Fri, Jul 11, 2025
Volume 4, Issue 1 (Winter 2018)
Iran J Neurosurg 2018, 4(1): 19-24 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rezvani M, Mohamadhoseini E, Rastgoo A, Kamangar M, Noorian M. Prognosis of Cauda Equina Syndrome Caused by Herniated Disk After Lumbar Disk Operation. Iran J Neurosurg 2018; 4 (1) :19-24
URL: http://irjns.org/article-1-104-en.html
URL: http://irjns.org/article-1-104-en.html
Majid Rezvani1 

 , Ehsan Mohamadhoseini *2
, Ehsan Mohamadhoseini *2 

 , Amin Rastgoo1
, Amin Rastgoo1 

 , Mohammad Kamangar1
, Mohammad Kamangar1 

 , Mohammad-Amin Noorian1
, Mohammad-Amin Noorian1 




 , Ehsan Mohamadhoseini *2
, Ehsan Mohamadhoseini *2 

 , Amin Rastgoo1
, Amin Rastgoo1 

 , Mohammad Kamangar1
, Mohammad Kamangar1 

 , Mohammad-Amin Noorian1
, Mohammad-Amin Noorian1 


1- Department of Surgery, Al-Zahra Hospital, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Department of Surgery, Al-Zahra Hospital, Isfahan University of Medical Sciences, Isfahan, Iran. ,ehsan_m_h76@yahoo.com
2- Department of Surgery, Al-Zahra Hospital, Isfahan University of Medical Sciences, Isfahan, Iran. ,
Full Text [PDF 555 kb]
(2833 Downloads)
| Abstract (HTML) (6350 Views)
Full Text: (2297 Views)
1. Introduction
Cauda Equina Syndrome (CES) is due to several lumbar and sacral nerve roots dysfunction in the lumbar channel. This radical dysfunction can produce a combination of clinical effects, but the term CES is only used once this clinical presentation involves sexual, intestinal, bladder dysfunction and numbness around the anus or the “saddle area” [1].The conus medullaris is the tapered, lower end of the spinal cord. It occurs near lumbar vertebral levels 1(L1) and 2(L2), occasionally lower. The upper end of the conus medullaris is usually not well defined. After the spinal cord tapers out, the spinal nerves continue to branch out diagonally, forming the cauda equina. The pia mater that surrounds the spinal cord, however, projects directly downward, forming a slender filament called the filum terminale, which connects the conus medullaris to the back of the coccyx. The filum terminale provides a connection between the conus medullaris and the coccyx which stabilizes the entire spinal cord [1].
In a study in Slovenia, the annual incidence of CES was estimated about 1.8 per million people. Considering the annual incidence rate of symptomatic disk herniation in the United States (1500 per million), an estimated score of 12% of herniated disks trigger CES every year [2]. Clinically, a history based on the lack of sensation around the anus and sphincter disorder (with or without urinary retention) can reveal the presence of a CES [3].
Three classic patterns of this syndrome have been described. This disorder can be manifested as follows: acute and as the first symptom of the lumbar disk herniation (type 1); as a last resort on a long history of chronic low back pain with or without sciatica (type 2); or gradually, with slow progress toward anaesthesia and urinary symptoms (type 3) [3, 4].
The most common cause of CES is the pressure caused by large central lumbar disk herniation at L5/L4 and S1/L5 levels. According to Park et al. there is a region with reduced blood vessels in the proximal section of the cauda equina root. Changes in blood pressure caused by pressure on the nerve root can be more important in this part of the neural roots than elsewhere and its rapid changes may lead to less compatibility with slower start-ups. Patients with congenital stenosis of the spinal canal or its acquired stenosis due to the combination of degenerative disk changes and posterior segmental joints, followed by thickening of the ligamentum flavum and shortening of channel cross-sectional area, are likely to develop CES [5]. Intradural disk has been reported as one of the rare causes of CES [6].
Various other factors with a lower prevalence have also been mentioned for CES; i.e. vertebrae damage in the form of fracture or dislocation. Primary or metastatic vertebral neoplasms can cause pressure, usually accompanied by obvious pain, often as a chronic condition. Infections associated with the formation of abscess or bone involvement, inside the spinal canal and with pressure on it, can cause CES. The vertebral column is the most common skeletal location for tuberculosis, and Pott paralysis is well-known term in the literature.
A wide range of iatrogenic causes including manipulation, spinal anaesthesia and postoperative complications like hematoma are also implicated as the cause of this syndrome. Other lesions such as nerve sheet tumours, schwannomas, ependymoma, synovial cysts, tarlov cysts, varicose veins and hydatid cysts have also been identified [7].
In case of CES suspicion, it is necessary to perform a neurological examination of the legs, including sensation around the anus, and an examination of the anus tone. Sensation around the anus can be pushed out to the sphincter with a mild blow (covered with gloves), or if uncertain, with a tissue cloth, or an open paper binder. Afterwards, a rectal examination can also be performed. Loss or decrease in bulbocavernosus reflex (clitoris or glans stimulation lead to contracts of the sphincter of the anus) can be a sign of CES, as the reflex is mediated by the sacral roots [8].
Surgical urgency for this disorder is controversial. CES causes a lack of sphincter control, in case of pressure on the nerve. So, optimal treatment should relieve surgical pressure in the shortest possible time. Ethical considerations prevented various studies to test this hypothesis and it is difficult to prove it by revising the articles on retrospective and cohort studies (level 3 evidence) for two reasons: first, it is difficult to determine the exact time that the symptoms have started.
Therefore, it is be difficult to determine the time lag between symptom onset and surgery. Second, any discussion in this area is ambiguous due to the large number of published articles (mostly retrospective) in the form of case series containing a mixture of patients with incomplete CES and those with CES accompanied by retention [9]. This study aimed to determine the prognosis of Cauda Equina Syndrome caused by herniated disk after lumbar disk surgery in patients referring to Al-Zahra Hospital of Isfahan City, Iran from 2013 to 2015.
2. Methods and Materials/Patients
This was a cross-sectional study carried out at Al-Zahra Hospital in Isfahan City, Iran from 2013 to 2015. Our samples included 33 patients diagnosed with CES, admitted to the hospital from the beginning of 2013 to the end of 2015. This study included all confirmed cases of CES who had related medical and hospital records and were accessible at any time.
Also, a defect in the patient’s medical record and the inaccessibility to the patient or family to complete the information and not referring of patients for post-operation follow-up were considered as exclusion criteria. The sampling method was total enumerative i.e., all patients with CES who were operated in this hospital from the beginning of 2013 to the end of 2015.
The statistical population consisted of 33 people. Since the beginning of 2013, patients referred to Al-Zahra Hospital who met the study criteria, were enrolled into the research and their demographic data, symptoms and history of their illness were recorded in the data collection forms (this form included two parts of demographic and clinical data) after obtaining their consent to participate in the study. The patients were evaluated in terms of recovery, presence of sensory disorders, sphincter problems, muscle weakness and leg weakness according to Oxford scale one day, one month, six months, and two years after the operation and the results obtained were registered in individual profiles. The Oxford scale measures patients’ muscle strength on a scale of 0 to 5 [10].
Eventually, the collected data were analysed by SPSS (version 22) using Independent samples t-test (to compare the quantitative data between two groups), Chi-square (to compare the qualitative data between levels of each variable), ANOVA (to compare the quantitative data between the two groups and Mann-Whitney U test (to compare the ordinal data between the two groups) at significant level of 0.05.
3. Results
In this study, 33 patients with Cauda Equina Syndrome were studied and evaluated. The mean (SD) duration of disease (from symptoms’ manifestation to surgical intervention) was 8.9(±6.4) day. This period was more than 48 hours in 15(45.5%) patients and was 48 hours or less in 18(54.5%) patients. The mean (SD) age of the patients was 48.9(±13.5) year (range: 29-79 y) and 28(84.8%) patients were male. The mean (SD) BMI of the patients was 28.63(3.96)kg/m2. Of all subjects, 7(21.2%) had normal weight, 10(30.3%) were overweight, and 16(48.5%) were obese.
The level of involvement in 22(66.7%) cases was L4-L5, in 4(12.1%) was L3-L4, in another 4(12.1%) was L5-S1, and in 3(9.1%) was L2-L3. All 33 patients (100%) had sensory impairment. Also, all 33 patients had varying degrees of muscle and leg weakness, observed on the right side of 9(27.3%) patients, on the left in 15(45.4%), and bilaterally in 9(27.3%) patients. Nineteen (57.6%) patients suffered from sphincter disorder and all suf
Cauda Equina Syndrome (CES) is due to several lumbar and sacral nerve roots dysfunction in the lumbar channel. This radical dysfunction can produce a combination of clinical effects, but the term CES is only used once this clinical presentation involves sexual, intestinal, bladder dysfunction and numbness around the anus or the “saddle area” [1].The conus medullaris is the tapered, lower end of the spinal cord. It occurs near lumbar vertebral levels 1(L1) and 2(L2), occasionally lower. The upper end of the conus medullaris is usually not well defined. After the spinal cord tapers out, the spinal nerves continue to branch out diagonally, forming the cauda equina. The pia mater that surrounds the spinal cord, however, projects directly downward, forming a slender filament called the filum terminale, which connects the conus medullaris to the back of the coccyx. The filum terminale provides a connection between the conus medullaris and the coccyx which stabilizes the entire spinal cord [1].
In a study in Slovenia, the annual incidence of CES was estimated about 1.8 per million people. Considering the annual incidence rate of symptomatic disk herniation in the United States (1500 per million), an estimated score of 12% of herniated disks trigger CES every year [2]. Clinically, a history based on the lack of sensation around the anus and sphincter disorder (with or without urinary retention) can reveal the presence of a CES [3].
Three classic patterns of this syndrome have been described. This disorder can be manifested as follows: acute and as the first symptom of the lumbar disk herniation (type 1); as a last resort on a long history of chronic low back pain with or without sciatica (type 2); or gradually, with slow progress toward anaesthesia and urinary symptoms (type 3) [3, 4].
The most common cause of CES is the pressure caused by large central lumbar disk herniation at L5/L4 and S1/L5 levels. According to Park et al. there is a region with reduced blood vessels in the proximal section of the cauda equina root. Changes in blood pressure caused by pressure on the nerve root can be more important in this part of the neural roots than elsewhere and its rapid changes may lead to less compatibility with slower start-ups. Patients with congenital stenosis of the spinal canal or its acquired stenosis due to the combination of degenerative disk changes and posterior segmental joints, followed by thickening of the ligamentum flavum and shortening of channel cross-sectional area, are likely to develop CES [5]. Intradural disk has been reported as one of the rare causes of CES [6].
Various other factors with a lower prevalence have also been mentioned for CES; i.e. vertebrae damage in the form of fracture or dislocation. Primary or metastatic vertebral neoplasms can cause pressure, usually accompanied by obvious pain, often as a chronic condition. Infections associated with the formation of abscess or bone involvement, inside the spinal canal and with pressure on it, can cause CES. The vertebral column is the most common skeletal location for tuberculosis, and Pott paralysis is well-known term in the literature.
A wide range of iatrogenic causes including manipulation, spinal anaesthesia and postoperative complications like hematoma are also implicated as the cause of this syndrome. Other lesions such as nerve sheet tumours, schwannomas, ependymoma, synovial cysts, tarlov cysts, varicose veins and hydatid cysts have also been identified [7].
In case of CES suspicion, it is necessary to perform a neurological examination of the legs, including sensation around the anus, and an examination of the anus tone. Sensation around the anus can be pushed out to the sphincter with a mild blow (covered with gloves), or if uncertain, with a tissue cloth, or an open paper binder. Afterwards, a rectal examination can also be performed. Loss or decrease in bulbocavernosus reflex (clitoris or glans stimulation lead to contracts of the sphincter of the anus) can be a sign of CES, as the reflex is mediated by the sacral roots [8].
Surgical urgency for this disorder is controversial. CES causes a lack of sphincter control, in case of pressure on the nerve. So, optimal treatment should relieve surgical pressure in the shortest possible time. Ethical considerations prevented various studies to test this hypothesis and it is difficult to prove it by revising the articles on retrospective and cohort studies (level 3 evidence) for two reasons: first, it is difficult to determine the exact time that the symptoms have started.
Therefore, it is be difficult to determine the time lag between symptom onset and surgery. Second, any discussion in this area is ambiguous due to the large number of published articles (mostly retrospective) in the form of case series containing a mixture of patients with incomplete CES and those with CES accompanied by retention [9]. This study aimed to determine the prognosis of Cauda Equina Syndrome caused by herniated disk after lumbar disk surgery in patients referring to Al-Zahra Hospital of Isfahan City, Iran from 2013 to 2015.
2. Methods and Materials/Patients
This was a cross-sectional study carried out at Al-Zahra Hospital in Isfahan City, Iran from 2013 to 2015. Our samples included 33 patients diagnosed with CES, admitted to the hospital from the beginning of 2013 to the end of 2015. This study included all confirmed cases of CES who had related medical and hospital records and were accessible at any time.
Also, a defect in the patient’s medical record and the inaccessibility to the patient or family to complete the information and not referring of patients for post-operation follow-up were considered as exclusion criteria. The sampling method was total enumerative i.e., all patients with CES who were operated in this hospital from the beginning of 2013 to the end of 2015.
The statistical population consisted of 33 people. Since the beginning of 2013, patients referred to Al-Zahra Hospital who met the study criteria, were enrolled into the research and their demographic data, symptoms and history of their illness were recorded in the data collection forms (this form included two parts of demographic and clinical data) after obtaining their consent to participate in the study. The patients were evaluated in terms of recovery, presence of sensory disorders, sphincter problems, muscle weakness and leg weakness according to Oxford scale one day, one month, six months, and two years after the operation and the results obtained were registered in individual profiles. The Oxford scale measures patients’ muscle strength on a scale of 0 to 5 [10].
Eventually, the collected data were analysed by SPSS (version 22) using Independent samples t-test (to compare the quantitative data between two groups), Chi-square (to compare the qualitative data between levels of each variable), ANOVA (to compare the quantitative data between the two groups and Mann-Whitney U test (to compare the ordinal data between the two groups) at significant level of 0.05.
3. Results
In this study, 33 patients with Cauda Equina Syndrome were studied and evaluated. The mean (SD) duration of disease (from symptoms’ manifestation to surgical intervention) was 8.9(±6.4) day. This period was more than 48 hours in 15(45.5%) patients and was 48 hours or less in 18(54.5%) patients. The mean (SD) age of the patients was 48.9(±13.5) year (range: 29-79 y) and 28(84.8%) patients were male. The mean (SD) BMI of the patients was 28.63(3.96)kg/m2. Of all subjects, 7(21.2%) had normal weight, 10(30.3%) were overweight, and 16(48.5%) were obese.
The level of involvement in 22(66.7%) cases was L4-L5, in 4(12.1%) was L3-L4, in another 4(12.1%) was L5-S1, and in 3(9.1%) was L2-L3. All 33 patients (100%) had sensory impairment. Also, all 33 patients had varying degrees of muscle and leg weakness, observed on the right side of 9(27.3%) patients, on the left in 15(45.4%), and bilaterally in 9(27.3%) patients. Nineteen (57.6%) patients suffered from sphincter disorder and all suf
fered from urinary incontinence, also 4(12.1%) cases had fecal incontinence.
According to the Oxford scale, the range of muscle weakness in these patients was between 0 and 3 (maximum score=5); 16(48.5%) patients with muscle strength of 0, 1(3%) person with muscle strength of 1, 3(9.1%) with muscle strength of 2, and 13(39.4%) had muscle strength of 3. Table 1 presents the frequency distribution of disorders types according to demographic and clinical characteristics of the patients. Accordingly, no significant difference was found in the presence of sphincter disorder in terms of age, gender and level of involvement; however, the patients with sphincter disorder had lower BMI (P=0.03). Muscle weakness was also not significantly different in terms of these characteristics.
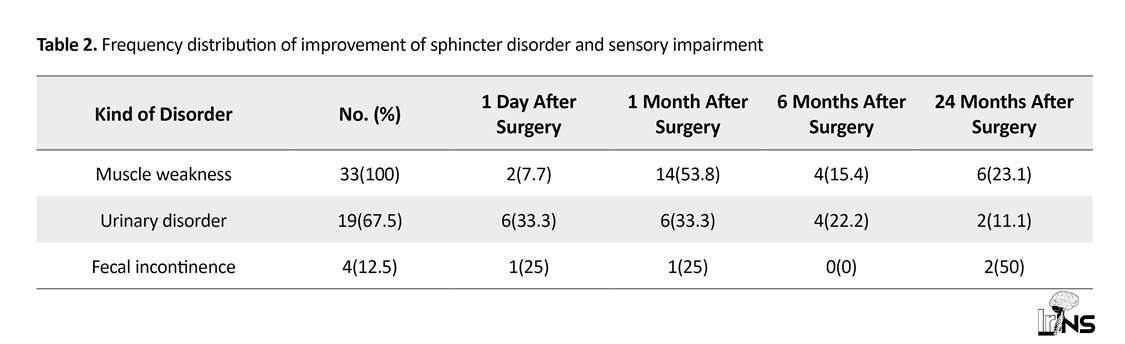
A 24-month follow-up of the patients showed an improved muscle weakness in 26(78.8%) subjects so that 2(7.7%) of them recovered one day after the surgery, 14(53.8%) one month later, 4(15.4%) within 6 months later, 6(23.1%) within 24 months post-operation, and 7(21.2%) cases did not show any changes. Out of 19 patients with urinary dysfunction, 18(94.7%) patients recovered that 6(33.3%) of them improved in one day, 6(33.3%) in one month, 4(2.22%) in 6 months, and 2(11.1%) 24 months after the surgery.
All 4 patients with stool disorder also recovered during the time of study (100%), i.e., 1(25%) person after one day, 1(25%) person within a month, and 2(50%) 24 months after the operation. Table 2 presents the frequency distribution of sensory and sphincter problem at 1 day, 1 month, 6 months, and 24 months after the operation.
Studying the status of muscle weakness recovery in patients with the onset of symptoms before surgery showed that all 15 patients with a disease duration of less than 48 hours recovered (100%), while the rate of recovery in patients with a duration of syndrome more than 48 hours was 38.9%, and a significant correlation was observed between improvement of muscle weakness and duration of the disease (P=0.007). Urinary disorder improved in 7(100%) patients with symptoms lasting less than 48 hours, and 11(91.7%) patients with symptom duration more than 48 hours also recovered. No significant difference was found between improvement of urinary disorder and duration of symptoms (P=0.99). All 4 patients with fecal disorder recovered (symptom lasted less than 48 hours in all of them). No significant difference was observed in disease symptoms according to the type of surgery. Table 3 presents the results.
4. Discussion
Cauda Equina Syndrome is a neurological emergency, because it can lead to sphincter disorders and incontinence of urinary and stool in the patients along with other local and paralytic symptoms, in case of contin
According to the Oxford scale, the range of muscle weakness in these patients was between 0 and 3 (maximum score=5); 16(48.5%) patients with muscle strength of 0, 1(3%) person with muscle strength of 1, 3(9.1%) with muscle strength of 2, and 13(39.4%) had muscle strength of 3. Table 1 presents the frequency distribution of disorders types according to demographic and clinical characteristics of the patients. Accordingly, no significant difference was found in the presence of sphincter disorder in terms of age, gender and level of involvement; however, the patients with sphincter disorder had lower BMI (P=0.03). Muscle weakness was also not significantly different in terms of these characteristics.
A 24-month follow-up of the patients showed an improved muscle weakness in 26(78.8%) subjects so that 2(7.7%) of them recovered one day after the surgery, 14(53.8%) one month later, 4(15.4%) within 6 months later, 6(23.1%) within 24 months post-operation, and 7(21.2%) cases did not show any changes. Out of 19 patients with urinary dysfunction, 18(94.7%) patients recovered that 6(33.3%) of them improved in one day, 6(33.3%) in one month, 4(2.22%) in 6 months, and 2(11.1%) 24 months after the surgery.
All 4 patients with stool disorder also recovered during the time of study (100%), i.e., 1(25%) person after one day, 1(25%) person within a month, and 2(50%) 24 months after the operation. Table 2 presents the frequency distribution of sensory and sphincter problem at 1 day, 1 month, 6 months, and 24 months after the operation.
Studying the status of muscle weakness recovery in patients with the onset of symptoms before surgery showed that all 15 patients with a disease duration of less than 48 hours recovered (100%), while the rate of recovery in patients with a duration of syndrome more than 48 hours was 38.9%, and a significant correlation was observed between improvement of muscle weakness and duration of the disease (P=0.007). Urinary disorder improved in 7(100%) patients with symptoms lasting less than 48 hours, and 11(91.7%) patients with symptom duration more than 48 hours also recovered. No significant difference was found between improvement of urinary disorder and duration of symptoms (P=0.99). All 4 patients with fecal disorder recovered (symptom lasted less than 48 hours in all of them). No significant difference was observed in disease symptoms according to the type of surgery. Table 3 presents the results.
4. Discussion
Cauda Equina Syndrome is a neurological emergency, because it can lead to sphincter disorders and incontinence of urinary and stool in the patients along with other local and paralytic symptoms, in case of contin
ued pressure on the spinal canal. Various studies have been carried out on the efficacy of different surgical procedures such as laminectomy, discectomy and vertebral fusion, but there is still no single theory to clarify to which extend these methods are effective and the differences in outcomes may be due to surgical skills, procedure, and symptoms duration before surgery [1].
Therefore, the present study was conducted with the aim of determining distribution of prognosis frequency in patients with CES in Al-Zahra Hospital in Isfahan City, Iran from 2013 to 2015. In this study, 33 patients with CES (age range:29-77y) were studied. The mean (SD) duration of symptoms before surgery was 8.9(6.4) day. Twenty-eight patients were male and the most common involved segment was L4-L5 observed in 22 cases.
Although intervertebral disk herniation symptoms are more common in young and middle-aged groups due to occupational causes, because of the progression of the disease on one hand and tendency of older people to develop the disease on the other hand, 50% of patients were 50 years or older. According to the results of our study, all 33 patients had sensory and muscular weakness and 19 suffered from sphincter disorder. Although the effect of surgery and urgency was still doubtful, all 33 patients underwent the operation.
A 2-year follow up of the patients showed that muscle weakness improved in 78.8% of them, specifically 7.7% of the patients recovered in one day, 53.8% within one month, 15.4% within six months, and 23.1% within 24 months after the operation. Also, 94.7% of patients with urinary disorder and 100% of patients with fecal dysfunction recovered within 24 months, and the prognosis of the treated patients was satisfactory altogether. Recent guidelines for treating patients with low back pain and neurological symptoms suggest that suspicious cases of CES be referred to surgery immediately, but due to the high percentage of false positives in clinical examinations, definitive diagnosis of the disease should be made by MRI, because even other imaging techniques, such as CT cannot fully confirm the presence of CES [11].
When a patient has clinical features of CES, and MRI confirms it, the current consensus recommends removal of pressure with surgery [9]. According to the results of our study, duration of symptoms prior to surgery affects the improvement of muscle weakness, but has no effect on the improvement rate of the sphincter problem. Results of a review study support that only incomplete CES requires urgent surgery to prevent bladder function degradation.
Based on the current study, in patients with CES accompanied by urinary disorder, the clinical outcome is undesirable in any case and does not correlate with the time of surgery. Therefore, such patients can wait until the next morning to perform an elective surgery, rather than suffer from a potentially difficult operation during the midnight while the conditions are less desirable. According to two recently published articles in the UK, the outcome is independent of the time of surgery [12].
A widely researched review article suggests that interventions within less than 48 hours of symptoms onset will result in a better outcome than delayed interventions after this period of time. These data have been selectively reconsidered, and it has been stated that the outcome of both types of CES (incomplete or with urinary retention) would be better with interventions within a 24-hour period compared to those after this time.
In another analysis of selective retrospective collections, the authors found that out of 47 patients undergoing surgery during the 24 hours, 41(87%) recovered with regard to the bladder function, while out of 46 patients who had undergone surgery after 24 hours only 2(4.3%) subjects improved [13]. Another research, supported the view that early surgery is associated with better results in incomplete CES, but less certain outcomes were found about CES with urinary retention [14].
5. Conclusion
According to the results of this study, the operation of the lumbar spine surgery leads to improvement in CES, including sphincter disorders and muscle weakness. However, due to the limitations of our study, including a small sample size, further studies are recommended to reach stronger conclusions.
Ethical Considerations
Compliance with ethical guidelines
The informed consent was obtained from the patients.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
The authors declared no conflict of interest. Conception and design: Majid Rezvani; Data Collection: Ehsan Mohamadhoseini, Amin Rastgoo, Mohammad Kamangar, Mohammad-Amin Noorian; Drafting the article: Ehsan Mohamadhoseini, Majid Rezvani, Amin Rastgoo, Mohammad Kamangar; Critically revising the article: All authors; Reviewing submitted version of manuscript: All authors; Approving the final version of the manuscript: All authors.
References
Therefore, the present study was conducted with the aim of determining distribution of prognosis frequency in patients with CES in Al-Zahra Hospital in Isfahan City, Iran from 2013 to 2015. In this study, 33 patients with CES (age range:29-77y) were studied. The mean (SD) duration of symptoms before surgery was 8.9(6.4) day. Twenty-eight patients were male and the most common involved segment was L4-L5 observed in 22 cases.
Although intervertebral disk herniation symptoms are more common in young and middle-aged groups due to occupational causes, because of the progression of the disease on one hand and tendency of older people to develop the disease on the other hand, 50% of patients were 50 years or older. According to the results of our study, all 33 patients had sensory and muscular weakness and 19 suffered from sphincter disorder. Although the effect of surgery and urgency was still doubtful, all 33 patients underwent the operation.
A 2-year follow up of the patients showed that muscle weakness improved in 78.8% of them, specifically 7.7% of the patients recovered in one day, 53.8% within one month, 15.4% within six months, and 23.1% within 24 months after the operation. Also, 94.7% of patients with urinary disorder and 100% of patients with fecal dysfunction recovered within 24 months, and the prognosis of the treated patients was satisfactory altogether. Recent guidelines for treating patients with low back pain and neurological symptoms suggest that suspicious cases of CES be referred to surgery immediately, but due to the high percentage of false positives in clinical examinations, definitive diagnosis of the disease should be made by MRI, because even other imaging techniques, such as CT cannot fully confirm the presence of CES [11].
When a patient has clinical features of CES, and MRI confirms it, the current consensus recommends removal of pressure with surgery [9]. According to the results of our study, duration of symptoms prior to surgery affects the improvement of muscle weakness, but has no effect on the improvement rate of the sphincter problem. Results of a review study support that only incomplete CES requires urgent surgery to prevent bladder function degradation.
Based on the current study, in patients with CES accompanied by urinary disorder, the clinical outcome is undesirable in any case and does not correlate with the time of surgery. Therefore, such patients can wait until the next morning to perform an elective surgery, rather than suffer from a potentially difficult operation during the midnight while the conditions are less desirable. According to two recently published articles in the UK, the outcome is independent of the time of surgery [12].
A widely researched review article suggests that interventions within less than 48 hours of symptoms onset will result in a better outcome than delayed interventions after this period of time. These data have been selectively reconsidered, and it has been stated that the outcome of both types of CES (incomplete or with urinary retention) would be better with interventions within a 24-hour period compared to those after this time.
In another analysis of selective retrospective collections, the authors found that out of 47 patients undergoing surgery during the 24 hours, 41(87%) recovered with regard to the bladder function, while out of 46 patients who had undergone surgery after 24 hours only 2(4.3%) subjects improved [13]. Another research, supported the view that early surgery is associated with better results in incomplete CES, but less certain outcomes were found about CES with urinary retention [14].
5. Conclusion
According to the results of this study, the operation of the lumbar spine surgery leads to improvement in CES, including sphincter disorders and muscle weakness. However, due to the limitations of our study, including a small sample size, further studies are recommended to reach stronger conclusions.
Ethical Considerations
Compliance with ethical guidelines
The informed consent was obtained from the patients.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
The authors declared no conflict of interest. Conception and design: Majid Rezvani; Data Collection: Ehsan Mohamadhoseini, Amin Rastgoo, Mohammad Kamangar, Mohammad-Amin Noorian; Drafting the article: Ehsan Mohamadhoseini, Majid Rezvani, Amin Rastgoo, Mohammad Kamangar; Critically revising the article: All authors; Reviewing submitted version of manuscript: All authors; Approving the final version of the manuscript: All authors.
References
- Lavy C, James A, Wilson-MacDonald J, Fairbank J. Cauda Equina Syndrome. Obstetric Anesthesia Digest. 2010; 30(1):16-7. [DOI:10.1097/01.aoa.0000366996.87147.18]
- Larner AJ. A dictionary of neurological signs. Berlin: Springer; 2010.
- Krämer J, Schleberger R, Hedtmann A. Intervertebral disk diseases: causes, diagnosis, treatment and prophylaxis. Stuttgart: Thieme; 1990.
- Gardner A, Gardner E, Morley T. Cauda Equina Syndrome: a review of the current clinical and medico-legal position. European Spine Journal. 2011; 20(5):690-7. [DOI:10.1007/s00586-010-1668-3] [PMID] [PMCID]
- Burke GL. Backache from occiput to coccyx. Chicago: MacDonald; 2014.
- Thiam AB, Thioub M, Agbo-Panzo MG, Sy CE, Faye M, Badiane SB. Intradural lumbar disc herniation: Report of two cases and review of the literature. Iranian Journal of Neurosurgery. 2017; 2(4):18-21. [DOI:10.29252/irjns.2.4.18]
- Walid MS, Ajjan M, Johnston KW, Robinson Jr JS. Cauda Equina Syndrome—think of cancer. The Permanente Journal. 2008; 12(2):48-51. [DOI:10.7812/TPP/07-054] [PMID] [PMCID]
- Eck JC. Cauda Equina Syndrome Causes [Internet]. 2017 [Updated 2017 November 21]. Available from: https://www.emedicinehealth.com/cauda_equina_syndrome/article_em.htm#what_is_cauda_equina_syndrome_definition)
- Radcliff KE, Kepler CK, Delasotta LA, Rihn JA, Harrop JS, Hilibrand AS, et al. Current management review of thoracolumbar cord syndromes. The Spine Journal. 2011; 11(9):884-92. [DOI:10.1016/j.spinee.2011.07.022] [PMID]
- Harrop JS, Hunt Jr GE, Vaccaro AR. Conus medullaris and Cauda Equina Syndrome as a result of traumatic injuries: management principles. Neurosurgical Focus. 2004; 16(6):1-23. [DOI:10.3171/foc.2004.16.6.4]
- Schoenfeld AJ, Bader JO. Cauda Equina Syndrome: an analysis of incidence rates and risk factors among a closed North American military population. Clinical neurology and neurosurgery. 2012; 114(7):947-50. [DOI:10.1016/j.clineuro.2012.02.012] [PMID]
- Eck JC. Cauda Equina Syndrome Prevention [Internet]. 2011 [Cited 2011 October 9]. Available from: http://www.orthoanswer.org/spine-neck/cauda-equina/prevention.html
- Ahn UM, Ahn NU, Buchowski JM, Garrett ES, Sieber AN, Kostuik JP. Cauda Equina Syndrome secondary to lumbar disc herniation: A meta-analysis of surgical outcomes. Spine. 2000; 25(12):1515-22. [DOI:10.1097/00007632-200006150-00010] [PMID]
- Shapiro S. Medical realities of Cauda Equina Syndrome secondary to lumbar disc herniation. Spine. 2000; 25(3):348-52. [DOI:10.1097/00007632-200002010-00015] [PMID]
Type of Study: Research |
Subject:
Basic Neurosurgery
References
1. Lavy C, James A, Wilson-MacDonald J, Fairbank J. Cauda Equina Syndrome. Obstetric Anesthesia Digest. 2010; 30(1):16-7. [DOI:10.1097/01.aoa.0000366996.87147.18] [DOI:10.1097/01.aoa.0000366996.87147.18]
2. Larner AJ. A dictionary of neurological signs. Berlin: Springer; 2010.
3. Krämer J, Schleberger R, Hedtmann A. Intervertebral disk diseases: causes, diagnosis, treatment and prophylaxis. Stuttgart: Thieme; 1990.
4. Gardner A, Gardner E, Morley T. Cauda Equina Syndrome: a review of the current clinical and medico-legal position. European Spine Journal. 2011; 20(5):690-7. [DOI:10.1007/s00586-010-1668-3] [PMID] [PMCID] [DOI:10.1007/s00586-010-1668-3]
5. Burke GL. Backache from occiput to coccyx. Chicago: MacDonald; 2014.
6. Thiam AB, Thioub M, Agbo-Panzo MG, Sy CE, Faye M, Badiane SB. Intradural lumbar disc herniation: Report of two cases and review of the literature. Iranian Journal of Neurosurgery. 2017; 2(4):18-21. [DOI:10.29252/irjns.2.4.18] [DOI:10.29252/irjns.2.4.18]
7. Walid MS, Ajjan M, Johnston KW, Robinson Jr JS. Cauda Equina Syndrome—think of cancer. The Permanente Journal. 2008; 12(2):48-51. [DOI:10.7812/TPP/07-054] [PMID] [PMCID] [DOI:10.7812/TPP/07-054]
8. Eck JC. Cauda Equina Syndrome Causes [Internet]. 2017 [Updated 2017 November 21]. Available from: https://www.emedicinehealth.com/cauda_equina_syndrome/article_em.htm#what_is_cauda_equina_syndrome_definition)
9. Radcliff KE, Kepler CK, Delasotta LA, Rihn JA, Harrop JS, Hilibrand AS, et al. Current management review of thoracolumbar cord syndromes. The Spine Journal. 2011; 11(9):884-92. [DOI:10.1016/j.spinee.2011.07.022] [PMID] [DOI:10.1016/j.spinee.2011.07.022]
10. Harrop JS, Hunt Jr GE, Vaccaro AR. Conus medullaris and Cauda Equina Syndrome as a result of traumatic injuries: management principles. Neurosurgical Focus. 2004; 16(6):1-23. [DOI:10.3171/foc.2004.16.6.4] [DOI:10.3171/foc.2004.16.6.4]
11. Schoenfeld AJ, Bader JO. Cauda Equina Syndrome: an analysis of incidence rates and risk factors among a closed North American military population. Clinical neurology and neurosurgery. 2012; 114(7):947-50. [DOI:10.1016/j.clineuro.2012.02.012] [PMID] [DOI:10.1016/j.clineuro.2012.02.012]
12. Eck JC. Cauda Equina Syndrome Prevention [Internet]. 2011 [Cited 2011 October 9]. Available from: http://www.orthoanswer.org/spine-neck/cauda-equina/prevention.html
13. Ahn UM, Ahn NU, Buchowski JM, Garrett ES, Sieber AN, Kostuik JP. Cauda Equina Syndrome secondary to lumbar disc herniation: A meta-analysis of surgical outcomes. Spine. 2000; 25(12):1515-22. [DOI:10.1097/00007632-200006150-00010] [PMID] [DOI:10.1097/00007632-200006150-00010]
14. Shapiro S. Medical realities of Cauda Equina Syndrome secondary to lumbar disc herniation. Spine. 2000; 25(3):348-52. [DOI:10.1097/00007632-200002010-00015] [PMID] [DOI:10.1097/00007632-200002010-00015]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |