Sat, Apr 27, 2024
Volume 4, Issue 3 (Summer 2018)
Iran J Neurosurg 2018, 4(3): 167-172 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Gaye M, Sakho Y, Moumouni A K, Aidara C M, Jalloh M, Latif A. Anatomo-Radiological Patterns of the Tethered Spinal Cord With Lipoma. Iran J Neurosurg 2018; 4 (3) :167-172
URL: http://irjns.org/article-1-99-en.html
URL: http://irjns.org/article-1-99-en.html
Magatte Gaye * 

 1, Youssoupha Sakho2
1, Youssoupha Sakho2 
 , Abd-El Kader Moumouni2
, Abd-El Kader Moumouni2 
 , Cherif Mohamadou Aidara3
, Cherif Mohamadou Aidara3 
 , Mohamed Jalloh4
, Mohamed Jalloh4 
 , Amadou Latif4
, Amadou Latif4 



 1, Youssoupha Sakho2
1, Youssoupha Sakho2 
 , Abd-El Kader Moumouni2
, Abd-El Kader Moumouni2 
 , Cherif Mohamadou Aidara3
, Cherif Mohamadou Aidara3 
 , Mohamed Jalloh4
, Mohamed Jalloh4 
 , Amadou Latif4
, Amadou Latif4 

1- Department of Neurosurgery, Hospital General Grand Yoff, Dakar, Senegal , magou762003@yahoo.fr
2- Department of Neurosurgery, Hospital General Grand Yoff, Dakar, Senegal
3- Department of Radiology, Hospital Pikine, Dakar, Senegal
4- Department of Urology, Hospital General Grand Yoff, Dakar, Senegal
2- Department of Neurosurgery, Hospital General Grand Yoff, Dakar, Senegal
3- Department of Radiology, Hospital Pikine, Dakar, Senegal
4- Department of Urology, Hospital General Grand Yoff, Dakar, Senegal
Full Text [PDF 826 kb]
(1455 Downloads)
| Abstract (HTML) (4148 Views)
Full Text: (2085 Views)
Highlights
• Median lumbar sacral dermatologic markers in childhood and infancy are highly suggestive of the tethered spinal cord with lipoma.
• It is difficult to assess the natural history of the malformation regarding the risk of vesical sphincterian and neuro-orthopedic deterioration.
• MRI has remained the gold standard diagnostic tool but it is still difficult to clearly define the demarcation line between lipoma and neural structure.
• It is hazardous to try to completely remove the lipoma rather it is better to leave a remnant of lipoma stuck to the neural placodes.
Plain Language Summary
In this article, we report our experience on the management of tethered spinal cord with lipoma that is usually stuck to the distal part of the spinal cord, though during the process of the growth a progressive stretching phenomenon occurs. The deleterious consequence is progressive suffering of the spinal cord with deterioration of lower limb function and sphincter disturbance. The goal of the operation is to untether the cord. This study was conducted at a University hospital in Dakar, Senegal. During 4 years, 8 patients with spinal cord lipoma underwent surgery. All patients were symptomatic and their diagnosis was confirmed with spinal cord ultrasound, CT scan, or MRI. But MRI is the gold standard diagnostic tool. However, it is only during operation that you can definitely know the type of attachment between lipoma and the cord. To avoid traumatizing neural structure during surgery, we recommend to leave a remnant of lipoma stuck to the spinal cord and to realize a watertight closure. Postoperative follow-up was good for 5 cases and unsatisfactory in 3 cases with persistent sensory-motor disorders.
1. Introduction
Tethered spinal cord with lipoma, also called spinal lipoma, belongs to occult dysraphism group. Its prevalence has been reported between 4.7% and 16% of all neural tube defects [1]. The epidemiological profile may be underestimated because some of them remain asymptomatic [2].
In the absence of these dermatological markers, the diagnosis is challenging but it may be suggested through vesico-sphincteric and or neuro-orthopedic dysfunction. MRI is the gold standard to study the critical relationship between the lipoma and the neural structure and describe the different anatomo-radiological patterns, second to assess the degree of the cord fixation. In addition, it allows good surgical planning for safe removal of the lesion of the tethered spinal cord with lipoma.
2. Methods & Materials/ Patients
We conducted a retrospective and descriptive study at the Department of Neurosurgery of General Grand Yoff Hospital and the Neurosurgical Clinic at Fann University Hospital of Dakar, Senegal. Out of all patients operated on for dysraphism from July 2007 to January 2011 (n=62), those with myelomeningocele were excluded and only patients with spinal lipoma were included in the study. Finally, 8 patients with tethered spinal cord associated with lipoma underwent surgery. As this study used all of the eligible statistical population, sampling was not applicable. Clinical assessment and neuroimaging were carried out for all subjects using spinal cord ultrasound, spinal X-rays, CT, and MRI, and finally, the surgical findings were also analyzed. The demographic characteristics and different anatomo-clinical and radiological patterns were identified; we reviewed the literature and used modified Chapman classification to assess the degree of intermingling of the lipoma with the spinal cord and roots [1].
3. Results
Our study included 7 (87.5%) infants with a mean age of 15 months and an adult (12.5%) aged 30 years old. The male/female ratio was 0.6. Clinically, lumbosacral skin abnormalities like subcutaneous lipoma were present in 7 (87.5%) patients. One patient had a subcutaneous lipoma and an adjacent midline dimple and in the others, the lipoma was associated with caudal appendage and skin spots. Orthopedic deformities were noted in 5 (62.5%) patients. In particular, a clubfoot was found in 4 cases and scoliosis in one case. The motor deficit was observed in 2 (25%) patients, with one case of paraplegia and one case of para-paresis.
The sensory deficit was present in one (12.5%) case. Sphincter disorders were reported in 2 (25%) patients. The lumbar spine plain X-ray was performed only for one (12.5%) patient. Dorso-lumbar scoliosis, dehiscence of the posterior arches of the L1, L2, and L3 spinous processes, and spinal canal widening and scalloping were observed, too (Figure 1). Spinal cord ultrasound was performed for 2 (25%) patients aged 45 days and 5 months, and a low position at L5 of the conus medullaris and a subcutaneous lipoma connected to neural structures were found (Figure 2).
• Median lumbar sacral dermatologic markers in childhood and infancy are highly suggestive of the tethered spinal cord with lipoma.
• It is difficult to assess the natural history of the malformation regarding the risk of vesical sphincterian and neuro-orthopedic deterioration.
• MRI has remained the gold standard diagnostic tool but it is still difficult to clearly define the demarcation line between lipoma and neural structure.
• It is hazardous to try to completely remove the lipoma rather it is better to leave a remnant of lipoma stuck to the neural placodes.
Plain Language Summary
In this article, we report our experience on the management of tethered spinal cord with lipoma that is usually stuck to the distal part of the spinal cord, though during the process of the growth a progressive stretching phenomenon occurs. The deleterious consequence is progressive suffering of the spinal cord with deterioration of lower limb function and sphincter disturbance. The goal of the operation is to untether the cord. This study was conducted at a University hospital in Dakar, Senegal. During 4 years, 8 patients with spinal cord lipoma underwent surgery. All patients were symptomatic and their diagnosis was confirmed with spinal cord ultrasound, CT scan, or MRI. But MRI is the gold standard diagnostic tool. However, it is only during operation that you can definitely know the type of attachment between lipoma and the cord. To avoid traumatizing neural structure during surgery, we recommend to leave a remnant of lipoma stuck to the spinal cord and to realize a watertight closure. Postoperative follow-up was good for 5 cases and unsatisfactory in 3 cases with persistent sensory-motor disorders.
1. Introduction
Tethered spinal cord with lipoma, also called spinal lipoma, belongs to occult dysraphism group. Its prevalence has been reported between 4.7% and 16% of all neural tube defects [1]. The epidemiological profile may be underestimated because some of them remain asymptomatic [2].
In the absence of these dermatological markers, the diagnosis is challenging but it may be suggested through vesico-sphincteric and or neuro-orthopedic dysfunction. MRI is the gold standard to study the critical relationship between the lipoma and the neural structure and describe the different anatomo-radiological patterns, second to assess the degree of the cord fixation. In addition, it allows good surgical planning for safe removal of the lesion of the tethered spinal cord with lipoma.
2. Methods & Materials/ Patients
We conducted a retrospective and descriptive study at the Department of Neurosurgery of General Grand Yoff Hospital and the Neurosurgical Clinic at Fann University Hospital of Dakar, Senegal. Out of all patients operated on for dysraphism from July 2007 to January 2011 (n=62), those with myelomeningocele were excluded and only patients with spinal lipoma were included in the study. Finally, 8 patients with tethered spinal cord associated with lipoma underwent surgery. As this study used all of the eligible statistical population, sampling was not applicable. Clinical assessment and neuroimaging were carried out for all subjects using spinal cord ultrasound, spinal X-rays, CT, and MRI, and finally, the surgical findings were also analyzed. The demographic characteristics and different anatomo-clinical and radiological patterns were identified; we reviewed the literature and used modified Chapman classification to assess the degree of intermingling of the lipoma with the spinal cord and roots [1].
3. Results
Our study included 7 (87.5%) infants with a mean age of 15 months and an adult (12.5%) aged 30 years old. The male/female ratio was 0.6. Clinically, lumbosacral skin abnormalities like subcutaneous lipoma were present in 7 (87.5%) patients. One patient had a subcutaneous lipoma and an adjacent midline dimple and in the others, the lipoma was associated with caudal appendage and skin spots. Orthopedic deformities were noted in 5 (62.5%) patients. In particular, a clubfoot was found in 4 cases and scoliosis in one case. The motor deficit was observed in 2 (25%) patients, with one case of paraplegia and one case of para-paresis.
The sensory deficit was present in one (12.5%) case. Sphincter disorders were reported in 2 (25%) patients. The lumbar spine plain X-ray was performed only for one (12.5%) patient. Dorso-lumbar scoliosis, dehiscence of the posterior arches of the L1, L2, and L3 spinous processes, and spinal canal widening and scalloping were observed, too (Figure 1). Spinal cord ultrasound was performed for 2 (25%) patients aged 45 days and 5 months, and a low position at L5 of the conus medullaris and a subcutaneous lipoma connected to neural structures were found (Figure 2).
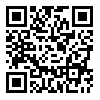
The Computed Tomography (CT) of the lumbar spine was performed for 2 patients which indicated dehiscence of the posterior vertebral arches. Lipoma was associated with presacral anterior meningocele in one case (Figure 3). CT findings confirmed the association with lumbar scoliosis in another case. MRI was performed for 4 patients and resulted in one case of filum terminale lipoma (Figure 4) and 3 cases of conus medullaris lipoma.
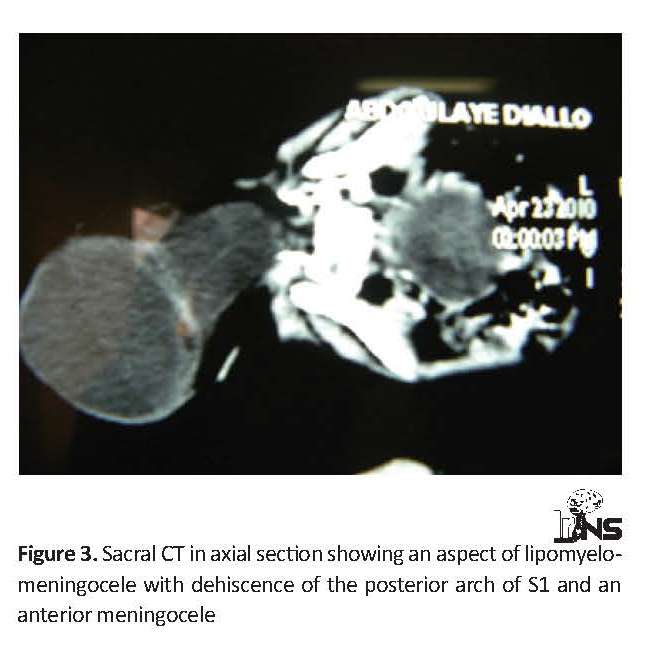
The tethered spinal cord was noted in all patients with low-lying conus medullaris. The level of insertion in 3 cases was L5 and in one case L4. Dehiscence of posterior lumbar and or sacral arches was found in 4 cases and scalloping of the posterior wall of L5 in one case. A combination of a conus medullaris lipoma and a retrocerebellar arachnoid cyst was found in one case (Figure 5). All patients underwent surgery which revealed 7 cases of conus medullaris lipoma and one case of filum terminale. According to surgical findings and Chapman modified classification [3] in the group of the conus medullaris lipoma, we described 4 cases of dorsal form, 2 cases of transitional, and 1 case of complex form. Postoperative follow-up was good in 5 cases and unsatisfactory in 3 cases with persistent sensory-motor disorders.
4. Discussion
Spinal dysraphism is due to perturbation of the embryological development of the caudal neural tube and the surrounding tissues [2, 3]. Regarding the spinal lipoma, several pathophysiological hypotheses have been presented, for example, it is a neurulation disorder, a defect of induction occurring after the phenomena of neurulation. Or it could be a post-neurulation disorder related to caudal pole abnormalities [4]. Spinal lipoma has remained a rare disease. We had recorded 2.28 cases per year in our study.
In France, the incidence is estimated to be 70 new cases per year [4]. In fact, the frequency of spinal lipoma has remained uncertain because the number of asymptomatic patients is unknown. Most often, the diagnosis is easily made at birth in the setting of lumbosacral cutaneous abnormalities. In our cases, the diagnosis was made essentially in infancy based on the diagnostic criteria described in the literature [5, 6].
In one of our patients, the diagnosis was made during adulthood (30 years of age) because of the late onset of vesico-sphincter dysfunction. The pathogenesis of these delayed symptoms may be because of the fact that during body growth a slow process of stretching occurs on the conus medullaris due to its fixation [5]. However, some patients remain asymptomatic during all their life. The clinical presentation comprises a symptomatic triad; a cutaneous marker like subcutaneous lump sometimes with a dimple or caudal appendicular, neuro-orthopedic deformities, and vesico-sphincteric dysfunction which is characteristic of spinal lipoma. However, in the absence of medio-lumbar skin signs, the diagnosis is more difficult and often delayed. The disease manifests itself by the progressive appearance of a vesico-sphincteric and or neuro-orthopedic dysfunction [7, 8].
Neuroimaging plays an important role in the complete investigation of this occult dysraphism. Antenatal diagnosis of the tethered spinal cord with lipoma can be made by ultrasound examination [9]. Spinal cord ultrasound provides the relevant information on newborns’ spinal cord and on infants less than 2 months [2]. In our study, the imaging was performed on two infants and provided very accurate information on the dehiscence of the posterior arch, suggesting the low-lying cord at L5.
X-ray images of the lumbosacral spine confirmed the dehiscence of posterior lumbar and or sacral vertebral arches [5, 9]. Other vertebral bone deformities and anomalies of the spine may be found, too. However, it does not detect lipoma and spinal cord lesions. All in all, it is a good diagnostic tool in any patient with suspicion of occult dysraphism. In our series, the standard X-ray showed dehiscence of the posterior arches. According to some studies [5, 6, 10], radiography along with myelography is an essential step for the diagnosis of spinal lipoma. Currently, myelography is practically abandoned in the diagnosis of spinal lipoma because of its invasiveness. When it is performed, the myelography shows an enlargement of the dural sheath facing the vertebral bodies where the lesion is located [10].
Spinal cord ultrasound provides the relevant information on newborns’ spinal cord and on infants less than 2 months [4]. In our series, it was possible to specify the insertion of the conus medullaris at L5, to describe the anatomical pattern of the lipoma and to detect dehiscence of the lumbar posterior vertebral arches. Antenatal diagnosis of the tethered spinal cord with lipoma could be made by ultrasound examination [11].
CT of the lumbosacral spine remains interesting in the absence of MRI. The lipoma appears at CT as a low-density lesion like an additional image in the vertebral canal [10]. CT can be combined with intrathecal injection of contrast to better visualize the nerve roots in the arachnoid spaces in a preoperative assessment. CT is particularly important in the evaluation of bone deformities. In our study, 2 patients underwent CT evaluation, and in one of them, the posterior lipomyelomeningocele was comorbid with anterior meningocele, which could raise the possibility of an aborted Currarino syndrome because no anal imperforation was found. Currently, CT scan has been replaced by MRI in the diagnostic evaluation of occult spinal dysraphism [12] because it does not allow studying the relationships between the conus and the lipoma.
MRI is considered as a gold standard in the diagnosis of the tethered spinal cord. It shows the existence of intra- or extra-dural lipoma and its anatomical connections [2, 13, 14]. The lipoma appears at T1 sequence as a spontaneously hyperintense structure, isointense signal to the subcutaneous fat in T1 as in T2. The postcontrast injection sequences are of no interest because there is no modification of the signal [10]. The importance of MRI should be emphasized.
Based on Chapman’s classification, there are three anatomic patterns of conus medullaris lipoma: dorsal form, caudal form, and transitional form. Pang has described the fourth form, so-called “chaotic” form where the lipoma has engulfed all the neural structures and it is harder to differentiate between lipoma, spinal cord, and roots [15]. Neuroimaging studies along with surgical findings, lead us to describe the 7 cases of lipomyelomeningocele intra- and extra-dural with precisely 4 dorsal forms, 2 caudal forms and 2 chaotic forms. Only one filum terminale lipoma was found.
To our experience, it is difficult to predict the preoperative and accurate outcome based only on MRI findings as well as the type of attachment of the lipoma to the cord interface and dorsal root entry, which means further investigation needs to be done in this regard. Indications for operation are still controversial, but because of no neurophysiological monitoring during operation, we choose the safe option of subtotal resection of the lipoma and reconstruction of the different layers. In fact, operation stops the progressive deterioration instead of curing the disease.
5. Conclusion
Tethered spinal cord with lipoma is not common. It is often discovered through clinical signs. Imaging techniques play a fundamental role in such conditions. MRI is the key examination strategy to confirm the diagnosis and study the relationship between lipoma and conus medullaris. X-ray and CT scan are mainly used to study the associated bone malformations.
Complete removal of lipoma is dangerous because it could lead to severe neural structure damage thus it is better to leave in place a remnant of lipoma in the proximity of the roots and cord than to remove the whole lipoma, also to untether the caudal pole and make a tight dura mater closure without compression of neural structures.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information; Moreover, They were allowed to leave the study whenever they wish, and if desired, the results of the research would be available to them.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed in designing, running, and writing all parts of the research.
Conflict of interest
The authors declared no conflict of interest.
References
Chapman PH. Congenital intra spinal lipoma: Anatomic considerations and surgical treatment. Childs Brain. 1982; 9(1):37-47. [PMID]
Saidi R, Farhane S, Touffahi M, Saad H. [Attached cord syndrome: An unusual cause of bladder dysfunction in adults (French)]. Urology Annals. 2003; 37(4):187-93. [DOI:10.1016/S0003-4401(03)00046-9]
Yamada S, Won DJ, Pezeshkpour G, Yamada BS, Yamada SM, Siddiqi J, et al. Pathophysiology of tethered cord syndrome and similar complex disorders. Neurosurgical Focus. 2007; 23(2):1-10. [DOI:10.3171/FOC-07/08/E6] [PMID]
Zerah M, Roujeau T, Catala M, Pierre-Kahn A. Spinal lipoma. In: Özek MM, Cinalli G, Maixner W, editors. Spina Bifida Management and Outcome. Berlin: Springer; 2008.
Xenos C, Sgouros S, Walsh R, Hockley A. Spinal lipomas in children. Pediatric Neurosurgery. 2000; 32(6):295-307. [DOI:10.1159/000028958] [PMID]
Sakho Y, Badiane SB, Kabre A, Ba S, Ba MC, Gueye EM, et al. Lumbosacral intraspinal lipomas associated or not with a tethered cord syndrome (Series of 8 cases). Dakar Medical. 1998; 43(1):13-20. [PMID]
Kasliwal MK, Mahapatra AK. Surgery for spinal cord lipomas. The Indian Journal of Pediatrics. 2007; 74(4):357-62. [DOI:10.1007/s12098-007-0060-8]
Tseng JH, Kuo MF, Tu YK, Tseng MY. Outcome of untethering for symptomatic spina bifida occulta with lumbosacral spinal cord tethering in 31 patients: Analysis of preoperative prognostic factors. The Spine Journal. 2008; 8(4):630-8. [DOI:10.1016/j.spinee.2005.11.005] [PMID]
EL Messaoudi YA. [Attached marrow syndrome: A rare cause of neurological bladder (about a case and review of the literature) (French)]. Journal Marocain d’Urologie. 2008; 1(10):26-9.
Venat L, Couturaud M, Negrier I, Bertin P, Moreau JJ, Boncoeur-Martel MP, et al. [An unusual case of late-onset spinal cord syndrome (French)]. Rachis. 1996; 8(5):279-82.
Chatelet-Cheront C, Houze De L’Aulnoit D, Ferrant L, Dhellemmes P, Delcroix M. [Prenatal diagnosis of an intraspinal lipoma. A case report (French)]. Journal de Gynécologie Obstétrique et Biologie de la Reproduction. 1997; 26(1):85-9. [Doi:JG-03-1997-26-1-0368-2315-101019-ART51]
Perez LM, Khoury J, Webster GD. The value of urodynamic studies in infants less than 1 year old with congenital spinal dysraphism. The Journal of Urology. 1992; 148(2):584-7. [DOI:10.1016/S0022-5347(17)36660-0]
Unsinn KM, Geley T, Freund MC, Gassner I. US of the spinal cord in newborns: Spectrum of normal findings, variants, congenital anomalies and acquired diseases. Radiographics 2000; 20(4):923-38. [DOI:10.1148/radiographics.20.4.g00jl06923] [PMID]
Patwardhan V, Patanakar T, Armao D, Mukherji SK. MR imaging findings of intramedullary lipomas. American Journal of Roentgenology. 2000; 174(6):1792-3. [DOI:10.2214/ajr.174.6.1741792] [PMID]
Pang D, Zovickian J, Oviedo A. Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode: Part I- surgical technique. Neurosurgery. 2009; 65(3):511-29. [DOI:10.1227/01.NEU.0000350879.02128.80] [PMID]
Spinal dysraphism is due to perturbation of the embryological development of the caudal neural tube and the surrounding tissues [2, 3]. Regarding the spinal lipoma, several pathophysiological hypotheses have been presented, for example, it is a neurulation disorder, a defect of induction occurring after the phenomena of neurulation. Or it could be a post-neurulation disorder related to caudal pole abnormalities [4]. Spinal lipoma has remained a rare disease. We had recorded 2.28 cases per year in our study.
In France, the incidence is estimated to be 70 new cases per year [4]. In fact, the frequency of spinal lipoma has remained uncertain because the number of asymptomatic patients is unknown. Most often, the diagnosis is easily made at birth in the setting of lumbosacral cutaneous abnormalities. In our cases, the diagnosis was made essentially in infancy based on the diagnostic criteria described in the literature [5, 6].
In one of our patients, the diagnosis was made during adulthood (30 years of age) because of the late onset of vesico-sphincter dysfunction. The pathogenesis of these delayed symptoms may be because of the fact that during body growth a slow process of stretching occurs on the conus medullaris due to its fixation [5]. However, some patients remain asymptomatic during all their life. The clinical presentation comprises a symptomatic triad; a cutaneous marker like subcutaneous lump sometimes with a dimple or caudal appendicular, neuro-orthopedic deformities, and vesico-sphincteric dysfunction which is characteristic of spinal lipoma. However, in the absence of medio-lumbar skin signs, the diagnosis is more difficult and often delayed. The disease manifests itself by the progressive appearance of a vesico-sphincteric and or neuro-orthopedic dysfunction [7, 8].
Neuroimaging plays an important role in the complete investigation of this occult dysraphism. Antenatal diagnosis of the tethered spinal cord with lipoma can be made by ultrasound examination [9]. Spinal cord ultrasound provides the relevant information on newborns’ spinal cord and on infants less than 2 months [2]. In our study, the imaging was performed on two infants and provided very accurate information on the dehiscence of the posterior arch, suggesting the low-lying cord at L5.
X-ray images of the lumbosacral spine confirmed the dehiscence of posterior lumbar and or sacral vertebral arches [5, 9]. Other vertebral bone deformities and anomalies of the spine may be found, too. However, it does not detect lipoma and spinal cord lesions. All in all, it is a good diagnostic tool in any patient with suspicion of occult dysraphism. In our series, the standard X-ray showed dehiscence of the posterior arches. According to some studies [5, 6, 10], radiography along with myelography is an essential step for the diagnosis of spinal lipoma. Currently, myelography is practically abandoned in the diagnosis of spinal lipoma because of its invasiveness. When it is performed, the myelography shows an enlargement of the dural sheath facing the vertebral bodies where the lesion is located [10].
Spinal cord ultrasound provides the relevant information on newborns’ spinal cord and on infants less than 2 months [4]. In our series, it was possible to specify the insertion of the conus medullaris at L5, to describe the anatomical pattern of the lipoma and to detect dehiscence of the lumbar posterior vertebral arches. Antenatal diagnosis of the tethered spinal cord with lipoma could be made by ultrasound examination [11].
CT of the lumbosacral spine remains interesting in the absence of MRI. The lipoma appears at CT as a low-density lesion like an additional image in the vertebral canal [10]. CT can be combined with intrathecal injection of contrast to better visualize the nerve roots in the arachnoid spaces in a preoperative assessment. CT is particularly important in the evaluation of bone deformities. In our study, 2 patients underwent CT evaluation, and in one of them, the posterior lipomyelomeningocele was comorbid with anterior meningocele, which could raise the possibility of an aborted Currarino syndrome because no anal imperforation was found. Currently, CT scan has been replaced by MRI in the diagnostic evaluation of occult spinal dysraphism [12] because it does not allow studying the relationships between the conus and the lipoma.
MRI is considered as a gold standard in the diagnosis of the tethered spinal cord. It shows the existence of intra- or extra-dural lipoma and its anatomical connections [2, 13, 14]. The lipoma appears at T1 sequence as a spontaneously hyperintense structure, isointense signal to the subcutaneous fat in T1 as in T2. The postcontrast injection sequences are of no interest because there is no modification of the signal [10]. The importance of MRI should be emphasized.
Based on Chapman’s classification, there are three anatomic patterns of conus medullaris lipoma: dorsal form, caudal form, and transitional form. Pang has described the fourth form, so-called “chaotic” form where the lipoma has engulfed all the neural structures and it is harder to differentiate between lipoma, spinal cord, and roots [15]. Neuroimaging studies along with surgical findings, lead us to describe the 7 cases of lipomyelomeningocele intra- and extra-dural with precisely 4 dorsal forms, 2 caudal forms and 2 chaotic forms. Only one filum terminale lipoma was found.
To our experience, it is difficult to predict the preoperative and accurate outcome based only on MRI findings as well as the type of attachment of the lipoma to the cord interface and dorsal root entry, which means further investigation needs to be done in this regard. Indications for operation are still controversial, but because of no neurophysiological monitoring during operation, we choose the safe option of subtotal resection of the lipoma and reconstruction of the different layers. In fact, operation stops the progressive deterioration instead of curing the disease.
5. Conclusion
Tethered spinal cord with lipoma is not common. It is often discovered through clinical signs. Imaging techniques play a fundamental role in such conditions. MRI is the key examination strategy to confirm the diagnosis and study the relationship between lipoma and conus medullaris. X-ray and CT scan are mainly used to study the associated bone malformations.
Complete removal of lipoma is dangerous because it could lead to severe neural structure damage thus it is better to leave in place a remnant of lipoma in the proximity of the roots and cord than to remove the whole lipoma, also to untether the caudal pole and make a tight dura mater closure without compression of neural structures.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information; Moreover, They were allowed to leave the study whenever they wish, and if desired, the results of the research would be available to them.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed in designing, running, and writing all parts of the research.
Conflict of interest
The authors declared no conflict of interest.
References
Chapman PH. Congenital intra spinal lipoma: Anatomic considerations and surgical treatment. Childs Brain. 1982; 9(1):37-47. [PMID]
Saidi R, Farhane S, Touffahi M, Saad H. [Attached cord syndrome: An unusual cause of bladder dysfunction in adults (French)]. Urology Annals. 2003; 37(4):187-93. [DOI:10.1016/S0003-4401(03)00046-9]
Yamada S, Won DJ, Pezeshkpour G, Yamada BS, Yamada SM, Siddiqi J, et al. Pathophysiology of tethered cord syndrome and similar complex disorders. Neurosurgical Focus. 2007; 23(2):1-10. [DOI:10.3171/FOC-07/08/E6] [PMID]
Zerah M, Roujeau T, Catala M, Pierre-Kahn A. Spinal lipoma. In: Özek MM, Cinalli G, Maixner W, editors. Spina Bifida Management and Outcome. Berlin: Springer; 2008.
Xenos C, Sgouros S, Walsh R, Hockley A. Spinal lipomas in children. Pediatric Neurosurgery. 2000; 32(6):295-307. [DOI:10.1159/000028958] [PMID]
Sakho Y, Badiane SB, Kabre A, Ba S, Ba MC, Gueye EM, et al. Lumbosacral intraspinal lipomas associated or not with a tethered cord syndrome (Series of 8 cases). Dakar Medical. 1998; 43(1):13-20. [PMID]
Kasliwal MK, Mahapatra AK. Surgery for spinal cord lipomas. The Indian Journal of Pediatrics. 2007; 74(4):357-62. [DOI:10.1007/s12098-007-0060-8]
Tseng JH, Kuo MF, Tu YK, Tseng MY. Outcome of untethering for symptomatic spina bifida occulta with lumbosacral spinal cord tethering in 31 patients: Analysis of preoperative prognostic factors. The Spine Journal. 2008; 8(4):630-8. [DOI:10.1016/j.spinee.2005.11.005] [PMID]
EL Messaoudi YA. [Attached marrow syndrome: A rare cause of neurological bladder (about a case and review of the literature) (French)]. Journal Marocain d’Urologie. 2008; 1(10):26-9.
Venat L, Couturaud M, Negrier I, Bertin P, Moreau JJ, Boncoeur-Martel MP, et al. [An unusual case of late-onset spinal cord syndrome (French)]. Rachis. 1996; 8(5):279-82.
Chatelet-Cheront C, Houze De L’Aulnoit D, Ferrant L, Dhellemmes P, Delcroix M. [Prenatal diagnosis of an intraspinal lipoma. A case report (French)]. Journal de Gynécologie Obstétrique et Biologie de la Reproduction. 1997; 26(1):85-9. [Doi:JG-03-1997-26-1-0368-2315-101019-ART51]
Perez LM, Khoury J, Webster GD. The value of urodynamic studies in infants less than 1 year old with congenital spinal dysraphism. The Journal of Urology. 1992; 148(2):584-7. [DOI:10.1016/S0022-5347(17)36660-0]
Unsinn KM, Geley T, Freund MC, Gassner I. US of the spinal cord in newborns: Spectrum of normal findings, variants, congenital anomalies and acquired diseases. Radiographics 2000; 20(4):923-38. [DOI:10.1148/radiographics.20.4.g00jl06923] [PMID]
Patwardhan V, Patanakar T, Armao D, Mukherji SK. MR imaging findings of intramedullary lipomas. American Journal of Roentgenology. 2000; 174(6):1792-3. [DOI:10.2214/ajr.174.6.1741792] [PMID]
Pang D, Zovickian J, Oviedo A. Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode: Part I- surgical technique. Neurosurgery. 2009; 65(3):511-29. [DOI:10.1227/01.NEU.0000350879.02128.80] [PMID]
Type of Study: Case report |
Subject:
Spine
Send email to the article author
| Rights and Permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |