Thu, Jul 31, 2025
Volume 11 - Continuous Publishing
Iran J Neurosurg 2025, 11 - Continuous Publishing: 1-9 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Parsa E, Ilaghi M, Reihani-Kermani H. Comparison of Intrathecal Morphine and Fentanyl in Postoperative Pain Management of Spine Surgeries: A Randomized Double-blind Clinical Trial. Iran J Neurosurg 2025; 11 : 1
URL: http://irjns.org/article-1-425-en.html
URL: http://irjns.org/article-1-425-en.html
1- Department of Neurosurgery, Kerman University of Medical Sciences, Kerman, Iran.
2- Kerman Neuroscience Research Center, Institute of Neuropharmacology, Kerman, Iran.
3- Department of Neurosurgery, Kerman University of Medical Sciences, Kerman, Iran. ,h_reihani@hotmail.com
2- Kerman Neuroscience Research Center, Institute of Neuropharmacology, Kerman, Iran.
3- Department of Neurosurgery, Kerman University of Medical Sciences, Kerman, Iran. ,
Full Text [PDF 1175 kb]
(399 Downloads)
| Abstract (HTML) (1079 Views)
Full Text: (380 Views)
1. Introduction
Spine surgery is a complex and invasive procedure often leading to considerable postoperative pain, which can significantly impact patients’ recovery and overall satisfaction [1]. Adequate pain management after spinal surgery is crucial to ensure optimal patient outcomes, early mobilization, and smooth transition to rehabilitation [2, 3]. Among various analgesic strategies, the use of intrathecal opioids has gained prominence due to its effectiveness in providing extended pain relief. Intrathecal morphine and fentanyl are commonly employed opioids in spinal anesthesia [4, 5], but their comparative efficacy in reducing postoperative pain remains a subject of debate.
Morphine is a prototypical opioid analgesic that acts mainly on mu-opioid receptors in the central nervous system [6]. It exerts its analgesic effects by binding to these receptors, inhibiting the release of a neurotransmitter known as substance P, thereby diminishing pain perception [7]. Morphine’s potency and efficacy stem from its high affinity for mu-opioid receptors, allowing for robust pain relief. Additionally, it exhibits other pharmacological actions, such as sedation, respiratory depression, and suppression of cough reflexes [8, 9].
In contrast, fentanyl is a highly potent opioid characterized by its swift onset and brief duration of effect [10]. It also acts primarily on mu-opioid receptors, producing analgesia by inhibiting neurotransmitter release. Fentanyl is highly lipophilic, allowing it to rapidly penetrate the blood-brain barrier, resulting in a rapid onset of analgesia [11].
Several factors contribute to select a specific opioid for intrathecal administration, including potency, duration of action, side-effect profile, and patient-specific characteristics. Although both intrathecal morphine and fentanyl have demonstrated efficacy in managing postoperative pain in various types of surgeries [5, 12, 13], there is limited direct comparative data on their effectiveness and safety in the context of spinal surgery.
The primary objective of this clinical trial is to compare the efficacy of intrathecal morphine and fentanyl in reducing postoperative pain intensity after spinal surgery. This study aims to improve pain management protocols, reduce opioid consumption, enhance patient comfort, and accelerate recovery in this surgical population.
2. Methods and Materials
This study was designed, conducted, and reported by the Consolidated Standards of Reporting Trials (CONSORT) 2010 guidelines to ensure transparency and comprehensive reporting of the study methodology and results [14].
Trial design
This study was a randomized parallel double-blind trial conducted to compare the efficacy of intrathecal morphine and fentanyl in reducing pain following spinal surgery. We hypothesized that intrathecal morphine would be more effective for postoperative pain control in spinal surgery. The study was conducted between October 2022 and April 2023 at the Neurospine Surgery Department of Shahid Bahonar Hospital, the main referral neurospine center in Kerman City, southeast Iran. The study protocol was reviewed and approved by the Institutional Ethics Committee of the Kerman University of Medical Sciences, before participant recruitment. This study adhered to the ethical guidelines outlined by the World Medical Association, as stated in the Declaration of Helsinki. The study protocol was approved by the Iranian Registry of Clinical Trials (IRCT). All participants provided informed consent before their involvement in the study.
Participants
Participants were selected among candidates for spine surgeries aged between 18 and 85 years and with American Society of Anesthesia (ASA) classification I or II. The exclusion criteria included being pregnant or breastfeeding, history of allergy to local anesthetic agents, history of cardiac or renal failure, opioid use disorder, uncontrolled blood pressure, body mass index above 40 kg/m2, and a heart rate below 50 beats/min, spinal cord injuries that could interfere with the pain assessment, and incidental durotomy.
Interventions
The patients were assigned to two groups: Morphine and fentanyl. Except for the type of drug studied, the anesthesia method was the same for both groups. All participants underwent general anesthesia using intravenous fentanyl (2 μg/kg), Nesdonal (4 mg/kg), atracurium (0.5 mg/kg), and midazolam (0.04 mg/kg). Isoflurane (1.2%) was used for the anesthesia maintenance. Patients were monitored for vital signs, including heart rate, arterial blood oxygen saturation, and arterial blood pressure, throughout the operation.
For all patients, the posterior approach was chosen in the prone position. The morphine group received intrathecal morphine (0.2 mg) at the end of the operation through a 23G spinal needle through the lumbar intervertebral space (L3-L4 or L4-L5). In cases in which the thecal sac was exposed at the operation site, the drug was directly injected at the end of the procedure. The fentanyl group received intrathecal fentanyl (25 µg) using the same protocol as the morphine group.
Outcomes
The outcomes were assessed by a neurosurgery resident blinded to the intervention assignment. The primary outcome was the postoperative pain intensity, which was evaluated 4, 6, 12, and 18 hours post-surgery using a 10 cm visual analogue scale (VAS), where 0 represented the absence of pain, and 10 denoted the most severe pain the patient had encountered [15]. The secondary outcome measure in this study involved assessing the time interval from the surgical procedure until the patient required supplementary analgesics (specifically, intramuscular ketorolac) in cases where the patient reported a VAS score of at least 3. All patients were evaluated for side effects, including postoperative nausea/vomiting, pruritus, dyspnea, or respiratory depression. In case of postoperative nausea/vomiting, patients were administered a single dose of metoclopramide (10 mg i.v.). In the case of pruritus, a single dose of diphenhydramine (50 mg i.v.) was administered. Patients’ vital signs, including arterial oxygen saturation, were monitored, and non-invasive oxygen supplementation was administrated via a face mask (3 L/m) in cases of oxygen saturation (SPO2) <96%.
Sample size
A priori power analysis was conducted using G*Power software, version 3.1 based on the findings of a previous study [16]. The analysis assumed a two-tailed t-test for the difference between two independent means, with the primary endpoint being the postoperative pain score at 6 hours. Using an expected effect size (Cohen’s d) of 1.56, an α level of 0.05, and a desired power of 0.99 with an allocation ratio of 1:1, it was determined that a total sample size of 34 participants (17 in each group) would be sufficient to detect a clinically significant difference in postoperative pain scores between the two groups, with an actual power of 99%. To account for potential dropouts and to increase the robustness of our findings, we increased the sample size to 80 participants (40 in each group).
Randomization and blinding
A computer-generated randomization sequence was used to assign participants to two groups with a 1:1 allocation ratio: Morphine (n=40) and fentanyl (n=40). The allocation was concealed, and on the day of surgery, after confirming eligibility, a research nurse communicated the assignment to an anesthesiologist. To ensure double-blinding, the participants and the research team in charge of assessing the outcomes were blinded to the treatment assignment.
Statistical analysis
Analyses were performed using SPSS software, version 26 (IBM Corp., N.Y., USA). Graphs were made using GraphPad Prism software, version 8. Quantitative variables were described using Mean±SD, and 95% confidence interval (CI), whereas categorical variables were described using frequency and percentage. The comparison of outcomes between the intervention groups was made utilizing an independent t-test, and the side effects were compared through chi-square or Fischer’s exact test. Additionally, a generalized estimation equation (GEE) analysis was conducted to examine the effects of the intervention group (morphine vs fentanyl) and time on postoperative pain scores, as well as to examine the interaction between group and time. Statistical significance was defined as P<0.05.
3. Results
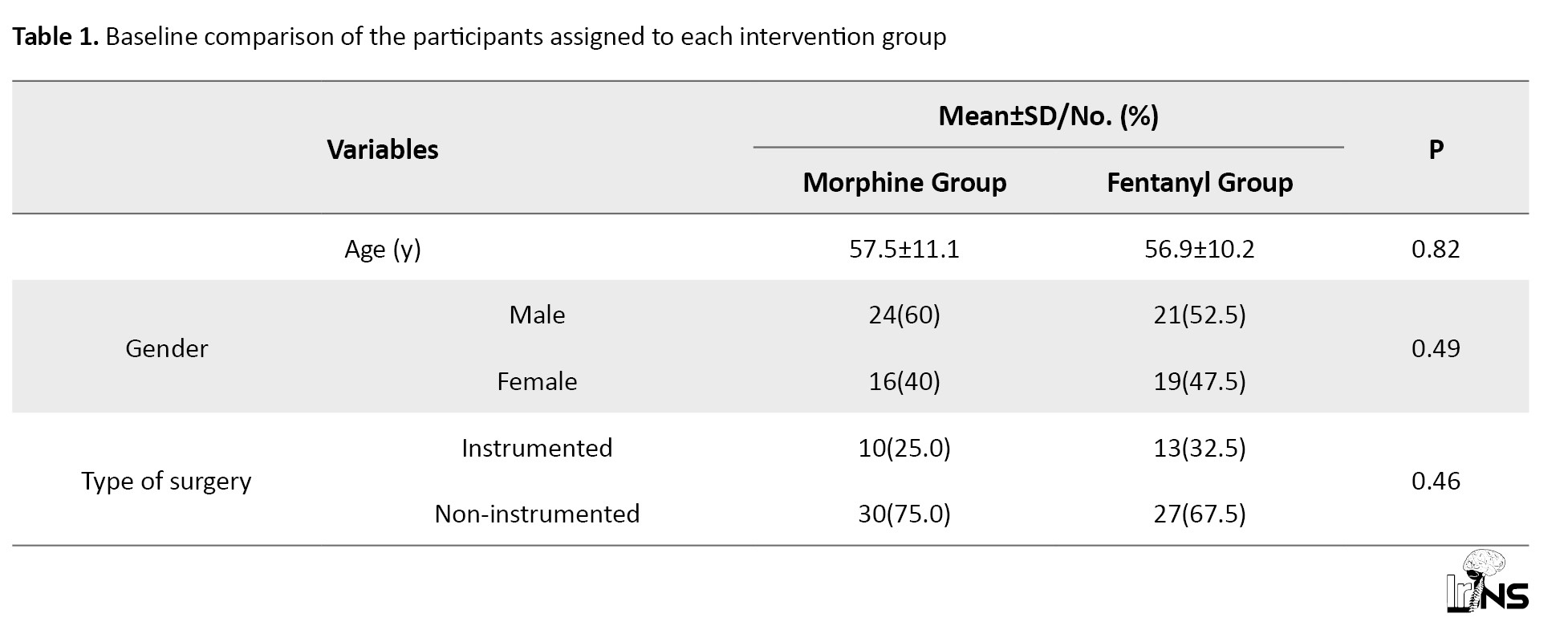
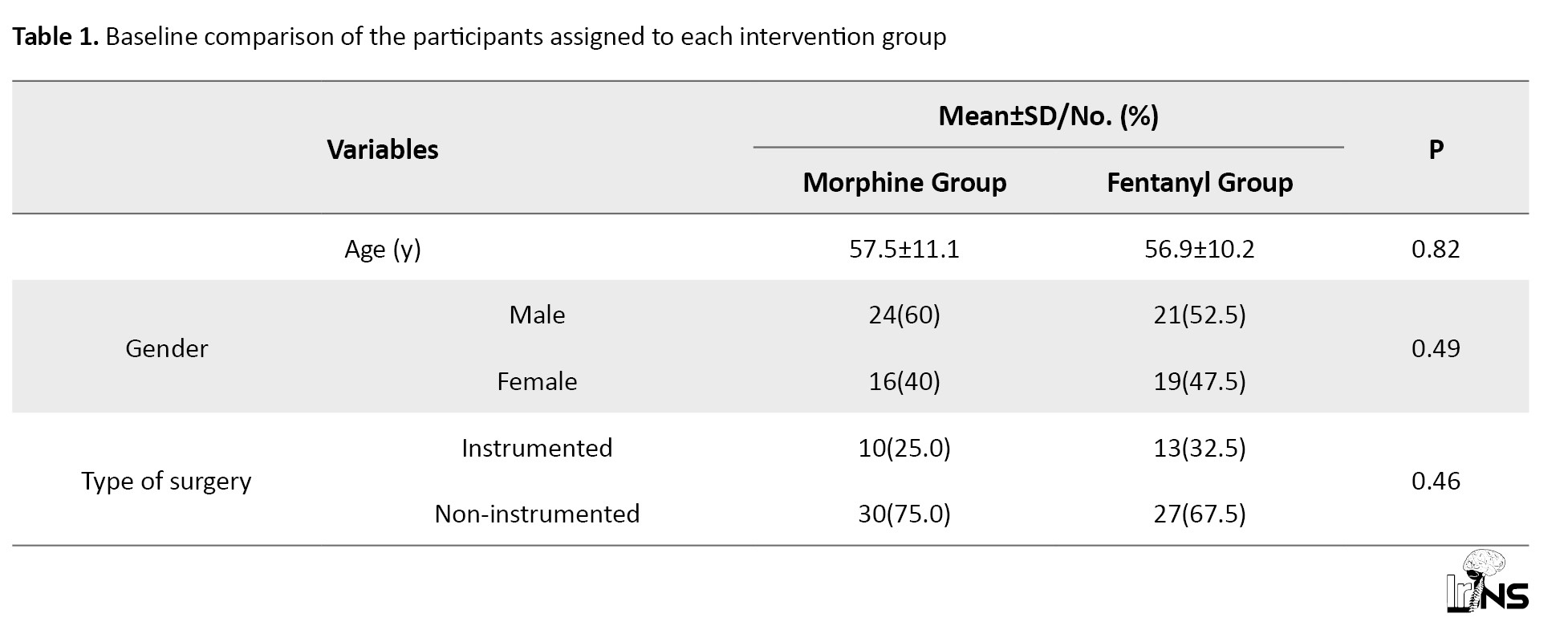
As depicted in the participant flow diagram (Figure 1), 112 patients were assessed for eligibility during the study period. Based on the inclusion and exclusion criteria, 80 patients were enrolled and randomly allocated to two groups, with 40 individuals in each group. All the participants completed the study and were included in the final analysis. The Mean±SD age of participants in the morphine and fentanyl groups was 57.5±11.1 and 56.9±10.2 years, respectively. Males constituted 60% of the morphine group and 52.5% of the fentanyl group. In the morphine group, 25% of patients underwent surgery with instrumentation, whereas this proportion was 32.5% in the fentanyl group. No significant difference existed in age (P=0.82), gender distribution (P=0.49), and surgery type (P=0.46) between the two groups (Table 1).
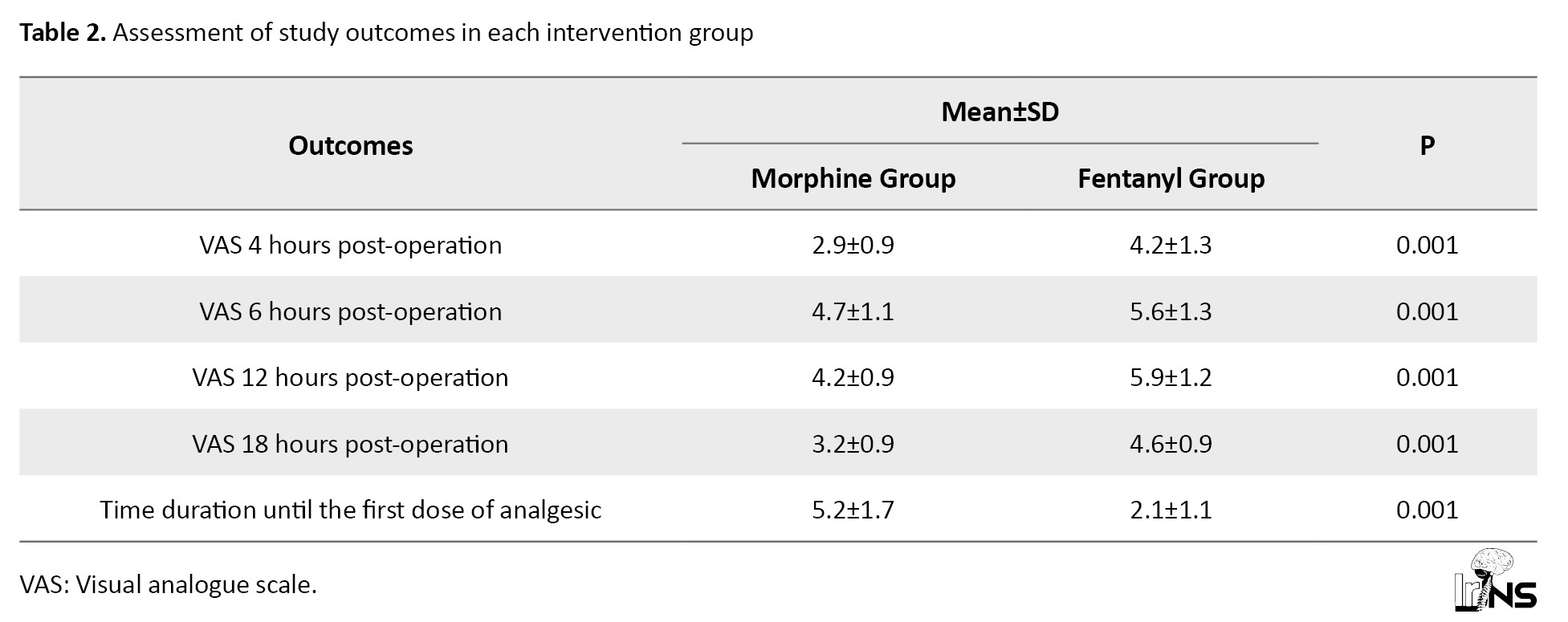
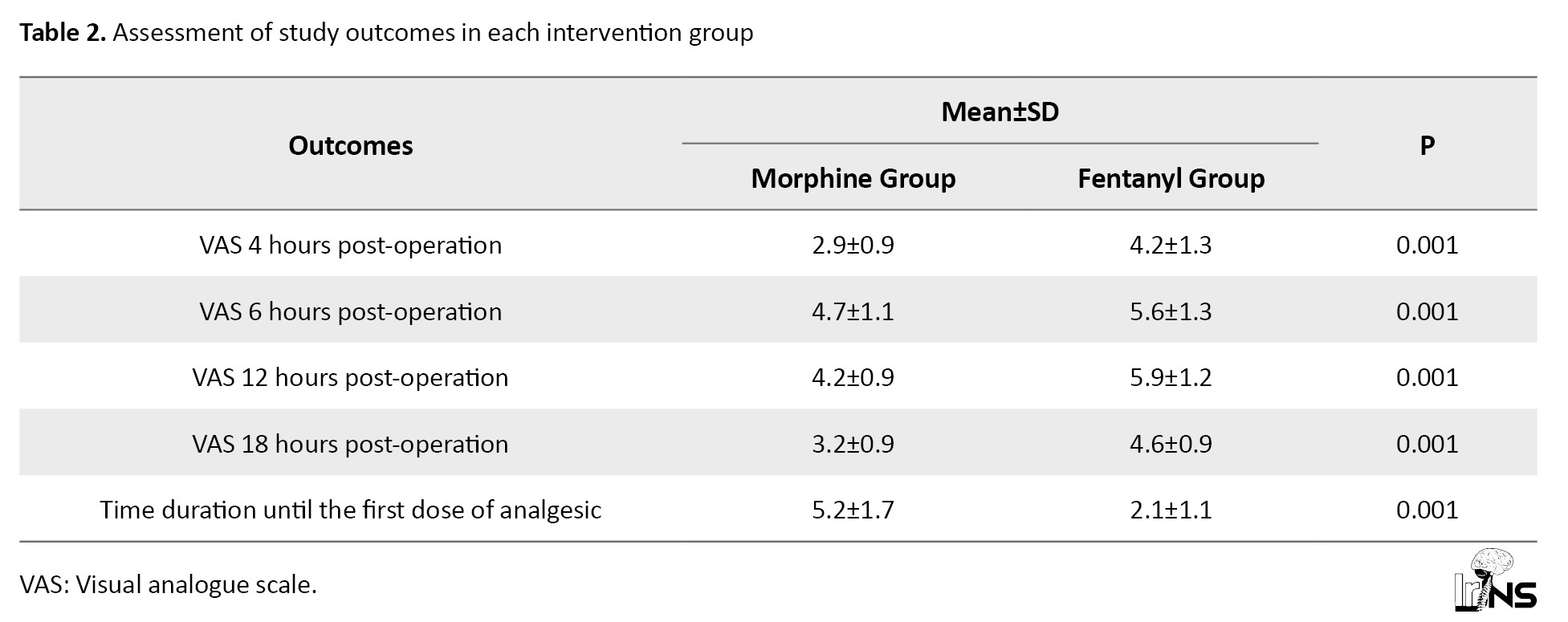
Assessment of postoperative pain intensity demonstrated that participants in the morphine group had a remarkably lower level of pain at 4 hours (P=0.001), 6 hours (P=0.001), 12 hours (P=0.001), and 18 hours (P=0.001) post-surgery compared to the fentanyl group. Additionally, the time interval between the operation’s conclusion and the patients’ request for ketorolac administration was significantly higher in the morphine group (5.2±1.7 hours) compared to the fentanyl group (2.1±1.1 hours) (P=0.001) (Table 2 and Figure 2).
Additionally, the GEE analysis revealed significant main effects of both groups (χ²(1)=72.832, P<0.001) and time (χ²(3)=208.390, P<0.001) on pain scores. Moreover, a significant interaction between group and time was observed (χ²(3)=8.150, P=0.043), indicating that the effect of the intervention on pain scores varied across the different time points. As shown in Table 3, the morphine group consistently demonstrated lower pain scores compared to the fentanyl group at all time points.
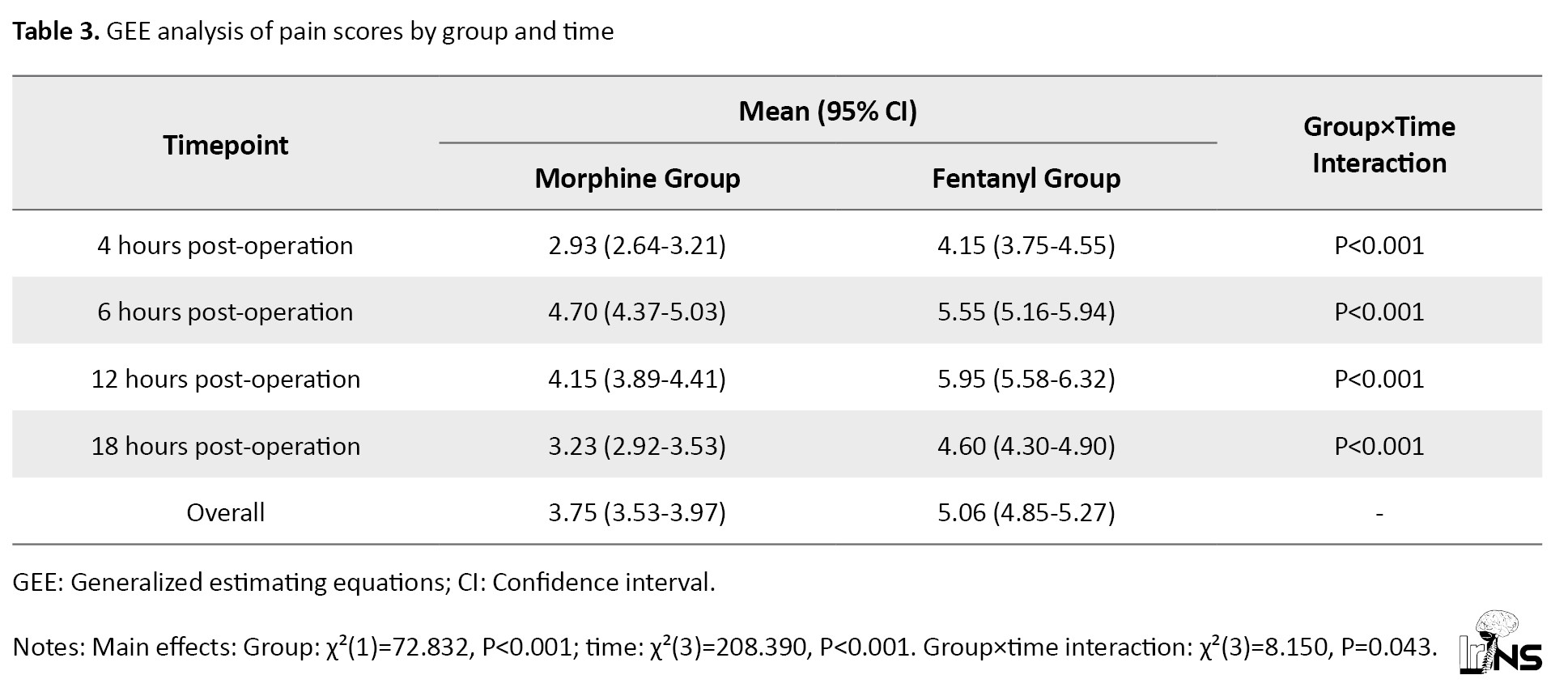
The mean pain score for the morphine group (3.75; 95% CI, 3.53%, 3.97%) was significantly lower than that of the fentanyl group (5.06; 95% CI, 4.85%, 5.27%). The group×time interaction was significant at each time point (P<0.001), showing the consistent superiority of morphine over fentanyl in pain management throughout the observation period. Both groups showed a similar pattern of pain intensity over time, with scores peaking at 6 and 12 hours post-intervention. The difference in pain scores between the two groups was most pronounced at 12 h post-intervention, with the morphine group reporting a mean score of 4.15 (95% CI, 3.89%, 4.41%) compared to 5.95 (95% CI, 5.58%, 6.32%) in the fentanyl group (Table 3).
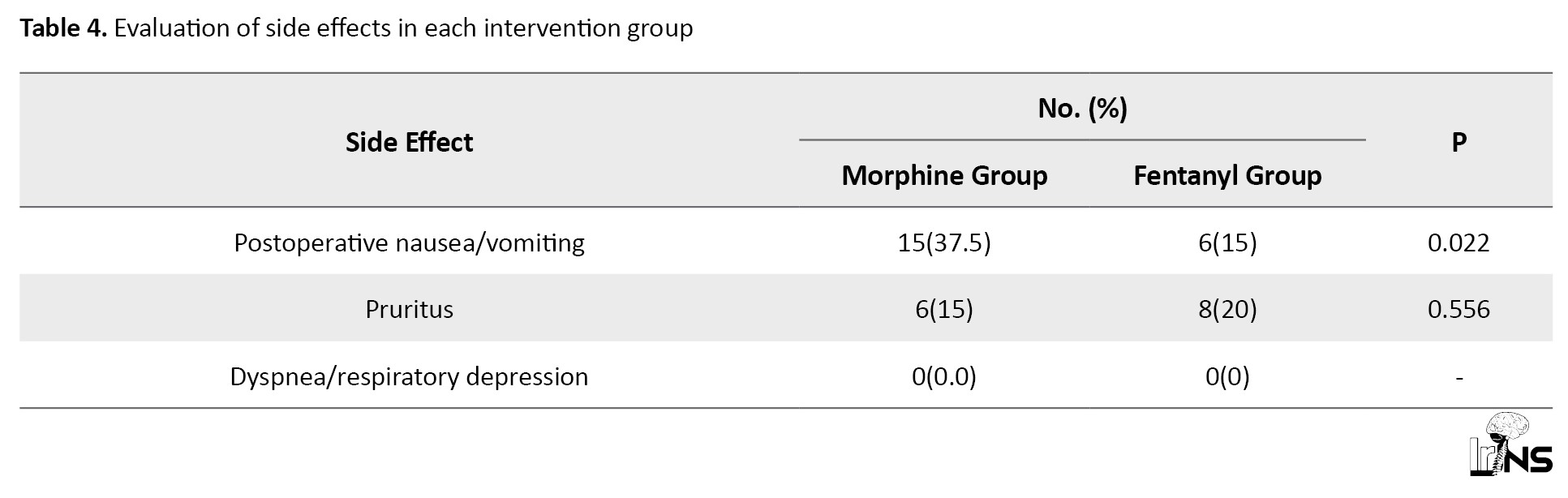
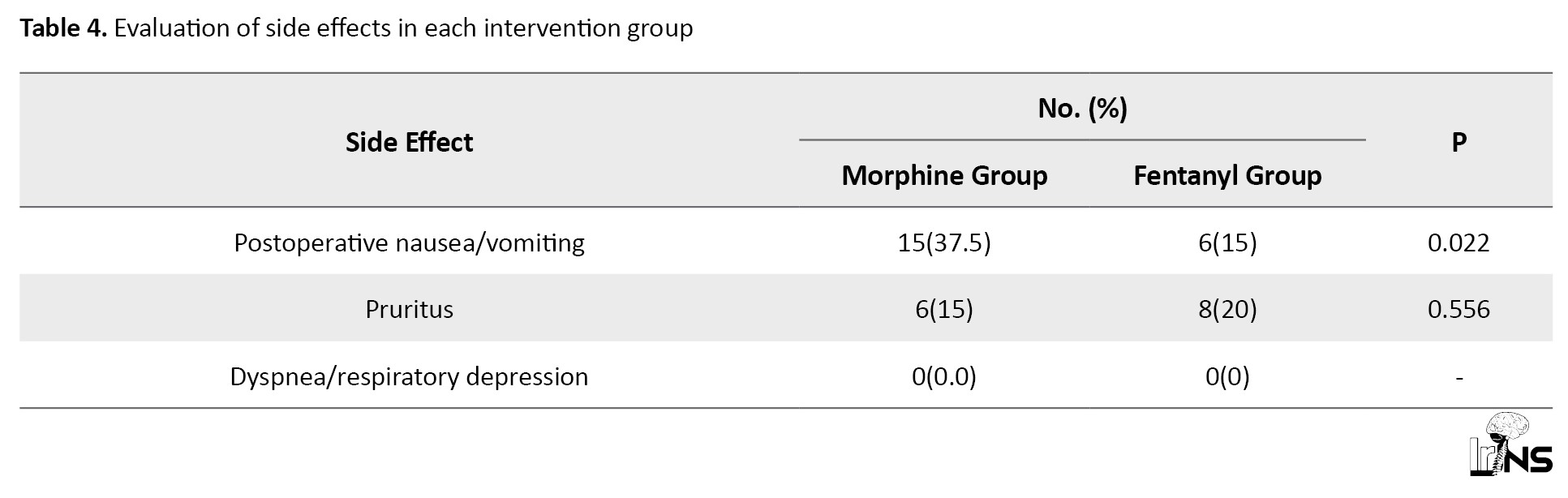
Monitoring for any potential side effects attributable to the interventions demonstrated that 37.5% of the morphine group participants experienced postoperative nausea/vomiting, which was notably elevated compared to the fentanyl group (P=0.022). Pruritus was reported in 15% of the morphine group and 20% of the fentanyl group patients, with no statistical difference between the groups (P=0.556). Post-hoc power analyses revealed that the study had 61.1% and 76.8% power to detect the observed differences in postoperative nausea/vomiting and pruritus rates between the groups, respectively. No cases of postoperative dyspnea or respiratory depression were reported (Table 4).
4. Discussion
This study compared the efficacy of intrathecal morphine and fentanyl in reducing postoperative pain in patients who underwent spinal surgery. To the best of our knowledge, this is the first study to use a randomized clinical trial design to directly compare these two opioid agents in the context of spine surgery. Our study found significant differences between the two groups in terms of postoperative pain intensity, time to analgesic administration and occurrence of postoperative nausea/vomiting.
Our results demonstrated that patients receiving morphine reported notably lower levels of pain at 4, 6, 12, and 18 h post-surgery than those in the fentanyl group. Moreover, GEE analysis confirmed that the morphine group consistently had lower pain scores compared to the fentanyl group at all measured time points. This result suggests that intrathecal morphine provides superior pain relief during the early postoperative period. Furthermore, our study showed a significant difference in the time to postoperative ketorolac administration between the two groups. Accordingly, the morphine group had a significantly longer time interval before requiring ketorolac compared to the fentanyl group. This result suggests that intrathecal morphine may provide longer-lasting pain control and reduce the need for rescue analgesics during the early postoperative period. The differences in pain intensity and the time interval to ketorolac administration were also clinically significant. Consistent with our results, studies comparing intrathecal morphine and fentanyl in other types of surgery have suggested the superiority of morphine in postoperative pain management. For instance, a study on the efficacy of these agents among patients undergoing elective total knee replacement surgery demonstrated that patients receiving intrathecal morphine had significantly lower pain 2, 6, 12, and 24 h after the surgery compared to those who received intrathecal fentanyl [16]. Another study on patients undergoing cesarean section also revealed that co-administration of morphine with hyperbaric bupivacaine was superior to the combination of fentanyl and hyperbaric bupivacaine in postoperative pain management [17].
Supporting our findings, results of a meta-analysis demonstrated that the use of intrathecal morphine significantly decreased the consumption of opioid analgesics and pain intensity in comparison with control patients within the first 24 h after spine surgeries [4]. A recent meta-analysis indicated a remarkable reduction in postoperative pain intensity with intrathecal morphine at 2 h, 4 h, 6 h, 8 h, 12 h, and 24 h following spinal surgery. However, no significant differences were observed 48 h post-operatively [12]. Taken together, this high-level evidence supports the efficacy of intrathecal morphine as a measure for postoperative pain management in spine surgery.
Other studies have also assessed various pharmacological interventions or different modes of drug delivery for postoperative pain management in spinal surgery. Shariat Moharari et al. compared the intraoperative infusion of fentanyl and remifentanil in patients with spinal canal stenosis or scoliosis undergoing spine surgery. Their study showed that remifentanil was not superior to fentanyl in terms of postoperative pain control, as patients receiving remifentanil required more morphine consumption and had higher VAS scores during the first 12 h after the surgery [18]. In another study, although the patients receiving intrathecal fentanyl during lumbar surgery demonstrated a significant decrease in postoperative VAS and less need for postoperative morphine administration, there was no control intervention to assess fentanyl’s superiority [5]. Additionally, a more recent study compared low-dose intravenous morphine and intravenous fentanyl in spine fusion surgeries and showed that continuous infusion of morphine was more effective than fentanyl for postoperative pain management [19]. Consistent with the latter study, our study also extended this observation to the intrathecal route of administration, demonstrating that intrathecal morphine is superior to intrathecal fentanyl for postoperative pain management in spinal surgeries, thus reinforcing the efficacy of morphine across different modes of delivery in this surgical context.
In assessing the safety profile of interventions, our results indicate that postoperative nausea/vomiting occurred at a higher frequency in the morphine group than in the fentanyl group. Relatively high rates of nausea/vomiting are consistent with the known side-effect profile of opioids reported in previous studies [20, 21]. The increased incidence of nausea/vomiting in the morphine group seems to have minimal clinical importance, as none of the patients suffered from this side effect. Although the difference in the incidence of pruritus between the two groups did not reach statistical significance, it is worth noting that pruritus was reported in both groups, albeit at a slightly higher proportion in the fentanyl group. Previous reports have also exhibited variations in the adverse effects of intrathecal opioids. Findings from a study by Kılıçkaya et al. revealed no significant difference in postoperative nausea between intrathecal morphine and fentanyl in knee replacement surgery [16]. However, the results of a study on patients undergoing caesarian section revealed a heightened risk of nausea and vomiting in fentanyl-treated patients compared to the morphine group [17]. The results of a meta-analysis by Pendi et al. also indicated that intrathecal morphine was not associated with increased rates of postoperative nausea and vomiting in spinal surgery; however, it was linked to an increased risk of pruritus [4]. These results are consistent with those of the meta-analysis by Wang et al. [12]. In our study, no cases of postoperative dyspnea or respiratory depression were reported in either group, indicating the safety of both intrathecal morphine and fentanyl in spinal surgery. The absence of respiratory complications suggests that the doses of intrathecal opioids used in this study were well tolerated and did not compromise respiratory function.
5. Conclusion
In conclusion, our study demonstrates that intrathecal morphine provides superior pain relief and prolongs the time to rescue analgesic administration compared to intrathecal fentanyl in the early postoperative period following spinal surgery. Indeed, our study found significant differences, both statistically and clinically, between patients who received intrathecal morphine and those who received intrathecal fentanyl regarding postoperative pain intensity and duration of analgesic administration. Although there is a notably higher rate of nausea/vomiting in a morphine-treated group compared to patients who received fentanyl, this difference is not of high clinical importance.
Although our study provides valuable insights into the effectiveness and safety profile of intrathecal morphine and fentanyl for postoperative pain management in spinal surgery, it is important to acknowledge certain limitations. Our study concentrated on short-term effects; therefore, the long-term outcomes of these interventions remain unknown. While our study focused on postoperative pain control as the primary outcome, evaluating the impact of intrathecal morphine and fentanyl on long-term functional outcomes, such as patient mobility, quality of life, and return to normal activities, would offer a broader understanding of the overall advantages of these interventions. Moreover, while our study was adequately powered to detect differences in postoperative pain scores (the primary outcome), a limitation is the potential underpower to definitively assess differences in side effects between the groups. These secondary outcomes should be interpreted cautiously, and future studies specifically designed to compare side effect profiles may provide more conclusive evidence.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was reviewed and approved by the Institutional Ethics Committee of the Kerman University of Medical Sciences, Kerman, Iran (Code: IR.KMU.AH.REC.1401.232) before participant recruitment. This study was conducted by the Code of Ethics of the World Medical Association (Declaration of Helsinki). The study protocol was approved by the Iranian Registry of Clinical Trials (IRCT), Tehran, Iran (Code: 20230717058820N1). Informed consent was obtained from all participants before their inclusion in the study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conception and design: Hamed Reihani-Kermani; Data collection: Ehsan Parsa, and Mehran Ilaghi; Data analysis and interpretation: Mehran Ilaghi; Drafting the article: Mehran Ilaghi; Critical revision of the article: Hamed Reihani-Kermani; Final Approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Spine surgery is a complex and invasive procedure often leading to considerable postoperative pain, which can significantly impact patients’ recovery and overall satisfaction [1]. Adequate pain management after spinal surgery is crucial to ensure optimal patient outcomes, early mobilization, and smooth transition to rehabilitation [2, 3]. Among various analgesic strategies, the use of intrathecal opioids has gained prominence due to its effectiveness in providing extended pain relief. Intrathecal morphine and fentanyl are commonly employed opioids in spinal anesthesia [4, 5], but their comparative efficacy in reducing postoperative pain remains a subject of debate.
Morphine is a prototypical opioid analgesic that acts mainly on mu-opioid receptors in the central nervous system [6]. It exerts its analgesic effects by binding to these receptors, inhibiting the release of a neurotransmitter known as substance P, thereby diminishing pain perception [7]. Morphine’s potency and efficacy stem from its high affinity for mu-opioid receptors, allowing for robust pain relief. Additionally, it exhibits other pharmacological actions, such as sedation, respiratory depression, and suppression of cough reflexes [8, 9].
In contrast, fentanyl is a highly potent opioid characterized by its swift onset and brief duration of effect [10]. It also acts primarily on mu-opioid receptors, producing analgesia by inhibiting neurotransmitter release. Fentanyl is highly lipophilic, allowing it to rapidly penetrate the blood-brain barrier, resulting in a rapid onset of analgesia [11].
Several factors contribute to select a specific opioid for intrathecal administration, including potency, duration of action, side-effect profile, and patient-specific characteristics. Although both intrathecal morphine and fentanyl have demonstrated efficacy in managing postoperative pain in various types of surgeries [5, 12, 13], there is limited direct comparative data on their effectiveness and safety in the context of spinal surgery.
The primary objective of this clinical trial is to compare the efficacy of intrathecal morphine and fentanyl in reducing postoperative pain intensity after spinal surgery. This study aims to improve pain management protocols, reduce opioid consumption, enhance patient comfort, and accelerate recovery in this surgical population.
2. Methods and Materials
This study was designed, conducted, and reported by the Consolidated Standards of Reporting Trials (CONSORT) 2010 guidelines to ensure transparency and comprehensive reporting of the study methodology and results [14].
Trial design
This study was a randomized parallel double-blind trial conducted to compare the efficacy of intrathecal morphine and fentanyl in reducing pain following spinal surgery. We hypothesized that intrathecal morphine would be more effective for postoperative pain control in spinal surgery. The study was conducted between October 2022 and April 2023 at the Neurospine Surgery Department of Shahid Bahonar Hospital, the main referral neurospine center in Kerman City, southeast Iran. The study protocol was reviewed and approved by the Institutional Ethics Committee of the Kerman University of Medical Sciences, before participant recruitment. This study adhered to the ethical guidelines outlined by the World Medical Association, as stated in the Declaration of Helsinki. The study protocol was approved by the Iranian Registry of Clinical Trials (IRCT). All participants provided informed consent before their involvement in the study.
Participants
Participants were selected among candidates for spine surgeries aged between 18 and 85 years and with American Society of Anesthesia (ASA) classification I or II. The exclusion criteria included being pregnant or breastfeeding, history of allergy to local anesthetic agents, history of cardiac or renal failure, opioid use disorder, uncontrolled blood pressure, body mass index above 40 kg/m2, and a heart rate below 50 beats/min, spinal cord injuries that could interfere with the pain assessment, and incidental durotomy.
Interventions
The patients were assigned to two groups: Morphine and fentanyl. Except for the type of drug studied, the anesthesia method was the same for both groups. All participants underwent general anesthesia using intravenous fentanyl (2 μg/kg), Nesdonal (4 mg/kg), atracurium (0.5 mg/kg), and midazolam (0.04 mg/kg). Isoflurane (1.2%) was used for the anesthesia maintenance. Patients were monitored for vital signs, including heart rate, arterial blood oxygen saturation, and arterial blood pressure, throughout the operation.
For all patients, the posterior approach was chosen in the prone position. The morphine group received intrathecal morphine (0.2 mg) at the end of the operation through a 23G spinal needle through the lumbar intervertebral space (L3-L4 or L4-L5). In cases in which the thecal sac was exposed at the operation site, the drug was directly injected at the end of the procedure. The fentanyl group received intrathecal fentanyl (25 µg) using the same protocol as the morphine group.
Outcomes
The outcomes were assessed by a neurosurgery resident blinded to the intervention assignment. The primary outcome was the postoperative pain intensity, which was evaluated 4, 6, 12, and 18 hours post-surgery using a 10 cm visual analogue scale (VAS), where 0 represented the absence of pain, and 10 denoted the most severe pain the patient had encountered [15]. The secondary outcome measure in this study involved assessing the time interval from the surgical procedure until the patient required supplementary analgesics (specifically, intramuscular ketorolac) in cases where the patient reported a VAS score of at least 3. All patients were evaluated for side effects, including postoperative nausea/vomiting, pruritus, dyspnea, or respiratory depression. In case of postoperative nausea/vomiting, patients were administered a single dose of metoclopramide (10 mg i.v.). In the case of pruritus, a single dose of diphenhydramine (50 mg i.v.) was administered. Patients’ vital signs, including arterial oxygen saturation, were monitored, and non-invasive oxygen supplementation was administrated via a face mask (3 L/m) in cases of oxygen saturation (SPO2) <96%.
Sample size
A priori power analysis was conducted using G*Power software, version 3.1 based on the findings of a previous study [16]. The analysis assumed a two-tailed t-test for the difference between two independent means, with the primary endpoint being the postoperative pain score at 6 hours. Using an expected effect size (Cohen’s d) of 1.56, an α level of 0.05, and a desired power of 0.99 with an allocation ratio of 1:1, it was determined that a total sample size of 34 participants (17 in each group) would be sufficient to detect a clinically significant difference in postoperative pain scores between the two groups, with an actual power of 99%. To account for potential dropouts and to increase the robustness of our findings, we increased the sample size to 80 participants (40 in each group).
Randomization and blinding
A computer-generated randomization sequence was used to assign participants to two groups with a 1:1 allocation ratio: Morphine (n=40) and fentanyl (n=40). The allocation was concealed, and on the day of surgery, after confirming eligibility, a research nurse communicated the assignment to an anesthesiologist. To ensure double-blinding, the participants and the research team in charge of assessing the outcomes were blinded to the treatment assignment.
Statistical analysis
Analyses were performed using SPSS software, version 26 (IBM Corp., N.Y., USA). Graphs were made using GraphPad Prism software, version 8. Quantitative variables were described using Mean±SD, and 95% confidence interval (CI), whereas categorical variables were described using frequency and percentage. The comparison of outcomes between the intervention groups was made utilizing an independent t-test, and the side effects were compared through chi-square or Fischer’s exact test. Additionally, a generalized estimation equation (GEE) analysis was conducted to examine the effects of the intervention group (morphine vs fentanyl) and time on postoperative pain scores, as well as to examine the interaction between group and time. Statistical significance was defined as P<0.05.
3. Results
As depicted in the participant flow diagram (Figure 1), 112 patients were assessed for eligibility during the study period. Based on the inclusion and exclusion criteria, 80 patients were enrolled and randomly allocated to two groups, with 40 individuals in each group. All the participants completed the study and were included in the final analysis. The Mean±SD age of participants in the morphine and fentanyl groups was 57.5±11.1 and 56.9±10.2 years, respectively. Males constituted 60% of the morphine group and 52.5% of the fentanyl group. In the morphine group, 25% of patients underwent surgery with instrumentation, whereas this proportion was 32.5% in the fentanyl group. No significant difference existed in age (P=0.82), gender distribution (P=0.49), and surgery type (P=0.46) between the two groups (Table 1).
Assessment of postoperative pain intensity demonstrated that participants in the morphine group had a remarkably lower level of pain at 4 hours (P=0.001), 6 hours (P=0.001), 12 hours (P=0.001), and 18 hours (P=0.001) post-surgery compared to the fentanyl group. Additionally, the time interval between the operation’s conclusion and the patients’ request for ketorolac administration was significantly higher in the morphine group (5.2±1.7 hours) compared to the fentanyl group (2.1±1.1 hours) (P=0.001) (Table 2 and Figure 2).
Additionally, the GEE analysis revealed significant main effects of both groups (χ²(1)=72.832, P<0.001) and time (χ²(3)=208.390, P<0.001) on pain scores. Moreover, a significant interaction between group and time was observed (χ²(3)=8.150, P=0.043), indicating that the effect of the intervention on pain scores varied across the different time points. As shown in Table 3, the morphine group consistently demonstrated lower pain scores compared to the fentanyl group at all time points.
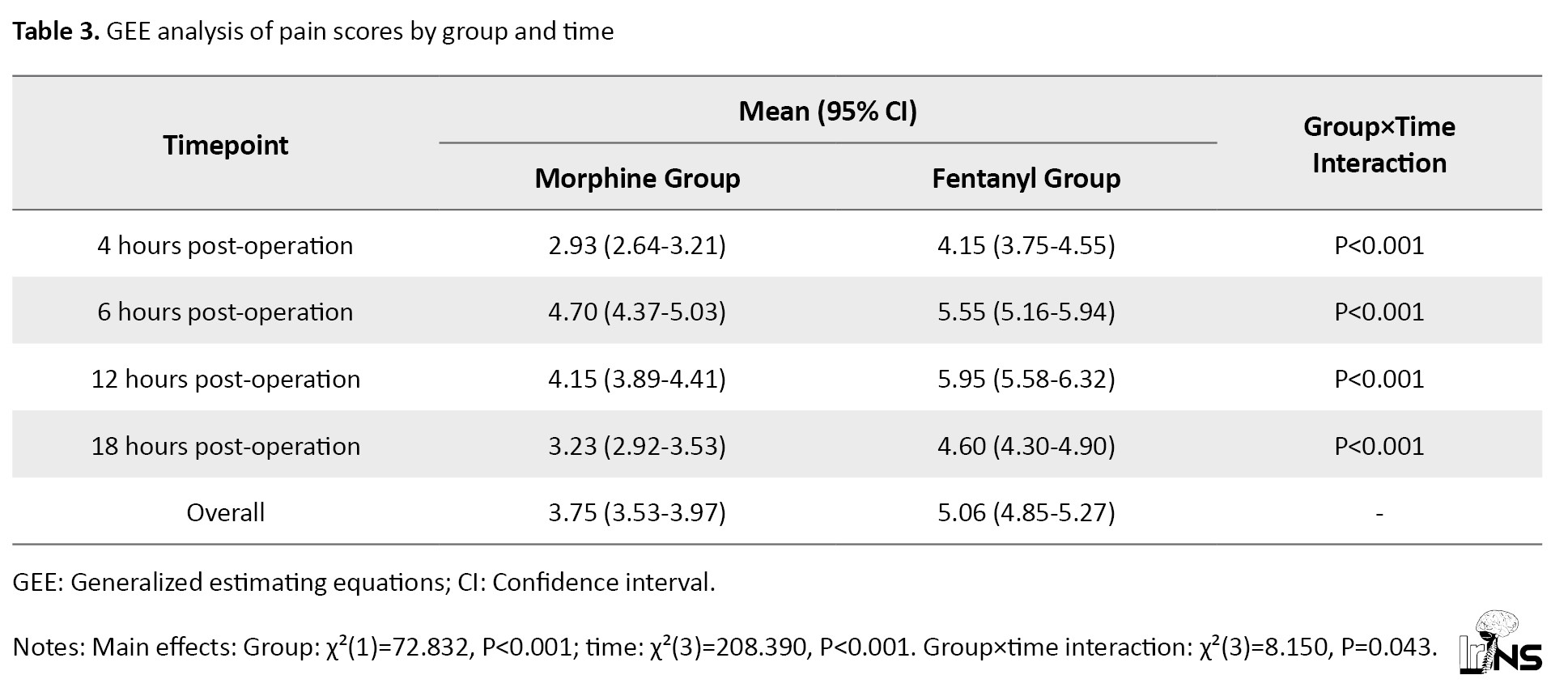
The mean pain score for the morphine group (3.75; 95% CI, 3.53%, 3.97%) was significantly lower than that of the fentanyl group (5.06; 95% CI, 4.85%, 5.27%). The group×time interaction was significant at each time point (P<0.001), showing the consistent superiority of morphine over fentanyl in pain management throughout the observation period. Both groups showed a similar pattern of pain intensity over time, with scores peaking at 6 and 12 hours post-intervention. The difference in pain scores between the two groups was most pronounced at 12 h post-intervention, with the morphine group reporting a mean score of 4.15 (95% CI, 3.89%, 4.41%) compared to 5.95 (95% CI, 5.58%, 6.32%) in the fentanyl group (Table 3).
Monitoring for any potential side effects attributable to the interventions demonstrated that 37.5% of the morphine group participants experienced postoperative nausea/vomiting, which was notably elevated compared to the fentanyl group (P=0.022). Pruritus was reported in 15% of the morphine group and 20% of the fentanyl group patients, with no statistical difference between the groups (P=0.556). Post-hoc power analyses revealed that the study had 61.1% and 76.8% power to detect the observed differences in postoperative nausea/vomiting and pruritus rates between the groups, respectively. No cases of postoperative dyspnea or respiratory depression were reported (Table 4).
4. Discussion
This study compared the efficacy of intrathecal morphine and fentanyl in reducing postoperative pain in patients who underwent spinal surgery. To the best of our knowledge, this is the first study to use a randomized clinical trial design to directly compare these two opioid agents in the context of spine surgery. Our study found significant differences between the two groups in terms of postoperative pain intensity, time to analgesic administration and occurrence of postoperative nausea/vomiting.
Our results demonstrated that patients receiving morphine reported notably lower levels of pain at 4, 6, 12, and 18 h post-surgery than those in the fentanyl group. Moreover, GEE analysis confirmed that the morphine group consistently had lower pain scores compared to the fentanyl group at all measured time points. This result suggests that intrathecal morphine provides superior pain relief during the early postoperative period. Furthermore, our study showed a significant difference in the time to postoperative ketorolac administration between the two groups. Accordingly, the morphine group had a significantly longer time interval before requiring ketorolac compared to the fentanyl group. This result suggests that intrathecal morphine may provide longer-lasting pain control and reduce the need for rescue analgesics during the early postoperative period. The differences in pain intensity and the time interval to ketorolac administration were also clinically significant. Consistent with our results, studies comparing intrathecal morphine and fentanyl in other types of surgery have suggested the superiority of morphine in postoperative pain management. For instance, a study on the efficacy of these agents among patients undergoing elective total knee replacement surgery demonstrated that patients receiving intrathecal morphine had significantly lower pain 2, 6, 12, and 24 h after the surgery compared to those who received intrathecal fentanyl [16]. Another study on patients undergoing cesarean section also revealed that co-administration of morphine with hyperbaric bupivacaine was superior to the combination of fentanyl and hyperbaric bupivacaine in postoperative pain management [17].
Supporting our findings, results of a meta-analysis demonstrated that the use of intrathecal morphine significantly decreased the consumption of opioid analgesics and pain intensity in comparison with control patients within the first 24 h after spine surgeries [4]. A recent meta-analysis indicated a remarkable reduction in postoperative pain intensity with intrathecal morphine at 2 h, 4 h, 6 h, 8 h, 12 h, and 24 h following spinal surgery. However, no significant differences were observed 48 h post-operatively [12]. Taken together, this high-level evidence supports the efficacy of intrathecal morphine as a measure for postoperative pain management in spine surgery.
Other studies have also assessed various pharmacological interventions or different modes of drug delivery for postoperative pain management in spinal surgery. Shariat Moharari et al. compared the intraoperative infusion of fentanyl and remifentanil in patients with spinal canal stenosis or scoliosis undergoing spine surgery. Their study showed that remifentanil was not superior to fentanyl in terms of postoperative pain control, as patients receiving remifentanil required more morphine consumption and had higher VAS scores during the first 12 h after the surgery [18]. In another study, although the patients receiving intrathecal fentanyl during lumbar surgery demonstrated a significant decrease in postoperative VAS and less need for postoperative morphine administration, there was no control intervention to assess fentanyl’s superiority [5]. Additionally, a more recent study compared low-dose intravenous morphine and intravenous fentanyl in spine fusion surgeries and showed that continuous infusion of morphine was more effective than fentanyl for postoperative pain management [19]. Consistent with the latter study, our study also extended this observation to the intrathecal route of administration, demonstrating that intrathecal morphine is superior to intrathecal fentanyl for postoperative pain management in spinal surgeries, thus reinforcing the efficacy of morphine across different modes of delivery in this surgical context.
In assessing the safety profile of interventions, our results indicate that postoperative nausea/vomiting occurred at a higher frequency in the morphine group than in the fentanyl group. Relatively high rates of nausea/vomiting are consistent with the known side-effect profile of opioids reported in previous studies [20, 21]. The increased incidence of nausea/vomiting in the morphine group seems to have minimal clinical importance, as none of the patients suffered from this side effect. Although the difference in the incidence of pruritus between the two groups did not reach statistical significance, it is worth noting that pruritus was reported in both groups, albeit at a slightly higher proportion in the fentanyl group. Previous reports have also exhibited variations in the adverse effects of intrathecal opioids. Findings from a study by Kılıçkaya et al. revealed no significant difference in postoperative nausea between intrathecal morphine and fentanyl in knee replacement surgery [16]. However, the results of a study on patients undergoing caesarian section revealed a heightened risk of nausea and vomiting in fentanyl-treated patients compared to the morphine group [17]. The results of a meta-analysis by Pendi et al. also indicated that intrathecal morphine was not associated with increased rates of postoperative nausea and vomiting in spinal surgery; however, it was linked to an increased risk of pruritus [4]. These results are consistent with those of the meta-analysis by Wang et al. [12]. In our study, no cases of postoperative dyspnea or respiratory depression were reported in either group, indicating the safety of both intrathecal morphine and fentanyl in spinal surgery. The absence of respiratory complications suggests that the doses of intrathecal opioids used in this study were well tolerated and did not compromise respiratory function.
5. Conclusion
In conclusion, our study demonstrates that intrathecal morphine provides superior pain relief and prolongs the time to rescue analgesic administration compared to intrathecal fentanyl in the early postoperative period following spinal surgery. Indeed, our study found significant differences, both statistically and clinically, between patients who received intrathecal morphine and those who received intrathecal fentanyl regarding postoperative pain intensity and duration of analgesic administration. Although there is a notably higher rate of nausea/vomiting in a morphine-treated group compared to patients who received fentanyl, this difference is not of high clinical importance.
Although our study provides valuable insights into the effectiveness and safety profile of intrathecal morphine and fentanyl for postoperative pain management in spinal surgery, it is important to acknowledge certain limitations. Our study concentrated on short-term effects; therefore, the long-term outcomes of these interventions remain unknown. While our study focused on postoperative pain control as the primary outcome, evaluating the impact of intrathecal morphine and fentanyl on long-term functional outcomes, such as patient mobility, quality of life, and return to normal activities, would offer a broader understanding of the overall advantages of these interventions. Moreover, while our study was adequately powered to detect differences in postoperative pain scores (the primary outcome), a limitation is the potential underpower to definitively assess differences in side effects between the groups. These secondary outcomes should be interpreted cautiously, and future studies specifically designed to compare side effect profiles may provide more conclusive evidence.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was reviewed and approved by the Institutional Ethics Committee of the Kerman University of Medical Sciences, Kerman, Iran (Code: IR.KMU.AH.REC.1401.232) before participant recruitment. This study was conducted by the Code of Ethics of the World Medical Association (Declaration of Helsinki). The study protocol was approved by the Iranian Registry of Clinical Trials (IRCT), Tehran, Iran (Code: 20230717058820N1). Informed consent was obtained from all participants before their inclusion in the study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conception and design: Hamed Reihani-Kermani; Data collection: Ehsan Parsa, and Mehran Ilaghi; Data analysis and interpretation: Mehran Ilaghi; Drafting the article: Mehran Ilaghi; Critical revision of the article: Hamed Reihani-Kermani; Final Approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Menendez JY, Omar NB, Chagoya G, Tabibian BE, Elsayed GA, Walters BC, et al. Patient satisfaction in Spine surgery: A systematic review of the literature. Asian Spine Journal. 2019; 13(6):1047-57. [DOI:10.31616/asj.2019.0032] [PMID]
- Devin CJ, McGirt MJ. Best evidence in multimodal pain management in spine surgery and means of assessing postoperative pain and functional outcomes. Journal of Clinical Neuroscience. 2015; 22(6):930-8. [DOI:10.1016/j.jocn.2015.01.003] [PMID]
- Bajwa SJ, Haldar R. Pain management following spinal surgeries: an appraisal of the available options. Journal of Craniovertebral Junction & Spine. 2015; 6(3):105-10. [DOI:10.4103/0974-8237.161589] [PMID]
- Pendi A, Acosta FL, Tuchman A, Movahedi R, Sivasundaram L, Arif I, et al. Intrathecal morphine in Spine surgery: a meta-analysis of randomized controlled trials. Spine. 2017; 42(12):E740-7. [DOI:10.1097/BRS.0000000000002198] [PMID]
- Chan JH, Heilpern GN, Packham I, Trehan RK, Marsh GD, Knibb AA. A prospective randomized double-blind trial of the use of intrathecal fentanyl in patients undergoing lumbar spinal surgery. Spine. 2006; 31(22):2529-33. [DOI:10.1097/01.brs.0000241135.79983.52] [PMID]
- Lugo RA, Kern SE. Clinical pharmacokinetics of Morphine. Journal of pain & palliative care pharmacotherapy. 2002; 16(4):5-18. [DOI:10.1080/J354v16n04_02] [PMID]
- Lipp J. Possible mechanisms of morphine analgesia. Clinical neuropharmacology. 1991; 14(2):131-47. [DOI:10.1097/00002826-199104000-00003] [PMID]
- Koning MV, Reussien E, Vermeulen BAN, Zonneveld S, Westerman EM, de Graaff JC, et al. Serious adverse events after a single shot of intrathecal Morphine: A case series and systematic review. Pain research & management. 2022; 2022:4567192.[DOI:10.1155/2022/4567192] [PMID]
- Ko S, Goldstein DH, VanDenKerkhof EG. Definitions of "respiratory depression" with intrathecal morphine postoperative analgesia: A review of the literature. Canadian journal of anaesthesia. 2003; 50(7):679-88. [DOI:10.1007/BF03018710] [PMID]
- Bossi P, Escobar Y, Pea F. Rapid-onset opioids for management of breakthrough cancer pain: Considerations for daily practice. Frontiers in Pain Research. 2022; 3:893530. [DOI:10.3389/fpain.2022.893530] [PMID]
- Gerhard GS, Kaniper S, Paynton B. Fentanyl overdoses and pharmacogenetics. Pharmacogenetics and Genomics. 2020; 30(1):5-8. [DOI:10.1097/FPC.0000000000000389] [PMID]
- Wang J, Sun H, Sun WT, Sun HP, Tian T, Sun J. Efficacy and safety of intrathecal morphine for pain control after spinal surgery: A systematic review and meta-analysis. European Review for Medical and Pharmacological Sciences. 2021; 25(6):2674-84. [doi:10.26355/eurrev_202103_25431] [PMID]
- Gomaa HM, Mohamed NN, Zoheir HAH, Ali MS. A comparison between post-operative analgesia after intrathecal nalbuphine with bupivacaine and intrathecal fentanyl with bupivacaine after cesarean section. Egyptian Journal of Anaesthesia. 2014; 30(4):405-10. [DOI:10.1016/j.egja.2014.03.008]
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Journal of Pharmacology and pharmacotherapeutics. 2010; 1(2):100-7. [DOI:10.4103/0976-500X.72352] [PMID]
- Kahl C, Cleland JA. Visual analogue scale, numeric pain rating scale and the McGill pain Questionnaire: an overview of psychometric properties. Physical Therapy Reviews. 2005; 10(2):123-8. [DOI:10.1179/108331905X55776]
- Kılıçkaya R, Orak Y, Balcı MA, Balcı F, Ünal İ. Comparison of the effects of intrathecal Fentanyl and Intrathecal Morphine on pain in elective total Knee replacement surgery. Pain research & management. 2016; 2016:3256583. [DOI:10.1155/2016/3256583] [PMID]
- Siti Salmah G, Choy YC. Comparison of morphine with fentanyl added to intrathecal 0.5% hyperbaric bupivacaine for analgesia after caesarean section. The Medical Journal of Malaysia. 2009; 64(1):71-4. [PMID]
- Shariat Moharari R, Shahinpour S, Saeedi N, Sahraei E, Najafi A, Etezadi F, et al. Comparison of Intraoperative Infusion of Remifentanil Versus Fentanyl on pain management in patients undergoing Spine surgery: A double blinded randomized clinical trial. Anesthesiology and pain medicine. 2021; 11(4):e115576. [DOI:10.5812/aapm.115576] [PMID]
- Venkatraman R, Pushparani A, Balaji R, Nandhini P. Comparison of low dose intravenous fentanyl and morphine infusion for postoperative analgesia in spine fusion surgeries-a randomized control trial. Brazilian Journal of Anesthesiology. 2021; 71(4):339-44. [DOI:10.1016/j.bjane.2020.12.013] [PMID]
- Chinachoti T, Nilrat P, Samarnpiboonphol P. Nausea, vomiting and pruritus induced by intrathecal morphine. Journal of the Medical Association of Thailand. 2013; 96(5):589-94. [PMID]
- Moraitis A, Hultin M, Walldén J. Risk of postoperative nausea and vomiting in hip and knee arthroplasty: a prospective cohort study after spinal anaesthesia including intrathecal morphine. BMC anesthesiology. 2020; 20(1):242. [DOI:10.1186/s12871-020-01154-z] [PMID]
Type of Study: Clinical Trial |
Subject:
Spine
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








