Mon, Oct 27, 2025
Volume 9 - Continuous Publishing
Iran J Neurosurg 2023, 9 - Continuous Publishing: 195-201 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hugues Brieux E M, Ruben Ange Florice L, Rel Gerald B K, Olivier Brice N, Sinclair Brice K B, Leon B. Treatment of Subaxial Cervical Spine Injuries at the University Hospital Center of Brazzaville, Congo. Iran J Neurosurg 2023; 9 : 24
URL: http://irjns.org/article-1-361-en.html
URL: http://irjns.org/article-1-361-en.html
Ekouele Mbaki Hugues Brieux *1 

 , Loko Ruben Ange Florice2
, Loko Ruben Ange Florice2 

 , Boukaka Kala Rel Gerald2
, Boukaka Kala Rel Gerald2 

 , Ngackosso Olivier Brice3
, Ngackosso Olivier Brice3 

 , Kinata Bambino Sinclair Brice3
, Kinata Bambino Sinclair Brice3 

 , Boukassa Leon4
, Boukassa Leon4 




 , Loko Ruben Ange Florice2
, Loko Ruben Ange Florice2 

 , Boukaka Kala Rel Gerald2
, Boukaka Kala Rel Gerald2 

 , Ngackosso Olivier Brice3
, Ngackosso Olivier Brice3 

 , Kinata Bambino Sinclair Brice3
, Kinata Bambino Sinclair Brice3 

 , Boukassa Leon4
, Boukassa Leon4 


1- Faculty of Health Sciences, Marien Ngouabi University, Brazzaville, Congo , hugues.ekouele-mbaki@umng.cg
2- Faculty of Health Sciences, Marien Ngouabi University, Brazzaville, Congo
3- Department of Multipurpose Surgery, University Hospital of Brazzaville, Brazzaville, Congo
4- Faculty of Health Sciences, Marien Ngouabi University, Brazzaville, Congo AND Department of Multipurpose Surgery, University Hospital of Brazzaville, Brazzaville, Congo
2- Faculty of Health Sciences, Marien Ngouabi University, Brazzaville, Congo
3- Department of Multipurpose Surgery, University Hospital of Brazzaville, Brazzaville, Congo
4- Faculty of Health Sciences, Marien Ngouabi University, Brazzaville, Congo AND Department of Multipurpose Surgery, University Hospital of Brazzaville, Brazzaville, Congo
Full Text [PDF 961 kb]
(640 Downloads)
| Abstract (HTML) (3052 Views)
Full Text: (861 Views)
1. Introduction
Spinal cord trauma is a public health problem, insofar as these lesions can be prevented and their management is complex with a high overall cost. The annual worldwide incidence of spinal cord trauma varies from 11 to 16 cases per 100,000 inhabitants and the rate of incidence has not varied significantly since 1990 [1].
The subaxial cervical spine is the most frequent seat of such injuries, which are linked to the increased frequency of road accidents. Post-traumatic lesions lead to neurological consequences that can affect the functional prognosis but above all vital [2, 3]. The prognosis of subaxial cervical spine trauma depends on the initial spinal cord injury and the delay of treatment. They affect the labor force in developing countries. In sub-Saharan Africa and the Republic of Congo, in particular, there is a qualitative insufficiency of data and difficulties in the treatment linked to the inadequacy of the technical platform and access to quality care [4, 5].
This study aims to describe the treatment of subaxial cervical spine injuries at the University Hospital Center of Brazzaville, the Republic of Congo.
2. Methods and Materials/Patients
This is a descriptive, cross-sectional, and observational study. The data collection was retrospective, over 7 years from January 1st, 2015 to December 31st, 2021. The study was carried out within the Department of Multipurpose Surgery of the University Hospital Center of Brazzaville which is a tertiary-level hospital center, with an Emergency Department, Multipurpose Resuscitation, Pediatric Surgery, Orthopedics-traumatology, Medical Imaging, and Functional Rehabilitation.
The Department of Multipurpose Surgery brings together the activities of neurosurgery, thoracic, and cardiovascular surgery. The neurosurgical activity is led by 5 specialists. In the operating room, there is an image intensifier, a box of instruments for spine surgery, a box of ancillaries for the cervical spine, and bipolar coagulation.
The Emergency Department includes 2 units, one of which is dedicated to surgical emergencies. The Multipurpose Intensive Care Unit consists of 11 beds. However, spinal surgery is not performed in the Pediatric Surgery and Orthopedics-traumatology departments.
The imaging service allows the performance of standard X-ray examinations for 6000 francs from the African Financial Community (equal to 9.9 USD). The computed tomography (CT) scan costs 99 USD and magnetic resonance imaging 132 USD. In the City of Brazzaville, Congo, 3 other public hospitals and 2 private clinics perform CT scans with variable costs, ranging from 82.5 to 165 USD.
The Functional Rehabilitation Department does not have hospital beds. It has outpatient care resources and can intervene, on request, for the benefit of hospitalized patients.
The patients are usually admitted to the surgical unit of the Emergency Department. After an initial assessment, the on-call neurosurgeon is asked to provide a specialist opinion. In case of subaxial spine injury, the patient is transferred to the Department of Multipurpose Surgery. An anti-decubitus mattress is prescribed when the patient and or their entourage can obtain it. For patients with signs of respiratory or hemodynamic severity, surgery is deferred until stabilization.
The surgical management protocol includes general anesthesia, transcranial traction, and on the hands to lower the shoulders, radiological tracking. The anterior approach is pre-sterno-cleido-mastoid, using a Cloward-type retractor. The posterior approach is recommended to remove impingement of the joints. The post-operative stay is assured with the systematic placement of a neck brace, antibiotic prophylaxis for 48 hours, analgesics, and enoxaparin at an iso-coagulant dose.
In the event of a surgical indication, an operative prescription is given to the family. It includes introns for the surgical procedure, anesthetic drugs, and payment for the operation at the hospital cash register. The cost of these items equals 1022 USD.
The target population corresponded to all patients with subaxial cervical spine injury. The population source corresponded to all cases hospitalized in the General Surgery Department. We included all patients hospitalized for subaxial cervical spine injury, having performed at least 1 radiological examination. We excluded all patients whose record was incomplete. The data were recorded by the Epi Info software (version 7.2.5.0). The Excel software, version 2016 was used to create the graphs. The Mantel-Haenszel chi-square test was used to verify the statistical association between age, American Spine Injury Association (ASIA) score, and types of imaging lesions with the occurrence of complications (including death). The significance level was set at 0.05 with a confidence interval of 95%. The binomial logistic regression was performed along with the chi-square likelihood test. The likelihood ratio was used to retain the final regression model that we presented.
3. Results
Frequency
We recorded the data on 2800 patients, including 90 cases of TRCI with a frequency of 3.2%. Among these 90 patients, 60 cases met the inclusion criteria with a frequency of 2.1%.
Socio-demographic and Diagnostic Aspects
The median age of the subjects was 37 years with quartile 1(Q1)=28 years and quartile 3(Q3)=45.5 years. Meanwhile, the minimum and maximum age was 6 and 83 years, respectively. Among the 60 cases, 47(78.3%) patients were male and 13(21.6%) were female with a sex ratio (male/female) of 3.6. The trauma was due to a road accident in 41 cases (68.3%) and a fall in 10 cases (16.7%). Three cases (5%) had medical insurance.
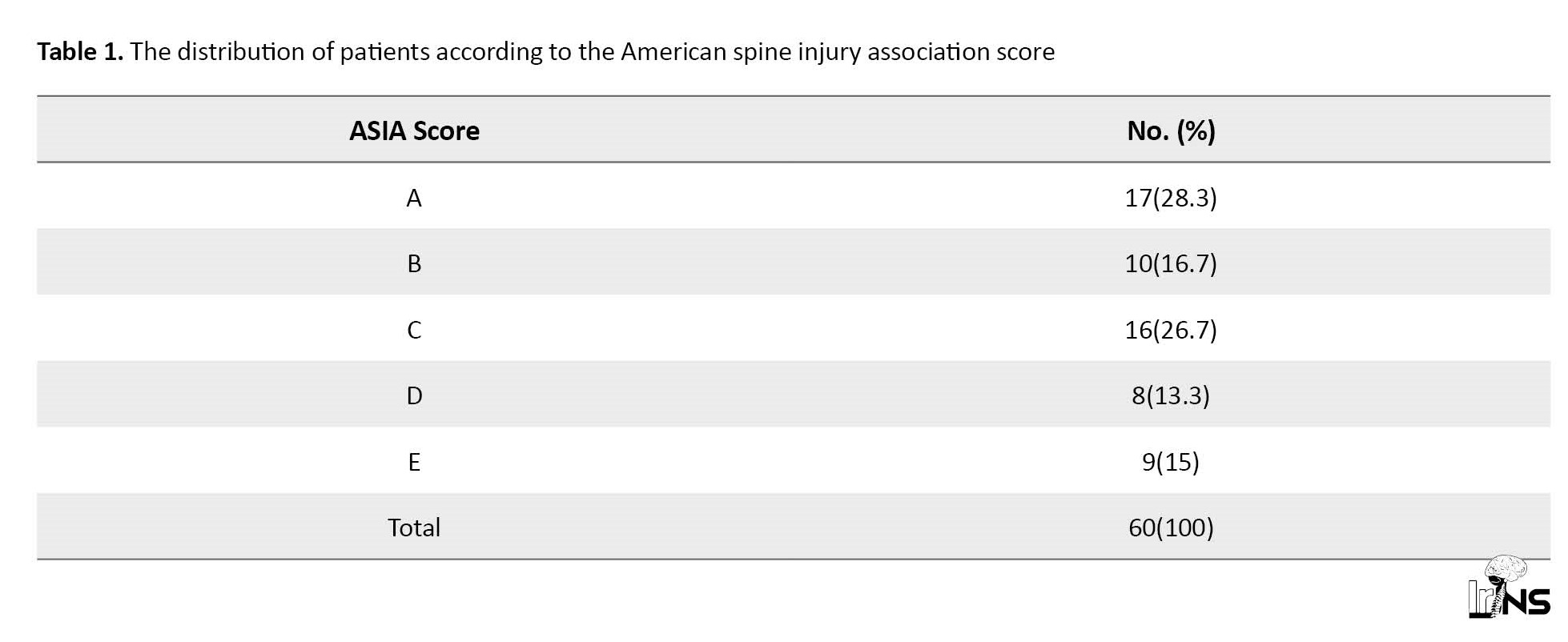
Table 1 represents the cases in the series according to the ASIA score.
Meanwhile, 6 patients (10%) had respiratory distress, 16(26.7%) experienced priapism and 1(1.7%) showed hypothermia. Among the 60 cases, 49(81.7%) presented a neurological deficit and 2(3.3%) subjects presented a disorder of consciousness.
The reached vertebral level was C5-C6 in 18 cases (30%), C4-C5 in 16 cases (26.7%), C6-C7 in 10 cases (16.7%), and C3-C4 in 4 cases (6.7%). It was a luxation in 18 cases (30%), fracture luxation in 16 cases (26.7%), and fracture in 12 cases (20%). Spinal contusion was identified in 12 cases (20%) and myelopathy decompensated by trauma in 8 cases (13.3%).
Treatment and Outcome
Among the 60 cases in the sample, 4(6.7%) had benefited from medical transport. The cervical collar was available in 59 cases (98.3%) and 9 patients (15%) benefited from resuscitation measures (respiratory assistance, vascular filling).
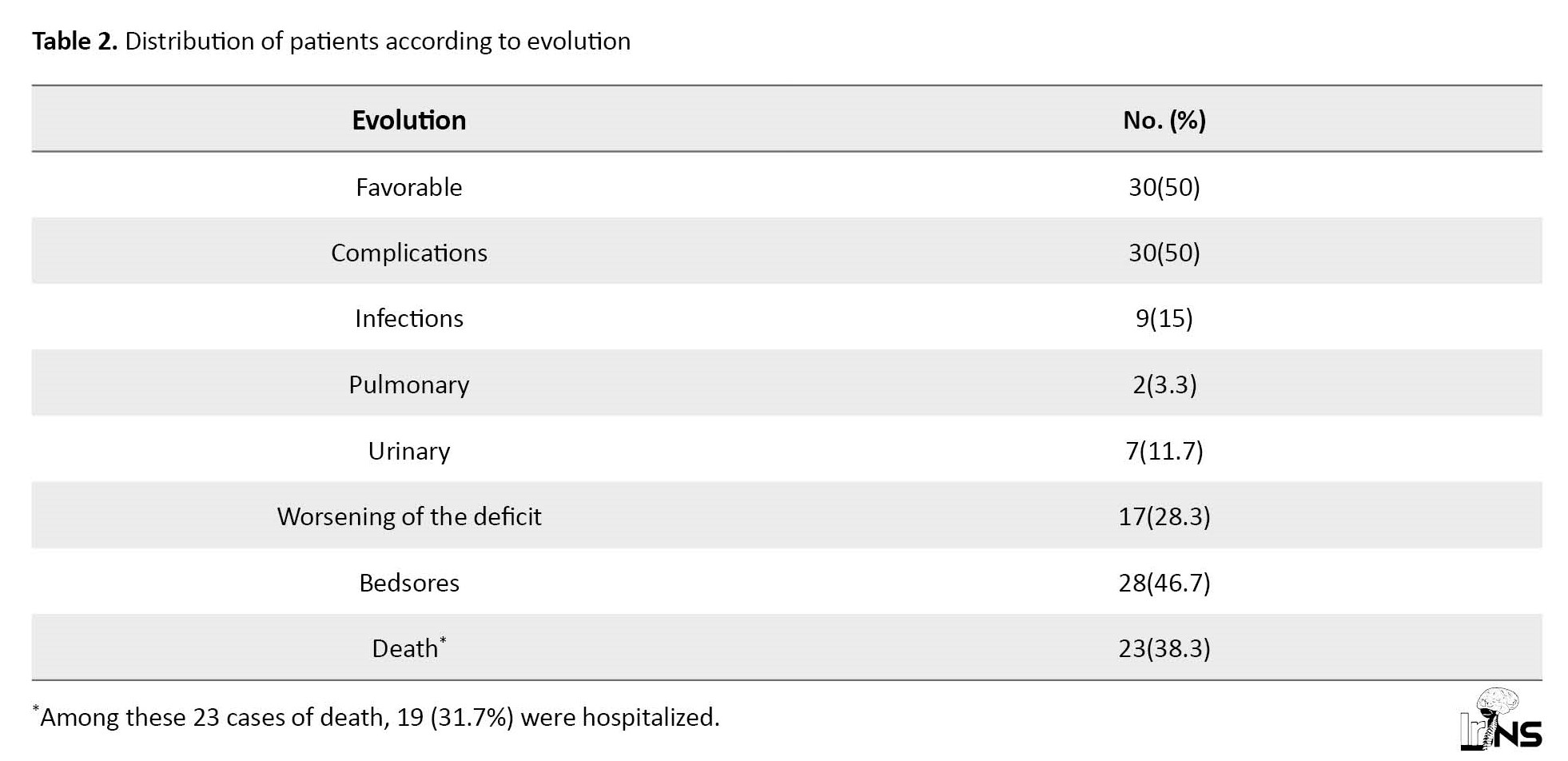
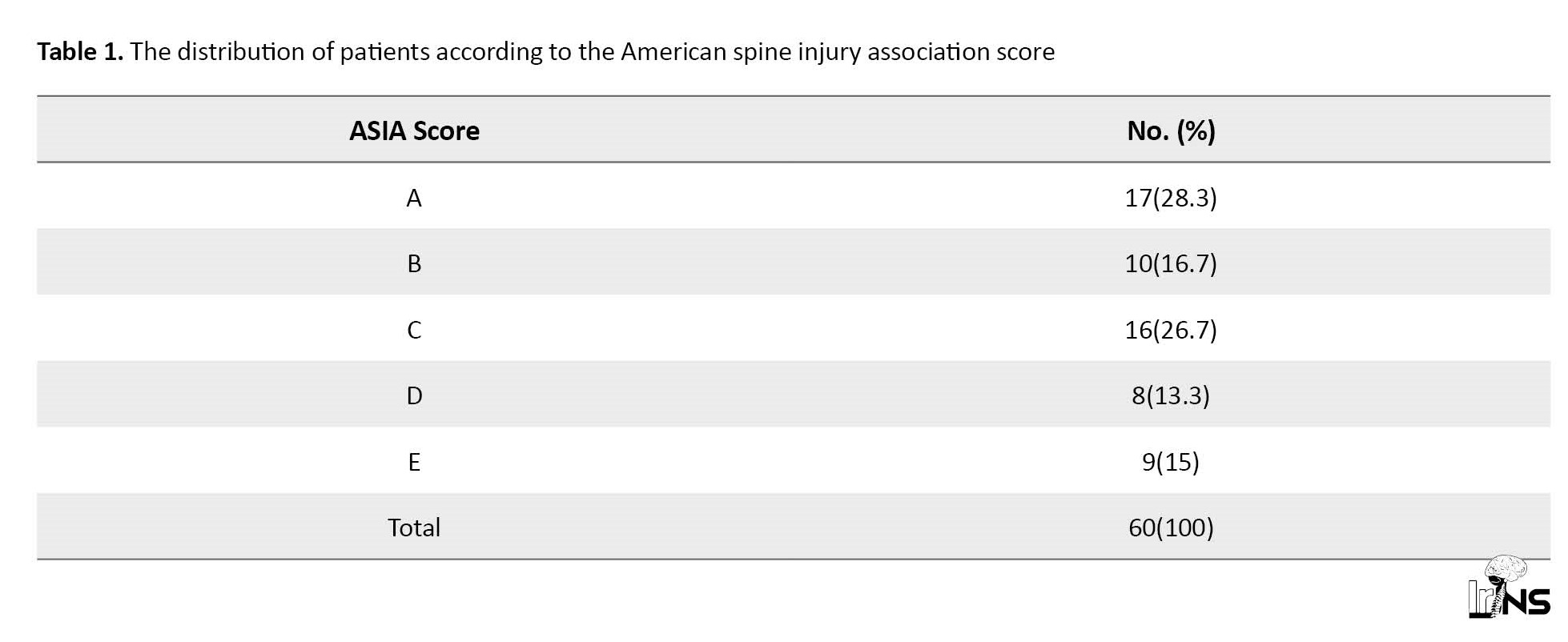
Surgery was indicated in 51 patients and on 32(53.3%) subjects the operation was done. Among the 19 non-operated patients, 12 had died before the intervention and 7 were discharged against medical advice. The median time between admission and surgery was 288 h with Q1=144 h and Q3=480 h. The minimum and maximum measures were 24 and 720 h. Among the operated patients, 7(21.8%) were ASIA level A, 8 were ASIA level B (25%), 10 were ASIA level C (31.3%), 5 were ASIA level D (15.6%), and 2 were ASIA level E (6.2%). Among the 32 operated cases, 31(96.9%) were operated by anterior approach and 1(3.1%) case by double approach due to joint impingement not relieved by intraoperative transcranial traction. Anterior osteosynthesis was performed in all cases. Corpectomy was performed in 3 cases (9.4%) and discectomy in 29 cases (90.6%). Table 2 represents the distribution of patients, based on the evolution.
Among the 32 operated cases, 18(56.3%) had a favorable evolution, 7(21.9%) had a worsening of the deficit, 5(15.6%) had a postoperative infection, 5(15.6%) experienced deep pressure ulcers, and 7(22%) had died.
The median duration of hospitalization was 15 days with Q1=6 days and Q3=22.5 days while the minimum and maximum values were 1 and 68 days, respectively.
Remote data collection by telephone contact provided the opportunity to obtain information on 13(31.7%) patients among the 41 contacted subjects. Among the 13 cases, 6(46.2%) were living without sequelae and 3(23.1%) with sequelae, such as paralysis of the limb, 4(30.8%) had died, of whom 3(75%) were among the 4 on whom the operation was conducted.
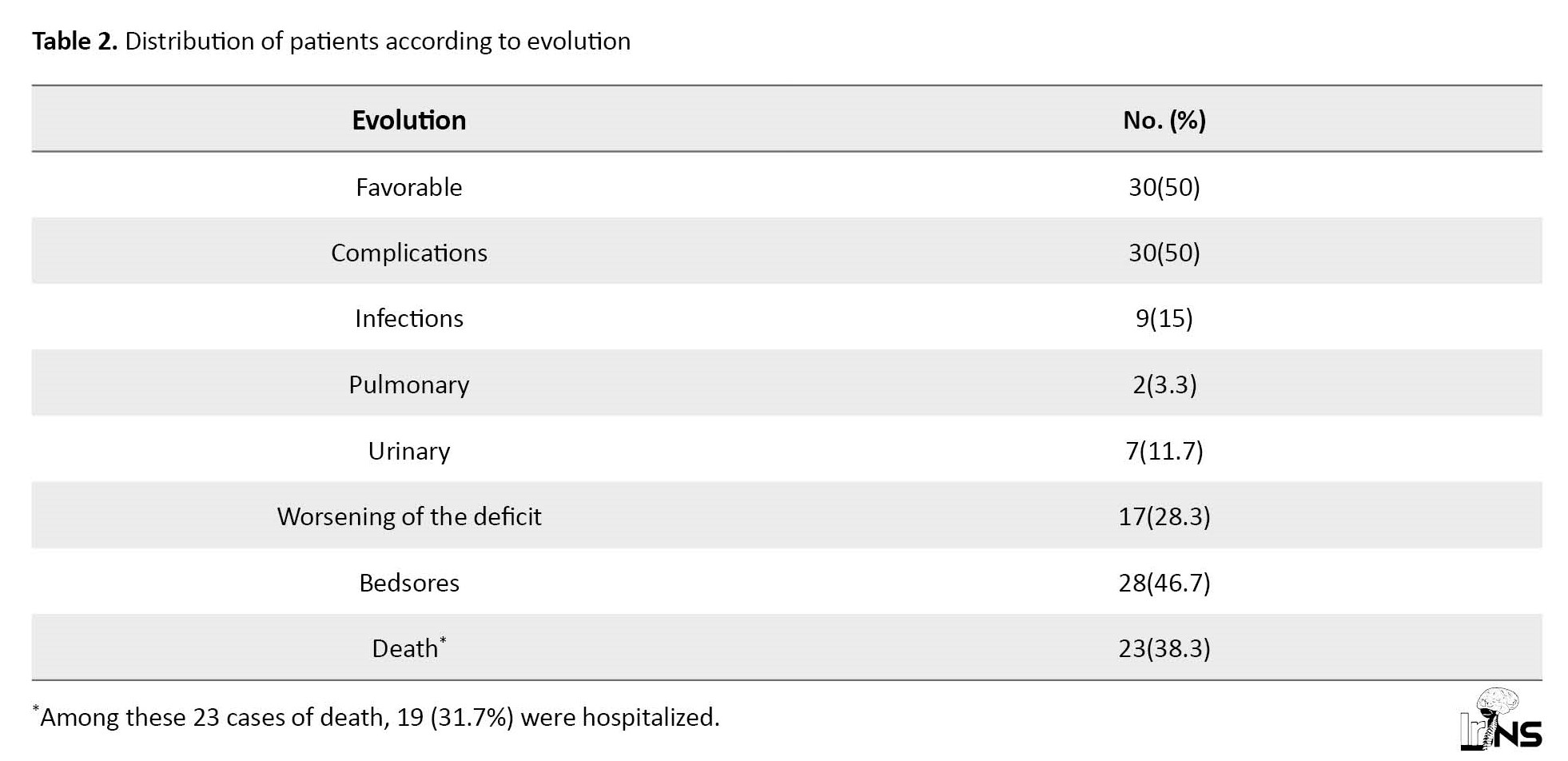
In univariate analysis, the occurrence of complications was associated with the ASIA score with a probability P=0.0115. No significant association was observed for age (P=0.7376) and type of radiological lesion (P=0.4446).
Table 3 represents the results of the logistic regression of the factors associated with the morbidity of TRCI.
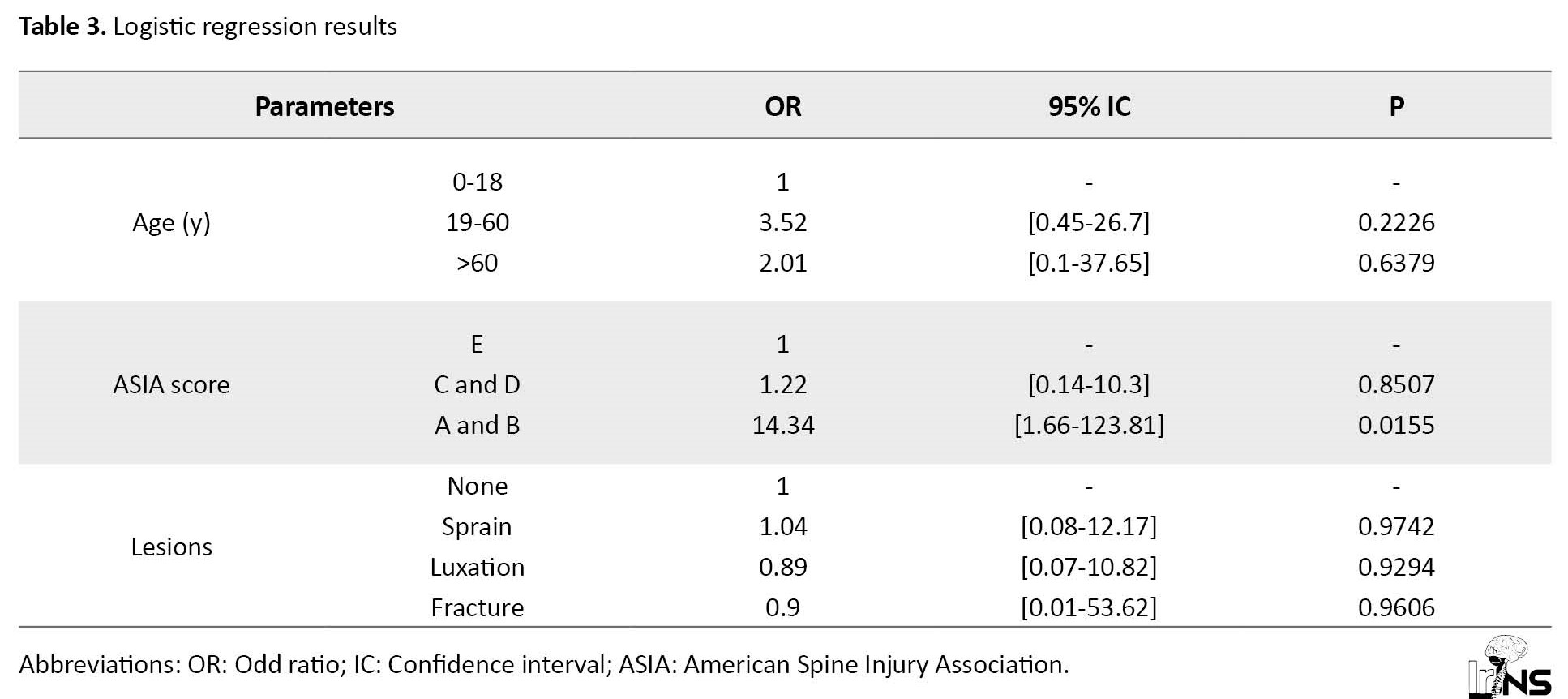
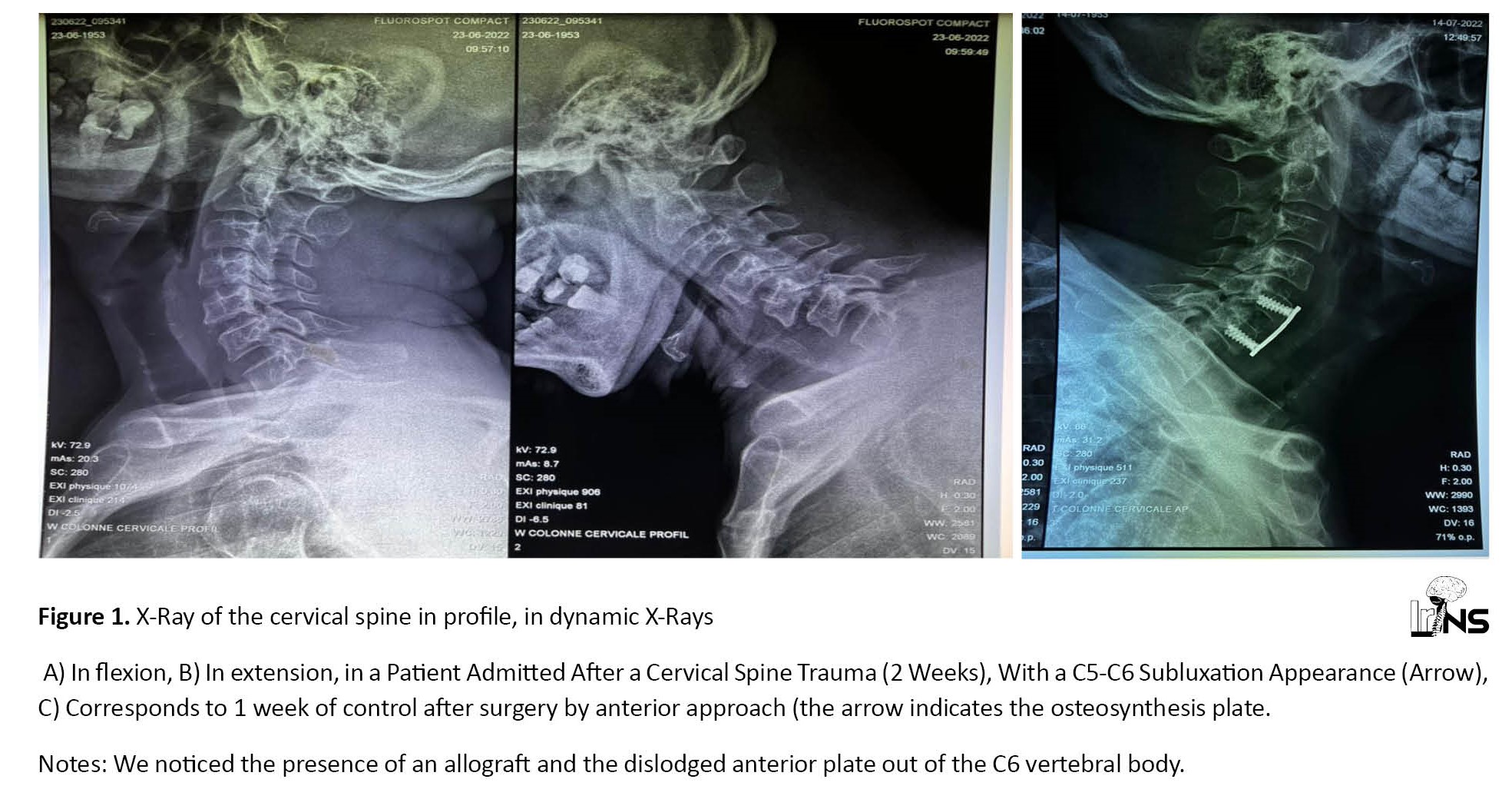
Figure 1 shows (in the A and B sections) the preoperative dynamic X-ray images of a C5-C6 dislocation. Meanwhile, Figure 1 C shows a postoperative image.
4. Discussion
Among the 60 cases in the series, 4 patients (6.7%) had benefited from medical transport from the place of the accident to admission. Bello et al. [6] found a frequency of 2.9%. Such low frequencies can be explained by the lack of prehospital management of road injuries in our context.
Surgery was performed in 32 cases (53.3%). This result is close to the results of Bello et al. [6] who performed the surgery on 42.6% of the cases. Kpelao et al. [4] performed the surgery on 83.8%. The latter research was conducted mainly on severe trauma.
In this research, the median time between admission and surgery was 288 hours (12 days). Bello et al. [6]performed surgery beyond 48 h in all patients. Kpelao et al. [4] reported a delay of 64.8 h (2 days). Most authors recommend surgery within 24 hours after a spine trauma [7, 8]. These prolonged waiting times are probably linked to the lack of health coverage (health insurance) for our patients.
Arthrodesis with anterior osteosynthesis was systematically performed in our series. Loembe et al. [9] performed anterior fixation in 72.2% of cases, posterior fixation in 23.5% of cases, and a combined approach in 4.3% of cases. In Greece, Kasimatis et al. [10], during a cohort study of 74 patients treated by an anterior approach, identified a fusion rate of 90% along with 3 surgical revisions. The anterior approach is preferred by some authors because of the comfort for the patient in terms of operating position (dorsal decubitus), access to the lesion site is quick, and less damage compared to disinsertion of the paravertebral muscles. Access to the intervertebral disc and vertebral bodies is easy, similar to anterior decompression of the spinal cord [11]. In Greece, Lambiris et al. [12], in a cohort study, compared the anterior and posterior approaches and found no difference in terms of complications between the 2 techniques.
As the Polyvalent Surgery Department does not have a functional rehabilitation unit, physiotherapy was provided on-demand or on an outpatient basis, regardless of the degree of motor deficit. Insufficient functional rehabilitation constitutes an obstacle in the management of these patients [4].
Among the 60 cases in the samples, 28(46.7%) had developed pressure ulcers, and 9(15%) had infections, including 3.3% pneumonia and 11.7% urinary tract infection. In a previous study on cervical spine trauma [5], we found 14.6% of cases of deep pressure ulcers and 15% of cases of infection. Bello et al. [6] found 20.6% pressure ulcers and 26.5% infectious complications (urinary and pulmonary). These complications can be explained by the lack of anti-decubitus mattresses and the delay in surgical treatment. The delay in care also affects the possibilities of moving the patient as soon as possible, when the latter has not recovered their autonomy.
Hospital deaths were about 38.3% in our sample. Bello et al. [6] found a frequency of 16.2%. Mortality related to spinal trauma in sub-Saharan Africa is in the range of 7% and 35% [4].
In both univariate and multivariate analysis, an unfavorable ASIA score (between A and B) was associated with the occurrence of complications, with a significant statistical difference (P<0.05). A previous study [5] reported that 7 out of 10 patients classified as A and B had not recovered from the motor deficit.
The D-class patients all recovered from their deficits. Thiam et al. [4], using the Frankel classification, reported on 90 cases, 36 patients were classified as A on admission, 33 patients were classified as A after treatment, 21 patients were classified as B on admission versus 11 patients after treatment, and no patients were classified E on admission versus 20 patients after treatment.
5. Conclusion
Subaxial cervical spine injuries represent nearly 3% of patients treated in the Department of Multipurpose Surgery of the University Hospital Center of Brazzaville. The most affected people in their thirties were males. Road accident is the primary cause. Prehospital care is not medicalized. The majority of trauma patients are admitted with a complete neurological deficit. The CT scan of the cervical spine is the main paraclinical examination and highlights the lesions with the most frequent luxation. Therapeutic care is delayed due to insufficient financial means for patients who do not have health insurance. The surgery consists of neural decompression, arthrodesis, and osteosynthesis, essentially by an anterior approach. The ongoing complications consisted of the development of pressure sores, followed by infections. The mortality rate is around 30%. The high frequency of complications is statistically linked to an unfavorable ASIA score (between A and B).
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Faculty of Health Sciences, Marien Ngouabi University, Brazzaville, Congo (Code: 0032/MESRSIT/DGRST/CERSSA/22). All ethical principles were considered in this article. The confidentiality of information was assured. Moreover, the cases were allowed to leave the study whenever they wished, and if desired, the results of the research would be available to them. The participants joined by phone were informed about the purpose of the research and its implementation stages. Informed consent was obtained from them.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Methodology, data collection and redaction: Hugues Brieux Ekouele Mbaki and Ruben Ange Florice Loko; Critical reading and data analysis: Rel Gerald Boukaka Kala, Sinclair Brice Kinata Bambino, Olivier Brice Ngackosso and Léon Boukassa; Conceptualization and design: Hugues Brieux Ekouele Mbaki and Ruben Ange Florice Lok; Data collection: Hugues Brieux Ekouele Mbaki and Ruben Ange Florice Loko; Data analysis and interpretation: Rel Gerald Boukaka Kala, Sinclair Brice Kinata Bambino, Olivier Brice Ngackosso and Léon Boukassa; Writing–original draft, writing–review, editing and Final approving: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
Thanks to Dr. Mbou Essie Darius and Dr. Bingui Outman Diogene for their contribution to the statistical processing of the data.
References
Spinal cord trauma is a public health problem, insofar as these lesions can be prevented and their management is complex with a high overall cost. The annual worldwide incidence of spinal cord trauma varies from 11 to 16 cases per 100,000 inhabitants and the rate of incidence has not varied significantly since 1990 [1].
The subaxial cervical spine is the most frequent seat of such injuries, which are linked to the increased frequency of road accidents. Post-traumatic lesions lead to neurological consequences that can affect the functional prognosis but above all vital [2, 3]. The prognosis of subaxial cervical spine trauma depends on the initial spinal cord injury and the delay of treatment. They affect the labor force in developing countries. In sub-Saharan Africa and the Republic of Congo, in particular, there is a qualitative insufficiency of data and difficulties in the treatment linked to the inadequacy of the technical platform and access to quality care [4, 5].
This study aims to describe the treatment of subaxial cervical spine injuries at the University Hospital Center of Brazzaville, the Republic of Congo.
2. Methods and Materials/Patients
This is a descriptive, cross-sectional, and observational study. The data collection was retrospective, over 7 years from January 1st, 2015 to December 31st, 2021. The study was carried out within the Department of Multipurpose Surgery of the University Hospital Center of Brazzaville which is a tertiary-level hospital center, with an Emergency Department, Multipurpose Resuscitation, Pediatric Surgery, Orthopedics-traumatology, Medical Imaging, and Functional Rehabilitation.
The Department of Multipurpose Surgery brings together the activities of neurosurgery, thoracic, and cardiovascular surgery. The neurosurgical activity is led by 5 specialists. In the operating room, there is an image intensifier, a box of instruments for spine surgery, a box of ancillaries for the cervical spine, and bipolar coagulation.
The Emergency Department includes 2 units, one of which is dedicated to surgical emergencies. The Multipurpose Intensive Care Unit consists of 11 beds. However, spinal surgery is not performed in the Pediatric Surgery and Orthopedics-traumatology departments.
The imaging service allows the performance of standard X-ray examinations for 6000 francs from the African Financial Community (equal to 9.9 USD). The computed tomography (CT) scan costs 99 USD and magnetic resonance imaging 132 USD. In the City of Brazzaville, Congo, 3 other public hospitals and 2 private clinics perform CT scans with variable costs, ranging from 82.5 to 165 USD.
The Functional Rehabilitation Department does not have hospital beds. It has outpatient care resources and can intervene, on request, for the benefit of hospitalized patients.
The patients are usually admitted to the surgical unit of the Emergency Department. After an initial assessment, the on-call neurosurgeon is asked to provide a specialist opinion. In case of subaxial spine injury, the patient is transferred to the Department of Multipurpose Surgery. An anti-decubitus mattress is prescribed when the patient and or their entourage can obtain it. For patients with signs of respiratory or hemodynamic severity, surgery is deferred until stabilization.
The surgical management protocol includes general anesthesia, transcranial traction, and on the hands to lower the shoulders, radiological tracking. The anterior approach is pre-sterno-cleido-mastoid, using a Cloward-type retractor. The posterior approach is recommended to remove impingement of the joints. The post-operative stay is assured with the systematic placement of a neck brace, antibiotic prophylaxis for 48 hours, analgesics, and enoxaparin at an iso-coagulant dose.
In the event of a surgical indication, an operative prescription is given to the family. It includes introns for the surgical procedure, anesthetic drugs, and payment for the operation at the hospital cash register. The cost of these items equals 1022 USD.
The target population corresponded to all patients with subaxial cervical spine injury. The population source corresponded to all cases hospitalized in the General Surgery Department. We included all patients hospitalized for subaxial cervical spine injury, having performed at least 1 radiological examination. We excluded all patients whose record was incomplete. The data were recorded by the Epi Info software (version 7.2.5.0). The Excel software, version 2016 was used to create the graphs. The Mantel-Haenszel chi-square test was used to verify the statistical association between age, American Spine Injury Association (ASIA) score, and types of imaging lesions with the occurrence of complications (including death). The significance level was set at 0.05 with a confidence interval of 95%. The binomial logistic regression was performed along with the chi-square likelihood test. The likelihood ratio was used to retain the final regression model that we presented.
3. Results
Frequency
We recorded the data on 2800 patients, including 90 cases of TRCI with a frequency of 3.2%. Among these 90 patients, 60 cases met the inclusion criteria with a frequency of 2.1%.
Socio-demographic and Diagnostic Aspects
The median age of the subjects was 37 years with quartile 1(Q1)=28 years and quartile 3(Q3)=45.5 years. Meanwhile, the minimum and maximum age was 6 and 83 years, respectively. Among the 60 cases, 47(78.3%) patients were male and 13(21.6%) were female with a sex ratio (male/female) of 3.6. The trauma was due to a road accident in 41 cases (68.3%) and a fall in 10 cases (16.7%). Three cases (5%) had medical insurance.
Table 1 represents the cases in the series according to the ASIA score.
Meanwhile, 6 patients (10%) had respiratory distress, 16(26.7%) experienced priapism and 1(1.7%) showed hypothermia. Among the 60 cases, 49(81.7%) presented a neurological deficit and 2(3.3%) subjects presented a disorder of consciousness.
The reached vertebral level was C5-C6 in 18 cases (30%), C4-C5 in 16 cases (26.7%), C6-C7 in 10 cases (16.7%), and C3-C4 in 4 cases (6.7%). It was a luxation in 18 cases (30%), fracture luxation in 16 cases (26.7%), and fracture in 12 cases (20%). Spinal contusion was identified in 12 cases (20%) and myelopathy decompensated by trauma in 8 cases (13.3%).
Treatment and Outcome
Among the 60 cases in the sample, 4(6.7%) had benefited from medical transport. The cervical collar was available in 59 cases (98.3%) and 9 patients (15%) benefited from resuscitation measures (respiratory assistance, vascular filling).
Surgery was indicated in 51 patients and on 32(53.3%) subjects the operation was done. Among the 19 non-operated patients, 12 had died before the intervention and 7 were discharged against medical advice. The median time between admission and surgery was 288 h with Q1=144 h and Q3=480 h. The minimum and maximum measures were 24 and 720 h. Among the operated patients, 7(21.8%) were ASIA level A, 8 were ASIA level B (25%), 10 were ASIA level C (31.3%), 5 were ASIA level D (15.6%), and 2 were ASIA level E (6.2%). Among the 32 operated cases, 31(96.9%) were operated by anterior approach and 1(3.1%) case by double approach due to joint impingement not relieved by intraoperative transcranial traction. Anterior osteosynthesis was performed in all cases. Corpectomy was performed in 3 cases (9.4%) and discectomy in 29 cases (90.6%). Table 2 represents the distribution of patients, based on the evolution.
Among the 32 operated cases, 18(56.3%) had a favorable evolution, 7(21.9%) had a worsening of the deficit, 5(15.6%) had a postoperative infection, 5(15.6%) experienced deep pressure ulcers, and 7(22%) had died.
The median duration of hospitalization was 15 days with Q1=6 days and Q3=22.5 days while the minimum and maximum values were 1 and 68 days, respectively.
Remote data collection by telephone contact provided the opportunity to obtain information on 13(31.7%) patients among the 41 contacted subjects. Among the 13 cases, 6(46.2%) were living without sequelae and 3(23.1%) with sequelae, such as paralysis of the limb, 4(30.8%) had died, of whom 3(75%) were among the 4 on whom the operation was conducted.
In univariate analysis, the occurrence of complications was associated with the ASIA score with a probability P=0.0115. No significant association was observed for age (P=0.7376) and type of radiological lesion (P=0.4446).
Table 3 represents the results of the logistic regression of the factors associated with the morbidity of TRCI.
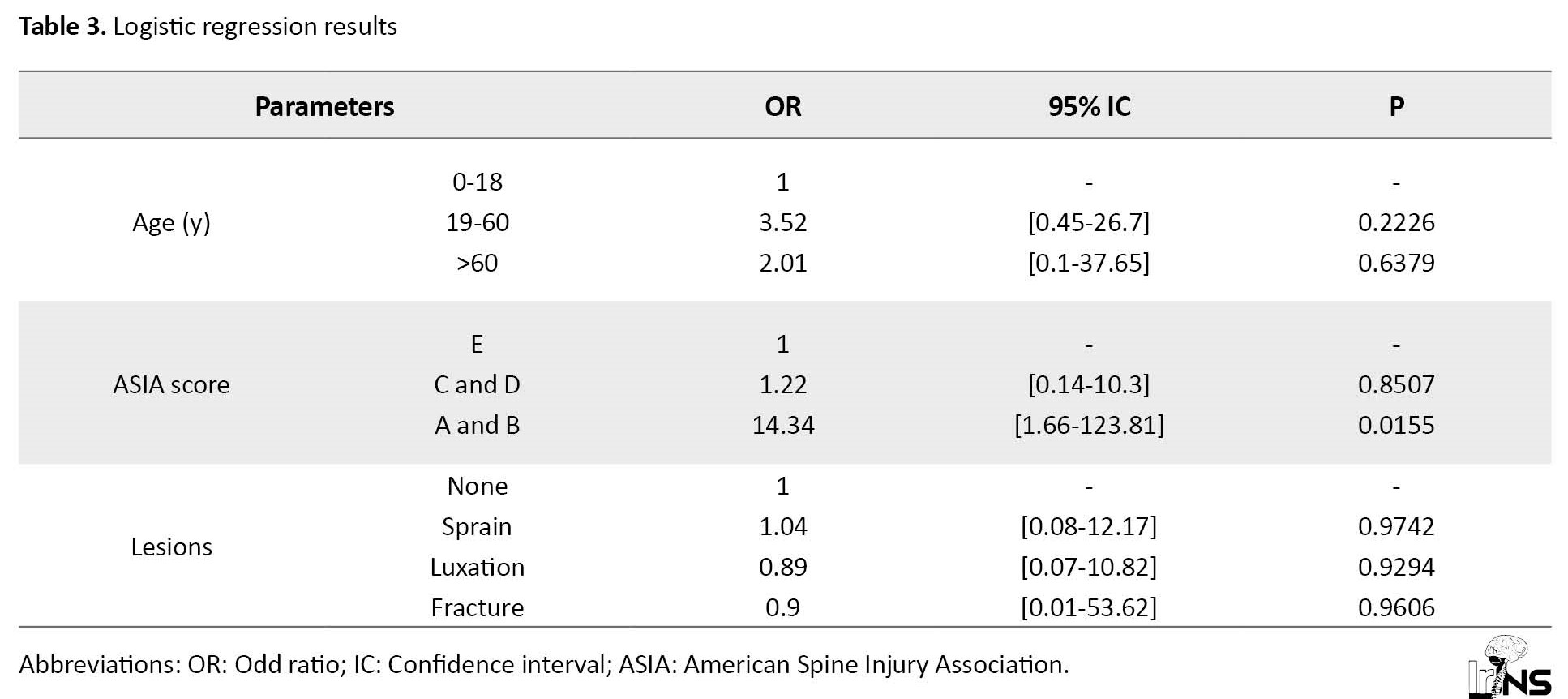
Figure 1 shows (in the A and B sections) the preoperative dynamic X-ray images of a C5-C6 dislocation. Meanwhile, Figure 1 C shows a postoperative image.
4. Discussion
Among the 60 cases in the series, 4 patients (6.7%) had benefited from medical transport from the place of the accident to admission. Bello et al. [6] found a frequency of 2.9%. Such low frequencies can be explained by the lack of prehospital management of road injuries in our context.
Surgery was performed in 32 cases (53.3%). This result is close to the results of Bello et al. [6] who performed the surgery on 42.6% of the cases. Kpelao et al. [4] performed the surgery on 83.8%. The latter research was conducted mainly on severe trauma.
In this research, the median time between admission and surgery was 288 hours (12 days). Bello et al. [6]performed surgery beyond 48 h in all patients. Kpelao et al. [4] reported a delay of 64.8 h (2 days). Most authors recommend surgery within 24 hours after a spine trauma [7, 8]. These prolonged waiting times are probably linked to the lack of health coverage (health insurance) for our patients.
Arthrodesis with anterior osteosynthesis was systematically performed in our series. Loembe et al. [9] performed anterior fixation in 72.2% of cases, posterior fixation in 23.5% of cases, and a combined approach in 4.3% of cases. In Greece, Kasimatis et al. [10], during a cohort study of 74 patients treated by an anterior approach, identified a fusion rate of 90% along with 3 surgical revisions. The anterior approach is preferred by some authors because of the comfort for the patient in terms of operating position (dorsal decubitus), access to the lesion site is quick, and less damage compared to disinsertion of the paravertebral muscles. Access to the intervertebral disc and vertebral bodies is easy, similar to anterior decompression of the spinal cord [11]. In Greece, Lambiris et al. [12], in a cohort study, compared the anterior and posterior approaches and found no difference in terms of complications between the 2 techniques.
As the Polyvalent Surgery Department does not have a functional rehabilitation unit, physiotherapy was provided on-demand or on an outpatient basis, regardless of the degree of motor deficit. Insufficient functional rehabilitation constitutes an obstacle in the management of these patients [4].
Among the 60 cases in the samples, 28(46.7%) had developed pressure ulcers, and 9(15%) had infections, including 3.3% pneumonia and 11.7% urinary tract infection. In a previous study on cervical spine trauma [5], we found 14.6% of cases of deep pressure ulcers and 15% of cases of infection. Bello et al. [6] found 20.6% pressure ulcers and 26.5% infectious complications (urinary and pulmonary). These complications can be explained by the lack of anti-decubitus mattresses and the delay in surgical treatment. The delay in care also affects the possibilities of moving the patient as soon as possible, when the latter has not recovered their autonomy.
Hospital deaths were about 38.3% in our sample. Bello et al. [6] found a frequency of 16.2%. Mortality related to spinal trauma in sub-Saharan Africa is in the range of 7% and 35% [4].
In both univariate and multivariate analysis, an unfavorable ASIA score (between A and B) was associated with the occurrence of complications, with a significant statistical difference (P<0.05). A previous study [5] reported that 7 out of 10 patients classified as A and B had not recovered from the motor deficit.
The D-class patients all recovered from their deficits. Thiam et al. [4], using the Frankel classification, reported on 90 cases, 36 patients were classified as A on admission, 33 patients were classified as A after treatment, 21 patients were classified as B on admission versus 11 patients after treatment, and no patients were classified E on admission versus 20 patients after treatment.
5. Conclusion
Subaxial cervical spine injuries represent nearly 3% of patients treated in the Department of Multipurpose Surgery of the University Hospital Center of Brazzaville. The most affected people in their thirties were males. Road accident is the primary cause. Prehospital care is not medicalized. The majority of trauma patients are admitted with a complete neurological deficit. The CT scan of the cervical spine is the main paraclinical examination and highlights the lesions with the most frequent luxation. Therapeutic care is delayed due to insufficient financial means for patients who do not have health insurance. The surgery consists of neural decompression, arthrodesis, and osteosynthesis, essentially by an anterior approach. The ongoing complications consisted of the development of pressure sores, followed by infections. The mortality rate is around 30%. The high frequency of complications is statistically linked to an unfavorable ASIA score (between A and B).
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Faculty of Health Sciences, Marien Ngouabi University, Brazzaville, Congo (Code: 0032/MESRSIT/DGRST/CERSSA/22). All ethical principles were considered in this article. The confidentiality of information was assured. Moreover, the cases were allowed to leave the study whenever they wished, and if desired, the results of the research would be available to them. The participants joined by phone were informed about the purpose of the research and its implementation stages. Informed consent was obtained from them.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Methodology, data collection and redaction: Hugues Brieux Ekouele Mbaki and Ruben Ange Florice Loko; Critical reading and data analysis: Rel Gerald Boukaka Kala, Sinclair Brice Kinata Bambino, Olivier Brice Ngackosso and Léon Boukassa; Conceptualization and design: Hugues Brieux Ekouele Mbaki and Ruben Ange Florice Lok; Data collection: Hugues Brieux Ekouele Mbaki and Ruben Ange Florice Loko; Data analysis and interpretation: Rel Gerald Boukaka Kala, Sinclair Brice Kinata Bambino, Olivier Brice Ngackosso and Léon Boukassa; Writing–original draft, writing–review, editing and Final approving: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
Thanks to Dr. Mbou Essie Darius and Dr. Bingui Outman Diogene for their contribution to the statistical processing of the data.
References
- GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: A systematic analysis for the global burden of disease study 2016. The Lancet. Neurology. 2019; 18(1):56-87. [DOI:10.1016/S1474-4422(18)30415-0] [PMID]
- Jackson AB, Dijkers M, Devivo MJ, Poczatek RB. A demographic profile of new traumatic spinal cord injuries: Change and stability over 30 years. Archives of Physical Medicine and Rehabilitation. 2004; 85(11):1740-8. [DOI:10.1016/j.apmr.2004.04.035] [PMID]
- DeVivo MJ, Rutt RD, Black KJ, Go BK, Stover SL. Trends in spinal cord injury demographics and treatment outcomes between 1973 and 1986. Archives of Physical Medicine and Rehabilitation. 1992; 73(5):424-30. [Link]
- Thiam AB, Ba MC. [Challenge of the management of severe trauma of cervical spine in sub-developed country (French)]. Neurochirurgie. 2013; 59(3):111-4. [DOI:10.1016/j.neuchi.2013.04.008] [PMID]
- Ekouele Mbaki HB, Boukassa L, Ngackosso OB, Kinata Bambino SB, Elombila M, Moyikoua R. [Prise en charge Hospitalière des Traumatismes du Rachis Cervical à Brazzaville (French)]. Health Sciences and Disease. 2017; 18(1):43-7. [Link]
- Bello F, Oumarou H, Nchufor R, Lekane Tsafack A, Mbele Messanga G, Dongmo Tchemeza A, et al. [Aspects diagnostiques, thérapeutiques et pronostiques des traumatismes du rachis à Yaoundé (French)]. Health Sciences and Disease. 2020; 21(12):59-62. [Link]
- Fehlings MG, Vaccaro A, Wilson JR, Singh A, Cadotte D, Harrop JS, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: Results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS One. 2012; 7(2):e32037. [DOI:10.1371/journal.pone.0032037] [PMID]
- Furlan JC, Noonan V, Cadotte DW, Fehlings MG. Timing of decompressive surgery of spinal cord after traumatic spinal cord injury: An evidence-based examination of pre-clinical and clinical studies. Journal of Neurotrauma. 2011; 28(8):1371-99. [DOI:10.1089/neu.2009.1147] [PMID]
- Loembe PM, Akoure-Davin S, Mwanyombet-Ompounga L, Koumba J, Assengone-Zeh Y, Kouna P, et al. [Fractures et luxations du rachis cervical inferieur (C3-C7) Attitudes thérapeutiques au Gabon (French)]. Médecine d'Afrique Noire. 1998; 45(11):630-32. [Link]
- Kasimatis GB, Panagiotopoulos E, Gliatis J, Tyllianakis M, Zouboulis P, Lambiris E. Complications of anterior surgery in cervical spine trauma: An overview. Clinical Neurology and Neurosurgery. 2009; 111(1):18-27. [DOI:10.1016/j.clineuro.2008.07.009] [PMID]
- Gelb DE, Aarabi B, Dhall SS, Hurlbert RJ, Rozzelle CJ, Ryken TC, et al. Treatment of subaxial cervical spinal injuries. Neurosurgery. 2013; 72(2):187-94. [DOI:10.1227/NEU.0b013e318276f637]
- Lambiris E, Kasimatis GB, Tyllianakis M, Zouboulis P, Panagiotopoulos E. Treatment of unstable lower cervical spine injuries by anterior instrumented fusion alone. Journal of Spinal Disorders & Techniques. 2008; 21(7):500-7.[DOI:10.1097/BSD.0b013e3181583b56] [PMID]
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |