Sat, Dec 20, 2025
Volume 9 - Continuous Publishing
Iran J Neurosurg 2023, 9 - Continuous Publishing: 221-227 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Saiedi E, Mahmoud-Nejad S, Mohazzab-Torabi S, Ganjeifar B. Concurrent Neurological Involvement in Chronic Lymphocytic Leukemia: A Rare Case with Brain and Spinal Manifestations. Iran J Neurosurg 2023; 9 : 28
URL: http://irjns.org/article-1-357-en.html
URL: http://irjns.org/article-1-357-en.html
1- Department of Neurosurgery, Mashhad University of Medical Sciences, Iran
2- Department of Neurosurgery, Mashhad University of Medical Sciences, Iran ,smntrb@gmail.com
2- Department of Neurosurgery, Mashhad University of Medical Sciences, Iran ,
Full Text [PDF 1451 kb]
(1007 Downloads)
| Abstract (HTML) (2754 Views)
Full Text: (1882 Views)
1. Background and Importance
2. Case Presentation
Chronic lymphocytic leukemia (CLL) is a neoplastic proliferation of mature B-cells that primarily involves the blood and bone marrow. However, extramedullary involvement, including central nervous system (CNS) infiltration, can occur in up to 4%-5% of patients with CLL with various types of manifestation [1]. Patients with CLL may experience a range of neurological symptoms that can vary in severity from mild to severe. These symptoms include cognitive impairment, such as memory loss and difficulty concentrating, peripheral neuropathy which can cause tingling or numbness in extremities, cerebellar ataxia which impacts coordination and balance, depression, anxiety, fatigue, and sleep disturbances [2]. In this study, we describe a CLL case with rare CNS involvement and review up-to-date literature about this issue.
2. Case Presentation
A 71-year-old man with a headache and progressive lower extremity weakness was referred to the neurosurgical department of the Mashhad University of Medical School. The medical history revealed hypertension, and diagnosed with CLL 1.5 months ago. The drug history showed a prescription for aspirin.
Neurologic examination demonstrated a Glasgow Coma scale (GCS) of 15 with normal pupil size. Examination of all cranial nerves was normal. Lower extremities forces were 4 out of 5. and plantar reflexes were flat for both feet with decreased DTR, but no sensory dysfunction was found.
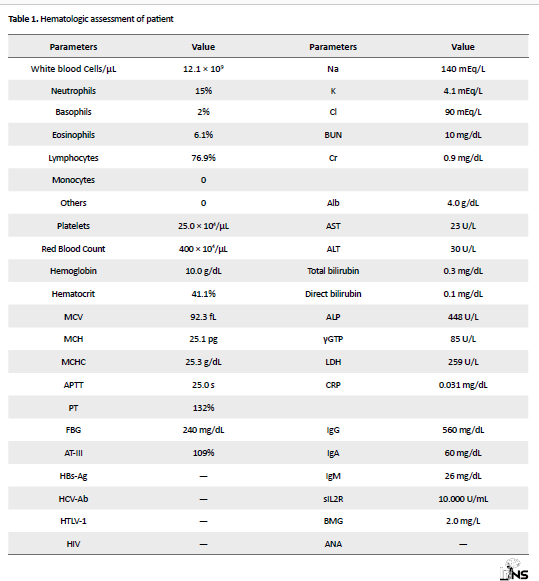
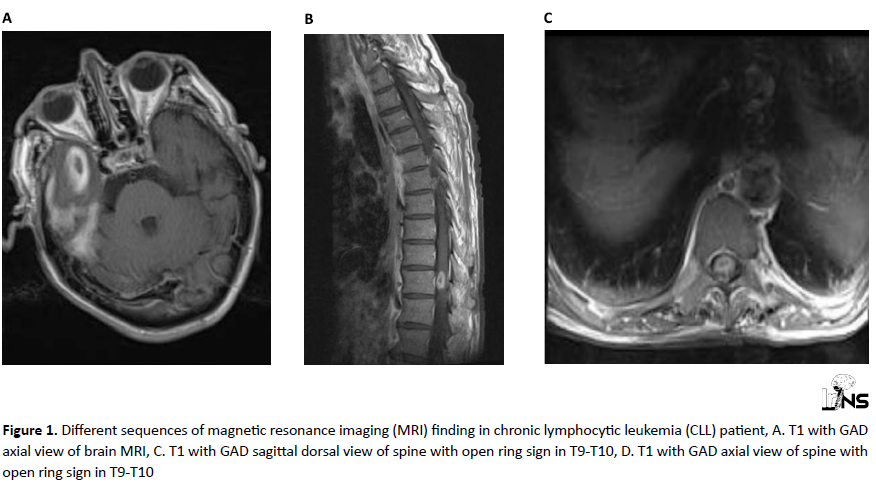
The patients underwent magnetic resonance imaging (MRI) which revealed a “ring or target sign” in the right temporal lobe and similar round shape intramedullary lesion enhanced by gadolinium in T1 according to T10 - T11 (Figure 1).
Before and after the surgery, the patient received dexamethasone (0.4 to 0.8 mg/kg/day), a type of corticosteroid, to help manage symptoms, such as inflammation and swelling in the brain. With high suspicion of metastatic origin, the patient underwent temporal lobe metastasis resection.
The imaging findings on MRI, specifically the “ring or target sign” in the right temporal lobe and the intramedullary lesion in the spinal cord raised concern for CNS infiltration. While CNS involvement can be detected through cerebrospinal fluid (CSF) analysis, a brain biopsy is often considered to make a definitive diagnosis and to rule out other potential differential diagnoses. Given the presence of a newly diagnosed CLL and the appearance of the lesions on imaging, a high suspicion was found that these CNS lesions were related to metastatic CLL involvement. The patient presented with neurological symptoms, including headache and lower extremity weakness. The surgical intervention was conducted to address these symptoms by removing the tumor mass and reducing pressure on the surrounding brain tissue and spinal cord.
The indication for surgery in this known case of CLL with CNS involvement lies in the severity of neurological symptoms and the need for a definitive diagnosis. Even though CLL is a hematologic disease, CNS involvement can lead to various neurological complications, including headaches, weakness, and cognitive impairments. In such cases, prompt intervention is essential to address the immediate neurological issues and potentially improve the patient’s quality of life. While CLL may be diagnosed based on specific markers and blood tests, the presence of CNS involvement adds complexity and requires more targeted management. Surgical intervention can aid in obtaining a tissue sample for accurate diagnosis, as imaging findings alone may not be sufficient to confirm the nature of the lesions. Additionally, surgery can offer symptomatic relief and pave the way for further treatment, such as chemotherapy or radiotherapy, to target the underlying CLL.
The pathological result revealed tumor infiltration of the brain in the background of CLL (Figure 2).
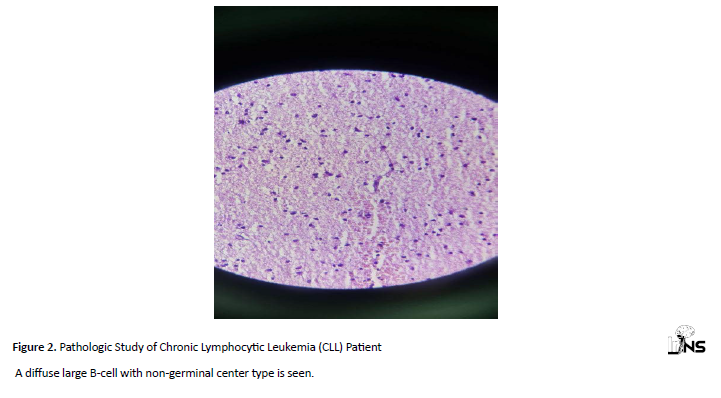
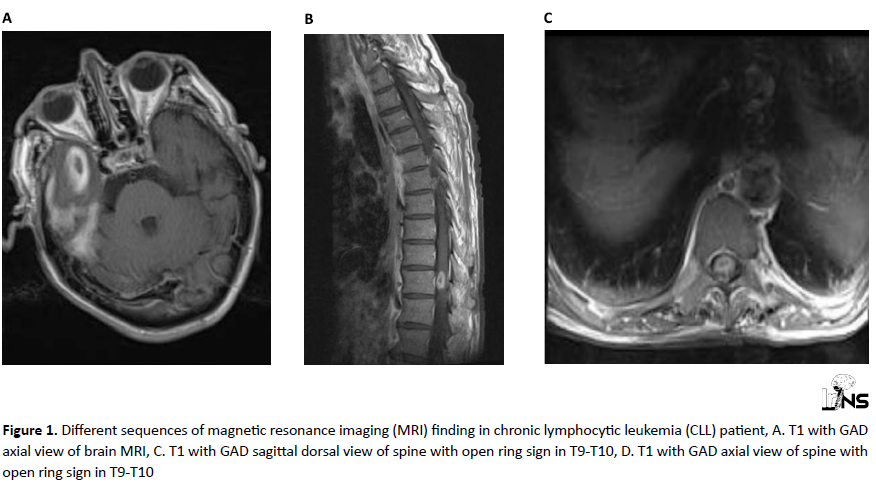
The mass was removed and pathology demonstrated disseminated large B-cell lymphoma of non-germinal center type according to Hans’ classification. Table 1 presents the hematologic assessment of the patient. The leukocyte count was 12.1 × 109/L (76.9% lymphocytes), and fluorescence-activated cell sorting analysis of blood revealed a clonal B-cell population (36.75% leukocytes) corresponding to the immunological chronic Myelogenous Leukemia (CML) profile. Bone marrow aspiration and biopsy also indicated CLL. Furthermore, the patient underwent chemotherapy. Two months after surgery, lower extremities forces were completely intact and referred to an oncologist for further treatment.
Abbreviations: MCV: mean corpuscular volume; MCH: mean corpuscular hemoglobin; MCHC: mean corpuscular hemoglobin concentration; APTT: activated partial thromboplastin time; PT: prothrombin time; FBG: fasting blood glucose; AT-III: antithrombin III; HBs-Ag: hepatitis B virus surface antigen; HCV-Ab: hepatitis C antibody; HTLV-1: human T-lymphotropic virus type 1; HIV: human immunodeficiency virus; Na: sodium; BUN: blood urea nitrogen; K: potassium; CI: Chloride; Cr: chromium; Alb: albumin; AST: aspartate aminotransferase; ALT: alanine transaminase; ALP: alkaline phosphatase; γGTP: gamma glutamyl transpeptidase; LDH: lactate dehydrogenase; CRP: C-reactive protein; IgG: immunoglobulin G; sIL2R: soluble interleukin 2 receptor; BMG: buried-metal-grid; ANA: anti-nuclear antibody
3. Discussion
We presented newly diagnosed CLL in a 71-year-old man complaining of headache and weakness of lower extremities forces. Although between 0.8% to 2% of CLL patients demonstrate CNS involvement, a concurrent presentation of brain and spinal invasion is rare and about 0.4%-2% [3]. CNS lesions are a completely rare consequence with no correlation to risk factors, such as age, gender, and ethnicity [4]. Moreover, the duration of the disease and Rai stage at the time of diagnosis are not related to CNS invasion [4].
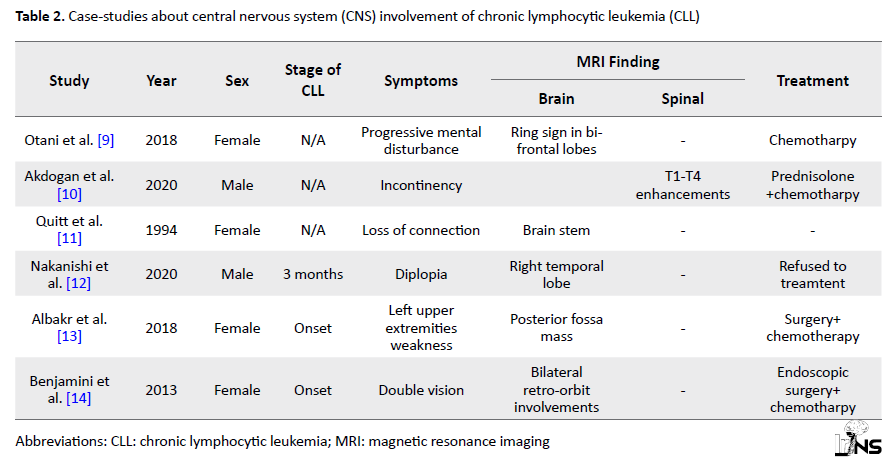
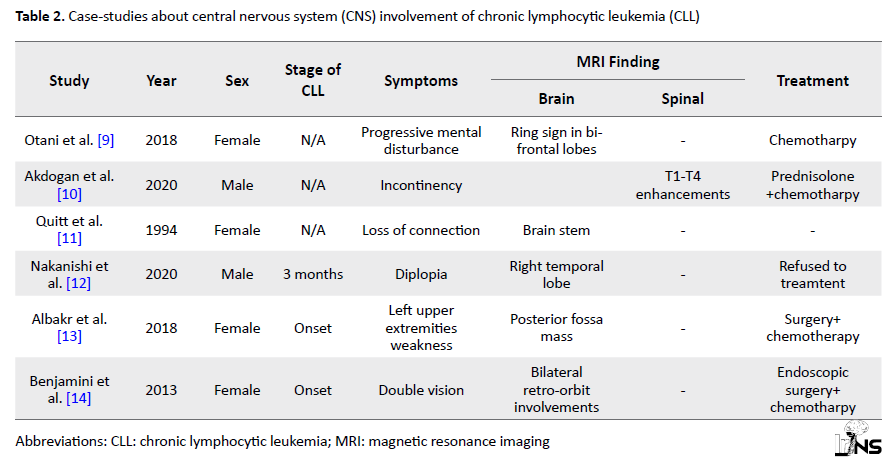
Bayliss et al. reported a 78-year-old case of CLL referred with confusion and a metastatic lesion of the right temporal lobe [5]. As demonstrated in Table 2, the temporal lobe involvement appears to be rare and many studies reported a parenchymal lesion in the occipital lobe, frontal, and basal ganglia [6].
Our patient complained of headache and lower extremity weakness. Although the clinical manifestation of CNS involvement is heterogeneous, reports indicate most symptoms in patients were headache, cranial nerves palsy, and vertigo [7].
We think that the surgical procedure performed on the patient was effective in several aspects. The brain biopsy and removal of the tumor mass allowed for a definitive diagnosis of disseminated large B-cell lymphoma of the non-germinal center type in the background of CLL. This information was crucial in tailoring the subsequent treatment plan. The surgery was conducted to alleviate the patient’s neurological symptoms, including headache and lower extremity weakness. By removing the tumor mass, pressure on the surrounding brain tissue and spinal cord was reduced, leading to an improvement in the patient’s condition. With a confirmed diagnosis, the patient can undergo chemotherapy targeted at treating both CLL and CNS involvement. The surgical intervention was a crucial step in the comprehensive treatment plan for the patient.
The mechanisms of leukemic infiltration in CNS are poorly understood. However, disseminating can be reached by one of three means. First, transmigration across perforating cerebral vessels into the subarachnoid space, second direct extension from seeded meninges into the CSF (especially via the ependymal lining and the choroid plexus), and third, via perineural sheaths on cranial and spinal nerve roots [8].
An open ring sign was found in both the temporal and spinal cord of our patient. Otani et al. reported an open ring sign in the bilateral frontal lobe as well [9]. In addition, Akdogan reported newly onset incontinency and upper motor neuron symptoms with T1-T4 spinal enhancement transverse myelitis which further evaluation confirmed with CLL [10]. Furthermore, the final diagnosis is confirmed by brain biopsy and ruling out other differential diagnosis. Moreover, CSF analysis by lumbar puncture may indicate tumor cells, although flow cytometry may be needed to verify the results. The confirmation of our case was based on the imaging and open craniectomy. In Table 2, we described important case studies about CNS involvement in CLL. No consensus and standard regiments exist for a complete cure for CNS leukemia. The treatment is based on a combination of surgery, chemotherapy, and radiotherapy. Chemotherapy is also applied in systemic or intrathecal manners.
As with any medical decision, the indication for surgery in cases of CLL with CNS involvement should be carefully evaluated individually. Each patient’s clinical presentation, extent of CNS involvement, overall health status, and response to initial treatments should be considered.
Surgery may be recommended in cases where CNS involvement is suspected and the presence of neurological symptoms requires immediate attention. Additionally, when imaging findings alone are inconclusive or when a definitive diagnosis is needed, a brain biopsy through surgical intervention may be warranted.
However, healthcare providers must work collaboratively in a multidisciplinary team, including neurosurgeons, hematologists, and oncologists, to make well-informed decisions regarding the best course of action for each patient. Treatment plans should be tailored to the individual’s unique circumstances and overall treatment goals.
4. Conclusion
In conclusion, CLL with CNS involvement as a primary presentation is a rare clinical manifestation. Although CNS involvement has no specific age, sex, or ethnicity factors and could appear at any stage, this situation should be noted when a patient with a history of CLL demonstrates neurological symptoms. In addition, other differential diagnoses based on imaging findings of both the brain and spine should be in the context. Despite various types of treatment, combination surgical and following chemotherapy is advised in CNS involvement. However, further precise treatment protocols and chemotherapy regiments in this regard are needed.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
Neurologic examination demonstrated a Glasgow Coma scale (GCS) of 15 with normal pupil size. Examination of all cranial nerves was normal. Lower extremities forces were 4 out of 5. and plantar reflexes were flat for both feet with decreased DTR, but no sensory dysfunction was found.
The patients underwent magnetic resonance imaging (MRI) which revealed a “ring or target sign” in the right temporal lobe and similar round shape intramedullary lesion enhanced by gadolinium in T1 according to T10 - T11 (Figure 1).
Before and after the surgery, the patient received dexamethasone (0.4 to 0.8 mg/kg/day), a type of corticosteroid, to help manage symptoms, such as inflammation and swelling in the brain. With high suspicion of metastatic origin, the patient underwent temporal lobe metastasis resection.
The imaging findings on MRI, specifically the “ring or target sign” in the right temporal lobe and the intramedullary lesion in the spinal cord raised concern for CNS infiltration. While CNS involvement can be detected through cerebrospinal fluid (CSF) analysis, a brain biopsy is often considered to make a definitive diagnosis and to rule out other potential differential diagnoses. Given the presence of a newly diagnosed CLL and the appearance of the lesions on imaging, a high suspicion was found that these CNS lesions were related to metastatic CLL involvement. The patient presented with neurological symptoms, including headache and lower extremity weakness. The surgical intervention was conducted to address these symptoms by removing the tumor mass and reducing pressure on the surrounding brain tissue and spinal cord.
The indication for surgery in this known case of CLL with CNS involvement lies in the severity of neurological symptoms and the need for a definitive diagnosis. Even though CLL is a hematologic disease, CNS involvement can lead to various neurological complications, including headaches, weakness, and cognitive impairments. In such cases, prompt intervention is essential to address the immediate neurological issues and potentially improve the patient’s quality of life. While CLL may be diagnosed based on specific markers and blood tests, the presence of CNS involvement adds complexity and requires more targeted management. Surgical intervention can aid in obtaining a tissue sample for accurate diagnosis, as imaging findings alone may not be sufficient to confirm the nature of the lesions. Additionally, surgery can offer symptomatic relief and pave the way for further treatment, such as chemotherapy or radiotherapy, to target the underlying CLL.
The pathological result revealed tumor infiltration of the brain in the background of CLL (Figure 2).
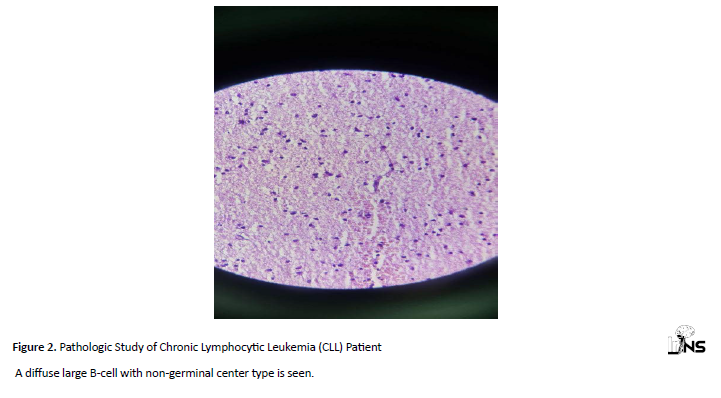
The mass was removed and pathology demonstrated disseminated large B-cell lymphoma of non-germinal center type according to Hans’ classification. Table 1 presents the hematologic assessment of the patient. The leukocyte count was 12.1 × 109/L (76.9% lymphocytes), and fluorescence-activated cell sorting analysis of blood revealed a clonal B-cell population (36.75% leukocytes) corresponding to the immunological chronic Myelogenous Leukemia (CML) profile. Bone marrow aspiration and biopsy also indicated CLL. Furthermore, the patient underwent chemotherapy. Two months after surgery, lower extremities forces were completely intact and referred to an oncologist for further treatment.
Abbreviations: MCV: mean corpuscular volume; MCH: mean corpuscular hemoglobin; MCHC: mean corpuscular hemoglobin concentration; APTT: activated partial thromboplastin time; PT: prothrombin time; FBG: fasting blood glucose; AT-III: antithrombin III; HBs-Ag: hepatitis B virus surface antigen; HCV-Ab: hepatitis C antibody; HTLV-1: human T-lymphotropic virus type 1; HIV: human immunodeficiency virus; Na: sodium; BUN: blood urea nitrogen; K: potassium; CI: Chloride; Cr: chromium; Alb: albumin; AST: aspartate aminotransferase; ALT: alanine transaminase; ALP: alkaline phosphatase; γGTP: gamma glutamyl transpeptidase; LDH: lactate dehydrogenase; CRP: C-reactive protein; IgG: immunoglobulin G; sIL2R: soluble interleukin 2 receptor; BMG: buried-metal-grid; ANA: anti-nuclear antibody
3. Discussion
We presented newly diagnosed CLL in a 71-year-old man complaining of headache and weakness of lower extremities forces. Although between 0.8% to 2% of CLL patients demonstrate CNS involvement, a concurrent presentation of brain and spinal invasion is rare and about 0.4%-2% [3]. CNS lesions are a completely rare consequence with no correlation to risk factors, such as age, gender, and ethnicity [4]. Moreover, the duration of the disease and Rai stage at the time of diagnosis are not related to CNS invasion [4].
Bayliss et al. reported a 78-year-old case of CLL referred with confusion and a metastatic lesion of the right temporal lobe [5]. As demonstrated in Table 2, the temporal lobe involvement appears to be rare and many studies reported a parenchymal lesion in the occipital lobe, frontal, and basal ganglia [6].
Our patient complained of headache and lower extremity weakness. Although the clinical manifestation of CNS involvement is heterogeneous, reports indicate most symptoms in patients were headache, cranial nerves palsy, and vertigo [7].
We think that the surgical procedure performed on the patient was effective in several aspects. The brain biopsy and removal of the tumor mass allowed for a definitive diagnosis of disseminated large B-cell lymphoma of the non-germinal center type in the background of CLL. This information was crucial in tailoring the subsequent treatment plan. The surgery was conducted to alleviate the patient’s neurological symptoms, including headache and lower extremity weakness. By removing the tumor mass, pressure on the surrounding brain tissue and spinal cord was reduced, leading to an improvement in the patient’s condition. With a confirmed diagnosis, the patient can undergo chemotherapy targeted at treating both CLL and CNS involvement. The surgical intervention was a crucial step in the comprehensive treatment plan for the patient.
The mechanisms of leukemic infiltration in CNS are poorly understood. However, disseminating can be reached by one of three means. First, transmigration across perforating cerebral vessels into the subarachnoid space, second direct extension from seeded meninges into the CSF (especially via the ependymal lining and the choroid plexus), and third, via perineural sheaths on cranial and spinal nerve roots [8].
An open ring sign was found in both the temporal and spinal cord of our patient. Otani et al. reported an open ring sign in the bilateral frontal lobe as well [9]. In addition, Akdogan reported newly onset incontinency and upper motor neuron symptoms with T1-T4 spinal enhancement transverse myelitis which further evaluation confirmed with CLL [10]. Furthermore, the final diagnosis is confirmed by brain biopsy and ruling out other differential diagnosis. Moreover, CSF analysis by lumbar puncture may indicate tumor cells, although flow cytometry may be needed to verify the results. The confirmation of our case was based on the imaging and open craniectomy. In Table 2, we described important case studies about CNS involvement in CLL. No consensus and standard regiments exist for a complete cure for CNS leukemia. The treatment is based on a combination of surgery, chemotherapy, and radiotherapy. Chemotherapy is also applied in systemic or intrathecal manners.
As with any medical decision, the indication for surgery in cases of CLL with CNS involvement should be carefully evaluated individually. Each patient’s clinical presentation, extent of CNS involvement, overall health status, and response to initial treatments should be considered.
Surgery may be recommended in cases where CNS involvement is suspected and the presence of neurological symptoms requires immediate attention. Additionally, when imaging findings alone are inconclusive or when a definitive diagnosis is needed, a brain biopsy through surgical intervention may be warranted.
However, healthcare providers must work collaboratively in a multidisciplinary team, including neurosurgeons, hematologists, and oncologists, to make well-informed decisions regarding the best course of action for each patient. Treatment plans should be tailored to the individual’s unique circumstances and overall treatment goals.
4. Conclusion
In conclusion, CLL with CNS involvement as a primary presentation is a rare clinical manifestation. Although CNS involvement has no specific age, sex, or ethnicity factors and could appear at any stage, this situation should be noted when a patient with a history of CLL demonstrates neurological symptoms. In addition, other differential diagnoses based on imaging findings of both the brain and spine should be in the context. Despite various types of treatment, combination surgical and following chemotherapy is advised in CNS involvement. However, further precise treatment protocols and chemotherapy regiments in this regard are needed.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
- Parikh SA. Chronic lymphocytic leukemia treatment algorithm 2018. Blood Cancer Journal. 2018; 8(10):93. [DOI:10.1038/s41408-018-0131-2] [PMID] [PMCID]
- de Souza SL, Santiago F, Ribeiro-Carvalho Mde M, Arnóbio A, Soares AR, Ornellas MH. Leptomeningeal involvement in B-cell chronic lymphocytic leukemia: A case report and review of the literature. BMC Research Notes. 2014; 7:645. [DOI:10.1186/1756-0500-7-645] [PMID] [PMCID]
- Strati P, Uhm JH, Kaufmann TJ, Nabhan C, Parikh SA, Hanson CA, et al. Prevalence and characteristics of central nervous system involvement by chronic lymphocytic leukemia. Haematologica. 2016; 101(4):458-65. [DOI:10.3324/haematol.2015.136556] [PMID] [PMCID]
- Moazzam AA, Drappatz J, Kim RY, Kesari S. Chronic lymphocytic leukemia with central nervous system involvement: Report of two cases with a comprehensive literature review. Journal of Neuro-Oncology. 2012; 106(1):185-200. [DOI:10.1007/s11060-011-0636-z] [PMID]
- Bayliss KM, Kueck BD, Hanson CA, Matthaeus WG, Almagro UA. Richter's syndrome presenting as primary central nervous system lymphoma. Transformation of an identical clone. American Journal of Clinical Pathology. 1990; 93(1):117-23. [DOI:10.1093/ajcp/93.1.117] [PMID]
- Braggio E, Van Wier S, Ojha J, McPhail E, Asmann YW, Egan J, et al. Genome-wide analysis uncovers novel recurrent alterations in primary central nervous system lymphomas. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 2015; 21(17):3986-94. [DOI:10.1158/1078-0432.CCR-14-2116] [PMID] [PMCID]
- Almhanna K, Wongchaowart N, Sweetenham J. Intracerebral Hodgkin's lymphoma in a patient with chronic lymphocytic leukemia/small lymphocytic lymphoma: A case report and literature review. Cancer Investigation. 2009; 27(2):215-20. [DOI:10.1080/07357900802189824] [PMID]
- Alakel N, Stölzel F, Mohr B, Kramer M, Oelschlägel U, Röllig C, et al. Symptomatic central nervous system involvement in adult patients with acute myeloid leukemia. Cancer Management and Research. 2017; 9:97-102. [DOI:10.2147/CMAR.S125259] [PMID] [PMCID]
- Otani R, Uzuka T, Matsuda H, Higuchi F, Kim P, Ueki K. Brain invasion by chronic lymphocytic leukemia. Neuropathology. 2019; 39(1):54-7. [DOI:10.1111/neup.12525] [PMID]
- Akdogan O, Guven T, Altindal S, Erdal Y, Emre U. An uncommon neurological manifestation of chronic lymphocytic leukemia: Longitudinally extensive transverse myelitis. Multiple Sclerosis and Related Disorders. 2020; 37:101455. [DOI:10.1016/j.msard.2019.101455] [PMID]
- Quitt M, Bazac I, Gross B, Aghai E. Fulminant bilateral cerebellar syndrome in a patient with chronic lymphocytic leukemia. Leukemia & Lymphoma. 1994; 15(5-6):507-10. [DOI:10.3109/10428199409049756] [PMID]
- Nakanishi T, Ito T, Fujita S, Satake A, Konishi A, Hotta M, et al. Refractory chronic lymphocytic leukemia with central nervous system involvement: A case report with literature review. Journal of Blood Medicine. 2020; 11:487-502. [DOI:10.2147/JBM.S271335] [PMID] [PMCID]
- Albakr A, Alhothali W, Samghabadi P, Maeda L, Nagpal S, Ajlan A. Central nervous system lymphoma in a patient with chronic lymphocytic leukemia: A case report and literature review. Cureus. 2018; 10(11):e3660. [DOI:10.7759/cureus.3660] [PMID] [PMCID]
- Benjamini O, Jain P, Schlette E, Sciffman JS, Estrov Z, Keating M. Chronic lymphocytic leukemia with central nervous system involvement: A high-risk disease? Clinical Lymphoma, Myeloma & Leukemia. 2013; 13(3):338-41. [DOI:10.1016/j.clml.2012.12.007] [PMID] [PMCID]
Type of Study: Case report |
Subject:
Brain Tumors
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |