Tue, Jul 8, 2025
Volume 5, Issue 3 And 4 (Summer & Autumn 2019)
Iran J Neurosurg 2019, 5(3 And 4): 155-160 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Aghapoor M, Alijani B A, Pakseresht-Mogharab * M. Aspergillus Spondylodiscitis After Spinal Stenosis Surgery: A Case ReportA Case Report. Iran J Neurosurg 2019; 5 (3 and 4) :155-160
URL: http://irjns.org/article-1-184-en.html
URL: http://irjns.org/article-1-184-en.html
1- Department of Neurosurgery, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran , maghapoor86@gmail.com
2- Guilan Road Trauma Research Center, Guilan University of Medical Sciences, Rasht, Iran
3- Department of Neurosurgery, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran
2- Guilan Road Trauma Research Center, Guilan University of Medical Sciences, Rasht, Iran
3- Department of Neurosurgery, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran
Full Text [PDF 661 kb]
(1652 Downloads)
| Abstract (HTML) (3648 Views)
Full Text: (1174 Views)
1. Background and Importance
Spondylodiscitis is a rare disease, and is responsible for 2-7% of pyogenic osteomyelitis cases. The incidence ranges from 1/10000 per year to 1/250000 per year, and it occurs three times higher in males [1, 2]. The incidence of invasive fungal infection has been increasing since 1980, and it believed that it is due to an increase in the population of patients with immune system dysfunction [3]. Therefore, the prevalence of Aspergillus – associated vertebral osteomyelitis is increasing in the population of patients with immune system disorders. However, due to nonspecific symptoms, there are still many challenges in diagnosis and its treatment [4].
Aggressive aspergillus rarely infects bony structures, but when occurs, the spine is the most common site of involvement [5]. Spinal fungal infections are relatively uncommon, and it has a prevalence of 0.05%-1.6% [1]. Until 2009, fewer than 50 cases of Aspergillus osteomyelitis have been reported in the literature, in which the majority of patients suffered from immune dysfunction, and only in 10 of them, patients had this type of fungal infection without immune dysfunction [6]. It has been reported that 34% of patients with Aspergillus osteomyelits were without any predisposing or immunosuppressive factors [7].
Causes of vertebral Aspergillus can be classified into three major categories; trauma-induced infection, spinal surgery or epidural injection, and spread of pleural effusion that affects the thoracic spine. A quarter of Aspergillus osteomyelits occurs due to spinal procedures [7].
Back pain is the most common symptom and most patients have disc inflammation and osteomyelitis at one or more vertebral levels. According to imaging results, it is difficult to diagnose Aspergillus and bacterial infection [4]. Aspergillus spondylodiscitis may be mistaken for tuberculosis spondylitis [1]. Most physicians recommend surgical treatment if there is progression of symptoms or neurological deficits [1, 8]. Patients who received both surgical and medical treatment showed more acceptable results [1]. The duration of antifungal therapy has not been established. Infectious Diseases Society of America (IDSA) guide line recommends at least 6-8 week antifungal therapy with amphotericin B or voriconazole in immunocompromised patients with Aspergillus spondylodiscitis [1].
2. Case presentation
A 63-year-old female patient referred to Medical Center of Poursina because of severe low back pain and radiculopathy. She had diabetes for 8 years and was treated with metformin 500 mg twice a day. She had not taken Immunosuppressive drugs and corticosteroids. She had surgery of lumbar canal stenosis in 2017 and 2018. Between the surgeries, she had radicular low back pain. Three months after the second surgery, the patient was admitted again because of severe low back pain and a probable diagnosis of spondylodiscitis.
Physical examination
In the initial study, the patient reported a low back pain score of 7 out of 10 on the VAS score. Vital signs were stable and without any fever. Clinical examination showed that the left lower extremity muscles force in distal and proximal was 3/5, and in other limbs in distal and proximal 5/5. She had radicular pain and paresthesia in the S1 nerve root pathway. There was no cervical pain and no sphincter dysfunction. Deep tendon reflexes were normal. Huffman, Clonus, and Babinski nerve tests were normal both in right and left sides. The patient had no spasticity and rigidity.
Paraclinical examination
MRI revealed spondylodiscitis at L4 vertebra (Figure 1). The initial CRP and ESR tests were 37 mg/L and 114 mm/h, respectively. Anti-Brucella IgG, Anti-Brucella IgM, Anti-HIV, Anti-HCV and Blood Culture tests were negative.
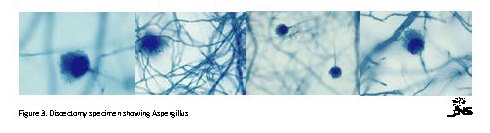
The patient underwent partial L2 and complete L3 and L4 corpectomy and L2 / L3, L3 / L4 discectomy with anterior retroperitoneal approach and fusion (Figure 2). Sampling from disc and vertebral body was performed for pathology and PCR for detection of fungi and tuberculosis. The debridement and irrigation of vertebrae were performed. On the fourth day after surgery, she was transferred to a cardiac center due to chest pain and ECG changes according to the advice of a cardiologist. Pathologic studies revealed Aspergillus fungi in the specimen (Figure 3), the patient was treated with Itraconazole antifungal drug 100 mg twice a day for two months.
Outcome and Follow-up
In the postoperative follow-up, the patient’s pain was reduced from a score of 7 to 2, and the latest test showed that CRP was decreased to 12 mg/l and ESR was also 120 mm/h. Parenthesis and lower extremity forces were also improved.
3. Discussion
The term spondylodiscitis means initial infection of intervertebral disc with a pathogen and secondary infection of vertebral body. The disease is very rare [1, 9]. Studies showed that any age group may be affected, but it is more frequent in the fifth to seventh decades of life [1, 10].
Today, there is an increasing prevalence of spondylodiscitis due to increased life expectancy associated with chronic debilitating diseases, immunosuppressive therapies, increased use of body implants, and a variety of spinal surgery [2, 4].
Spondylodiscitis is a rare disease, and is responsible for 2-7% of pyogenic osteomyelitis cases. The incidence ranges from 1/10000 per year to 1/250000 per year, and it occurs three times higher in males [1, 2]. The incidence of invasive fungal infection has been increasing since 1980, and it believed that it is due to an increase in the population of patients with immune system dysfunction [3]. Therefore, the prevalence of Aspergillus – associated vertebral osteomyelitis is increasing in the population of patients with immune system disorders. However, due to nonspecific symptoms, there are still many challenges in diagnosis and its treatment [4].
Aggressive aspergillus rarely infects bony structures, but when occurs, the spine is the most common site of involvement [5]. Spinal fungal infections are relatively uncommon, and it has a prevalence of 0.05%-1.6% [1]. Until 2009, fewer than 50 cases of Aspergillus osteomyelitis have been reported in the literature, in which the majority of patients suffered from immune dysfunction, and only in 10 of them, patients had this type of fungal infection without immune dysfunction [6]. It has been reported that 34% of patients with Aspergillus osteomyelits were without any predisposing or immunosuppressive factors [7].
Causes of vertebral Aspergillus can be classified into three major categories; trauma-induced infection, spinal surgery or epidural injection, and spread of pleural effusion that affects the thoracic spine. A quarter of Aspergillus osteomyelits occurs due to spinal procedures [7].
Back pain is the most common symptom and most patients have disc inflammation and osteomyelitis at one or more vertebral levels. According to imaging results, it is difficult to diagnose Aspergillus and bacterial infection [4]. Aspergillus spondylodiscitis may be mistaken for tuberculosis spondylitis [1]. Most physicians recommend surgical treatment if there is progression of symptoms or neurological deficits [1, 8]. Patients who received both surgical and medical treatment showed more acceptable results [1]. The duration of antifungal therapy has not been established. Infectious Diseases Society of America (IDSA) guide line recommends at least 6-8 week antifungal therapy with amphotericin B or voriconazole in immunocompromised patients with Aspergillus spondylodiscitis [1].
2. Case presentation
A 63-year-old female patient referred to Medical Center of Poursina because of severe low back pain and radiculopathy. She had diabetes for 8 years and was treated with metformin 500 mg twice a day. She had not taken Immunosuppressive drugs and corticosteroids. She had surgery of lumbar canal stenosis in 2017 and 2018. Between the surgeries, she had radicular low back pain. Three months after the second surgery, the patient was admitted again because of severe low back pain and a probable diagnosis of spondylodiscitis.
Physical examination
In the initial study, the patient reported a low back pain score of 7 out of 10 on the VAS score. Vital signs were stable and without any fever. Clinical examination showed that the left lower extremity muscles force in distal and proximal was 3/5, and in other limbs in distal and proximal 5/5. She had radicular pain and paresthesia in the S1 nerve root pathway. There was no cervical pain and no sphincter dysfunction. Deep tendon reflexes were normal. Huffman, Clonus, and Babinski nerve tests were normal both in right and left sides. The patient had no spasticity and rigidity.
Paraclinical examination
MRI revealed spondylodiscitis at L4 vertebra (Figure 1). The initial CRP and ESR tests were 37 mg/L and 114 mm/h, respectively. Anti-Brucella IgG, Anti-Brucella IgM, Anti-HIV, Anti-HCV and Blood Culture tests were negative.
The patient underwent partial L2 and complete L3 and L4 corpectomy and L2 / L3, L3 / L4 discectomy with anterior retroperitoneal approach and fusion (Figure 2). Sampling from disc and vertebral body was performed for pathology and PCR for detection of fungi and tuberculosis. The debridement and irrigation of vertebrae were performed. On the fourth day after surgery, she was transferred to a cardiac center due to chest pain and ECG changes according to the advice of a cardiologist. Pathologic studies revealed Aspergillus fungi in the specimen (Figure 3), the patient was treated with Itraconazole antifungal drug 100 mg twice a day for two months.
Outcome and Follow-up
In the postoperative follow-up, the patient’s pain was reduced from a score of 7 to 2, and the latest test showed that CRP was decreased to 12 mg/l and ESR was also 120 mm/h. Parenthesis and lower extremity forces were also improved.
3. Discussion
The term spondylodiscitis means initial infection of intervertebral disc with a pathogen and secondary infection of vertebral body. The disease is very rare [1, 9]. Studies showed that any age group may be affected, but it is more frequent in the fifth to seventh decades of life [1, 10].
Today, there is an increasing prevalence of spondylodiscitis due to increased life expectancy associated with chronic debilitating diseases, immunosuppressive therapies, increased use of body implants, and a variety of spinal surgery [2, 4].
Aspergillus exists as a safe microorganism in the upper respiratory tract and is rarely invasive. It is common in people with immunodeficiency disorder. Bone fungal infection can be due to (iatrogenic) treatment or direct trauma infection [6]. Contamination during surgery and other procedures in immunocompromised patients is usually caused by air pollution [5].
The Aspergillus infection of the vertebral body and intervertebral disc is one of the rare causes of spinal osteomyelitis. These types of infections are mostly limited to patients with predisposing factors such as leukocyte dysfunction, neutropenia-related malignancy, antibiotic and steroid therapy, respiratory Aspergillus, and surgical manipulation. Diabetes is known to be a detrimental factor in phagocytic function. Therefore, it may be effective in causing infection and growth of microorganisms [6].
Sethi et al. (2012) reported the largest number of patients without immunodeficiency with Aspergillus spodomyelitis [11]. D’Agostin et al. reported, in their 7-year prospective study of 81 patients with spondylodiscitis, only 6 of them had fungal infections [2]. In a study by Gabrielli, 310 cases of Aspergillus osteomyelitis from 1939-2013 were studied. The results of this study showed that 49% of people had Aspergillus osteomyelitis in the spine area. Also, 13% of people in this study had no risk factors for Aspergillus osteomyelitis [12].
The Aspergillus infection of the vertebral body and intervertebral disc is one of the rare causes of spinal osteomyelitis. These types of infections are mostly limited to patients with predisposing factors such as leukocyte dysfunction, neutropenia-related malignancy, antibiotic and steroid therapy, respiratory Aspergillus, and surgical manipulation. Diabetes is known to be a detrimental factor in phagocytic function. Therefore, it may be effective in causing infection and growth of microorganisms [6].
Sethi et al. (2012) reported the largest number of patients without immunodeficiency with Aspergillus spodomyelitis [11]. D’Agostin et al. reported, in their 7-year prospective study of 81 patients with spondylodiscitis, only 6 of them had fungal infections [2]. In a study by Gabrielli, 310 cases of Aspergillus osteomyelitis from 1939-2013 were studied. The results of this study showed that 49% of people had Aspergillus osteomyelitis in the spine area. Also, 13% of people in this study had no risk factors for Aspergillus osteomyelitis [12].
Early detection of Aspergillus spondylodiscitis remains a challenge and needs high suspicion [1]. Definitive diagnosis of Aspergillus spondylodiscitis is performed by biopsy. However, biomarkers such as galactomanan and serum beta D-glucan have recently been used to confirm the diagnosis [1]. Nandeesh et al., conducted early detection of Aspergillus osteomyelitis by Fine-needle Aspiration (FNA) Cytology. This procedure led to early detection and timely treatment without any life-threatening complication [6].
When fungal contamination occurs in the body, polymorphonuclear leukocytes play the most important role in removing hyphae [13]. The oxidative process done by phagocytes is required for the release of invading Aspergillus [13, 14]. Diabetes is known to be a detrimental factor in phagocytic function. Therefore, it may play a pivotal role in causing infection and making a suitable environment for the growth of microorganisms [6]. The prevalence of neutrophil oxidative dysfunction and phagocyte function in diabetic patients can make them more susceptible to Aspergillosis [13]. In Gabrielli’s study on 310 cases of Aspergillus osteomyelitis, 6% were diabetic [12].
When fungal contamination occurs in the body, polymorphonuclear leukocytes play the most important role in removing hyphae [13]. The oxidative process done by phagocytes is required for the release of invading Aspergillus [13, 14]. Diabetes is known to be a detrimental factor in phagocytic function. Therefore, it may play a pivotal role in causing infection and making a suitable environment for the growth of microorganisms [6]. The prevalence of neutrophil oxidative dysfunction and phagocyte function in diabetic patients can make them more susceptible to Aspergillosis [13]. In Gabrielli’s study on 310 cases of Aspergillus osteomyelitis, 6% were diabetic [12].
In this patient, the only significant predisposing factor is a history of diabetes as well as spinal surgery. Previous reports have indicated that the duration of symptoms until a definitive diagnosis ranged 5-7 months. In this patient, there were nonspecific signs and symptoms such as radicular low back pain and parenthesis. Due to the heart problems that occur in this time, it took 9 months before a definitive diagnosis. Laboratory tests are often less helpful in the diagnosis of Aspergillosis infection, and the final diagnosis is confirmed by microscopic examination of the fresh tissue specimens and culture in Sabouraud agar medium in which fungi are observed in 74% of the cases [13]. In this patient, a definitive diagnosis was made by observing the fungi in an intraoperative biopsy specimen.
Aspergillosis is highly fatal in patients with immune system dysfunction and amphotericin B should be prescribed intravenously at the maximum tolerable dose [13]. Treatment of Aspergillus osteomyelitis is multimodal, which includes improvement of chronic hyperglycemia, surgical intervention, and rapid starting of antifungal medication [14]. Whereas the British Infectious Disease Society recommends the use of amphotericin in combination with Flucytosine in severe cases of Aspergillus osteomyelitis, in stable patients Itraconazole has been recommended [7]. The patient was treated with Itraconazole 100 mg twice daily for two months.
4. Conclusion
Fungal Spodylodiscitis is particularly rare in patients with an appropriate immune system. Only a small number of patients without immune system disorders have been reported to date. Delay in diagnosis can lead to life-threatening risks. Diagnosis and treatments for this disease are challenging. It seems that debridement surgery combined with antifungal drugs has the best curable results. This diagnosis should also be considered in patients with chronic low back pain who have risk factors for fungal infections.
Ethical Considerations
Compliance with ethical guidelines
The participant was informed about the purpose of the research and its implementation stages; she was also assured about the confidentiality of her information. Moreover, she was allowed to leave the study whenever she wished, and if desired, the results of the research would be available to her.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conception and design: Mohsen Aghapoor, Babak Alijani; Data collection: Mahsa Pakseresht-Mogharab; Drafting the article: Mohsen Aghapoor, Mahsa Pakseresht-Mogharab; Critically revising the article, Reviewing the submitted version, and Approving the final version of the manuscript: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Pillai SS, Reddy S, Thampy S. Aspergillus fumigates Spondylodiscitis in an immunocompetent Patient. MOJ Clinical & Medical Case Reports. 2017; 7(1):170-2. [DOI:10.15406/mojcr.2017.07.00188]
D’agostino C, Scorzolini L, Massetti AP, Carnevalini M, d’Ettorre G, Venditti M, et al. A seven-year prospective study on spondylodiscitis: Epidemiological and microbiological features. Infection. 2010; 38(2):102-7. [DOI:10.1007/s15010-009-9340-8] [PMID]
Zussman BM, Penn DL, Harrop JS. Surgical management of fungal vertebral osteomyelitis. JHN Journal. 2011; 6(2):2. [DOI:10.29046/JHNJ.006.2.001]
Jiang Z, Wang Y, Jiang Y, Xu Y, Meng B. Vertebral osteomyelitis and epidural abscess due to Aspergillus nidulans resulting in spinal cord compression: Case report and literature review. Journal of International Medical Research. 2013; 41(2):502-10. [DOI:10.1177/0300060513476432] [PMID]
Shweikeh F, Zyck S, Sweiss F, Sangtani A, Shweikeh M, Issa H, et al. Aspergillus spinal epidural abscess: Case presentation and review of the literature. Spinal Cord Series and Cases. 2018; 4:19. [DOI:10.1038/s41394-018-0046-y] [PMID] [PMCID]
BN N, Kini U, Alexander B. Vertebral osteomyelitis with a rare etiology diagnosed by fine‐needle aspiration cytology. Diagnostic Cytopathology. 2010; 38(5):360-3. [DOI:10.1002/dc.21212]
Studemeister A, Stevens DA. Aspergillus vertebral osteomyelitis in immunocompetent hosts: Role of triazole antifungal therapy. Clinical Infectious Diseases. 2011; 52(1):e1-e6. [DOI:10.1093/cid/ciq039] [PMID]
van Ooij A, Beckers JMH, Herpers MJHM, Walenkamp GHIM. Surgical treatment of aspergillus spondylodiscitis. European Spine Journal. 2000; 9(1):75-9. [DOI:10.1007/s005860050014] [PMID] [PMCID]
Sobottke R, Seifert H, Fätkenheuer G, Schmidt M, Goßmann A, Eysel P. Current diagnosis and treatment of spondylodiscitis. Deutsches Ärzteblatt International. 2008; 105(10):181-7. [DOI:10.3238/arztebl.2008.0181] [PMID] [PMCID]
Gouliouris T, Aliyu SH, Brown NM. Spondylodiscitis: Update on diagnosis and management. Journal of Antimicrobial Chemotherapy. 2010; 65(suppl_3):iii11-iii24. [DOI:10.1093/jac/dkq303] [PMID]
Sethi S, Siraj F, Kalra KL, Chopra P. Aspergillus vertebral osteomyelitis in immunocompetent patients. Indian Journal of Orthopaedics. 2012; 46(2):246-50. [DOI:10.4103/0019-5413.93693] [PMID] [PMCID]
Gabrielli E, Fothergill AW, Brescini L, Sutton DA, Marchionni E, Orsetti E, et al. Osteomyelitis caused by Aspergillus species: A review of 310 reported cases. Clinical Microbiology and Infection. 2014; 20(6):559-65. [DOI:10.1111/1469-0691.12389] [PMID]
Chi CY, Fung CP, Liu CY. Aspergillus flavus epidural abscess and osteomyelitis in a diabetic patient. Journal of Microbiology Immunology, and Infection. 2003; 36(2):145-8. [PMID]
Nicolle A, de la Blanchardière A, Bonhomme J, Hamon M, Leclercq R, Hitier M. Aspergillus vertebral osteomyelitis in immunocompetent subjects: Case report and review of the literature. Infection. 2013; 41(4):833-40. [DOI:10.1007/s15010-013-0463-6] [PMID]
Aspergillosis is highly fatal in patients with immune system dysfunction and amphotericin B should be prescribed intravenously at the maximum tolerable dose [13]. Treatment of Aspergillus osteomyelitis is multimodal, which includes improvement of chronic hyperglycemia, surgical intervention, and rapid starting of antifungal medication [14]. Whereas the British Infectious Disease Society recommends the use of amphotericin in combination with Flucytosine in severe cases of Aspergillus osteomyelitis, in stable patients Itraconazole has been recommended [7]. The patient was treated with Itraconazole 100 mg twice daily for two months.
4. Conclusion
Fungal Spodylodiscitis is particularly rare in patients with an appropriate immune system. Only a small number of patients without immune system disorders have been reported to date. Delay in diagnosis can lead to life-threatening risks. Diagnosis and treatments for this disease are challenging. It seems that debridement surgery combined with antifungal drugs has the best curable results. This diagnosis should also be considered in patients with chronic low back pain who have risk factors for fungal infections.
Ethical Considerations
Compliance with ethical guidelines
The participant was informed about the purpose of the research and its implementation stages; she was also assured about the confidentiality of her information. Moreover, she was allowed to leave the study whenever she wished, and if desired, the results of the research would be available to her.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conception and design: Mohsen Aghapoor, Babak Alijani; Data collection: Mahsa Pakseresht-Mogharab; Drafting the article: Mohsen Aghapoor, Mahsa Pakseresht-Mogharab; Critically revising the article, Reviewing the submitted version, and Approving the final version of the manuscript: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Pillai SS, Reddy S, Thampy S. Aspergillus fumigates Spondylodiscitis in an immunocompetent Patient. MOJ Clinical & Medical Case Reports. 2017; 7(1):170-2. [DOI:10.15406/mojcr.2017.07.00188]
D’agostino C, Scorzolini L, Massetti AP, Carnevalini M, d’Ettorre G, Venditti M, et al. A seven-year prospective study on spondylodiscitis: Epidemiological and microbiological features. Infection. 2010; 38(2):102-7. [DOI:10.1007/s15010-009-9340-8] [PMID]
Zussman BM, Penn DL, Harrop JS. Surgical management of fungal vertebral osteomyelitis. JHN Journal. 2011; 6(2):2. [DOI:10.29046/JHNJ.006.2.001]
Jiang Z, Wang Y, Jiang Y, Xu Y, Meng B. Vertebral osteomyelitis and epidural abscess due to Aspergillus nidulans resulting in spinal cord compression: Case report and literature review. Journal of International Medical Research. 2013; 41(2):502-10. [DOI:10.1177/0300060513476432] [PMID]
Shweikeh F, Zyck S, Sweiss F, Sangtani A, Shweikeh M, Issa H, et al. Aspergillus spinal epidural abscess: Case presentation and review of the literature. Spinal Cord Series and Cases. 2018; 4:19. [DOI:10.1038/s41394-018-0046-y] [PMID] [PMCID]
BN N, Kini U, Alexander B. Vertebral osteomyelitis with a rare etiology diagnosed by fine‐needle aspiration cytology. Diagnostic Cytopathology. 2010; 38(5):360-3. [DOI:10.1002/dc.21212]
Studemeister A, Stevens DA. Aspergillus vertebral osteomyelitis in immunocompetent hosts: Role of triazole antifungal therapy. Clinical Infectious Diseases. 2011; 52(1):e1-e6. [DOI:10.1093/cid/ciq039] [PMID]
van Ooij A, Beckers JMH, Herpers MJHM, Walenkamp GHIM. Surgical treatment of aspergillus spondylodiscitis. European Spine Journal. 2000; 9(1):75-9. [DOI:10.1007/s005860050014] [PMID] [PMCID]
Sobottke R, Seifert H, Fätkenheuer G, Schmidt M, Goßmann A, Eysel P. Current diagnosis and treatment of spondylodiscitis. Deutsches Ärzteblatt International. 2008; 105(10):181-7. [DOI:10.3238/arztebl.2008.0181] [PMID] [PMCID]
Gouliouris T, Aliyu SH, Brown NM. Spondylodiscitis: Update on diagnosis and management. Journal of Antimicrobial Chemotherapy. 2010; 65(suppl_3):iii11-iii24. [DOI:10.1093/jac/dkq303] [PMID]
Sethi S, Siraj F, Kalra KL, Chopra P. Aspergillus vertebral osteomyelitis in immunocompetent patients. Indian Journal of Orthopaedics. 2012; 46(2):246-50. [DOI:10.4103/0019-5413.93693] [PMID] [PMCID]
Gabrielli E, Fothergill AW, Brescini L, Sutton DA, Marchionni E, Orsetti E, et al. Osteomyelitis caused by Aspergillus species: A review of 310 reported cases. Clinical Microbiology and Infection. 2014; 20(6):559-65. [DOI:10.1111/1469-0691.12389] [PMID]
Chi CY, Fung CP, Liu CY. Aspergillus flavus epidural abscess and osteomyelitis in a diabetic patient. Journal of Microbiology Immunology, and Infection. 2003; 36(2):145-8. [PMID]
Nicolle A, de la Blanchardière A, Bonhomme J, Hamon M, Leclercq R, Hitier M. Aspergillus vertebral osteomyelitis in immunocompetent subjects: Case report and review of the literature. Infection. 2013; 41(4):833-40. [DOI:10.1007/s15010-013-0463-6] [PMID]
Type of Study: Case report |
Subject:
Spine
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |