fossa approach. In case 1, we have paradoxical CSF leakage from the mastoid air cell origin in the third week of post-operation period which sealed by fat and glue successfully.
Main clues and tools indicating the diagnosis:
Any long lasting lesions involving the Meckel’s cave. In other words any lesion involving the middle and the posterior fossa could be indicative of the presence of the 5th nerve neurinoma. However bone window CT scan to clarify the extent of bone destruction and to define neighboring bony structures (middle ear , Petrous Tip and Meckel’s cave) and also brain MRI± GAD T1,T2 coronal and sagittal are the main diagnostic tools.
We should remember that the location of the 5th nerve neurinoma includes subtentorial Intradural, supratentorial Intradural and pure Interdural in some of them.
Conclusions
In general neurosurgery preoperative list of differential diagnosis should be limited and indicative of real anatomopathology in order to get the best result intra operatively and post-operatively. In order to have a safe surgical result, we do recommend that any masses located in the boundary of middle and posterior fossa in the Mediobasal portion (Meckel’s Cave), should be defined delicately by skull base CT scan. In the cases of solid masses with different consistency we should keep in mind that, whether it is inter-dural or intra-durally located. We do also recommend pre-operative full examination of corneal sensation, facial motor function (blinking) and tearing status. Early Post-op examination of VII nerve function and corneal sensation are another recommendation. Occurrence of herpes ophthalmicus in any of such approaches is an ominous symptom in favor of the development of painless corneal perforation. At last warning the patient of corneal anesthesia in the cases of combined approaches because of the possible simultaneous damage to V and VII nerve should be considered. Consultation with an expert ophthalmologist for corneal care and temporary tarsoraphy if necessary is also recommended.
Funding
None declared.
Conflicts of Interest
The authors declare that they have no competing interests.
References
Corneal anesthesia is a major threat regarding corneal preservation, so some questions may be posed as follows: 1) Is it wise to warn a neurosurgical patient about the lack of corneal sensation which was intact pre-operatively and the motor division of VII nerve is functional post-operatively? 2) Is the corneal nutrition impaired in iatrogenic corneal anesthesia cases? 3) Is the corneal preservation dependent on facial nerve function (intact vidian nerve) or the corneal somatic sensation is the only major determinant?
Secretion and production of tear:
Although the cornea is clear and seems to lack substance, it is actually a highly organized group of cells and proteins. Unlike most tissues in the body, the Cornea contains no blood vessels to nourish or protect it against infection. Instead, the cornea receives its nourishment from the tears and aqueous humor (a fluid in the anterior portion of the eye) that fills the chamber behind it (3). As we know, the secretion and production of tear is completely dependent on intact vidian nerve (a parasympathetic component of VII nerve) (4) Therefore it must be considered that in the cases of combined (Subtemporal + Retrosigmoid) approaches we should drill some of the basi temporal petrous bone where the vidian nerve may be injured inadvertently. (5) The least believable result of such a nerve injury would be xerophthalmia which the patient with intact corneal sensation complains of dry eye and burning sensation unilaterally but in the cases of iatrogenic post-op corneal anesthesia the patient may develop corneal ulceration without any painful complaint (6). In the cases of patients with 5th nerve neurinomas who undergo combined approach, we are exposed with iatrogenic post-op corneal anesthesia and at the same time we have no tear production due to vidian nerve damage which is in part approach dependent. Although the VII nerve motor function is intact but we have no enough tear to nourish and protect the cornea. On the other hand in the cases of retrosigmoid approach alone we should have intact vidian nerve and sufficient tear production to nourish the cornea is ensured (7). The role of intact V and VII nerve functions are the cornerstone of corneal preservation and protection (nutritional and mechanical view point). In preoperative period, the patient with intact corneal sensation and intact facial motor function should have intact blinking reflex. We recommend strictly to check corneal sensation, facial nerve function and preserved tearing post-operatively in order to protect the cornea (8). In the combined approach when the tumor located in pre-ganglionic or ganglionic portion, the injury of corneal sensation during operation is more likely to develop but when the tumor is located in post-ganglionic divisions, only those one involving the v1 division are likely to injure the corneal sensation (7). One extraordinary threat which we have had exposed with was the occurrence of Herpes ophthalmicus and corneal perforation without painful complaint (9). Finally the ambulated patients would have face wash and sweating so water and sweat exposure to cornea is a real danger to an anesthetic cornea in everyday activities.
Advantages and disadvantages of the approaches:
Better following of the proximal portion of the5th nerve, better handling of subtentorial component, preparing a trans-lesional window to petroclinoidal junction in the case of cystic lesions are the advantages of Retrosigmoid (Suprameatal) approach and the threat to the vidian nerve damage is less probable than combined approach. On the other hand better visualization of all of the mass and neighboring structures, better access to interdurally entrapped solid masses and also better handling of the neighboring vessels are the advantages of the combined (Retrosigmoid + Subtemporal)approach while the threat of simultaneous damage to V and VII nerves is considerable in this approach.
Complications
Corneal anesthesia CSF leakage (direct, paradoxical), cranial nerve damage (other than fifth) and vascular injuries are some of the surgical complications. We have been exposed with two of them in our cases.
CSF leak after a retromastoid approach can drain through open mastoid air cells into the middle ear cavity and then through the Eustachian tube to present as CSF rhinorrhea. This type of leak has been referred to as paradoxical CSF rhinorrhea (5). Watertight dural closure should be the goal following any posterior fossa approach. In case 1, we have paradoxical CSF leakage from the mastoid air cell origin in the third week of post-operation period which sealed by fat and glue successfully.
Main clues and tools indicating the diagnosis:
Any long lasting lesions involving the Meckel’s cave. In other words any lesion involving the middle and the posterior fossa could be indicative of the presence of the 5th nerve neurinoma. However bone window CT scan to clarify the extent of bone destruction and to define neighboring bony structures (middle ear , Petrous Tip and Meckel’s cave) and also brain MRI± GAD T1,T2 coronal and sagittal are the main diagnostic tools.
We should remember that the location of the 5th nerve neurinoma includes subtentorial Intradural, supratentorial Intradural and pure Interdural in some of them.
Conclusions
In general neurosurgery preoperative list of differential diagnosis should be limited and indicative of real anatomopathology in order to get the best result intra operatively and post-operatively. In order to have a safe surgical result, we do recommend that any masses located in the boundary of middle and posterior fossa in the Mediobasal portion (Meckel’s Cave), should be defined delicately by skull base CT scan. In the cases of solid masses with different consistency we should keep in mind that, whether it is inter-dural or intra-durally located. We do also recommend pre-operative full examination of corneal sensation, facial motor function (blinking) and tearing status. Early Post-op examination of VII nerve function and corneal sensation are another recommendation. Occurrence of herpes ophthalmicus in any of such approaches is an ominous symptom in favor of the development of painless corneal perforation. At last warning the patient of corneal anesthesia in the cases of combined approaches because of the possible simultaneous damage to V and VII nerve should be considered. Consultation with an expert ophthalmologist for corneal care and temporary tarsoraphy if necessary is also recommended.
Funding
None declared.
Conflicts of Interest
The authors declare that they have no competing interests.
References
- Smith JH, Cutrer FM. Numbness matters: A clinical review of trigeminal neuropathy. Cephalalgia [Internet]. SAGE Publications; 2011 May 31;31(10):1131–44. Available from: http://dx.doi.org/10.1177/0333102411411203
- Nurmikko TJ, Eldridge PR. Trigeminal neuralgia--pathophysiology, diagnosis and current treatment. Br J Anaesth. 2001 Jul;87(1):117-32.
- Chikalo II. Oftalmol Zh. Entrance of amino acids into the cornea through the aqueous humor of the eye. (Apropos of the nourishment of the cornea with special reference to the graft in penetrating keratoplasty). 1965;20(5):364-7 [Article in Russian].
- Schiefer U, Wilhelm H, Hart W, editors. Clinical Neuro-Ophthalmology: A Practical Guide. Springer-Verlag Berlin Heidelberg; 2007.
- Nanda A. Principles of Posterior Fossa Surgery. J NeuroIntervent Surg. 2012;4:234 doi:10.1136/neurintsurg-2012-010300.
- Krachmer Jay H, Mannis MJ, Holland, Edward J. Cornea. 2nd ed. Philadelphia, Elselvier Mosby; 2005. pp. 615-28.
- Samii M, Gerganov V. Surgery of Cerebellopontine Lesions. Springer-Verlag Berlin Heidelberg; 2013. 10.1007/978-3-642-35422-9.
- Arteaga P.A, Goyal J. Neuro-Ophthalmology. McGraw-Hill; 2011.
- Sanjay S1, Huang P, Lavanya R. Herpes zoster ophthalmicus. Curr Treat Options Neurol. 2011 Feb;13(1):79-91. doi: 10.1007/s11940-010-0098-1.
Type of Study: Case report |
Subject:
Gamma Knife Radiosurgery
References
1. Smith JH, Cutrer FM. Numbness matters: A clinical review of trigeminal neuropathy. Cephalalgia [Internet]. SAGE Publications; 2011 May 31;31(10):1131–44. Available from: http://dx.doi.org/10.1177/0333102411411203 [DOI:10.1177/0333102411411203]
2. Nurmikko TJ, Eldridge PR. Trigeminal neuralgia--pathophysiology, diagnosis and current treatment. Br J Anaesth. 2001 Jul;87(1):117-32. [DOI:10.1093/bja/87.1.117] [PMID]
3. Chikalo II. Oftalmol Zh. Entrance of amino acids into the cornea through the aqueous humor of the eye. (Apropos of the nourishment of the cornea with special reference to the graft in penetrating keratoplasty). 1965;20(5):364-7 [Article in Russian].
4. Schiefer U, Wilhelm H, Hart W, editors. Clinical Neuro-Ophthalmology: A Practical Guide. Springer-Verlag Berlin Heidelberg; 2007. [DOI:10.1007/978-3-540-32708-0]
5. Nanda A. Principles of Posterior Fossa Surgery. J NeuroIntervent Surg. 2012;4:234 doi:10.1136/neurintsurg-2012-010300. [DOI:10.1136/neurintsurg-2012-010300]
6. Krachmer Jay H, Mannis MJ, Holland, Edward J. Cornea. 2nd ed. Philadelphia, Elselvier Mosby; 2005. pp. 615-28.
7. Samii M, Gerganov V. Surgery of Cerebellopontine Lesions. Springer-Verlag Berlin Heidelberg; 2013. 10.1007/978-3-642-35422-9. [DOI:10.1007/978-3-642-35422-9]
8. Arteaga P.A, Goyal J. Neuro-Ophthalmology. McGraw-Hill; 2011.
9. Sanjay S1, Huang P, Lavanya R. Herpes zoster ophthalmicus. Curr Treat Options Neurol. 2011 Feb;13(1):79-91. doi: 10.1007/s11940-010-0098-1. [DOI:10.1007/s11940-010-0098-1]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |