Tue, Feb 3, 2026
Volume 2, Issue 1 (6-2016)
Iran J Neurosurg 2016, 2(1): 15-18 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Gupta R, Narayan S. Post-operative Pseudomeningocele after Spine Surgery: Rare Cause of Failed Back Syndrome. Iran J Neurosurg 2016; 2 (1) :15-18
URL: http://irjns.org/article-1-32-en.html
URL: http://irjns.org/article-1-32-en.html
1- MD, Professor, Department of Neurosurgery, Sri Aurobindo Medical College and PG Institute, Indore, India
2- MD, MCh Resident, Department of Neurosurgery, Sri Aurobindo Medical College and PG Institute, Indore, India ,sharad_jsr@yahoo.com
2- MD, MCh Resident, Department of Neurosurgery, Sri Aurobindo Medical College and PG Institute, Indore, India ,
Full Text [PDF 588 kb]
(12098 Downloads)
| Abstract (HTML) (8362 Views)
References
Full Text: (8462 Views)
Background and Importance
Lumbar pseudomeningocele is an extradural cystic collection of cerebrospinal fluid with no dural covering. It results from a breach in the dura–arachnoid layer. This rare complication results from a dural rent or dehiscence after laminectomy.
The exact cause of postoperative pseudomeningocele incidence is unknown and is usually under reported, as most of these patients remain asymptomatic (1). The other possible reason for under reporting may be reluctance on part of the operative surgeon. Diagnosis of this rare entity is reached on a post-operative magnetic resonance imaging scan. We came across two post-laminectomy patients with symptoms of low back pain, radicular pain and swelling over the operative site in past one year.
An MRI scan was performed in these patients which revealed the presence of a pseudomeningocele at the site of previous surgery. Both patients were managed with reexploration and surgical closure of the dural defect. Patients showed improvement in symptoms post operatively. This prompted us to revisit pseudomeningocele as a possible cause of failed back syndrome with its literature review.
Case presentation
Failed back syndrome or post-laminectomy syndrome is increasingly observed by surgeons in clinical practice due to the large number of spine surgeries being performed. The common cause of this often cited entity can be persistent disc herniation, post-operative infection, post-operative fibrosis or improper spinal instrumentation and fusion. Traumatic pseudomeningocele is an uncommon and rarely seen complication following spine surgery, and may be a cause of failed back syndrome in some symptomatic patients.
We routinely came across numerous operated patients with persistent symptoms of low back nd radicular pain. These patients should undergo a thorough clinical and radiological evaluation to determine the cause of their symptoms. We came across two patients with post-operative pseudomeningoceles in the past year. A literature review was done to determine the incidence of this entity and its optimal management.
CASE 1
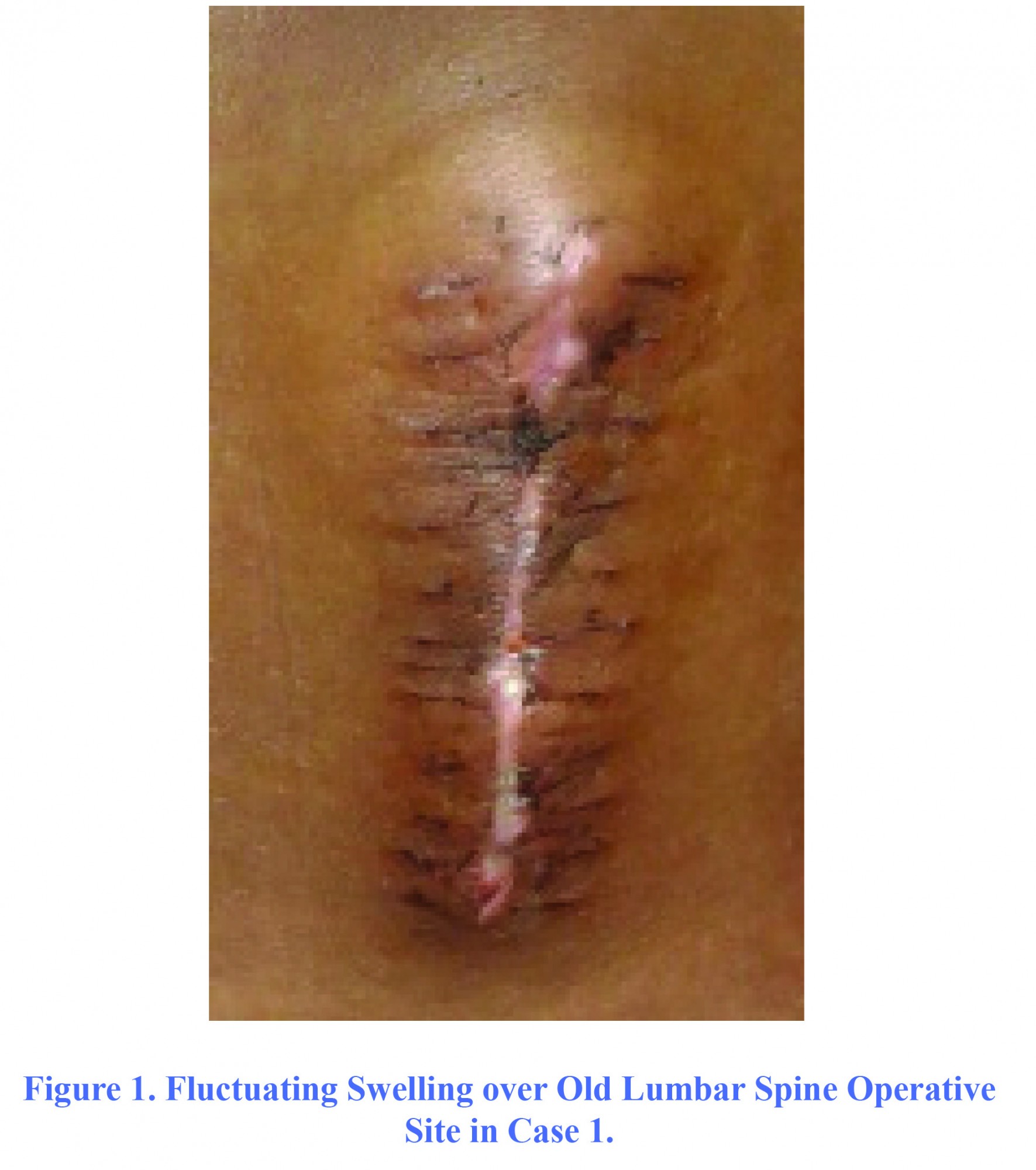
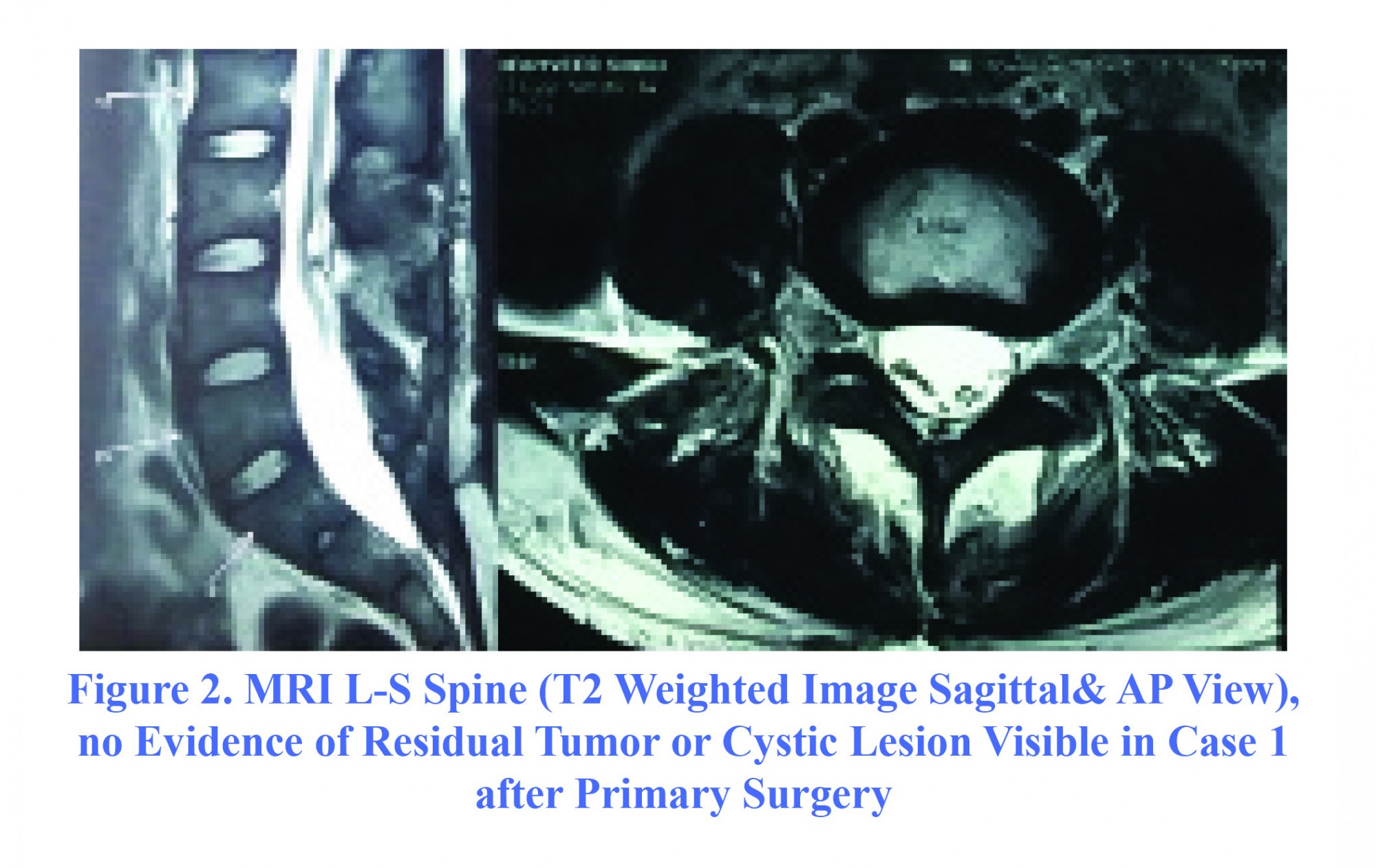
A 29-year-old male presented with complaints of low back pain and progressive fluctuating swelling over the operative site (Figure 1). There was associated low back and radicular pain over both lower limbs for last 6 months. The patient had history of having undergone a right sided keyhole L4 laminotomy with microsurgical excision of a filum terminale dermoid cyst with detethering of low-lying cord 10 months ago. The patient gave history of an uneventful post-operative period. Immediate post-operative MRI scan did not reveal evidence of any cerebrospinal fluid (CSF) collection or residual tumor (Figure 2).
The exact cause of postoperative pseudomeningocele incidence is unknown and is usually under reported, as most of these patients remain asymptomatic (1). The other possible reason for under reporting may be reluctance on part of the operative surgeon. Diagnosis of this rare entity is reached on a post-operative magnetic resonance imaging scan. We came across two post-laminectomy patients with symptoms of low back pain, radicular pain and swelling over the operative site in past one year.
An MRI scan was performed in these patients which revealed the presence of a pseudomeningocele at the site of previous surgery. Both patients were managed with reexploration and surgical closure of the dural defect. Patients showed improvement in symptoms post operatively. This prompted us to revisit pseudomeningocele as a possible cause of failed back syndrome with its literature review.
Case presentation
Failed back syndrome or post-laminectomy syndrome is increasingly observed by surgeons in clinical practice due to the large number of spine surgeries being performed. The common cause of this often cited entity can be persistent disc herniation, post-operative infection, post-operative fibrosis or improper spinal instrumentation and fusion. Traumatic pseudomeningocele is an uncommon and rarely seen complication following spine surgery, and may be a cause of failed back syndrome in some symptomatic patients.
We routinely came across numerous operated patients with persistent symptoms of low back nd radicular pain. These patients should undergo a thorough clinical and radiological evaluation to determine the cause of their symptoms. We came across two patients with post-operative pseudomeningoceles in the past year. A literature review was done to determine the incidence of this entity and its optimal management.
CASE 1
A 29-year-old male presented with complaints of low back pain and progressive fluctuating swelling over the operative site (Figure 1). There was associated low back and radicular pain over both lower limbs for last 6 months. The patient had history of having undergone a right sided keyhole L4 laminotomy with microsurgical excision of a filum terminale dermoid cyst with detethering of low-lying cord 10 months ago. The patient gave history of an uneventful post-operative period. Immediate post-operative MRI scan did not reveal evidence of any cerebrospinal fluid (CSF) collection or residual tumor (Figure 2).
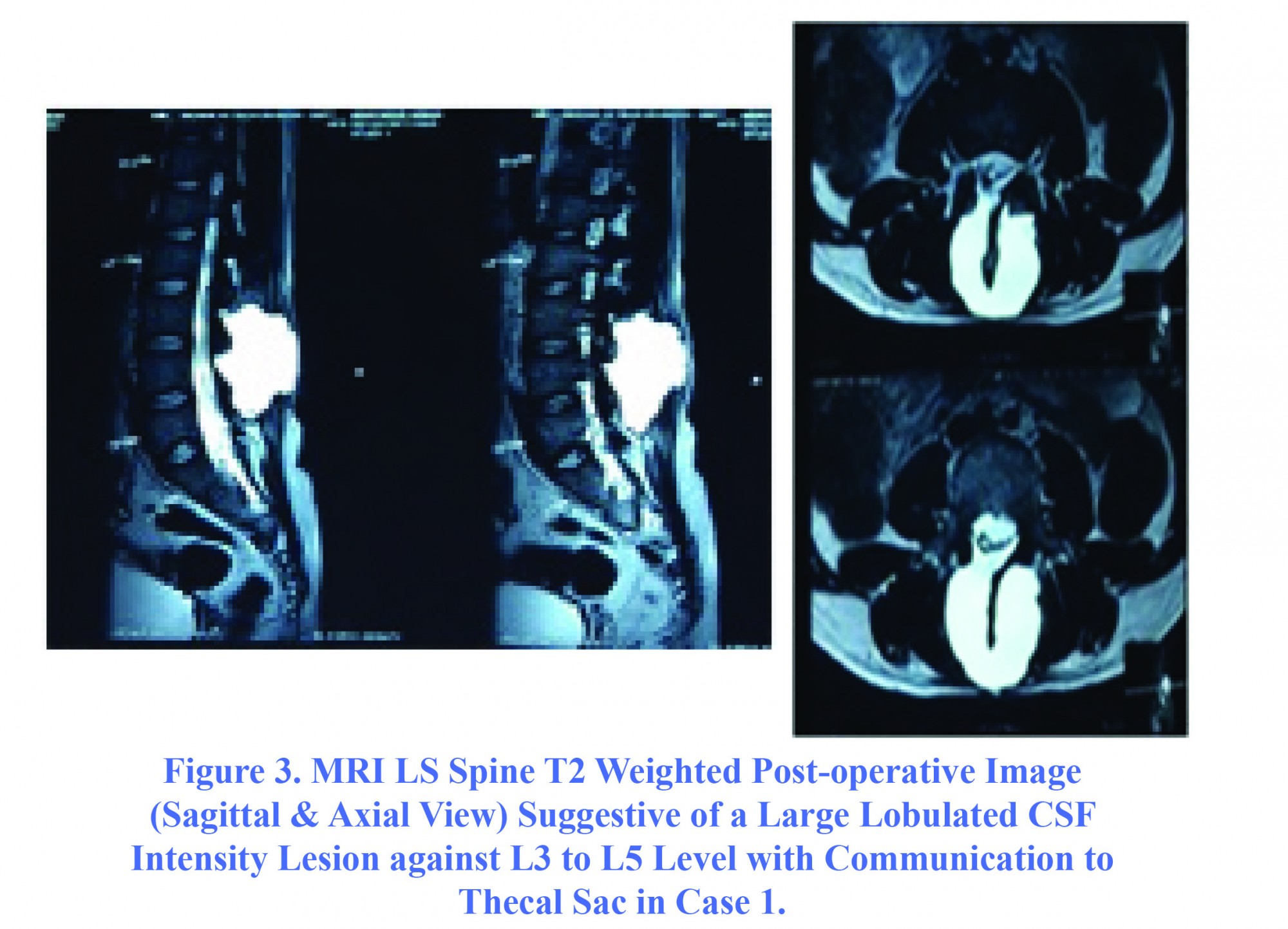
Repeated MRI scan revealed the presence of a 8.1×6.1×5.6 cm lobulated CSF intensity collection overlying the laminotomy defect opposite L4 vertebral body (Figure 3). The collection was extending craniocaudally from L3 to L5 level and anteroposteriorly from subcutaneous plane to dorsal aspect of thecal sac. The patient was diagnosed as a case of giant lumbar pseudomeningocele. He was initially managed with a lumbar drain for four days. The swelling subsided on lumbar drain insertion and reappeared on closing the drain.
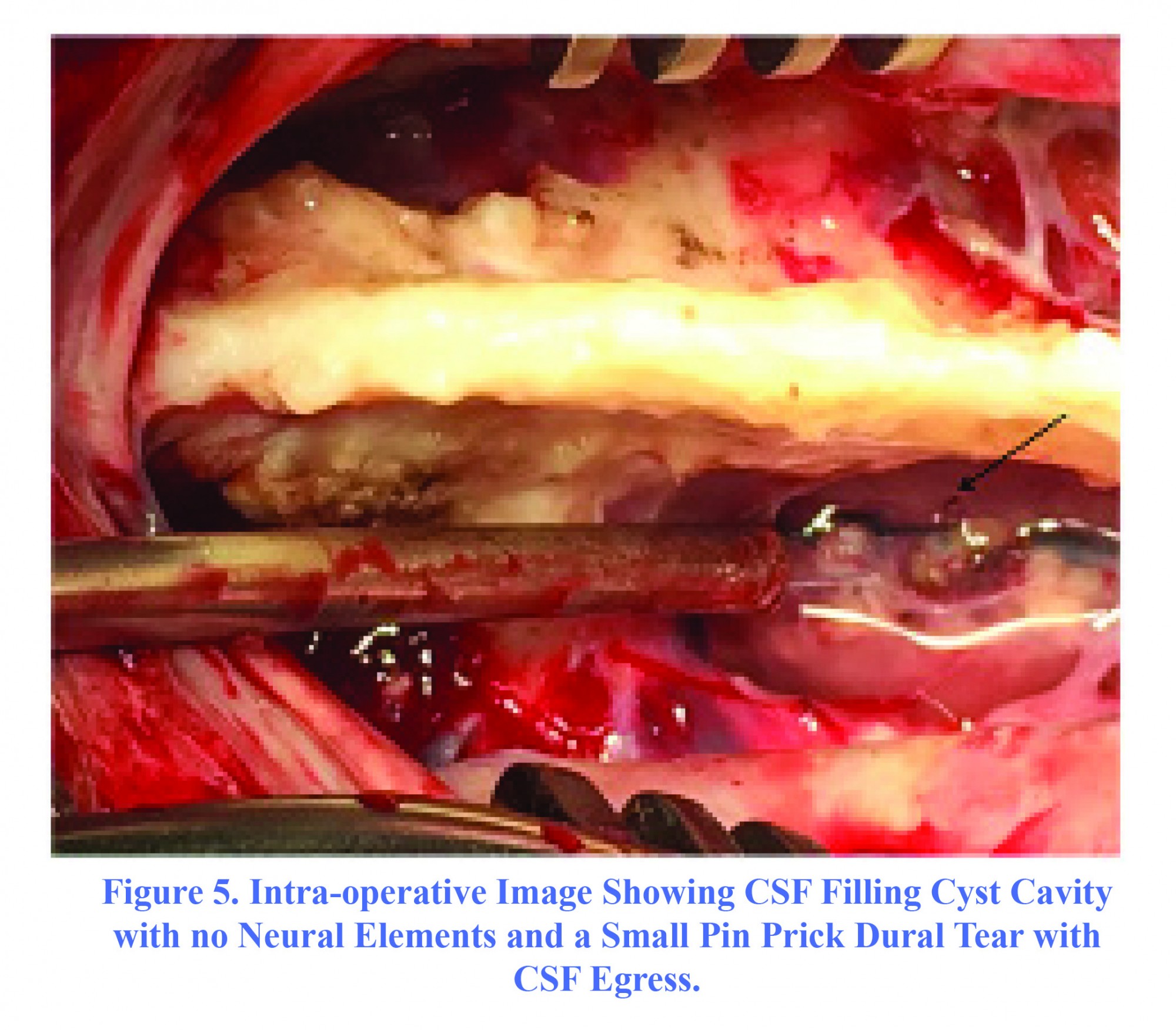
In view of established communication between the dura and subcutaneous tissue plane, surgical exploration was done. Tiny dural tear was seen medial to site of previous dural repair with egress of CSF (Figure 4). Extirpation of pseudomeningocele sac was done. Dura was repaired with silk 4-0 and reinforced with fat graft and fibrin glue. The patient had an uneventful post-operative stay and was discharged on the 10th post- operative day. He is on regular follow up and has no recurrence of any swelling or pain. Post-operative MRI showed substantial reduction in size of CSF collection with no communication with thecal sac (Figure 5).
CASE 2
A 50-year-old female patient with complaints of swelling over lower back and recurrence of radicular pain in both lower limbs referred to neurosurgery department. The patient had a history of having undergone a laminectomy and discectomy for L4-L5 and L5-S1 prolapsed in intervertebral disc three years ago at another institution. There was no associated lower limb weakness, bowel or bladder dysfunction noted on present clinical examination. The patient had a fluctuating swelling over the previous operative site. Previous MRI scans revealed progressively increasing cystic collection in lumbar paraspinous area. An MRI scan was performed on the present admission, which showed an extradural CSF intensity cystic collection in the lumbar paraspinous area (Figure 6). The cyst cavity was connected with the subarachnoid space, and was diagnosed as a post-operative lumbar pseudomeningocele. On re-exploration, a three mm dural rent was visualized intraoperatively with egress of CSF. Extirpation of the pseudomeningocele sac was done. Dural rent was repaired with a silk 4-0 suture and reinforced with a fascia patch. The patient had gradual improvement in her symptoms in the post-operative period. A post-operative MRI showed resolution of the lobulated CSF intensity lesion (Figure 7). The patient had no recurrence of similar symptoms for the past 12 months of follow-up.
A 50-year-old female patient with complaints of swelling over lower back and recurrence of radicular pain in both lower limbs referred to neurosurgery department. The patient had a history of having undergone a laminectomy and discectomy for L4-L5 and L5-S1 prolapsed in intervertebral disc three years ago at another institution. There was no associated lower limb weakness, bowel or bladder dysfunction noted on present clinical examination. The patient had a fluctuating swelling over the previous operative site. Previous MRI scans revealed progressively increasing cystic collection in lumbar paraspinous area. An MRI scan was performed on the present admission, which showed an extradural CSF intensity cystic collection in the lumbar paraspinous area (Figure 6). The cyst cavity was connected with the subarachnoid space, and was diagnosed as a post-operative lumbar pseudomeningocele. On re-exploration, a three mm dural rent was visualized intraoperatively with egress of CSF. Extirpation of the pseudomeningocele sac was done. Dural rent was repaired with a silk 4-0 suture and reinforced with a fascia patch. The patient had gradual improvement in her symptoms in the post-operative period. A post-operative MRI showed resolution of the lobulated CSF intensity lesion (Figure 7). The patient had no recurrence of similar symptoms for the past 12 months of follow-up.
Discussion
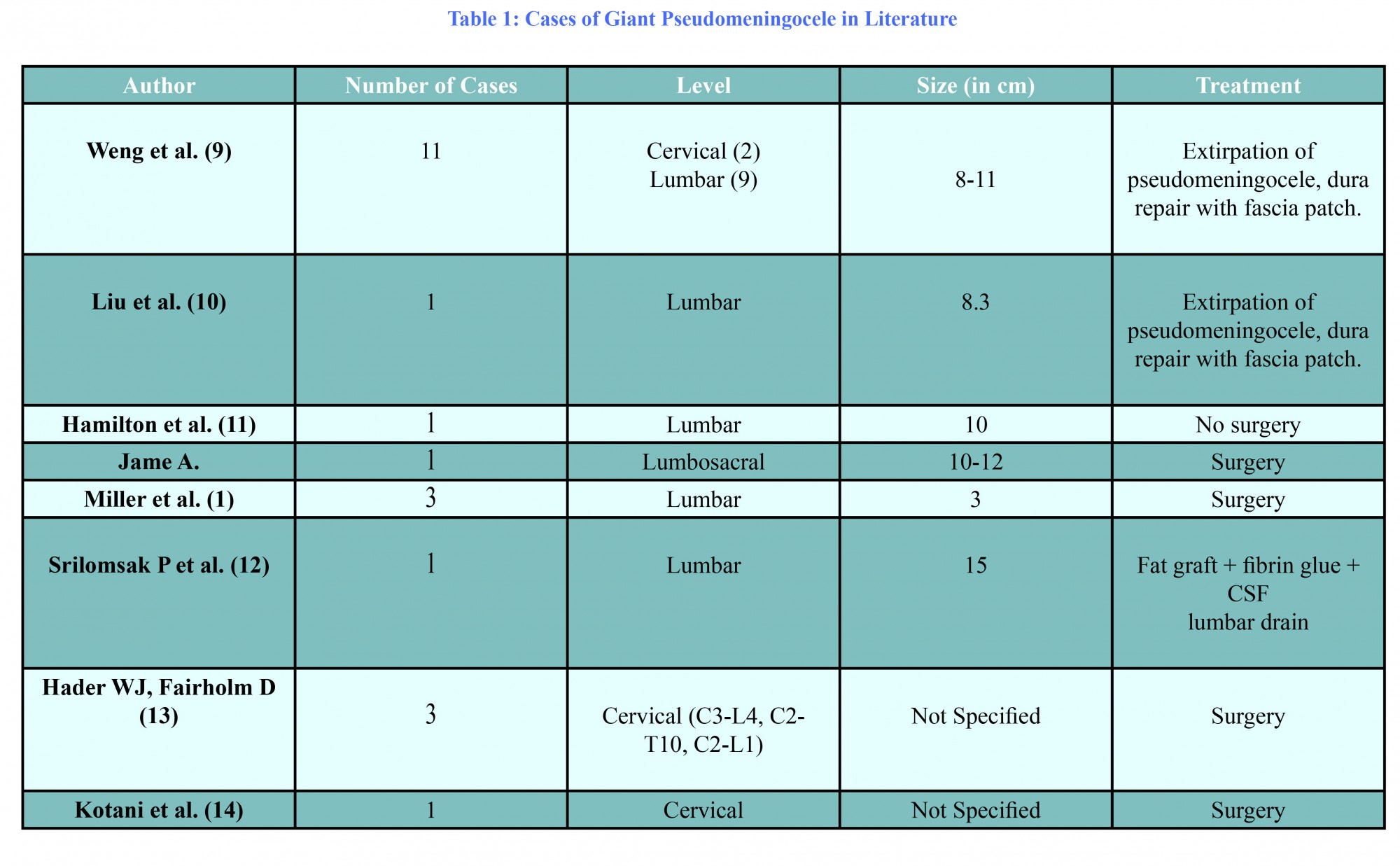
Pseudomeningocele is a rare complication of an unintended durotomy during spinal surgery. Three types of pseudomeningoceles have been reported in literature; congenital, postoperative and traumatic (2). The post-laminectomy pseudomeningocele was first described by Hyndman and Gerber in 1946 (3). The incidence of post operative pseudomeningocele in lumbar laminectomy patients varies from 0.07% to 2% according to studies by Swanson (4) and Teplick (5), respectively. Approximately 61 cases of post laminectomy pseudomeningoceles have been reported so far in literature since the first case was reported in 1946 (6).
If the tear is limited to the dural layer with an intact arachnoid layer, the cerebrospinal fluid collects in the extradural space. The cerebrospinal fluid accumulation is subject to a ball valve phenomenon, and results in formation of an extradural cyst. Tear of both the dural and arachnoid layers results in extravasation of cerebrospinal fluid in the paraspinal tissue. The cerebrospinal fluid is absorbed easily initially, but as the reactive fibrous septations are formed the reabsorption is hindered. The reactionary process results in formation of a fibrous capsule forming, in turn, the pseudocyst wall. The extravasation of cerebrospinal fluid may also result in herniation of nerve roots in the cyst cavity.
Pseudomeningocele causes signs and symptoms due to mass effect exerted over neural structures. A pseudomeningocele usually presents with low back pain which is exacerbated on sneezing and coughing. Patients may also present with radicular symptoms in event of herniation of nerve roots in the cyst cavity. Rarely motor deficits and sphincter dysfunction may be seen in patients. Delayed infection of pseudomeningocele was reported by Koo et al.(7) in 1986 and James et al.(8) in 1996.
The interval between primary surgery and the formation of a pseudomeningocele usually ranges from a few months to years. The size of the pseudomeningocele depends on the size of the dural tear and also on the level of incidental durotomy. The lumbar spine has a higher intraspinal pressure in erect posture, and hence there is a greater incidence of pseudomeningocele formation noted at this level.
Giant pseudomeningocele is a pathology where the size of the lesion is ≥ 8 cm in diameter (9). It is a very rare entity and only 22 cases have been reported in literature so far (10-14). MRI is the gold standard for diagnosis of a pseudomeningocele. A pseudomeningocele appears as a hypointense lesion on T1 weighted sequences, and hyperintense lesion on T2 weighted sequences.
The treatment modalities are varied, the small asymptomatic pseudomeningoceles are monitored periodically and are managed conservatively (3), whereas the symptomatic, large pseudomeningocele are managed with surgery. Extirpation of pseudomeningocele sac with repair of incidental durotomy and post-operative subarachnoid drain remains the standard treatment. If nerve roots are present within the cyst, they need to be repositioned inside dural cavity. Some patients are seen to benefit from a trial of lumbar drain prior to open surgery. Aoki (15) reported the treatment of ten patients with post-operative pseudomeningoceles with lumbar drains.
Pseudomeningocele is a rare complication of an unintended durotomy during spinal surgery. Three types of pseudomeningoceles have been reported in literature; congenital, postoperative and traumatic (2). The post-laminectomy pseudomeningocele was first described by Hyndman and Gerber in 1946 (3). The incidence of post operative pseudomeningocele in lumbar laminectomy patients varies from 0.07% to 2% according to studies by Swanson (4) and Teplick (5), respectively. Approximately 61 cases of post laminectomy pseudomeningoceles have been reported so far in literature since the first case was reported in 1946 (6).
If the tear is limited to the dural layer with an intact arachnoid layer, the cerebrospinal fluid collects in the extradural space. The cerebrospinal fluid accumulation is subject to a ball valve phenomenon, and results in formation of an extradural cyst. Tear of both the dural and arachnoid layers results in extravasation of cerebrospinal fluid in the paraspinal tissue. The cerebrospinal fluid is absorbed easily initially, but as the reactive fibrous septations are formed the reabsorption is hindered. The reactionary process results in formation of a fibrous capsule forming, in turn, the pseudocyst wall. The extravasation of cerebrospinal fluid may also result in herniation of nerve roots in the cyst cavity.
Pseudomeningocele causes signs and symptoms due to mass effect exerted over neural structures. A pseudomeningocele usually presents with low back pain which is exacerbated on sneezing and coughing. Patients may also present with radicular symptoms in event of herniation of nerve roots in the cyst cavity. Rarely motor deficits and sphincter dysfunction may be seen in patients. Delayed infection of pseudomeningocele was reported by Koo et al.(7) in 1986 and James et al.(8) in 1996.
The interval between primary surgery and the formation of a pseudomeningocele usually ranges from a few months to years. The size of the pseudomeningocele depends on the size of the dural tear and also on the level of incidental durotomy. The lumbar spine has a higher intraspinal pressure in erect posture, and hence there is a greater incidence of pseudomeningocele formation noted at this level.
Giant pseudomeningocele is a pathology where the size of the lesion is ≥ 8 cm in diameter (9). It is a very rare entity and only 22 cases have been reported in literature so far (10-14). MRI is the gold standard for diagnosis of a pseudomeningocele. A pseudomeningocele appears as a hypointense lesion on T1 weighted sequences, and hyperintense lesion on T2 weighted sequences.
The treatment modalities are varied, the small asymptomatic pseudomeningoceles are monitored periodically and are managed conservatively (3), whereas the symptomatic, large pseudomeningocele are managed with surgery. Extirpation of pseudomeningocele sac with repair of incidental durotomy and post-operative subarachnoid drain remains the standard treatment. If nerve roots are present within the cyst, they need to be repositioned inside dural cavity. Some patients are seen to benefit from a trial of lumbar drain prior to open surgery. Aoki (15) reported the treatment of ten patients with post-operative pseudomeningoceles with lumbar drains.
Conclusion
The reappearance of neurological symptoms in a previously operated patient of spine surgery needs careful evaluation. An accidental durotomy needs careful repair as it may lead to formation of a pseudomeningocele. An MRI scan is the investigation of choice in diagnosis of a pseudomeningocele. Surgery is advised in all symptomatic patients to prevent neurological deterioration.
The reappearance of neurological symptoms in a previously operated patient of spine surgery needs careful evaluation. An accidental durotomy needs careful repair as it may lead to formation of a pseudomeningocele. An MRI scan is the investigation of choice in diagnosis of a pseudomeningocele. Surgery is advised in all symptomatic patients to prevent neurological deterioration.
Funding
None.
None.
References
- Lee KS, Hardy IM. Post laminectomy lumbar pseudomeningocele: report of four cases.Neurosurgery. 1992;30:111-114.
- Miller PR, Elder FW Jr. Meningeal pseudocysts (meningocele spurius) following laminectomy. Report of ten cases. J Bone Joint Surg Am. 1968;50:268-276.
- Hyndman OR, Gerber WF. Spinal extradural cysts, congenital and acquired: report of cases. Journal of Neurosurgery. 1946;3(6):474-86.
- Swanson HS, Fincher EF. Extradural arachnoidal cysts of traumatic origin. Journal of Neurosurgery. 1947;4(6):530-8.
- Teplick JG, Peyster RG, Teplick SK, Goodman LR, Haskin ME. CT identification of postlaminectomy pseudomeningocele. American Journal of Neuroradiology. 1983;4(2):179-82.
- Rahimizadeh A et al. Post laminectomy lumbar pseudomeningocele: Report of three cases and review of the literature. WScJ. 2013;4:103-108.
- Koo J, Adamson R, Wagner FC, Hrdy DB. A new cause of chronic meningitis: infected lumbar pseudomeningocele. The American Journal of Medicine. 1989;86(1):103-4.
- Dastur HM. The radiological appearances of spinal extradural arachnoid cysts. Journal of Neurology, Neurosurgery & Psychiatry. 1963;26(3):231-5.
- Weng YJ, Cheng CC, Li YY, Huang TJ, Hsu RW. Management of giant pseudomeningoceles after spinal surgery. BMC Musculoskeletal Disorders. 2010;11(1):1.
- Liu C, Cai HX, Fan SW, Liu YJ. Postoperative pseudomeningocele in a 40-year-old man. Irish Journal of Medical Science. 2011;180(4):925-7.
- Hamilton RG, Brown SW, Goetz LL, Miner M. Lumbar pseudomeningocele causing hydronephrosis. The journal of Spinal Cord Medicine. 2009;32(1):95.
- Srilomsak P, Okuno K, Sakakibara T, Wang Z, Kasai Y. Giant pseudomeningocele after spinal surgery: A case report. World Journal of Orthopedics. 2012;3(7):109.
- Hader WJ, Fairholm D. Giant intraspinal pseudomeningoceles cause delayed neurological dysfunction after brachial plexus injury: report of three cases. Neurosurgery. 2000;46(5):1245-9.
- Kotani Y, Abumi K, Ito M, Terae S, Hisada Y, Minami A. Neurological recovery after surgical treatment of giant cervical pseudomeningoceles extending to lumbar spine associated with previous brachial plexus injury. European Spine Journal. 2010;19(2):206-10.
- Aoki N. Lumboperitoneal shunt for the treatment of postoperative persistent collection of subcutaneous cerebrospinal fluid (pseudomeningocoele). Acta Neurochirurgica. 1989;98(1-2):32-4.
Type of Study: Case report |
Subject:
Gamma Knife Radiosurgery
References
1. Lee KS, Hardy IM. Post laminectomy lumbar pseudomeningocele: report of four cases.Neurosurgery. 1992;30:111-114. [DOI:10.1227/00006123-199201000-00020]
2. Miller PR, Elder FW Jr. Meningeal pseudocysts (meningocele spurius) following laminectomy. Report of ten cases. J Bone Joint Surg Am. 1968;50:268-276. [DOI:10.2106/00004623-196850020-00005] [PMID]
3. Hyndman OR, Gerber WF. Spinal extradural cysts, congenital and acquired: report of cases. Journal of Neurosurgery. 1946;3(6):474-86. [DOI:10.3171/jns.1946.3.6.0474] [PMID]
4. Swanson HS, Fincher EF. Extradural arachnoidal cysts of traumatic origin. Journal of Neurosurgery. 1947;4(6):530-8. [DOI:10.3171/jns.1947.4.6.0530] [PMID]
5. Teplick JG, Peyster RG, Teplick SK, Goodman LR, Haskin ME. CT identification of postlaminectomy pseudomeningocele. American Journal of Neuroradiology. 1983;4(2):179-82.
6. Rahimizadeh A et al. Post laminectomy lumbar pseudomeningocele: Report of three cases and review of the literature. WScJ. 2013;4:103-108.
7. Koo J, Adamson R, Wagner FC, Hrdy DB. A new cause of chronic meningitis: infected lumbar pseudomeningocele. The American Journal of Medicine. 1989;86(1):103-4. [DOI:10.1016/0002-9343(89)90238-6]
8. Dastur HM. The radiological appearances of spinal extradural arachnoid cysts. Journal of Neurology, Neurosurgery & Psychiatry. 1963;26(3):231-5. [DOI:10.1136/jnnp.26.3.231]
9. Weng YJ, Cheng CC, Li YY, Huang TJ, Hsu RW. Management of giant pseudomeningoceles after spinal surgery. BMC Musculoskeletal Disorders. 2010;11(1):1. [DOI:10.1186/1471-2474-11-53] [PMID] [PMCID]
10. Liu C, Cai HX, Fan SW, Liu YJ. Postoperative pseudomeningocele in a 40-year-old man. Irish Journal of Medical Science. 2011;180(4):925-7. [DOI:10.1007/s11845-010-0598-8] [PMID]
11. Hamilton RG, Brown SW, Goetz LL, Miner M. Lumbar pseudomeningocele causing hydronephrosis. The journal of Spinal Cord Medicine. 2009;32(1):95. [DOI:10.1080/10790268.2009.11760758] [PMID] [PMCID]
12. Srilomsak P, Okuno K, Sakakibara T, Wang Z, Kasai Y. Giant pseudomeningocele after spinal surgery: A case report. World Journal of Orthopedics. 2012;3(7):109. [DOI:10.5312/wjo.v3.i7.109] [PMID] [PMCID]
13. Hader WJ, Fairholm D. Giant intraspinal pseudomeningoceles cause delayed neurological dysfunction after brachial plexus injury: report of three cases. Neurosurgery. 2000;46(5):1245-9. [DOI:10.1097/00006123-200005000-00044]
14. Kotani Y, Abumi K, Ito M, Terae S, Hisada Y, Minami A. Neurological recovery after surgical treatment of giant cervical pseudomeningoceles extending to lumbar spine associated with previous brachial plexus injury. European Spine Journal. 2010;19(2):206-10. [DOI:10.1007/s00586-010-1387-9] [PMID] [PMCID]
15. Aoki N. Lumboperitoneal shunt for the treatment of postoperative persistent collection of subcutaneous cerebrospinal fluid (pseudomeningocoele). Acta Neurochirurgica. 1989;98(1-2):32-4. [DOI:10.1007/BF01407173]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |