Fri, Feb 6, 2026
Volume 4, Issue 2 (Spring 2018)
Iran J Neurosurg 2018, 4(2): 101-108 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rezaeian A. Buccal Fat Pad for Management of Cerebrospinal Fluid Leakage Using Endoscopy: A Randomized Clinical Trial. Iran J Neurosurg 2018; 4 (2) :101-108
URL: http://irjns.org/article-1-119-en.html
URL: http://irjns.org/article-1-119-en.html
Department of Ear, Nose & Throat, and Head & Neck surgery, School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran , dr.ahmadrezaeian@gmail.com
Full Text [PDF 846 kb]
(2079 Downloads)
| Abstract (HTML) (6925 Views)
2. Methods & Materials/Patients
Study patients
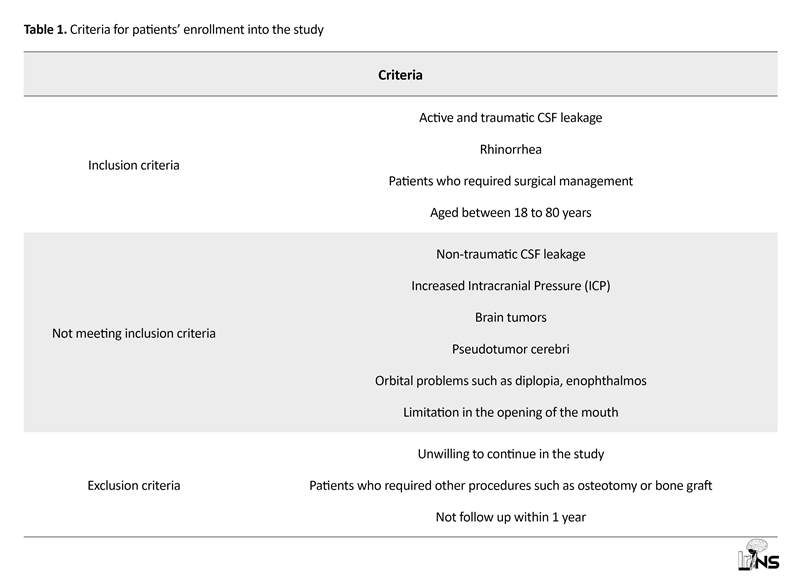
We conducted a research on 46 of 55 patients who had traumatic CSF leakage. The inclusion and exclusion criteria of the study were summarized in Table 1. The enrollment was done in Amin Hospital, Isfahan, Iran between 2013 and 2016. The patients were diagnosed according to clinical, preclinical (β2-transferrin test) and imaging (CT scan with contrast in axial and coronal views and Magnetic Resonance Imaging [MRI]) findings. Additionally, before treatments, endoscopic sinus (zero degree) was recommended for all patients in order to evaluate the extent of the defect. All information of the patients such as age, gender, trauma mechanism, underlying diseases, and localization were recorded in a checklist. Before the intervention, patients were divided into intervention and control groups. The randomization was done using Random Allocation Software that was a blinded method. The intervention group were treated with using buccal fat pad and the control group with using abdominal fat.
Surgical technique
All patients underwent general anesthesia with standard protocol and also25 mg of 10% fluorescein solution was injected intrathecally. The patients were in supine position with their head bend toward the surgeon and all operations were performed by a single ear, nose and throat surgeon. Nasal area was impregnated with adrenaline mesh. Adrenaline (1:100000) and lidocaine 1% were injected into the nasal cavity, also endoscopic performance was done with rigid 0° to 30° one in order to identify the defects. There are 3 approaches for extracting of the buccal fat pad.
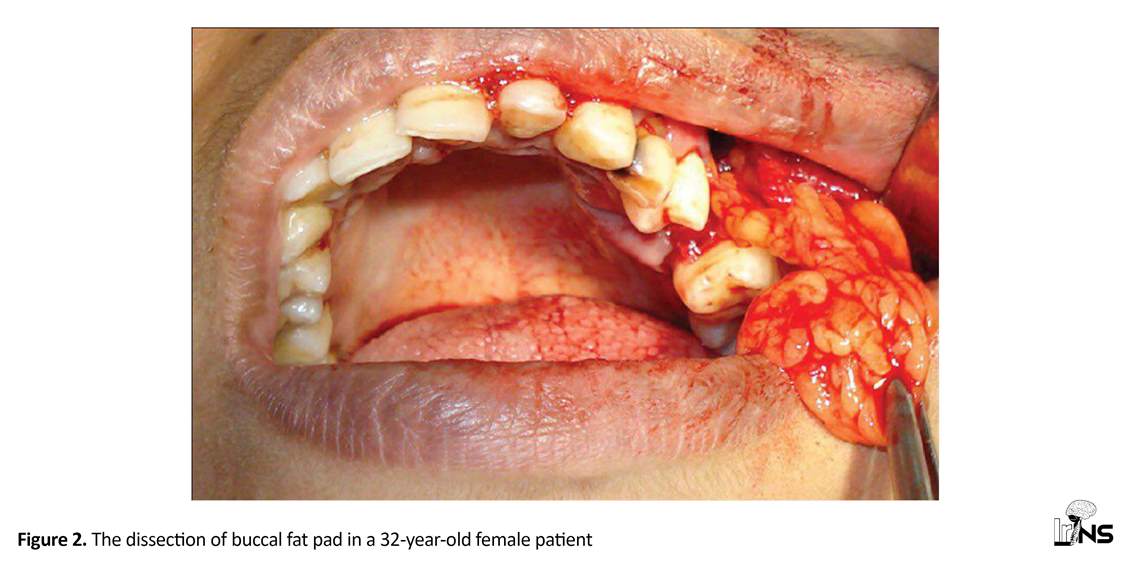
In this study, we used the most common approach for the intervention group, i.e. an incision wasmade on superior gingivobuccal sulcus in the superomedial wall of the buccal space [9]. Then, a 2-3 cm vestibular incision was done from the second molar to the first premolar and this incision was disseminated to the mucosa, buccinators muscle and periosteum up to the zygomatic bone. Next, the fascia of the buccal fat pad was dissected off with caution to avoid making injuries to nerves in the lateral wall of buccal space. Afterward, the buccal fat pad as a pedicle flap was freed [6] (Figure 2). If filling the defect needed more fat, buccal fat would extracted from the other side, too. It is worth mentioning that the incision place was sutured with 5.0 Vicryl. The extracted buccal fat pad was inserted into defect with the endoscopic method and afterward, a layer of hemostasis such as Gelfoam was placed between the fat flap and nasal pack.
In the control group, we used graft harvesting technique for using abdominal free fat. In this technique, the abdominal fat was prepared according to the standard method and a curvilinear incision was done on periumbilical area (4 to 8 cm) [11]. In our study, we prepared abdominal fat 30% to 40% more than the defect size. After removing the fat from the abdomen and suturing of the abdominal incision, we inserted fat with endoscope similar to the intervention group.
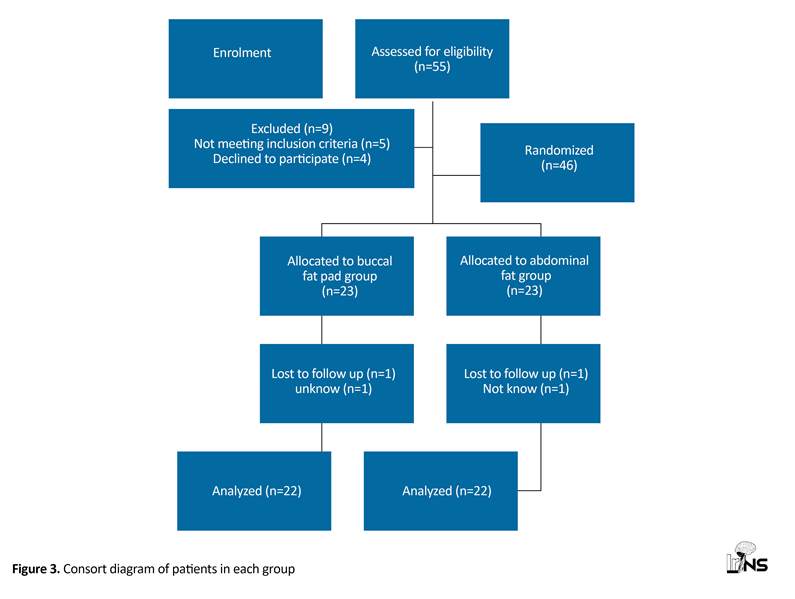
After operations, all patients received co-amoxiclav 150 mg/kg/d for 14 days and patients with meningitis were treated according to standard protocol. Additionally, patients remained in half-sitting and resting position for 1 week. Nasal packs were removed after 2 days and the patients were visited in the first and second weeks, first, second, and fourth months and one year after operation. In the follow-up, neurological exam, CT scan with contrast and MRI (for evaluation of defect), paraclinical exam (for meningitis) such as CRP, ESR, CBC were performed for all patients, including those who had symptoms such as rhinorrhea and were tested with β2-transferrin test and endoscopic evaluation. In addition, the complications of patients were recorded in each visit. One patient in intervention and one patient in control group did not continue their follow up for one year (Figure 3).
Statistical analysis
The sample size was calculated according to formula and a previous study. Assuming a power detection of 80%, and confidence level of 95%, the standard deviation of 1.32 and difference between means as 0.5, the sample size was obtained as 46 (23 for each group). The data were analyzed in SPSS 24 (Chicago, IL). In addition, the Independent t test and Chi-square test were used to compare results of the intervention and control groups. The quantitative data are presented as mean±SD and also qualitative data are presented as number or percentage. In addition, P<0.05 was considered as significane level.
3. Results
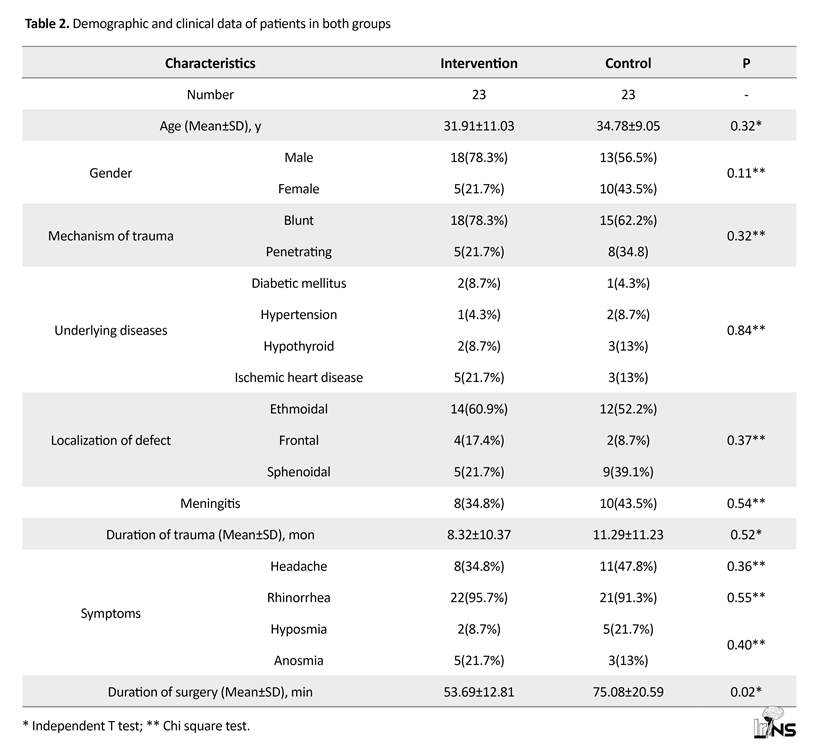
In this study, 46 patients (31 males and 15 females, mean±SD age: 33.34±10.08 y) with CSF leakage were participated. They were divided into two groups as intervention (18 males and 13 females, mean±SD age: 31.91±11.03 y) and control (13 males and 10 females, mean±SD age: 34.78±9.05 y). The mechanisms of trauma were blunt in 33 (71.7%) patients and penetrating in 13(28.3%). Three (6.5%) patients had diabetes, 3 (6.5%) hypertension, 5 (10.9%) hypothyroid and the 8(17.4%) ischemic heart disease; also 18(39.1%) patients had a history of meningitis during the time of trauma and the mean±SD duration of trauma was 9.08±10.79 months.
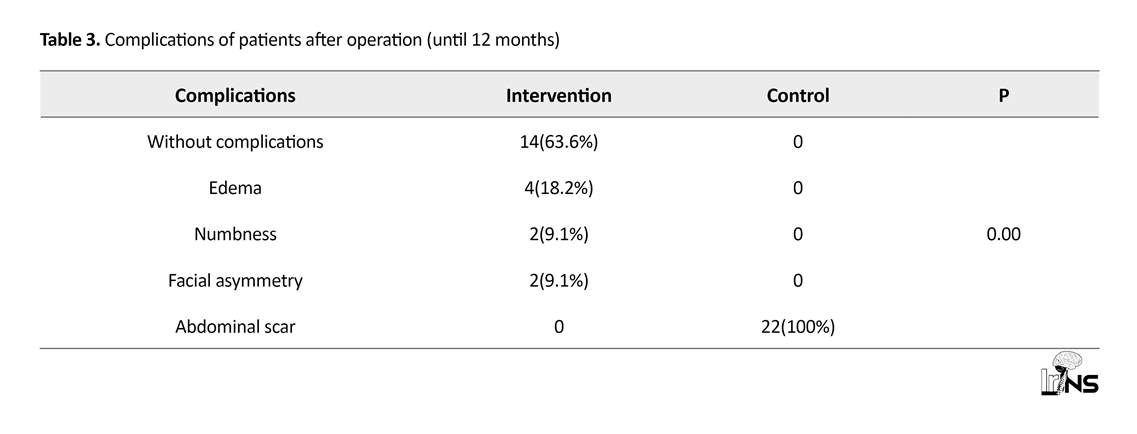
Before treatments, all patients had symptoms such as headache (41.3%), hyposmia (15.2%) or anosmia (17.4%) and rhinorrhea (93.5%). The most common symptom was rhinorrhea. Locations of defects were ethmoidal (56.5%), frontal (13%) and sphenoidal (30.4%) regions. In addition, there were no significant differences between intervention and control regarding age (P=0.32), gender (P=0.11), mechanism of trauma (P=0.32), underlining disease (P=0.84), localization of defect (P=0.37), meningitis (P=0.54), duration of trauma (P=0.52) and symptoms such as headache (P=0.36), rhinorrhea (P=0.55) and olfactory dysfunction (P=0.40) (demographic and clinical data of patients were presented in Table 2). The mean±SD duration of operation in the intervention and control groups were 53.69±12.81 and 75.08±20.59 minutes, respectively, so the duration of surgery in the intervention group was significantly shorter than the control (P=0.02). All patients were followed up for 1 year and CSF leakage was improved in all patients with no report of recurrence of symptoms. The complications of the intervention group were 18.2% edema, 9.1% numbness, and 9.1% facial asymmetry, these symptoms, however, temporary. In addition, all patients of the intervention group had an abdominal scar, therefore this difference was significant (P=0.00) (Table 3).
4. Discussion
The current study was the first report of buccal fat pad use for patients with CSF leakage. We demonstrated that all patients improved 100% with no recurrence of the problem. Moreover, there were temporary complications in the intervention group such as edema, numbness, and facial asymmetry in place of the buccal fat pad due to endoscopic procedures for management of CSF leakage. However, these complications were totally improved after 6 months. However, there was an abdominal scar in all patients of the control group. In addition, the duration of operation in the intervention group was shorter than that in the control group.
These autologous materials can be coated with a fibrin gel, Vaseline gas, surgical, and bone wax. Flaps of mucoperiosteal and middle concha have also been used. The size of the defect should be less than 15 mm in order to use the mucoperiosteal nail flap [14]. However, closure of the large defects with these flaps has also been done. The size of the flap should be a bit larger than the size of the defect, and if a combined flap is used, the size of the mucus must be larger than the interior cartilage [2]. Buccal fat pad is a graft with high blood supply which is used for filling of defects [6, 9].
It should be noted that to the best of our knowledge, there has been no studies about usage of buccal fat pad for filling of defect in CSF leakage and our study was first intervention about utilization of buccal fat pad in the management of traumatic CSF leakage. The volume of the buccal fat pad is approximately 10 mL [15]. Most studies have suggested that the usage of the buccal fat pad is effective and successful with low complication for the simple graft surgical procedure [16]. Likewise, in a review article reported by Kim [10], it is suggested that buccal fat pad is a reliable flap with simple surgical procedure and can be used in various clinical conditions.
5. Conclusion
In conclusion, our report along with other studies suggest that the use of the buccal fat pad for filling of the defect is a simple and reliable procedure with lower complications and shorter duration of surgery and use of abdominal fat is associated with an abdominal scar and long duration of surgery. Additionally, there have been no studies about using the buccal fat pad for filling the defects in CSF leakage, so our study was the first study in this category. According to our results, use of the buccal fat pad as a flap for management of CSF leakage was a highly effective and a very simple procedure with temporary complications and 100% improvement. In addition, using buccal fat pad has better cosmetic results with no or very little scar, so we suggest this surgical method for patients with CSF leakage. Finally, we recommend that more studies be conducted with larger sample size on using the buccal fat pad for management of CSF leakage.
Ethical Considerations
Compliance with ethical guidelines
This open, randomized trial was approved by Ethics Committee of Isfahan University of Medical Sciences and was registered in Iranian Registry of Clinical Trial (IRCT2017100312782N21). Also, all patients signed written informed consent for participating in the study.
Funding
This study was supported and funded by Isfahan University of Medical Sciences.
Authors contributions
All authors have read and approved the manuscript.
Conflicts of interest
The author declared no conflict of interest..
Acknowledgements
I appreciate all the people who helped us to preparing of this study.
References
Full Text: (2631 Views)
1. Introduction
Rhinorrhea or Cerebrospinal Fluid (CSF) leakage refers to leakage from the nose due to a defect between subarachnoid and upper respiratory spaces [1-3]. In order to prevent CSF leakage, surgeons use an autologous material such as fat, fascia, muscle graft, septal flap, or mucosal graft for reconstruction of the defective area. All these methods have beneficial effects on the management of CSF leakage [4, 5]. Using autologous fat grafts is a well-tolerable technique for filling of superficial intromission in traumatic and congenital defects and the subcutaneous fat such as abdominal fat is commonly used [6].
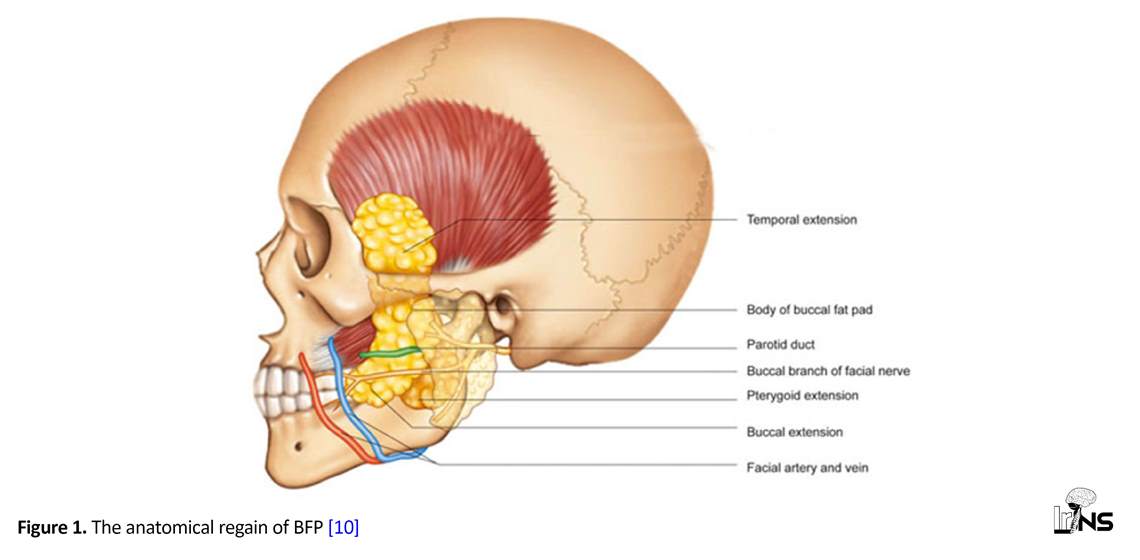
Buccal Fat Pad (BFP) use has been mentioned for the first time by Heister [7] in 1732. BFP is a biconvex, encapsulated, rounded, and adipose structure. The anatomy area of buccal fat is in masticatory space between masseter muscle (in lateral area) and the buccinator muscle (in medical area). Moreover, BFP includes 3 lobes: anterior, posterior, and intermediate [8]. The blood supply of BFP is driven by superficial temporal and facial arteries , which together, prevents necrosis of BPF (Figure 1) [9, 10]. Based on Khiabani et al. [6] report, the BFP flap is a small to medium flap for filling soft and bony defects, however, few studies exist about the use of BFP as the fat flap.
The use of other flap or graft such as abdominal fat creates some complications for management of CSF leakage, including but not limited to, the requirement of several surgeons in different fields for each stage of resection and insertion and of course cosmetic complications such as the surgical scar on donor’s body. It seems that use of a facial fat such as buccal fat is preferable in the management of CSF leakage because all procedures are at the same site and can be done with only one surgeon. Taken together, we hypothesized that using BFP flap could be an effective and beneficial technique in treating CSF leakage and to the best of our knowledge, this technique has been administered for the first time.
Rhinorrhea or Cerebrospinal Fluid (CSF) leakage refers to leakage from the nose due to a defect between subarachnoid and upper respiratory spaces [1-3]. In order to prevent CSF leakage, surgeons use an autologous material such as fat, fascia, muscle graft, septal flap, or mucosal graft for reconstruction of the defective area. All these methods have beneficial effects on the management of CSF leakage [4, 5]. Using autologous fat grafts is a well-tolerable technique for filling of superficial intromission in traumatic and congenital defects and the subcutaneous fat such as abdominal fat is commonly used [6].
Buccal Fat Pad (BFP) use has been mentioned for the first time by Heister [7] in 1732. BFP is a biconvex, encapsulated, rounded, and adipose structure. The anatomy area of buccal fat is in masticatory space between masseter muscle (in lateral area) and the buccinator muscle (in medical area). Moreover, BFP includes 3 lobes: anterior, posterior, and intermediate [8]. The blood supply of BFP is driven by superficial temporal and facial arteries , which together, prevents necrosis of BPF (Figure 1) [9, 10]. Based on Khiabani et al. [6] report, the BFP flap is a small to medium flap for filling soft and bony defects, however, few studies exist about the use of BFP as the fat flap.
The use of other flap or graft such as abdominal fat creates some complications for management of CSF leakage, including but not limited to, the requirement of several surgeons in different fields for each stage of resection and insertion and of course cosmetic complications such as the surgical scar on donor’s body. It seems that use of a facial fat such as buccal fat is preferable in the management of CSF leakage because all procedures are at the same site and can be done with only one surgeon. Taken together, we hypothesized that using BFP flap could be an effective and beneficial technique in treating CSF leakage and to the best of our knowledge, this technique has been administered for the first time.
2. Methods & Materials/Patients
Study patients
We conducted a research on 46 of 55 patients who had traumatic CSF leakage. The inclusion and exclusion criteria of the study were summarized in Table 1. The enrollment was done in Amin Hospital, Isfahan, Iran between 2013 and 2016. The patients were diagnosed according to clinical, preclinical (β2-transferrin test) and imaging (CT scan with contrast in axial and coronal views and Magnetic Resonance Imaging [MRI]) findings. Additionally, before treatments, endoscopic sinus (zero degree) was recommended for all patients in order to evaluate the extent of the defect. All information of the patients such as age, gender, trauma mechanism, underlying diseases, and localization were recorded in a checklist. Before the intervention, patients were divided into intervention and control groups. The randomization was done using Random Allocation Software that was a blinded method. The intervention group were treated with using buccal fat pad and the control group with using abdominal fat.
Surgical technique
All patients underwent general anesthesia with standard protocol and also25 mg of 10% fluorescein solution was injected intrathecally. The patients were in supine position with their head bend toward the surgeon and all operations were performed by a single ear, nose and throat surgeon. Nasal area was impregnated with adrenaline mesh. Adrenaline (1:100000) and lidocaine 1% were injected into the nasal cavity, also endoscopic performance was done with rigid 0° to 30° one in order to identify the defects. There are 3 approaches for extracting of the buccal fat pad.
In this study, we used the most common approach for the intervention group, i.e. an incision wasmade on superior gingivobuccal sulcus in the superomedial wall of the buccal space [9]. Then, a 2-3 cm vestibular incision was done from the second molar to the first premolar and this incision was disseminated to the mucosa, buccinators muscle and periosteum up to the zygomatic bone. Next, the fascia of the buccal fat pad was dissected off with caution to avoid making injuries to nerves in the lateral wall of buccal space. Afterward, the buccal fat pad as a pedicle flap was freed [6] (Figure 2). If filling the defect needed more fat, buccal fat would extracted from the other side, too. It is worth mentioning that the incision place was sutured with 5.0 Vicryl. The extracted buccal fat pad was inserted into defect with the endoscopic method and afterward, a layer of hemostasis such as Gelfoam was placed between the fat flap and nasal pack.
In the control group, we used graft harvesting technique for using abdominal free fat. In this technique, the abdominal fat was prepared according to the standard method and a curvilinear incision was done on periumbilical area (4 to 8 cm) [11]. In our study, we prepared abdominal fat 30% to 40% more than the defect size. After removing the fat from the abdomen and suturing of the abdominal incision, we inserted fat with endoscope similar to the intervention group.
After operations, all patients received co-amoxiclav 150 mg/kg/d for 14 days and patients with meningitis were treated according to standard protocol. Additionally, patients remained in half-sitting and resting position for 1 week. Nasal packs were removed after 2 days and the patients were visited in the first and second weeks, first, second, and fourth months and one year after operation. In the follow-up, neurological exam, CT scan with contrast and MRI (for evaluation of defect), paraclinical exam (for meningitis) such as CRP, ESR, CBC were performed for all patients, including those who had symptoms such as rhinorrhea and were tested with β2-transferrin test and endoscopic evaluation. In addition, the complications of patients were recorded in each visit. One patient in intervention and one patient in control group did not continue their follow up for one year (Figure 3).
Statistical analysis
The sample size was calculated according to formula and a previous study. Assuming a power detection of 80%, and confidence level of 95%, the standard deviation of 1.32 and difference between means as 0.5, the sample size was obtained as 46 (23 for each group). The data were analyzed in SPSS 24 (Chicago, IL). In addition, the Independent t test and Chi-square test were used to compare results of the intervention and control groups. The quantitative data are presented as mean±SD and also qualitative data are presented as number or percentage. In addition, P<0.05 was considered as significane level.
3. Results
In this study, 46 patients (31 males and 15 females, mean±SD age: 33.34±10.08 y) with CSF leakage were participated. They were divided into two groups as intervention (18 males and 13 females, mean±SD age: 31.91±11.03 y) and control (13 males and 10 females, mean±SD age: 34.78±9.05 y). The mechanisms of trauma were blunt in 33 (71.7%) patients and penetrating in 13(28.3%). Three (6.5%) patients had diabetes, 3 (6.5%) hypertension, 5 (10.9%) hypothyroid and the 8(17.4%) ischemic heart disease; also 18(39.1%) patients had a history of meningitis during the time of trauma and the mean±SD duration of trauma was 9.08±10.79 months.
Before treatments, all patients had symptoms such as headache (41.3%), hyposmia (15.2%) or anosmia (17.4%) and rhinorrhea (93.5%). The most common symptom was rhinorrhea. Locations of defects were ethmoidal (56.5%), frontal (13%) and sphenoidal (30.4%) regions. In addition, there were no significant differences between intervention and control regarding age (P=0.32), gender (P=0.11), mechanism of trauma (P=0.32), underlining disease (P=0.84), localization of defect (P=0.37), meningitis (P=0.54), duration of trauma (P=0.52) and symptoms such as headache (P=0.36), rhinorrhea (P=0.55) and olfactory dysfunction (P=0.40) (demographic and clinical data of patients were presented in Table 2). The mean±SD duration of operation in the intervention and control groups were 53.69±12.81 and 75.08±20.59 minutes, respectively, so the duration of surgery in the intervention group was significantly shorter than the control (P=0.02). All patients were followed up for 1 year and CSF leakage was improved in all patients with no report of recurrence of symptoms. The complications of the intervention group were 18.2% edema, 9.1% numbness, and 9.1% facial asymmetry, these symptoms, however, temporary. In addition, all patients of the intervention group had an abdominal scar, therefore this difference was significant (P=0.00) (Table 3).
4. Discussion
The current study was the first report of buccal fat pad use for patients with CSF leakage. We demonstrated that all patients improved 100% with no recurrence of the problem. Moreover, there were temporary complications in the intervention group such as edema, numbness, and facial asymmetry in place of the buccal fat pad due to endoscopic procedures for management of CSF leakage. However, these complications were totally improved after 6 months. However, there was an abdominal scar in all patients of the control group. In addition, the duration of operation in the intervention group was shorter than that in the control group.
The anterior cranial cavity is highly susceptible to trauma and iatrogenic injuries. The diagnosis of CSF leakage is usually simple. A nasal discharge following a head injury or intranasal surgery is suggestive of cerebrospinal fluid rhinorrhea. Furthermore, the patient might have recurrent meningitis after a traumatic event [12]. The initial treatment of traumatic cerebrospinal fluid leakage is conservative. One important factor is restriction of the activities that increase intracranial pressure (avoiding trendelenburg position). The use of prophylactic antibiotics is still under debate. If CSF leakage was not treated with conservative therapy within 6 weeks, surgical management would be required. Additional indications for a surgical approach is relapsing, intermittent, and spontaneous CSF leakage, as well as diagnosis of leakage within an operation, pneumocephalus, and repeated meningitis [13]. A great deal of material and a number of techniques have been used to close the CSF leakage, including using autologous materials such as abdominal fat, nasal septum, bone, fascia lata, and muscle grafts.
These autologous materials can be coated with a fibrin gel, Vaseline gas, surgical, and bone wax. Flaps of mucoperiosteal and middle concha have also been used. The size of the defect should be less than 15 mm in order to use the mucoperiosteal nail flap [14]. However, closure of the large defects with these flaps has also been done. The size of the flap should be a bit larger than the size of the defect, and if a combined flap is used, the size of the mucus must be larger than the interior cartilage [2]. Buccal fat pad is a graft with high blood supply which is used for filling of defects [6, 9].
It should be noted that to the best of our knowledge, there has been no studies about usage of buccal fat pad for filling of defect in CSF leakage and our study was first intervention about utilization of buccal fat pad in the management of traumatic CSF leakage. The volume of the buccal fat pad is approximately 10 mL [15]. Most studies have suggested that the usage of the buccal fat pad is effective and successful with low complication for the simple graft surgical procedure [16]. Likewise, in a review article reported by Kim [10], it is suggested that buccal fat pad is a reliable flap with simple surgical procedure and can be used in various clinical conditions.
5. Conclusion
In conclusion, our report along with other studies suggest that the use of the buccal fat pad for filling of the defect is a simple and reliable procedure with lower complications and shorter duration of surgery and use of abdominal fat is associated with an abdominal scar and long duration of surgery. Additionally, there have been no studies about using the buccal fat pad for filling the defects in CSF leakage, so our study was the first study in this category. According to our results, use of the buccal fat pad as a flap for management of CSF leakage was a highly effective and a very simple procedure with temporary complications and 100% improvement. In addition, using buccal fat pad has better cosmetic results with no or very little scar, so we suggest this surgical method for patients with CSF leakage. Finally, we recommend that more studies be conducted with larger sample size on using the buccal fat pad for management of CSF leakage.
Ethical Considerations
Compliance with ethical guidelines
This open, randomized trial was approved by Ethics Committee of Isfahan University of Medical Sciences and was registered in Iranian Registry of Clinical Trial (IRCT2017100312782N21). Also, all patients signed written informed consent for participating in the study.
Funding
This study was supported and funded by Isfahan University of Medical Sciences.
Authors contributions
All authors have read and approved the manuscript.
Conflicts of interest
The author declared no conflict of interest..
Acknowledgements
I appreciate all the people who helped us to preparing of this study.
References
- Kerr JT, Chu FW, Bayles SW. Cerebrospinal fluid rhinorrhea: Diagnosis and management. Otolaryngologic Clinics of North America. 2005; 38(4):597-611. [DOI:10.1016/j.otc.2005.03.011] [PMID]
- Schmerber S, Righini C, Lavieille JP, Passagia JG, Reyt E. Endonasal endoscopic closure of cerebrospinal fluid rhinorrhea. Journal of Neurological Surgery Part B: Skull Base. 2001; 11(1):47-58. [DOI:10.1055/s-2001-12787]
- Ozturk K, Karabagli H, Bulut S, Egilmez M, Duran M. Is the use of topical fluorescein helpful for management of CSF leakage? The Laryngoscope. 2012; 122(6):1215-8. [DOI:10.1002/lary.23277] [PMID]
- El-Banhawy OA, Halaka AN, Altuwaijri MA, Ayad H, El-Sharnoby MM. Long-term outcome of endonasal endoscopic skull base reconstruction with nasal turbinate graft. Journal of Neurological Surgery Part B: Skull Base. 2008; 18(5):297-308. [DOI:10.1055/s-0028-1086055] [PMID] [PMCID]
- Amano K, Hori T, Kawamata T, Okada Y. Repair and prevention of cerebrospinal fluid leakage in transsphenoidal surgery: A sphenoid sinus mucosa technique. Neurosurgical Review. 2016; 39(1):123-31. [DOI:10.1007/s10143-015-0667-6] [PMID]
- Khiabani K, Keyhan SO, Varedi P, Hemmat S, Razmdideh R, Hoseini E. Buccal fat pad lifting: An alternative open technique for malar augmentation. Journal of Oral and Maxillofacial Surgery. 2014; 72(2):403.e1-15. [DOI:10.1016/j.joms.2013.10.002] [PMID]
- Baumann A, Ewers R. Application of the buccal fat pad in oral reconstruction. Journal of Oral and Maxillofacial Surgery. 2000; 58(4):389-92. [DOI:10.1016/S0278-2391(00)90919-4]
- Zhang HM, Yan YP, Qi KM, Wang JQ, Liu ZF. Anatomical structure of the buccal fat pad and its clinical adaptations. Plastic and Reconstructive Surgery. 2002; 109(7):2509-18. [DOI:10.1097/00006534-200206000-00052] [PMID]
- Dubin B, Jackson IT, Halim A, Triplett W, Ferreira M. Anatomy of the buccal fat pad and its clinical significance. Plastic and Reconstructive Surgery. 1989; 83(2):257-62. [DOI:10.1097/00006534-198902000-00009] [PMID]
- Kim MK, Han W, Kim SG. The use of the buccal fat pad flap for oral reconstruction. Maxillofacial Plastic and Reconstructive Surgery. 2017; 39(1):5. [DOI:10.1186/s40902-017-0105-5] [PMID] [PMCID]
- Ackerman PD, Hammers R, Ibrahim T, Origitano T. The use of abdominal free fat for volumetric augmentation and primary dural closure in supratentorial skull base surgery: Managing the stigma of a temporal defect. Journal of Neurological Surgery Part B: Skull Base. 2012; 73(2):139-44. [DOI:10.1055/s-0032-1301399] [PMID] [PMCID]
- McMains KC, Gross CW, Kountakis SE. Endoscopic management of cerebrospinal fluid rhinorrhea. The Laryngoscope. 2004; 114(10):1833-7. [DOI:10.1097/00005537-200410000-00029] [PMID]
- Oberascher G. A modern concept of cerebrospinal fluid diagnosis in oto-and rhinorrhea. Rhinology International Journal. 1988; 26(2):89-103. [PMID]
- Le C, Strong EB, Luu Q. Management of anterior skull base cerebrospinal fluid leaks. Journal of Neurological Surgery Part B: Skull Base. 2016; 77(5):404-11. [DOI:10.1055/s-0036-1584229] [PMID] [PMCID]
- Arce K. Buccal fat pad in maxillary reconstruction. Atlas of the Oral and Maxillofacial Surgery Clinics of North America. 2007; 15(1):23-32. [DOI:10.1016/j.cxom.2006.11.003] [PMID]
- Singh J, Prasad K, Lalitha R, Ranganath K. Buccal pad of fat and its applications in oral and maxillofacial surgery: A review of published literature (February) 2004 to (July) 2009. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2010; 110(6):698-705. [DOI:10.1016/j.tripleo.2010.03.017] [PMID]
Type of Study: Clinical Trial |
Subject:
Skull Base
References
1. Kerr JT, Chu FW, Bayles SW. Cerebrospinal fluid rhinorrhea: Diagnosis and management. Otolaryngologic Clinics of North America. 2005; 38(4):597-611. [DOI:10.1016/j.otc.2005.03.011] [PMID] [DOI:10.1016/j.otc.2005.03.011]
2. Schmerber S, Righini C, Lavieille JP, Passagia JG, Reyt E. Endonasal endoscopic closure of cerebrospinal fluid rhinorrhea. Journal of Neurological Surgery Part B: Skull Base. 2001; 11(1):47-58. [DOI:10.1055/s-2001-12787] [DOI:10.1055/s-2001-12787]
3. Ozturk K, Karabagli H, Bulut S, Egilmez M, Duran M. Is the use of topical fluorescein helpful for management of CSF leakage? The Laryngoscope. 2012; 122(6):1215-8. [DOI:10.1002/lary.23277] [PMID] [DOI:10.1002/lary.23277]
4. El-Banhawy OA, Halaka AN, Altuwaijri MA, Ayad H, El-Sharnoby MM. Long-term outcome of endonasal endoscopic skull base reconstruction with nasal turbinate graft. Journal of Neurological Surgery Part B: Skull Base. 2008; 18(5):297-308. [DOI:10.1055/s-0028-1086055] [PMID] [PMCID] [DOI:10.1055/s-0028-1086055]
5. Amano K, Hori T, Kawamata T, Okada Y. Repair and prevention of cerebrospinal fluid leakage in transsphenoidal surgery: A sphenoid sinus mucosa technique. Neurosurgical Review. 2016; 39(1):123-31. [DOI:10.1007/s10143-015-0667-6] [PMID] [DOI:10.1007/s10143-015-0667-6]
6. Khiabani K, Keyhan SO, Varedi P, Hemmat S, Razmdideh R, Hoseini E. Buccal fat pad lifting: An alternative open technique for malar augmentation. Journal of Oral and Maxillofacial Surgery. 2014; 72(2):403.e1-15. [DOI:10.1016/j.joms.2013.10.002] [PMID] [DOI:10.1016/j.joms.2013.10.002]
7. Baumann A, Ewers R. Application of the buccal fat pad in oral reconstruction. Journal of Oral and Maxillofacial Surgery. 2000; 58(4):389-92. [DOI:10.1016/S0278-2391(00)90919-4] [DOI:10.1016/S0278-2391(00)90919-4]
8. Zhang HM, Yan YP, Qi KM, Wang JQ, Liu ZF. Anatomical structure of the buccal fat pad and its clinical adaptations. Plastic and Reconstructive Surgery. 2002; 109(7):2509-18. [DOI:10.1097/00006534-200206000-00052] [PMID] [DOI:10.1097/00006534-200206000-00052]
9. Dubin B, Jackson IT, Halim A, Triplett W, Ferreira M. Anatomy of the buccal fat pad and its clinical significance. Plastic and Reconstructive Surgery. 1989; 83(2):257-62. [DOI:10.1097/00006534-198902000-00009] [PMID] [DOI:10.1097/00006534-198902000-00009]
10. Kim MK, Han W, Kim SG. The use of the buccal fat pad flap for oral reconstruction. Maxillofacial Plastic and Reconstructive Surgery. 2017; 39(1):5. [DOI:10.1186/s40902-017-0105-5] [PMID] [PMCID] [DOI:10.1186/s40902-017-0105-5]
11. Ackerman PD, Hammers R, Ibrahim T, Origitano T. The use of abdominal free fat for volumetric augmentation and primary dural closure in supratentorial skull base surgery: Managing the stigma of a temporal defect. Journal of Neurological Surgery Part B: Skull Base. 2012; 73(2):139-44. [DOI:10.1055/s-0032-1301399] [PMID] [PMCID] [DOI:10.1055/s-0032-1301399]
12. McMains KC, Gross CW, Kountakis SE. Endoscopic management of cerebrospinal fluid rhinorrhea. The Laryngoscope. 2004; 114(10):1833-7. [DOI:10.1097/00005537-200410000-00029] [PMID] [DOI:10.1097/00005537-200410000-00029]
13. Oberascher G. A modern concept of cerebrospinal fluid diagnosis in oto-and rhinorrhea. Rhinology International Journal. 1988; 26(2):89-103. [PMID]
14. Le C, Strong EB, Luu Q. Management of anterior skull base cerebrospinal fluid leaks. Journal of Neurological Surgery Part B: Skull Base. 2016; 77(5):404-11. [DOI:10.1055/s-0036-1584229] [PMID] [PMCID] [DOI:10.1055/s-0036-1584229]
15. Arce K. Buccal fat pad in maxillary reconstruction. Atlas of the Oral and Maxillofacial Surgery Clinics of North America. 2007; 15(1):23-32. [DOI:10.1016/j.cxom.2006.11.003] [PMID] [DOI:10.1016/j.cxom.2006.11.003]
16. Singh J, Prasad K, Lalitha R, Ranganath K. Buccal pad of fat and its applications in oral and maxillofacial surgery: A review of published literature (February) 2004 to (July) 2009. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2010; 110(6):698-705. [DOI:10.1016/j.tripleo.2010.03.017] [PMID] [DOI:10.1016/j.tripleo.2010.03.017]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |