Sun, Dec 7, 2025
Volume 11 - Continuous Publishing
Iran J Neurosurg 2025, 11 - Continuous Publishing: 0-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hassani S H, Kazeminezhad A, Ghadirian H, Mouodi S. Osteochondroma as a Rare Cause of Lower Limb Radiculopathy: A Case Report. Iran J Neurosurg 2025; 11 : 4
URL: http://irjns.org/article-1-450-en.html
URL: http://irjns.org/article-1-450-en.html
1- Department of Neurosurgery, School of Medicine, Babol University of Medical Sciences, Babol, Iran.
2- Department of Neurosurgery, Peymanieh Hospital, Jahrom University of Medical Sciences, Jahrom, Iran.
3- Department of Neurosurgery, Sina Hospital, Tehran University of Medical Sciences, Tehran, Iran.
4- Social Determinants of Health Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran.
2- Department of Neurosurgery, Peymanieh Hospital, Jahrom University of Medical Sciences, Jahrom, Iran.
3- Department of Neurosurgery, Sina Hospital, Tehran University of Medical Sciences, Tehran, Iran.
4- Social Determinants of Health Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran.
Full Text [PDF 2390 kb]
(556 Downloads)
| Abstract (HTML) (2574 Views)
Full Text: (610 Views)
1. Background and Importance
Osteochondroma is a benign tumor caused by cartilage cells from the growth plate that remain on the bone surface [1, 2]. While osteochondromas of the long bones are frequent, intraspinal osteochondromas are relatively rare, accounting for only 1%–4% of all osteochondromas. The most common location of spinal osteochondroma is the cervical region (50%–58%) followed by thoracic spine [3-5]. It is more prevalent in men than women [4, 5].
The clinical manifestations of spinal osteochondroma vary from asymptomatic features and incidental tumor findings to radiculopathy, spinal cord compression, or physical deformity. The lesions may be solitary or multiple as part of hereditary multiple exostoses (HME) [5].
Asymptomatic solitary osteochondromas usually require no surgical intervention. In some patients with larger lesions, surgical management is recommended to provide marginal excision of the lesion from the base [2].
Here, we report a solitary intraspinal vertebral osteochondroma in the lumbar region presenting with right limb radiculopathy.
2. Case Presentation
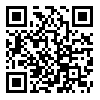
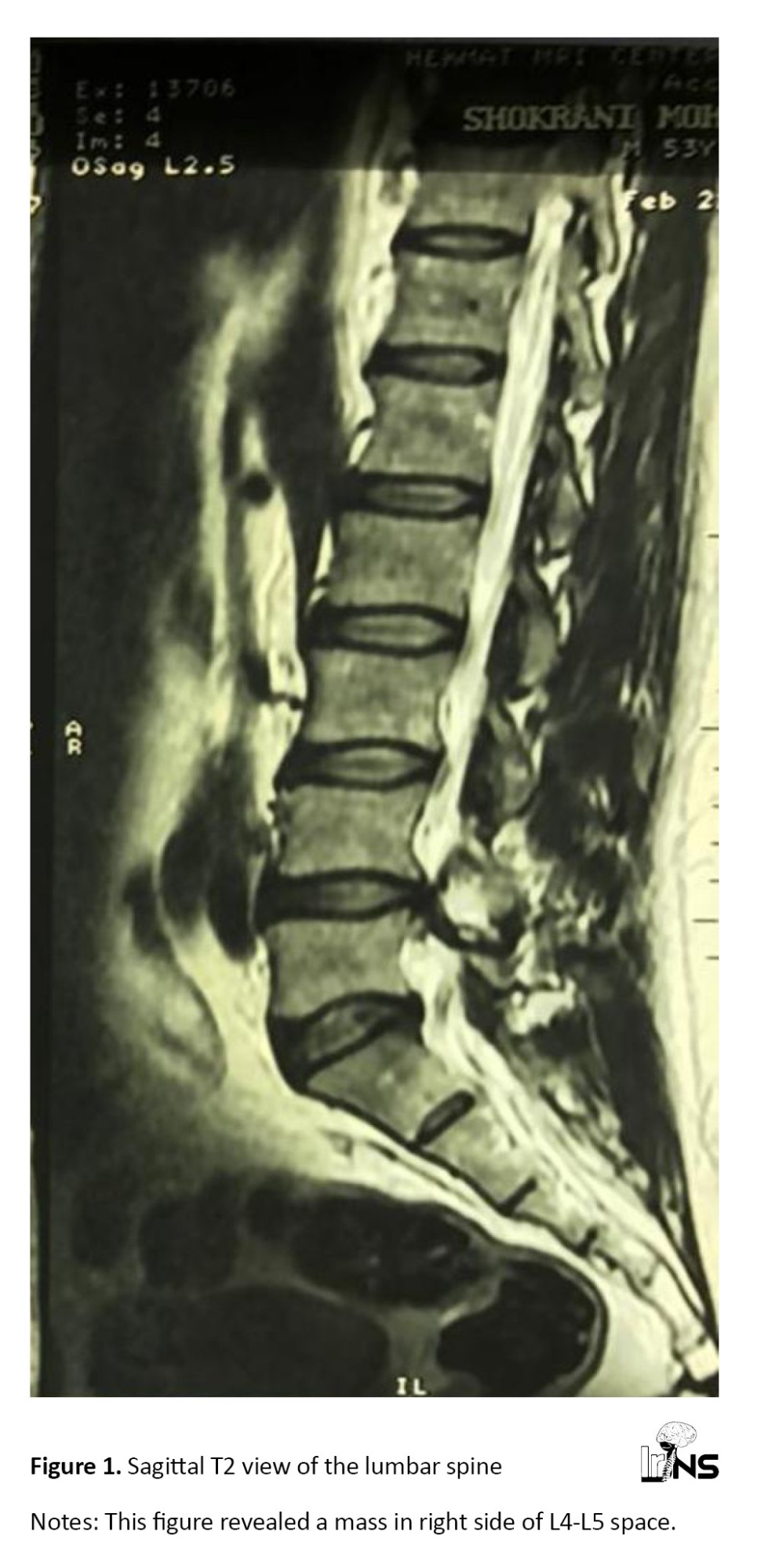
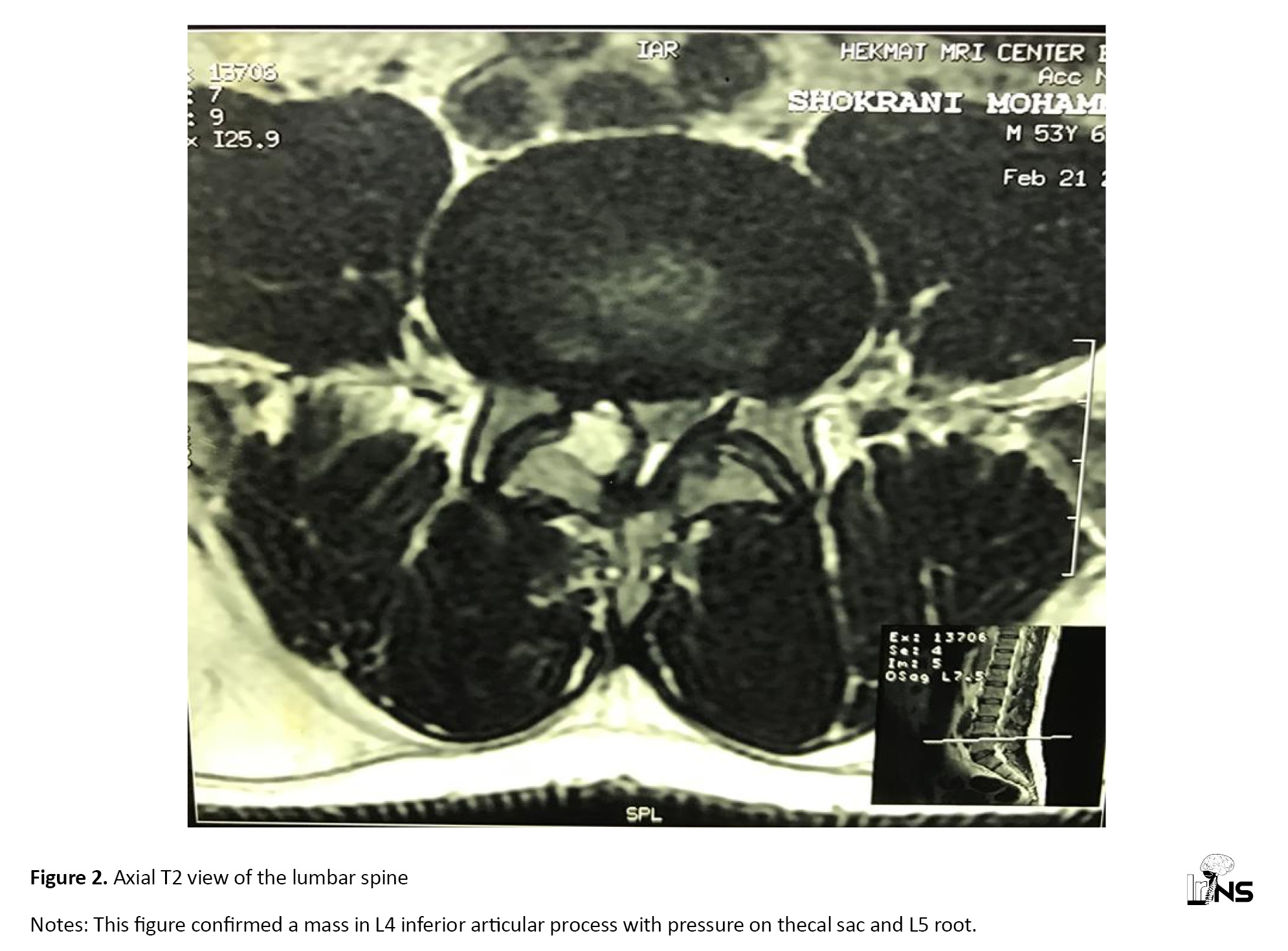
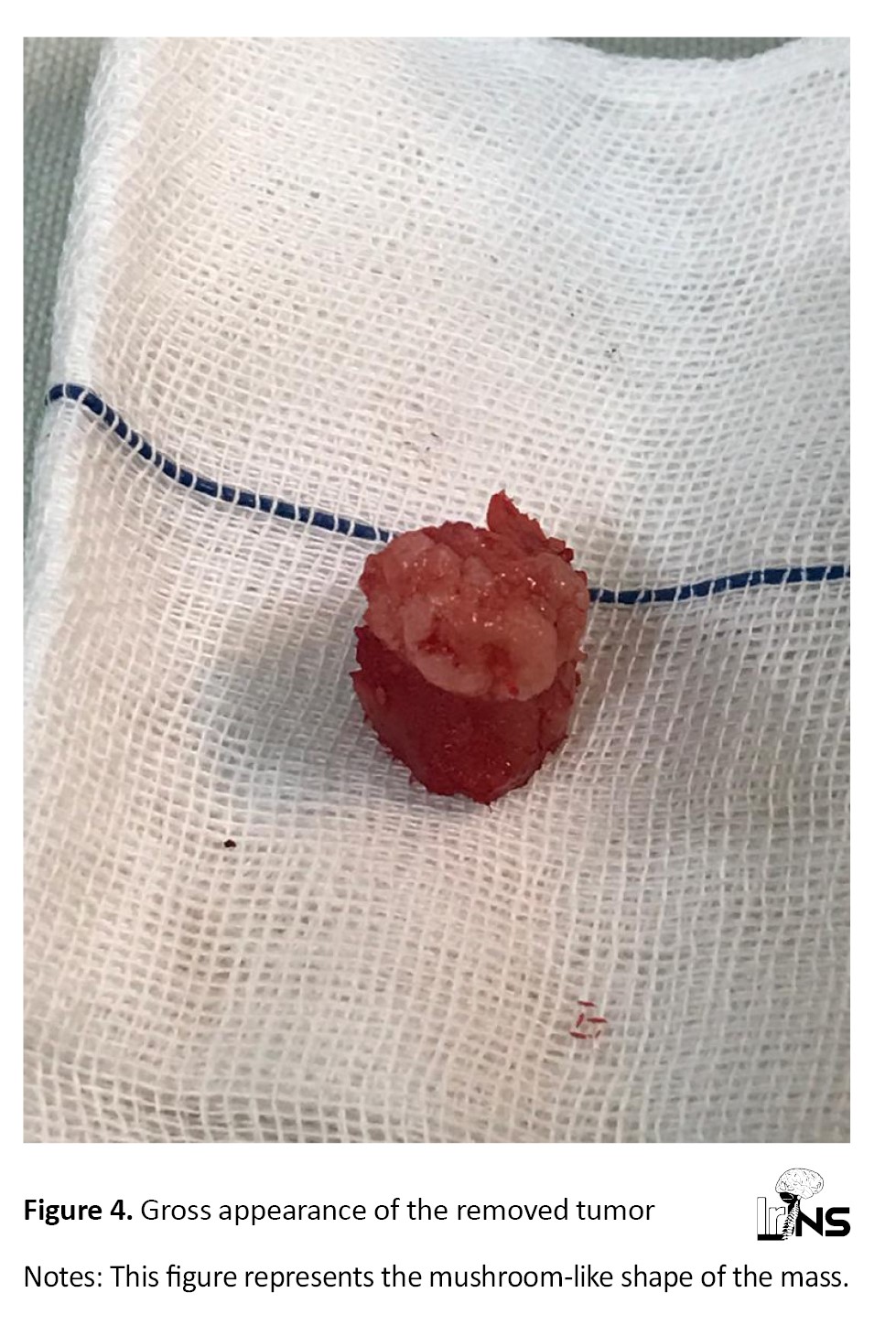
A 53-year-old male of Iranian ethnicity presented to our clinic with acute radiculopathy in the right lower limb for 10 days. The patient’s pain worsened daily; therefore, he was unable to walk when referred to our clinic. No previous history of physical or mental disorders has been reported. At the initial physical examination, the only clinical finding in the patient was a positive straight leg raise test. No further positive signs were found on physical examination. The patient’s pain did not respond to oral analgesics; therefore, we decided to hospitalize the patient for further evaluation. Following imaging, an extradural tumor was found on magnetic resonance imaging (MRI) that was medial to the right L4-L5 facet joint, involved the inferior articular process of L4, and had a compressive effect on the spinal canal and the right L5 root. This mass had high intensity in T2 views on MRI (Figures 1 and 2). Computed tomography (CT) revealed a solitary well-circumscribed bone tumor arising from the right inferior articular process of L4 with hypodensity in the central portion (Figure 3). Because the patient experienced severe pain and gait disturbance, we recommended surgical treatment. After obtaining informed consent from the patient, he underwent hemilaminectomy and medial facetectomy, and the mass was removed (Figure 4). The tumor had a mushroom-like shape and was completely attached to the underlying bone. Histopathological assessment of the removed bone mass confirmed a diagnosis of spinal osteochondroma.
Following surgery, the patient had no pain, and his complaints improved. The patient was followed up five years after surgery; fortunately, no symptoms or signs of recurrence were observed.
3. Discussion
Although osteochondroma is the most prevalent benign bone tumor, it occurs most commonly in long bones and rarely in spine. Osteochondroma can be associated with an inherited condition known as hereditary multiple exostosis or a solitary lesion, although the latter is more common than the former [2].
This patient was a 53-year-old man. Osteochondromas have male preponderance. These tumors are often asymptomatic and undiagnosed; therefore, their actual incidence remains unknown. Osteochondromas are most commonly present during the first four decades of life. Three of the four neoplasms were found before the age of 20 years [2].
This patient had a solitary lesion. Solitary osteochondromas are six times more common than hereditary multiple exostosis and account for 85% of all the presenting osteochondromas [1, 2].
In the present case, the lesion in the lumbar region (L4-L5) of the spinal column involved the facet joint with a compressive effect on the spinal canal and the right L5 root. The most common site of benign tumors in the spinal column is the cervical region. The most frequently involved parts of the spine are the spinous process, transverse process, vertebral body, pedicle, and rarely the facet joints [5]. Spinal involvement is more frequent in HME than in solitary osteochondroma. However, sacral involvement is rare. Cord compression rarely occurs in patients with osteochondroma, usually those with HME [1].
Our patient experienced severe pain due to L5 root compression. Spinal osteochondromas usually grow outside the spinal canal; therefore, cord compression is uncommon in these patients. If cord compression is present, different neurological manifestations can develop, such as radiating pain in the limbs, decreased muscle motor strength, numbness, paresthesia, and muscle atrophy [1]. Symptoms related to lumbar osteochondromas may be due to the involvement of the cauda equina, cauda equina syndrome, or compression of the root and the associated symptoms of radiculopathy.
MRI showed a cartilage cap thickness of less than 2 cm. The pathognomonic diagnostic feature of osteochondroma is the continuity between the cortex and medulla of the lesion and underlying bone. Pathologically, there is a cartilage cap and medullary continuity with the host bone. Osteochondroma can be sessile or pedunculated. Measurement of maximal cartilage cap thickness can be useful for detecting malignant transformation, and MRI is the best modality. A cartilage cap thickness >2 cm in adults and >3 cm in children may reflect cancerous transformation of the lesion [1].
Plain radiographs make the detection of osteochondroma difficult. CT and MRI are the best methods for detecting osteochondroma and imaging the exact morphology of a tumor. A CT scan can recognize the cartilaginous and osseous components of the lesion, and the extension of the tumor to the adjacent structures. MRI shows isointense lesions with a low-signal rim produced by the cortical bone. MRI is useful for detecting neurological compressions [1].
The patient then underwent surgery. Several treatment approaches have been proposed to osteochondroma. Conservative management is recommended for asymptomatic lesions, and surgical intervention should be considered in patients without a definitive diagnosis, painful lesions, or progressive neurological manifestations [1, 6].
Local recurrence following incomplete removal of osteochondroma occurs in 2%–5% of lesions, with an average recurrence time of approximately 5 years. Complete removal of the cartilaginous cap is essential to prevent recurrence [1, 5, 7, 8].
4. Conclusion
Although osteochondroma usually occurs in the cervical region, in this case, the lesion was observed in the lumbar region with clinical features of acute radiculopathy. Therefore, osteochondroma should be considered a differential diagnosis for lower-limb radiculopathies.
Ethical Considerations
Compliance with ethical guidelines
The patient gave written informed consent to the publication of this case report and any accompanying images.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results, and manuscript drafting. Each author approved the submission of the final version of the manuscript.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The cooperation of the patient for different aspects of this research is appreciated.
References
Osteochondroma is a benign tumor caused by cartilage cells from the growth plate that remain on the bone surface [1, 2]. While osteochondromas of the long bones are frequent, intraspinal osteochondromas are relatively rare, accounting for only 1%–4% of all osteochondromas. The most common location of spinal osteochondroma is the cervical region (50%–58%) followed by thoracic spine [3-5]. It is more prevalent in men than women [4, 5].
The clinical manifestations of spinal osteochondroma vary from asymptomatic features and incidental tumor findings to radiculopathy, spinal cord compression, or physical deformity. The lesions may be solitary or multiple as part of hereditary multiple exostoses (HME) [5].
Asymptomatic solitary osteochondromas usually require no surgical intervention. In some patients with larger lesions, surgical management is recommended to provide marginal excision of the lesion from the base [2].
Here, we report a solitary intraspinal vertebral osteochondroma in the lumbar region presenting with right limb radiculopathy.
2. Case Presentation
A 53-year-old male of Iranian ethnicity presented to our clinic with acute radiculopathy in the right lower limb for 10 days. The patient’s pain worsened daily; therefore, he was unable to walk when referred to our clinic. No previous history of physical or mental disorders has been reported. At the initial physical examination, the only clinical finding in the patient was a positive straight leg raise test. No further positive signs were found on physical examination. The patient’s pain did not respond to oral analgesics; therefore, we decided to hospitalize the patient for further evaluation. Following imaging, an extradural tumor was found on magnetic resonance imaging (MRI) that was medial to the right L4-L5 facet joint, involved the inferior articular process of L4, and had a compressive effect on the spinal canal and the right L5 root. This mass had high intensity in T2 views on MRI (Figures 1 and 2). Computed tomography (CT) revealed a solitary well-circumscribed bone tumor arising from the right inferior articular process of L4 with hypodensity in the central portion (Figure 3). Because the patient experienced severe pain and gait disturbance, we recommended surgical treatment. After obtaining informed consent from the patient, he underwent hemilaminectomy and medial facetectomy, and the mass was removed (Figure 4). The tumor had a mushroom-like shape and was completely attached to the underlying bone. Histopathological assessment of the removed bone mass confirmed a diagnosis of spinal osteochondroma.
Following surgery, the patient had no pain, and his complaints improved. The patient was followed up five years after surgery; fortunately, no symptoms or signs of recurrence were observed.
3. Discussion
Although osteochondroma is the most prevalent benign bone tumor, it occurs most commonly in long bones and rarely in spine. Osteochondroma can be associated with an inherited condition known as hereditary multiple exostosis or a solitary lesion, although the latter is more common than the former [2].
This patient was a 53-year-old man. Osteochondromas have male preponderance. These tumors are often asymptomatic and undiagnosed; therefore, their actual incidence remains unknown. Osteochondromas are most commonly present during the first four decades of life. Three of the four neoplasms were found before the age of 20 years [2].
This patient had a solitary lesion. Solitary osteochondromas are six times more common than hereditary multiple exostosis and account for 85% of all the presenting osteochondromas [1, 2].
In the present case, the lesion in the lumbar region (L4-L5) of the spinal column involved the facet joint with a compressive effect on the spinal canal and the right L5 root. The most common site of benign tumors in the spinal column is the cervical region. The most frequently involved parts of the spine are the spinous process, transverse process, vertebral body, pedicle, and rarely the facet joints [5]. Spinal involvement is more frequent in HME than in solitary osteochondroma. However, sacral involvement is rare. Cord compression rarely occurs in patients with osteochondroma, usually those with HME [1].
Our patient experienced severe pain due to L5 root compression. Spinal osteochondromas usually grow outside the spinal canal; therefore, cord compression is uncommon in these patients. If cord compression is present, different neurological manifestations can develop, such as radiating pain in the limbs, decreased muscle motor strength, numbness, paresthesia, and muscle atrophy [1]. Symptoms related to lumbar osteochondromas may be due to the involvement of the cauda equina, cauda equina syndrome, or compression of the root and the associated symptoms of radiculopathy.
MRI showed a cartilage cap thickness of less than 2 cm. The pathognomonic diagnostic feature of osteochondroma is the continuity between the cortex and medulla of the lesion and underlying bone. Pathologically, there is a cartilage cap and medullary continuity with the host bone. Osteochondroma can be sessile or pedunculated. Measurement of maximal cartilage cap thickness can be useful for detecting malignant transformation, and MRI is the best modality. A cartilage cap thickness >2 cm in adults and >3 cm in children may reflect cancerous transformation of the lesion [1].
Plain radiographs make the detection of osteochondroma difficult. CT and MRI are the best methods for detecting osteochondroma and imaging the exact morphology of a tumor. A CT scan can recognize the cartilaginous and osseous components of the lesion, and the extension of the tumor to the adjacent structures. MRI shows isointense lesions with a low-signal rim produced by the cortical bone. MRI is useful for detecting neurological compressions [1].
The patient then underwent surgery. Several treatment approaches have been proposed to osteochondroma. Conservative management is recommended for asymptomatic lesions, and surgical intervention should be considered in patients without a definitive diagnosis, painful lesions, or progressive neurological manifestations [1, 6].
Local recurrence following incomplete removal of osteochondroma occurs in 2%–5% of lesions, with an average recurrence time of approximately 5 years. Complete removal of the cartilaginous cap is essential to prevent recurrence [1, 5, 7, 8].
4. Conclusion
Although osteochondroma usually occurs in the cervical region, in this case, the lesion was observed in the lumbar region with clinical features of acute radiculopathy. Therefore, osteochondroma should be considered a differential diagnosis for lower-limb radiculopathies.
Ethical Considerations
Compliance with ethical guidelines
The patient gave written informed consent to the publication of this case report and any accompanying images.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results, and manuscript drafting. Each author approved the submission of the final version of the manuscript.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The cooperation of the patient for different aspects of this research is appreciated.
References
- Tepelenis K, Papathanakos G, Kitsouli A, Troupis T, Barbouti A, Vlachos K, et al. Osteochondromas: An updated review of epidemiology, pathogenesis, clinical presentation, radiological features and treatment options. In vivo (Athens, Greece). 2021; 35(2):681-91. [DOI:10.21873/invivo.12308] [PMID]
- Alabdullrahman LW, Mabrouk A, Byerly DW. Osteochondroma. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. [PMID]
- Fowler J, Takayanagi A, Fiani B, Cathel A, Sarhadi KJ, Arshad M, et al. Diagnosis, management, and treatment options: A cervical Spine osteochondroma meta-analysis. World Neurosurgery. 2021; 149:215-25.e6. [DOI:10.1016/j.wneu.2021.01.148] [PMID]
- Riahi H, Mechri M, Barsaoui M, Bouaziz M, Vanhoenacker F, Ladeb M. Imaging of benign Tumors of the Osseous Spine. Journal of the Belgian Society of Radiology. 2018; 102(1):13. [DOI:10.5334/jbsr.1380] [PMID]
- Sinelnikov A, Kale H. Osteochondromas of the spine. Clinical Radiology. 2014; 69(12):e584-90. [DOI:10.1016/j.crad.2014.08.017] [PMID]
- Sakai Y, Nakashima H, Takatsu T, Imagama S. Clinical features and surgical outcomes of osteochondroma of the Spine. Malaysian orthopaedic journal. 2023; 17(1):117-23. [DOI:10.5704/MOJ.2303.014] [PMID]
- Sciubba DM, Macki M, Bydon M, Germscheid NM, Wolinsky JP, Boriani S, et al. Long-term outcomes in primary spinal osteochondroma: A multicenter study of 27 patients. Journal of Neurosurgery. Spine. 2015; 22(6):582-8. [DOI:10.3171/2014.10.SPINE14501] [PMID]
- Zaijun L, Xinhai Y, Zhipeng W, Wending H, Quan H, Zhenhua Z, et al. Outcome and prognosis of myelopathy and radiculopathy from osteochondroma in the mobile spine: A report on 14 patients. Journal of Spinal Disorders & Techniques. 2013; 26(4):194-9. [DOI:10.1097/BSD.0b013e31823eb239] [PMID]
Type of Study: Case report |
Subject:
Spine
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |