Sun, Jul 13, 2025
Volume 8, Issue 1 (Continuous publishing 2022)
Iran J Neurosurg 2022, 8(1): 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Khizar A, Zahid S. Anal Protrusion of Peritoneal End of Ventriculoperitoneal Shunt and Multiple Brain Abscesses: A Case Report With Review of Literature. Iran J Neurosurg 2022; 8 (1) : 5
URL: http://irjns.org/article-1-305-en.html
URL: http://irjns.org/article-1-305-en.html
1- Department of Neurosurgery, Pakistan Institute of Medical Sciences, Islamabad, Pakistan , arwain.6n2@gmail.com
2- Department of Neurosurgery, Jinnah Medical and Dental College, Karachi, Pakistan
2- Department of Neurosurgery, Jinnah Medical and Dental College, Karachi, Pakistan
Full Text [PDF 1850 kb]
(938 Downloads)
| Abstract (HTML) (2798 Views)
Full Text: (1988 Views)
1. Background and Importance
Hydrocephalus can be effectively treated by putting a mechanical shunt in place to drain the Cerebrospinal Fluid (CSF). Despite the fact that Ventriculoperitoneal (VP) shunting is a well-known treatment, it has a number of drawbacks, including shunt failure, blockage, infection, and abdominal complications (10%-30% of patients). CSF ascites, peritoneal pseudocyst, mesenteric pseudotumor, volvulus, inguinal hernia, peritonitis, intestinal obstruction, and catheter relocation through the scrotum, vagina, umbilicus and intestinal tract have all been reported as abdominal complications. Bowel perforation following VP shunt surgery is an incredibly intriguing complication that accounts for only 0.01%-0.07% of abdominal complications yet has a 15% mortality rate. The colon is the most well-known site of intestinal perforation, and more than half of these individuals are asymptomatic, with anal protrusion of the shunt catheter being the most prevalent symptom [1]. The exact pathophysiology of shunt extrusion is unclear so far and various mechanisms have been proposed to explain it. A satisfactory outcome requires early diagnosis followed by proper management.
2. Case Presentation
A case of a 3.5-year-old boy who presented to us through the emergency department with complaints of fever, vomiting, and seizures (two episodes) for the last ten days is reported. The peritoneal end of the VP shunt was seen protruding out of his anus with a clear discharge of CSF through it as shown in Figure 1.
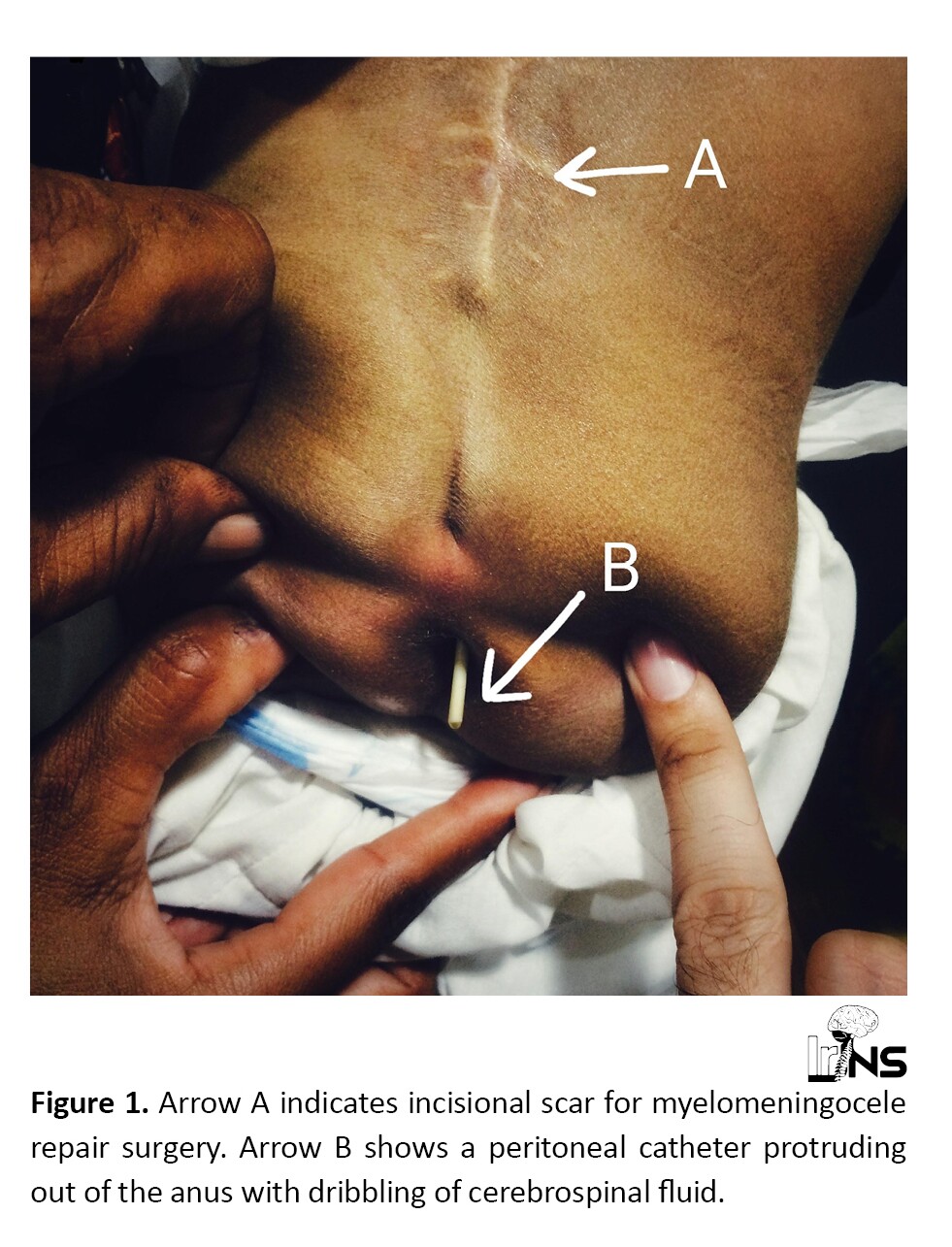
He had lumbar myelomeningocele, which was operated on at the age of one year. Following repair surgery of myelomeningocele, he developed hydrocephalus and underwent ventriculoperitoneal shunt surgery. He remained fine until the age of 3.4 years when he developed a brain abscess and underwent drainage at some other center. According to parents, this peritoneal end of the VP shunt occasionally comes out of the anus after defecation and then goes back by itself.
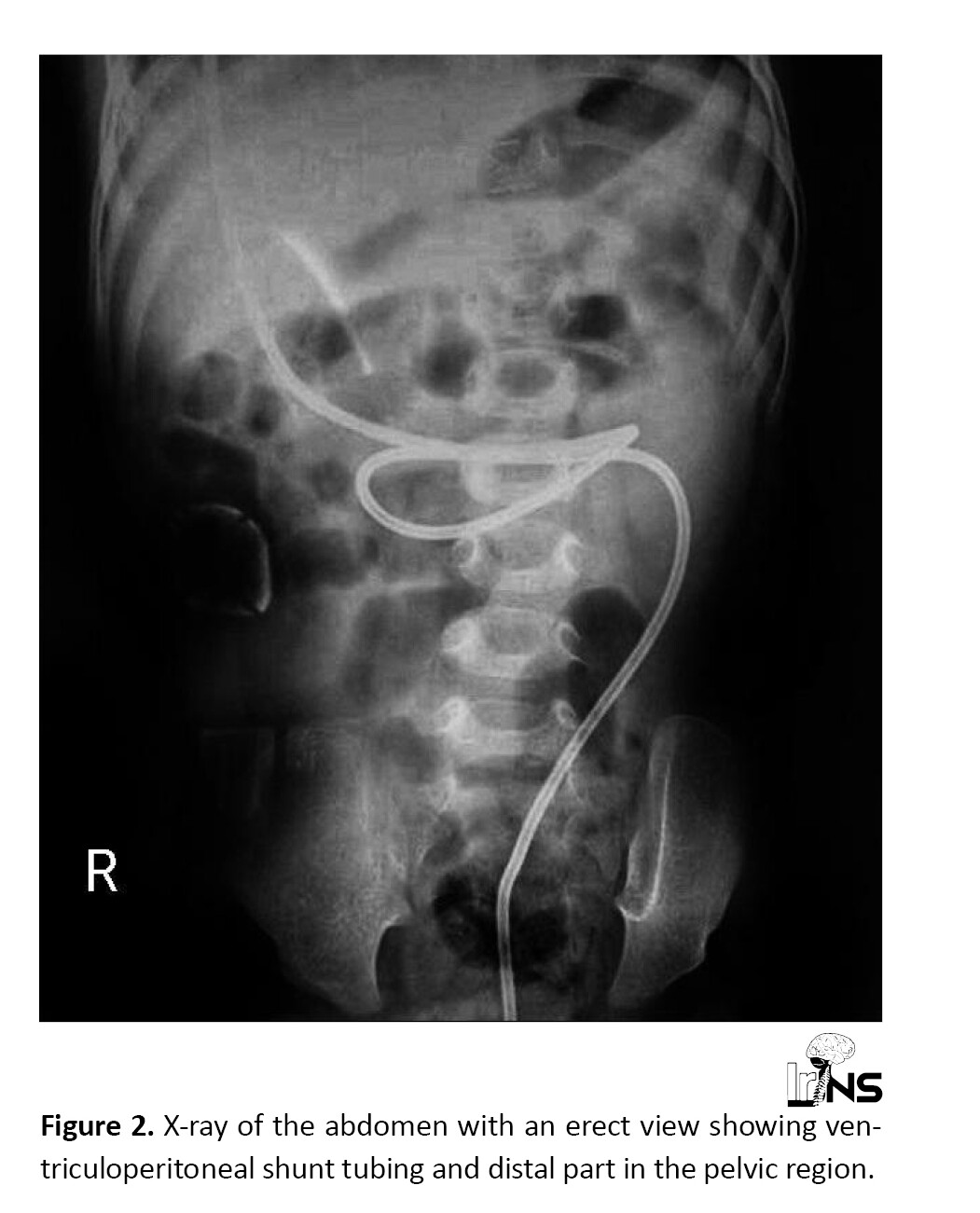
On examination, the child was conscious and febrile, and dribbling of CSF from the protruded part of the VP shunt could be seen. No signs of meningeal irritation and peritonitis were noted. We did erect abdominal X-rays and plain Computed Tomography (CT) of the brain. X-ray showed complete shunt tubing and part of tubing in the pelvic region as shown in Figure 2.
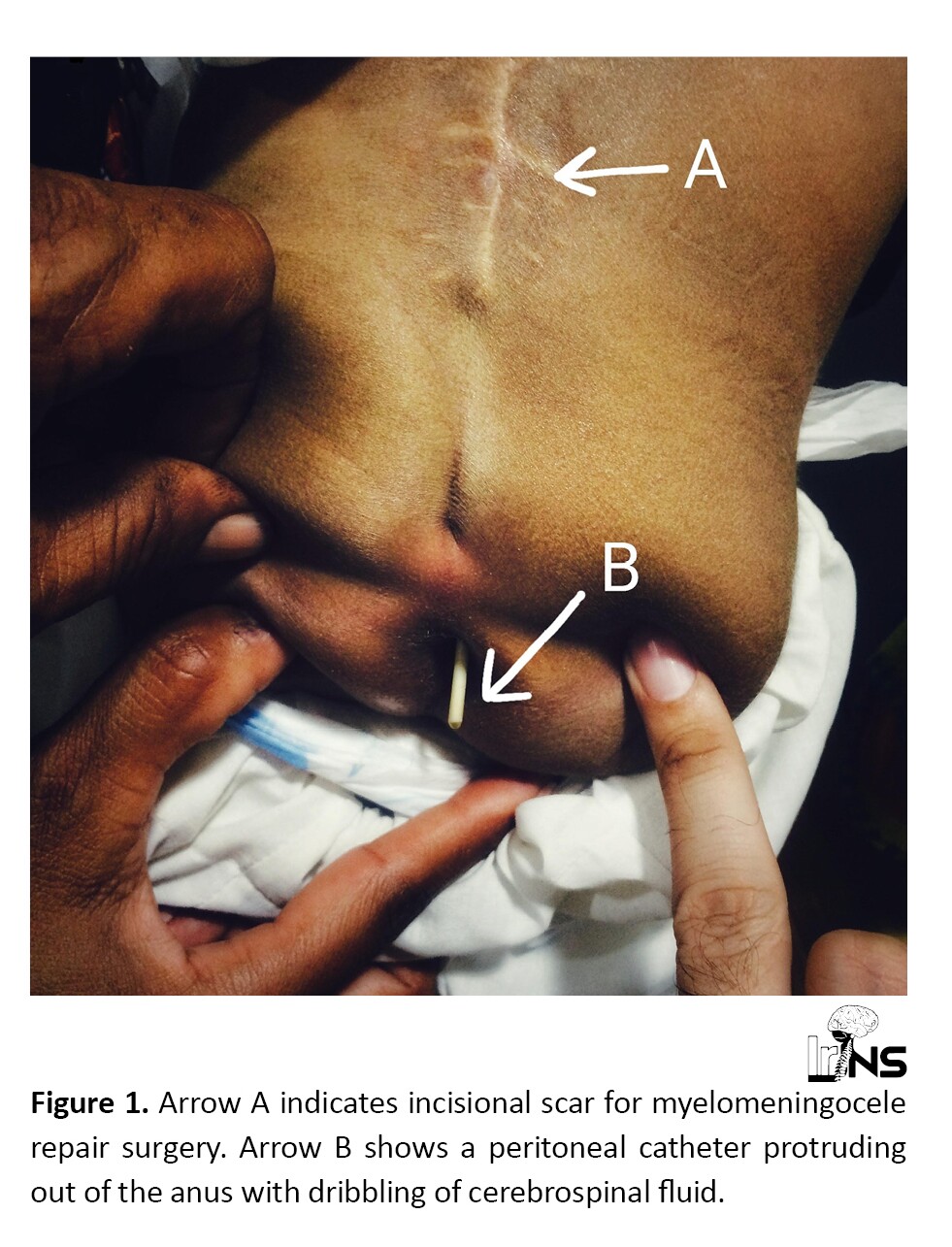
Plain CT of the brain showed multiple brain abscesses as shown in Figure 3. The rest of the lab investigations were normal except raised total leukocyte count. The child underwent surgery in mild sedation. An incision of about 1.5 cm was given in the clavicular region of the child, and then the shunt tubing was cut and separated. The protruding part of the shunt was gently pulled out through the anus. The ventricular end was exteriorized. CSF was sent for culture and sensitivity. Empirical antibiotics, antiepileptics, and steroids were given. No microorganism was found in culture and sensitivity. The child improved over a period of two weeks and his brain abscesses resolved. After the collection of three clear CSF samples, the ventricular end of the VP shunt was removed followed by a new VP shunt insertion on the opposite side.

3. Discussion
A VP shunt anal protrusion is a rare condition. The majority of cases appear months after surgery, and the majority of patients are asymptomatic, with diagnosis based only on visualization of the prolapsed catheter from the anus. The exact pathophysiology behind shunt extrusion is not well-established, but various mechanisms have been proposed to explain it [2]. Children’s thin intestine walls, the VP shunt’s pointed and stiff end, operating surgeons’ use of trocars, previous surgery, chronic shunt irritation, infection, and silicone allergy are only a few factors that could affect the rate of abdominal complications of VP shunt [3, 4]. In 1966, Wilson and Bertan published the first case of anal extrusion of the distal VP shunt [5]. The literature review revealed 68 reported cases of anal protrusion of ventriculoperitoneal shunt, as shown in Table 1.

Abdominal peritonitis may or may not be present in patients with per anal shunt extrusion. As the fibrous tract gets developed at the perforated site, it frequently plugs the breach and prevents fecal matter’s leakage into the peritoneum, which would otherwise result in peritonitis; however, many patients do not have substantial abdominal symptoms. As a result, the correct diagnosis may not be made until gram-negative or anaerobic meningitis, encephalitis, or ventriculitis has fully progressed, resulting in significant morbidity and/or fatality. The cause of shunt ejection is unknown so far, but the most widely accepted theory is that after intestinal perforation, the tubing of the shunt is propelled out by the peristaltic movements in the gut [6].
The time between shunt placement and catheter protrusion from the anus might be between 2 and 20 months, with an average of about 6.1 months [7]. Early diagnosis, thorough clinical, radiographic, and biochemical examinations, and prompt treatment are essential for successful treatment. The conventional treatment strategy involves the removal of the extruded shunt, infection control, and general improvement of the patient, which is then followed by a CSF diversion surgery [6].
Bacterial migration backward through the shunt system can cause infections in the Central Nnervous System (CNS), such as meningitis and ventriculitis, and in rare cases, a brain abscess. The most common organism found in these cases is Escherichia coli and sometimes other enteric pathogens are also present [8]. Gram-negative meningitis or abdominal symptoms in a patient with a VP shunt increase the risk of bowel perforation. The patient’s primary treatment is determined by the presence of sepsis, peritonitis, or intraperitoneal abscess symptoms. A formal exploratory laparotomy is usually not required in a patient with a minor intestinal perforation and no accompanying problems, as in our reported case. After disconnecting the shunt tubing at the clavicular area or the abdominal wall, the bottom end of the shunt tubing should be removed via the rectum, either by proctoscopy, colonoscopy, and sigmoidoscopy, or gently pulling on the protruding tube [4, 9].
The VP shunt’s distal end must never be pulled back into the peritoneal cavity, as this might cause contamination throughout the tract. To prevent CSF infection, an external ventriculostomy should be in place for at least three weeks, coupled with the use of broad-spectrum antibiotics [4, 9, 10]. The patient should get another VP shunt on the other or the same side after recurrent CSF cultures are determined to be sterile. An exploratory laparotomy with shunt removal, thorough lavage, and primary gut wall closure should be performed on patients with bowel perforation peritonitis [4].
4. Conclusion
The risk of bowel perforation in symptomatic ventriculoperitoneal shunt patients must be kept high in case they develop gastrointestinal symptoms or maybe gram-negative or anaerobic meningitis. In children, the time between initial shunt operation and later the discovery of bowel perforation is shortest, and it gradually increases with age. The majority of them have an asymptomatic peritoneal end of the ventriculoperitoneal shunt per anus route. The extruded shunt is removed, infection is controlled, and then a CSF diversion surgery is performed. The extruded end can safely be removed from the migrating orifice. Revision surgery should be considered once recurrent CSF cultures are sterile and the patient is determined to be non-toxic. Early detection and treatment are critical for minimizing and possibly preventing infectious and neurological problems.
Ethical Considerations
Compliance with ethical guidelines
The parents of the child provided written informed consent for the publication of this case report and associated pictures.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conception and design, Reviewing submitted version of manuscript: Ahtesham Khizar; Data collection: Ahtesham Khizar; Drafting the article: Ahtesham Khizar and Soha Zahid; Critically revising the article and Approving the final version: Ahtesham Khizar and Soha Zahid.
Conflict of interest
The authors declared no conflict of interest.
References
Hydrocephalus can be effectively treated by putting a mechanical shunt in place to drain the Cerebrospinal Fluid (CSF). Despite the fact that Ventriculoperitoneal (VP) shunting is a well-known treatment, it has a number of drawbacks, including shunt failure, blockage, infection, and abdominal complications (10%-30% of patients). CSF ascites, peritoneal pseudocyst, mesenteric pseudotumor, volvulus, inguinal hernia, peritonitis, intestinal obstruction, and catheter relocation through the scrotum, vagina, umbilicus and intestinal tract have all been reported as abdominal complications. Bowel perforation following VP shunt surgery is an incredibly intriguing complication that accounts for only 0.01%-0.07% of abdominal complications yet has a 15% mortality rate. The colon is the most well-known site of intestinal perforation, and more than half of these individuals are asymptomatic, with anal protrusion of the shunt catheter being the most prevalent symptom [1]. The exact pathophysiology of shunt extrusion is unclear so far and various mechanisms have been proposed to explain it. A satisfactory outcome requires early diagnosis followed by proper management.
2. Case Presentation
A case of a 3.5-year-old boy who presented to us through the emergency department with complaints of fever, vomiting, and seizures (two episodes) for the last ten days is reported. The peritoneal end of the VP shunt was seen protruding out of his anus with a clear discharge of CSF through it as shown in Figure 1.
He had lumbar myelomeningocele, which was operated on at the age of one year. Following repair surgery of myelomeningocele, he developed hydrocephalus and underwent ventriculoperitoneal shunt surgery. He remained fine until the age of 3.4 years when he developed a brain abscess and underwent drainage at some other center. According to parents, this peritoneal end of the VP shunt occasionally comes out of the anus after defecation and then goes back by itself.
On examination, the child was conscious and febrile, and dribbling of CSF from the protruded part of the VP shunt could be seen. No signs of meningeal irritation and peritonitis were noted. We did erect abdominal X-rays and plain Computed Tomography (CT) of the brain. X-ray showed complete shunt tubing and part of tubing in the pelvic region as shown in Figure 2.
Plain CT of the brain showed multiple brain abscesses as shown in Figure 3. The rest of the lab investigations were normal except raised total leukocyte count. The child underwent surgery in mild sedation. An incision of about 1.5 cm was given in the clavicular region of the child, and then the shunt tubing was cut and separated. The protruding part of the shunt was gently pulled out through the anus. The ventricular end was exteriorized. CSF was sent for culture and sensitivity. Empirical antibiotics, antiepileptics, and steroids were given. No microorganism was found in culture and sensitivity. The child improved over a period of two weeks and his brain abscesses resolved. After the collection of three clear CSF samples, the ventricular end of the VP shunt was removed followed by a new VP shunt insertion on the opposite side.

3. Discussion
A VP shunt anal protrusion is a rare condition. The majority of cases appear months after surgery, and the majority of patients are asymptomatic, with diagnosis based only on visualization of the prolapsed catheter from the anus. The exact pathophysiology behind shunt extrusion is not well-established, but various mechanisms have been proposed to explain it [2]. Children’s thin intestine walls, the VP shunt’s pointed and stiff end, operating surgeons’ use of trocars, previous surgery, chronic shunt irritation, infection, and silicone allergy are only a few factors that could affect the rate of abdominal complications of VP shunt [3, 4]. In 1966, Wilson and Bertan published the first case of anal extrusion of the distal VP shunt [5]. The literature review revealed 68 reported cases of anal protrusion of ventriculoperitoneal shunt, as shown in Table 1.

Abdominal peritonitis may or may not be present in patients with per anal shunt extrusion. As the fibrous tract gets developed at the perforated site, it frequently plugs the breach and prevents fecal matter’s leakage into the peritoneum, which would otherwise result in peritonitis; however, many patients do not have substantial abdominal symptoms. As a result, the correct diagnosis may not be made until gram-negative or anaerobic meningitis, encephalitis, or ventriculitis has fully progressed, resulting in significant morbidity and/or fatality. The cause of shunt ejection is unknown so far, but the most widely accepted theory is that after intestinal perforation, the tubing of the shunt is propelled out by the peristaltic movements in the gut [6].
The time between shunt placement and catheter protrusion from the anus might be between 2 and 20 months, with an average of about 6.1 months [7]. Early diagnosis, thorough clinical, radiographic, and biochemical examinations, and prompt treatment are essential for successful treatment. The conventional treatment strategy involves the removal of the extruded shunt, infection control, and general improvement of the patient, which is then followed by a CSF diversion surgery [6].
Bacterial migration backward through the shunt system can cause infections in the Central Nnervous System (CNS), such as meningitis and ventriculitis, and in rare cases, a brain abscess. The most common organism found in these cases is Escherichia coli and sometimes other enteric pathogens are also present [8]. Gram-negative meningitis or abdominal symptoms in a patient with a VP shunt increase the risk of bowel perforation. The patient’s primary treatment is determined by the presence of sepsis, peritonitis, or intraperitoneal abscess symptoms. A formal exploratory laparotomy is usually not required in a patient with a minor intestinal perforation and no accompanying problems, as in our reported case. After disconnecting the shunt tubing at the clavicular area or the abdominal wall, the bottom end of the shunt tubing should be removed via the rectum, either by proctoscopy, colonoscopy, and sigmoidoscopy, or gently pulling on the protruding tube [4, 9].
The VP shunt’s distal end must never be pulled back into the peritoneal cavity, as this might cause contamination throughout the tract. To prevent CSF infection, an external ventriculostomy should be in place for at least three weeks, coupled with the use of broad-spectrum antibiotics [4, 9, 10]. The patient should get another VP shunt on the other or the same side after recurrent CSF cultures are determined to be sterile. An exploratory laparotomy with shunt removal, thorough lavage, and primary gut wall closure should be performed on patients with bowel perforation peritonitis [4].
4. Conclusion
The risk of bowel perforation in symptomatic ventriculoperitoneal shunt patients must be kept high in case they develop gastrointestinal symptoms or maybe gram-negative or anaerobic meningitis. In children, the time between initial shunt operation and later the discovery of bowel perforation is shortest, and it gradually increases with age. The majority of them have an asymptomatic peritoneal end of the ventriculoperitoneal shunt per anus route. The extruded shunt is removed, infection is controlled, and then a CSF diversion surgery is performed. The extruded end can safely be removed from the migrating orifice. Revision surgery should be considered once recurrent CSF cultures are sterile and the patient is determined to be non-toxic. Early detection and treatment are critical for minimizing and possibly preventing infectious and neurological problems.
Ethical Considerations
Compliance with ethical guidelines
The parents of the child provided written informed consent for the publication of this case report and associated pictures.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conception and design, Reviewing submitted version of manuscript: Ahtesham Khizar; Data collection: Ahtesham Khizar; Drafting the article: Ahtesham Khizar and Soha Zahid; Critically revising the article and Approving the final version: Ahtesham Khizar and Soha Zahid.
Conflict of interest
The authors declared no conflict of interest.
References
- Etus V. Ventriculoperitoneal shunt catheter protrusion through the anus: Case report of an uncommon complication and literature review. Commentary. Child's Nervous System. 2011; 27(11):2015. [DOI:10.1007/s00381-011-1555-1] [PMID]
- Alhendawy I, Dhaliwal T, Siedler DG, Homapour B. Early postoperative colonic ventriculoperitoneal shunt migration with trans-anal protrusion: A unique case report. International Journal of Surgery Case Reports. 2021; 81:105796. [DOI:10.1016/j.ijscr.2021.105796] [PMID] [PMCID]
- Hai A, Rab AZ, Ghani I, Huda MF, Quadir AQ. Perforation into gut by ventriculoperitoneal shunts: A report of two cases and review of the literature. Journal of Indian Association of Pediatric Surgeons. 2011; 16(1):31-3. [DOI:10.4103/0971-9261.74521] [PMID] [PMCID]
- Hasan A, Sharma S, Chopra S, Purohit DK. Anal extrusion of ventriculoperitoneal shunt: A report of two cases and review of literature. Journal of Pediatric Neurosciences. 2018; 13(1):8-12. [PMID]
- Wilson CB, Bertan V. Perforation of the bowel complicating peritoneal shunt for hydrocephalus. Report of two cases. The American Surgeon. 1966; 32(9):601-3. [PMID]
- Bodeliwala S, Agrawal A, Mittal A, Singh D, Vageesh BG, Singh H. Transanal protrusion of ventriculoperitoneal shunt via appendicular perforation: A rare case report. Journal of Pediatric Neurosciences. 2016; 11(3):274-6. [DOI:10.4103/1817-1745.193383] [PMID] [PMCID]
- Akcora B, Serarslan Y, Sangun O. Bowel perforation and transanal protrusion of a ventriculoperitoneal shunt catheter. Pediatric Neurosurgery. 2006; 42(2):129-31. [DOI:10.1159/000090470] [PMID]
- Marino M, Phillips C. Methicillin-resistant staphylococcus aureus meningitis from transanal migration of a ventriculoperitoneal shunt.The Journal of Emergency Medicine. 2019; 57(3):e81-4. [DOI:10.1016/j.jemermed.2019.06.015] [PMID]
- Sathyanarayana S, Wylen EL, Baskaya MK, Nanda A. Spontaneous bowel perforation after ventriculoperitoneal shunt surgery: Case report and a review of 45 cases. Surgical Neurology. 2000; 54(5):388-96. [DOI:10.1016/S0090-3019(00)00334-7]
- Yılmaz N, Kıymaz N, Yılmaz C, Çaksen H, Yuca SA. Anal protrusion of ventriculo-peritoneal shunt catheter: Report of two infants. Journal of Pediatric Neurology. 2004; 2(4):241-4. [DOI:10.1055/S-0035-1557227]
- Miserocchi G, Sironi VA, Ravagnati L. Anal protrusion as a complication of ventriculo-peritoneal shunt. Case report and review of the literature. Journal of Neurosurgical Sciences. 1984; 28(1):43-6. [PMID]
- Aricó M, Beluffi G, Fiori P, Chiari G, Pezzotta S, Podesta AF, et al. Rectal extrusion of the catheter and air ventriculography following bowel perforation in ventriculo-peritoneal shunt. Pediatric Radiology. 1985; 15(1):53-5. [DOI:10.1007/BF02387854] [PMID]
- Ali J, Cheah FK. Per rectal extrusion of a ventriculo peritoneal shunt catheter. A case report. The Medical Journal of Malaysia. 1987; 42(3):201-3. [PMID]
- Sharma BS, Kak VK. Multiple subdural abscesses following colonic perforation--a rare complication of a ventriculoperitoneal shunt. Pediatric Radiology. 1988; 18(5):407-8. [DOI:10.1007/BF02388048] [PMID]
- Aranda G, Pretto R, Velarde C. [Asymptomatic rectosigmoid perforation and peranal extrusion of a catheter of ventriculoperitoneal derivation (Spanish)]. Revista Médica de Panamá. 1989; 14(2):108-11. [PMID]
- Adeloye A. Protrusion of ventriculo peritoneal shunt through the anus: Report of two cases. East African Medical Journal. 1997; 74(5):337-9. [PMID]
- Caksen H, Kiymaz N, Odabaş D, Tuncer O, Ataş B. Anal protrusion of ventriculo-peritoneal shunt catheter in an infant. Brain and Development. 2003; 25(2):146-7. [DOI:10.1016/S0387-7604(02)00158-4]
- Sharma A, Pandey AK, Radhakrishnan M, Kumbhani D, Das HS, Desai N. Endoscopic management of anal protrusion of ventriculo-peritoneal shunt. Indian Journal of Gastroenterology . 2003; 22(1):29-30. [PMID]
- Ferreira PR, Bizzi JJ, Amantéa SL. Protrusion of ventriculoperitoneal shunt catheter through the anal orifice. A rare abdominal complication. Journal of Pediatric Surgery. 2005; 40(9):1509-10. [DOI:10.1016/j.jpedsurg.2005.05.073] [PMID]
- Gupta SK, Jaiswal AK, Kumar S. Ventriculoperitoneal shunt catheter masquerading as ascariasis. Journal of Clinical Neuroscience. 2005; 12(8):966-7. [DOI:10.1016/j.jocn.2004.11.016] [PMID]
- Ansari S, Nejat F, Dadmehr M. Extrusion of ventriculoperitoneal shunt catheter through the rectum and retrograde meningitis. The Pediatric Infectious Disease Journal. 2005; 24(11):1027. [PMID]
- Ghritlaharey RK, Budhwani KS, Shrivastava DK, Gupta G, Kushwaha AS, Chanchlani R, et al. Trans-anal protrusion of ventriculo-peritoneal shunt catheter with silent bowel perforation: Report of ten cases in children. Pediatric Surgery International. 2007; 23(6):575-80. [PMID]
- Zhou F, Chen G, Zhang J. Bowel perforation secondary to ventriculoperitoneal shunt: Case report and clinical analysis. Journal of International Medical Research. 2007; 35(6):926-9. [DOI:10.1177/147323000703500624] [PMID]
- Matsuoka H, Takegami T, Maruyama D, Hamasaki T, Kakita K, Mineura K. Transanal prolapse of a ventriculoperitoneal shunt catheter: Case report. Neurologia Medico-Chirurgica. 2008; 48(11):526-8. [DOI:10.2176/nmc.48.526] [PMID]
- Li HN, Tan TC, Cheung FC. Transanal protrusion of ventriculoperitoneal shunt. Surgical Practice. 2008; 12(3):93-6. [DOI:10.1111/j.1744-1633.2008.00407.x]
- Sengul G, Akar A. Transanal prolapse of a ventriculoperitoneal shunt. Neurosciences. 2008; 13(2):174-5. [PMID]
- Glatstein M, Constantini S, Scolnik D, Shimoni N, Roth J. Ventriculoperitoneal shunt catheter protrusion through the anus: Case report of an uncommon complication and literature review. Child's Nervous System. 2011; 27(11):2011-4. [DOI:10.1007/s00381-011-1551-5] [PMID]
- Hayama T, Ishihara S, Yamazaki N, Akahane T, Shimada R, Horiuchi A, et al. Severance of a ventriculoperitoneal shunt catheter implanted between the cerebral ventricle and peritoneal cavity, resulting in protrusion from the anus. International Surgery. 2011; 96(2):148-52. [DOI:10.9738/1392.1] [PMID]
- Ozturk H, Is M, Ozturk H, Kucuk A, Dosoglu M. Transanal protrusion of a ventriculoperitoneal shunt catheter. Journal of the College of Physicians and Surgeons--Pakistan. 2012; 22(11):733-4. [PMID]
- Borkar SA, Mahapatra AK. Ventriculoperitoneal shunt catheter protrusion through the anus. Child's Nervous System. 2012; 28(3):341-2. [DOI:10.1007/s00381-012-1684-1] [PMID]
- Sharifian A, Abdollahi A, Maddah G, Anaraki F, Alvandipour M, Abbasi Sahebi M, et al. Spontaneous transanal protrusion of ventriculoperitoneal catheter: A case report. Acta Medica Iranica. 2013; 51(2):135-8. [PMID]
- Phani K. Transanal protrusion of ventriculo-peritoneal shunt catheter. Journal of Dr. NTR University of Health Sciences. 2013; 2(2):115-7. [DOI:10.4103/2277-8632.112336]
- Gedik AH, Uzuner S, Cindemir E, Bayraktar S, Torun E, Seyithanoglu H, et al. [Transanal protrusion of ventriculo-peritoneal shunt related to colon perforation: Two case reports (Turkish)]. Turkish Pediatrics Archive. 2013; 48(3):255-9. https://dergipark.org.tr/en/download/article-file/140541
- Plummer NR, Tokala A, Date RS. Transanal protrusion of ventriculoperitoneal shunt reflecting asymptomatic perforation of the large bowel. BMJ Case Reports. 2014; 2014:bcr2014204842. [DOI:10.1136/bcr-2014-204842] [PMID] [PMCID]
- Grewal SS, Jhawar SS, Gupta B, Bedi NK. Silent bowel perforation with per anal protrusion of ventriculoperitoneal shunt. CHRISMED Journal of Health and Research. 2014; 1(2):113-5. [DOI:10.4103/2348-3334.134278]
- Bansal H, Gupta G, Gupta M, Kaushal R. Unusual ventriculoperitoneal (VP) shunt tube extrusion through anus in a child with dandy walker malformation: A rare case report. Journal of Clinical and Diagnostic Research: JCDR. 2015; 9(1):PD25-6. [PMID]
- Thiong’o GM, Luzzio C, Albright AL. Ventriculoperitoneal shunt perforations of the gastrointestinal tract. Journal of Neurosurgery: Pediatrics. 2015; 16(1):36-41. [DOI:10.3171/2014.11.PEDS14347] [PMID]
- Kumar TR, Kishore MS. En-masse Protrusion of Ventriculo-peritoneal Shunt Tube Through the Anus. Indian Pediatrics. 2016; 53:747-48. https://www.indianpediatrics.net/aug2016/aug-747-748.htm
- Bales J, Morton RP, Airhart N, Flum D, Avellino AM. Transanal presentation of a distal ventriculoperitoneal shunt catheter: Management of bowel perforation without laparotomy. Surgical Neurology International. 2016; 7(Suppl 44):S1150-3. [PMID] [PMCID]
- Sosuncu E, Gülşen İ, Kıymaz N, Ağengin K, Şimşek M, Melek M. Anal protrusion caused by a ventriculoperitoneal shunt. Van Medical Journal. 2016; 23(1):95-7. [DOI:10.5505/vtd.2016.15046]
- Indra Gunawan P, Gunadi Ranuh IR, Fardah Atthiyah A. Anal extrusion of the ventriculoperitoneal shunt catheter. Acta Medica Academica. 2017; 46(1):65-6. [DOI:10.5644/ama2006-124.190] [PMID]
- Liu, Li C, Tian Y. Ventriculo-peritoneal shunt trans-anal protrusion causing Escherichia coli ventriculitis in child: Case report and review of the literature. Chinese Neurosurgical Journal. 2017; 3:9[DOI:10.1186/s41016-016-0064-1]
- Amouei A, Babaei-Zarch M, Ehsani F, Tabataei SM, Asadi MJ. Penetration of ventriculoperitoneal shunt into the transverse colon and anal extrusion in a child: A rare case report. Case Reports in Clinical Practice. 2017; 2(2):29-32. https://crcp.tums.ac.ir/index.php/crcp/article/view/103
- Burhan B, Serdar KB, Abdurrahman A, Edip AM, Ebuzer D. Abdominal complications of ventriculoperitoneal shunt in pediatric patients: Experiences of a pediatric surgery clinic. World Neurosurgery. 2018; 118:e129-36. [PMID]
- Guthe SP, Pravin S, Darade P, Velho V. Silent migration of ventriculoperitoneal shunt per anus in a child: Management and review of literature. Asian Journal of Neurosurgery. 2018; 13(2):446-8. [DOI:10.4103/1793-5482.228559] [PMID] [PMCID]
- Turkis OF, Karadag A, Middlebrooks EH, Senoglu M. Anal extrusion of a ventriculoperitoneal shunt. Journal of the College of Physicians and Surgeons--Pakistan: JCPSP. 2019; 29(5):478-80. [DOI:10.29271/jcpsp.2019.05.478] [PMID]
- Bakshi S. Spontaneous trans-anal extrusion of caudally migrated ventriculo-peritoneal shunt tip in a child: A case report. Surgical Case Reports. 2020; 6(1):50. [DOI:10.1186/s40792-020-00813-0] [PMID] [PMCID]
- Jonuzi A, Begic S, Zvizdic Z, Karavdic K, Popovic N, Milisic E, et al. A rare case of colon perforation complicating a vetriculoperitoneal shunt with trans-anal protrusion. Acta Chirurgica Croatica. 2021; 18(1):11-4. https://www.acc.hkd.com.hr/index.php/ACC/article/view/125
- Heng YW, Yap KB. Trans-anal protrusion of the distal end of ventriculo-peritoneal (VP) shunt-The role of ommaya shunt. Journal of Pediatric Surgery Case Reports. 2021; 72:101965. [DOI:10.1016/j.epsc.2021.101965]
- Lim SL, Shahrulsalam M, Shah M, Omar N. Protrusion of ventriculoperitoneal shunt catheter tip through anus with silence abdomen. Polish Annals of Medicine. 2021; 28(2):210-3. [DOI:10.29089/2020.20.00158]
- Bosy HH, Albarnawi BM, Ashour KM, Alyasi A, Alsulaihebi AS. Early anal protrusion of distal ventriculoperitoneal catheter due to iatrogenic colonic perforation: A case report and review of literature. Cureus. 2021; 13(12):e20296. Published 2021. [DOI:10.7759/cureus.20296] [PMID] [PMCID]
Type of Study: Case report |
Subject:
Pediatric Neurosurgery
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






