Thu, Nov 6, 2025
Volume 10 - Continuous Publishing
Iran J Neurosurg 2024, 10 - Continuous Publishing: 64-75 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Parambil R M, Thavara B D, Jose B V, Sasi P, Maniyan R, Cholakkal S et al . Transcranial Extraventricular Endoscopic Surgeries: Expanding the Role of Endoscope in Neurosurgery. Iran J Neurosurg 2024; 10 : 7
URL: http://irjns.org/article-1-410-en.html
URL: http://irjns.org/article-1-410-en.html
Rajeev Mandaka Parambil1 

 , Binoy Damodar Thavara *2
, Binoy Damodar Thavara *2 

 , Byjo Valiyaveetil Jose1
, Byjo Valiyaveetil Jose1 

 , Premkumar Sasi1
, Premkumar Sasi1 

 , Radhakrishnan Maniyan1
, Radhakrishnan Maniyan1 

 , Shanavas Cholakkal1
, Shanavas Cholakkal1 

 , Shinas Hussain1
, Shinas Hussain1 




 , Binoy Damodar Thavara *2
, Binoy Damodar Thavara *2 

 , Byjo Valiyaveetil Jose1
, Byjo Valiyaveetil Jose1 

 , Premkumar Sasi1
, Premkumar Sasi1 

 , Radhakrishnan Maniyan1
, Radhakrishnan Maniyan1 

 , Shanavas Cholakkal1
, Shanavas Cholakkal1 

 , Shinas Hussain1
, Shinas Hussain1 


1- Department of Neurosurgery, Government Medical College, Kozhikode, India.
2- Department of Neurosurgery, Government Medical College, Kozhikode, India. ,drbinoytd@gmail.com
2- Department of Neurosurgery, Government Medical College, Kozhikode, India. ,
Keywords: Endoscope, Extraventricular, Microvascular decompression, Transcranial, Trigeminal neuralgia
Full Text [PDF 5809 kb]
(693 Downloads)
| Abstract (HTML) (3098 Views)
4. Discussion
The endoscope helps with in-depth perception, tactile sensation, and maneuverability. It provides an angled view and can access small regions. The disadvantage includes blood obscuring the field. Its use is limited to some procedures only [2]. To improve navigation during interventions in the posterior fossa, endoscopic-assisted techniques with surgical corridors have been described. The pineal region was accessed through a supracerebellar infratentorial approach and the CPA region was accessed through a retrosigmoid approach [3].
The utilization of the endoscope in MVD allows for unparalleled panoramic views and illumination of the neurovascular structures. The endoscope can be used as an adjunct to the microscope in MVD surgery. It has a wide field of view compared to the microscope. It allows for less brain retraction and reduces the morbidity for the patient [4]. Matmusaev et al. [5], performed an endoscopic MVD for an 83-year-old female patient with HFS. The offending vessel anterior inferior cerebellar artery (AICA) was successfully decompressed. No surgery-related complications occurred and there were excellent outcomes with the complete resolution of HFS immediately after the operation. Endoscopic surgery can provide a more panoramic surgical view than conventional microscopic surgery. However, it has a learning curve and is technically challenging [5]. Authors have performed 6 MVDs using an endoscope.
Surgical approaches to pineal lesions present a challenge because of limited visibility and maneuverability within the posterior fossa. Shahrestani et al. [6], used a pure endoscopic supracerebellar infratentorial approach for pineal tumors. They noted that this approach is a safe and effective approach for deep-seated pineal lesions. It allows for visibility and maneuverability around the lesion and facilitates high rates of gross total resection (GTR) [6]. The authors noted that the pineal tumor was well visualized when the endoscope was navigated to the deep narrow corridor of the pineal region. The great cerebral vein and the brainstem were visualized and hence were protected while excising the tumor.
CP angle and prepontine epidermoid tumors grow along the subarachnoid spaces around the neurovascular structures. Chowdhury et al. [7] performed a similar case by pure endoscopic visualization through a retrosigmoid retromastoid lateral suboccipital approach. The epidermoid tumor was removed nearly totally using a 0-degree endoscope. The petrosal vein and trigeminal nerve were completely freed. Visualization provided by the endoscope is outstanding and this advantage can minimize the risk of morbidity to vital neurovascular structures [7].
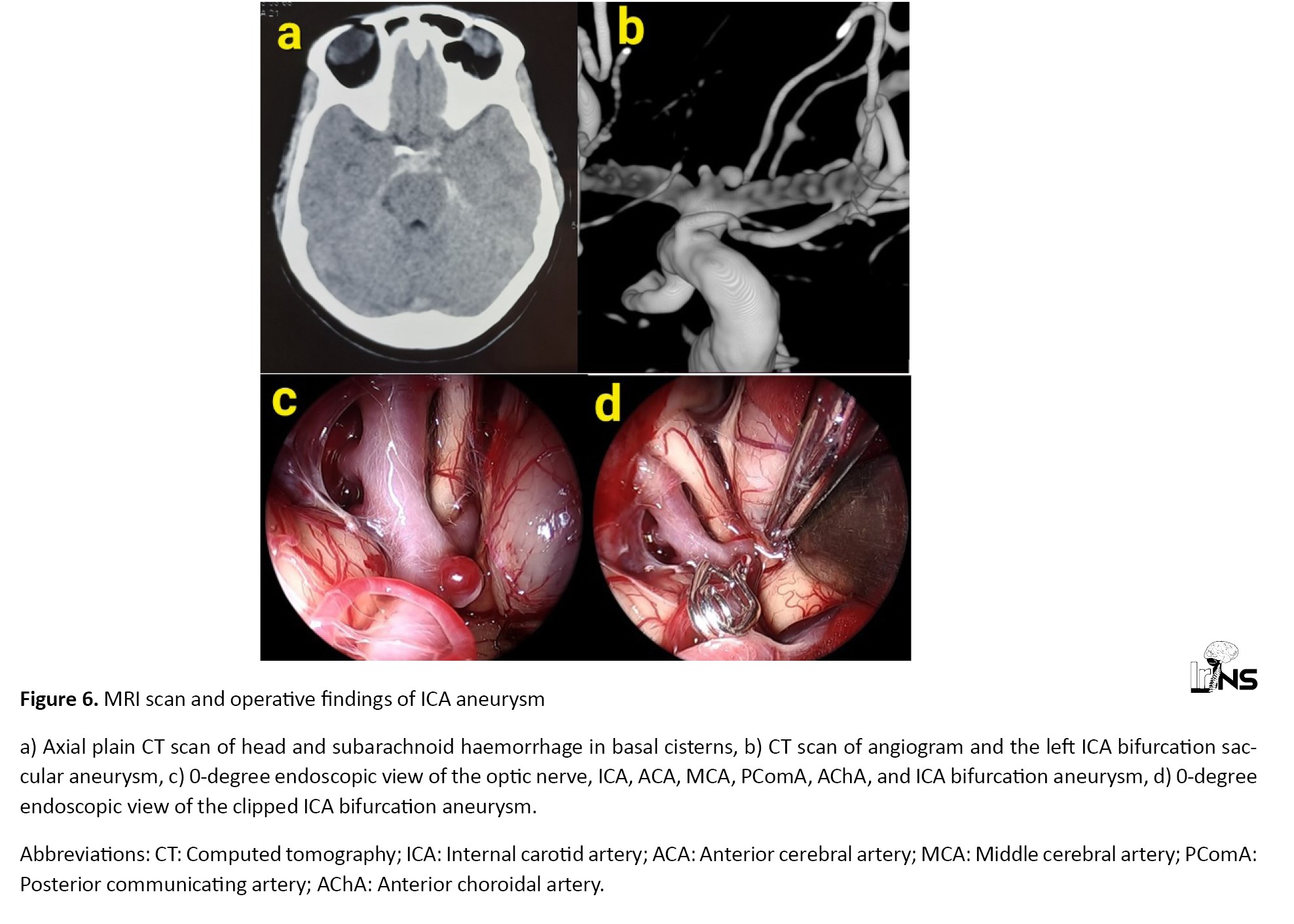
Cai et al., clipped a posterior communicating artery aneurysm using a transcranial neuroendoscopic approach. Transcranial endoscopic clipping of aneurysm is very rare [8]. In transcranial aneurysm surgery, the endoscope can carry out a supportive role in planning surgical maneuvers and in verifying whether clipping has been performed correctly or not. The 30-degree endoscope can view concealed areas without retraction. This prevents the possibility of the aneurysm being ruptured and also reduces the use of temporary clips [9]. Authors have performed endoscopic assisted microscopic surgery to clip ICA bifurcation aneurysm.
Wu et al. [10], performed an endoscopic transcranial transdiaphragmatic approach for giant pituitary adenomas with suprasellar extension. They noted that this approach can be efficiently and safely performed for maximal excision of tumor [10]. The authors used an endoscopic subfrontal approach for suprasellar craniopharyngiomas. They were able to delineate the vital neurovascular structures clearly and the tumor was separated from them. The tumor in the third ventricular area was not visualized in the microscope, but easily visualized through the inter-optic window on using an endoscope. This eliminated the need for a translamina terminalis approach. Hence with minimal dissection, an endoscope helped in craniopharyngioma excision.
One drawback of an endoscope is the intracranial blind area between the field lens of the endoscope and the site of the dural opening. This blind area cannot be viewed on the endoscopic monitor, and accidental intracranial neurovascular structural injury can occur in this area [11].
Authors noted that only a few centers are using an endoscope for transcranial extraventricular regions, and many of them are performing endoscopic surgery for one pathology only. A single center performing TEES for a wide range of pathologies in different areas of the brain as described by the authors is rare. The training in various TEES will improve hand-eye coordination and improve adaptability to the endoscopic monitor during transcranial surgeries. This will decrease the training necessity for the neurosurgeons who are shifting from microscope to exoscope. Authors believe that it is very important to train neurosurgeons in TEES because of its wide applications.
5. Conclusion
Endoscopic magnified close vision of the deeper extraventricular structures helps in decreasing the damage to vital structures and enhances the surgical result. TEES is very beneficial for operating on deep-seated lesions like the pineal region, CP angle region, and suprasellar region. In aneurysm surgery, it helps to preserve the vessels around the aneurysm and also helps to confirm the completeness of clipping. The endoscope is used as a complementary to the microscope to access the microscopic invisible areas. TEES improves hand-eye coordination in transcranial surgeries which helps in adapting to exoscope easily.
Limitations
This is a retrospective study. A smaller number of cases is the limitation of the study.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Institutional Ethical Committee of Government Medical College (Code: GMCKKD/RP2023/IEC/155). Appropriate consent was obtained from the patients whose clinical details are described in the illustrative cases.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Binoy Damodar Thavara; Data collection: Binoy Damodar Thavara, Shanavas Cholakkal, Shinas Hussain and Radhakrishnan Maniyan; Data analysis and interpretation: Binoy Damodar Thavara, Byjo Valiyaveetil Jose; Drafting the article: Binoy Damodar Thavara, Rajeev Mandaka Parambil and Prem Kumar Sasi; Supervision, review and editing: Rajeev Mandaka Parambil and Binoy Damodar Thavara; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors gratefully acknowledge the support of the Department of Neurosurgery, Government Medical College, Kozhikode, India.
Full Text: (737 Views)
1. Introduction
Technologies are developing in neurosurgery for better visualization of surgical fields. Better vision will in turn improve surgical results. Majority of the brain surgeries are done using a microscope. The use of exoscope is a recent development in this area. Transcranial endoscopic usage is limited mainly to intraventricular lesions. Endoscopic use in extraventricular regions of the brain is not much developed due to a lack of endoscopic training and a lack of awareness of endoscopic use. The authors have taken a step ahead and used endoscopes for a wide range of transcranial surgeries other than ventricular surgeries.
Virani et al., used an endoscope to visualize vascular loops in trigeminal neuralgia (TN) and hemifacial spasm (HFS) and also to search small cerebellopontine (CP) angle lesions [1]. Authors have used endoscope by transcranial route for performing pineal tumor excision, microvascular decompression (MVD), cerebellopontine angle (CPA) lesion excision, craniopharyngioma excision, and internal carotid artery (ICA) bifurcation aneurysm clipping. The authors have analyzed the benefits of endoscopes in transcranial extraventricular surgeries.
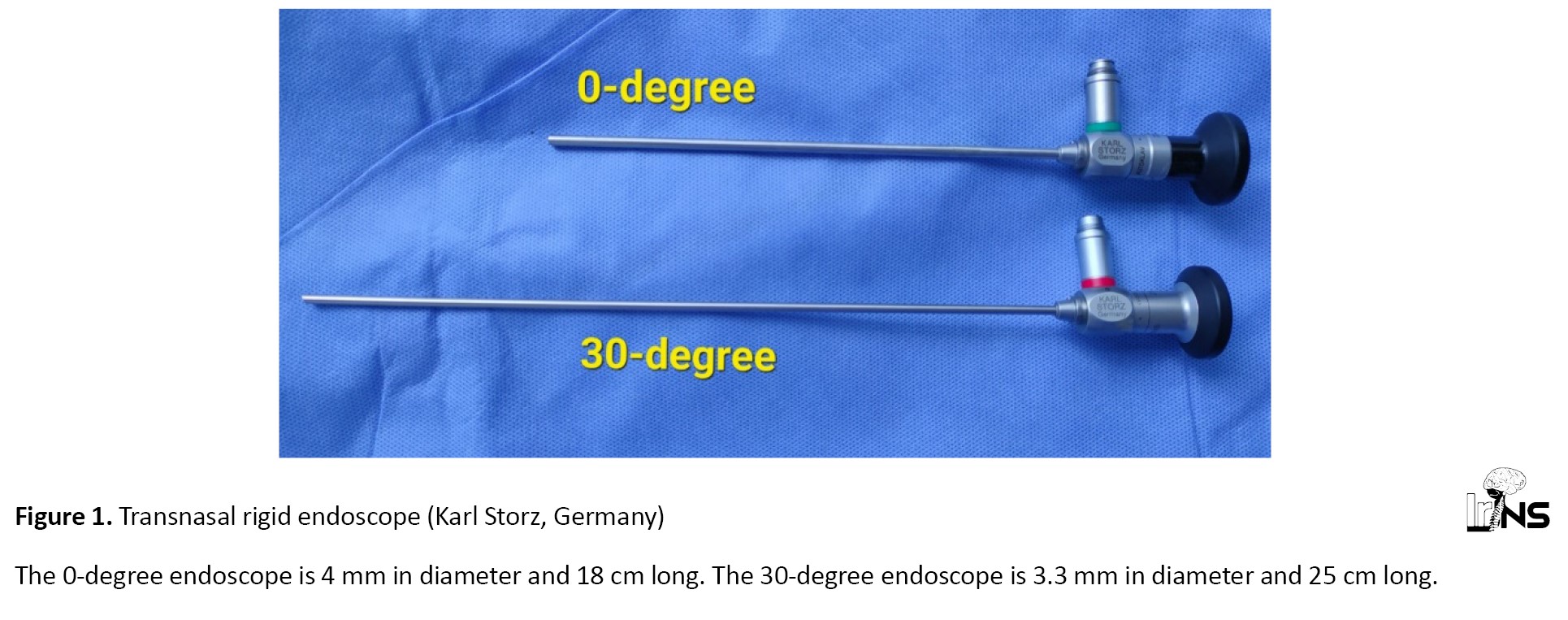
2. Methods and Materials/Patients
This is a retrospective study of transcranial extraventricular endoscopic surgeries (TEESs) operated between June 2022 to May 2023 (1 year) in the Department of Neurosurgery. The aim was to study the benefits of the endoscope in transcranial extraventricular surgeries. The authors described the surgeries done for brain lesions other than intraventricular lesions as extraventricular surgeries. Access to the intracranial region was obtained through craniotomy or craniectomy which is called transcranial approach. The transnasal rigid endoscope (Karl Storz, Germany) was used for the surgeries (Figure 1).
Technologies are developing in neurosurgery for better visualization of surgical fields. Better vision will in turn improve surgical results. Majority of the brain surgeries are done using a microscope. The use of exoscope is a recent development in this area. Transcranial endoscopic usage is limited mainly to intraventricular lesions. Endoscopic use in extraventricular regions of the brain is not much developed due to a lack of endoscopic training and a lack of awareness of endoscopic use. The authors have taken a step ahead and used endoscopes for a wide range of transcranial surgeries other than ventricular surgeries.
Virani et al., used an endoscope to visualize vascular loops in trigeminal neuralgia (TN) and hemifacial spasm (HFS) and also to search small cerebellopontine (CP) angle lesions [1]. Authors have used endoscope by transcranial route for performing pineal tumor excision, microvascular decompression (MVD), cerebellopontine angle (CPA) lesion excision, craniopharyngioma excision, and internal carotid artery (ICA) bifurcation aneurysm clipping. The authors have analyzed the benefits of endoscopes in transcranial extraventricular surgeries.
2. Methods and Materials/Patients
This is a retrospective study of transcranial extraventricular endoscopic surgeries (TEESs) operated between June 2022 to May 2023 (1 year) in the Department of Neurosurgery. The aim was to study the benefits of the endoscope in transcranial extraventricular surgeries. The authors described the surgeries done for brain lesions other than intraventricular lesions as extraventricular surgeries. Access to the intracranial region was obtained through craniotomy or craniectomy which is called transcranial approach. The transnasal rigid endoscope (Karl Storz, Germany) was used for the surgeries (Figure 1).
A ventriculoscope was not used for surgeries. Endoscopic intraventricular and endoscopic transnasal surgeries were excluded from the study. The surgery was performed as either pure endoscopic surgery or endoscopic-assisted microscopic surgery. The endoscope was navigated inside the cranium to the site of the lesion during surgery. Statistical analysis was done using Epi info software. The data analyzed include age, sex, diagnosis, clinical features, duration of symptoms, computed tomography (CT), magnetic resonance imaging (MRI) finding, surgery performed, endoscope used (0-degree, 30-degree), pure endoscopic/endoscopic assisted microscopic surgery, surgical findings, benefits of the endoscope, post-operative status, and postoperative duration of stay in hospital.
3. Results
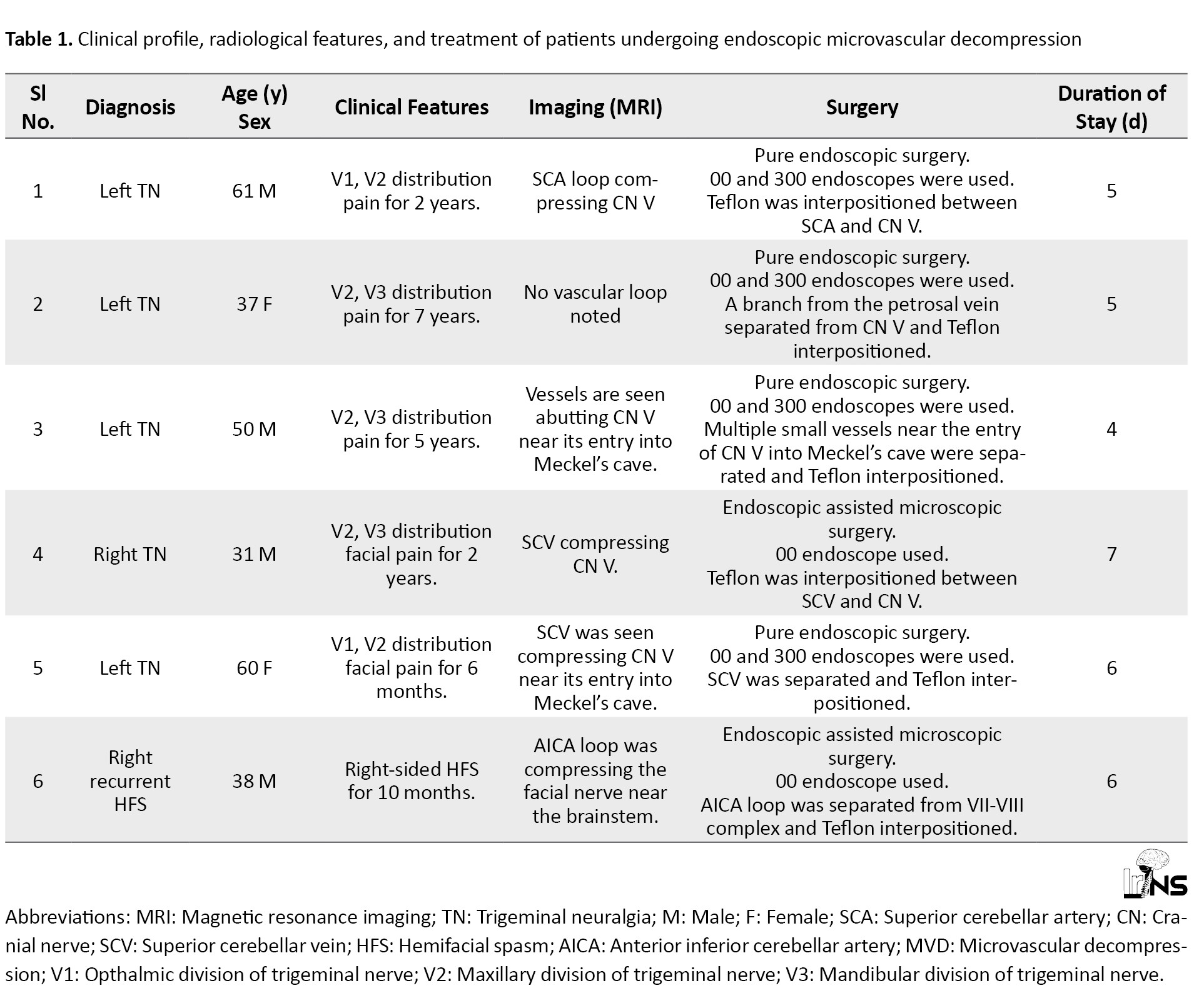
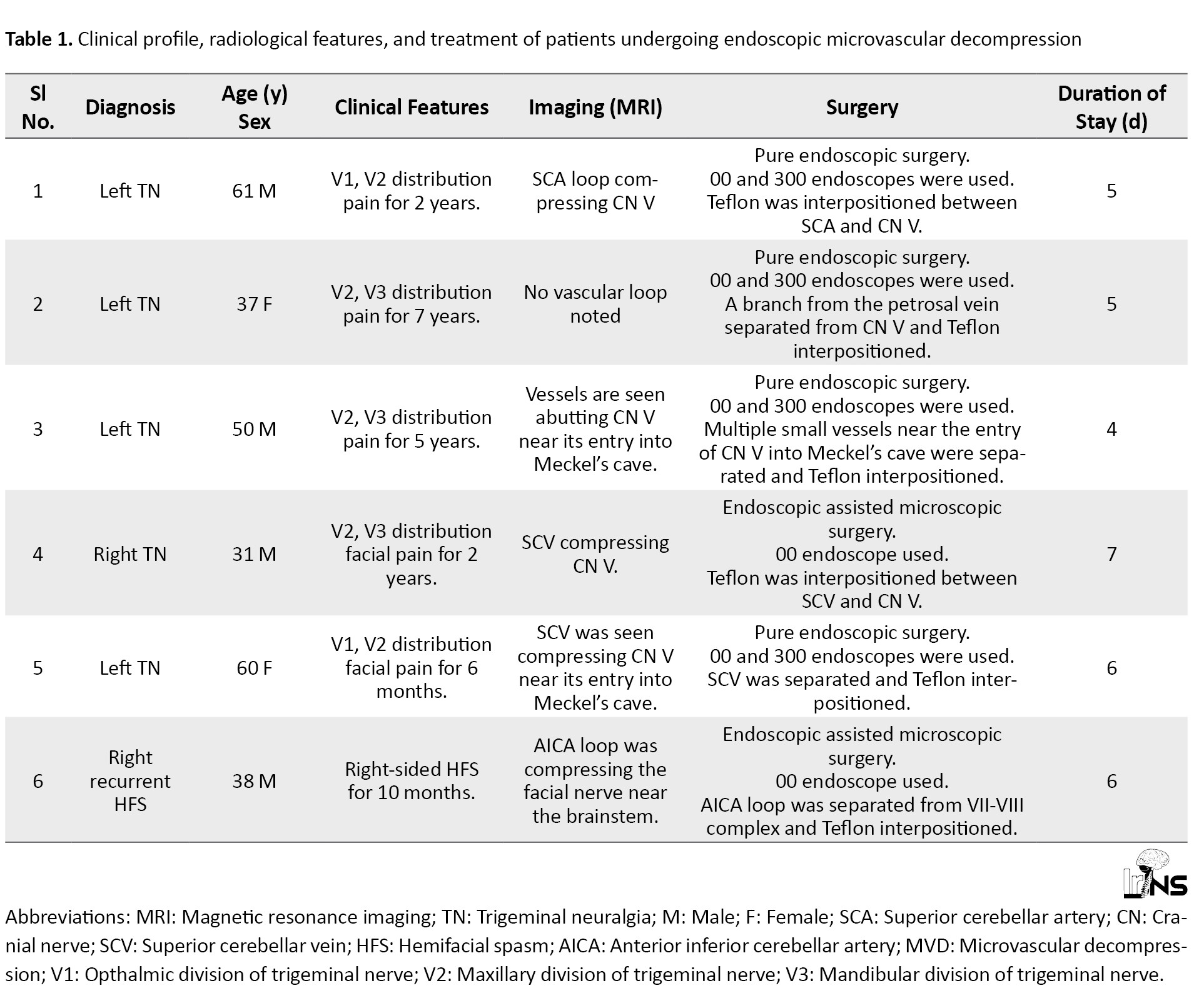
The authors have performed endoscopic MVDs for 5 cases of TN and one recurrent HFS by retrosigmoid retromastoid approach (Table 1).
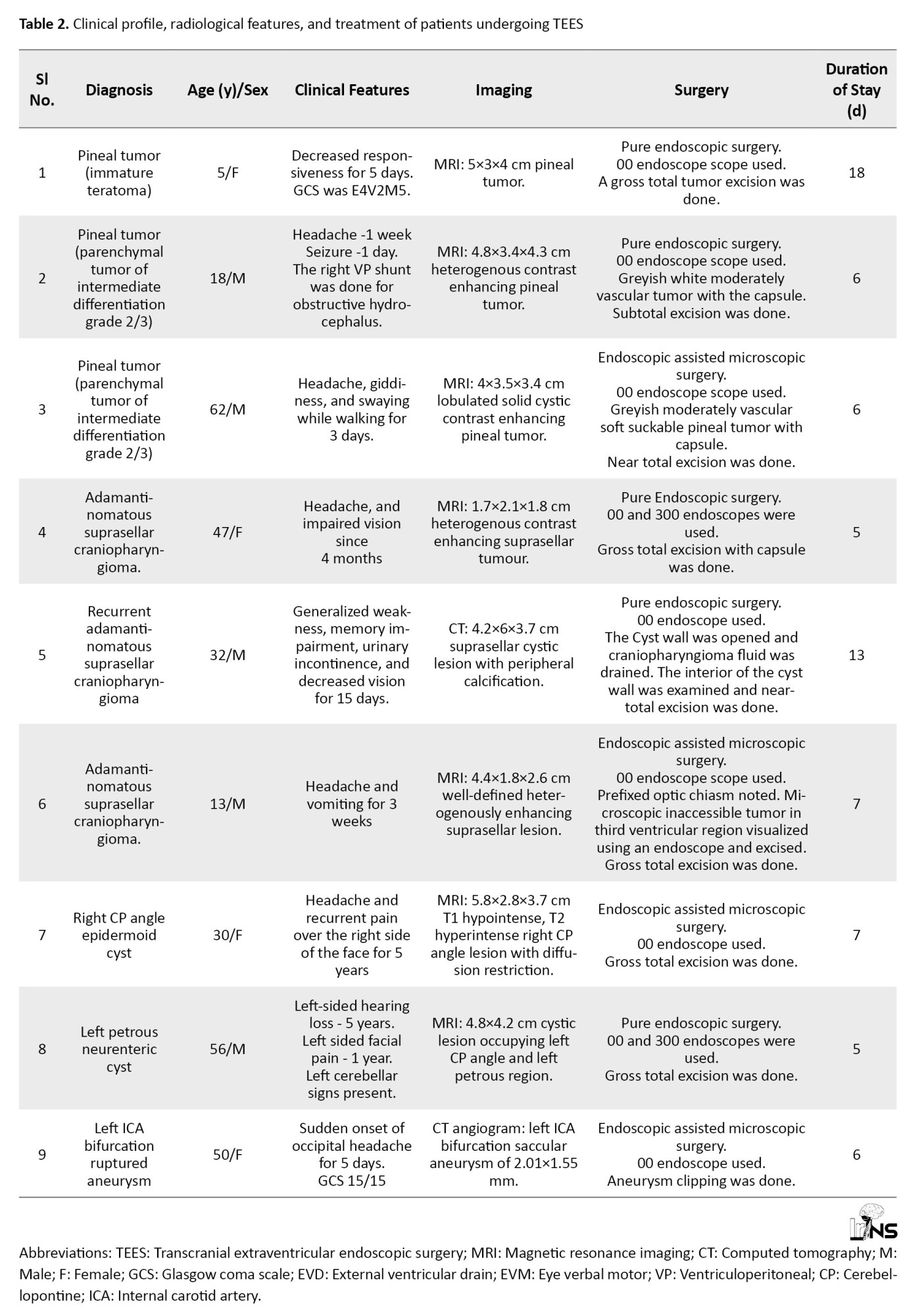
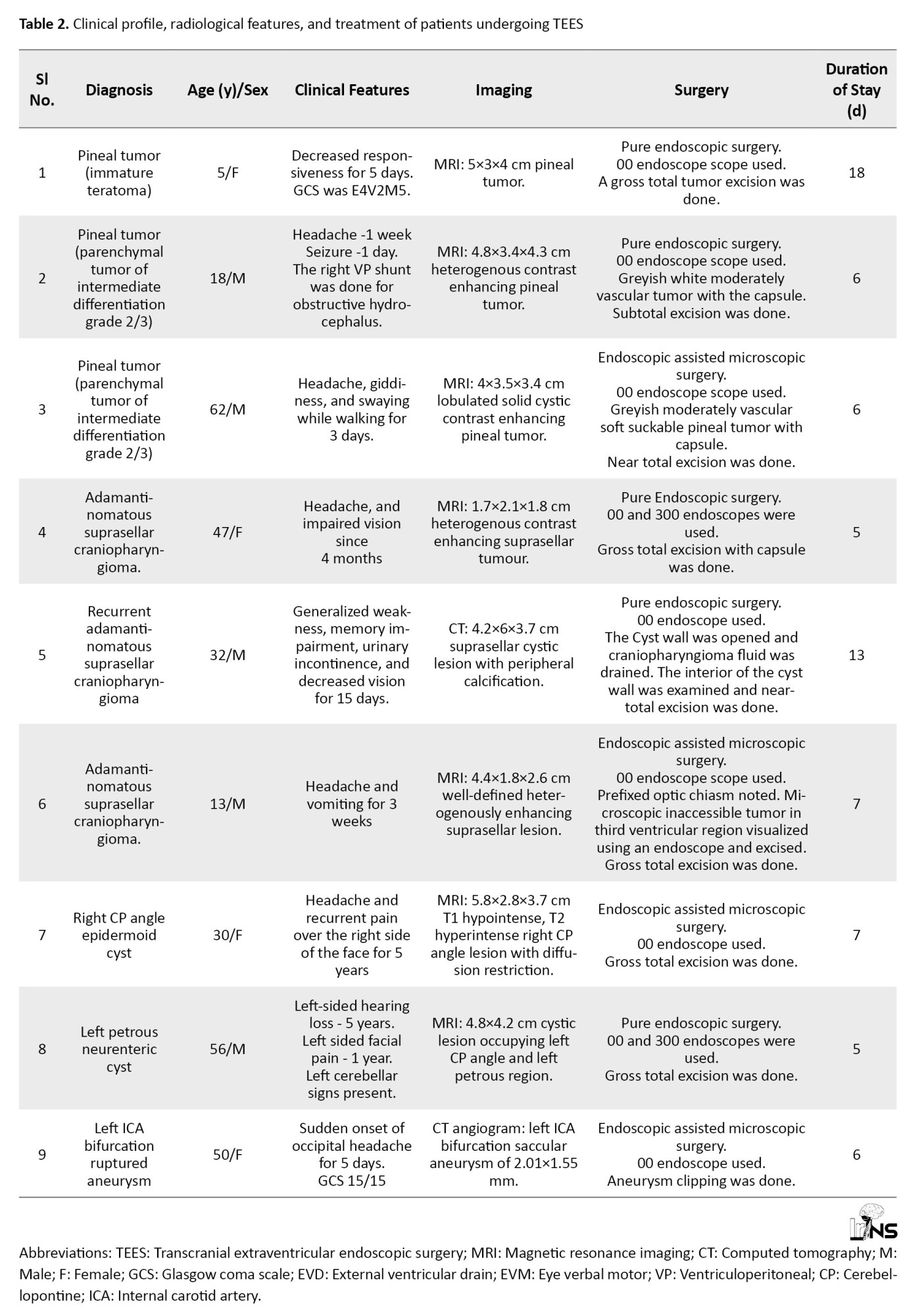
The endoscope was used for the excisions of 3 pineal tumors using the supracerebellar infratentorial approach and 3 suprasellar craniopharyngiomas using the right subfrontal approach. One CP angle epidermoid cyst and 1 petrous neurenteric cyst extending into the CP angle region underwent endoscopic surgery using a retrosigmoid retromastoid approach. One case of ruptured ICA bifurcation aneurysm underwent pterional craniotomy. The endoscope was used to delineate the vessels and the aneurysm was clipped. All the patients improved in the postoperative period (Table 2).
In endoscopic assisted microscopic MVD, the microscope was used only in the initial part of surgery till reaching the site of neurovascular conflict. The 0-degree endoscope was able to visualize CNs, neurovascular conflict, vertebrobasilar arteries, and the anterior surface of the brainstem under good magnification and illumination. All structures were seen in a panoramic view. The 30-degree endoscope was used to visualize the medial side of the CNs and its compression by the loop of vessels. The conflicting vessels were separated from the CN V in TN and CN VII in HFS and a Teflon patch was interpositioned between them to complete MVD (Table 1). Delineation of the neurovascular conflict was superior using an endoscope when compared to the author’s microscopic experience. There was no misinterpretation of structures. The authors were very much satisfied with the endoscopic vision and comfort of doing surgery using it.
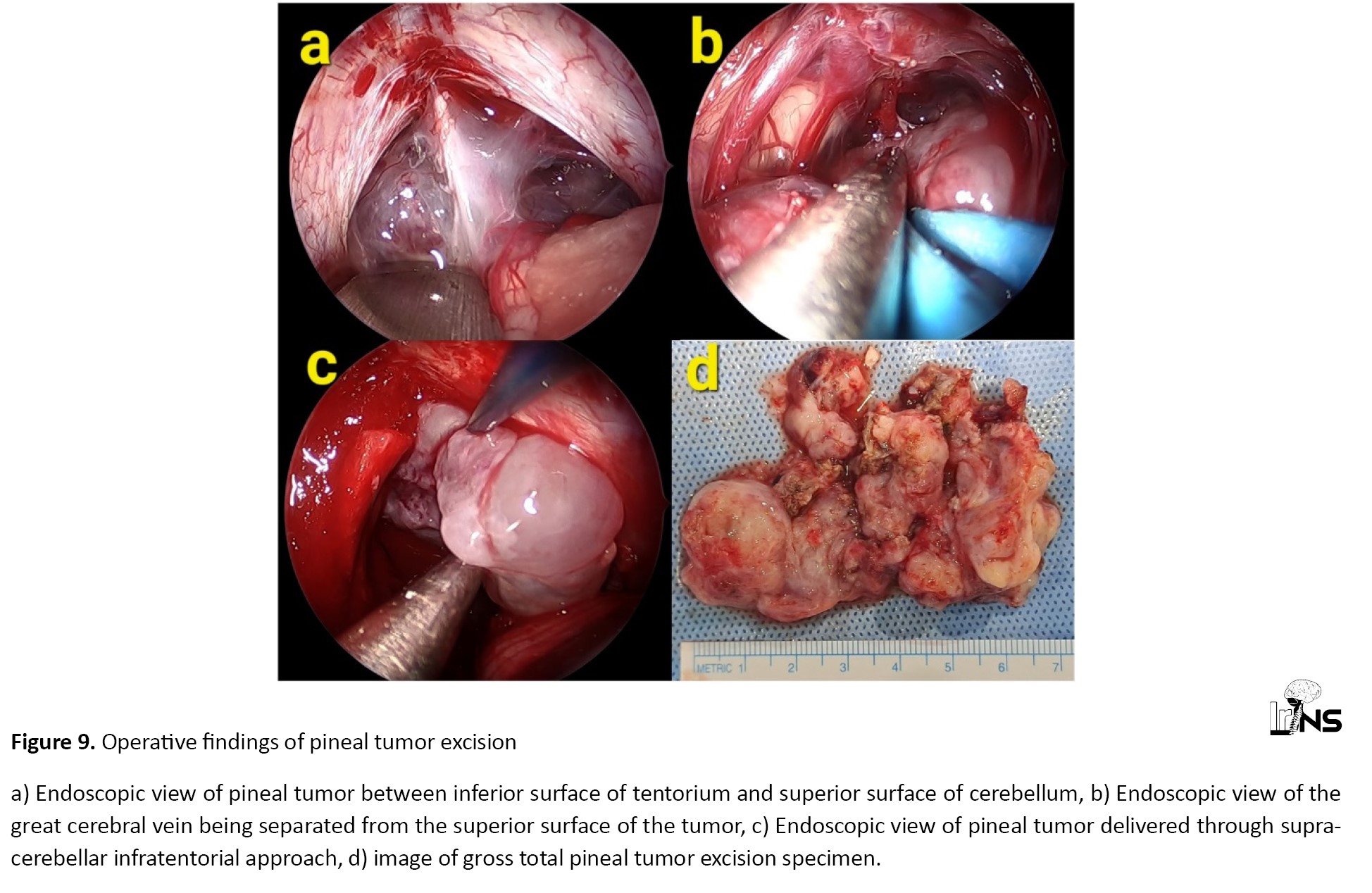
Pineal tumors were operated in left three-quarter prone positions. Midline suboccipital craniectomy was done and the tumor was reached using supracerebellar infratentorial approach. The endoscope was navigated to the superior surface of the pineal tumor and the great cerebral vein was visualized and separated. Inferiorly, the brainstem was seen clearly and the tumor was separated from it. The tumor was decompressed and the wall was excised. Since the endoscope was able to reach a deep narrow corridor of the pineal region, there was an excellent magnified vision with good illumination of the tumor, brainstem, and great cerebral vessels. The surgeon and assistants were able to stand in a neutral position during surgery. In endoscopic-assisted microscopic surgery, the microscope was used only during the initial part of surgery until the pineal region was reached.
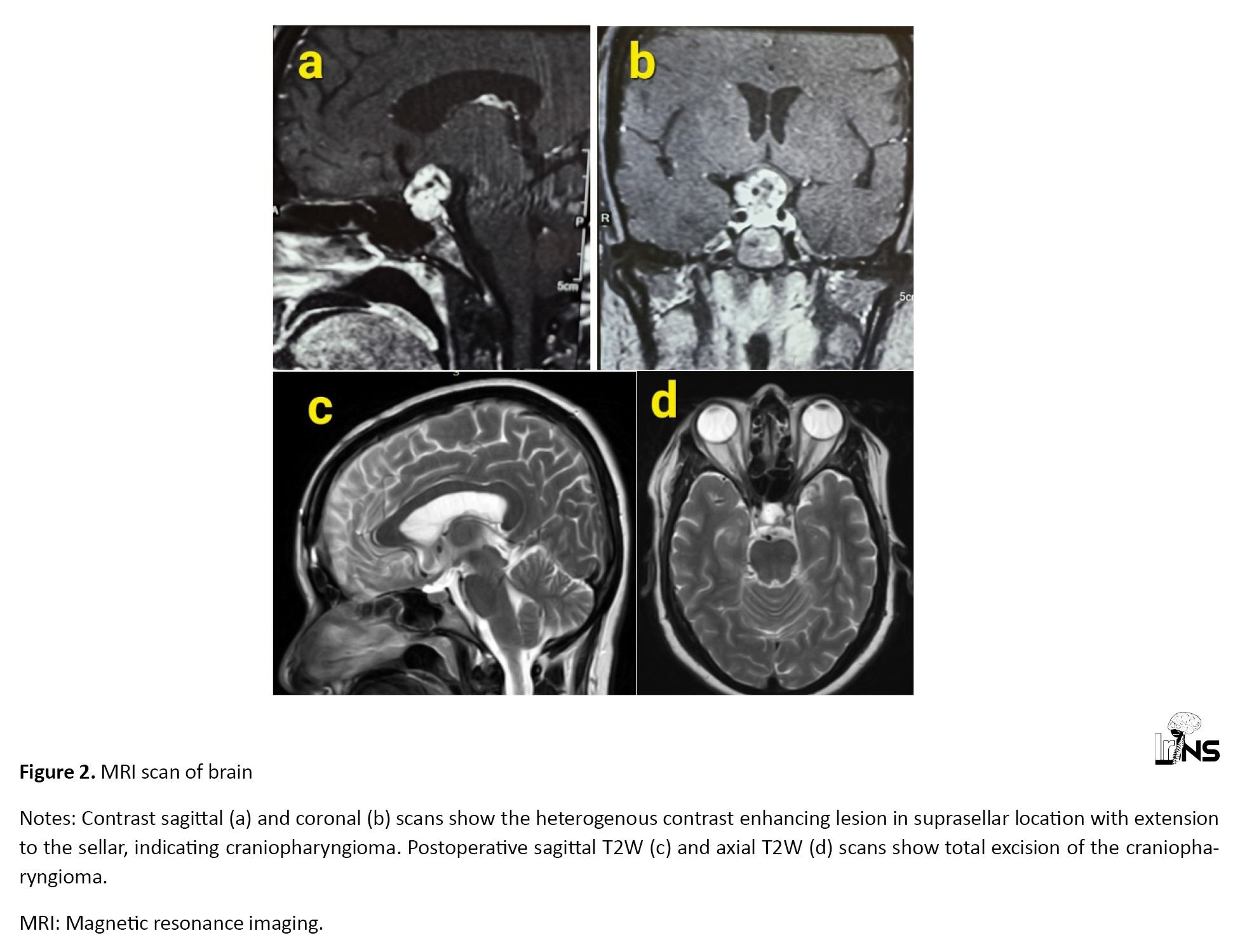
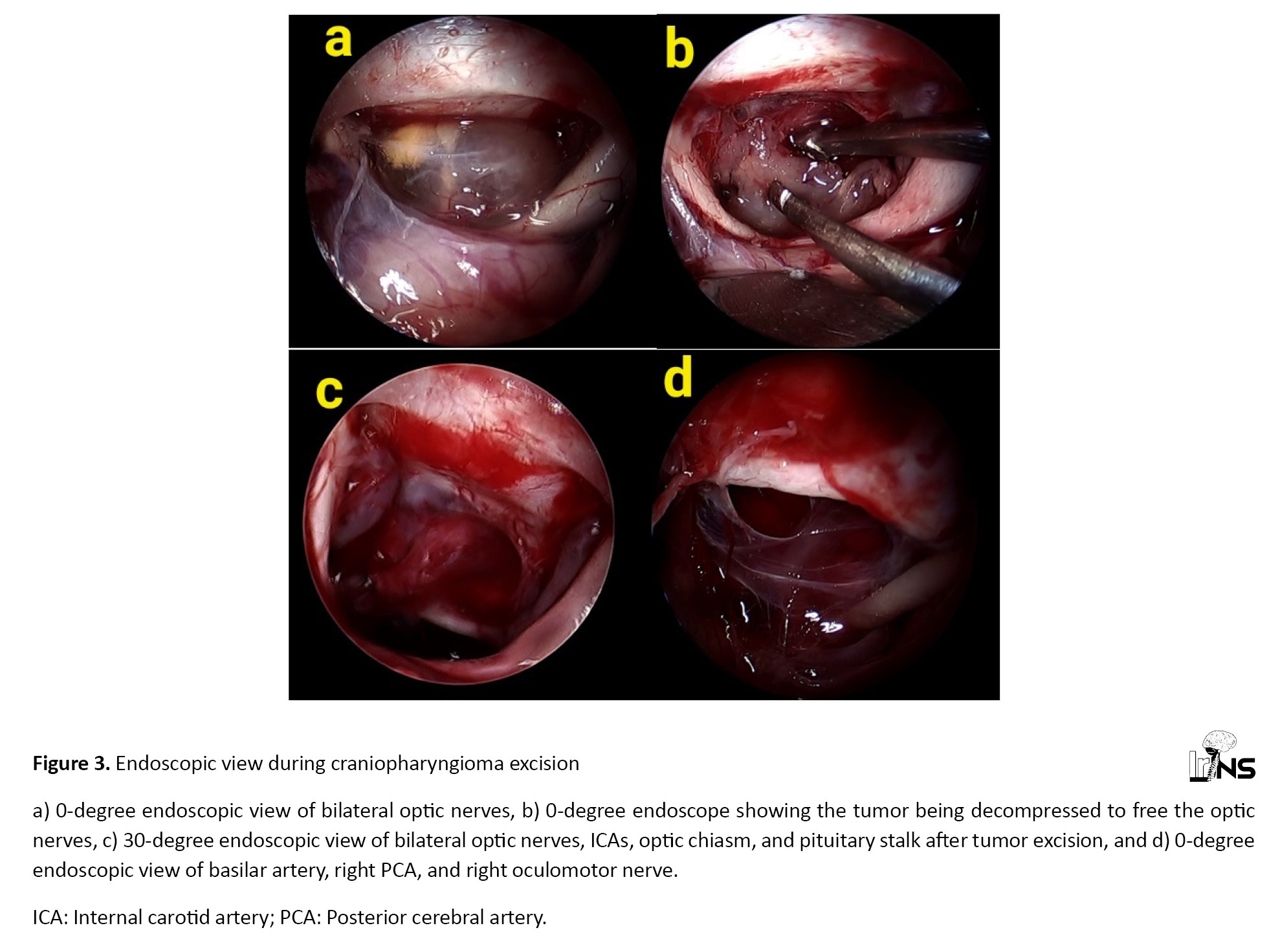
In craniopharyngioma excisions, the right suprabrow frontal craniotomy was done and the endoscope was navigated through a subfrontal approach to reach the tumor. The anatomy of the optic nerves, ICAs, and optic chiasm were visualized under good magnification which helped in an easy dissection of the tumor from these structures. The endoscope was navigated inside the tumor capsule to visualize its internal architecture and tumor excision was done (Figures 2 and 3).
3. Results
The authors have performed endoscopic MVDs for 5 cases of TN and one recurrent HFS by retrosigmoid retromastoid approach (Table 1).
The endoscope was used for the excisions of 3 pineal tumors using the supracerebellar infratentorial approach and 3 suprasellar craniopharyngiomas using the right subfrontal approach. One CP angle epidermoid cyst and 1 petrous neurenteric cyst extending into the CP angle region underwent endoscopic surgery using a retrosigmoid retromastoid approach. One case of ruptured ICA bifurcation aneurysm underwent pterional craniotomy. The endoscope was used to delineate the vessels and the aneurysm was clipped. All the patients improved in the postoperative period (Table 2).
In endoscopic assisted microscopic MVD, the microscope was used only in the initial part of surgery till reaching the site of neurovascular conflict. The 0-degree endoscope was able to visualize CNs, neurovascular conflict, vertebrobasilar arteries, and the anterior surface of the brainstem under good magnification and illumination. All structures were seen in a panoramic view. The 30-degree endoscope was used to visualize the medial side of the CNs and its compression by the loop of vessels. The conflicting vessels were separated from the CN V in TN and CN VII in HFS and a Teflon patch was interpositioned between them to complete MVD (Table 1). Delineation of the neurovascular conflict was superior using an endoscope when compared to the author’s microscopic experience. There was no misinterpretation of structures. The authors were very much satisfied with the endoscopic vision and comfort of doing surgery using it.
Pineal tumors were operated in left three-quarter prone positions. Midline suboccipital craniectomy was done and the tumor was reached using supracerebellar infratentorial approach. The endoscope was navigated to the superior surface of the pineal tumor and the great cerebral vein was visualized and separated. Inferiorly, the brainstem was seen clearly and the tumor was separated from it. The tumor was decompressed and the wall was excised. Since the endoscope was able to reach a deep narrow corridor of the pineal region, there was an excellent magnified vision with good illumination of the tumor, brainstem, and great cerebral vessels. The surgeon and assistants were able to stand in a neutral position during surgery. In endoscopic-assisted microscopic surgery, the microscope was used only during the initial part of surgery until the pineal region was reached.
In craniopharyngioma excisions, the right suprabrow frontal craniotomy was done and the endoscope was navigated through a subfrontal approach to reach the tumor. The anatomy of the optic nerves, ICAs, and optic chiasm were visualized under good magnification which helped in an easy dissection of the tumor from these structures. The endoscope was navigated inside the tumor capsule to visualize its internal architecture and tumor excision was done (Figures 2 and 3).
It was able to access the sellar region, third ventricular region, and the area behind the optic nerves which are difficult to visualize using the microscope. Superior extension of the tumor into the third ventricle was visualized through an inter-optic window and further dissection like the translamina terminalis approach was avoided.
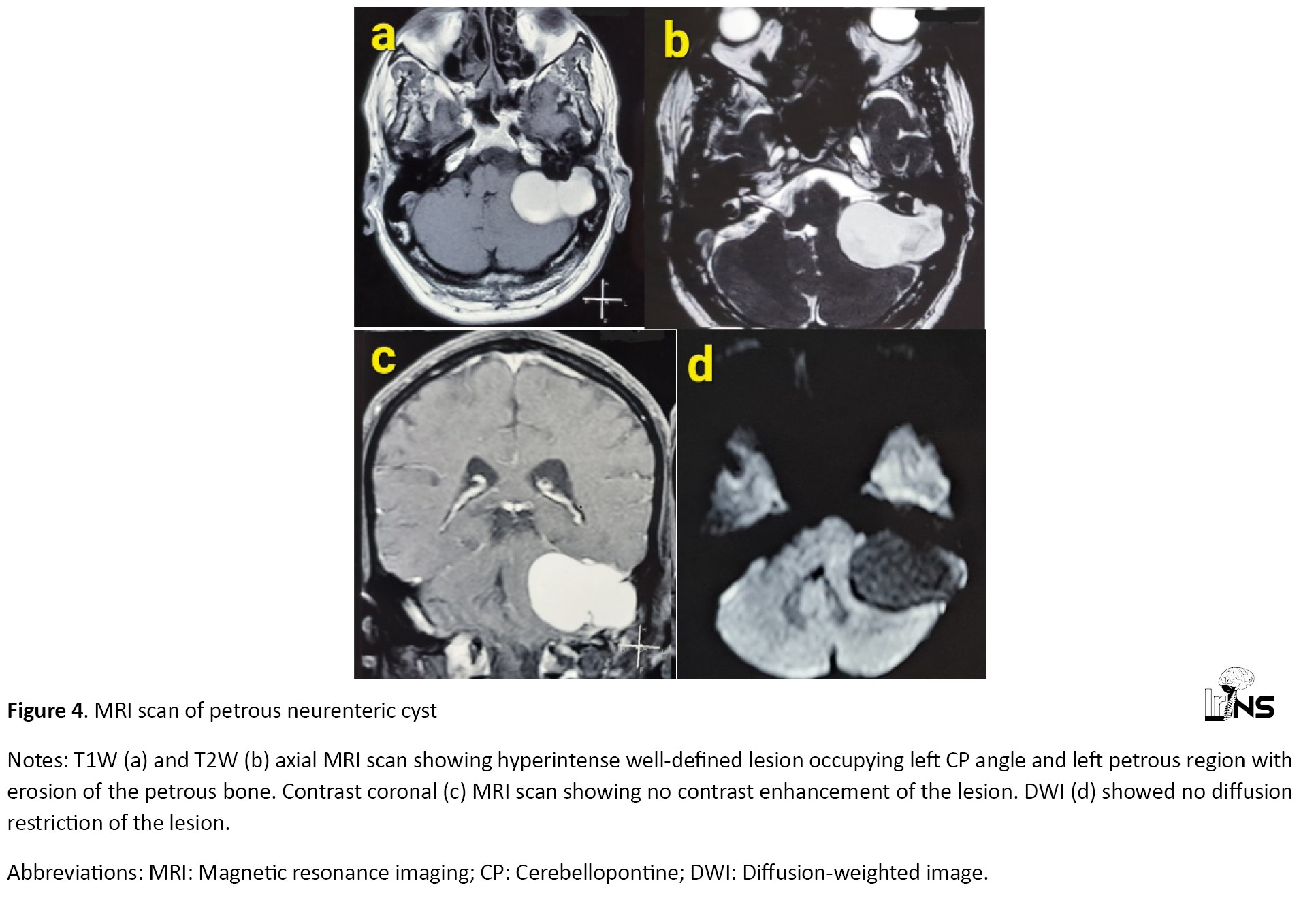
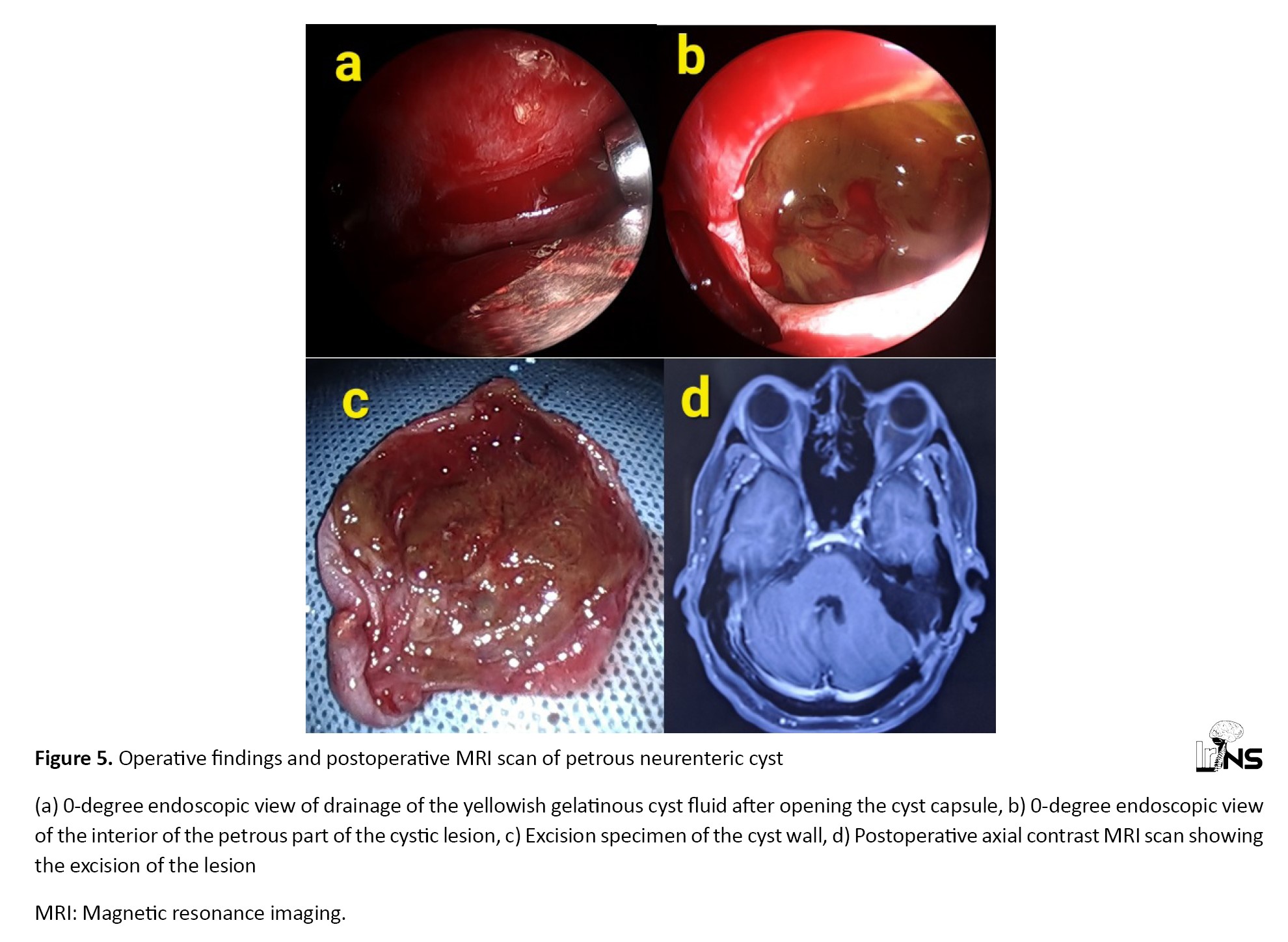
One case of CP angle epidermoid was operated using endoscopic assisted microscopic surgery. The major part of the epidermoid was removed using the microscope. However, part of the epidermoid in the medial and superior aspect of CN V was not under direct vision of the microscope. The 0-degree endoscope was navigated to these inaccessible areas and the epidermoid was removed. One petrous neurenteric cyst extending into the CP angle cistern was operated using an endoscope (Figure 4).
One case of CP angle epidermoid was operated using endoscopic assisted microscopic surgery. The major part of the epidermoid was removed using the microscope. However, part of the epidermoid in the medial and superior aspect of CN V was not under direct vision of the microscope. The 0-degree endoscope was navigated to these inaccessible areas and the epidermoid was removed. One petrous neurenteric cyst extending into the CP angle cistern was operated using an endoscope (Figure 4).
The 0-degree endoscope was able to enter the cyst wall inside the eroded petrous bone and yellowish gelatinous cyst fluid was drained. Inaccessible areas inside the eroded petrous bone were accessed using a 30-degree endoscope. Cyst wall was excised (Figure 5).
One case of a ruptured ICA bifurcation aneurysm was operated by pterional craniotomy. The sylvian fissure was split using the microscope. The 0-degree endoscope showed a magnified panoramic view of the optic nerve, ICA, anterior cerebral artery (ACA), middle cerebral artery (MCA), and ICA bifurcation aneurysm. Posterior communicating artery (PCom) and anterior choroidal artery (AChA) were also visualized. The endoscope visualized all around the aneurysm and clipping of the aneurysm was done safely (Figure 6).
The patient recovered in the postoperative period (Table 2).
Technical points
The authors have performed surgery using 4 hand technique in which one neurosurgeon holds and navigates the endoscope and another neurosurgeon performs surgery. Both neurosurgeons should be trained in using endoscopes to better perform these surgeries. Since the endoscope was navigated inside the cranium, there are chances of injury to vital structures. Certain techniques were used to prevent such injuries. It was navigated in and out longitudinally during the surgery. The horizontal movement was avoided when the endoscope was in a deeper location. It was placed away from the brain to prevent injury to vital structures. In the CP region, it was navigated along the petrous bone. In the pineal region, it was navigated along the tentorium, and in the suprasellar region, it was navigated along the anterior skull base. Surgical instruments were inserted only with endoscopic guidance. Surgeries were done mainly using a 0-degree scope. It was easy to navigate in and out. Higher-degree endoscopes are difficult to navigate because of their side-viewing vision. The 30-degree scope was used to visualize behind the obstructing anatomical structure and also to visualize sides and corners. The endoscope occupies extra space in the operating field and obstructs the instruments. But this was overcome by placing endoscopes and instruments at different angles. There was blood staining of the endoscopic lens and obstruction of vision. This was overcome by placing the endoscope a little away from the bleeding site and also by irrigating it with saline during surgery. The lens can also be cleared by wiping its surface. The authors noted that the difficulties of endoscopic surgeries can be overcome by operating more cases.
Benefits of endoscope
The endoscope was easily able to reach deep narrow corridors like the pineal region, CP angle region, and suprasellar region. Deep structures were visualized clearly with good illumination and magnification. There was no loss of endoscopic illumination on superficial unwanted areas. Hence less dissection was required to delineate the structures. There was no misinterpretation of structures. Surgeons were able to stand in a neutral position while doing the surgery. This has increased the ease of doing surgery, decreased complications, and improved the surgical result.
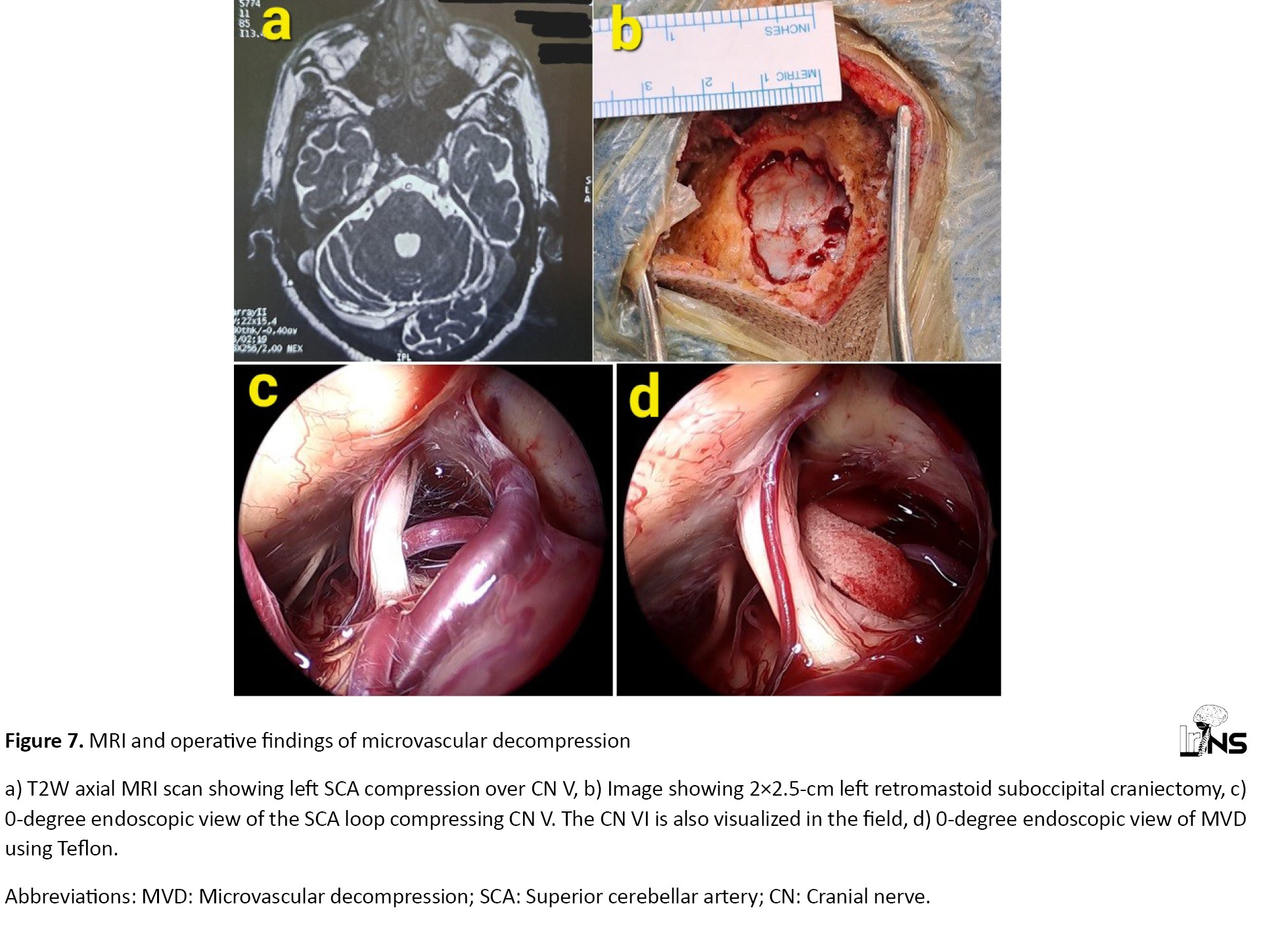
Illustrative case – microvascular decompression
A 61-year-old male diabetic patient presented with left-sided TN for the last 2 years (Table 1). MRI scan showed the neurovascular conflict between the superior cerebellar artery (SCA) loop and CN V (Figure 7).
Technical points
The authors have performed surgery using 4 hand technique in which one neurosurgeon holds and navigates the endoscope and another neurosurgeon performs surgery. Both neurosurgeons should be trained in using endoscopes to better perform these surgeries. Since the endoscope was navigated inside the cranium, there are chances of injury to vital structures. Certain techniques were used to prevent such injuries. It was navigated in and out longitudinally during the surgery. The horizontal movement was avoided when the endoscope was in a deeper location. It was placed away from the brain to prevent injury to vital structures. In the CP region, it was navigated along the petrous bone. In the pineal region, it was navigated along the tentorium, and in the suprasellar region, it was navigated along the anterior skull base. Surgical instruments were inserted only with endoscopic guidance. Surgeries were done mainly using a 0-degree scope. It was easy to navigate in and out. Higher-degree endoscopes are difficult to navigate because of their side-viewing vision. The 30-degree scope was used to visualize behind the obstructing anatomical structure and also to visualize sides and corners. The endoscope occupies extra space in the operating field and obstructs the instruments. But this was overcome by placing endoscopes and instruments at different angles. There was blood staining of the endoscopic lens and obstruction of vision. This was overcome by placing the endoscope a little away from the bleeding site and also by irrigating it with saline during surgery. The lens can also be cleared by wiping its surface. The authors noted that the difficulties of endoscopic surgeries can be overcome by operating more cases.
Benefits of endoscope
The endoscope was easily able to reach deep narrow corridors like the pineal region, CP angle region, and suprasellar region. Deep structures were visualized clearly with good illumination and magnification. There was no loss of endoscopic illumination on superficial unwanted areas. Hence less dissection was required to delineate the structures. There was no misinterpretation of structures. Surgeons were able to stand in a neutral position while doing the surgery. This has increased the ease of doing surgery, decreased complications, and improved the surgical result.
Illustrative case – microvascular decompression
A 61-year-old male diabetic patient presented with left-sided TN for the last 2 years (Table 1). MRI scan showed the neurovascular conflict between the superior cerebellar artery (SCA) loop and CN V (Figure 7).
Retromastoid craniectomy was done near the transverse-sigmoid sinus junction. The 0-degree endoscope showed a loop of left SCA compressing and displacing the CN V anterolaterally. A 30-degree endoscope showed structures medial to CN V and also the entry of CN V into Meckel’s cave. The vessel loop was separated medially from CN V and a Teflon patch was interpositioned between them to complete MVD. The patient was relieved of TN.
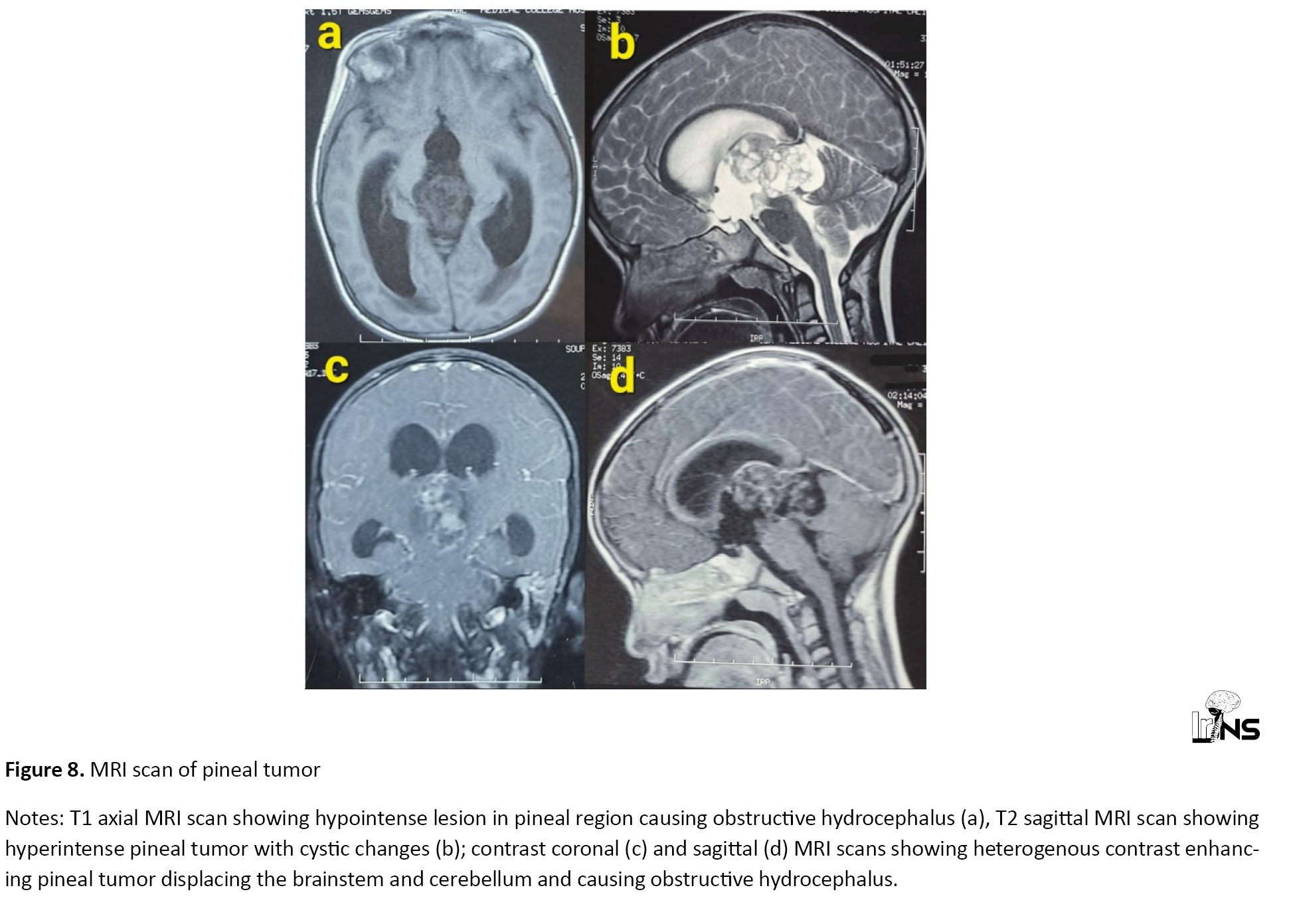
Illustrative case - pineal tumor
A 5-year-old female child was presented with reduced responsiveness with a Glasgow coma scale (GCS) score of E4V2M5 (E: Eye, V: Verbal, M: Motor). MRI scan revealed a 5x3x4 cm heterogenous contrast-enhancing pineal tumor with obstructive hydrocephalus (Figure 8).
Illustrative case - pineal tumor
A 5-year-old female child was presented with reduced responsiveness with a Glasgow coma scale (GCS) score of E4V2M5 (E: Eye, V: Verbal, M: Motor). MRI scan revealed a 5x3x4 cm heterogenous contrast-enhancing pineal tumor with obstructive hydrocephalus (Figure 8).
Magnetic resonance (MR) angiogram and MR venogram were normal. External ventricular drain (EVD) was inserted into the right frontal horn to drain cerebrospinal fluid (CSF) and the patient was taken up for surgical excision of pineal tumor. The tumor was reached using a supracerebellar infratentorial approach. Zero-degree endoscope showed an excellent view of the pineal tumor. Internal decompression of greyish red, moderately vascular lobulated pineal tumor was done. The tumor was separated from the great cerebral vein superiorly and the brainstem inferiorly. Capsule was reflected all around and gross total excision was done (Figure 9).
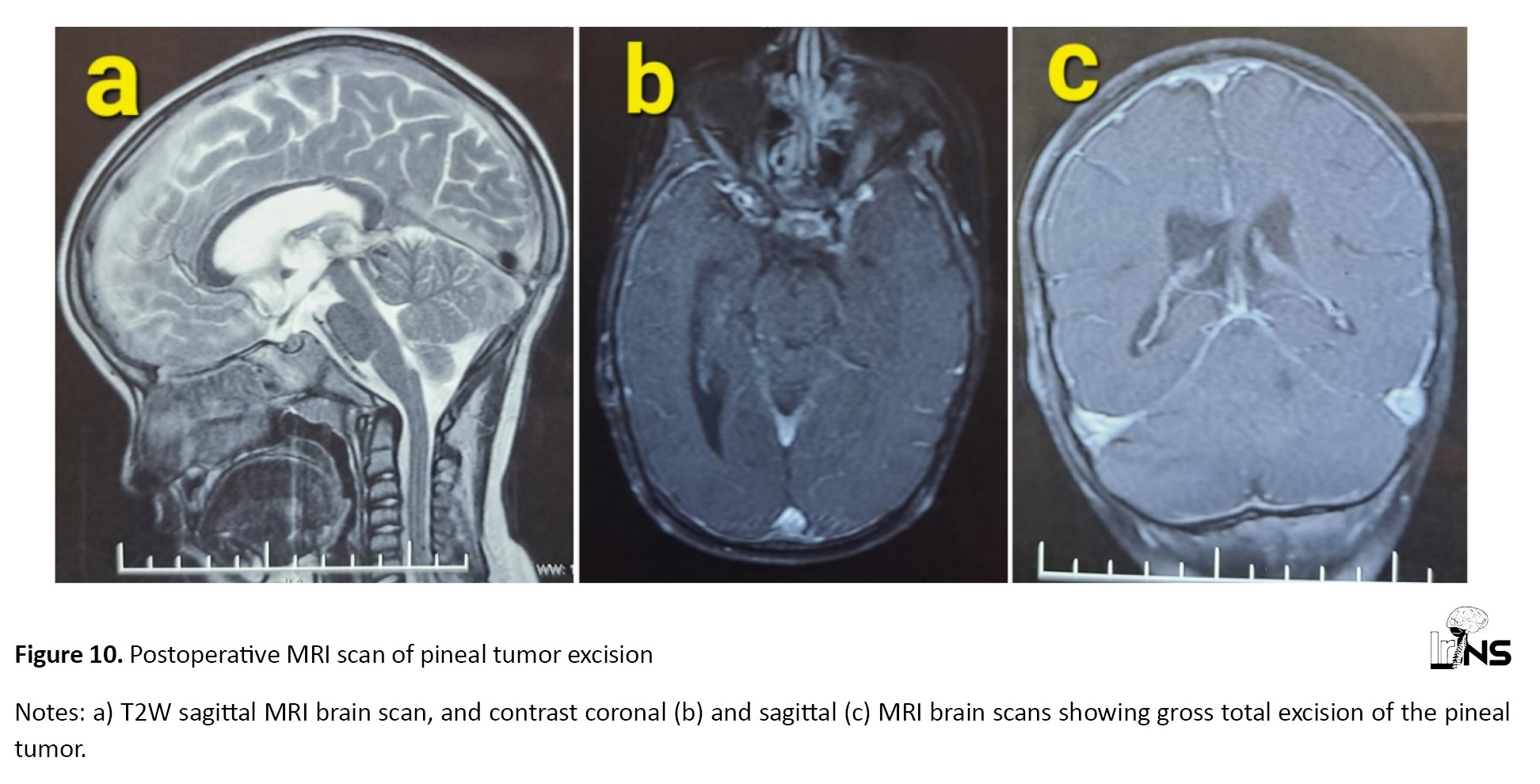
EVD was removed in the postoperative period and the patient recovered well with a GCS score of 15/15 (Table 2). Postoperative MRI showed gross total excision of the tumor (Figure 10).
4. Discussion
The endoscope helps with in-depth perception, tactile sensation, and maneuverability. It provides an angled view and can access small regions. The disadvantage includes blood obscuring the field. Its use is limited to some procedures only [2]. To improve navigation during interventions in the posterior fossa, endoscopic-assisted techniques with surgical corridors have been described. The pineal region was accessed through a supracerebellar infratentorial approach and the CPA region was accessed through a retrosigmoid approach [3].
The utilization of the endoscope in MVD allows for unparalleled panoramic views and illumination of the neurovascular structures. The endoscope can be used as an adjunct to the microscope in MVD surgery. It has a wide field of view compared to the microscope. It allows for less brain retraction and reduces the morbidity for the patient [4]. Matmusaev et al. [5], performed an endoscopic MVD for an 83-year-old female patient with HFS. The offending vessel anterior inferior cerebellar artery (AICA) was successfully decompressed. No surgery-related complications occurred and there were excellent outcomes with the complete resolution of HFS immediately after the operation. Endoscopic surgery can provide a more panoramic surgical view than conventional microscopic surgery. However, it has a learning curve and is technically challenging [5]. Authors have performed 6 MVDs using an endoscope.
Surgical approaches to pineal lesions present a challenge because of limited visibility and maneuverability within the posterior fossa. Shahrestani et al. [6], used a pure endoscopic supracerebellar infratentorial approach for pineal tumors. They noted that this approach is a safe and effective approach for deep-seated pineal lesions. It allows for visibility and maneuverability around the lesion and facilitates high rates of gross total resection (GTR) [6]. The authors noted that the pineal tumor was well visualized when the endoscope was navigated to the deep narrow corridor of the pineal region. The great cerebral vein and the brainstem were visualized and hence were protected while excising the tumor.
CP angle and prepontine epidermoid tumors grow along the subarachnoid spaces around the neurovascular structures. Chowdhury et al. [7] performed a similar case by pure endoscopic visualization through a retrosigmoid retromastoid lateral suboccipital approach. The epidermoid tumor was removed nearly totally using a 0-degree endoscope. The petrosal vein and trigeminal nerve were completely freed. Visualization provided by the endoscope is outstanding and this advantage can minimize the risk of morbidity to vital neurovascular structures [7].
Cai et al., clipped a posterior communicating artery aneurysm using a transcranial neuroendoscopic approach. Transcranial endoscopic clipping of aneurysm is very rare [8]. In transcranial aneurysm surgery, the endoscope can carry out a supportive role in planning surgical maneuvers and in verifying whether clipping has been performed correctly or not. The 30-degree endoscope can view concealed areas without retraction. This prevents the possibility of the aneurysm being ruptured and also reduces the use of temporary clips [9]. Authors have performed endoscopic assisted microscopic surgery to clip ICA bifurcation aneurysm.
Wu et al. [10], performed an endoscopic transcranial transdiaphragmatic approach for giant pituitary adenomas with suprasellar extension. They noted that this approach can be efficiently and safely performed for maximal excision of tumor [10]. The authors used an endoscopic subfrontal approach for suprasellar craniopharyngiomas. They were able to delineate the vital neurovascular structures clearly and the tumor was separated from them. The tumor in the third ventricular area was not visualized in the microscope, but easily visualized through the inter-optic window on using an endoscope. This eliminated the need for a translamina terminalis approach. Hence with minimal dissection, an endoscope helped in craniopharyngioma excision.
One drawback of an endoscope is the intracranial blind area between the field lens of the endoscope and the site of the dural opening. This blind area cannot be viewed on the endoscopic monitor, and accidental intracranial neurovascular structural injury can occur in this area [11].
Authors noted that only a few centers are using an endoscope for transcranial extraventricular regions, and many of them are performing endoscopic surgery for one pathology only. A single center performing TEES for a wide range of pathologies in different areas of the brain as described by the authors is rare. The training in various TEES will improve hand-eye coordination and improve adaptability to the endoscopic monitor during transcranial surgeries. This will decrease the training necessity for the neurosurgeons who are shifting from microscope to exoscope. Authors believe that it is very important to train neurosurgeons in TEES because of its wide applications.
5. Conclusion
Endoscopic magnified close vision of the deeper extraventricular structures helps in decreasing the damage to vital structures and enhances the surgical result. TEES is very beneficial for operating on deep-seated lesions like the pineal region, CP angle region, and suprasellar region. In aneurysm surgery, it helps to preserve the vessels around the aneurysm and also helps to confirm the completeness of clipping. The endoscope is used as a complementary to the microscope to access the microscopic invisible areas. TEES improves hand-eye coordination in transcranial surgeries which helps in adapting to exoscope easily.
Limitations
This is a retrospective study. A smaller number of cases is the limitation of the study.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Institutional Ethical Committee of Government Medical College (Code: GMCKKD/RP2023/IEC/155). Appropriate consent was obtained from the patients whose clinical details are described in the illustrative cases.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Binoy Damodar Thavara; Data collection: Binoy Damodar Thavara, Shanavas Cholakkal, Shinas Hussain and Radhakrishnan Maniyan; Data analysis and interpretation: Binoy Damodar Thavara, Byjo Valiyaveetil Jose; Drafting the article: Binoy Damodar Thavara, Rajeev Mandaka Parambil and Prem Kumar Sasi; Supervision, review and editing: Rajeev Mandaka Parambil and Binoy Damodar Thavara; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors gratefully acknowledge the support of the Department of Neurosurgery, Government Medical College, Kozhikode, India.
References
- Virani MJ, Palande DA, Katikar DB, Chopra IS, Trivedi NP. Video endoscopic neurosurgery (VENS): A prospective study of 55 patients. Neurology India. 1998; 46(1):54-65. [PMID]
- Panchal S, Yamada Y, Nagatani T, Watanabe T, Kishida Y, Sayah A, et al. A practice survey to compare and identify the usefulness of neuroendoscope and exoscope in the current neurosurgery practice. Asian Journal of Neurosurgery. 2020; 15(3):601-7. [DOI:10.4103/ajns.AJNS_339_19] [PMID]
- Ries Centeno T, Villamil F, Marco Del Pont F, Giovannini S, Caffaratti G, Cervio A. Posterior fossa endoscopic-assisted surgery: A systematization of its surgical corridors. Neurochirurgie. 2022; 68(1):21-8. [DOI:10.1016/j.neuchi.2021.07.001] [PMID]
- Piazza M, Lee JY. Endoscopic and microscopic microvascular decompression. Neurosurgery Clinics of North America. 2016; 27(3):305-13. [DOI:10.1016/j.nec.2016.02.008] [PMID]
- Matmusaev M, Kumar RS, Yamada Y, Nagatani T, Kawase T, Tanaka R, et al. Endoscopic microvascular decompression for hemifacial spasm. Asian Journal of Neurosurgery. 2020; 15(4):833-8. [DOI:10.4103/ajns.AJNS_152_20] [PMID]
- Shahrestani S, Ravi V, Strickland B, Rutkowski M, Zada G. Pure endoscopic supracerebellar infratentorial approach to the pineal region: A case series. World Neurosurgery. 2020; 137:e603-9. [DOI:10.1016/j.wneu.2020.02.074] [PMID]
- Chowdhury FH, Haque MR. Endoscopic assisted microsurgical removal of cerebello-pontine angle and prepontine epidermoid. Journal of Neurosciences in Rural Practice. 2012; 3(3):414-9. [DOI:10.4103/0976-3147.102647] [PMID]
- Cai Q, Guo Q, Zhang W, Ji B, Chen Z, Chen Q. Extradural anterior clinoidectomy and aneurysm clipping using transcranial neuroendoscopic approach: A case report. Medicine (Baltimore). 2019; 98(17):e15288. [DOI:10.1097/MD.0000000000015288] [PMID]
- Profeta G, De Falco R, Ambrosio G, Profeta L. Endoscope-assisted microneurosurgery for anterior circulation aneurysms using the angle-type rigid endoscope over a 3-year period. Child's Nervous System. 2004; 20(11-12):811-5. [DOI:10.1007/s00381-004-0935-1] [PMID]
- Wu X, Bao Z, Tian W, Wang J, Miao Z, Wang Q, et al. Endoscopic transcranial transdiaphragmatic approach in a single-stage surgery for giant pituitary adenomas. Frontiers in Oncology. 2023; 13:1133861. [DOI:10.3389/fonc.2023.1133861] [PMID]
- Nagata Y, Watanabe T, Nagatani T, Takeuchi K, Chu J, Wakabayashi T. The multiscope technique for microvascular decompression. World Neurosurgery. 2017; 103:310-4. [DOI:10.1016/j.wneu.2017.04.059] [PMID]
Type of Study: Research |
Subject:
Skull Base
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |