Wed, May 8, 2024
Volume 3, Issue 2 (9-2017)
Iran J Neurosurg 2017, 3(2): 67-63 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Valderrama J, Garcia R, Satyarthee G, Calderon W, Hoz S, Narvaez-Rojas A et al . Intracranial Pial Arteriovenous Fistula Mimicking a Vein of Galen Aneurysm with Hydrocephalus Managed with Endovascular Method: Case Report. Iran J Neurosurg 2017; 3 (2) :67-63
URL: http://irjns.org/article-1-76-en.html
URL: http://irjns.org/article-1-76-en.html
Jorge Valderrama * 

 1, Ricardo Garcia2
1, Ricardo Garcia2 
 , Guru Satyarthee3
, Guru Satyarthee3 
 , Willem Calderon4
, Willem Calderon4 
 , Samer Hoz5
, Samer Hoz5 
 , Alexis Narvaez-Rojas6
, Alexis Narvaez-Rojas6 
 , Luis Moscote7
, Luis Moscote7 



 1, Ricardo Garcia2
1, Ricardo Garcia2 
 , Guru Satyarthee3
, Guru Satyarthee3 
 , Willem Calderon4
, Willem Calderon4 
 , Samer Hoz5
, Samer Hoz5 
 , Alexis Narvaez-Rojas6
, Alexis Narvaez-Rojas6 
 , Luis Moscote7
, Luis Moscote7 

1- National Institute of Neurology and Neurosurgery Manuel Velasco Suarez, Mexico City, Mexico , diplomadoneurotrauma@gmail.com
2- National Institute of Neurology and Neurosurgery Manuel Velasco Suarez, Mexico City, Mexico
3- Department of Neurosurgery, Jai Prakash Narayan Apex Trauma Center, All India Institute of Medical Sciences, New Delhi, India
4- Hospital General Dr.Manuel Gea González, Mexico City, Mexico
5- Neurosurgeon, Neurosurgery Teaching Hospital, Baghdad, Iraq
6- The National Autonomous University of Nicaragua, Managua, Nicaragua
7- Department of Neurosurgery, University of Cartagena, Colombia. Telephone: +57 5 6646183. rafaelmoscote21@gmail.com
2- National Institute of Neurology and Neurosurgery Manuel Velasco Suarez, Mexico City, Mexico
3- Department of Neurosurgery, Jai Prakash Narayan Apex Trauma Center, All India Institute of Medical Sciences, New Delhi, India
4- Hospital General Dr.Manuel Gea González, Mexico City, Mexico
5- Neurosurgeon, Neurosurgery Teaching Hospital, Baghdad, Iraq
6- The National Autonomous University of Nicaragua, Managua, Nicaragua
7- Department of Neurosurgery, University of Cartagena, Colombia. Telephone: +57 5 6646183. rafaelmoscote21@gmail.com
Full Text [PDF 1372 kb]
(2371 Downloads)
| Abstract (HTML) (5017 Views)
In 2012, Hetts et al. retrospectively reviewed the data of 25 patients with non-galenic arteriovenous fistula. They found 7.3% of pediatric intracranial vascular lesions with a nondual arteriovenous shunt. Seven cases that presented in the first month had congestive cardiac failure, with large, complex fistulas, but those presented later in childhood had comparatively simple angioarchitecture with predominantly single arterial feeder and usually presented with seizure. The researchers concluded that patients presenting in the first two years of life were more likely to have a multi-hole fistula and had poorer clinical outcome [13].
Initial imaging is CT scan as it is easily available, less costly as well as less time consuming. Although MRI of the brain delineates the lesion better, the gold standard is still digital subtraction angiography and confirms the diagnosis of IPAVF and aids in planning on the therapeutic program, either surgical or endovascular, while endovascular treatment can be carried out in the same setting.
Management of IPAVF poses a challenge to both neurosurgical and neurointerventional teams as it is associated with high mortality and poor neurological outcome irrespective of the treatment used. The occlusion of the arteriovenous shunt is necessary [5,13,14].
The treatment should be decided according to both neurosurgical as well as neurointerventional team available at the treatment center. The endovascular approach allows radiological delineation of venous and arterial part of the pial fistula, even if the vein is enlarged to form varicose veins, which is a quite common association. However, an engorged, tortuous, dilated, arterialized and varicose vein makes surgical exploration tedious.
Full Text: (1538 Views)
Background and Importance
Intracranial pial arteriovenous fistula (IPAVF) is a group of infrequently occurring vascular malformation in children [1-7]. IPAVF represents a subpial vascular malformation with high-flow shunt fed by mostly one or more pial arterial feeders and drainage by a solitary vein and lacking nidus [1,3,4]. Characteristically, these pediatric cases become symptomatic with catastrophic presentations. Thus, early treatment is advised for good neurological outcome. Intracranial pial arteriovenous fistulas can be managed by either endovascular method or direct attack of craniotomy with surgical resection or rarely a combination of procedures [5-7].
Case Presenation
A 2-year-old boy was referred to the emergency department with macrocrania and seizures.
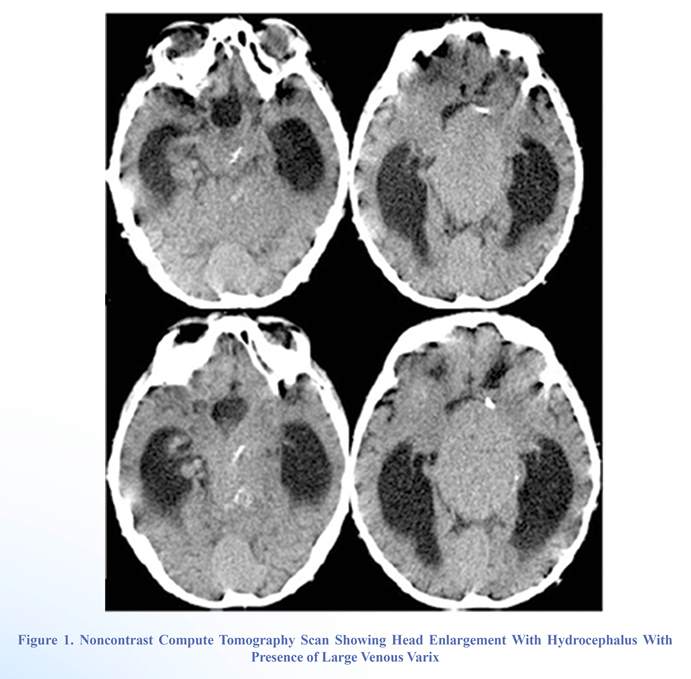
Eight months before that, his mother had noticed signs which suggested psychomotor development retardation (PDR). His mental status was postictal. The patient had normal vital signs with the physical examination otherwise being unremarkable. Axial computed tomography (CT) scan of the brain without contrast showed hydrocephalus, a hyperdense vein of Galen in the midline and associated enlarged straight sinus. The probable diagnosis could be an aneurysm of the vein of Galen (Figure 1).
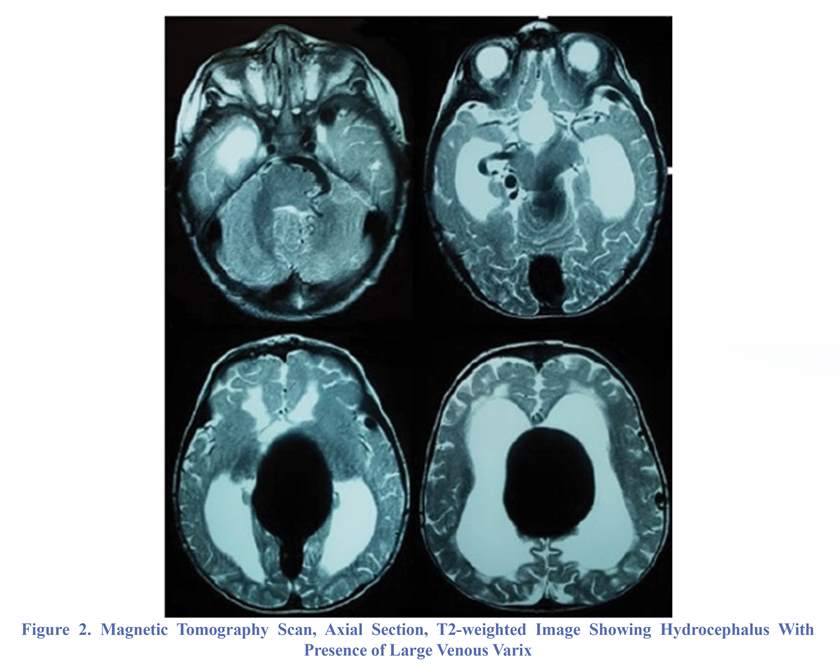
Magnetic resonance imaging (MRI) was performed in which an enlargement of the right posterior cerebral artery at the level of the circle of Willis and a large dilated vascular structure in the upper portion were found (Figure 2). To further delineate the architecture of vascular lesion, a digital subtraction angiography was carried out, right internal carotid and vertebral injection angiograms demonstrated the presence of a high-flow fistula being supplied by the right posterior cerebral artery (PCA) and the fistula was draining into the straight sinus (Figure 3). However, no intervening nidus could be identified. The child underwent endovascular embolization in order to reduce high-flow arteriovenous shunt (Figure 4). He tolerated the procedure well and was discharged with a good clinical condition.
Conclusion
An IPAVF is characterized by the presence of a direct arteriovenous connection with high-flow shunt located in the subpial space [6]. Most of the arteries feeding the IPAVF are drained into a single vein, which becomes dilated, elongated and tortuous due to high flow. They also become arterialized and often associated with a giant varicose vein [10,12]. These IPAVFs have single or multiple arterial feeders [6,7,10-12]. An IPAVF is usually congenital in nature in most cases, but may occasionally occur following head trauma, cranial surgery, or brain ischemia and after an episode of cortical vein thrombosis [8].
Intracranial pial arteriovenous fistula accounts for about 4.7% of pial arteriovenous malformations [11]. High-flow fistula causes hyperdynamic circulation leading to increased circulatory volume with intracranial venous hypertension, and increased cardiac load. Intracranial venous hypertension can cause congestive cardiac failure in the neonates, and some children may develop seizures, and rupture of intracranial arterialized cortical veins can lead to intracranial intracerebral, intraventricular, and subarachnoid hemorrhage. During infancy, intracranial venous hypertension may lead to hydrocephalus development. The current case also had head circumference enlargement which was noticed by the parents in the second year [6].
Intracranial pial arteriovenous fistula (IPAVF) is a group of infrequently occurring vascular malformation in children [1-7]. IPAVF represents a subpial vascular malformation with high-flow shunt fed by mostly one or more pial arterial feeders and drainage by a solitary vein and lacking nidus [1,3,4]. Characteristically, these pediatric cases become symptomatic with catastrophic presentations. Thus, early treatment is advised for good neurological outcome. Intracranial pial arteriovenous fistulas can be managed by either endovascular method or direct attack of craniotomy with surgical resection or rarely a combination of procedures [5-7].
Case Presenation
A 2-year-old boy was referred to the emergency department with macrocrania and seizures.
Eight months before that, his mother had noticed signs which suggested psychomotor development retardation (PDR). His mental status was postictal. The patient had normal vital signs with the physical examination otherwise being unremarkable. Axial computed tomography (CT) scan of the brain without contrast showed hydrocephalus, a hyperdense vein of Galen in the midline and associated enlarged straight sinus. The probable diagnosis could be an aneurysm of the vein of Galen (Figure 1).
Magnetic resonance imaging (MRI) was performed in which an enlargement of the right posterior cerebral artery at the level of the circle of Willis and a large dilated vascular structure in the upper portion were found (Figure 2). To further delineate the architecture of vascular lesion, a digital subtraction angiography was carried out, right internal carotid and vertebral injection angiograms demonstrated the presence of a high-flow fistula being supplied by the right posterior cerebral artery (PCA) and the fistula was draining into the straight sinus (Figure 3). However, no intervening nidus could be identified. The child underwent endovascular embolization in order to reduce high-flow arteriovenous shunt (Figure 4). He tolerated the procedure well and was discharged with a good clinical condition.
Conclusion
An IPAVF is characterized by the presence of a direct arteriovenous connection with high-flow shunt located in the subpial space [6]. Most of the arteries feeding the IPAVF are drained into a single vein, which becomes dilated, elongated and tortuous due to high flow. They also become arterialized and often associated with a giant varicose vein [10,12]. These IPAVFs have single or multiple arterial feeders [6,7,10-12]. An IPAVF is usually congenital in nature in most cases, but may occasionally occur following head trauma, cranial surgery, or brain ischemia and after an episode of cortical vein thrombosis [8].
Intracranial pial arteriovenous fistula accounts for about 4.7% of pial arteriovenous malformations [11]. High-flow fistula causes hyperdynamic circulation leading to increased circulatory volume with intracranial venous hypertension, and increased cardiac load. Intracranial venous hypertension can cause congestive cardiac failure in the neonates, and some children may develop seizures, and rupture of intracranial arterialized cortical veins can lead to intracranial intracerebral, intraventricular, and subarachnoid hemorrhage. During infancy, intracranial venous hypertension may lead to hydrocephalus development. The current case also had head circumference enlargement which was noticed by the parents in the second year [6].
In 2012, Hetts et al. retrospectively reviewed the data of 25 patients with non-galenic arteriovenous fistula. They found 7.3% of pediatric intracranial vascular lesions with a nondual arteriovenous shunt. Seven cases that presented in the first month had congestive cardiac failure, with large, complex fistulas, but those presented later in childhood had comparatively simple angioarchitecture with predominantly single arterial feeder and usually presented with seizure. The researchers concluded that patients presenting in the first two years of life were more likely to have a multi-hole fistula and had poorer clinical outcome [13].
Initial imaging is CT scan as it is easily available, less costly as well as less time consuming. Although MRI of the brain delineates the lesion better, the gold standard is still digital subtraction angiography and confirms the diagnosis of IPAVF and aids in planning on the therapeutic program, either surgical or endovascular, while endovascular treatment can be carried out in the same setting.
Management of IPAVF poses a challenge to both neurosurgical and neurointerventional teams as it is associated with high mortality and poor neurological outcome irrespective of the treatment used. The occlusion of the arteriovenous shunt is necessary [5,13,14].
The treatment should be decided according to both neurosurgical as well as neurointerventional team available at the treatment center. The endovascular approach allows radiological delineation of venous and arterial part of the pial fistula, even if the vein is enlarged to form varicose veins, which is a quite common association. However, an engorged, tortuous, dilated, arterialized and varicose vein makes surgical exploration tedious.
Under certain circumstances, surgical method may be the only option, for instance, in cases where embolization is dangerous or catheterization of smaller feeder vessels is not possible or unfits due to angioarchitecture of IPAVF [14]. Cases with IPAVF require regular follow-up to check for new dural IPAVF development and recanalization [12,14].
Every child with focal neurological deficit along with enlarging head should be investigated for suspected IPAVF, although its occurrence is extremely rare. The authors of present case report advocate cranial screening with computed tomography for suspected early diagnosis and providing an opportunity to preserve good neurological outcomes after digital angiography as well as providing a tailor-made treatment.
Funding
None
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contribution
Conception and Design: Luis Rafael Moscote-Salazar
Data Collection: Jorge Valderrama, Ricardo Garcia, Guru Satyarthee, Willem Guillermo Calderon-Miranda, Luis Rafael Moscote-Salazar
Drafting the Article: Willem Guillermo Calderon-Miranda, Samer Hoz, Alexis Narvaez Rojas, Luis Rafael Moscote-Salazar
Critically Revising the Article: Samer Hoz, Alexis Narvaez Rojas, Luis Rafael Moscote-Salazar
Reviewed Submitted Version of the Manuscript: All authors
Approved the Final Version of the Manuscript: All authors
References
1. Mirza FA, Fraser JF. Multiple Dural and Pial Arteriovenous Fistulae in a Twenty-Four-Year-Old Woman in the Setting of Superior Sagittal Sinus Thrombosis: Case Report and Review of Literature. J Stroke Cerebrovasc Dis. 2016;25(10):e192-9.
2. Yu J, Shi L, Lv X, Wu Z, Yang H. Intracranial non-galenic pial arteriovenous fistula: A review of the literature. Interv Neuroradiol. 2016;22(5):557-68.
3. Hetts SW, Moftakhar P, Maluste N, Fullerton HJ, Cooke DL, Amans MR, et al. Pediatric intracranial dural arteriovenous fistulas: age-related differences in clinical features, angioarchitecture, and treatment outcomes. J Neurosurg Pediatr. 2016;18(5):602-10.
4. Kraneburg UM, Nga VD, Ting EY, Hui FK, Lwin S, Teo C, Chou N, Yeo TT. Intracranial pial arteriovenous fistula in infancy: a case report and literature review. Childs Nerv Syst: ChNS Off J Int Soc Pediatr Neurosurg 2014;30(2):365–369.
5. Madsen PJ, Lang SS, Pisapia JM, Storm PB, Hurst RW, Heuer GG. An institutional series and literature review of pial arteriovenous fistulas in the pediatric population: clinical article. Neurosurg Pediatr. 2013;12(4):344–50.
6. Lasjaunias P, ter Brugge KG, Berenstein A. Cerebral arteriovenous fistulas. In: Lasjaunias P, ter Brugge KG, Berenstein A, eds. Surgical neuroangiography, vol 3. 2nd ed. Berlin: Springer-Verlag Berlin Heidelberg; 2006. p. 227–89.
7. Weon YC, Yoshida Y, Sachet M, Mahadevan J, Alvarez H, Rodesch G, Lasjaunias P. Supratentorial cerebral arteriovenous fistulas (AVFs) in children: review of 41 cases with 63 nonchoroidal single-hole AVF. Acta Nerochir. 2005; 147(1):17–31.
8. Nishiyama Y, Kanemaru K, Yoshioka H, Hanihara M, Horikoshi T, Kinouchi H Intracranial pial arteriovenous fistula caused by dural tenting: case report. Neurol Med Chir. 2014;54(3):242-4. doi:10.2176/nmc.cr2012-0239
9. Panigrahi S, Mishra SS, Das S, Parida DK. Intracerebralpialarteriovenous fistula with large venous varix: a rare case report. Surg Neurol Int. 2013;4:22.
10. Paramasivam S, Toma N, Niimi Y, Berenstein. A Development, clinical presentation and endovascular management of congenital intracranial pial arteriovenous fistulas. J Neurointerv Surg. 2013;5(3):184–90.
11. Tomlinson FH, Rüfenacht DA, Sundt TM Jr, Nichols DA, Fode NC. Arteriovenous fistulas of the brain and the spinal cord. J Neurosurg 1993;79(1):16–27.
12. Requejo, F., Jaimovich, R., Marelli, J. et al. Intracranial pial fistulas in pediatric population. Clinical features and treatment modalities. Childs Nerv Syst. 2015;31(9):1509-14.
13. Hetts SW, Keenan K, Fullerton HJ, Young WL, English JD, Gupta N, Dowd CF, Higashida RT, Lawton MT, Halbach VV. Pediatric intracranial nongalenic pial arteriovenous fistulas: clinical features, angioarchitecture, and outcomes. AJNR Am J Neuroradiol. 2012;33(9):1710–9.
14. Nelson PK, Nimmy Y, Lasjaunias P, et al. Endovascular embolization of congenital intracranial pial arteriovenous fistulas. Neuroimaging Clin N Am. 1999;2(2):309–17.
15. Sugimoto T, Park YS, Nakagawa I, Nishimura F, Motoyama Y, Nakase H. Effectiveness of intraoperative indocyanine green video angiography in direct surgical treatment of pediatric intracranial pial arteriovenous fistula. J Neurosurg Pediatr. 2015;15(1):55–9.
Type of Study: Case report |
References
1. Mirza FA, Fraser JF. Multiple Dural and Pial Arteriovenous Fistulae in a Twenty-Four-Year-Old Woman in the Setting of Superior Sagittal Sinus Thrombosis: Case Report and Review of Literature. J Stroke Cerebrovasc Dis. 2016;25(10):e192-9. [DOI:10.1016/j.jstrokecerebrovasdis.2016.07.037] [PMID]
2. Yu J, Shi L, Lv X, Wu Z, Yang H. Intracranial non-galenic pial arteriovenous fistula: A review of the literature. Interv Neuroradiol. 2016;22(5):557-68. [DOI:10.1177/1591019916653934] [PMID] [PMCID]
3. Hetts SW, Moftakhar P, Maluste N, Fullerton HJ, Cooke DL, Amans MR, et al. Pediatric intracranial dural arteriovenous fistulas: age-related differences in clinical features, angioarchitecture, and treatment outcomes. J Neurosurg Pediatr. 2016;18(5):602-10. [DOI:10.3171/2016.5.PEDS15740] [PMID]
4. Kraneburg UM, Nga VD, Ting EY, Hui FK, Lwin S, Teo C, Chou N, Yeo TT. Intracranial pial arteriovenous fistula in infancy: a case report and literature review. Childs Nerv Syst: ChNS Off J Int Soc Pediatr Neurosurg 2014;30(2):365–369. [DOI:10.1007/s00381-013-2217-2] [PMID]
5. Madsen PJ, Lang SS, Pisapia JM, Storm PB, Hurst RW, Heuer GG. An institutional series and literature review of pial arteriovenous fistulas in the pediatric population: clinical article. Neurosurg Pediatr. 2013;12(4):344–50. [DOI:10.3171/2013.6.PEDS13110] [PMID]
6. Lasjaunias P, ter Brugge KG, Berenstein A. Cerebral arteriovenous fistulas. In: Lasjaunias P, ter Brugge KG, Berenstein A, eds. Surgical neuroangiography, vol 3. 2nd ed. Berlin: Springer-Verlag Berlin Heidelberg; 2006. p. 227–89.
https://doi.org/10.1007/978-3-540-68320-9_5 [DOI:10.1007/978-3-540-68320-9_4]
7. Weon YC, Yoshida Y, Sachet M, Mahadevan J, Alvarez H, Rodesch G, Lasjaunias P. Supratentorial cerebral arteriovenous fistulas (AVFs) in children: review of 41 cases with 63 nonchoroidal single-hole AVF. Acta Nerochir. 2005; 147(1):17–31. [DOI:10.1007/s00701-004-0341-1] [PMID]
8. Nishiyama Y, Kanemaru K, Yoshioka H, Hanihara M, Horikoshi T, Kinouchi H Intracranial pial arteriovenous fistula caused by dural tenting: case report. Neurol Med Chir. 2014;54(3):242-4. doi:10.2176/nmc.cr2012-0239 [DOI:10.2176/nmc.cr2012-0239]
9. Panigrahi S, Mishra SS, Das S, Parida DK. Intracerebralpialarteriovenous fistula with large venous varix: a rare case report. Surg Neurol Int. 2013;4:22. [DOI:10.4103/2152-7806.107891] [PMID] [PMCID]
10. Paramasivam S, Toma N, Niimi Y, Berenstein. A Development, clinical presentation and endovascular management of congenital intracranial pial arteriovenous fistulas. J Neurointerv Surg. 2013;5(3):184–90. [DOI:10.1136/neurintsurg-2011-010241] [PMID]
11. Tomlinson FH, Rüfenacht DA, Sundt TM Jr, Nichols DA, Fode NC. Arteriovenous fistulas of the brain and the spinal cord. J Neurosurg 1993;79(1):16–27. [DOI:10.3171/jns.1993.79.1.0016] [PMID]
12. Requejo, F., Jaimovich, R., Marelli, J. et al. Intracranial pial fistulas in pediatric population. Clinical features and treatment modalities. Childs Nerv Syst. 2015;31(9):1509-14. [DOI:10.1007/s00381-015-2778-3] [PMID]
13. Hetts SW, Keenan K, Fullerton HJ, Young WL, English JD, Gupta N, Dowd CF, Higashida RT, Lawton MT, Halbach VV. Pediatric intracranial nongalenic pial arteriovenous fistulas: clinical features, angioarchitecture, and outcomes. AJNR Am J Neuroradiol. 2012;33(9):1710–9. [DOI:10.3174/ajnr.A3194] [PMID]
14. Nelson PK, Nimmy Y, Lasjaunias P, et al. Endovascular embolization of congenital intracranial pial arteriovenous fistulas. Neuroimaging Clin N Am. 1999;2(2):309–17.
15. Sugimoto T, Park YS, Nakagawa I, Nishimura F, Motoyama Y, Nakase H. Effectiveness of intraoperative indocyanine green video angiography in direct surgical treatment of pediatric intracranial pial arteriovenous fistula. J Neurosurg Pediatr. 2015;15(1):55–9. [DOI:10.3171/2014.9.PEDS13683] [PMID]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |