Sun, Oct 26, 2025
Volume 10 - Continuous Publishing
Iran J Neurosurg 2024, 10 - Continuous Publishing: 134-139 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Thavara B D, Parambil R M, Jose B V, Parol U, Sasi P K, Sai Sree Krishna G. A Rare Case of Spinal Intradural Neurenteric Cyst in a Septuagenarian Causing Acute Paraparesis. Iran J Neurosurg 2024; 10 : 15
URL: http://irjns.org/article-1-428-en.html
URL: http://irjns.org/article-1-428-en.html
Binoy Damodar Thavara *1 

 , Rajeev Mandaka Parambil2
, Rajeev Mandaka Parambil2 

 , Byjo Valiyaveetil Jose2
, Byjo Valiyaveetil Jose2 

 , Umasankar Parol3
, Umasankar Parol3 

 , Prem kumar Sasi2
, Prem kumar Sasi2 

 , Gorijavolu Sai Sree Krishna2
, Gorijavolu Sai Sree Krishna2 




 , Rajeev Mandaka Parambil2
, Rajeev Mandaka Parambil2 

 , Byjo Valiyaveetil Jose2
, Byjo Valiyaveetil Jose2 

 , Umasankar Parol3
, Umasankar Parol3 

 , Prem kumar Sasi2
, Prem kumar Sasi2 

 , Gorijavolu Sai Sree Krishna2
, Gorijavolu Sai Sree Krishna2 


1- Department of Neurosurgery, Government Medical College, Kozhikode, India. , drbinoytd@gmail.com
2- Department of Neurosurgery, Government Medical College, Kozhikode, India.
3- Department of Pathology, Government Medical College, Kozhikode, India.
2- Department of Neurosurgery, Government Medical College, Kozhikode, India.
3- Department of Pathology, Government Medical College, Kozhikode, India.
Full Text [PDF 3233 kb]
(1351 Downloads)
| Abstract (HTML) (2267 Views)
3. Discussion
Holcomb and Matson coined the term NC [4]. They are also known as intraspinal enterogenous cysts [5]. At the 3rd week of fetal development, NCs are derived from endodermal remnants during the period of notochordal formation. In about 50% of cases, NCs are associated with vertebral abnormalities, like spina bifida, cleft vertebra, hemivertebra, absent or fused vertebra, or diastematomyelia, and Klippel-Feil anomaly, as well as anomalies that may be fatal [1].
These cysts are observed in males twice as often as in females. The mean age of presentation is 22 years (range 1–59 years). It is very rare to see patients presenting after the age of 50 [5]. More than half of cases are located in the cervical region. In the spinal canal, the intradural extramedullary compartment is the most common location [1].
They commonly present with spine pain and radicular or myelopathic symptoms, such as neck pain, sphincter disturbances, quadriplegia, and paraplegia. It is a slowly progressive disease, and symptoms of acute onset are rare. A thoracic neurenteric cyst with a ten-day history of progressive weakness of the lower limbs was reported by Liu et al. in a 39-year-old female patient [5]. But our case had a rare presentation of acute onset of paraparesis, which occurred within 24 hours of admission due to spinal cord compression by an NC.
The oldest reported case of an NC was an 81-year-old male patient presenting with myelopathic symptoms in the upper limbs that had lasted for one year. The patient underwent partial excision of the NC at the C1-3 level [2]. Before this, Kim et al. reported the oldest patient with spinal NC, who was 72 years old [1]. But our case involved a septuagenarian (aged 71 to 80 years) who presented with symptoms at the age of 77.
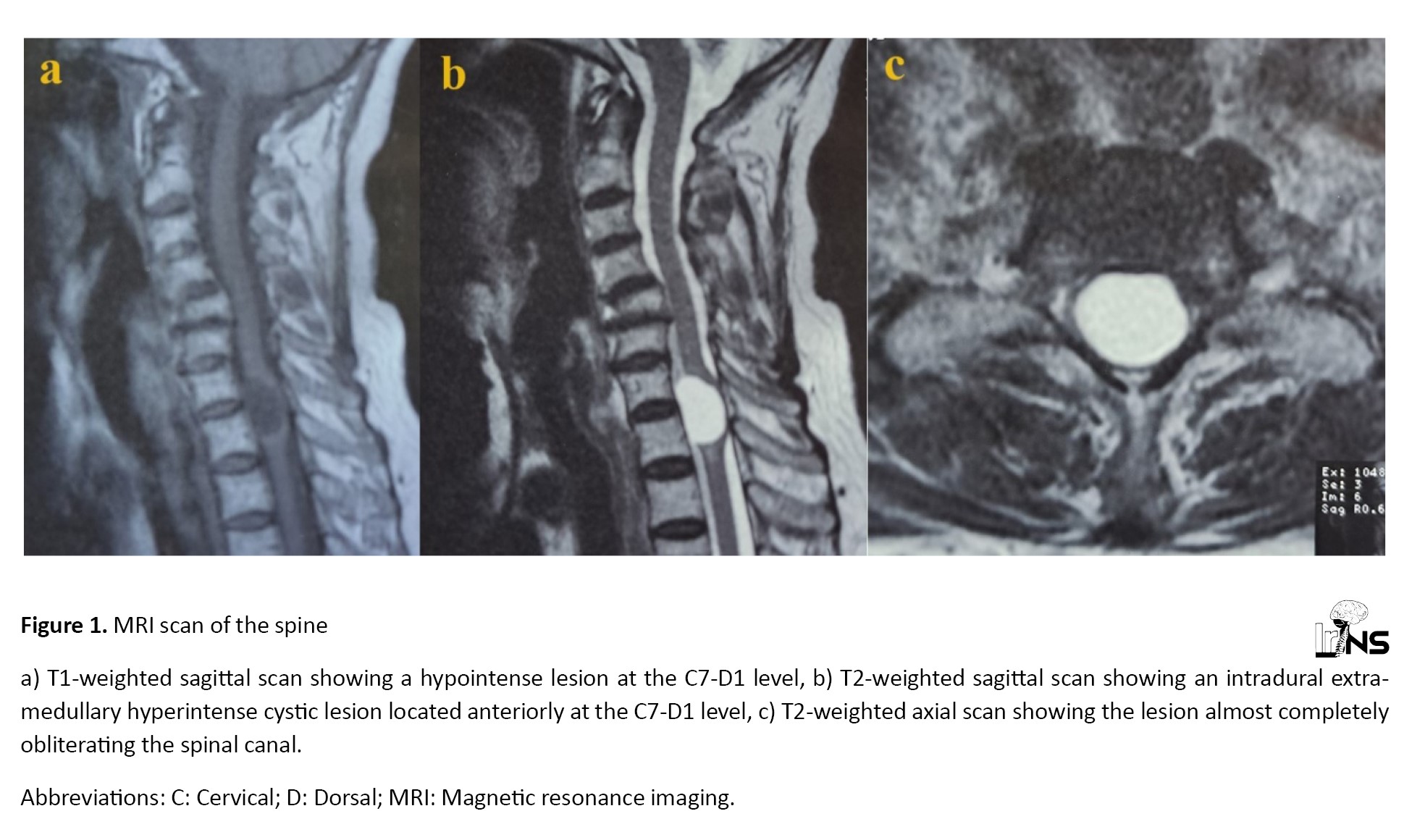
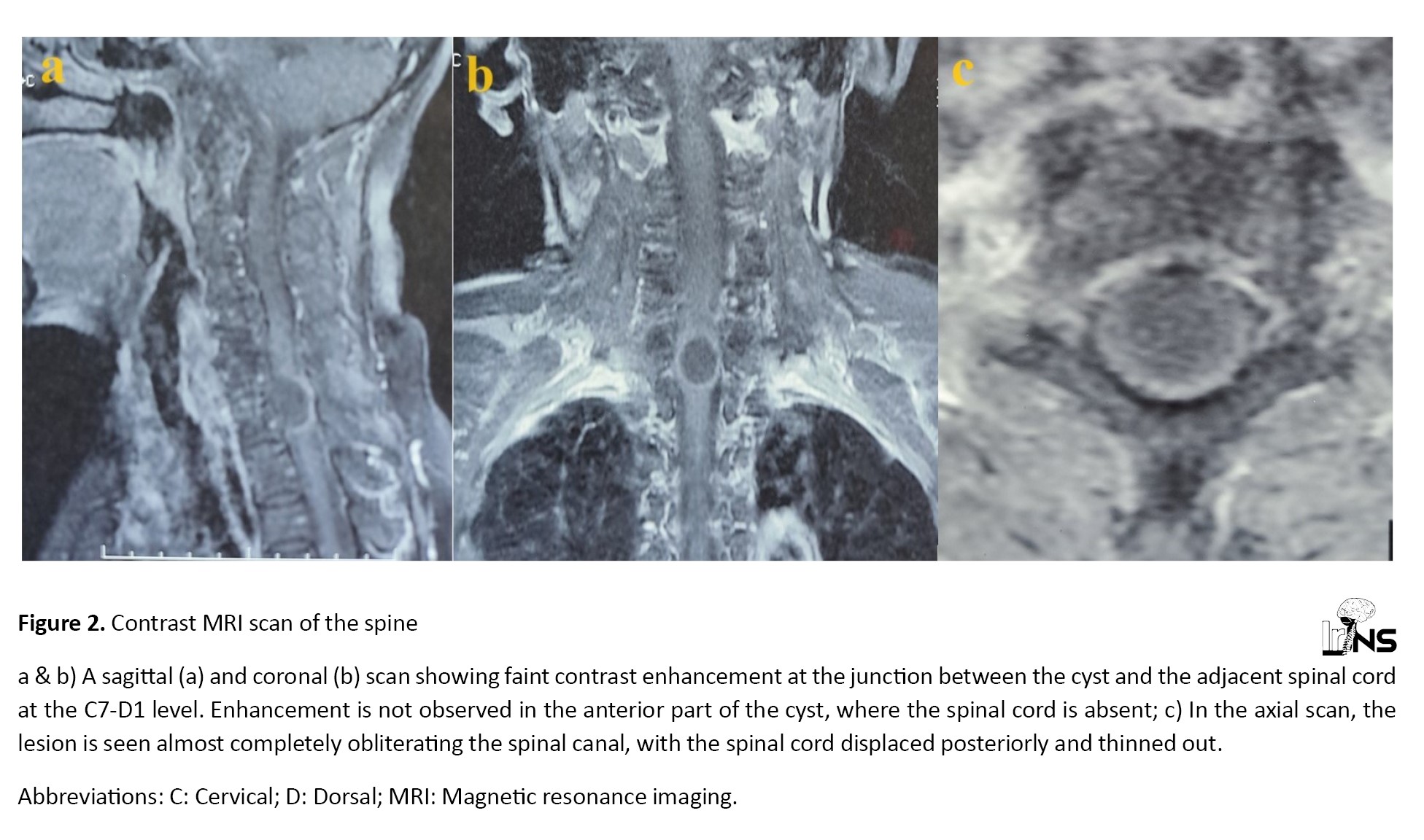
MRI is the investigation of choice. It shows a ventrally located T2 hyperintense, non-contrast-enhancing lesion. The T1-weighted image shows isointensity, hypointensity, or hyperintensity of the lesion, depending on the density of the content [6]. Frequent variations in the MRI findings are observed. An NC showing T1 hypointensity and T2 hyperintensity was reported by Nagi et al. [7]. One rare case of an NC mimicking an abscess with intense peripheral contrast enhancement were reported [8]. Preece et al. analyzed five cases of intracranial NCs with posterior rim enhancement at the junction with the brain parenchyma; however, this enhancement did not show any pathological correlation [9]. In this case, the cyst had a grayish-white thin wall and contained clear fluid. It showed hypointensity on the T1-weighted image and hyperintensity on the T2-weighted image. Contrast MRI revealed faint enhancement at the interface between the cyst and the adjacent spinal cord; however, this contrast rim enhancement of the cyst did not correlate with histological findings. An NC with vertebral anomalies can be diagnosed using a CT scan. The close differential diagnosis of an NC is an arachnoid cyst, which is located dorsal to the cord and shows T1 hypointensity and T2 hyperintensity [6].
Symptomatic patients are managed with surgical excision. Most symptoms disappear following surgery, except in a few cases where they recur or exacerbate [5]. The posterior approach is the most widely used technique due to fewer intraoperative complications. In this approach, the obscuring cord is manipulated, and the cyst is aspirated before excision. The anterior surgical approach reduces the risk of cyst rupture during surgery, thereby preventing leakage of contents; however, it increases surgical complexity, necessitates instrumented fusion, and raises the risk of complications. No postoperative improvement was seen in 18% of cases, and worsening of symptoms was documented in 11% of cases [3]. In the author’s case, the NC was located anteriorly at the C7-D1 level and was found to be displacing the spinal cord posteriorly. It was operated on using the posterior approach, and partial excision of the cyst wall was performed. The patient improved following the surgery. Total excision carries an excellent prognosis, but in older patients, it is safer to perform partial excision due to the adherence of the cyst to the spinal cord. The recurrence rates have ranged between 0% and 37% [5].
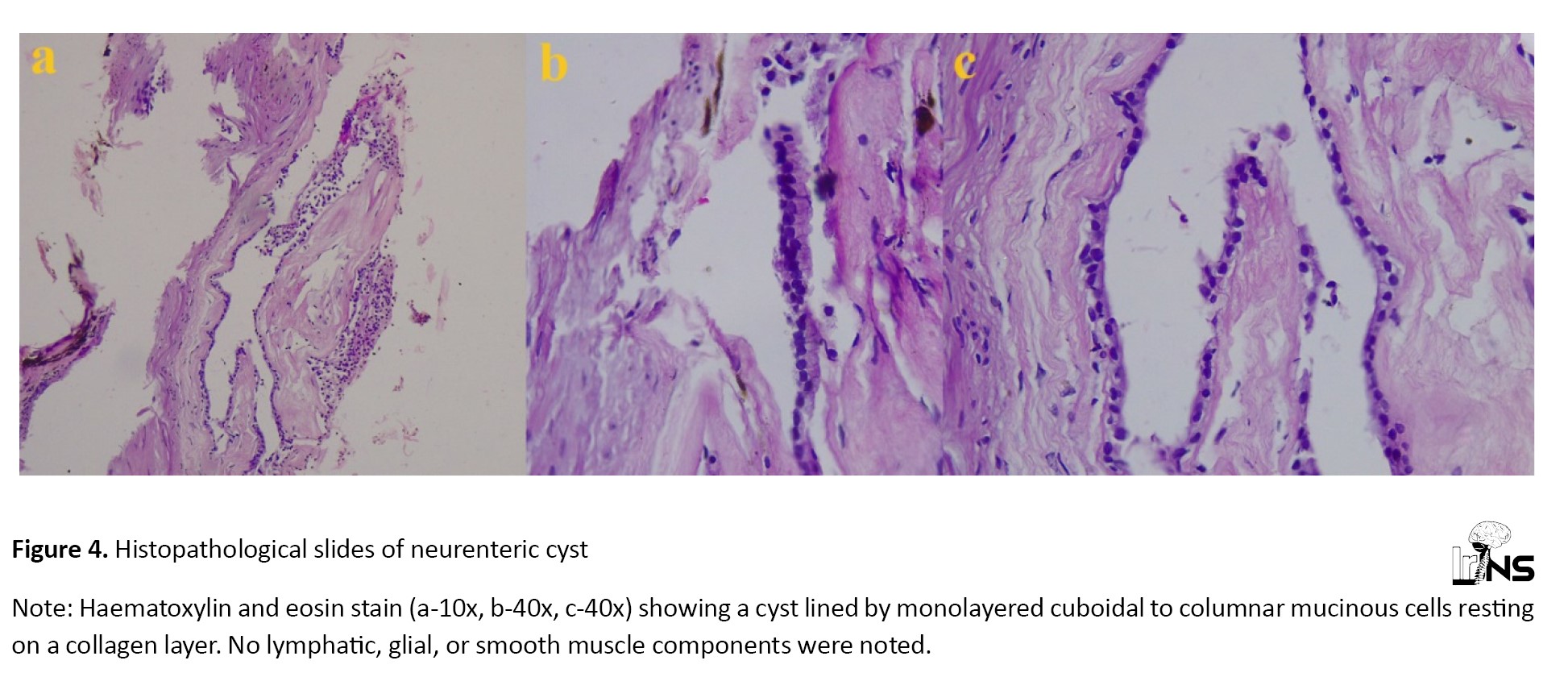
Hematoxylin and eosin staining of the NC showed a collection of mucin-producing simple columnar or cuboidal ciliated and non-ciliated goblet cells surrounding a central cystic cavity. Wilkins and Odom classified three histopathological presentations of NC. The author’s case exhibited the ‘Type A’ pattern proposed by Wilkins and Odom. Type A cysts contain either columnar or cuboidal cells, with ciliated and non-ciliated components atop a basal membrane composed of type IV collagen [3].
Our patient was a 77-year-old woman with a recent history of myocardial infarction (MI). She developed acute onset paraparesis due to spinal cord compression caused by an NC. This presented a difficult situation for the authors, as the cardiac risk was higher for this elderly patient with a recent MI if she underwent surgery in the prone position. Since surgery was unavoidable, the patient underwent surgery after receiving clearance from the cardiologist. She recovered well in the postoperative period. This is a very rare case of an NC presenting in a septuagenarian with acute onset paraparesis.
4. Conclusion
An anteriorly placed intradural cystic lesion at the C7-D1 level should raise the suspicion of a neurenteric cyst, even if the patient presents in the seventh decade of life. An MRI scan of an NC may show uncommon findings, such as T1 hypointensity and faint contrast enhancement of the cyst wall. In elderly patients, part of the cyst wall may be left behind if it is adhering to the spinal cord to avoid the risk of neurological deterioration.
Ethical Considerations
Compliance with ethical guidelines
Informed consent was obtained from the patient.
Funding
This case report did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conception and design: Binoy Damodar Thavara; Data collection: Binoy Damodar Thavara, Prem kumar Sasi, Gorijavolu Sai Sree Krishna; Data analysis and interpretation: Binoy Damodar Thavara, Byjo Valiyaveetil Jose, Umasankar Parol; Drafting the article: Binoy Damodar Thavara, Rajeev Mandaka Parambil, Byjo Valiyaveetil Jose; Supervision, review and editing: Binoy Damodar Thavara, Rajeev Mandaka Parambil; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interests.
Acknowledgements
The authors gratefully acknowledge the support of the Department of Neurosurgery, Government Medical College, Kozhikode, India.
References
Full Text: (2456 Views)
1. Background and Importance
Neurenteric cysts (NCs) are rare spinal malformations that account for 0.7 to 1.3% of spinal tumors and 16% of cysts [1]. During embryogenesis, endodermal remnants fail to separate from ectodermal counterparts, resulting in the formation of NCs. These cysts are more common in men and typically present during the first three decades of life. They occur rarely in elderly patients, with only two cases ever described in individuals over 70 years of age [2]. The majority of NCs show isointensity or mild hyperintensity on T1-weighted magnetic resonance imaging (MRI) scans. The intensity pattern depends on the protein content of the cyst. The cyst usually shows no contrast enhancement, and there is an absence of a mural nodule. These findings help differentiate NCs from more common spinal cord tumors [1]. Wilkins and Odom described three histopathological presentations of NC [3].
Here, we reported a case of a 77-year-old female patient presenting with acute onset of paraparesis due to spinal cord compression by an NC. This case exhibited hypointensity on T1-weighted imaging and faint contrast enhancement at the interface between the spinal cord and the cyst, which are atypical findings. An NC presenting in an elderly woman in her seventh decade of life with acute paraparesis is very rare.
2. Case Presentation
A 77-year-old female patient presented to the emergency department with acute onset left-sided chest pain of 1 day’s duration. She had a known history of hypertension and coronary artery disease for which she was receiving treatment. The patient was evaluated by a cardiologist and diagnosed with myocardial infarction. She was advised to start antiplatelet medications. While in the hospital, the patient developed acute onset weakness in both lower limbs within 24 hours of admission. Examination revealed Medical Research Committee (MRC) grade 1 power in the right lower limb and grade 2 power in the left lower limb. There was a decrease in sensation over the trunk and both lower limbs. The patient’s urinary bladder was catheterized. She underwent an MRI of the spine, which showed a 13.6×14.1×15.4 mm intradural extramedullary cystic lesion that was anteriorly located at the C7-D1 level. It was T1 hypointense and T2 hyperintense on MRI (Figure 1).
Neurenteric cysts (NCs) are rare spinal malformations that account for 0.7 to 1.3% of spinal tumors and 16% of cysts [1]. During embryogenesis, endodermal remnants fail to separate from ectodermal counterparts, resulting in the formation of NCs. These cysts are more common in men and typically present during the first three decades of life. They occur rarely in elderly patients, with only two cases ever described in individuals over 70 years of age [2]. The majority of NCs show isointensity or mild hyperintensity on T1-weighted magnetic resonance imaging (MRI) scans. The intensity pattern depends on the protein content of the cyst. The cyst usually shows no contrast enhancement, and there is an absence of a mural nodule. These findings help differentiate NCs from more common spinal cord tumors [1]. Wilkins and Odom described three histopathological presentations of NC [3].
Here, we reported a case of a 77-year-old female patient presenting with acute onset of paraparesis due to spinal cord compression by an NC. This case exhibited hypointensity on T1-weighted imaging and faint contrast enhancement at the interface between the spinal cord and the cyst, which are atypical findings. An NC presenting in an elderly woman in her seventh decade of life with acute paraparesis is very rare.
2. Case Presentation
A 77-year-old female patient presented to the emergency department with acute onset left-sided chest pain of 1 day’s duration. She had a known history of hypertension and coronary artery disease for which she was receiving treatment. The patient was evaluated by a cardiologist and diagnosed with myocardial infarction. She was advised to start antiplatelet medications. While in the hospital, the patient developed acute onset weakness in both lower limbs within 24 hours of admission. Examination revealed Medical Research Committee (MRC) grade 1 power in the right lower limb and grade 2 power in the left lower limb. There was a decrease in sensation over the trunk and both lower limbs. The patient’s urinary bladder was catheterized. She underwent an MRI of the spine, which showed a 13.6×14.1×15.4 mm intradural extramedullary cystic lesion that was anteriorly located at the C7-D1 level. It was T1 hypointense and T2 hyperintense on MRI (Figure 1).
Contrast MRI showed faint enhancement at the junction between the cyst and the spinal cord (Figure 2).
Contrast enhancement was not observed in the anterior part of the cyst, where the spinal cord was absent. The lesion was noted to be almost completely obliterating the spinal canal. The spinal cord was displaced posteriorly and thinned out, with adjacent cord signal changes. No other congenital abnormalities were observed on the MRI of the spine. In light of the anteriorly located cystic lesion at the C7-D1 level, the authors’ initial diagnosis was neurenteric cyst (NC), with arachnoid cyst as the differential diagnosis.
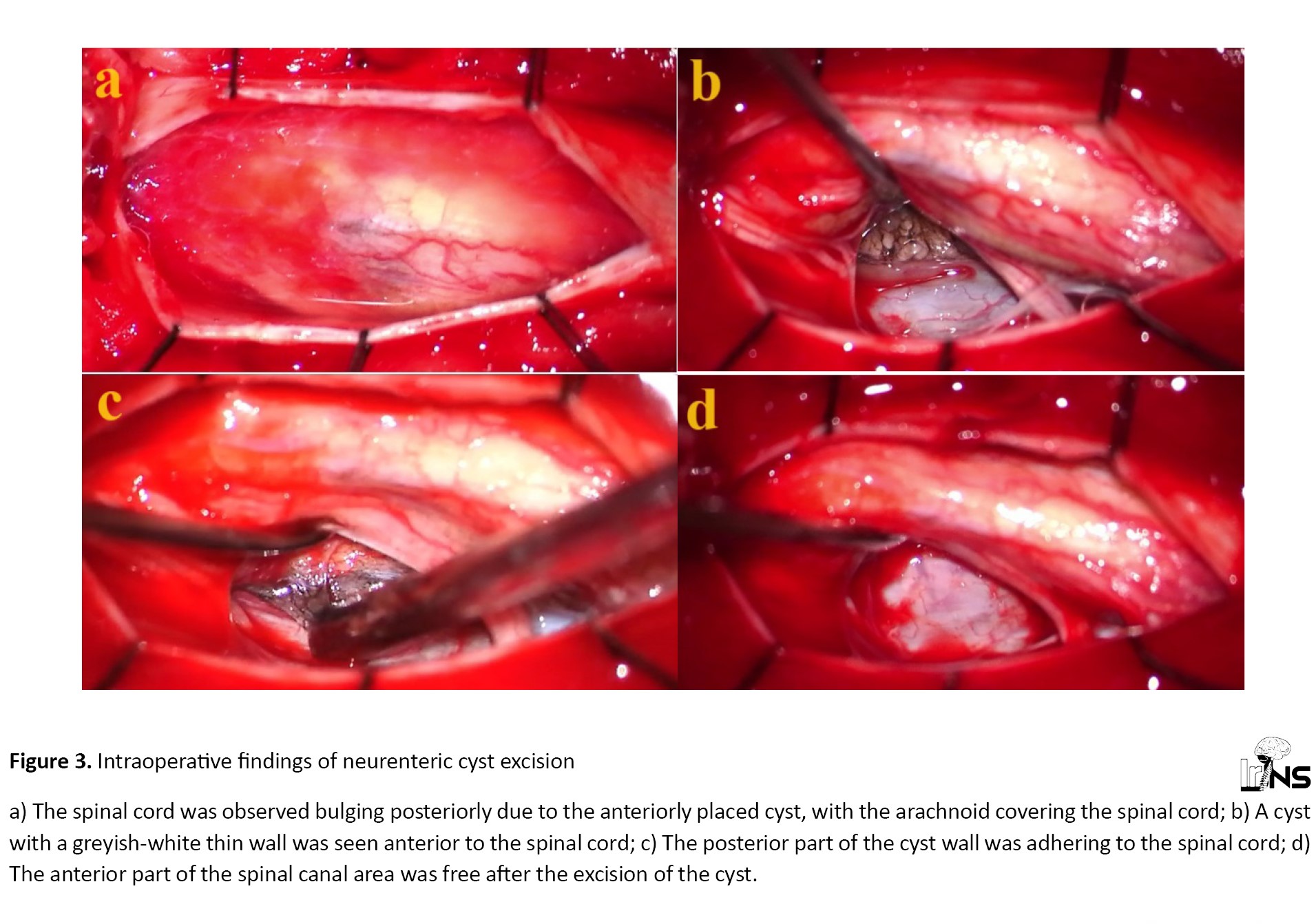
The patient underwent surgery in a prone position under general anesthesia. A C7-D1 laminectomy was done, and the dura was opened. The spinal cord was noted to be bulging posteriorly due to the anteriorly placed lesion (Figure 3a).
The patient underwent surgery in a prone position under general anesthesia. A C7-D1 laminectomy was done, and the dura was opened. The spinal cord was noted to be bulging posteriorly due to the anteriorly placed lesion (Figure 3a).
The arachnoid was opened, and cerebrospinal fluid (CSF) was drained. The lesion in the anterior part of the spinal cord was accessed from the left side of the spinal canal. The spinal cord was mobilized with care. A cyst with a greyish-white thin wall was observed in the spinal canal, displacing the spinal cord posteriorly (Figure 3b). It was identified as an intradural-extramedullary lesion. The cyst wall was opened, and clear fluid was drained. The posterior part of the cyst wall was adhering to the spinal cord (Figure 3c), but it was not adhering to the dura mater. Partial excision of the cyst wall was done, leaving a small portion adhering to the spinal cord. The C7-D1 spinal canal area was found to be free and lax after the excision of the cyst (Figure 3d). The dura mater was sutured, and the wound was closed in layers. At the 2-week follow-up, her power had improved to MRC grade 3 in both lower limbs. The patient was advised to continue physiotherapy. Histopathological examination using hematoxylin and eosin stain confirmed the diagnosis as a neurenteric cyst (NC), resembling the “Type A” pattern of NC proposed by Wilkins and Odum (Figure 4).
3. Discussion
Holcomb and Matson coined the term NC [4]. They are also known as intraspinal enterogenous cysts [5]. At the 3rd week of fetal development, NCs are derived from endodermal remnants during the period of notochordal formation. In about 50% of cases, NCs are associated with vertebral abnormalities, like spina bifida, cleft vertebra, hemivertebra, absent or fused vertebra, or diastematomyelia, and Klippel-Feil anomaly, as well as anomalies that may be fatal [1].
These cysts are observed in males twice as often as in females. The mean age of presentation is 22 years (range 1–59 years). It is very rare to see patients presenting after the age of 50 [5]. More than half of cases are located in the cervical region. In the spinal canal, the intradural extramedullary compartment is the most common location [1].
They commonly present with spine pain and radicular or myelopathic symptoms, such as neck pain, sphincter disturbances, quadriplegia, and paraplegia. It is a slowly progressive disease, and symptoms of acute onset are rare. A thoracic neurenteric cyst with a ten-day history of progressive weakness of the lower limbs was reported by Liu et al. in a 39-year-old female patient [5]. But our case had a rare presentation of acute onset of paraparesis, which occurred within 24 hours of admission due to spinal cord compression by an NC.
The oldest reported case of an NC was an 81-year-old male patient presenting with myelopathic symptoms in the upper limbs that had lasted for one year. The patient underwent partial excision of the NC at the C1-3 level [2]. Before this, Kim et al. reported the oldest patient with spinal NC, who was 72 years old [1]. But our case involved a septuagenarian (aged 71 to 80 years) who presented with symptoms at the age of 77.
MRI is the investigation of choice. It shows a ventrally located T2 hyperintense, non-contrast-enhancing lesion. The T1-weighted image shows isointensity, hypointensity, or hyperintensity of the lesion, depending on the density of the content [6]. Frequent variations in the MRI findings are observed. An NC showing T1 hypointensity and T2 hyperintensity was reported by Nagi et al. [7]. One rare case of an NC mimicking an abscess with intense peripheral contrast enhancement were reported [8]. Preece et al. analyzed five cases of intracranial NCs with posterior rim enhancement at the junction with the brain parenchyma; however, this enhancement did not show any pathological correlation [9]. In this case, the cyst had a grayish-white thin wall and contained clear fluid. It showed hypointensity on the T1-weighted image and hyperintensity on the T2-weighted image. Contrast MRI revealed faint enhancement at the interface between the cyst and the adjacent spinal cord; however, this contrast rim enhancement of the cyst did not correlate with histological findings. An NC with vertebral anomalies can be diagnosed using a CT scan. The close differential diagnosis of an NC is an arachnoid cyst, which is located dorsal to the cord and shows T1 hypointensity and T2 hyperintensity [6].
Symptomatic patients are managed with surgical excision. Most symptoms disappear following surgery, except in a few cases where they recur or exacerbate [5]. The posterior approach is the most widely used technique due to fewer intraoperative complications. In this approach, the obscuring cord is manipulated, and the cyst is aspirated before excision. The anterior surgical approach reduces the risk of cyst rupture during surgery, thereby preventing leakage of contents; however, it increases surgical complexity, necessitates instrumented fusion, and raises the risk of complications. No postoperative improvement was seen in 18% of cases, and worsening of symptoms was documented in 11% of cases [3]. In the author’s case, the NC was located anteriorly at the C7-D1 level and was found to be displacing the spinal cord posteriorly. It was operated on using the posterior approach, and partial excision of the cyst wall was performed. The patient improved following the surgery. Total excision carries an excellent prognosis, but in older patients, it is safer to perform partial excision due to the adherence of the cyst to the spinal cord. The recurrence rates have ranged between 0% and 37% [5].
Hematoxylin and eosin staining of the NC showed a collection of mucin-producing simple columnar or cuboidal ciliated and non-ciliated goblet cells surrounding a central cystic cavity. Wilkins and Odom classified three histopathological presentations of NC. The author’s case exhibited the ‘Type A’ pattern proposed by Wilkins and Odom. Type A cysts contain either columnar or cuboidal cells, with ciliated and non-ciliated components atop a basal membrane composed of type IV collagen [3].
Our patient was a 77-year-old woman with a recent history of myocardial infarction (MI). She developed acute onset paraparesis due to spinal cord compression caused by an NC. This presented a difficult situation for the authors, as the cardiac risk was higher for this elderly patient with a recent MI if she underwent surgery in the prone position. Since surgery was unavoidable, the patient underwent surgery after receiving clearance from the cardiologist. She recovered well in the postoperative period. This is a very rare case of an NC presenting in a septuagenarian with acute onset paraparesis.
4. Conclusion
An anteriorly placed intradural cystic lesion at the C7-D1 level should raise the suspicion of a neurenteric cyst, even if the patient presents in the seventh decade of life. An MRI scan of an NC may show uncommon findings, such as T1 hypointensity and faint contrast enhancement of the cyst wall. In elderly patients, part of the cyst wall may be left behind if it is adhering to the spinal cord to avoid the risk of neurological deterioration.
Ethical Considerations
Compliance with ethical guidelines
Informed consent was obtained from the patient.
Funding
This case report did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conception and design: Binoy Damodar Thavara; Data collection: Binoy Damodar Thavara, Prem kumar Sasi, Gorijavolu Sai Sree Krishna; Data analysis and interpretation: Binoy Damodar Thavara, Byjo Valiyaveetil Jose, Umasankar Parol; Drafting the article: Binoy Damodar Thavara, Rajeev Mandaka Parambil, Byjo Valiyaveetil Jose; Supervision, review and editing: Binoy Damodar Thavara, Rajeev Mandaka Parambil; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interests.
Acknowledgements
The authors gratefully acknowledge the support of the Department of Neurosurgery, Government Medical College, Kozhikode, India.
References
- Kim H, Min K, Kim Y, Kim D. Cervical intramedullary neurenteric cyst in an elderly patient.Journal of Korean Neurosurgical Society. 2004; 36:249-53. [Link]
- Kemp OAG, Deepak S, Salem O, Arzoglou V. The oldest presenting neurenteric cyst of the spinal cord. British Journal of Neurosurgery. 2023; 37(4):856-9. [DOI:10.1080/02688697.2019.1681361] [PMID]
- Savage JJ, Casey JN, McNeill IT, Sherman JH. Neurenteric cysts of the spine. Journal of Craniovertebral Junction & Spine. 2010; 1(1):58-63. [DOI:10.4103/0974-8237.65484] [PMID] [PMCID]
- Holcomb GW Jr, Matson DD. Thoracic neurenteric cyst. Surgery. 1954; 35(1):115-21. [PMID]
- Liu CX, Meng B, Li YB, Bai H, Wu ZX. A rare case of thoracic spinal intradural extramedullary enterogenous cyst with acute onset: Case report and literature review. Annals of the Royal College of Surgeons of England. 2019; 101(6):e142-6. [DOI:10.1308/rcsann.2019.0066] [PMID] [PMCID]
- Unnithan AKA. A case of neurenteric cyst of spine mimicking an arachnoid cyst. Spinal Cord Series and Cases. 2022; 8(1):31. [DOI:10.1038/s41394-022-00500-2] [PMID] [PMCID]
- Nagi S, Ghorbel D, Drissi C, Maatallah Y, Hammami N, Hamouda M. Intramedullary neurenteric cyst without concurrent malformation. Australasian Radiology. 2007; 51 Spec No.:B14-7. [PMID]
- Muzumdar D, Bhatt Y, Sheth J. Intramedullary cervical neurenteric cyst mimicking an abscess. Pediatric Neurosurgery. 2008; 44(1):55-61. [DOI:10.1159/000110664] [PMID]
- Preece MT, Osborn AG, Chin SS, Smirniotopoulos JG. Intracranial neurenteric cysts: Imaging and pathology spectrum. AJNR. American Journal of Neuroradiology. 2006; 27(6):1211-6. [PMID]
Type of Study: Case report |
Subject:
Basic Neurosurgery
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |