Fri, Oct 24, 2025
Volume 9 - Continuous Publishing
Iran J Neurosurg 2023, 9 - Continuous Publishing: 107-112 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shafizad M, Sobhanian P, Ghadirzadeh E, Poormousa R, Godazandeh G. A Case Report of Early Surgical Intervention for Diffuse Idiopathic Skeletal Hyperostosis of the Cervical Spine: Challenges in Management. Iran J Neurosurg 2023; 9 : 14
URL: http://irjns.org/article-1-352-en.html
URL: http://irjns.org/article-1-352-en.html
Misagh Shafizad1 

 , Pooria Sobhanian *2
, Pooria Sobhanian *2 

 , Erfan Ghadirzadeh3
, Erfan Ghadirzadeh3 

 , Rostam Poormousa4
, Rostam Poormousa4 

 , Gholam-ali Godazandeh5
, Gholam-ali Godazandeh5 




 , Pooria Sobhanian *2
, Pooria Sobhanian *2 

 , Erfan Ghadirzadeh3
, Erfan Ghadirzadeh3 

 , Rostam Poormousa4
, Rostam Poormousa4 

 , Gholam-ali Godazandeh5
, Gholam-ali Godazandeh5 


1- Department of Neurosurgery, School of Medicine, Orthopedic Research Center, Mazandaran University of Medical Sciences, Sari, Iran
2- Student Research Committee, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran ,Drpooriasobhanian@outlook.com
3- Student Research Committee, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran
4- Department of Otolaryngology, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran
5- Department of Surgery, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran
2- Student Research Committee, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran ,
3- Student Research Committee, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran
4- Department of Otolaryngology, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran
5- Department of Surgery, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran
Full Text [PDF 1488 kb]
(806 Downloads)
| Abstract (HTML) (2772 Views)
Full Text: (1332 Views)
1. Introduction
Diffuse idiopathic skeletal hyperostosis (DISH, or Forestier’s disease) is characterized by bony hardening at sites of tendon and ligament insertion around the vertebral column [1]. Resnick and Niwayama’s diagnostic criteria for DISH include “four continuous levels of ossification, relative preservation of disc spaces, and the absence of apophyseal joint ankylosis, and sacroiliac sclerosis” [2].
DISH is typically asymptomatic and discovered incidentally on spine radiography [3]. However, cervical DISH can cause annoying symptoms for the patient related to airway or neural compression at the spine, such as dysphagia, dysphonia, paralysis of the vocal cords, dyspnea, snoring, or decreased range of motion [3-5]. Anterior cervical osteophyte resection is indicated in patients with airway obstruction and/or dysphagia in whom conservative treatment fails.
The following is a report of a rare case in which early surgical intervention in a patient with cervical DISH yielded favorable outcomes with minimal complications. Based on previously published research, we investigated whether it is preferable to perform the early surgical intervention in symptomatic patients, especially patients with secondary dysphagia, or to wait and administer supportive care and perform late surgical intervention regardless of whether symptoms progress.
2. Case Presentation
A 70-year-old man presented to our clinic complaining of neck pain, swallowing difficulties, and voice changes. According to his medical history, he had arterial hypertension and hypercholesterolemia. In addition, he had no other co-morbidities and his diabetes test was negative. He had experienced mild symptoms, such as dysphagia for several years. His dysphagia and hoarseness worsened in the last two months. In addition to experiencing painful swallowing, the patient had also lost a significant amount of weight over the past month. On physical examination, movements of the cervical spine, such as lateral bending and axial rotation, were painful, and the patient complained of muscle stiffness. No motor or sensory deficits were present, and deep tendon reflexes were normal.
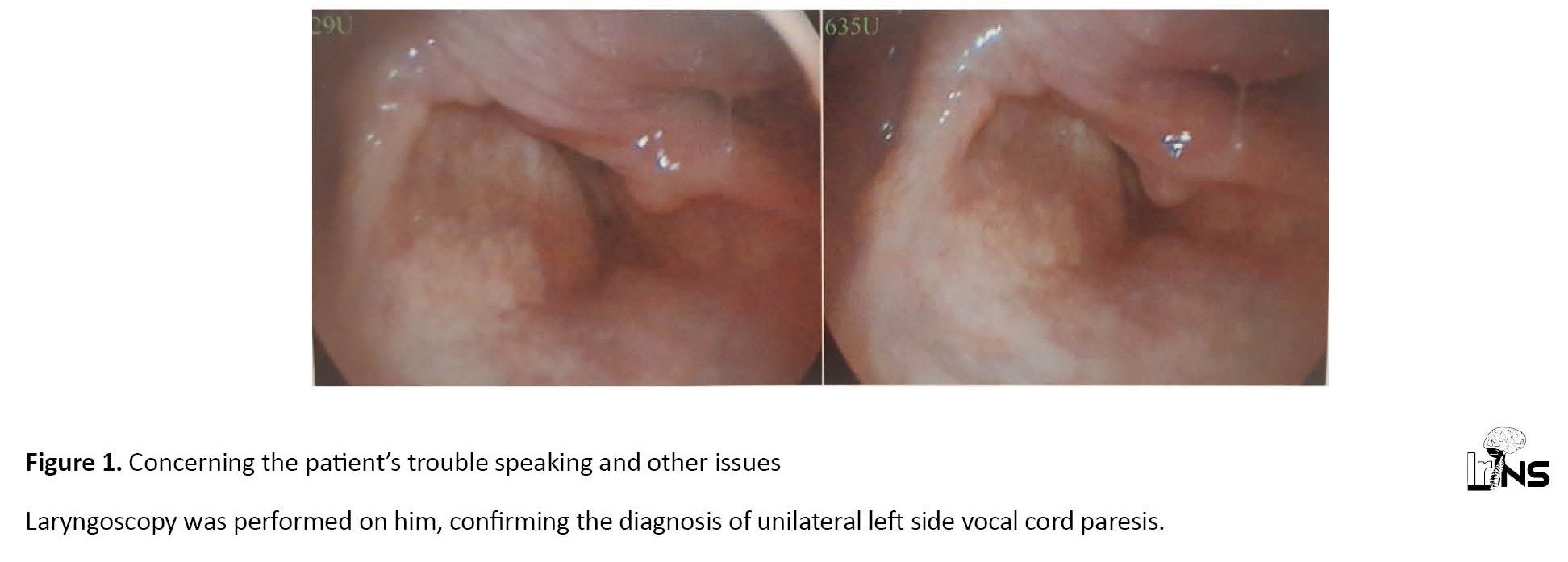
Concerning the patient’s trouble speaking and other issues, a laryngoscopy was performed on him, confirming the diagnosis of unilateral left-side vocal cord paresis (Figure 1). We obtained a computed tomography (CT) scan (Figure 2), radiographs, and magnetic resonance imaging (MRI) of the cervical spine (Figure 3). Normal bone density and the presence of new bone formation at C2-C3, and C4-C6 vertebrae with anterior fusion appeared on the lateral cervical X-ray (Figure 4). The cervical spine was scanned using T1 and T2 images in the sagittal and axial planes. The radiologist noted disc bulging with moderate compression effect on the central canal and neural foramina at different levels from C1 to C6; two enormous osteophytes, one measuring approximately 25.3 mm on C2-C4 and the other measuring approximately 10.3 mm on C5-C6, and a moderate to severe anterior compression effect on the pharynx region, consistent with a DISH diagnosis of disc dehydration and degenerative changes. However, no proof of cervical myelopathy was found. After consulting with a gastroenterologist to check the differential diagnoses of secondary dysphagia, the cervical DISH diagnosis topped the list of differential diagnoses. He was referred to the neurosurgery clinic for a surgical consultation and future care.
Surgery
The surgical technique was done using the Smith-Robinson approach. We used a generous horizontal mid-cervical skin incision. Platysma was split longitudinally. This allowed generous access from C3 down to C6. We were able to achieve satisfactory exposure through a horizontal incision. By elevating the longus colli, the lateral aspects of the osteophytes were exposed. No adhesions to the esophagus existed. To remove osteophytes, we used a high-speed drill. Standard suturing was used. The procedure was performed by a neurosurgeon with 10 years of experience in spine surgery. The day after the operation, the patient reported a significant improvement in swallowing and a reduction in local pain in the cervical spine area.
Quality of life (QoL)
We followed up the patient at intervals of 2, 6, and 12 months after surgery. A lateral cervical radiograph was performed for the patient, which showed no evidence of regrowth. The neurological examination was normal, and the patient’s dysphagia and sleep quality had also improved significantly. According to him, he had gained a little extra weight, he was happier and did not wake up with shortness of breath. He is now more satisfied with his life. The patient reported a significant improvement in swallowing, breathing, and cervical spine range of motion.
3. Discussion
Clinical manifestations of DISH may include musculoskeletal symptoms, such as neck and back pain, cervical involvement symptoms like dysphagia, hoarseness, sleep apnea, and neurological defects due to ossification of the posterior longitudinal ligament (OPLL) [6]. Mechanical factors, some dietary factors, such as retinol and its medical derivatives, high levels of osteocalcin, and lower levels of dickkopf-1 (DKK1) are suspected to be involved in the development of DISH. Spondylosis deformans, ankylosing spondylitis, and OPLL are conditions that present similarly to DISH and should be carefully evaluated [7].
The incidence of dysphagia in DISH patients ranges from 0.2% to 28.2%. DISH occurs between 2% and 4% of the time in patients older than 40 years, and this rate reaches 28% in patients older than 80 years old [8]. When mild symptoms, such as mild pain, stiffness, and decreased range of motion are present, DISH can be managed pharmacologically with non-steroidal anti-inflammatory drugs (NSAIDs) and local glucocorticoid injections, and conservatively with physical therapy [9]. Certain conditions necessitate a surgical consultation to determine if an intervention is appropriate [10, 11, 12, 13]. These conditions include dysphagia resulting from cervical osteophytes and spurs, OPLL, and neurological defects resulting from nerve root compression or thoracic outlet syndrome [10-12, 14].
According to previously published studies, this study was conducted to determine whether or not early surgical intervention in symptomatic patients, particularly in patients with secondary dysphagia, yields better clinical outcomes than late surgical intervention when symptoms have progressed to OPLL or thoracic outlet syndrome (TOS) or become more severe. Julian L. Genreau et al. [8] conducted a systematic review and meta-analysis of 22 papers reporting 119 DISH patients with dysphagia. Most papers included case reports or case series. According to their findings, after surgery, 89% of patients were relieved of their symptoms. In the remaining 11% of patients, failure to alleviate dysphagia after the surgical intervention was associated with a longer duration of preoperative symptoms (P<0.01) and increased severity of preoperative symptoms (RR=2.86, 95% CI: 1.19-6.09, P=0.02). Their findings were consistent with those of Kei Miyamoto et al. [12], who investigated the recurrence of osteophytes in seven DISH patients with dysphagia. In their study, patients with more severe symptoms and a longer postoperative period did not experience relief. They also concluded that as symptoms progress, the likelihood of osteophyte recurrence after surgery increases. Therefore, it is preferable to monitor patients for at least 10 years after surgery.
Additionally, Francesco Mattioli et al. [9] examined 41 DISH patients who underwent surgical intervention. In their study, patients with more severe and advanced dysphagia did not benefit as much from the intervention as patients with milder symptoms. They concluded that early surgical intervention has a higher success rate and therefore benefits patients.
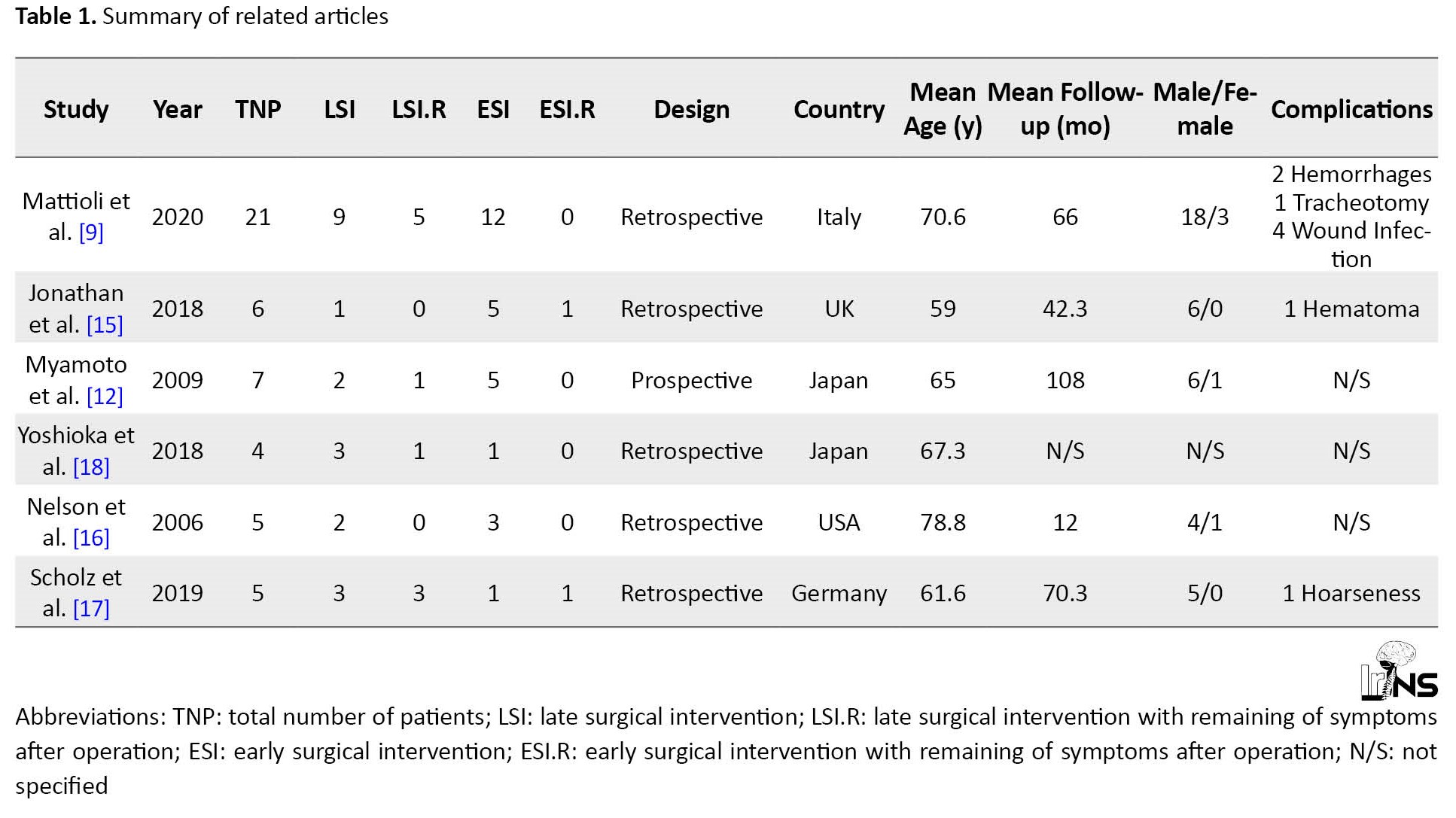
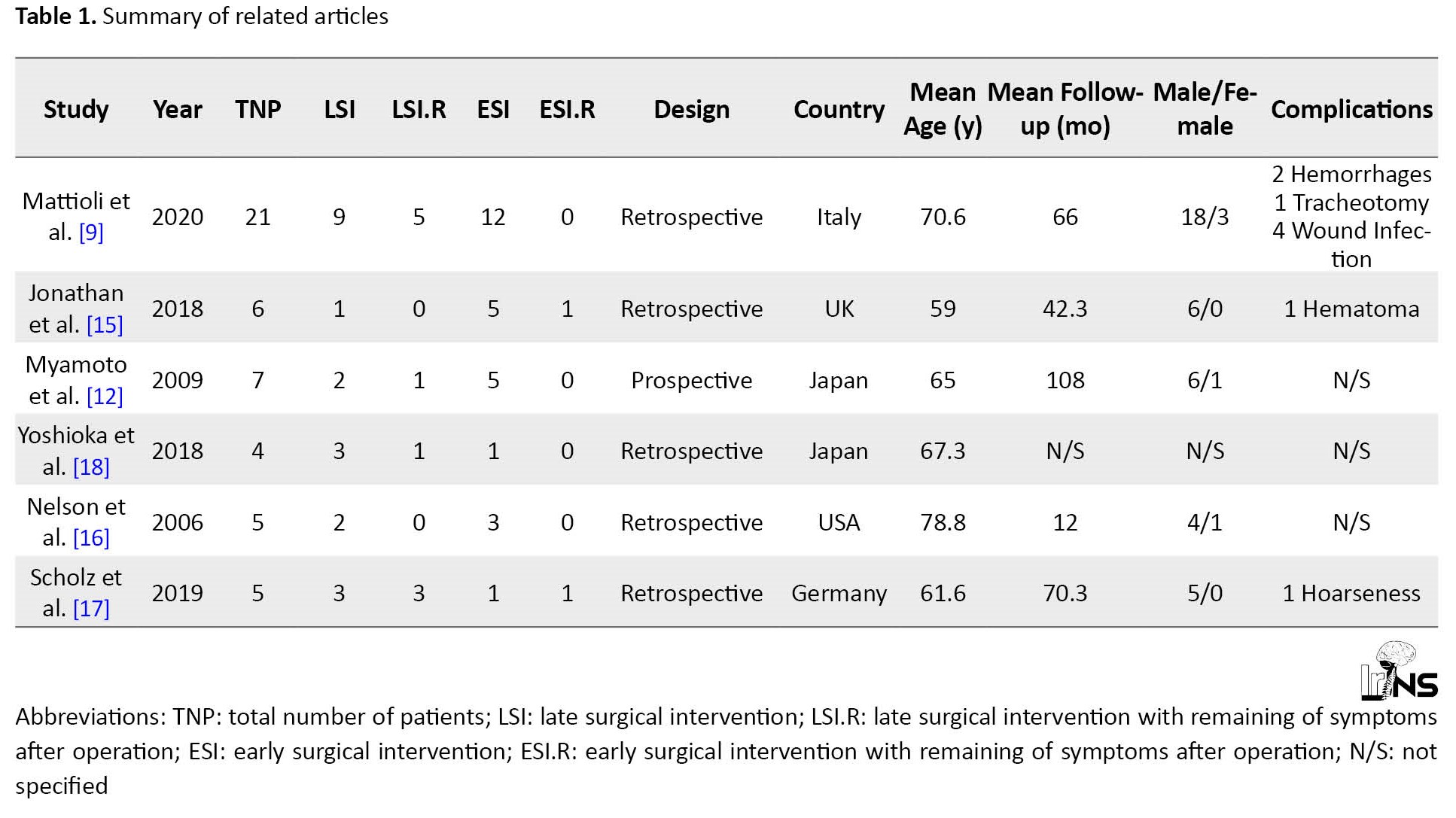
As described in Table 1, patients who were symptomatic for longer before surgical intervention also experienced more post-operative complications.
Since the resection of osteophytes is a simpler surgical intervention, it seems that surgical intervention in the early stage of cervical DISH and before the appearance of neurological deficits or respiratory symptoms can be associated with a lower rate of post-operative complications [9, 12, 15, 16, 17, 18].
4. Conclusion
According to our experience and a review of the relevant literature, to achieve a higher success rate and less recurrence, it is preferable to perform surgical intervention earlier in the disease’s progression. But more studies are necessary to confirm this as most of the present results are from case reports and have a lower level of evidence.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from the patient before the operation and for the rest of the procedure.
Funding
This research did not receive any financial support from funding agencies in governmental, commercial, or non-profit institutions.
Authors' contributions
Conception and design: Misagh Shafizad, Rostam Poormousa; Data Analysis and interpretation: Misagh Shafizad, Pooria Sobhanian; Drafting the article: Pooria Sobhanian, Erfan Ghadirzadeh; Critically revising the article: Pooria Sobhanian, Erfan Ghadirzadeh; Reviewing submitted version of manuscript: Rostam Poormousa, Gholam-ali Godazandeh; Approving the final version of the manuscript: Misagh Shafizad, Gholam-ali Godazandeh.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
None.
References
Diffuse idiopathic skeletal hyperostosis (DISH, or Forestier’s disease) is characterized by bony hardening at sites of tendon and ligament insertion around the vertebral column [1]. Resnick and Niwayama’s diagnostic criteria for DISH include “four continuous levels of ossification, relative preservation of disc spaces, and the absence of apophyseal joint ankylosis, and sacroiliac sclerosis” [2].
DISH is typically asymptomatic and discovered incidentally on spine radiography [3]. However, cervical DISH can cause annoying symptoms for the patient related to airway or neural compression at the spine, such as dysphagia, dysphonia, paralysis of the vocal cords, dyspnea, snoring, or decreased range of motion [3-5]. Anterior cervical osteophyte resection is indicated in patients with airway obstruction and/or dysphagia in whom conservative treatment fails.
The following is a report of a rare case in which early surgical intervention in a patient with cervical DISH yielded favorable outcomes with minimal complications. Based on previously published research, we investigated whether it is preferable to perform the early surgical intervention in symptomatic patients, especially patients with secondary dysphagia, or to wait and administer supportive care and perform late surgical intervention regardless of whether symptoms progress.
2. Case Presentation
A 70-year-old man presented to our clinic complaining of neck pain, swallowing difficulties, and voice changes. According to his medical history, he had arterial hypertension and hypercholesterolemia. In addition, he had no other co-morbidities and his diabetes test was negative. He had experienced mild symptoms, such as dysphagia for several years. His dysphagia and hoarseness worsened in the last two months. In addition to experiencing painful swallowing, the patient had also lost a significant amount of weight over the past month. On physical examination, movements of the cervical spine, such as lateral bending and axial rotation, were painful, and the patient complained of muscle stiffness. No motor or sensory deficits were present, and deep tendon reflexes were normal.
Concerning the patient’s trouble speaking and other issues, a laryngoscopy was performed on him, confirming the diagnosis of unilateral left-side vocal cord paresis (Figure 1). We obtained a computed tomography (CT) scan (Figure 2), radiographs, and magnetic resonance imaging (MRI) of the cervical spine (Figure 3). Normal bone density and the presence of new bone formation at C2-C3, and C4-C6 vertebrae with anterior fusion appeared on the lateral cervical X-ray (Figure 4). The cervical spine was scanned using T1 and T2 images in the sagittal and axial planes. The radiologist noted disc bulging with moderate compression effect on the central canal and neural foramina at different levels from C1 to C6; two enormous osteophytes, one measuring approximately 25.3 mm on C2-C4 and the other measuring approximately 10.3 mm on C5-C6, and a moderate to severe anterior compression effect on the pharynx region, consistent with a DISH diagnosis of disc dehydration and degenerative changes. However, no proof of cervical myelopathy was found. After consulting with a gastroenterologist to check the differential diagnoses of secondary dysphagia, the cervical DISH diagnosis topped the list of differential diagnoses. He was referred to the neurosurgery clinic for a surgical consultation and future care.
Surgery
The surgical technique was done using the Smith-Robinson approach. We used a generous horizontal mid-cervical skin incision. Platysma was split longitudinally. This allowed generous access from C3 down to C6. We were able to achieve satisfactory exposure through a horizontal incision. By elevating the longus colli, the lateral aspects of the osteophytes were exposed. No adhesions to the esophagus existed. To remove osteophytes, we used a high-speed drill. Standard suturing was used. The procedure was performed by a neurosurgeon with 10 years of experience in spine surgery. The day after the operation, the patient reported a significant improvement in swallowing and a reduction in local pain in the cervical spine area.
Quality of life (QoL)
We followed up the patient at intervals of 2, 6, and 12 months after surgery. A lateral cervical radiograph was performed for the patient, which showed no evidence of regrowth. The neurological examination was normal, and the patient’s dysphagia and sleep quality had also improved significantly. According to him, he had gained a little extra weight, he was happier and did not wake up with shortness of breath. He is now more satisfied with his life. The patient reported a significant improvement in swallowing, breathing, and cervical spine range of motion.
3. Discussion
Clinical manifestations of DISH may include musculoskeletal symptoms, such as neck and back pain, cervical involvement symptoms like dysphagia, hoarseness, sleep apnea, and neurological defects due to ossification of the posterior longitudinal ligament (OPLL) [6]. Mechanical factors, some dietary factors, such as retinol and its medical derivatives, high levels of osteocalcin, and lower levels of dickkopf-1 (DKK1) are suspected to be involved in the development of DISH. Spondylosis deformans, ankylosing spondylitis, and OPLL are conditions that present similarly to DISH and should be carefully evaluated [7].
The incidence of dysphagia in DISH patients ranges from 0.2% to 28.2%. DISH occurs between 2% and 4% of the time in patients older than 40 years, and this rate reaches 28% in patients older than 80 years old [8]. When mild symptoms, such as mild pain, stiffness, and decreased range of motion are present, DISH can be managed pharmacologically with non-steroidal anti-inflammatory drugs (NSAIDs) and local glucocorticoid injections, and conservatively with physical therapy [9]. Certain conditions necessitate a surgical consultation to determine if an intervention is appropriate [10, 11, 12, 13]. These conditions include dysphagia resulting from cervical osteophytes and spurs, OPLL, and neurological defects resulting from nerve root compression or thoracic outlet syndrome [10-12, 14].
According to previously published studies, this study was conducted to determine whether or not early surgical intervention in symptomatic patients, particularly in patients with secondary dysphagia, yields better clinical outcomes than late surgical intervention when symptoms have progressed to OPLL or thoracic outlet syndrome (TOS) or become more severe. Julian L. Genreau et al. [8] conducted a systematic review and meta-analysis of 22 papers reporting 119 DISH patients with dysphagia. Most papers included case reports or case series. According to their findings, after surgery, 89% of patients were relieved of their symptoms. In the remaining 11% of patients, failure to alleviate dysphagia after the surgical intervention was associated with a longer duration of preoperative symptoms (P<0.01) and increased severity of preoperative symptoms (RR=2.86, 95% CI: 1.19-6.09, P=0.02). Their findings were consistent with those of Kei Miyamoto et al. [12], who investigated the recurrence of osteophytes in seven DISH patients with dysphagia. In their study, patients with more severe symptoms and a longer postoperative period did not experience relief. They also concluded that as symptoms progress, the likelihood of osteophyte recurrence after surgery increases. Therefore, it is preferable to monitor patients for at least 10 years after surgery.
Additionally, Francesco Mattioli et al. [9] examined 41 DISH patients who underwent surgical intervention. In their study, patients with more severe and advanced dysphagia did not benefit as much from the intervention as patients with milder symptoms. They concluded that early surgical intervention has a higher success rate and therefore benefits patients.
As described in Table 1, patients who were symptomatic for longer before surgical intervention also experienced more post-operative complications.
Since the resection of osteophytes is a simpler surgical intervention, it seems that surgical intervention in the early stage of cervical DISH and before the appearance of neurological deficits or respiratory symptoms can be associated with a lower rate of post-operative complications [9, 12, 15, 16, 17, 18].
4. Conclusion
According to our experience and a review of the relevant literature, to achieve a higher success rate and less recurrence, it is preferable to perform surgical intervention earlier in the disease’s progression. But more studies are necessary to confirm this as most of the present results are from case reports and have a lower level of evidence.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from the patient before the operation and for the rest of the procedure.
Funding
This research did not receive any financial support from funding agencies in governmental, commercial, or non-profit institutions.
Authors' contributions
Conception and design: Misagh Shafizad, Rostam Poormousa; Data Analysis and interpretation: Misagh Shafizad, Pooria Sobhanian; Drafting the article: Pooria Sobhanian, Erfan Ghadirzadeh; Critically revising the article: Pooria Sobhanian, Erfan Ghadirzadeh; Reviewing submitted version of manuscript: Rostam Poormousa, Gholam-ali Godazandeh; Approving the final version of the manuscript: Misagh Shafizad, Gholam-ali Godazandeh.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
None.
References
- Anshori F, Hutami WD, Tobing SDAL. Diffuse idiopathic skeletal hyperostosis (DISH) with ossification of the posterior longitudinal ligament (OPLL) in the cervical spine without neurological deficit-A Case report. Annals of Medicine and Surgery. 2020; 60:451-5. [DOI:10.1016/j.amsu.2020.11.028] [PMID] [PMCID]
- Certo F, Sciacca G, Caltabiano R, Albanese G, Borderi A, Albanese V, et al. Anterior, extracanalar, cervical spine osteochondroma associated with DISH: Description of a very rare tumor causing bilateral vocal cord paralysis, laryngeal compression and dysphagia. Case report and review of the literature. European Review for Medical and Pharmacological Sciences. 2014; 18(1 Suppl):34-40. [PMID]
- Dąbrowski M, Sulewski A, Kaczmarczyk J, Kubaszewski Ł. Surgical treatment of diffuse idiopathic skeletal hyperostosis of cervical spine with dysphagia - Case report. Annals of Medicine and Surgery (2012). 2020; 57:37-40. [DOI:10.1016/j.amsu.2020.07.009] [PMID] [PMCID]
- Forestier J, Lagier R. Ankylosing hyperostosis of the spine. Clinical Orthopaedics and Related Research. 1971; 74:65-83. [DOI:10.1097/00003086-197101000-00009] [PMID]
- Egerter AC, Kim ES, Lee DJ, Liu JJ, Cadena G, Panchal RR, et al. Dysphagia secondary to anterior osteophytes of the cervical spine. Global Spine Journal. 2015; 5(5):e78-83. [DOI:10.1055/s-0035-1546954] [PMID] [PMCID]
- Kolz JM, Alvi MA, Bhatti AR, Tomov MN, Bydon M, Sebastian AS, et al. Anterior cervical osteophyte resection for treatment of dysphagia. Global Spine Journal. 2021; 11(4):488-99. [DOI:10.1177/2192568220912706] [PMID] [PMCID]
- Mata S, Fortin PR, Fitzcharles MA, Starr MR, Joseph L, Watts CS, et al. A controlled study of diffuse idiopathic skeletal hyperostosis. Clinical features and functional status. Medicine. 1997; 76(2):104-17. [DOI:10.1097/00005792-199703000-00003] [PMID]
- Gendreau JL, Sheaffer K, Bennett J, Abraham M, Patel NV, Herschman Y, et al. Timing of surgical intervention for dysphagia in patients with diffuse idiopathic skeletal hyperostosis: A systematic review and meta-analysis. Clinical Spine Surgery. 2021; 34(6):220-7. [DOI:10.1097/BSD.0000000000001105] [PMID]
- Mattioli F, Ghirelli M, Trebbi M, Silvestri M, Presutti L, Fermi M. Improvement of swallowing function after surgical treatment of diffuse idiopathic skeletal hyperostosis: Our experience. World Neurosurgery. 2020; 134:e29-36. [DOI:10.1016/j.wneu.2019.08.124] [PMID]
- Resnick D, Niwayama G. Radiographic and pathologic features of spinal involvement in diffuse idiopathic skeletal hyperostosis (DISH). Radiology. 1976; 119(3):559-68. [DOI:10.1148/119.3.559] [PMID]
- Trojan DA, Pouchot J, Pokrupa R, Ford RM, Adamsbaum C, Hill RO, et al. Diagnosis and treatment of ossification of the posterior longitudinal ligament of the spine: Report of eight cases and literature review. The American Journal of Medicine. 1992; 92(3):296-306. [DOI:10.1016/0002-9343(92)90080-U] [PMID]
- Miyamoto K, Sugiyama S, Hosoe H, Iinuma N, Suzuki Y, Shimizu K. Postsurgical recurrence of osteophytes causing dysphagia in patients with diffuse idiopathic skeletal hyperostosis. European Spine Journal. 2009; 18(11):1652-8. [DOI:10.1007/s00586-009-1133-3] [PMID] [PMCID]
- Mader R, Verlaan JJ, Eshed I, Bruges-Armas J, Puttini PS, Atzeni F, et al. Diffuse idiopathic skeletal hyperostosis (DISH): Where we are now and where to go next. RMD Open. 2017; 3(1):e000472. [DOI:10.1136/rmdopen-2017-000472] [PMID] [PMCID]
- Utsinger PD. Diffuse idiopathic skeletal hyperostosis. Clinics in Rheumatic Diseases. 1985; 11(2):325-51. [DOI:10.1016/S0307-742X(21)00544-0] [PMID]
- Lui Jonathan YC, Sayal P, Prezerakos G, Russo V, Choi D, Casey ATH. The surgical management of dysphagia secondary to diffuse idiopathic skeletal hyperostosis. Clinical Neurology and Neurosurgery. 2018; 167:36-42. [DOI:10.1016/j.clineuro.2018.02.010] [PMID]
- Nelson RS, Urquhart AC, Faciszewski T. Diffuse idiopathic skeletal hyperostosis: A rare cause of dysphagia, airway obstruction, and dysphonia. Journal of the American College of Surgeons. 2006; 202(6):938-42. [DOI:10.1016/j.jamcollsurg.2006.02.030] [PMID]
- Scholz C, Naseri Y, Hohenhaus M, Hubbe U, Klingler JH. Long-term results after surgical treatment of diffuse idiopathic skeletal hyperostosis (DISH) causing dysphagia. Journal of Clinical Neuroscience. 2019; 67:151-5. [DOI:10.1016/j.jocn.2019.05.057] [PMID]
- Yoshioka K, Murakami H, Demura S, Kato S, Yonezawa N, Takahashi N, et al. Surgical treatment for cervical diffuse idiopathic skeletal hyperostosis as a cause of dysphagia. Spine Surgery and Related Research. 2018; 2(3):197-201. [DOI:10.22603/ssrr.2017-0045] [PMID] [PMCID]
Type of Study: Case report |
Subject:
Spine
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |