Thu, Jul 17, 2025
Volume 6, Issue 1 (Winter 2020)
Iran J Neurosurg 2020, 6(1): 29-34 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Apostolakis S, Karagianni A, Chiotaki E, Vlachos K. Attenuation of Motor Evoked Potentials Following Prone PositioningPositioning. Iran J Neurosurg 2020; 6 (1) :29-34
URL: http://irjns.org/article-1-192-en.html
URL: http://irjns.org/article-1-192-en.html
1- Department of Neurosurgery, KAT General Hospital of Attica, Kifisia, Greece , sotapostolakis@gmail.com
2- Department of Neurosurgery, KAT General Hospital of Attica, Athens 145 61, Greece
3- Intraoperative Monitoring Service, GE Scientific, G. Vasios & Co, Ioannina, Greece
4- Department of Neurosurgery, KAT General Hospital of Attica, Kifisia, Greece
2- Department of Neurosurgery, KAT General Hospital of Attica, Athens 145 61, Greece
3- Intraoperative Monitoring Service, GE Scientific, G. Vasios & Co, Ioannina, Greece
4- Department of Neurosurgery, KAT General Hospital of Attica, Kifisia, Greece
Keywords: Endoscopic discectomy, Lumbar disk herniation, Motor evoked potentials, Prone position, Spine surgery
Full Text [PDF 781 kb]
(1432 Downloads)
| Abstract (HTML) (4272 Views)
At the operating theatre, after the establishment of a definitive airway, the patient was placed in the typical prone position for lumbar discectomy, with appropriate padding of the bony surfaces and sites of pressure being meticulously taken care of. Baseline Motor Evoked Potentials (MEP) demonstrated significant asymmetry of the responses between the limbs, with those from the left being disproportionately low, provided the pre-operative clinical examination (Figure 2A). This was more prominent for the tibialis anterior, the gastrocnemius and extensor digitalis longus and to a lesser extent for the abductor hallucis and the quadriceps. The patient was returned to the supine position for a wake-up test (Figure 2B). Propofol was discontinued and with time, motor responses gradually improved. The patient was returned to the prone position, when MEP were deemed satisfactory. Yet, shortly after repositioning, new, though less pronounced, MEP attenuation was observed. At that point, having established once more that every precaution has been taken to avoid excessive external compression of vascular or neuronal structures, it was decided to proceed with the operation under continuous neurophysiological monitoring. The operation was completed successfully, without further incidents. Post-operatively, neurophysiological evaluation demonstrated improved MEP of the left lower limb (Figure 2C), while the patient did not demonstrate any additional neurological deficits and was discharged the day following the operation.
3. Discussion
Considering the particularities of the case presented, it could be deduced that since MEP were normalised following the return in the supine position, this diminution is possibly associated with the positioning of the patient on the operating table. Systematic causes of attenuation of MEP include hypotension, hypothermia, increased levels of halogenated inhalational anaesthetics and intravenous sedation, [5]; however, these should lead to bilaterally affected recordings. In particular, the administration of propofol has a dose dependent effect on motor and somatosensory evoked potentials, decreasing their amplitude bilaterally, whereas no effect has been identified on their latencies [6]. Herein, lack of baseline MEP in the prone position in the absence of propofol, does not allow for an effective evaluation of its effect and thus imposes a great limitation in the present study. In addition, besides the possibility of hardware malfunction, potential mechanisms could be identified following meticulous investigation of the regional anatomy and of the potential particularities of the case.
As far as the anatomy is concerned, direct insult from compression of vascular structures in the iliac fossa, although rare, has been reported previously [7-11]. Interestingly, some cases were thin adolescents in whom MEP were progressively attenuated over more than an hour. In turn, direct neuronal compression is primarily an issue when positioning the upper limbs, while it is scarce in peripheral nerves of the lower limbs [12].
Taking into consideration the nature of the pathology under treatment and the particularities of the anatomy of the individual, additional potential pathogenetic mechanisms could be identified. This is particularly the case when significant stenosis of the spinal canal is the reason for the primary complaint of the patient. In such instances, extreme flexion or extension of the spinal cord could be detrimental [5, 13, 14]. Moreover, intra-operative insults to peripheral nerves secondary to stenosis in their course have been documented [15].
The attenuation of MEP in the present case could potentially be likely attributed to the positioning of the patient, since a significant amelioration was observed shortly after the return to the supine position. However, unlike the aforementioned cases, the anatomic location of the muscles affected, points towards a pathogenetic mechanism different from vascular or neuronal compression.
In particular, muscles of both the ventral (quadriceps, tibialis anterior, extensor digitorum longus) and dorsal (gastrocnemius) compartments of the leg were affected, including the foot (abductor hallucis), innervated by different peripheral nerves (Table 1) and vascularised from various feeding arteries, in which case only occlusion of the iliac artery could lead to the neurophysiologic picture. This is because branches of the internal iliac artery provide sufficient collateral supply to the muscles of the leg, in case of occlusion of the femoral artery proximal to the profunda femoris artery [16].
On the other hand, it is noteworthy that most of the muscles affected are innervated from lower lumbar and upper sacral roots and in particular from the L4, L5 and S1, where the pathology was located. Therefore, the etiology of the neurophysiologic presentation of the patient should be sought at the level of the spinal cord/spinal nerves and could most likely be attributed to a reduced cross-sectional area of the vertebral canal or intervertebral foramen. Previous studies in healthy adults showed that flexion of the lumbar spine does not significantly affect the size of the disc, or the diameter of canal, however it does lead to an overall increase in the area of the canal, resulting from an increase in the subarticular sagittal diameters bilaterally [17]. At the same time, an increase in the diameter and area of the dural sac is observed compared with the neutral position. In addition, it has been demonstrated that the lumbar intervertebral foramina have an increased cross-sectional area in the flexed position [18]. Hence, having excluded other potential causes of MEP attenuation reported in the literature, it could be hypothesised that in the present case their attenuation was possibly caused from the direct compression of the dural sac from the existing pathology, as its cross-sectional area increased relatively to the unaffected diameter of the spinal canal. It is speculated that this bulging of the dural sac over of the free disk fragment further exacerbated the pressure phenomena leading to the failure of any autoregulatory mechanisms.
A similar case has been reported by Ammar et al. [19], in which the patient also post-operatively had no neurological deficits. The attenuation of MOP again was attributed to the biomechanical alterations of the spine due to the prone position.
4. Conclusion
One of the key elements for the success of a neurosurgical procedure is proper patient positioning. Still, even if all precautions have been taken and any potential pitfalls have been accounted for, it is possible that neuronal insult might be caused provided the altered anatomy due to the pathology. Hence, the importance of timely intervention in cases of abnormal intra-operative neurophysiologic study is strongly recommended.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles are considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information; moreover, they were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
All authors have contributed equally to the manuscript.
Conflict of interest
The authors declare that there is no conflict of interest.
References
Rozet I, Vavilala MS. Risks and benefits of patient positioning during neurosurgical care. Anesthesiology Clinics. 2007; 25(3):631-53. [DOI:10.1016/j.anclin.2007.05.009] [PMID] [PMCID]
Lalkhen AG, Bhatia K. Perioperative peripheral nerve injuries. Continuing Education in Anaesthesia Critical Care & Pain. 2012; 12(1):38-42. [DOI:10.1093/bjaceaccp/mkr048]
Bagshaw ON, Jardine A. Cardiopulmonary complications during anaesthesia and surgery for severe thoracic lordoscoliosis. Anaesthesia. 1995; 50(10):890-2. [DOI:10.1111/j.1365-2044.1995.tb05857.x] [PMID]
Edgcombe H, Carter K, Yarrow S. Anaesthesia in the prone position. British Journal of Anaesthesia. 2008; 100(2):165-83. [DOI:10.1093/bja/aem380] [PMID]
Anderson RC, Emerson RG, Dowling KC, Feldstein NA. Attenuation of somatosensory evoked potentials during positioning in a patient undergoing suboccipital craniectomy for chiari i malformation with syringomyelia. Journal of Child Neurology. 2001; 16(12):936-9. [DOI:10.1177/088307380101601214] [PMID]
Nathan N, Tabaraud F, Lacroix F, Mouliès D, Viviand X, Lansade A, et al. Influence of propofol concentrations on multipulse transcranial motor evoked potentials. British Journal of Anaesthesia. 2003; 91(4):493-7. [DOI:10.1093/bja/aeg211] [PMID]
Pankowski R, Roclawski M, Dziegiel K, Ceynowa M, Mikulicz M, Mazurek T, et al. Transient monoplegia as a result of unilateral femoral artery ischemia detected by multimodal intraoperative neuromonitoring in posterior scoliosis surgery: A case report. Medicine (Baltimore). 2016; 95(6):e2748. [DOI:10.1097/MD.0000000000002748] [PMID] [PMCID]
Akagi S, Yoshida Y, Kato I, Sasai K, Saito T, Imamura A, et al. External iliac artery occlusion in posterior spinal surgery. Spine. 1999; 24(8):823-5. [DOI:10.1097/00007632-199904150-00016] [PMID]
Tseng MD, Cappetto L, Majid K, Sternberg D, Settecerri JJ. Bilateral femoral artery ischemia detected by multimodality neuromonitoring during posterior scoliosis surgery: A case report. Spine. 2010; 35(16):E799-803. [DOI:10.1097/BRS.0b013e3181d5577d] [PMID]
Vossler DG, Stonecipher T, Millen MD. Femoral artery ischemia during spinal scoliosis surgery detected by posterior tibial nerve somatosensory-evoked potential monitoring. Spine. 2000; 25(11):1457-9. [DOI:10.1097/00007632-200006010-00021] [PMID]
Trammell TR, Friedlander JK, Reed DB. The effect of lower limb ischemia on somatosensory evoked potentials during spinal surgery. Report of two cases and review of the literature. Spine. 1993; 18(3):413-5. [DOI:10.1097/00007632-199303000-00023] [PMID]
Khan NR, Muhlbauer MS. Differential diagnosis, treatment, and prognosis of peripheral nerve injuries associated with neurosurgical procedures. In: Arthur A, Foley K, Hamm CW, editors. Perioperative considerations and positioning for neurosurgical procedures - a clinical guide: Springer; 2018. pp. 251-64. [DOI:10.1007/978-3-319-72679-3_20] [PMCID]
Kim C, Blank J, McClain BC. Transient paraparesis after general anesthesia in a patient in the prone position. Anesthesiology. 1994; 81(3):775-7. [DOI:10.1097/00000542-199409000-00033] [PMID]
Ofiram E, Lonstein JE, Skinner S, Perra JH. The disappearing evoked potentials: A special problem of positioning patients with skeletal dysplasia: case report. Spine. 2006; 31(14):E464-70. [DOI:10.1097/01.brs.0000222122.37415.4d] [PMID]
Li XJ, Lenke LG, Thuet E, Tan LA, Tuchman A. Prone Position-Induced Quadriceps transcranial motor evoked potentials signal loss-a case report. Spine Deformity. 2018; 6(5):627-30. [DOI:10.1016/j.jspd.2018.02.008] [PMID]
Schuenke M, Schulte E, Schumacher U. The lower limb - Neurovascular Systems: Topographical anatomy. In: Ross LM, Lamperti ED, editors. Thieme atlas of anatomy - general anatomy and musculoskeletal system. Stuttgart: Thieme; 2010. pp. 484-509. https://books.google.com/
Chung SS, Lee CS, Kim SH, Chung MW, Ahn JM. Effect of low back posture on the morphology of the spinal canal. Skeletal Radiology. 2000; 29(4):217-23. [DOI:10.1007/s002560050596] [PMID]
Inufusa A, An HS, Lim TH, Hasegawa T, Haughton VM, Nowicki BH. Anatomic changes of the spinal canal and intervertebral foramen associated with flexion-extension movement. Spine. 1996; 21(21):2412-20. [DOI:10.1097/00007632-199611010-00002] [PMID]
Ammar A, Zarnegar R, Yassari R, Kinon M. Large central lumbar disc herniation causing acute cauda equina syndrome with loss of evoked potentials during prone positioning for surgery. Surgical Neurology International. 2018; 9:66. [DOI:10.4103/sni.sni_482_17] [PMID] [PMCID]
Full Text: (1356 Views)
1. Background and Importance
roper positioning is one of the most crucial determinants of success in neurosurgical operations. An appropriately positioned patient will provide an unobscured visual field, an easily accessible surgical plane, and effortless and comfortable positioning of the surgical team. However, the role of the positioning of the neurosurgical patient is not limited to the ease of the surgeon but is also critical for the avoidance of post-operative complications. The complex nature of the operation per se frequently undermines its importance. In practice, even the slightest deviation from optimal practice may lead to numerous and often disastrous complications, compromising the outcome of an otherwise successful operation.
One of the most technically and logistically demanding positions is the prone position, which is frequently applied in spinal and posterior fossa procedures [1]. This is because the patient, particularly if obese, is subjected to increased weight loads, increasing the risk for formation of pressure sores or for peripheral nerve injury [2], but also at the same time, limited access to the endotracheal tube, changes in respiratory physiology and tracheal or large vessel compression [3, 4] may compromise the administration of proper anesthesia.
Here we report the case of position-related intra-operative diminution of Motor Evoked Potentials (MEP) in a patient who underwent endoscopic lumbar discectomy in the prone position.
2. Case Presentation
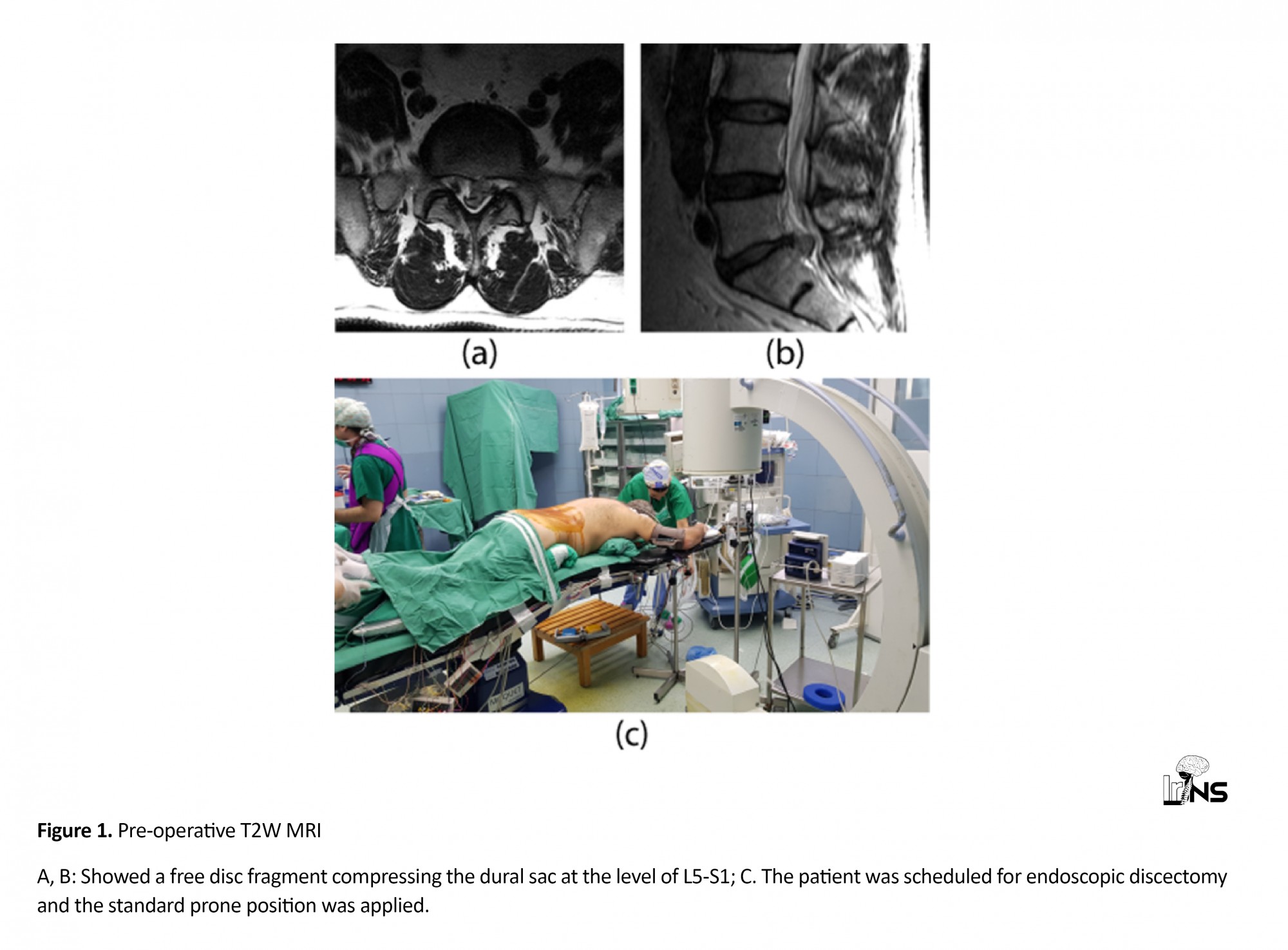
A 52-years-old male patient presented at the outpatient department with sciatica and hypoesthesia of the left lower limb. His medical history was unremarkable of any pathology. Pre-operative neurological examination revealed decreased muscle strength during flexion and extension of the thigh bilaterally (with the left side being more affected), as well as decreased dorsiflexion and plantar flexion of the left foot. Magnetic Resonance Imaging (MRI) of the lumbar spine revealed the presence of a herniated disc at the L5-S1 level with a free disc fragment in the epidural space compressing the L5 nerve root (Figure 1 A, B) and was scheduled for endoscopic discectomy.
roper positioning is one of the most crucial determinants of success in neurosurgical operations. An appropriately positioned patient will provide an unobscured visual field, an easily accessible surgical plane, and effortless and comfortable positioning of the surgical team. However, the role of the positioning of the neurosurgical patient is not limited to the ease of the surgeon but is also critical for the avoidance of post-operative complications. The complex nature of the operation per se frequently undermines its importance. In practice, even the slightest deviation from optimal practice may lead to numerous and often disastrous complications, compromising the outcome of an otherwise successful operation.
One of the most technically and logistically demanding positions is the prone position, which is frequently applied in spinal and posterior fossa procedures [1]. This is because the patient, particularly if obese, is subjected to increased weight loads, increasing the risk for formation of pressure sores or for peripheral nerve injury [2], but also at the same time, limited access to the endotracheal tube, changes in respiratory physiology and tracheal or large vessel compression [3, 4] may compromise the administration of proper anesthesia.
Here we report the case of position-related intra-operative diminution of Motor Evoked Potentials (MEP) in a patient who underwent endoscopic lumbar discectomy in the prone position.
2. Case Presentation
A 52-years-old male patient presented at the outpatient department with sciatica and hypoesthesia of the left lower limb. His medical history was unremarkable of any pathology. Pre-operative neurological examination revealed decreased muscle strength during flexion and extension of the thigh bilaterally (with the left side being more affected), as well as decreased dorsiflexion and plantar flexion of the left foot. Magnetic Resonance Imaging (MRI) of the lumbar spine revealed the presence of a herniated disc at the L5-S1 level with a free disc fragment in the epidural space compressing the L5 nerve root (Figure 1 A, B) and was scheduled for endoscopic discectomy.
At the operating theatre, after the establishment of a definitive airway, the patient was placed in the typical prone position for lumbar discectomy, with appropriate padding of the bony surfaces and sites of pressure being meticulously taken care of. Baseline Motor Evoked Potentials (MEP) demonstrated significant asymmetry of the responses between the limbs, with those from the left being disproportionately low, provided the pre-operative clinical examination (Figure 2A). This was more prominent for the tibialis anterior, the gastrocnemius and extensor digitalis longus and to a lesser extent for the abductor hallucis and the quadriceps. The patient was returned to the supine position for a wake-up test (Figure 2B). Propofol was discontinued and with time, motor responses gradually improved. The patient was returned to the prone position, when MEP were deemed satisfactory. Yet, shortly after repositioning, new, though less pronounced, MEP attenuation was observed. At that point, having established once more that every precaution has been taken to avoid excessive external compression of vascular or neuronal structures, it was decided to proceed with the operation under continuous neurophysiological monitoring. The operation was completed successfully, without further incidents. Post-operatively, neurophysiological evaluation demonstrated improved MEP of the left lower limb (Figure 2C), while the patient did not demonstrate any additional neurological deficits and was discharged the day following the operation.
3. Discussion
Considering the particularities of the case presented, it could be deduced that since MEP were normalised following the return in the supine position, this diminution is possibly associated with the positioning of the patient on the operating table. Systematic causes of attenuation of MEP include hypotension, hypothermia, increased levels of halogenated inhalational anaesthetics and intravenous sedation, [5]; however, these should lead to bilaterally affected recordings. In particular, the administration of propofol has a dose dependent effect on motor and somatosensory evoked potentials, decreasing their amplitude bilaterally, whereas no effect has been identified on their latencies [6]. Herein, lack of baseline MEP in the prone position in the absence of propofol, does not allow for an effective evaluation of its effect and thus imposes a great limitation in the present study. In addition, besides the possibility of hardware malfunction, potential mechanisms could be identified following meticulous investigation of the regional anatomy and of the potential particularities of the case.
As far as the anatomy is concerned, direct insult from compression of vascular structures in the iliac fossa, although rare, has been reported previously [7-11]. Interestingly, some cases were thin adolescents in whom MEP were progressively attenuated over more than an hour. In turn, direct neuronal compression is primarily an issue when positioning the upper limbs, while it is scarce in peripheral nerves of the lower limbs [12].
Taking into consideration the nature of the pathology under treatment and the particularities of the anatomy of the individual, additional potential pathogenetic mechanisms could be identified. This is particularly the case when significant stenosis of the spinal canal is the reason for the primary complaint of the patient. In such instances, extreme flexion or extension of the spinal cord could be detrimental [5, 13, 14]. Moreover, intra-operative insults to peripheral nerves secondary to stenosis in their course have been documented [15].
The attenuation of MEP in the present case could potentially be likely attributed to the positioning of the patient, since a significant amelioration was observed shortly after the return to the supine position. However, unlike the aforementioned cases, the anatomic location of the muscles affected, points towards a pathogenetic mechanism different from vascular or neuronal compression.
In particular, muscles of both the ventral (quadriceps, tibialis anterior, extensor digitorum longus) and dorsal (gastrocnemius) compartments of the leg were affected, including the foot (abductor hallucis), innervated by different peripheral nerves (Table 1) and vascularised from various feeding arteries, in which case only occlusion of the iliac artery could lead to the neurophysiologic picture. This is because branches of the internal iliac artery provide sufficient collateral supply to the muscles of the leg, in case of occlusion of the femoral artery proximal to the profunda femoris artery [16].
On the other hand, it is noteworthy that most of the muscles affected are innervated from lower lumbar and upper sacral roots and in particular from the L4, L5 and S1, where the pathology was located. Therefore, the etiology of the neurophysiologic presentation of the patient should be sought at the level of the spinal cord/spinal nerves and could most likely be attributed to a reduced cross-sectional area of the vertebral canal or intervertebral foramen. Previous studies in healthy adults showed that flexion of the lumbar spine does not significantly affect the size of the disc, or the diameter of canal, however it does lead to an overall increase in the area of the canal, resulting from an increase in the subarticular sagittal diameters bilaterally [17]. At the same time, an increase in the diameter and area of the dural sac is observed compared with the neutral position. In addition, it has been demonstrated that the lumbar intervertebral foramina have an increased cross-sectional area in the flexed position [18]. Hence, having excluded other potential causes of MEP attenuation reported in the literature, it could be hypothesised that in the present case their attenuation was possibly caused from the direct compression of the dural sac from the existing pathology, as its cross-sectional area increased relatively to the unaffected diameter of the spinal canal. It is speculated that this bulging of the dural sac over of the free disk fragment further exacerbated the pressure phenomena leading to the failure of any autoregulatory mechanisms.
A similar case has been reported by Ammar et al. [19], in which the patient also post-operatively had no neurological deficits. The attenuation of MOP again was attributed to the biomechanical alterations of the spine due to the prone position.
4. Conclusion
One of the key elements for the success of a neurosurgical procedure is proper patient positioning. Still, even if all precautions have been taken and any potential pitfalls have been accounted for, it is possible that neuronal insult might be caused provided the altered anatomy due to the pathology. Hence, the importance of timely intervention in cases of abnormal intra-operative neurophysiologic study is strongly recommended.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles are considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information; moreover, they were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
All authors have contributed equally to the manuscript.
Conflict of interest
The authors declare that there is no conflict of interest.
References
Rozet I, Vavilala MS. Risks and benefits of patient positioning during neurosurgical care. Anesthesiology Clinics. 2007; 25(3):631-53. [DOI:10.1016/j.anclin.2007.05.009] [PMID] [PMCID]
Lalkhen AG, Bhatia K. Perioperative peripheral nerve injuries. Continuing Education in Anaesthesia Critical Care & Pain. 2012; 12(1):38-42. [DOI:10.1093/bjaceaccp/mkr048]
Bagshaw ON, Jardine A. Cardiopulmonary complications during anaesthesia and surgery for severe thoracic lordoscoliosis. Anaesthesia. 1995; 50(10):890-2. [DOI:10.1111/j.1365-2044.1995.tb05857.x] [PMID]
Edgcombe H, Carter K, Yarrow S. Anaesthesia in the prone position. British Journal of Anaesthesia. 2008; 100(2):165-83. [DOI:10.1093/bja/aem380] [PMID]
Anderson RC, Emerson RG, Dowling KC, Feldstein NA. Attenuation of somatosensory evoked potentials during positioning in a patient undergoing suboccipital craniectomy for chiari i malformation with syringomyelia. Journal of Child Neurology. 2001; 16(12):936-9. [DOI:10.1177/088307380101601214] [PMID]
Nathan N, Tabaraud F, Lacroix F, Mouliès D, Viviand X, Lansade A, et al. Influence of propofol concentrations on multipulse transcranial motor evoked potentials. British Journal of Anaesthesia. 2003; 91(4):493-7. [DOI:10.1093/bja/aeg211] [PMID]
Pankowski R, Roclawski M, Dziegiel K, Ceynowa M, Mikulicz M, Mazurek T, et al. Transient monoplegia as a result of unilateral femoral artery ischemia detected by multimodal intraoperative neuromonitoring in posterior scoliosis surgery: A case report. Medicine (Baltimore). 2016; 95(6):e2748. [DOI:10.1097/MD.0000000000002748] [PMID] [PMCID]
Akagi S, Yoshida Y, Kato I, Sasai K, Saito T, Imamura A, et al. External iliac artery occlusion in posterior spinal surgery. Spine. 1999; 24(8):823-5. [DOI:10.1097/00007632-199904150-00016] [PMID]
Tseng MD, Cappetto L, Majid K, Sternberg D, Settecerri JJ. Bilateral femoral artery ischemia detected by multimodality neuromonitoring during posterior scoliosis surgery: A case report. Spine. 2010; 35(16):E799-803. [DOI:10.1097/BRS.0b013e3181d5577d] [PMID]
Vossler DG, Stonecipher T, Millen MD. Femoral artery ischemia during spinal scoliosis surgery detected by posterior tibial nerve somatosensory-evoked potential monitoring. Spine. 2000; 25(11):1457-9. [DOI:10.1097/00007632-200006010-00021] [PMID]
Trammell TR, Friedlander JK, Reed DB. The effect of lower limb ischemia on somatosensory evoked potentials during spinal surgery. Report of two cases and review of the literature. Spine. 1993; 18(3):413-5. [DOI:10.1097/00007632-199303000-00023] [PMID]
Khan NR, Muhlbauer MS. Differential diagnosis, treatment, and prognosis of peripheral nerve injuries associated with neurosurgical procedures. In: Arthur A, Foley K, Hamm CW, editors. Perioperative considerations and positioning for neurosurgical procedures - a clinical guide: Springer; 2018. pp. 251-64. [DOI:10.1007/978-3-319-72679-3_20] [PMCID]
Kim C, Blank J, McClain BC. Transient paraparesis after general anesthesia in a patient in the prone position. Anesthesiology. 1994; 81(3):775-7. [DOI:10.1097/00000542-199409000-00033] [PMID]
Ofiram E, Lonstein JE, Skinner S, Perra JH. The disappearing evoked potentials: A special problem of positioning patients with skeletal dysplasia: case report. Spine. 2006; 31(14):E464-70. [DOI:10.1097/01.brs.0000222122.37415.4d] [PMID]
Li XJ, Lenke LG, Thuet E, Tan LA, Tuchman A. Prone Position-Induced Quadriceps transcranial motor evoked potentials signal loss-a case report. Spine Deformity. 2018; 6(5):627-30. [DOI:10.1016/j.jspd.2018.02.008] [PMID]
Schuenke M, Schulte E, Schumacher U. The lower limb - Neurovascular Systems: Topographical anatomy. In: Ross LM, Lamperti ED, editors. Thieme atlas of anatomy - general anatomy and musculoskeletal system. Stuttgart: Thieme; 2010. pp. 484-509. https://books.google.com/
Chung SS, Lee CS, Kim SH, Chung MW, Ahn JM. Effect of low back posture on the morphology of the spinal canal. Skeletal Radiology. 2000; 29(4):217-23. [DOI:10.1007/s002560050596] [PMID]
Inufusa A, An HS, Lim TH, Hasegawa T, Haughton VM, Nowicki BH. Anatomic changes of the spinal canal and intervertebral foramen associated with flexion-extension movement. Spine. 1996; 21(21):2412-20. [DOI:10.1097/00007632-199611010-00002] [PMID]
Ammar A, Zarnegar R, Yassari R, Kinon M. Large central lumbar disc herniation causing acute cauda equina syndrome with loss of evoked potentials during prone positioning for surgery. Surgical Neurology International. 2018; 9:66. [DOI:10.4103/sni.sni_482_17] [PMID] [PMCID]
Type of Study: Case report |
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |